Abstract
Background
Surgical site infections (SSIs) are infections that occur within 30 days of surgery or within 1 year in patients with implants at or around the surgical site. They are among the dangerous complications of surgical procedures that expose patients to higher costs and increase the risk of death because of severe morbidity and associated longer hospital stays. This study aimed to determine the extent and determinants of surgical site infections in surgically treated cases during the study period.
Methods
A hospital-based cross-sectional study was conducted among surgically treated patients at Dilla University Referral Hospital in the surgical department. The calculated sample size was 408, calculated using the single population proportion formula, and the required information was collected from the medical records of the study participants using checklists. Bivariate logistic regression was performed to identify candidate variables, and all candidate variables with a P-value < of 0.25 were included in multivariable logistic regression. Variables with a P-value < 0.05 were considered statically significant, and the strength of association was measured by odds ratio (OR) with 95% confidence intervals (CIs).
Result
As our finding showed magnitude of surgical site infections was 19.3%. The factors which had significant association with surgical wound infections were blood transfusion (AOR = 0.16 (0.04–0.73), hemoglobin level < 7 g/dl (AOR = 10.40 (3.39–32.49), shock (AOR = 19.09 (4.69–77.51), previous surgery (AOR = 11.53(3.73–35.61), hospitalization 7–14 days (AOR = 5.51(1.52–19.91) and hospitalization >14 days (AOR = 8.18(1.84–36.75).
Conclusion
The percentage of surgical site infections was high. Shock, low haemoglobin level, blood transfusion, previous surgery, and longer length of hospital stay were significantly related to surgical site infections.
Keywords: Blood transfusion, Hemoglobin level, Hospital stay, Surgical site infection
Highlights
-
•
Magnitude of Surgical site infection was high.
-
•
Low haemoglobin level has significant association with occurrence of surgical site infection.
-
•
Longer hospital stay has association with development of surgical site infection.
1. Introduction
Surgical site infections (SSIs) are infections that happen at or around the surgical site within 30 days of operation or within 1 year among those with implants which accounts for 20% of all Hospital-acquired infections (HAIs) with a pooled prevalence of 2.5–41.9% worldwide [1]. Low and middle-income countries are significantly affected by SSIs when compared to countries with high-income, particularly among patients in Intensive care units (ICU) [2].
SSI is one of the dangerous complications of surgical procedures that expose the patient to higher costs due to severe morbidity and associated longer hospital stays(additional 7–11 postoperative days) as well as to increase risk of death (2–11 times increased risk of death compared to post-operative patients without SSI) [1,3].
It is a preventable complication of surgery that can be achieved by practicing the recommended basic principles of infection prevention strategies like complete adherence to WHO surgical safety checklists, surgical hand washing practices, utilization of skin antisepsis over the operation field, and providing antibiotic prophylaxis before starting the procedure as well shortening the duration of the surgery and improving ventilation system [4].
Despite of improvements in operating room practices, sterilization techniques, and the best efforts of infection prevention strategies applied even in the best and well-equipped health facilities; the incidences, complications, and the burden of SSI in terms of patient morbidity, treatment costs, and mortality rates are still significantly rising [5,6].
There are several risk factors for SSI. Patient-related factors are age obesity, poor nutritional state, substances abuse, morbid illness, anemia, and elevated pre-operative or postoperative serum glucose concentration. Procedure-related factors include use of a drain, prolonged duration of the operation, significant contamination of the incision, long pre-operative, and post-operative, hospital stay, emergency operation, multi-level osteotomy, surgical resident participation in the operative procedure inadequate prophylactic antibiotic therapy [7,8].
In developing countries where resources are limited, even basic life-saving operations, such as appendectomies and cesarean sections will get infected and result in high morbidity and mortality. Indeed many studies are conducted across the globe to identify the magnitude and risk factor of SSIs, there is significant variation by incidences from region to region.
Based on currently available data, the magnitude of SSI in Ethiopia shows great variability with a range of 10.9–75% [9] and has provided limited information's regarding factors related to the development of SSI [10]. Hence generalization of these studies and bringing them into clinical practice is difficult. This study aimed to determine the magnitude and determinant factors of surgical site infections among surgically managed cases within the study period.
2. Methodology
An institutional-based cross-sectional study was conducted on patients who had surgery from July 01, 2020–June 30, 2021 in Dilla University Referral Hospital. Ethical clearance was obtained from the Institutional review board of Dilla University College of Health Science and Medicine before the start of the study. Written informed consent was obtained from each study participant and from their family for the patient whose age was <18. The study was reported in line with the STROCSS guideline [11]. This study was also registered on the research registry with the unique identification number of research registry 7356 https://www.researchregistry.com/browse-the-registry#home. All patients who had surgery and admitted to surgical ward were included in this study. A patient who has an implant and the one who got an operation in other hospitals besides came with complications of the surgeries were excluded from the study.
Data were collected by four BSc Nurses and two health officers after giving training for them. A pre-test was conducted on 5% of the sample size. Depending on the result of the pretest, correction and modification were done on the checklist before applying to the study subjects.
The required information was collected from the patient's medical charts using a structured checklist which contains socio-demographic characteristics of the subjects, diagnosis at presentation, type of anesthesia, and laboratory data. During data collection, no identification of the patient's information was collected.
For this study, the following definitions were used:
SSI: A surgeon's diagnosis of infection, or deliberately re-opened the wound, or any history of wound care given.
-
➢
Class I wound (clean) - no inflammations, the respiratory, alimentary, genital, or urinary tracts are not entered.
-
➢
Class II wound (Clean-contaminated) - no evidence of infection, respiratory, alimentary, genital, or urinary tract is entered under controlled conditions
-
➢
Cass III wound (Contaminated) - Inflammation is encountered. All accidental wounds
-
➢
Class IV wound (Dirty or infected) - Old delayed >6 h traumatic wounds with retained devitalized tissue, perforated viscera.
-
➢
Superficial SSI (skin/subcutaneous) - Purulent drainage (pus) from superficial incision or organism identified (if culture done)
Deep SSI (fascia/muscle) - Purulent drainage (pus) from the deep incision or deep incision dehiscence or deep infection/abscess found on imaging/examination.
Organ/space SSI - Deeper than fascia/muscle purulent drainage (pus) from organ or space (from an inserted drain) or organ or space infection/abscess found on imaging/examination.
2.1. Sample size determination
The Sample size was determined by taking previous study results which showed a 19.1% prevalence of SSIs [12].
By considering 95% confidence interval and 4% margin of error 371 participants were considered. By adding a 10% non-response rate a total of 408 patients were selected using a simple random sampling method.
2.2. Data processing and analysis
Data were checked manually for completeness and then coded and entered into EPI info version 7 then transferred to SPSS version 20 computer program for analysis. Categorical variables were summarized as numbers and percentages. Bivariate logistic regression analysis was run to identify association and those variables with a p-value less than or equal to 0.25 were considered candidates for multivariable logistic regression. The strength of statistical association was measured by odds ratios (OR) with a 95% confidence interval and variables with P-value, less than 0.05 were considered as statistically significant.
3. Result
3.1. Socio-demographic and personal characteristics
From the total of 408 samples that fulfilled the inclusion criteria, 9.6% of the subjects were excluded because of incomplete information, and data of 373 samples were analyzed. Among 373 patients 221 (59.2%) were males. The median age of the patients was 42 with an IQR of 20 years. Of 373 patients 45 (12.1%) had a habit of drinking alcohol while 13 (3.4%) were smokers. Twenty-nine (7.8%) patients had co-morbidities, from which 6 (20.7%) were with Diabetic mellitus, 12 (41.4%) with Hypertension, 4 (13.8%) HIV/AIDS and 7 (24.1%) were with others (Table 1).
Table 1.
Socio-demographic and personal characterstics patient admitted to surgical wards of Dilla University Referral Hospital, 2021.
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Age | <19 | 30 | 8.0% |
| 19–64 | 271 | 72.7% | |
| >64 | 72 | 19.3% | |
| Sex | Male | 221 | 59.2% |
| Female | 152 | 40.8% | |
| Alcohol | Yes | 45 | 12.1% |
| No | 324 | 86.9% | |
| Not recorded | 4 | 1.1% | |
| Smoking | Yes | 13 | 3.5% |
| No | 356 | 95.4% | |
| Not recorded | 4 | 1.1% | |
| Past medical illness | Yes | 29 | 7.8% |
| No | 333 | 89.3% | |
| Not recorded | 11 | 2.9% | |
| Type of past medical illnesses(n = 29) | DM | 6 | 20.7% |
| Hypertension | 12 | 41.4% | |
| HIV | 4 | 13.8% | |
| Other | 7 | 24.1% |
3.2. Pre-operative charactersitcs of study participants
As finding of this study showed 187 (50.1%) of the patients had a hemoglobin level of >10 g/dl, while 86 (23.1%) of them had hemoglobin levels below 7 g/dl. Seventy-nine (21.2%) patients had systolic blood pressure records below 90 mmHg, and 48 (12.9%) of patients under study had blood transfusions. 19 (21.4%) patients had a history of previous surgery, and 321 (83.1%) of the operations were done for emergency indications. All of the patients under study had received prophylactic antibiotics, 184 (49.3%) and 179 (48%) of them received both ceftriaxone and metronidazole (Table 2).
Table 2.
Pre-operative characterstics of patients admitted to surgical wards of Dilla University Referral Hospital, 2021.
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Hemoglobin | <7 | 79 | 21.2% |
| 7–10 | 100 | 28.7% | |
| >10 | 187 | 50.1% | |
| Shock | Yes | 79 | 21.2% |
| No | 294 | 78.8% | |
| Blood transfusion | Yes | 48 | 12.9% |
| No | 325 | 87.1% | |
| Time of transfusion(n = 48) | Pre-Operative | 14 | 29.2% |
| Intraoperatively | 15 | 31.3% | |
| Post Operatively | 19 | 39.5% | |
| Prophylactic antibiotics given | Yes | 373 | 100% |
| No | 0 | 0% | |
| Type of antibiotics given | Ceftriaxone | 184 | 49.3% |
| Ceftriaxone and Metronidazole | 179 | 48.0% | |
| Others | 10 | 2.7% | |
| History of previous surgery | Yes | 90 | 24.1% |
| No | 283 | 75.9% | |
| Nature of operation | Elective | 52 | 13.9% |
| Emergency | 321 | 86.1% |
The majority of pre-operative diagnoses were peritonitis 176 (47.18%). Fig. 1.
Fig. 1.
preoperative diagnosis of patients admitted at the surgical ward of Dilla University Referral Hospital, 2021.
3.3. Intraoperative charactersitcs of study participants
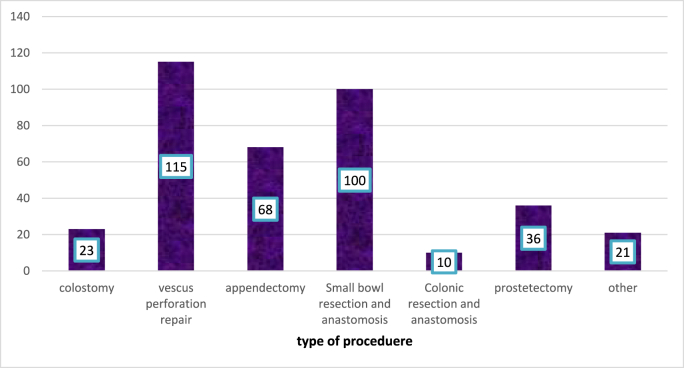
Among the total of 373 patients who underwent surgery, 297 (79.6%) of them are done under general anesthesia while 76 (20.4%) of the procedures are done under spinal anesthesia, from the total of the procedures 210 (56.3%) of them are done on dirty wounds, about 361 (96.8%) surgeries have taken more than 1 hour, and in all cases, the WHOs instrument count checklist has filled (Table 3). The most commonly done procedure was viscous perforation repair 115 (30.83%). Fig. 2.
Table 3.
Intraoperative factors at the surgical ward of Dilla university Referral Hospital, 2021.
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Type of anesthesia used | General | 297 | 79.6% |
| Spinal | 76 | 20.4% | |
| Class of the wound | Clean | 19 | 5.1% |
| Clean Contaminated | 53 | 14.2% | |
| Contaminated | 91 | 24.4% | |
| Dirty | 210 | 56.3% |
Fig. 2.
Type of procedures done at Dilla University Referral Hospital, 2021.
3.4. Post-operative charactersitcs of study participants
In this study, 72 (19.3%) of the patients had developed SSI (Fig. 3), from which 44 (62.9%) had superficial SSIs, 22 (31.4%) had deep, the rest 4 (5.7%) of them had organ space or post-operative collections and drain was used in 236 (63.3%) cases and most cases 116 (49.2%) kept for 3–6 days while it was removed within three days in 94 (39.8%). wound care is given for all cases with SSI, in most cases 32 (43.2%) wound care was given daily, From total patients about 315 (84.5%) stayed for 7 days in the hospital, while only 8 (2.1%) of the patients stayed for more than 14 days (Table 4).
Fig. 3.
prevalence of Surgical site infection in surgical ward of Dilla University Referral Hospital 2021.
Table 4.
Postoperative characterstics of patients admitted to surgical wards of Dilla University Referral Hospital, 2021.
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Type of SSI | Superficial | 46 | 63.9% |
| Deep | 22 | 30.6% | |
| Organ space | 4 | 5.5% | |
| Wound care given | Yes | 72 | 19.3% |
| No | 301 | 80.7% | |
| Frequency of wound care(n=72) | Every other day | 24 | 33.4% |
| Daily | 33 | 43.8% | |
| Twice a day | 15 | 20.8% | |
| Drain used | Yes | 236 | 63.3% |
| No | 137 | 36.7% | |
| Duration of drain used(n=236) | <3 | 94 | 39.8% |
| 3-6 | 116 | 49.2% | |
| >6 | 26 | 11.0% | |
| Total Duration of hospital stay | <8 | 287 | 76.9% |
| 8-14 | 56 | 15.0% | |
| >14 | 30 | 8.1% |
Determinants of surgical site infections
3.5. Determinants of surgical site infections
Bivariate logistic regression shows, variables associated with the occurrence of SSIs at p < 0.25, are hemoglobin level, shock(systolic blood pressure record of <90), blood transfusion, previous surgery, class of wound, and duration of hospital stay more than 7 days were associated with the occurrence of SSIs.
As a result of multivariable logistic regression analysis, showed hemoglobin level, Systolic blood pressure record of <90, blood transfusion, previous surgery, and duration of hospital stay were significantly associated with the occurrence of SSIs. Patients with blood transfusion were 84% less likely to develop SSIs compared with patients who didn't transfused (AOR = 0.16 (0.04–0.73), and Hemoglobin levels below 7 g/dl were 10.4 times more likely to develop SSI (AOR = 10.40 (3.39–32.49), and Patients with pre-operative shock were 19.1 times more likely to develop SSIs compared to patients with no record of shock (AOR = 19.09 (4.69–77.51). patients who had previous surgery were 11.5 times more likely to develop SSIs compared to patients who had no history of surgery (AOR = 11.53 (3.73–35.61) and patients who stayed in the hospital for 7–14 days in total were 5.5 times more likely to develop SSIs compared to patients who stayed less than 7 days (AOR = 5.51 (1.52–19.91) and those stayed for more than 14 days were 8.2 times more likely to develop SSI (AOR = 8.18 (1.84–36.75) (Table 5).
Table 5.
Bivariable and multivariable analysis for factors associated with Surgical site infection at the surgical ward of Dilla University Referral Hospital, 2021.
| Variable | Category | COR | p-value | AOR | p-value |
|---|---|---|---|---|---|
| Hemoglobin | <7g/dl | 21.42 (10.26-44.78) | 0.00 | 10.40 (3.39-32.49) | 0.00 |
| 7-10 | 2.02 (0.88-4.59) | 0.09 | 1.10 (0.32-3.85) | ||
| >10 | 1 | 1 | |||
| Blood transfusion | Yes | 1 | 1 | ||
| No | 0.03 (0.01-0.059) | 0.00 | 0.16 (0.036–0.727) | 0.017 | |
| The total duration of hospital stay | <7 | 1 | 1 | ||
| 7-14 | 6.01 (3.17-11.35) | 0.00 | 5.51 (1.52 - 19.91) | 0.009 | |
| >14 | 5.69 (2.54-12.74) | 0.00 | 8.18 (1.84 -36.75) | 0.006 | |
| Shock | Yes | 26.38 (13.78-50.53) | 0.00 | 19.09 (4.69–77.58) | 0.00 |
| No | 1 | 1 | |||
| Wound class | Clean | 1 | 1 | ||
| Clean contaminated | 0.77 (0.206-2.859) | 0.693 | 2.54 (0.339-18.994) | 0.365 | |
| contaminated | 0.084 (0.014-0.501) | 0.007 | 0.15 (0.339-18.994) | 0.101 | |
| Dirty | 1.40 (0.445-4.386) | 0.567 | 2.34 (0.382-4.321) | 0.358 | |
| History of previous surgery | Yes | 6.72 (3.60-10.93) | 0.00 | 11.53 (3.73-35.61) | 0.00 |
| No | 1 | 1 |
4. Discussion
Surgical site infections are the most common form of hospital-acquired infections after surgical procedures, affecting approximately 1.2–23.6 per 100 surgical procedures worldwide. Although various prevention strategies are used, SSIs continue to affect large numbers of patients and families, which is reflected in patient morbidity mortality and rising treatment cost. Patients with SSIs who are frequently exposed to various antibiotics over an extended period develop resistance to the most commonly used broad-spectrum antibiotics.
The result of this study showed that out of a 373 patients who underwent surgical intervention, 19.3% (72) of the patients developed SSI. The result of this study is comparable to the studies from the Central African Republic and Hawassa, which showed a prevalence of 18% and 19.1%, respectively [13,14]. However, the results of this study were higher than similar studies conducted in Cameroon (9.16%), South Africa (12%), and Wolayita Sodo university referral hospital (13%). This could be due to the fact that these studies were performed only in elective procedures, whereas in our study we included both elective and emergencies procedures [[15], [16], [17]].
In our study, previous surgery, shock (systolic blood pressure<90), blood transfusion, low hemoglobin level, and longer duration of hospital stay were factors associated with SSIs.
Patients who had already undergone surgery were 11.5 times more likely to develop SSIs than patients who had not undergone surgery (AOR = 11.53 (3.73–35.61), which may be due to the longer duration of surgery and associated blood loss. Patients with hemoglobin levels below 7 g/dl were 10.4 times more likely to develop SSI than those patients with hemoglobin levels above 7 g/dl (AOR = 10.40 (3.39–32.49). The result is consistent with the study conducted at the Basel University Hospital in Switzerland to determine the association of perioperative blood transfusions and preoperative anemia with the occurrence of SSI [18]. This suggests that preoperative optimization of hemoglobin levels and shortening the duration of surgery significantly reduces the risk of SSI.
Patients who stayed in the hospital for a total of 7–14 days were 5.5 times more likely to develop SSI than those who stayed less than 7 days (AOR = 5.51 (1.52–19.91), whereas patients who stayed in the hospital for more than 14 days were 8.2 times more likely to develop SSI than those who stayed for <7 days (AOR = 8.18 (1.84–36.75), which is consistent with a study from another area [8]. This suggests that a longer hospital stay increases the risk of surgical site infection. Patients with preoperative shock were 19.1 times more likely to develop SSI than those without shock (any evidence of systolic blood pressure <90mmg) (AOR = 19.09(4.69–77.51) and patients who received a blood transfusion were 84% less likely to develop SSI (AOR = 0.16 (0.04–0.73). The results are consistent with a study from Switzerland on the physiologic states that determine the risk of SSI and suggest that early treatment or prevention of shock can significantly reduce SSI(18).
In contrast to other studies, our study showed a significant association between SSI and use of a drain, prolonged duration of surgery, inadequate prophylactic antibiotic therapy, poor wound care, and smoking, [19,20].
Extreme age, obesity, uncontrolled diabetes, retroviral infections(HIV) and malignancies, preoperative anemia, surgery under emergency conditions, especially in patients with shock, were noted as some of the common conditions leading to SSI in the study conducted in Tanzania [5]. Our result showed that low hemoglobin levels or anemia and shock had a significant association with SSI, while age, comorbidity, and type of surgery had no significant association with SSIs.
Limitation: since it is secondary data due to fearing of some missed information we excluded were forced to excluded some data's.
5. Conclusion
The magnitude of SSIs is 19.3%, which is high compared with most of the similar studies, although all infection prevention strategies are applied according to national infection prevention and control guidelines. Previous surgery, shock, low hemoglobin, blood transfusion, and prolonged hospital stay were associated with a high risk of SSI. Attention should be given to early and appropriate management of shock, optimization of hemoglobin levels before surgery, and also to the management of patients who have had previous surgery.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Abbreviations
AOR Adjusted odds ratio, CDC Center for disease control, CRS Colorectal surgery, DURH Dilla university referral hospital, ICU Intensive care unit, IPP Infection prevention practice, LMIC Low and middle-income countries, SPSS Statistical package for social science, SSI surgical site infections.
Please state any sources of funding for your research
Dilla University funded the study but the university have no role in collection, analysis and interpretation of data.
Ethical approval
Ethical approval was secured from Dilla University institutional review board.
Consent
Informed consent was obtained from all study participants and from parent before data were collected. Participant’s privacy was kept confidential.
Author contribution
All author made substantial contributions to conception, design, analysis, and interpretation of data, participated in the critical review, editing of the manuscript drafts for scientific merit and depth as well as on preparing the manuscript to this study.
Registration of research studies name of the registry
Name of the registry:
Unique Identifying number or registration ID: 7356
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Timsel Girma
Declaration of competing interest
None
Acknowledgments
The authors would like to acknowledge Dilla University for technical support and encouragement in carrying out the project.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104324.
Contributor Information
Azaria Birhanu, Email: gazebirhanu@gmail.com.
Hiwot Hailu Amare, Email: hiwothailu14@yahoo.com.
Mintesinot G/Mariam, Email: mintesurg@gmail.com.
Timsel Girma, Email: timsikebron15@gmail.com.
Muhiddin Tadesse, Email: muhiddinhassen@gmail.com.
Dawit Getachew Assefa, Email: dawit.getachew@aau.edu.et.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.WHO. Preventing Surgical Site Infections: Implementation Approaches for Evidence-Based Recommendations. 2018. [Google Scholar]
- 2.Gulland A. WHO launches global guidelines to stop surgical site infections. Br. Med. J. 2016;355 doi: 10.1136/bmj.i5942. [DOI] [PubMed] [Google Scholar]
- 3.Mawalla B., Mshana S.E., Chalya P.L., Imirzalioglu C., Mahalu W. Predictors of surgical site infections among patients undergoing major surgery at Bugando Medical Centre in Northwestern Tanzania. BMC Surg. 2011;11:21. doi: 10.1186/1471-2482-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sway A., Solomkin J.S., Pittet D., Kilpatrick C. Methodology and background for the world health organization global guidelines on the prevention of surgical site infection. Surg. Infect. 2018;19(1):33–39. doi: 10.1089/sur.2017.076. [DOI] [PubMed] [Google Scholar]
- 5.Mawalla B., Mshana S.E., Chalya P.L., Imirzalioglu C., W M. Predictors of surgical site infections among patients undergoing major surgery at Bugando medical Centre in Northwestern Tanzania. BMC Surg. 2011;11(1):21. doi: 10.1186/1471-2482-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toru M., Beyene G., Kassa T., Gizachew Z., Howe R., Yeshitela B., et al. Prevalence and phenotypic characterization of Enterococcus species isolated from clinical samples of pediatric patients in Jimma University Specialized Hospital, south west Ethiopia. BMC Res. Notes. 2018;11(1):281. doi: 10.1186/s13104-018-3382-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alamanda V.K., Springer B.D. Perioperative and modifiable risk factors for periprosthetic joint infections (PJI) and recommended guidelines. Curr. rev. musculoskel. med. 2018;11(3):325–331. doi: 10.1007/s12178-018-9494-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wojcik B.M., Han K., Peponis T., Velmahos G., Kaafarani H.M.A. Impact of intra-operative adverse events on the risk of surgical site infection in abdominal surgery. Surg. Infect. 2019;20(3):174–183. doi: 10.1089/sur.2018.157. [DOI] [PubMed] [Google Scholar]
- 9.Mulu W., Kibru G., Beyene G., Damtie H. Associated risk factors for postoperative nosocomial infections among patients admitted at Felege Hiwot Referral Hospital, Bahir Dar, Northwest Ethiopia. Clin. Med. Res. 2013;2(6):140–147. [Google Scholar]
- 10.Afenigus A., Shbabawu A., Melese T. Surgical site infection and associated factors among adult patients admitted in west and east Gojjam zone hospitals, Amhara region. Ethiopia Nurse Care Open Acces. J. 2019;6(3):107–112. [Google Scholar]
- 11.Mathew G., Agha R. Strocss 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Ann. med. surg. 2012;72 doi: 10.1016/j.amsu.2021.103026. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laloto T.L., Gemeda D.H., Abdella S.H. Incidence and predictors of surgical site infection in Ethiopia: prospective cohort. BMC Infect. Dis. 2017;17(1):1–9. doi: 10.1186/s12879-016-2167-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bercion R., Gaudeuille A., Mapouka P.A., Behounde T., Guetahoun Y. [Surgical site infection survey in the orthopaedic surgery department of the "Hôpital communautaire de Bangui," Central African Republic] Bull. Soc. Pathol. Exot. 1990;100(3):197–200. 2007. [PubMed] [Google Scholar]
- 14.Legesse Laloto T., Hiko Gemeda D., Abdella S.H. Incidence and predictors of surgical site infection in Ethiopia: prospective cohort. BMC Infect. Dis. 2017;17(1):119. doi: 10.1186/s12879-016-2167-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amenu D., Belachew T., F A. Surgical site infection rate and risk factors among obstetric cases of Jimma University Specialized Hospital, Southwest Ethiopia. Ethiop. J. Health Sci. 2011;21:91–100. doi: 10.4314/ejhs.v21i2.69049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jjuuko G., Moodley J. Abdominal wound sepsis associated with gynaecological surgery at King Edward VIII Hospital, Durban. South African j. surg. Suid-Afrikaanse tydskrif vir chirurgie. 2002;40(1):11–14. [PubMed] [Google Scholar]
- 17.Awoke N., Arba A., Girma A. Magnitude of surgical site infection and its associated factors among patients who underwent a surgical procedure at Wolaita Sodo University Teaching and Referral Hospital, South Ethiopia. PLoS One. 2019;14(12) doi: 10.1371/journal.pone.0226140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weber W.P., Zwahlen M., Reck S., Misteli H., Rosenthal R., Buser A.S., et al. The association of preoperative anemia and perioperative allogeneic blood transfusion with the risk of surgical site infection. Transfusion. 2009;49(9):1964–1970. doi: 10.1111/j.1537-2995.2009.02204.x. [DOI] [PubMed] [Google Scholar]
- 19.Shiferaw W.S., Aynalem Y.A., Akalu T.Y., Petrucka P.M. Surgical site infection and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Surg. 2020;20(1):107. doi: 10.1186/s12893-020-00764-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Milne J., Vowden P., Fumarola S., Leaper D. Postoperative incision management made easy. Wounds U. K. 2012;8(4):1–4. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.