Abstract
Background:
Despite understanding the long-term risks associated with early substance use, less is known about the specific patterns of age of onset (AO) across multiple substances and whether these patterns of early exposure are linked to substance use later in young adulthood. Consequently, the present study sought to (1) identify distinct classes regarding AO for alcohol, cannabis, and tobacco and (2) compare these classes on patterns of individual and simultaneous alcohol, cannabis, and tobacco use, other substance use, and mental health symptoms.
Methods:
Participants were 510 emerging adults (M age = 21.35; 88.6% men) who reported past-year use of alcohol, cannabis, and tobacco.
Results:
Latent profile analysis was used to identify classes based on three indicators: AO for alcohol, cannabis, and tobacco. Results revealed that four classes best fit the data: Earliest AO for Alcohol (19.8%); Latest AO for Substances (6.5%); Late AO for Substances (67.8%); Earliest AO for Cannabis and Tobacco (5.9%). Classes varied on current patterns of individual substance use, co-use of substances, other illicit drug use, and mental health symptomology. The Latest AO of Substances class reported the lowest alcohol use, cannabis use, other illicit drug use, and mental health symptomology than the other classes. The Earliest AO for Alcohol and the Late AO of Substances reported lower frequency of tobacco compared to the other classes. The Late AO of Substance class reported the highest past-year frequency of simultaneous alcohol and cannabis use.
Conclusions:
The current study contributed to the larger polysubstance literature by identifying profiles that may signify risky patterns of use. Findings may help guide prevention and intervention work with adolescents and young adults.
Keywords: alcohol, cannabis, tobacco, simultaneous drug use, age of onset
Alcohol, cannabis, and tobacco are the most commonly used substances in the United States1. Among young adults, 81.4% report using alcohol, 40.1% report using cannabis, and 21.6% report using tobacco (cigarettes) within the past year.1 Co-use, either using two or more substances concurrently or simultaneously, is also common.2,3 Specifically, approximately three quarters of tobacco-using young adults report current alcohol use,2,4 and additionally, between 25% and nearly 60% (depending on tobacco product) of individuals who report tobacco use also report current cannabis use.2,5,6 Over 75% of individuals reporting cannabis use also report current alcohol use.7 The co-use of one substance has been associated with greater levels in use of other substances.7 Further, compared to individuals who use alcohol, cannabis, or tobacco only, individuals who co-use these substances experience more adverse consequences (e.g., neurocognitive effects, psychosocial and mental health problems, heavier alcohol use, and poorer treatment outcomes).8-12 Given that individuals who co-use alcohol, cannabis, and tobacco are at increased risk for harms, investigations that determine underlying factors of co-use are needed.
One factor that has been shown to predict level of substance use involvement is age of onset (AO). In particular, an earlier AO of a specific substance is robustly associated with heavier substance use and substance use problems later in life.13,14 Specifically among individuals who use multiple substances, the gateway hypothesis suggests that the initiation and progression of substance use occurs in discrete stages, such that AO for alcohol and tobacco precede AO for cannabis and then AO for other illicit drugs.15 Early AO for alcohol, cannabis, and tobacco are linked to early AO use of other substances,16-18 but patterns of progression between these substances are not universal across individuals.
Several studies have examined the relationship between AO and patterns of substance use later in adulthood;19-21 however, less research has focused on the progression of use among individuals who co-use multiple substances. Using four waves of data from the National Longitudinal Study of Adolescent to Adult Health, Richmond-Rakerd and colleagues (2017) utilized multivariate latent growth curve analysis to examine alcohol, cannabis, and tobacco involvement, individually and co-use, over time and how patterns of use were related to the AO for each substance.22 Findings revealed significant negative associations between AO across all substances and rates of change in substance use individually, although some discrepancies were found for use quantity (i.e., how much of substance is used) versus frequency (i.e., how often a substance is used). When examining polysubstance use as the outcome, Richmond-Rakerd et al. (2017) found steeper increases in tobacco and alcohol use and alcohol and cannabis use among those with earlier AO across all substances.22 Thus, AO across multiple substances may have differential patterns of substance use involvement later in adulthood. Although the investigation found associations using a traditional variable-centered approach, a person-centered approach (e.g., latent profile analysis [LPA]) may further identify AO typologies that pose greatest risk for increased levels of co-use in adulthood.
Substance use involvement commonly co-occurs with other psychological symptoms that are often described as internalizing and include anxiety, depression, and somatic symptoms.23,24 Robust associations have been found between mental health symptoms and levels of alcohol,25 cannabis,26 and tobacco use.27 Further, mental health symptoms are more likely in young adults who use multiple substances.28-29 The association between mental health symptoms and substance use may be bidirectional, as indicated in prior research on alcohol30,31 and tobacco use.32,33 That is, increased mental health symptoms may increase risk towards initiating early use of substances and increased substance use involvement exacerbates mental health symptoms. Given the high prevalence of co-occurring mood and substance use disorders during the adolescent and young adult developmental periods,31 determining whether patterns of AO across multiple substances are related to mental health symptomology during young adulthood could identify at-risk individuals.
Individuals who co-use alcohol, cannabis, and tobacco are at increased risk for harms. The present study sought to explore how AO may contribute to current patterns of substance use among young adults. Specifically, we examined patterns of early exposure to alcohol, cannabis, and tobacco and whether patterns of AO were associated with current patterns of substance use and mental health symptoms. The aims of the present investigation were to (1) determine patterns of AO with young adults using LPA to identify latent classes or groups of young adults who share similarities in their profiles based on AO for alcohol, cannabis, and tobacco; and (2) examine differences between latent classes on current patterns of substance use (individual and simultaneous use of alcohol, cannabis, and tobacco), other illicit drug use, and mental health symptoms. It was hypothesized that there would be distinct groups of individuals based on their AO profiles and that these latent groups would be differentiated based on current alcohol, cannabis, and tobacco use, other illicit drug use, and mental health symptoms.
Methods
Participants and Procedures
The present study was part of a larger study conducted online on alcohol and substance use behaviors among young adults between ages 18 and 25. Participants were recruited via Craigslist, a web-based service for posting classified advertisements between February to July 2016. Recruitment advertisements were posted once a week in most U.S. cities listed on the website. A description of the public post included a link to a five-minute screening form that determined their eligibility to participate in the study. If eligible, participants were redirected to the online study survey that took approximately 40 minutes to complete. Participation was voluntary, and participants were compensated $15 for their participation. The current study was approved by the university’s institutional review board and we followed all APA ethical guidelines.
Several validity checkpoints were included to ensure the integrity of the data: (1) participants were asked to provide unique identifying information twice in the survey, and these data were required to match; (2) completion time was taken into consideration as to exclude those that very quickly completed the survey; (3) there were five validity questions (e.g., “how many days are in a week?”) asked throughout the survey to ensure participants were responding appropriately to survey items. Although 1,732 participants completed the survey, 485 participants were removed because they did not pass these validity checkpoints. These strategies support the integrity of study data.
In order to be included in analyses, participants had to have reported past-year use of alcohol, cannabis, and tobacco. The final sample used for study analyses were 510 emerging adults (88.6% men, n = 452). The mean age of the sample was 21.35 years (SD = 1.59 years). Most of the sample identified as White (85.7%), were employed (90.8%), and were living in a campus dormitory, residence hall, or apartment (47.0%). Full demographic characteristics of the sample can be found in Table 1.
Table 1.
Demographic Frequencies by Class
| Latent Profile | |||||||
|---|---|---|---|---|---|---|---|
| Total n = 510 (%) |
Class 1 n = 101 (%) |
Class 2 n = 33 (%) |
Class 3 n = 346 (%) |
Class 4 n = 30 (%) |
df | χ 2 | |
| Sex | 3 | 39.99** | |||||
| Male | 452 (88.6) | 86 (19.0) | 22 (4.9) | 324 (71.7) | 20 (4.4) | ||
| Female | 58 (11.4) | 15 (25.9) | 11 (19.0) | 22 (37.9) | 10 (17.2) | ||
| Ethnicity | 15 | 77.76** | |||||
| Caucasian/White | 437 (85.7) | 92 (21.1) | 18 (4.1) | 308 (70.5) | 19 (4.3) | ||
| African American/Black | 48 (9.4) | 4 (8.3) | 7 (14.6) | 29 (60.4) | 8 (16.7) | ||
| Native American/Indian | 2 (0.4) | 0 | 2 (66.7) | 1 (33.3) | 0 | ||
| Asian/Pacific American | 3 (0.6) | 0 | 2 (66.7) | 1 (33.3) | 0 | ||
| Hispanic/Latino | 14 (2.7) | 4 (28.6) | 2 (14.3) | 5 (35.7) | 3 (21.4) | ||
| Employment | 3 | 10.23* | |||||
| Unemployed | 47 (9.2) | 10 (21.3) | 5 (10.6) | 25 (53.2) | 7 (14.9) | ||
| Employed | 462 (90.8) | 90 (19.5) | 28 (6.1) | 321 (69.5) | 23 (5.0) | ||
| Highest Grade Completed | 6 | 39.97** | |||||
| < high school | 8 (1.6) | 2 (25.0) | 0 | 5 (62.5) | 1 (12.5) | ||
| GED/high school diploma | 44 (8.6) | 2 (4.5) | 9 (20.5) | 24 (54.5) | 9 (20.5) | ||
| Some college/college | 456 (89.4) | 97 (21.3) | 24 (5.3) | 315 (69.1) | 20 (4.4) | ||
| Missing | 2 (0.4) | -- | -- | -- | -- | ||
| Living Situation | 12 | 82.45** | |||||
| Parent’s or relative’s home | 179 (35.1) | 46 (25.7) | 11 (6.1) | 105 (58.7) | 17 (9.5) | ||
| College dorm/residence/apartment | 239 (46.9) | 39 (16.3) | 3 (1.3) | 193 (80.8) | 4 (1.7) | ||
| House/apartment/room (not college-affiliated) | 88 (17.3) | 15 (17.0) | 18 (20.5) | 47 (53.4) | 8 (9.1) | ||
| Fraternity/sorority house | |||||||
| Other | 1 (0.2) | 0 | 0 | 0 | 1 (100) | ||
| Missing | 2 (0.4) | -- | -- | -- | -- | ||
| Yearly Total Individual Income | 12 | 108.586** | |||||
| Under $10,000 | 56 (11.0) | 13 (23.2) | 12 (21.4) | 23 (41.1) | 8 (14.3) | ||
| $10,001-$20,000 | 35 (6.9) | 4 (11.4) | 10 (28.6) | 16 (45.7) | 5 (14.3) | ||
| $20,001-$40,000 | 49 (9.6) | 18 (36.7) | 6 (12.2) | 22 (44.9) | 3 (6.1) | ||
| $40,001-$60,000 | 314 (61.6) | 61 (19.4) | 4 (1.3) | 240 (76.4) | 9 (2.9) | ||
| $60,001-$80,000 | 51 (10.0) | 4 (7.8) | 1 (2.0) | 41 (80.4) | 5 (9.8) | ||
| Missing | 5 (1.0) | -- | -- | -- | -- | ||
Note. Class 1 = Earliest AO for Alcohol; Class 2 = Latest AO of Substances; Class 3 = Late AO of Substances; Class 4 = Earliest AO for Cannabis and Tobacco. For Ethnicity, three participants identified as “Other”.
p < .001
p < .05
Measures
Age of Onset
Age of onset was assessed by one item for alcohol, cannabis, and tobacco. Participants were asked “at what age did you first drink alcohol?”; “at what age did you first use cannabis?”; and “at what age did you first smoke tobacco?” with a drop-down response scale of ages ranging from N/A and 0 to 25 in one-year increments. This approach is similar to prior research.34,35
Alcohol, Cannabis, and Tobacco Use
The Daily Drinking Questionnaire36 (DDQ) was used to assess typical frequency of alcohol, cannabis, and tobacco use.37,38 Participants reported the typical number of standard drinks consumed each day of the week over the last three months. The DDQ was modified for cannabis and tobacco use. For cannabis, participants were asked to report the number of joints they used on each day of the week over the last three months. For tobacco, participants were asked to report the number of cigarettes on each day of the week over the last three months. Days in which substances were used were totaled for a frequency score (i.e., the total number of days in which the substance was used in a typical week).
Other Substance Use
A checklist indicating illicit substances other than alcohol, cannabis, and tobacco (e.g., cocaine, LSD, stimulants, depressants, ecstasy, opioids) was utilized to measure other substance use in the past year. Participants indicated whether or not they had used each substance in the past year with a yes/no response scale. Each substance was coded as 0 or 1 to indicate if substance was used in the past year, and items were summed for a total score. Higher scores indicated higher number of substances used in the past year.
Simultaneous Drug Use
The Simultaneous Polydrug Use Questionnaire (DUQ) was used to assess simultaneous drug use of alcohol and cannabis, alcohol and tobacco, and cannabis and tobacco.39 Simultaneous use was defined as when two or more of the substances listed were used within a few hours of each other. Participants were asked about their frequency of use with responses including “never in the past year” (0), “once a month or less” (1), “2-3 times per month” (2), “once a week” (3), -2-4 times per week” (4), and “5-7 times per week” (5).
Mental Health Symptoms
The Brief Symptoms Inventory-18 was used to assess mental health symptoms in the past year.40 This measure assesses three areas of mental health symptoms including somatization (e.g., “nausea or upset stomach”), anxiety (e.g., “spells of terror or panic”), and depression (e.g., “feeling no interest in things). Participants indicated how often they had experienced these feelings with responses ranging from “(0) not at all” to “(4) nearly everyday.” Score were summed for a total score. Higher scores indicated greater mental health symptoms. Cronbach’s alpha was .87.
Data Analytic Plan
Data were inspected for outliers and missing data prior to study analyses. Missing data ranged from 0% (AO for alcohol) to 3.7% (AO for tobacco). All models were tested in Mplus version 8.3 using full information maximum likelihood.21 Latent profile analysis (LPA) was used to identify profiles based on participants’ AO for alcohol, cannabis, and tobacco use. LPA identifies classes of individuals that are similar on observed continuous indicators (e.g., AO) by identifying each individual's likelihood, or posterior probability, of being in each class. Individuals are assigned to the class in which their posterior probability is highest. Several models were estimated indicating different numbers of classes and the optimal number is determined using model comparison criteria including: (1) the Akaike Information Criteria (AIC) and sample size adjusted Bayesian Information Criteria (SSA BIC) to assess model fit, with lower values indicating better model fit41 (2) the Lo-Mendell-Rubin (LMR) likelihood ratio test to assess if the current number of classes (k) is a better fitting model than a model with one fewer class (k – 142); (3) relative entropy (range from 0.0 to 1.0) to evaluate classification accuracy, with higher values indicating greater accuracy; and (4) the size of each latent group was considered to ensure that the smallest group contained enough individuals to allow meaningful generalizations. These criteria together were used to determine the best-fitting model. After the ideal number of latent classes was established, associations between class memberships and outcomes were subsequently examined using the bch weight method. This approach examines whether average values of continuous auxiliary variables (i.e., frequency of simultaneous substances, other substance use, and mental health symptoms) differed across classes using a weight multiple group method.
Results
Descriptives for Overall Sample
The entire sample’s average AO was 13.86 (SD = 2.64) years for alcohol, 16.63 (SD = 1.26) for cannabis, and 16.07 (SD = 1.30) for tobacco. Frequency of use in a typical week was 6.41 (SD = 1.52) days for alcohol, 6.18 (SD = 2.00) for cannabis, and 6.53 (SD = 6.54) for tobacco among the overall sample. Frequency of simultaneous alcohol and cannabis use was 3.42 (SD = 1.15; “2-4” to “5-7 times per week”), frequency of simultaneous alcohol and tobacco use was 2.47 (SD = 1.41; “once a week” to “2-4 times per week”), and frequency of simultaneous cannabis and tobacco use was 2.34 (SD = 1.34; “once a week” to “2-4 times per week”).
Latent Profile Models
Models with a 1-, 2-, 3-, 4-, 5-, and 6-class solution were examined. Fit statistics for the six LPA models are presented in Table 2, and the selection criteria for each model collectively indicated that the 4-class solution had the best fit. The AIC and SSA-BIC consistently decreased as more classes were added. Based on the LMR likelihood ratio test, we determined that either a 4- or 5-class solution were most optimal. However, the 4-class model had an entropy value of .970, slightly higher than the 5-class model, which indicated a superior level of classification accuracy.
Table 2.
Model Fit Based on Number of Classes
| Classes | AIC | BIC | Adjusted BIC |
Relative Entropy |
LMR LRT p |
Proportion of smallest group |
|---|---|---|---|---|---|---|
| 1 | 5721.773 | 5747.179 | 5728.135 | -- | -- | -- |
| 2 | 5251.262 | 5293.607 | 5261.865 | .98 | <.001 | .22 |
| 3 | 5168.254 | 5227.536 | 5183.098 | .96 | .025 | .03 |
| 4 | 5047.170 | 5123.390 | 5066.255 | .97 | .028 | .06 |
| 5 | 4980.585 | 5074.015 | 5004.184 | .93 | .017 | .05 |
| 6 | 4930.348 | 5040.443 | 4957.916 | .96 | .115 | .02 |
Note. AIC = Akaike Information Criterion, BIC = Bayesian Information Criterion, LMR LRT = Lo-Mendell-Rubin likelihood ratio test. Proportion of smallest group comes from estimated posterior probabilities rather than most likely class membership.
As can be seen in Figure 1 and Table 2, Class 1 appeared to be characterized by the earliest AO for alcohol use, early AO for cannabis use, and early AO for tobacco use and represented 19.8% (n = 101) of the sample with mean AOs (SE) ranging from 9.03 (.03), 16.34 (.14), and 15.79 (.16) for alcohol, cannabis, and tobacco, respectively. As such, this class was labeled “Earliest AO for Alcohol” group. Class 2 was characterized by the latest AO for alcohol, cannabis, and tobacco use and represented 6.5% (n = 33) of the sample with mean AOs (SE) ranging from 17.42 (.19), 18.17 (.22), and 17.06 (.22) for alcohol, cannabis, and tobacco, respectively. As such, this class was labeled “Latest AO for Substances”. Class 3 was characterized by later AOs for alcohol, cannabis, and tobacco use and represented 67.8% (n = 346) of the sample with mean AOs (SE) ranging from 15.07 (.04), 16.66 (.07), and 16.18 (.07) for alcohol, cannabis, and tobacco, respectively. This class was labeled “Late AO for Substances”. Lastly, Class 4 was characterized by early AO for alcohol use and the earliest AOs for cannabis and tobacco and represented 5.9% (n = 30) of the sample with mean AOs (SE) ranging from 12.30 (.34), 15.63 (.51), and 14.72 (.46) for alcohol, cannabis, and tobacco, respectively. This class was labeled “Earliest AO for Cannabis and Tobacco”.
Figure 1.
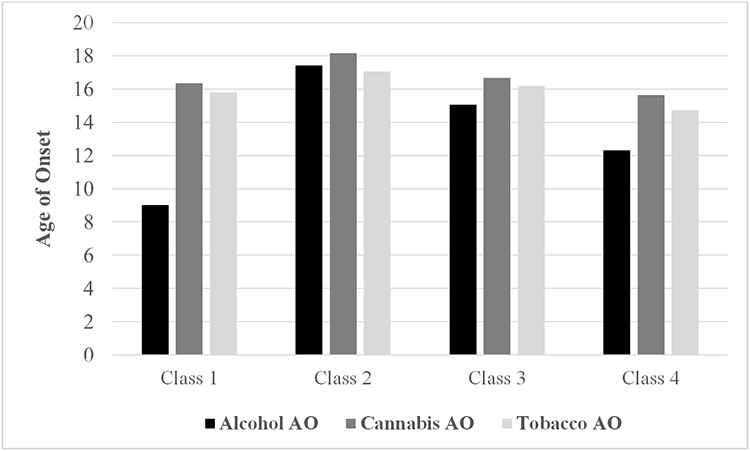
Estimated means for unconditional 4-class LPA model.
There were significant differences between latent class means for each of the AO indicators: AO for alcohol, F(3,509) = 2995.79, p < .001; AO for cannabis, F(3,492) = 28.89, p < .001; and AO for tobacco, F(3,490) = 20.90, p < .001. Post hoc tests revealed that the Earliest AO for Alcohol group had the earliest AO for alcohol use, and AO for cannabis and tobacco use was later than the Earliest AO for Cannabis and Tobacco group but earlier than the later AO groups. The Latest AO for Substances group reported the latest AO for alcohol, cannabis, and tobacco use compared to all other groups. The Late AO for Substances reported later AO for alcohol, cannabis, and tobacco use compared to the early groups, but had earlier AO for all substances than the Latest AO for Substances group. Lastly, the Earliest AO for Cannabis and Tobacco reported the earliest AO for cannabis and tobacco use, and AO for alcohol use was later than the Earliest AO for Alcohol group but earlier than the later AO groups (see Table 3). Comparisons between groups on demographics revealed significant differences on sex, ethnicity, employment, highest grade completed, living situation, and income, p < .05 (see Table 1).
Table 3.
Means and SDs of Indicator Variables for 4-class LPA Model
| Alcohol AO M (SE) |
Cannabis AO M (SE) |
Tobacco AO M (SE) |
|
|---|---|---|---|
| Class 1: Earliest AO for Alcohol | 9.03 (.03)a | 16.34 (.14)a | 15.79 (.16)a |
| Class 2: Latest AO of Substances | 17.42 (.19)b | 18.17 (.22)b | 17.06 (.22)b |
| Class 3: Late AO of Substances | 15.07 (.04)c | 16.66 (.07)c | 16.18 (.07)c |
| Class 4: Earliest AO for Cannabis and Tobacco | 12.30 (.34)d | 15.63 (.51)d | 14.72 (.46)d |
Note. AOs significantly varied across classes. Class values that do not share the same superscript are significantly different on the indicator between the classes. AO = age of onset. Sample sizes by classes were: Class 1 = 101; Class 2 = 33; Class 3 = 346; Class 4 = 30. M = Mean, SE = standard error.
Class Comparisons on Substance Use and Mental Health Symptoms
A comparison of latent classes on measures of individual and simultaneous substance use, other drug use, and mental health symptoms are presented in Table 4. Sex, ethnicity, employment, highest grade completed, and living situation were included as covariates. For alcohol use, the Latest AO of Substances class reported the lowest frequency of alcohol use in a typical week than the other classes. For cannabis use, the Latest AO of Substances reported lower frequency of cannabis use in a typical week than the other classes. For tobacco use, the Earliest AO for Alcohol and the Late AO of Substances reported lower frequency of tobacco compared to the other classes. All other group comparisons were nonsignificant.
Table 4.
Comparisons among Latent Profiles on Current Substance Use Outcomes
| Latent Profile | |||||
|---|---|---|---|---|---|
| Class 1 (n = 101) M (SD) |
Class 2 (n = 33) M (SD) |
Class 3 (n = 343) M (SD) |
Class 4 (n = 30) M (SD) |
Differences | |
| Frequency of Individual Substances | |||||
| Alcohol | 6.53 (0.33) | 5.13 (2.38) | 6.59 (1.33) | 5.63 (2.04) | 2 < 1,3,4 |
| Cannabis | 6.35 (1.82) | 3.37 (2.57) | 6.49 (1.66) | 4.93 (2.80) | 2 < 1,3,4 |
| Tobacco | 6.39 (1.95) | 6.48 (1.65) | 6.62 (1.48) | 6.37 (1.88) | 1 < 2,4; 3 < 2,4 |
| Frequency of Simultaneous Substance Use | |||||
| Alcohol + Cannabis | 3.04 (1.25) | 2.68 (1.47) | 3.66 (0.98) | 2.72 (1.41) | 1,2,4 < 3 |
| Alcohol + Tobacco | 2.12 (1.24) | 3.77 (1.65) | 2.37 (1.35) | 3.41 (1.21) | 1 < 2,3,4; 3 < 2,4 |
| Cannabis + Tobacco | 2.47 (1.30) | 2.77 (1.80) | 2.23 (1.28) | 2.82 (1.33) | 1 < 2; 3 < 2,4 |
| Other Health Outcomes | |||||
| Other Substance Use | 5.46 (1.43) | 2.208 (1.86) | 5.50 (1.41) | 4.25 (2.15) | 2 < 1,3,4 |
| Psychological Distress | 43.44 (9.04) | 27.93 (16.30) | 44.13 (11.41) | 37.90 (18.21) | 2 < 1,3,4 |
Note. Class 1 = Earliest AO for Alcohol; Class 2 = Latest AO of Substances; Class 3 = Late AO of Substances; Class 4 = Earliest AO for Cannabis and Tobacco; M = mean; SD = standard deviation.
For simultaneous alcohol and cannabis use, the Late AO of Substances class, as compared to the other classes, reported the highest past-year frequency. For simultaneous alcohol and tobacco use, the Earliest AO for Alcohol class reported lower past-year frequency than the other classes and the Late AO of Substances reported lower past-year frequency compared to the Latest AO of Substances and Earliest AO for Cannabis and Tobacco classes. For simultaneous cannabis and tobacco use, the Earliest AO for Alcohol reported less frequency than the Latest AO of Substances classes. The Earliest AO for Cannabis and Tobacco reported higher past-year frequency than the Late AO of Substances classes. All other group comparisons were nonsignificant. For other substances used, the Earliest AO for Alcohol, the Late AO of Substances, and the Earliest AO for Cannabis and Tobacco classes reported a greater number of other substances used in the past year compared to the Latest AO of Substances class. For mental health symptoms, the Latest AO of Substances reported lower mental health symptoms compared to the other classes. All other group comparisons were nonsignificant.
Discussion
The present study examined patterns of AO for alcohol, cannabis, and tobacco. A person-based technique was used to identify latent classes of young adults sharing similarity in AO across multiple substances. These classes were further examined by determining whether they differed in terms of current substance use patterns, including co-use and other illicit drug use, and mental health symptoms.
LPA analyses identified four latent classes of young adults based on their AO for alcohol, cannabis, and tobacco use. The “Earliest AO for Alcohol” class was characterized by the earliest AO for alcohol use and early AO for cannabis and tobacco use. The “Latest AO for Substances” class was characterized by the latest AO for alcohol, cannabis, and tobacco use. The “Late AO for Substances” Class 3 was characterized by later AOs for alcohol, cannabis, and tobacco use. The “Earliest AO for Cannabis and Tobacco” class reported the earliest AO for cannabis and tobacco use. Across the four classes, the range in AO for cannabis and tobacco use was between two and three years whereas for alcohol use was approximately eight years, suggesting that most variability in AO occurred for early use of alcohol. Each latent class’ sequencing of AO across substances is in line with the gateway hypothesis suggesting that substance use initiation typically begins with alcohol and tobacco prior to cannabis;15 however, this does not assume that an earlier AO would necessarily lead to use of other substances in adulthood43 or that individuals who use one substance would progress to using other “harder” substances.20, 44
The latent classes were compared on current single substance use of alcohol, cannabis, and tobacco use frequency. The most distinct finding to emerge was that the “Late AO of Substances”, “Earliest AO for Alcohol”, and the “Earliest AO for Cannabis and Tobacco” classes reported higher frequency of alcohol and cannabis use in a typical week than the other class, and these classes did not differ from each other. Prior research has strongly supported that an earlier AO of a specific substance is predictive of heavier substance use later in life.13,14 However, findings also suggested that the “Late AO of Substance” class also indicated risk for increased alcohol and cannabis use. The “Latest AO of Substances” and the Earliest AO for Cannabis and Tobacco” use reported higher frequency of tobacco use. Each class reported a tobacco use frequency of approximately six days, indicating that our sample included those who use tobacco daily.
Another aim was to examine whether profiles of AO across multiple substances predicted current co-use patterns and other illicit drug use. Results varied depending on co-use pattern; specifically, the “Late AO of Substances” class engaged in the highest past-year frequency of simultaneous alcohol and cannabis use, the “Latest AO of Substances” and “Earliest AO for Cannabis and Tobacco” engaged in the highest past-year frequency of simultaneous alcohol and tobacco use, and the “Latest AO of Substances” and “Earliest AO for Cannabis and Tobacco” reported higher past-year frequency of simultaneous cannabis and tobacco. The “Latest AO of Substances” class reported the lowest levels of other illicit drug use, with no differences among the other classes. Thus, a clear pattern of co-use risk did not emerge between our classes. That is, based on the literature, we expected that the earliest AO classes would pose greatest risk for later substance use. However, it is possible that the risk posed by earlier AO of individual substances does not fully explain later patterns of co-use. It may be more important to examine when regular use of individual substances began or AO for when co-use of substances began. Further, there was some evidence that delaying AO for individual substances was associated with lower use of other illicit substances. This is in line with prior research suggesting that early exposure to substances during adolescence may increase sensitivity towards subsequent drug use through changes in neurobiological processes.45,46 Another potential explanation could be related to age. If participants in the “Latest AO of Substances” class began individual substance use between ages 17 and 18, then it is possible that experimentation or transition to illicit substance use has not occurred.
Our last aim was to examine differences in profile memberships on mental health symptoms. Findings indicated that individuals in the “Latest AO for Substances” reported lowest levels of mental health symptoms compared to the other classes. There were no differences among the other classes on mental health symptoms. Thus, there was a distinct association that later AO across substances was characterized by fewer mental health symptoms related to anxiety, depression, and somatization. Although scant research has examined how AO across multiple substances is associated with mental health symptoms, our findings are in line with previous research suggesting that mental health symptoms are more likely to occur among individuals who use multiple substances.28 Our findings support delaying AO of substances may serve as a protective factor for mental health symptoms. Although, another plausible explanation may be that individuals with predisposing mental health symptoms initiated early use of multiple substances. Findings indicated that individuals who initiate alcohol, cannabis, and tobacco use prior to age 17 reported the highest levels of mental health symptoms.
Our findings have potential clinical implications. Among our sample of individuals with past-year alcohol, cannabis, and tobacco use, all individuals began using these substances individually during adolescence. Prevention efforts have been largely focused at delaying an individual’s AO for individual substances, but prevention efforts may want to consider delaying AO across multiple substances. Further, prevention and intervention efforts may want to consider polysubstance use behaviors in addition to targeting individual substances. Understanding the pattern of onset across multiple substances and polysubstance use behaviors may provide a clearer picture of use among high-risk individuals. Lastly, for adolescents and young adults, mental health symptoms should be assessed during prevention and intervention efforts. Findings from our study suggesting that individuals with an alcohol, cannabis, and tobacco AO prior to age 17 reported higher levels of mental health symptoms. Assessing mental health symptomology among individuals that engage in polysubstance use may determine who is at greatest risk for developing co-morbid substance use and mental health disorders.
The present study has several limitations. First, the sample was voluntary on an online platform (e.g., Craigslist) and may have been susceptible to bias. Participants were mostly men, and thus, generalizability to other populations (e.g., women) may be limited. Further, our sample included individuals who engaged in past year alcohol, tobacco, and cannabis use. The decision for this inclusion criteria was to examine how AO across multiple substances associated with recent co-use patterns of substances in young adulthood. However, findings may not generalize to individuals who do not engage in at least yearly use of these substances. Further, many participants engaged in frequent use of alcohol, cannabis, and tobacco use, and thus, findings may not be generalizable to individuals who use these substances less frequently. Future research could include individuals who have not recently used these substances to determine whether there are patterns of AO associated with infrequent and no current use of substances. Another limitation is that the data were based on retrospective self-reports and thus, data may have been susceptible to recall bias. Another limitation of this study utilized a cross-sectional design which limits our ability to make causal inferences. Although we controlled for several covariates in our models, future research should explore other covariates related to personality, family structure, or transitioning from adolescence to young adulthood and use which may impact substance use behaviors.47-50 The present study focused on a specific definition of onset (i.e., the age of one’s first use) and did not include other assessments, such as age of intoxication or age when regular use began, and we did not assess AO for other illicit drug use. Future research examining profiles of early use should consider patterns of first use to regular use and AO for other drug use to fully understand the development of polysubstance use. Lastly, we did not assess substance use disorder symptoms which may associated with early individual substance use and polysubstance use.
The present study was the first to identify profiles based on AO for alcohol, cannabis, and tobacco. In addition, specific profiles posed risk for individual substance use patterns of alcohol, cannabis, and tobacco use, co-use patterns of these substances, and other illicit drug use. Lastly, mental health symptomology was lowest among individuals who delayed AO across multiple substances. Our findings were in line with the gateway hypothesis, and we expanded on this area of research by identifying profiles of AO who may be at greatest substance use-related risk during young adulthood. Knowledge gained from this study may be used to design and improve tailored prevention and intervention programs for those most at-risk for substance use harms and mental health symptomology.
Acknowledgments
This research was supported by grant K01 AA018383 (PI: Cathy Lau-Barraco) from the National Institute on Alcohol Abuse and Alcoholism. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Schulenberg JE, Johnston LD, O'Malley PM, Bachman JG, Miech RA, Patrick ME. Monitoring the Future national survey results on drug use, 1975–2019: Volume II, college students and adults ages 19–60. https://monitoringthefuture.org/pubs.html#monographs. Ann Arbor: Institute for Social Research, The University of Michigan. Published 2020. [Google Scholar]
- 2.Cohn A, Villanti A, Richardson A, Rath JM, Williams V, Stanton C, Mermelstein R. The association between alcohol, marijuana use, and new and emerging tobacco products in a young adult population. Addict Behav. 2015;48:79–88. doi: 10.1016/j.addbeh.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 3.Fix BV, O’Connor RJ, Vogl L, Smith D, Bansal-Travers M, Conway KP, et al. Patterns and correlates of polytobacco use in the United States over a decade: NSDUH 2002–2011. Addict Behav. 2014;39(4):768–781. doi: 10.1016/j.addbeh.2013.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villanti AC, Cobb CO, Cohn AM, Williams VF, Rath JM. Correlates of hookah use and predictors of hookah trial in US young adults. Am J Prev Med. 2015;48(6):742–746. doi: 10.1016/j.amepre.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 5.Cohn A, Johnson A, Ehlke S, Villanti AC. Characterizing substance use and mental health profiles of cigar, blunt, and non-blunt marijuana users from the National Survey of Drug Use and Health. Drug and Alcohol Depend. 2016;160:105–111. doi: 10.1016/j.drugalcdep.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 6.Schauer GL, Berg CJ, Kegler MC, Donovan DM, Windle M. Assessing the overlap between tobacco and marijuana: Trends in patterns of co-use of tobacco and marijuana in adults from 2003–2012. Addict Behav. 2015;49:26–32. doi: 10.1016/j.addbeh.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Yurasek AM, Aston ER, Metrik J. Co-use of alcohol and cannabis: A review. Curr Addict Rep. 2017;4(2):184–193. doi: 10.1007/s40429-017-0149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agrawal A, Budney AJ, Lynskey MT. The co-occurring use and misuse of cannabis and tobacco: A review. Addict. 2012;107(7):1221–1233. doi: 10.1111/j.1360-0443.2012.03837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durazzo TC, Gazdzinski S, Meyerhoff DJ. The neurobiological and neurocognitive consequences of chronic cigarette smoking in alcohol use disorders. Alcohol Alcohol. 2007;42(3):174–185. doi: 10.1093/alcalc/agm020. [DOI] [PubMed] [Google Scholar]
- 10.Ebbert JO, Janney CA, Sellers TA, Folsom AR., Cerhan JR. The association of alcohol consumption with coronary heart disease mortality and cancer incidence varies by smoking history. J Gen Intern Med. 2005;20(1):14–20. doi: 10.1111/j.1525-1497.2005.40129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore BA, Budney AJ. Tobacco smoking in marijuana-dependent outpatients. J Subst Abuse Treat. 2001;13(4):583–596. doi: 10.1016/S0899-3289(01)00093-1. [DOI] [PubMed] [Google Scholar]
- 12.Schauer GL, Peters EN. Correlates and trends in youth co-use of marijuana and tobacco in the United States, 2005–2014. Drug and Alcohol Depend. 2018;185:238–244. doi: 10.1016/j.drugalcdep.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 13.Behrendt S, Wittchen HU, Höfler M, Lieb R, Beesdo K. (2009). Transitions from first substance use to substance use disorders in adolescence: is early onset associated with a rapid escalation?. Drug and Alcohol Depend. 2009;99(1-3):68–78. doi: 10.1016/j.drugalcdep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 14.Dawson DA, Goldstein RB, Patricia Chou S, June Ruan W, Grant BF. Age at first drink and the first incidence of adult-onset DSM-IV alcohol use disorders. Alcohol Clin Exp Res. 2008;32(12):2149–2160. doi: 10.1111/j.1530-0277.2008.00806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kandel D, Faust R. Sequence and stages in patterns of adolescent drug use. Arch Gen Psychiatry. 1975;32(7):923–932. doi: 10.1001/archpsyc.1975.01760250115013. [DOI] [PubMed] [Google Scholar]
- 16.Behrendt S, Beesdo-Baum K, Höfler M, Perkonigg A, Bühringer G, Lieb R, Wittchen HU. The relevance of age at first alcohol and nicotine use for initiation of cannabis use and progression to cannabis use disorders. Drug and Alcohol Depend. 2012;123(1-3):48–56. doi: 10.1016/j.drugalcdep.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 17.Ramo DE, Liu H, Prochaska JJ. Tobacco and marijuana use among adolescents and young adults: a systematic review of their co-use. Clin Psychol Rev. 2012;32(2):105–121. doi: 10.1016/j.cpr.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buu A, Dabrowska A, Mygrants M, Puttler LI, Jester JM, Zucker RA. Gender differences in the developmental risk of onset of alcohol, nicotine, and marijuana use and the effects of nicotine and marijuana use on alcohol outcomes. J Stud Alcohol Drugs, 2014;75(5):850–858. doi: 10.15288/jsad.2014.75.850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson KM, Sher KJ, Cooper ML, Wood PK. Adolescent alcohol and tobacco use: onset, persistence and trajectories of use across two samples. Addict. 2012;97(5):517–531. doi: 10.1046/j.1360-0443.2002.00082.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moss HB, Chen CM, Yi HY. Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug and Alcohol Depend. 2014;136:51–62. doi: 10.1016/j.drugalcdep.2013.12.011 [DOI] [PubMed] [Google Scholar]
- 21.Muthen BO, Muthen LK. The development of heavy drinking and alcohol-related problems from ages 18 to 37 in a US national sample. J Stud Alcohol. 2000;61(2):290–300. doi: 10.15288/jsa.2000.61.290. [DOI] [PubMed] [Google Scholar]
- 22.Richmond-Rakerd LS, Slutske WS, Wood PK. Age of initiation and substance use progression: A multivariate latent growth analysis. Psychol Addict Behav. 2017;31(6):664. doi: 10.1037/adb0000304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychaitry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 24.Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20(2):173–189. doi: 10.1016/S0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- 25.Caldwell TM, Rodgers B, Jorm AF, Christensen H, Jacomb PA, Korten AE, Lynskey MT. Patterns of association between alcohol consumption and symptoms of depression and anxiety in young adults. Addict, 2012;97(5):583–594. doi: 10.1046/j.1360-0443.2002.00092.x. [DOI] [PubMed] [Google Scholar]
- 26.Agosti V, Nunes E, Levin F. Rates of psychiatric comorbidity among US residents with lifetime cannabis dependence. Am J Drug Alcohol Abuse, 2002;28(4):643–652. doi: 10.1081/ADA-120015873. [DOI] [PubMed] [Google Scholar]
- 27.Ziedonis D, Hitsman B, Beckham JC, Zvolensky M, Adler LE, Audrain-McGovern J, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine Tob Res., 2008;10(12):1691–1715. doi: 10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]
- 28.Kelly AB, Chan GC, Mason WA, Williams JW. The relationship between psychological distress and adolescent polydrug use. Psychol Addict Behav. 2015;29(3):787. doi: 10.1037/adb0000068. [DOI] [PubMed] [Google Scholar]
- 29.Salom CL, Betts KS, Williams GM, Najman JM, Alati R. Predictors of comorbid polysubstance use and mental health disorders in young adults—a latent class analysis. Addict. 2016;111(1):156–164. doi: 10.1111/add.13058. [DOI] [PubMed] [Google Scholar]
- 30.Donovan JE. Adolescent alcohol initiation: A review of psychosocial risk factors. J Adolesc Health. 2004;35(6):529-e7–529.e18. doi: 10.1016/j.jadohealth.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Pedrelli P, Shapero B, Archibald A, Dale C. Alcohol use and depression during adolescence and young adulthood: A summary and interpretation of mixed findings. Curr Addict Rep. 2016;3(1):91–97. doi: 10.1007/s40429-016-0084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chaiton MO, Cohen JE, O'Loughlin J, Rehm J. A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC Public Health. 2009;9(1):356. doi: 10.1186/1471-2458-9-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wellman RJ, Dugas EN, Dutczak H, O’Loughlin EK, Datta GD, Lauzon B, O’Loughlin J. Predictors of the onset of cigarette smoking: A systematic review of longitudinal population-based studies in youth. Am J Prev Med. 2016;51(5):767–778. doi: 10.1016/j.amepre.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 34.Azagba S, Asbridge M. Age of first use, current marijuana use and driving after use among Canadian high school students. Addict Behav. 2019;90:329–333. doi: 10.1016/j.addbeh.2018.11.042. [DOI] [PubMed] [Google Scholar]
- 35.Stamates AL, Lau-Barraco C, Linden-Carmichael AN. Alcohol expectancies mediate the relationship between age of first intoxication and drinking outcomes in college binge drinkers. Subst Use Misuse, 2016;51(5):598–607. doi: 10.3109/10826084.2015.1126745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. J Consult Clin Psychol. 1985;53(2):189. [DOI] [PubMed] [Google Scholar]
- 37.Collins RL, Bradizza CM, Vincent PC. Young-adult malt liquor drinkers: Prediction of alcohol problems and marijuana use. Psychol Addict Behav. 2007;21(2):138. doi: 10.1037/0893-164X.21.2.138. [DOI] [PubMed] [Google Scholar]
- 38.Pearson MR, Hustad JT, Neighbors C, Conner BT, Bravo AJ, Marijuana Outcomes Study Team. Personality, marijuana norms, and marijuana outcomes among college students. Addict Behav. 2018;76:291–297. doi: 10.1016/j.addbeh.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 39.Martin CS, Clifford PR, Maisto SA, Earleywine M, Kirisci L, et al. Polydrug use in an inpatient treatment sample of problem drinkers. Alcohol Clin Exp Res. 1996;20(3):413–417. doi: 10.1111/j.1530-0277.1996.tb01067.x. [DOI] [PubMed] [Google Scholar]
- 40.Derogatis LR, Fitzpatrick M. The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18. In: Maruish ME, eds. The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults. 3rd ed. Mahwah, NJ: Lawrence Erlbaum Associates; 2004:1–41. [Google Scholar]
- 41.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Struct Equ Modeling. 2007;14(4):535–569. doi: 10.1080/10705510701575396. [DOI] [Google Scholar]
- 42.Wang J, Wang X. Structural equation modeling: Applications using Mplus. 1st ed. Chichester, UK: John Wiley & Sons Ltd; 2012. [Google Scholar]
- 43.Nkansah-Amankra S, Minelli M. “"Gateway hypothesis" and early drug use: Additional findings from tracking a population-based sample of adolescents to adulthood.” Prev Med Rep. 2016;4:134–141. doi: 10.1016/j.pmedr.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tarter RE, Vanyukov M, Kirisci L, Reynolds M, Clark DB. Predictors of marijuana use in adolescents before and after licit drug use: examination of the gateway hypothesis. Am J Psychiatry. 2006;163(12):2134–2140. [DOI] [PubMed] [Google Scholar]
- 45.Spear LP. Adolescent alcohol exposure: Are there separable vulnerable periods within adolescence?. Physiol Behav. 2015;148:122–130. doi: 10.1016/j.physbeh.2015.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wade NE, Thomas AM, Gruber SA, Tapert SF, Filbey FM, Lisdahl KM. Binge and cannabis co-use episodes in relation to white matter integrity in emerging adults. Cannabis Cannabinoid Res. 2020;5(1):62–72. doi: 10.1089/can.2018.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Peterson SJ, Davis HA, Smith GT. Personality and learning predictors of adolescent alcohol consumption trajectories. J Abnorm Psychol. 2018;127:482–495. doi: 10.1037/abn0000351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nelson SE, Van Ryzin MJ, Dishion TJ. Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: Demographic correlates and young adult substance use problems. Dev Psychopathol. 2014;27:253–277. doi: 10.1017/S0954579414000650. [DOI] [PubMed] [Google Scholar]
- 49.Clergue-Duval V, Mary-Krause M, Bolze C, et al. Early predictors of trajectories of tobacco use level from adolescence to young adulthood: A 16-year follow-up of the TEMPO Cohort Study (1999-2015). Eur Addict Res. 2019;25:2–9. doi: 10.1159/000495759. [DOI] [PubMed] [Google Scholar]
- 50.Walden B, Iacono WG, McGue M. Trajectories of change in adolescent substance use and symptomatology: Impact of paternal and maternal substance use disorders. Psychol Addict Behav. 2007;21:35–43. doi: 10.1037/0893-164X.21.1.35. [DOI] [PubMed] [Google Scholar]
- 51.Windle M, Windle RC. Early onset problem behaviors and alcohol, tobacco, and other substance use disorders in young adulthood. Drug Alcohol Depend. 2012;121:152–158. doi: 10.1016/j.drugalcdep.2011.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]


