Abstract
Background
Despite the push for complementary medicine (CM) practitioners to engage in evidence implementation, and arguments in support of evidence-based practice (EBP), uptake of EBP amongst most CM professions remains low. This review aimed to synthesise the evidence examining the barriers and enablers to evidence implementation in CM.
Methods
Any primary study examining enablers and barriers to evidence implementation in CM were eligible for inclusion. Eight databases and search engines were searched for eligible studies. Reference lists of included studies were screened, and authors of included studies were contacted to identify current or unpublished studies that met the inclusion criteria.
Results
Thirty-nine published and unpublished studies were included in this review. The seven published qualitative studies and 25 published quantitative studies were rated as moderate to high quality. Fifty-two distinct barriers and 62 discrete enablers were identified. Reported barriers were predominantly structural (e.g. limited availability of time and clinical evidence) and cognitive (e.g. skills deficits), with relatively fewer studies reporting cultural (e.g. lack of industry support) or attitudinal barriers (e.g. lack of interest in, or relevance to CM). Enablers of evidence implementation largely focussed on improving access to bibliographic databases and evidence reviews, supporting skills acquisition, and cultivating leadership and interprofessional/interagency collaboration.
Conclusion
The findings of this review highlight the diverse barriers and enablers to evidence implementation in CM that span multiple dimensions. The interplay between these various factors highlights the complexity of evidence implementation, and the need for a targeted multistakeholder, multidimensional solution to optimise evidence-based practice in CM.
Keywords: Complementary medicine, Evidence-based practice, Evidence translation, Implementation science, Systematic review
1. Introduction
Health care and health service delivery have undergone considerable transformation over the past century. Several factors have contributed to these changes, including advances in diagnostic technology, improved understanding of disease aetiology and pathology, and new approaches to disease management.1 These advances have occurred alongside changes in health care resourcing, health workforce composition and scopes of practice, and the complexity of patient presentations.2 In order to keep abreast of these changes, and to ensure the provision of consistent, transparent, safe, effective, and quality care for all, governments and regulators are placing increasing pressure on health professions to deliver care informed by the best available evidence; a construct often referred to as evidence-based practice (EBP), evidence translation or evidence implementation.3,4
Evidence implementation is a “purposeful and enabling set of activities designed to engage key stakeholders with research evidence to inform decision-making and generate sustained improvement in the quality of healthcare delivery”.5 Essentially, evidence implementation endeavours to close the gap between the best available research evidence and clinical practice. Despite more than a century of discourse on the research-practice gap, there remains a disconnect between research and practice in many health disciplines,6, 7, 8 including those in the field of complementary medicine (CM).9,10
Complementary medicine (CM) represents a range of healthcare practices, technologies and knowledge systems that place considerable emphasis on wellbeing, disease prevention, health promotion and supportive treatment, and which largely sit outside the sphere of conventional medicine.11 The use of CM is widespread, with CM prevalence rates in some populations exceeding eighty percent.12, 13, 14 Given the popularity of CM, and increasing public scrutiny regarding CM safety, effectiveness, and professional accountability,15,16 it is not surprising then that CM practitioners are under increasing pressure to implement evidence into their practices.17
Despite the push for CM practitioners to engage in evidence implementation, and the arguments in support of evidence-based practice, the uptake of EBP amongst most CM professions remains low.18, 19, 20, 21 Drawing upon the field of implementation science, it is likely that a range of factors may be contributing to the low level of EBP uptake in CM. These factors can be broadly categorised as attitudinal (e.g., beliefs), structural (e.g., time, access to resources), cognitive (e.g., skill level, self-efficacy) or cultural (e.g., philosophical alignment, availability of clinical evidence) in nature.22
While several studies have examined the factors impacting EBP uptake in the field of complementary medicine, there is currently no synthesis of the evidence examining the barriers and enablers to evidence implementation in CM. Such a synthesis would provide a clearer understanding of the state of the art, including key knowledge gaps; and in doing so, would help better inform CM policy, education, research, and practice relevant to this issue.23 A synthesis of the evidence (such as that reported in this paper) would also play a pivotal role in shaping the development of future strategies aimed at improving evidence implementation in CM, which would in turn, support improvements in the quality of CM care, including patient outcomes.
2. Methods
2.1. Design
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The review protocol was registered with PROSPERO (CRD42022308527). The objective of this review was to synthesise the evidence on the reported enablers and barriers to evidence implementation in complementary medicine.
2.2. Selection criteria
This review considered any primary study (quantitative or qualitative, published, or unpublished) examining the enablers and barriers to evidence implementation in complementary medicine. For the purposes of this review, evidence implementation was defined as the process of moving findings or guidance from evidence-based resources (e.g., research articles or clinical guidelines) into clinical practice.24 The population of interest, complementary medicine providers, encompassed health professionals that administer “a broad set of health care practices that are not part of that country's own tradition or conventional medicine and are not fully integrated into the dominant health-care system”.25 These service providers included (but were not necessarily limited to): acupuncturists, ayurvedic medicine practitioners, chiropractors, herbalists, homeopaths, kinesiologists, massage therapists, myotherapists, naturopaths, nutritionists, osteopaths, reflexologists, reiki practitioners, Tai Chi practitioners, traditional Chinese medicine practitioners, and yoga therapists.26 Excluded from the review were secondary studies (e.g., systematic reviews), editorials, commentaries, case reports, opinion pieces, conference abstracts, and intervention studies examining the effectiveness of strategies aimed at addressing barriers to evidence implementation.
2.3. Outcomes
The primary outcomes of this review were the barriers and enablers to evidence implementation. We defined barriers and enablers as any factor that has a negative or positive impact, respectively, on a complementary medicine provider's ability to engage in evidence implementation. These barriers/enablers may be attitudinal (e.g., beliefs), structural (e.g., time, access to resources), cognitive (e.g., skill level, self-efficacy) or cultural (e.g., philosophical alignment, availability of clinical evidence) in nature.
2.4. Search strategy
The following electronic bibliographic databases were searched for eligible studies (from inception to February 2022): MEDLINE, CINAHL, EMBASE, AMED and ProQuest Health & Medical Collection. Relevant dissertations were identified using ProQuest Dissertations and Theses. A Google Scholar search was also undertaken, with the number of results limited to the first ten pages. The reference lists of included studies were screened for eligible publications also. In addition, the authors of included studies were contacted to identify any current or unpublished studies that met the inclusion criteria. There were no limits to the date or language of publication. The search terms and combinations are provided in Supplementary file.
2.5. Screening
The search results were initially imported into EndNote X9 (Clarivate, Philadelphia, Pennsylvania) for duplicate removal, and subsequently imported into Covidence (Veritas Health Innovation, Melbourne, Australia) for screening. Title and abstract screening, and full-text screening, were undertaken by two reviewers (ML and YV). Disagreements were resolved by discussion.
2.6. Data extraction
Pertinent data from included studies were extracted using an a priori, customised, and piloted data extraction tool. Information collected by the tool included: author, year, country, study design, discipline, participants (e.g., sample size, demographic characteristics), data collection method/tool, barriers to evidence implementation, and enablers of evidence implementation. Data extraction was undertaken by ML and YV, independently, with any disagreements resolved by discussion.
2.7. Critical appraisal
The quality of included studies was assessed by ML and YV, independently, using one of two appraisal tools, depending on study design. Qualitative studies were appraised using the Critical Appraisal Checklist for Qualitative Research Studies (CACQRS).27 The CACQRS comprises 10 items, addressing constructs such as study purpose, rationale for approach, conceptual framework, ethical implications, sampling strategy, data collection and procedures, data organisation, data analysis methods, reliability and validity, and conclusions. Each item was scored as either 1 (criterion met) or 0 (criterion not met or unclear), with total score representing the mean of all items.
The McMaster Critical Review Form for Quantitative Studies (MCRFQS) was used to appraise quantitative studies.28 The 15-item MCRFQS assessed the following constructs: study purpose, background literature, design, sample, outcomes, intervention, results, and conclusions. Each item was rated as either 1 (criterion met), 0 (criterion not met or unclear) or NA (not applicable), with the mean of all items generating a total score.
2.8. Data analysis
Given the descriptive nature of the review outcomes, extracted data were synthesised in narrative form. The reviewers deliberated on a range of implementation science frameworks/theories to guide the data analysis; however, existing frameworks/theories were deemed inappropriate for this review as they were either too complex, ambiguous, intervention-focussed, or misaligned with the extracted data. Accordingly, the extracted barriers and enablers were aligned with, and reported against, the four categories of barriers/enablers (i.e., attitudinal, structural, cognitive, cultural) defined in previous work examining implementation science in complementary medicine.42 Data within each of the four categories were reviewed and coded to identify appropriate subthemes. Data were subsequently sorted and reported against each of these subthemes (where appropriate) to aid analysis and interpretation.
3. Results
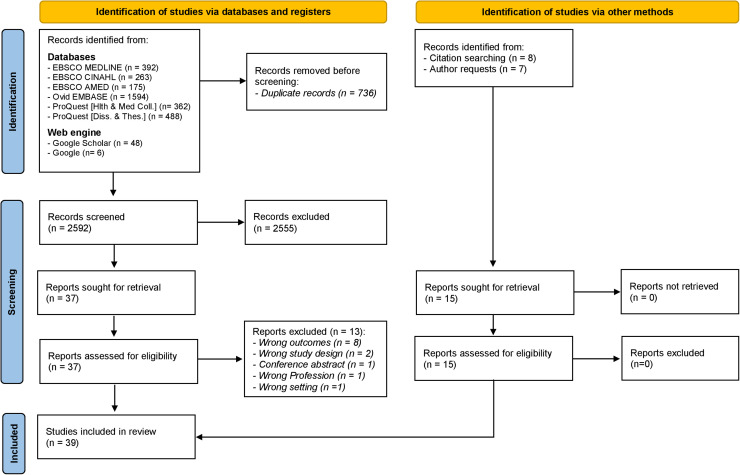
The search of databases, web engines and other methods (i.e., citation searching and author requests) identified 3343 records (Fig. 1). After the removal of duplicates (n = 736) and ineligible records at the title/abstract screening stage (n = 2555), 52 reports remained and underwent full-text screening. Thirteen reports were excluded (for reasons outlined in Fig. 1), resulting in a total of 39 studies (including 32 published studies18, 19, 20, 21,29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56 and 7 unpublished studies)57, 58, 59, 60, 61, 62, 63 being included in this review.
Fig. 1.
PRISMA Flow Diagram.
3.1. Characteristics of included studies
The 39 included studies were published between 2002 and 2022 (Supplementary file). The studies were conducted across 12 countries, primarily Australia (28.2%), USA (18.0%), Canada (12.8%) and UK (10.3%). Thirty-two (82.1%) studies were quantitative (of which 96.9% used a survey design), and 7 (18.0%) were qualitative (with all reporting ambiguous study designs, and 42.9% reporting the use of interviews). The most frequently reported data collection tool was the Evidence-Based practice Attitude and utilization SurvEy (EBASE; 53.9% of all studies).
The 39 included studies recruited a total of 10,384 participants, with a median sample size of 174 (range 8 to 1314) (Supplementary file). Included studies recruited participants from 20 distinct CM disciplines; chiropractic (10 [25.6%] studies), osteopathy (8 [20.5%] studies), and naturopathy (7 [18.0%] studies) were the most frequently investigated disciplines. Approximately one-half of participants were female (median 49%, range 9% to 91%), and reportedly held a post-graduate degree (median 45%, range 0.3% to 76%). In relation to participant age, 15 (38.5%) studies indicated most participants were aged between 30 and 49 years, and 11 (28.2%) studies indicated most participants were aged between 40 and 59 years.
3.2. Quality of included studies
Overall, the seven published qualitative studies were deemed to be of moderate-high quality, with total CACQRS scores ranging between 0.70–0.90 (median 0.76) (Table 1). All published qualitative studies reported the purpose of the study, rationale for the approach, sampling strategy, data collection procedures, data organisation procedures, data analysis methods, and the progression from research question to conclusions. Less than one-half of studies reported the conceptual framework (28.6%) and ethical implications (42.9%), and no studies reported the threats to reliability and validity. It was not possible to appraise the unpublished studies as these were primarily datasets or summaries of results, rather than manuscripts.
Table 1.
Critical appraisal of included qualitative studies (n = 7).
| Author (date) | Study purpose | Rationale for approach | Conceptual framework | Ethical implications | Sampling strategy | Data collection | Data organisation | Data analysis | Reliability & validity | Conclusions | Total Score* |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Canaway et al. (2018)32 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0.70 |
| Goldenberg et al. (2017)33 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0.90 |
| Lawrence et al. (2008)36 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0.70 |
| Leach et al. (2018)39 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0.70 |
| Spence and Li (2013)46 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0.80 |
| Wong et al. (2021)55 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0.80 |
| Woo and Cho (2012)56 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0.70 |
Scoring: Studies were assessed using the Critical Appraisal Checklist for Qualitative Research Studies. Each item was scored as either 1 (criterion met) or 0 (criterion not met or unclear). Total score represents the mean of all items.
Total MCRFQS scores for the 25 published quantitative studies ranged between 0.50–1.00 (median 0.87), and overall, were considered to be of moderate-high quality (Table 2). All studies reported the study purpose, study design, sample characteristics, sample size, clinical importance, and appropriate conclusions. Most studies reported relevant background literature (92%), the statistical significance of results (76%), and an appropriate method of analysis (84%), and most used a valid (84%) and reliable (84%) outcome measure. Few studies (28%) reported dropouts (i.e., number/proportion of incomplete surveys).
Table 2.
Critical appraisal of included quantitative studies (n = 32).
| Author (date) | Study purpose | Background literature | Study design | Description of sample | Sample size | Outcome measure reliable | Outcome measure valid | Description of intervention | Contamination avoided | Cointervention avoided | Statistical significance reported | Appropriate analysis | Clinical importance reported | Drop-outs reported | Appropriate conclusions | Total Score* |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PUBLISHED STUDIES | ||||||||||||||||
| Alcantara et al. (2015)29 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Alvarez et al. (2021)30 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 1 | 1 | 1.00 |
| Braun et al. (2013)31 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Bussieres et al. (2015)18 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Cerritelli et al. (2021)19 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Gowan-Moody et al. (2013)34 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.75 |
| Hadley et al. (2008)35 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.75 |
| Hu et al. (2004)37 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 0 | 1 | 1 | 0 | 1 | 0.75 |
| Kim and Cho (2014)20 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | NA | NA | NA | 0 | 0 | 1 | 0 | 1 | 0.50 |
| Leach (2022)42 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 1 | 1 | 1.00 |
| Leach and Gillham (2011)38 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 1 | 1 | 1.00 |
| Leach et al. (2019)21 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 1 | 1 | 1.00 |
| Leach et al. (2020)40 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Leach et al. (2021)41 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Roecker et al. (2013)43 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 0 | 0 | 1 | 0 | 1 | 0.75 |
| Schneider et al. (2015)44 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 0 | 0 | 1 | 0 | 1 | 0.75 |
| Snow et al. (2017)45 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Stomski et al. (2008)47 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Stuttard (2002)48 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | NA | NA | NA | 0 | 0 | 1 | 0 | 1 | 0.67 |
| Sullivan et al. (2017)49 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.92 |
| Sundberg et al. (2018)50 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 1 | 1 | 1.00 |
| Suter et al. (2007)51 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | NA | NA | NA | 1 | 1 | 1 | 0 | 1 | 0.83 |
| Veziari et al. (2021)52 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 1 | 1 | 1.00 |
| Walker et al. (2014)53 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 0 | 1 | 1 | 0 | 1 | 0.83 |
| Weber and Rajendran (2018)54 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | NA | NA | NA | 1 | 1 | 1 | 1 | 1 | 1.00 |
| UNPUBLISHED STUDIES | ||||||||||||||||
| Leach et al. (2022a)57 | NA | NA | NA | NA | NA | 1 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Leach et al. (2022b)58 | NA | NA | NA | NA | NA | 1 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Leach et al. (2022c)59 | NA | NA | NA | NA | NA | 1 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Leach et al. (2022d)60 | NA | NA | NA | NA | NA | 1 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Leach et al. (2022e)61 | NA | NA | NA | NA | NA | 1 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Myhrvold et al. (2022)62 | NA | NA | NA | NA | NA | 1 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Pelletier et al. (2022)63 | NA | NA | NA | NA | NA | 1 | 1 | NA | NA | NA | NA | NA | NA | NA | NA | NA |
NA – Not applicable.
Scoring: Studies were assessed using the McMaster Critical Review Form for Quantitative Studies. Each item is rated as either 1 (criterion met), 0 (criterion not met or unclear) or NA (not applicable). Total score represents the mean of all items.
3.3. Barriers to evidence implementation
3.3.1. Attitudinal barriers
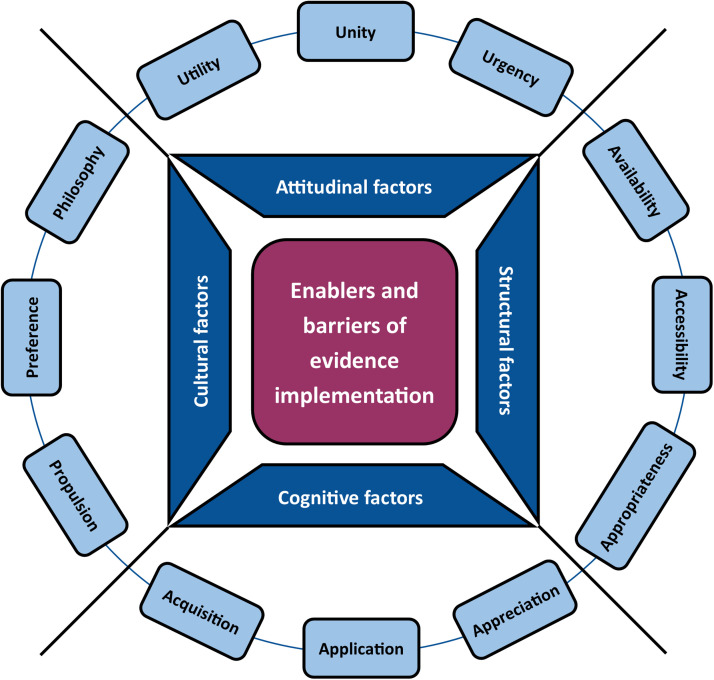
Seven included studies reported seven distinct attitudinal barriers to evidence implementation, all of which aligned with the subtheme, ‘utility’ (i.e., perceived usefulness or relevance of evidence implementation to CM) (Fig. 2; Supplementary file). The most frequently reported barriers within this subtheme were a perceived lack of relevance of EBP to CM (n = 3 studies), and a lack of interest in EBP (n = 2 studies).
Fig. 2.
Themes (dark blue boxes) and subthemes (light blue boxes) related to the enablers and barriers of evidence implementation in complementary medicine.
3.3.2. Structural barriers
Thirteen distinct structural barriers to evidence implementation were reported in 31 studies. These barriers aligned with three subthemes; ‘availability’ (i.e., opportunity to engage in evidence implementation; 3 different barriers), ‘accessibility’ (i.e., ability to acquire the best available evidence; 5 barriers) and ‘appropriateness’ (i.e., quality and suitability of the evidence for CM practice; 5 barriers) (Fig. 2; Supplementary file). In relation to availability, the two most frequently reported barriers were lack of time (n = 23 studies) and lack of clinical evidence in the field (n = 21 studies). The barriers reported most frequently within the subtheme of accessibility, were lack of resources (n = 5 studies) and limited access to databases (n = 3 studies). Limited reliability of evidence (n = 3 studies) and limited external validity of evidence (n = 3 studies) were amongst the leading barriers reported under the subtheme of appropriateness.
3.3.3. Cognitive barriers
Seventeen different cognitive barriers to evidence implementation (in 21 studies) were identified in this review; these were captured within three discrete subthemes (Fig. 2; Supplementary file). Eight different barriers were captured within the subtheme of ‘acquisition’ (i.e., attainment of knowledge and skills pertinent to evidence implementation), of which insufficient skills in critical appraisal (n = 10 studies) and insufficient skills in interpreting research (n = 8 studies) were most frequently reported. Amongst the six barriers included within the subtheme of ‘application’ (i.e., experience or perceived ability to translate and apply research findings to individual patients), the two reported most frequently were difficulty applying research findings to practice (n = 4 studies) and lack of engagement with research evidence (n = 2 studies). Limited understanding of research (n = 3 studies) and limited understanding of EBP (n = 3 studies) were amongst the leading barriers reported under the subtheme of ‘appreciation’ (i.e., awareness and understanding of research and EBP; 3 different barriers).
3.3.4. Cultural barriers
A total of fifteen cultural barriers were reported in 19 included studies. These barriers to evidence implementation were aligned with three subthemes; ‘preference’ (i.e., stakeholder proclivity for EBP in CM; 5 different barriers), ‘propulsion’ (i.e., motivation and incentivisation to engage in EBP; 4 barriers) and ‘philosophy’ (i.e., compatibility between EBP and CM philosophies, theories, and paradigms; 6 different barriers) (Fig. 2; Supplementary file). Under the subtheme of preference, the most frequently reported barriers were lack of industry support (n = 7 studies) and patient preference for a particular treatment (n = 5 studies). Lack of incentive (n = 5 studies) and lack of leadership (n = 2 studies) were amongst the leading barriers within the subtheme of propulsion. The barriers reported most frequently within the subtheme of philosophy, were fear that EBP may harm the identity/integrity of CM (n = 2 studies) and perceived incompatibility of the positivist paradigm of EBP and CM (n = 2 studies).
3.4. Enablers of evidence implementation
3.4.1. Attitudinal enablers
Thirteen different attitudinal enablers of evidence implementation (in 26 included studies) were identified in this review, which were captured within three discrete subthemes (Fig. 2; Supplementary file). Seven different enablers were captured within the subtheme of ‘utility’ (i.e., perceived usefulness or relevance of evidence implementation to CM), of which holding a belief that professional literature and research findings are useful for day-to-day practice (n = 21 studies) and holding a belief that EBP assists with clinical decision-making (n = 19 studies) were most frequently reported. Amongst the enablers included within the subtheme of ‘unity’ (i.e., harmonising practices and professional relationships; 3 different enablers) were perceiving EBP as a means of standardising care (1 enabler) and sharing positive evidence to promote interprofessional collaboration (1 enabler). Perceiving EBP as necessary in CM (n = 21 studies) was the leading enabler reported under the subtheme of ‘urgency’ (i.e., recognising evidence implementation as a priority for CM practice; 3 different enablers).
3.4.2. Structural enablers
Twenty-eight included studies reported eighteen distinct structural enablers of evidence implementation, which aligned with the subthemes of ‘accessibility’ (i.e., ability to acquire the best available evidence; 8 different enablers), ‘appropriateness’ (i.e., quality and suitability of the evidence for CM practice; 6 enablers) and ‘availability’ (i.e., opportunity to engage in evidence implementation; 4 enablers) (Fig. 2; Supplementary file). The enablers most frequently reported within the subtheme of accessibility were providing access to online databases (n = 22 studies) and providing access to the internet in the workplace (n = 20 studies). Provision of critical reviews of research evidence relevant to CM (n = 17 studies) and provision of critically appraised topics relevant to CM (n = 14 studies) were the leading enablers under the subtheme of appropriateness. For the subtheme of availability, there were no frequently reported enablers; some of the enablers reported under this subtheme included generating CM guidelines and protocols (n = 1 study) and supporting researchers in generating CM evidence (n = 1 study).
3.4.3. Cognitive enablers
A total of thirteen cognitive enablers were reported in 30 included studies. These enablers of evidence implementation were aligned with three subthemes; ‘acquisition’ (i.e., attainment of knowledge and skills pertinent to evidence implementation; 7 different enablers), ‘application’ (i.e., experience or perceived ability to translate and apply research findings to individual patients; 4 enablers) and ‘appreciation’ (i.e., awareness and understanding of research and EBP; 2 enablers) (Fig. 2; Supplementary file). Under the subtheme of acquisition, the most frequently reported enablers were a desire to improve EBP skills (n = 20 studies) and providing access to online EBP education materials (n = 18 studies). Guiding clinicians on how to translate evidence into practice (n = 2 studies) and improving clinician self-efficacy with finding and reviewing literature (n = 1 study) were the leading enablers under the subtheme of application. The enablers reported most frequently within the subtheme of appreciation, were recognising the multiple tenets of EBP (n = 2 studies) and recognising the skills required to support research utilisation (n = 1 study).
3.4.4. Cultural enablers
Eighteen distinct cultural enablers to evidence implementation were reported in 9 included studies. These enablers aligned with three subthemes; ‘preference’ (i.e., stakeholder proclivity for EBP in CM; 6 different enablers), ‘propulsion’ (i.e., motivation and incentivisation to engage in EBP; 6 enablers) and ‘philosophy’ (i.e., compatibility between EBP and CM philosophies, theories, and paradigms; 6 enablers) (Fig. 2; Supplementary file). In relation to preference, the two most frequently reported enablers were empowering consumers to be better informed, activated and interested in EBP and CM (n = 4 studies), and encouraging clinicians to collaborate with regulatory bodies and other health professions (n = 2 studies). The enablers reported most frequently within the subtheme of propulsion were providing EBP leadership (n = 4 studies), and enabling pertinent agencies (i.e., regulators, insurers) to drive changes in CM practice (n = 2 studies). Integrating EBP into the value system of educational institutions (n = 1 study) and creating an EBP method that encompasses CM theory (n = 1 study) were some of the enablers reported under the subtheme of philosophy.
4. Discussion
This is the first known review of the barriers and enablers to evidence implementation in complementary medicine. The 39 included studies were of moderate-high quality and provided data on a multidisciplinary and geographically diverse CM workforce. The review uncovered a considerable number of determinants of evidence implementation – including 52 distinct barriers and 62 discrete enablers. Most of these determinants were structural or cognitive in nature, with the remaining factors categorised as either cultural or attitudinal.
Structural factors represent major barriers to evidence implementation for most health professions64, 65, 66, 67; this was no exception for CM practitioners. Consistent with other professions,64, 65, 66, 67 ‘availability’ of time and ‘availability’ of clinical evidence were amongst the most frequently reported structural barriers. Notwithstanding, few studies in this review reported enablers specifically targeting this barrier (with suggestions limited to supporting the generation of CM evidence and CM guidelines). Rather, most included studies examining structural factors reported on enablers to improve accessibility to online bibliographic databases and the internet, and the provision of more appropriate forms of evidence (such as the provision of critical reviews or critically appraised topics relevant to CM).
While many of the abovementioned enablers may help improve perceived availability of clinical evidence, and efficiency in evidence acquisition, they do not necessarily address time constraints on evidence implementation. Disciplines outside the field of CM have proposed innovative strategies, and/or made attempts to mitigate these constraints on clinician time to improve engagement in EBP. Such strategies have included the implementation of collaborative/shared models of care, and the introduction of digital information systems and evidence-adaptive decision-support systems.68,69 Although these strategies may potentially increase efficiency in evidence implementation, it is unclear whether these strategies would be suitable, acceptable, or effective within the context of CM practice. The feasibility and effectiveness of these strategies in CM therefore warrants further investigation.
Efficiency of evidence implementation (e.g., evidence-based clinical decision-making) also may be impacted by cognitive factors, such as EBP-related knowledge, skills, and self-efficacy.70 In our review, cognitive barriers were a common determinant of evidence implementation amongst CM practitioners, with skills deficits (i.e., insufficient skills in critical appraisal and interpretation of research) reported most frequently. These barriers corresponded directly with reported enablers, which largely focussed on skills acquisition (i.e., desire to improve EBP skills, and providing access to online EBP education materials).
Attempts at facilitating evidence implementation, both in CM and other health professions, have predominantly focussed on the use of education interventions.69,71,72 Findings from these studies suggest that EBP education interventions may be effective in increasing EBP self-efficacy, as well as improving attitudes towards, and/or application of EBP.44,69,71,73 This might suggest that education alone may be sufficient in addressing many of the cognitive and attitudinal barriers to evidence implementation. While this may be the case for some disciplines (such as nursing and allied health),69,71 the evidence is weak, inconsistent and/or absent for many CM disciplines.44,73,74 There is also little evidence to suggest that EBP education interventions alone generate sustainable changes in CM practice behaviours or have any impact on structural or cultural barriers to evidence implementation. These knowledge/evidence gaps represent priorities for future research in this field.
Cultural factors (i.e., a profession's values, beliefs, customs, and ways of thinking)75 have been shown to influence health practitioner behaviours, including evidence implementation.76,77 As revealed in this review, one of the leading cultural barriers to evidence implementation in CM was lack of industry support. Given that industry (e.g. professional associations) typically provide guidance on practice standards and professional conduct, and often represent the voice of a profession, the lack of explicit industry support for evidence implementation may be not only disadvantageous to CM practice, but also potentially detrimental to the reputation of CM. Studies included in this review reported a number of strategies to circumvent this cultural barrier, including provision of EBP leadership, enabling other pertinent agencies (i.e. health insurers, government bodies) to mandate evidence-based CM practices, and fostering collaboration between CM practitioners, regulatory bodies and other health professions. While it is uncertain to what extent the latter two enabling strategies would improve the EBP culture of CM, the former shows promise, with studies of other disciplines indicating leadership has a positive influence on EBP uptake.78,79
Another cultural factor negatively impacting evidence implementation in CM was patient preference for particular treatments. This is a noteworthy finding because even though patient preference is a core tenet of EBP,80 integrating patient preference with the other tenets of EBP in clinical practice could be problematic for some CM practitioners. This tension has not gone unnoticed, with some authorities arguing that patient preference directly conflicts with the first tenet of EBP (i.e., selecting the best available evidence).81 Fortunately, the findings of this review point to a possible solution - empowering consumers to be better informed, activated and interested in EBP and CM. Although earlier work suggests that patient training in EBP fosters research appreciation, and improves patient-practitioner interactions,82 further work is required to determine whether these outcomes translate into improvements in evidence implementation in CM.
A construct closely related to culture is attitude. Previous studies have reported generally favourable attitudes toward EBP amongst CM practitioners,10,21,33,45,50 which might explain why few attitudinal barriers to evidence implementation were identified in this review. In fact, the only attitudinal barrier reported amongst CM practitioners (in seven studies) was the perceived inutility of EBP (i.e., perceived lack of relevance of EBP to CM, and lack of interest in EBP). Previous research suggests that these perceptions of EBP are multifactorial in origin, stemming from a range of cognitive (i.e., limited understanding of EBP), structural (i.e., lack of time), and cultural factors (i.e., resistance to change, threat to the integrity of CM practice, lack of leadership).33,83, 84, 85 The interplay between these various factors highlights the complexity of evidence implementation, and the need for a complex multidimensional solution to optimise EBP in CM.
Although this review was novel, comprehensive, and conducted in accordance with PRISMA guidelines, there are some limitations worth noting. The inclusion of unpublished studies may have introduced some degree of bias as the methodological quality of these studies could have been potentially lower than published studies; particularly as the quality of these unpublished studies could not be adequately assessed due to insufficient/missing information on the study methods. Notwithstanding, it has been argued that such bias is likely to be less than that introduced by excluding unpublished studies due to the increased risk of publication bias.86 Another potential source of bias is the perceived conflict of interest of reviewers, in that they were authors of several included studies. In accordance with the Cochrane Handbook,86 the reviewers mitigated this risk of bias by ensuring the review protocol was registered a priori, there were no deviations from the original protocol, and that data extraction and critical appraisal were undertaken by two reviewers, independently.
In conclusion, the findings of this systematic review highlight the multifarious barriers and enablers to evidence implementation in complementary medicine practice. These factors spanned multiple dimensions (i.e. structural, cognitive, cultural, and attitudinal), and appear to be interrelated. The interplay between these various factors highlights the complexity of evidence implementation, and the need for a targeted multidimensional solution to optimise EBP in CM. The solution also would require a well-coordinated, collaborative approach with the involvement of diverse stakeholder groups. The implementation of such a solution - if shown to be both effective and sustainable - will almost certainly contribute to improvements in the quality of CM practice, including patient outcomes.
CRediT authorship contribution statement
Matthew J. Leach: Conceptualization, Funding acquisition, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. Yasamin Veziari: Data curation, Formal analysis, Writing – original draft, Writing – review & editing.
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgments
Funding
This project was supported by a Southern Cross University Grant. The funder had no influence on the study design, data collection, data analysis, data interpretation, or manuscript preparation or submission.
Ethical statement
No ethical approval was required as this study did not involve human participants or laboratory animals.
Data availability
The data that support the findings of this study are available within the article and supplementary material.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.imr.2022.100899.
Appendix. Supplementary materials
References
- 1.Hofmann B., Svenaeus F. How medical technologies shape the experience of illness. Life Sci Soc Policy. 2018;14:3. doi: 10.1186/s40504-018-0069-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Salvatore F.P., Fanelli S. Patient-related complexity of care in healthcare organizations: a management and evaluation model. Int J Environ Res Public Health. 2020;17:3463. doi: 10.3390/ijerph17103463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Braithwaite J., Travaglia J.F. An overview of clinical governance policies, practices and initiatives. Aust Health Rev. 2008;32:10–22. doi: 10.1071/ah080010. [DOI] [PubMed] [Google Scholar]
- 4.Jylhä V., Oikarainen A., Perälä M.L., et al. World Health Organisation; Copenhagen: 2017. Facilitating Evidence-Based Practice in Nursing and Midwifery in the WHO European region. [Google Scholar]
- 5.Jordan Z., Lockwood C., Munn Z., et al. The updated Joanna Briggs Institute model of evidence-based healthcare. Int J Evid Based Healthcare. 2019;17:58–71. doi: 10.1097/XEB.0000000000000155. [DOI] [PubMed] [Google Scholar]
- 6.Battista S., Salvioli S., Millotti S., et al. Italian physiotherapists’ knowledge of and adherence to osteoarthritis clinical practice guidelines: a cross-sectional study. BMC Musculoskelet Disord. 2021;22:380. doi: 10.1186/s12891-021-04250-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Leo A., Bayes S., Geraghty S., et al. Midwives' use of best available evidence in practice: an integrative review. J Clin Nurs. 2019;28:4225–4235. doi: 10.1111/jocn.15027. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leach M.J., Tucker B. Current understandings of the research-practice gap in nursing: a mixed-method study. Collegian. 2018;25:171–179. [Google Scholar]
- 9.Leach M.J., Tucker B. Current understandings of the research-practice gap from the viewpoint of complementary medicine academics: a mixed-method investigation. EXPLORE. 2017;13:53–61. doi: 10.1016/j.explore.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Schneider M.J., Evans R., Haas M., et al. US chiropractors' attitudes, skills and use of evidence-based practice: a cross-sectional national survey. Chiropr Man Ther. 2015;23:16. doi: 10.1186/s12998-015-0060-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wieland L.S., Manheimer E., Berman B.M. Development and classification of an operational definition of complementary and alternative medicine for the Cochrane collaboration. Altern Ther Health Med. 2011;17:50–59. 2011. [PMC free article] [PubMed] [Google Scholar]
- 12.Alzahrani A.S., Price M.J., Greenfield S.M., et al. Global prevalence and types of complementary and alternative medicines use amongst adults with diabetes: systematic review and meta-analysis. Eur J Clin Pharmacol. 2021;77:1259–1274. doi: 10.1007/s00228-021-03097-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hill J., Mills C., Li Q., Smith J.S. Prevalence of traditional, complementary, and alternative medicine use by cancer patients in low income and lower-middle income countries. Glob Public Health. 2018;14:418–430. doi: 10.1080/17441692.2018.1534254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yalcin S., Hurmuz P., McQuinn L., et al. Prevalence of complementary medicine use in patients with cancer: a Turkish comprehensive cancer center experience. J Global Oncol. 2018;4:1–6. doi: 10.1200/JGO.2016.008896. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carè J., Steel A., Wardle J. Stakeholder attitudes to the regulation of traditional and complementary medicine professions: a systematic review. Hum Resour Health. 2021;19:42. doi: 10.1186/s12960-021-00579-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Front Pharmacol. 2014;4:177. doi: 10.3389/fphar.2013.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLean L., Micalos P.S., McClean R., Pak S.C. Evidence based practice within the complementary medicine context. TANG. 2016;6:e15. 2016. [Google Scholar]
- 18.Bussieres A.E., Terhorst L., Leach M.J., et al. Self-reported attitudes, skills and use of evidence-based practice among Canadian doctors of chiropractic: a national survey. J Can Chiropr Assoc. 2015;59:332–348. [PMC free article] [PubMed] [Google Scholar]
- 19.Cerritelli F., Iacopini A., Galli M., et al. Evidence-based practice among Italian osteopaths: a national cross-sectional survey. BMC Complement Med Ther. 2021;21:252. doi: 10.1186/s12906-021-03430-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim Y., Cho S.H. A survey of complementary and alternative medicine practitioner's perceptions of evidence-based medicine. Eur J Integr Med. 2014;6:211–219. [Google Scholar]
- 21.Leach M.J., Sundberg T., Fryer G., et al. An investigation of Australian osteopaths’ attitudes, skills and utilisation of evidence-based practice: a national cross-sectional survey. BMC Health Serv Res. 2019;19:498. doi: 10.1186/s12913-019-4329-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Damschroder L.J., Aron D.C., Keith R.E., et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gough D., Davies P., Jamtvedt G., et al. Evidence Synthesis International (ESI): position Statement. Syst Rev. 2020;9:155. doi: 10.1186/s13643-020-01415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lockwood C., Porritt K., McArthur A., Munn Z. In: JBI Handbook for Evidence Implementation. Porritt K., McArthur A., Lockwood C., Munn Z., editors. Joanna Briggs Institute; Adelaide: 2020. An introduction to evidence implementation. [Google Scholar]
- 25.World Health Organisation . World Health Organisation; 2022. Traditional, Complementary and Integrative Medicine.https://www.who.int/health-topics/traditional-complementary-and-integrative-medicine#tab=tab_1 (Accessed 25th January 2022) [Google Scholar]
- 26.Complementary and Alternative Medicine in the United States. National Academies Press; Washington: 2005. Institute of medicine committee on the use of complementary and alternative medicine by the American public. [PubMed] [Google Scholar]
- 27.Treloar C., Champness S., Simpson P., Higginbotham N. Critical appraisal checklist for qualitative research studies. Indian J Pediatr. 2000;67:347–351. doi: 10.1007/BF02820685. [DOI] [PubMed] [Google Scholar]
- 28.Law M., Stewart D., Pollock N., et al. McMaster University; Canada: 1998. Critical Review Form - Qualitative Studies. [Google Scholar]
- 29.Alcantara J., Leach M.J. Chiropractic attitudes and utilization of evidence-based practice: the use of the EBASE questionnaire. EXPLORE. 2015;11:367–376. doi: 10.1016/j.explore.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 30.Alvarez G., Justribo C., Sundberg T., et al. A national cross-sectional survey of the attitudes, skills and use of evidence-based practice amongst Spanish osteopaths. BMC Health Serv Res. 2021;2:130. doi: 10.1186/s12913-021-06128-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Braun L.A., Spitzer O., Tiralongo E., et al. Naturopaths and Western herbalists’ attitudes to evidence, regulation, information sources and knowledge about popular complementary medicine. Complement Ther Med. 2013;21:58–64. doi: 10.1016/j.ctim.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 32.Canaway R., Leach M., Hunter J. Setting an agenda for strengthening the evidence-base for traditional and complementary medicines: perspectives from an expert forum in Australia. Adv Integr Med. 2018:103–111. [Google Scholar]
- 33.Goldenberg J.Z., Burlingham B.S., Guiltinan J., et al. Shifting attitudes towards research and evidence-based medicine within the naturopathic medical community: the power of people, money and acceptance. Adv Integr Med. 2017;4:49–55. [Google Scholar]
- 34.Gowan-Moody D.M., Leis A.M., Abonyl S., et al. Research utilization and evidence-based practice among Saskatchewan massage therapists. J Complemeny Integr Med. 2012;10:189–198. doi: 10.1515/jcim-2012-0044. [DOI] [PubMed] [Google Scholar]
- 35.Hadley J., Hassan I., Khan K.S. Knowledge and beliefs concerning evidence-based practice amongst complementary and alternative medicine health care practitioners and allied health care professionals: a questionnaire. BMC Complement Altern Med. 2004;8:45. doi: 10.1186/1472-6882-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lawrence D.J., Polipnick J., Colby E. Barriers to and opportunities for the implementation of best practice ecommendations in Chiropractic. J Allied Health. 2008;37:82. [PubMed] [Google Scholar]
- 37.Hu X., Wang L. A primary survey of evidence-based medicine and traditional Chinese medicine. Chin J Evid Based Med. 2004;4:737–739. [Google Scholar]
- 38.Leach M.J., Gillham D. Are complementary medicine practitioners implementing evidence-based practice? Complement Ther Med. 2011;19:128–136. doi: 10.1016/j.ctim.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 39.Leach M.J., Canaway R., Hunter J. Evidence based practice in traditional & complementary medicine: an agenda for policy, practice, education and research. Complement Ther Clin Pract. 2018;31:38–46. doi: 10.1016/j.ctcp.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 40.Leach M.J., Shaw R., Austin P., et al. Attitudes, skills, and use of evidence-based practice: a cross-sectional survey of Swedish osteopaths. Int J Osteopath Med. 2020;38:41–49. 2020. [Google Scholar]
- 41.Leach M.J., Palmgren P.J., Thomson O.P., et al. Skills, attitudes and uptake of evidence-based practice: a cross-sectional study of chiropractors in the Swedish Chiropractic Association. Chiropr Man Ther. 2021;29(2) doi: 10.1186/s12998-020-00359-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leach M.J. Implementation science in New Zealand naturopathic practice: a cross-sectional study. J Complement Integr Med. 2022 doi: 10.1515/jcim-2021-0508. In Press. [DOI] [PubMed] [Google Scholar]
- 43.Roecker C.B., Long C.R., Vining R.D., et al. Attitudes toward evidence-based clinical practice among doctors of chiropractic with diplomate level training in orthopedics. Chiropr Manual Ther. 2013;21:43. doi: 10.1186/2045-709X-21-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schneider M.J., Evans R., Haas M., et al. US chiropractors' attitudes, skills and use of evidence-based practice: a cross-sectional national survey. Chiropr ManTher. 2015;23:16. doi: 10.1186/s12998-015-0060-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Snow J., Leach M.J., Clare B. Attitudes, skill and use of evidence-based practice among US Western herbal medicine providers: a national survey. J Complement Integr Med. 2017;14 doi: 10.1515/jcim-2015-0101. np. [DOI] [PubMed] [Google Scholar]
- 46.Spence W., Li N. An exploration of traditional chinese medicine practitioners’ perceptions of evidence based medicine. Complement Ther Clin Pract. 2013;19:63–68. doi: 10.1016/j.ctcp.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 47.Stomski N., Gimmer-Sommers K., Petkov J. A survey of the uptake and implementation of research evidence by South Australian acupuncturists in clinical practice: attitudes and associated predictive factors. Complement Ther Med. 2008;16:199–205. doi: 10.1016/j.ctim.2007.08.002. 2008. [DOI] [PubMed] [Google Scholar]
- 48.Stuttard P. Working in partnership to develop evidence-based practice within the massage profession. Complement Ther Nurs Midwifery. 2002;8:185–190. doi: 10.1054/ctnm.2002.0635. 2002. [DOI] [PubMed] [Google Scholar]
- 49.Sullivan M., Leach M., Snow J., et al. Understanding North American yoga therapists' attitudes, skills and use of evidence-based practice: a cross-national survey. Complement Ther Med. 2017;32:11–18. doi: 10.1016/j.ctim.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 50.Sundberg T., Leach M.J., Thomson O.P., et al. Attitudes, skills and use of evidence-based practice among UK Osteopaths: a national cross-sectional survey. BMC Musculoskel Dis. 2018;19:439. doi: 10.1186/s12891-018-2354-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Suter E., Vanderheyden L.C., Trojan L.S., et al. How important is research-based practice to chiropractors and massage therapists? J Manip Physiol Ther. 2007;30:109–115. doi: 10.1016/j.jmpt.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 52.Veziari Y., Kumar S., Leach M.J. Barriers to the conduct and application of research among complementary and alternative medicine professions in Australia and New Zealand: a cross sectional study. Complement Ther Med. 2021;60 doi: 10.1016/j.ctim.2021.102752. [DOI] [PubMed] [Google Scholar]
- 53.Walker B.F., Stomski N.J., Hebert J.J., et al. Evidence-based practice in chiropractic practice: a survey of chiropractors’ knowledge, skills, use of research literature and barriers to the use of research evidence. Complement Ther Med. 2014;22:286–295. doi: 10.1016/j.ctim.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 54.Weber V., Rajendran D. UK trained osteopaths’ relationship to evidence based practice – an analysis of influencing factors. Int J Osteopat Med. 2018;29:15–25. [Google Scholar]
- 55.Wong C.H.L., Tse J.V.H., Nilsen P., et al. Barriers and facilitators to promoting evidence uptake in Chinese medicine: a qualitative study in Hong Kong. BMC Complement Med Ther. 2021;21:200. doi: 10.1186/s12906-021-03372-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Woo J.M., Cho S.H. Traditional Korean medicine practitioners’ attitudes toward evidence-based medicine: a qualitative study. Eur J Integr Med. 2012;4:e448–e454. [Google Scholar]
- 57.Leach M.J., Sundberg T. Southern Cross University; Lismore: 2022. Skills, Attitudes and Uptake of Evidence-Based Practice Among Swedish Naprapaths [Unpublished Raw Data] [Google Scholar]
- 58.Leach M.J. Southern Cross University; Lismore: 2022. Attitudes, Skills, and Use of Evidence-Based Practice Among Australian naturopaths [Unpublished Raw Data] [Google Scholar]
- 59.Leach M.J. Southern Cross University; Lismore: 2022. Attitudes, skills, and Use of Evidence-Based Practice Among Australian manual Complementary Therapists [Unpublished Raw Data] [Google Scholar]
- 60.Leach M.J. Southern Cross University; Lismore: 2022. Attitudes, skills, and Use of Evidence-Based Practice Among Australian complementary Therapists [Unpublished Raw Data] [Google Scholar]
- 61.Leach M.J. Southern Cross University; Lismore, Australia: 2022. A National Cross-Sectional Survey of Canadian Naturopathic Doctor engagement, Preparedness and Perceptions of Evidence-Based Practice [Unpublished Raw Data] [DOI] [PubMed] [Google Scholar]
- 62.Myhrvold B.L., Axen I., Leach M.J., et al. University of Oslo; Oslo: 2022. Investigating attitudes, skills, and Uptake of Evidence-Based Practice Among Norwegian chiropractors; a Cross-Sectional Study [Unpublished Manuscript] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pelletier R., Thomson O.P., Leach M.J., et al. Université de Sherbrooke; Sherbrooke, Québec: 2022. Osteopaths/Osteopathic Manual practitioners’ attitudes, Skills and Use of Evidence-Based Practice [Unpublished Raw Data] [Google Scholar]
- 64.Harding K.E., Porter J., Horne-Thompson A., et al. Not enough time or a low priority? Barriers to evidence-based practice for allied health clinicians. J Contin Educ Health Prof. 2014;34:224–231. doi: 10.1002/chp.21255. 2014. [DOI] [PubMed] [Google Scholar]
- 65.McArthur C., Bai Y., Hewston P., et al. Barriers and facilitators to implementing evidence-based guidelines in long-term care: a qualitative evidence synthesis. Implementation Sci. 2021;16:70. doi: 10.1186/s13012-021-01140-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Paci M., Faedda G., Ugolini A., et al. Barriers to evidence-based practice implementation in physiotherapy: a systematic review and meta-analysis. Int J Qual Health Care. 2021;33:mzab093. doi: 10.1093/intqhc/mzab093. 2021. [DOI] [PubMed] [Google Scholar]
- 67.Sadeghi-Bazargani H., Tabrizi J.S., Azami-Aghdash S. Barriers to EBM. J Eval Clin Pract. 2014;20:793–802. doi: 10.1111/jep.12222. [DOI] [PubMed] [Google Scholar]
- 68.Johnson M.P., Zheng K., Padman R. Modeling the longitudinality of user acceptance of technology with an evidence-adaptive clinical decision support system. Decis Support Syst. 2014;57:444–453. [Google Scholar]
- 69.Mathieson A., Grande G., Luker K. Strategies, facilitators and barriers to implementation of evidence-based practice in community nursing: a systematic mixed-studies review and qualitative synthesis. Prim Health Care Res Dev. 2019;20:E6. doi: 10.1017/S1463423618000488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hagbaghery M.A., Salsali M., Ahmadi F. The factors facilitating and inhibiting effective clinical decision-making in nursing: a qualitative study. BMC Nurs. 2004;3:2. doi: 10.1186/1472-6955-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Goorts K., Dizon J., Milanese S. The effectiveness of implementation strategies for promoting evidence informed interventions in allied healthcare: a systematic review. BMC Health Serv Res. 2021;21:241. doi: 10.1186/s12913-021-06190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Veziari Y., Kumar S., Leach M. Addressing barriers to the conduct and application of research in complementary and alternative medicine: a scoping review. BMC Complement Med Ther. 2021;21:201. doi: 10.1186/s12906-021-03371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wong C.H.L., Wu I.X.Y., Cheung W.K.W., et al. Impact of evidence-based healthcare education for Chinese medicine practitioners: a pre-post evaluation. Complement Ther Med. 2019;45:38–44. doi: 10.1016/j.ctim.2019.05.004. 2019. [DOI] [PubMed] [Google Scholar]
- 74.Veziari Y., Kumar S., Leach M.J. An exploration of barriers and enablers to the conduct and application of research among complementary and alternative medicine stakeholders in Australia and New Zealand: a qualitative descriptive study. PLoS ONE. 2022;17 doi: 10.1371/journal.pone.0264221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hall P. Interprofessional teamwork: professional cultures as barriers. J Interprof Care. 2005;19:188–196. doi: 10.1080/13561820500081745. [DOI] [PubMed] [Google Scholar]
- 76.Dodek P., Cahill N.E., Heyland D.K. The relationship between organizational culture and implementation of clinical practice guidelines. J Parenteral Enteral Nutr. 2010;34:669–674. doi: 10.1177/0148607110361905. [DOI] [PubMed] [Google Scholar]
- 77.Williams B., Perillo S., Brown T. What are the factors of organisational culture in health care settings that act as barriers to the implementation of evidence-based practice? A scoping review. Nurs Educ Today. 2015;35:e34–e41. doi: 10.1016/j.nedt.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 78.Flodgren G., O'Brien M.A., Parmelli E., et al. Local opinion leaders: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2019;6 doi: 10.1002/14651858.CD000125.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sandström B., Borglin G., Nilsson R., et al. Promoting the implementation of evidence-based practice: a literature review focusing on the role of nursing leadership. Worldviews Evid Based Nurs. 2011;8:212–223. doi: 10.1111/j.1741-6787.2011.00216.x. [DOI] [PubMed] [Google Scholar]
- 80.Sackett D.L., Rosenberg W.M., Gray J.A., et al. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gandjour A. Patient preferences: a Trojan horse for evidence-based medicine? Eur J Health Econ. 2018;19:167–172. doi: 10.1007/s10198-017-0916-4. [DOI] [PubMed] [Google Scholar]
- 82.Gibson A., Boddy K., Maguire K., et al. Exploring the impact of providing evidence-based medicine training to service users. Res Involv Engag. 2015;1:10. doi: 10.1186/s40900-015-0010-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dagne A.H., Beshah M.H. Implementation of evidence-based practice: the experience of nurses and midwives. PLoS ONE. 2021;16 doi: 10.1371/journal.pone.0256600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lin N.X.Y. Attitudes, self-efficacy, and feasibility: exploring social work students’ perceptions of evidence-based practice. J Evid Based Soc Work. 2020;17:538–557. doi: 10.1080/26408066.2020.1781728. [DOI] [PubMed] [Google Scholar]
- 85.Wardle J.L., Adams J., Lui C.W., et al. Current challenges and future directions for naturopathic medicine in Australia: a qualitative examination of perceptions and experiences from grassroots practice. BMC Complement Altern Med. 2013;13:15. doi: 10.1186/1472-6882-13-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Higgins J.P.T., Thomas J., Chandler J., et al. John Wiley; Chichester: 2019. Cochrane Handbook for Systematic Reviews of Interventions. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available within the article and supplementary material.