Abstract
Context
Football continues to demonstrate the highest rate of sport-related concussion (SRC) in high school athletics. To mitigate the SRC risk, the Michigan High School Athletic Association (MHSAA) implemented rules aimed at reducing the number of collisions occurring in practices.
Objective
To estimate the rates of SRC in MHSAA football programs and evaluate progressive limitations to collision practices over 5 consecutive seasons.
Design
Retrospective cohort study.
Setting
Michigan high school football.
Patients or Other Participants
High school (9th–12th grade) football athletes (>99% male) participating in MHSAA-sanctioned events.
Main Outcome Measure(s)
Designated administrators at each school recorded the total number of participating athletes and SRCs (defined as head injuries resulting from athletic participation that required the student-athletes to be withheld from activity after exhibiting signs, symptoms, or behaviors consistent with an SRC) in the MHSAA injury-surveillance system each season (2015–2016 through 2019–2020). Progressive limitations to collision practices occurred across the study period. We estimated athlete-exposures (AEs) as the total number of players multiplied by the total number of possible practices (11 weeks, 4 days each) or competitions (9 weeks, 1 day each) during each season. Incidence rates and rate ratios (RRs) with 95% CIs were used to compare practice and competition SRCs and each season with the most recent season.
Results
A total of 7755 football SRCs were diagnosed across the 5-year period. The overall SRC rate was 8.03 per 10 000 AEs (95% CI = 7.85, 8.21). The competition SRC rate (30.13/10 000 AEs) was higher than the practice rate (3.51/10 000 AEs; RR = 8.58; 95% CI = 8.19, 9.00). The practice SRC rate was lower in 2017–2018 (RR = 0.86; 95% CI = 0.77, 0.97), 2018–2019 (RR = 0.89; 95% CI = 0.79, 1.0), and 2019–2020 (RR = 0.83; 95% CI = 0.74, 0.94) relative to 2015–2016.
Conclusions
We found that the progressive limitations to collision practices were protective against SRCs, as the rate of SRC was lower in the 3 most recent seasons relative to 2015–2016.
Keywords: American football, epidemiology, policies, injury prevention
Key Points
The overall estimated sport-related concussion (SRC) rate in high school football was 8.03 per 10 000 athlete-exposures, with higher rates occurring during competitions compared with practices.
Estimated practice SRC rates decreased after the implementation of rules restricting the amount of allowed collision time.
Estimated competition SRC rates also decreased across the study period, suggesting that risk mitigation occurred in competition when collision limitations in practice were imposed.
Football has the highest incidence of sport-related concussion (SRC) among high school athletes.1 Recent authors2 using statewide surveillance found SRCs in football players to be as high as 16.0/10 000 athlete-exposures (AEs). Researchers studying other high school populations reported an injury rate of 9.2/10 000 AEs3 based on the National Athletic Treatment, Injury and Outcomes Network database and 10.4/10 000 AEs1 based on the High School Reporting Information Online database. Moreover, the literature1,4,5 suggests that the risk of SRC in high school football is particularly elevated in competition, being 5 to 7 times higher than the risk of SRC in practice. Over the 5-year period from the 2013–2014 through 2017–2018 academic years, high school football competition concussion rates in the US increased from 33.2 to 39.1 per 10 000 AEs, whereas practice concussion rates decreased from 5.47 to 4.44 per 10 000 AEs.1 However, practice SRCs still accounted for 36% to 58% of all concussions.1,6,7 Although all 50 states and the District of Columbia have youth concussion laws, these laws do not limit the number of contact practices. Therefore, numerous organizations have implemented rule changes to try to mitigate the risk for SRC.
Over the past decade, the National Football League (NFL) and National Collegiate Athletic Association (NCAA) have implemented rule changes in football. For example, the NFL moved the kickoff up 5 yd (4.62 m), modified where the returning team can stand on a kickoff, and changed blocking rules for the returning player.8 Both the NFL and the NCAA now allow the ball to be placed on the 25-yd line for a touchback; the latter allows a fair catch anywhere within 25 yards. Individual NCAA conferences have also changed rules in hope of decreasing SRCs. The Ivy League not only added the touchback rule of 25 yards but also changed the kickoff line to 40 yards. These changes resulted in a decrease in SRCs.9 Recently, the Ivy League limited the number of contact practices, which, combined with the touchback rule, resulted in 81% fewer SRCs on kickoffs.9
Similarly, at the high school level, in 2014, the National Federation of State High School Associations recommended that states limit full-contact football practices. Consistent with that recommendation, the Wisconsin Interscholastic Athletic Association limited the number of full-contact practices to 1 hour per week after the second week of games (week 1: no contact practices, week 2: 75 minutes).10 After the rule change, practice-related SRCs in Wisconsin high school football athletes decreased by 57%, whereas the SRCs occurring in competitions did not change.10 The Michigan High School Athletic Association (MHSAA) has made numerous rule changes over the past few years to try to decrease the number of head impacts and SRC risk. In 2014, MHSAA–sanctioned football teams were allowed to schedule only 1 collision practice per day in the preseason and 2 collision practices per week during the regular season.11 This rule change corresponded to a 42% decline in head-impact exposure as monitored in a single high school football program; however, because of the small sample size, whether a similar decline occurred in the overall SRC risk was uncertain.12 In 2016, the MHSAA recommended that in addition to the limit of 2 collision practices per week, collision practices should not exceed 90 total minutes per week. The 90-minutes-per-week limit to collision practices became a requirement the following year. The MHSAA further restricted practices in 2019, such that 2 weeks before the first competition (ie, preseason), teams may only practice for 6 hours total per week. In addition, after the first competition, collision practices were limited to 30 minutes per week. No researchers to date have examined whether these rule changes resulted in a decrease in practice and competition SRCs. Therefore, the purpose of our study was to estimate the rates of SRCs in high school football athletes (ie, 9th to 12th grade) participating at the freshman, junior varsity, or varsity competition level to evaluate the effect of rule changes over 5 seasons. We compared incidence rates per 100 players per season between practice and competition and compared incidence rates for the most recent football season relative to prior seasons, separately for practice and competition. We hypothesized that, because the greatest limitations to contact practice time were in the most recent season, the 2019–2020 athletic season would have a lower SRC rate relative to prior seasons.
METHODS
The MHSAA prospectively records the total numbers of participating athletes and circumstances of each SRC occurring in athletic-sanctioned events. We obtained data for the 2015–2016 through the 2019–2020 football seasons from the surveillance system, including all 9th- through 12th-grade participants. The Michigan State University Institutional Review Board approved this study as exempt because the data were deidentified.
Data Reporting and Definitions
Data Reporting
The MHSAA initiated the surveillance system in 2015–2016. Details on the MHSAA surveillance system have been previously described.13,14 The MHSAA requires each SRC to be recorded via an online repository. Primary data recorders at each school include athletic trainers (ATs); in the absence of ATs, coaches, school officials, or both provide the required data entry. Coaches, school officials, and ATs were responsible only for being the primary data recorders and did not confirm or diagnose concussions. Unique identification codes were given to each SRC case to ensure anonymity of the data. Accordingly, subsequent SRCs were recorded as separate injuries and could not be matched to individual athletes. Staff at the MHSAA regularly monitored data entries; if an error was identified, the staff contacted the school for clarification. Schools that recorded no SRCs in a season were required to indicate that zero occurred; MHSAA staff followed up with schools in such instances to ensure full capture of the data. The MHSAA deemed data collection complete when no fewer than 99% of member schools had completed their SRC reports. Sanctions existed for noncompliance with SRC management policies. Only MHSAA staff members were authorized to edit the SRC reports once submitted.
Progressive Limitations to Collision Practice
Across the 5 seasons, MHSAA progressively limited the time for collision practices. In 2016–2017, the policy stated that teams could not conduct more than 2 collision practices per week after the first regular season game and recommended that collision practices not exceed 90 minutes. In 2017–2018, the policy changed, mandating that collision practices not exceed 90 minutes. No restrictions were added in 2018–2019. By the 2019–2020 season, the limitations had become the most restrictive: during the first 2 weeks before a contest, collision contact was limited to 6 hours per week, and after the first regular-season game, collision practice could not exceed 30 minutes in any week.
Sport-Related Concussion
An SRC was defined as (1) an injury that resulted from athletic participation during regular season (ie, preseason, in-season, and postseason) practices, scrimmages, or games for MHSAA–sanctioned events that provided a postseason tournament and (2) required the student-athlete to be withheld from activity after exhibiting signs, symptoms, or behaviors consistent with an SRC.15–19 All SRCs confirmed as true diagnoses were included in this study.
Characteristics of SRC Cases
For each SRC case, the demographic data included sex, grade, level of competition (ie, freshman, junior varsity, varsity), and previous concussion history (ie, yes or no). Characteristics of each SRC injury event data included the date of injury; date of authorized clearance; whether the injury occurred in a practice or game; whether the injury occurred at the start, middle, or end of the event; mechanism of injury (ie, contact with another player, contact with an object, uncertain); and initial evaluator (AT: yes or no). Authorized clearance to return was unconditional, meaning the athlete first completed a return-to-play progression. The only individuals able to provide written authorized clearance to return to unrestricted activity were a medical doctor, doctor of osteopathic medicine, nurse practitioner, or physician assistant. No other health care provider could authorize an athlete to return to sport.
Statistical Analysis
Descriptive statistics are presented for practice and competition SRCs each year. We calculated the incidence rate for SRCs per 100 players per season and 95% CIs by dividing the number of SRC cases by the total number of participants each season and multiplying by 100. We tested whether the mechanism of injury differed between practices and competitions using χ2 analysis. We also used logistic regression with robust SEs and 95% CIs to estimate the odds ratios (ORs) for AT involvement in the initial evaluation across seasons and completed a test for trend. Significance was set a priori at P < .05, and all P values were 2 sided.
The MHSAA schedules each team for 9 total regular-season games during the season, after 1.5 weeks of preseason practice. As not all teams go on to participate in postseason tournaments, we estimated AEs (player-days exposed) as the total number of players multiplied by the total number of possible practices (11 weeks, 4 days each) or competitions (9 weeks, 1 day each) each regular season. Using these estimated AEs, we calculated incidence rates and 95% CIs for the SRCs that occurred during the preseason and regular season. Using robust SEs, we applied logistic regression to determine ORs that provided estimates of rate ratios (RRs) and 95% CIs to compare the rate of SRCs in competition relative to practice and each season relative to the first and least restrictive season (2015–2016). The RRs were considered significant if the bounds of the 95% CI did not include 1. We conducted all analyses in StataCorp 2019 (version 16; StataCorp LLC).
RESULTS
A total of 7755 reported and confirmed SRC cases occurred in football during the 2015–2016 through 2019–2020 academic years. Missing and excluded data are presented in Figure 1. The largest proportion of SRCs occurred in athletes participating in varsity football, or the highest competitive level (46.2%; n = 3583 of 7755; Table 1). The largest proportion of cases occurred in 9th-grade football athletes (31.2%; n = 2417 of 7755), followed by 10th grade (27.9%; n = 2165 of 7755), 11th grade (20.4%; n = 1584 of 7755), and 12th grade (20.5%; n = 1589 of 7755). More than one-third (37.6%) of patients with SRC had a history of concussion. Approximately one-quarter of SRC cases (24.6%; n = 1905 of 7755) occurred during the 2015–2016 season, followed by the 2016–2017 season (21.0%, n = 1627 of 7755). The overall incidence rate for SRCs across all seasons was 4.38 per 100 players per season (95% CI = 4.28, 4.47). The incidence rate stratified by season is displayed in Table 2. Across all seasons, more than 60% of SRCs occurred in competition (63.8%; n = 4951 of 7755; Figure 2). The percentage of SRC cases that occurred across each week of the athletic season, in total and separately for practice and competition, is shown in Figure 3A through C. A majority of SRC cases (79.7%, n = 6181 of 7755) had an AT involved in the initial evaluation. Logistic regression using robust SEs revealed that the odds of AT involvement in the initial evaluation were higher in 2018–2019 (OR = 1.28; 95% CI = 1.07, 1.52; P = .006) and 2019–2020 (OR = 1.38; 95% CI = 1.16, 1.65; P ≤ .001) relative to 2015–2016. The test for trend similarly revealed that AT involvement increased across the 5 seasons (OR = 1.09; 95% CI = 1.05, 1.14; P ≤ .001).
Figure 1.
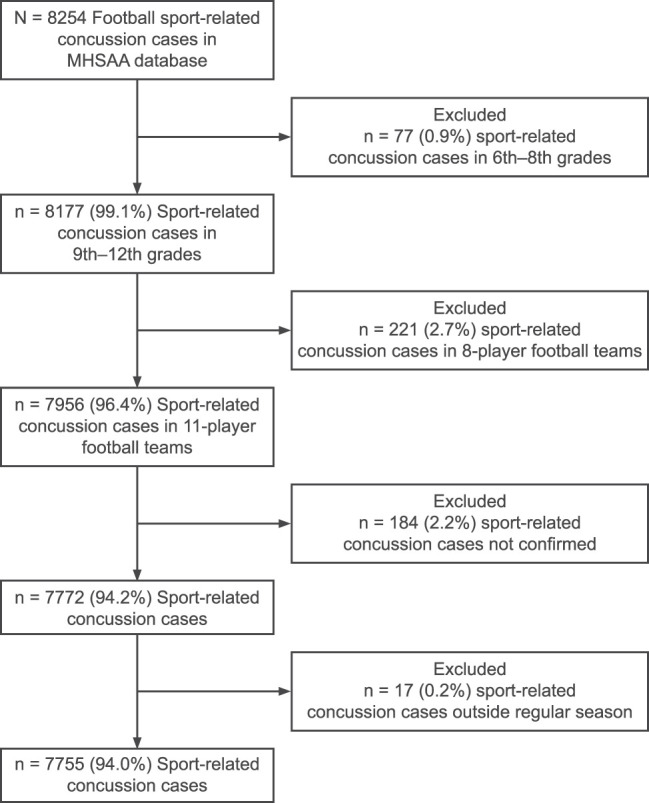
Michigan High School Athletic Association (MHSAA) head injury surveillance database.
Table 1.
Descriptive Characteristics of Sport-Related Concussion Cases Occurring in Michigan High School Athletic Association Football During the 2015–2016 Through 2019–2020 Athletic Seasons
| Characteristic |
No. (%) |
| Grade | |
| 9 | 2417 (31.2) |
| 10 | 2165 (27.9) |
| 11 | 1584 (20.4) |
| 12 | 1589 (20.5) |
| Level | |
| Varsity | 3583 (46.2) |
| Junior varsity | 2862 (36.9) |
| Freshman | 1310 (16.9) |
| Previous concussion history? | |
| Yes | 2897 (37.4) |
| No | 4858 (62.6) |
| Season | |
| 2015–2016 | 1905 (24.6) |
| 2016–2017 | 1627 (21.0) |
| 2017–2018 | 1423 (18.3) |
| 2018–2019 | 1437 (18.5) |
| 2019–2020 | 1363 (17.6) |
| Initial evaluation | |
| Athletic trainer | 6181 (79.7) |
| No athletic trainer | 1574 (20.3) |
Table 2.
Incidence Rate per 100 Players per Season of Sport-Related Concussion by Academic Year
| Season |
Sport-Related Concussions |
Participants, No. |
Incidence Rate |
95% CI |
| 2015–2016 | 1905 | 38 591 | 4.94 | 4.72, 5.16 |
| 2016–2017 | 1627 | 36 571 | 4.45 | 4.24, 4.67 |
| 2017–2018 | 1423 | 35 583 | 4.00 | 3.80, 4.21 |
| 2018–2019 | 1437 | 33 962 | 4.23 | 4.02, 4.45 |
| 2019–2020 | 1363 | 32 728 | 4.16 | 3.95, 4.39 |
| Overall | 7755 | 177 435 | 4.38 | 4.28, 4.47 |
Figure 2.
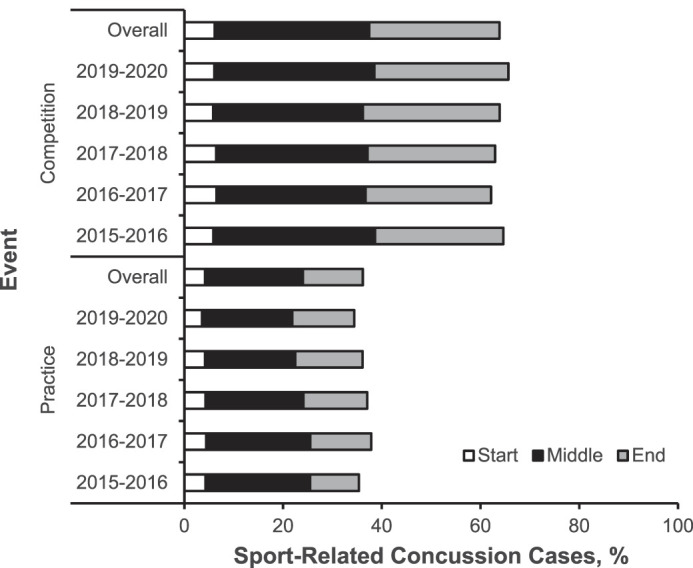
Sport-related concussions (SRCs) occurring in practice versus competition and timing during each practice or competition event. Timing of event refers to whether an SRC occurred at the start, middle, or end of a given practice or competition.
Figure 3.
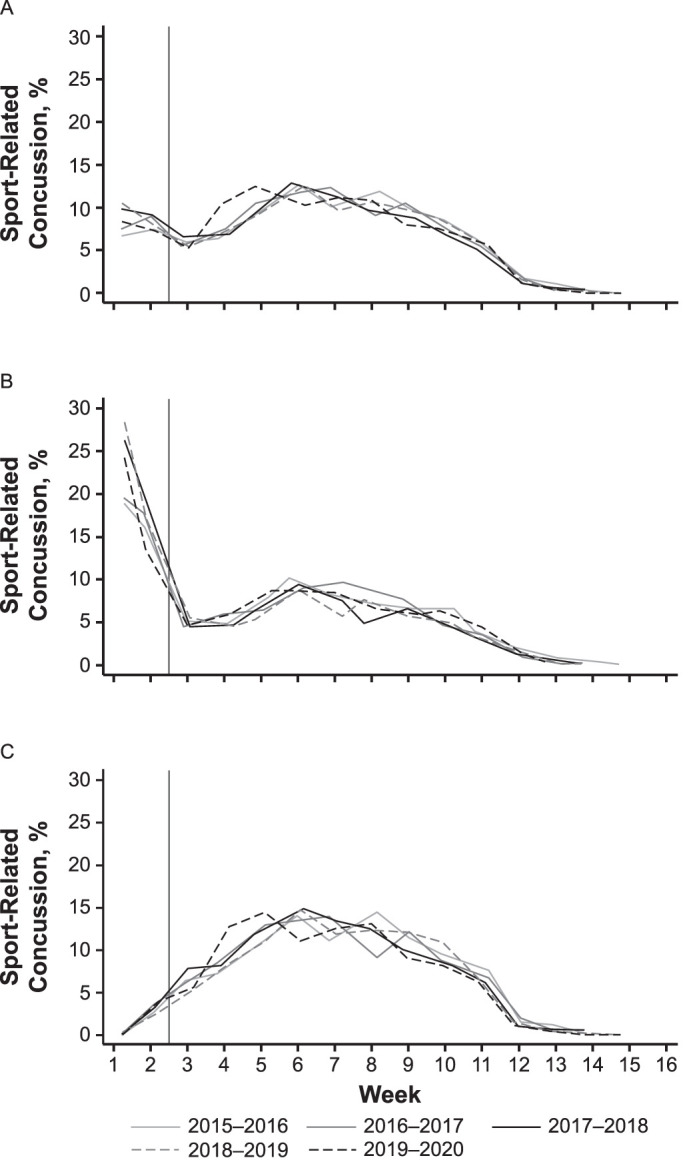
Sport-related concussions (SRCs) occurring in A, both practice and competition, and in B, practice, and C, competition, separately, each week throughout the season, by athletic season. The vertical line represents the end of the preseason and start of the regular season.
Almost three-fourths (73.7%, n = 5718 of 7755) of SRCs occurred because of contact with another person. Approximately 14% (13.7%, n = 1061 of 7755) occurred from person-to-object contact (eg, wall, ground, equipment), and for 12.6% (n = 976 of 7755), the cause of the injury was uncertain. For practice-related SRCs, the leading mechanism of injury was contact with another person (71.1%, n = 1994 of 2804), followed by 18.1% from contact with an object (n = 506 of 2804) and 10.8% (n = 304 of 2804) from an uncertain cause. The mechanism of injury varied as a function of play type (χ2 = 75.843, P < .001), with the majority of competition-related SRCs resulting from contact with another person (75.2%, n = 3724 of 4951), followed by an uncertain cause (13.6%, n = 672 of 4951) and contact with an object (11.2%, n = 555 of 4951).
Overall, the estimated rate of SRCs occurring during the regular season (weeks 1 to 11) across all seasons was 8.03 per 10 000 AEs (95% CI = 7.85, 8.21). The estimated rates of SRC overall and stratified by practice or competition across seasons are provided in Table 3. The rate of SRC was 8.58 (95% CI = 8.19, 9.00) times greater in competition (30.13 per 10 000 AEs; 95% CI = 29.28, 31.00) relative to practice (3.51 per 10 000 AEs; 95% CI = 3.38, 3.65). For practice, the rate of SRC was lower in 2017–2018 (RR = 0.86; 95% CI = 0.77, 0.97), 2018–2019 (RR = 0.89; 95% CI = 0.79, 1.0), and 2019–2020 (RR = 0.83; 95% CI = 0.74, 0.94) relative to the first, least restrictive season (ie, 2015–2016; Table 3). The 2016–2017 season did not differ relative to the 2015–2016 season. For competition, the rate of SRC was lower in 2016–2017 (RR = 0.86; 95% CI = 0.79, 0.94), 2017–2018 (RR = 0.79; 95% CI = 0.73, 0.87), 2018–2019 (RR = 0.85; 95% CI = 0.78, 0.93), and 2019–2020 (RR = 0.87; 95% CI = 0.80, 0.94) relative to 2015–2016.
Table 3.
Estimated Rate of Sport-Related Concussion (SRC) per 10 000 Athlete-Exposures (AEs) in Practice and Competition During the Regular Season (Weeks 1–11)
| Event |
Year |
SRCs |
No. of Players |
Weeks |
Days |
AEs |
SRCs per 10 000 AEs |
95% CI |
| Practice | 2015–2016 | 650 | 38 591 | 11 | 4 | 1 698 004 | 3.83 | 3.53, 4.12 |
| 2016–2017 | 607 | 36 571 | 11 | 4 | 1 609 124 | 3.77 | 3.47, 4.07 | |
| 2017–2018 | 516 | 35 583 | 11 | 4 | 1 565 652 | 3.30 | 3.01, 3.58 | |
| 2018–2019 | 508 | 33 962 | 11 | 4 | 1 494 328 | 3.40 | 3.10, 3.70 | |
| 2019–2020 | 460 | 32 728 | 11 | 4 | 1 440 032 | 3.19 | 2.90, 3.50 | |
| Overall | 2741 | 177 435 | 55 | 4 | 7 807 140 | 3.51 | 3.38, 3.65 | |
| Competition | 2015–2016 | 1191 | 38 591 | 9 | 1 | 347 319 | 34.29 | 32.4, 36.3 |
| 2016–2017 | 976 | 36 571 | 9 | 1 | 329 139 | 29.65 | 27.8, 31.6 | |
| 2017–2018 | 873 | 35 583 | 9 | 1 | 320 247 | 27.26 | 25.5, 29.1 | |
| 2018–2019 | 894 | 33 962 | 9 | 1 | 305 658 | 29.25 | 27.4, 31.2 | |
| 2019–2020 | 877 | 32 728 | 9 | 1 | 294 552 | 29.77 | 27.8, 31.8 | |
| Overall | 4811 | 177 435 | 45 | 1 | 1 596 915 | 30.13 | 29.28, 31.00 | |
| Overall | 7552 | 177 435 | 9 404 055 | 8.03 | 7.85, 8.21 |
In considering the most recent and restrictive season that specifically limited collision practice before the first competition, we compared the estimated SRC rates that occurred in practices during the first 2 weeks of the regular season. The SRC rate was lower in 2019–2020 (5.44 per 10 000 AEs; 95% CI = 4.67, 6.23) relative to 2018–2019 (6.98 per 10 000 AEs; 95% CI = 6.12, 7.93; RR = 0.78; 95% CI = 0.64, 0.95) and 2017–2018 (6.75 per 10 000 AEs, 95% CI = 5.92, 7.65; RR = 0.81; 95% CI = 0.66, 0.98). No other differences were observed between the most recent and restrictive season and prior seasons.
DISCUSSION
This large, prospective study of SRCs in a statewide football program demonstrated that the overall SRC incidence rate across the study period was 4.38 (95% CI = 4.28, 4.47) per 100 players per season. With respect to AEs, the estimated rate of SRC across all seasons was 8.03 per 10 000 AEs. Notably, a greater proportion of SRCs occurred in competition versus practice. Importantly, the estimated practice SRC rate decreased during the study period, suggesting that the restrictions progressively introduced for collision practices across 5 seasons of play were protective against SRC. Approximately 40% of practice-related SRCs occurred during the preseason. Furthermore, preseason practice SRC rates decreased in the most recent and restrictive season compared with earlier seasons, indicating a protective effect of limiting collision practices to no more than 30 minutes in a given preseason week.
We estimated exposure using total athlete participation (ie, documented roster size) and estimated practice and allowed competition days. The MHSAA schedules 9 days for contests during the regular season.20–24 Communications with local clinicians reflected that teams typically schedule 4 practices per week. Our estimated SRCs were similar to those in previous studies, which lends support to our approach. For example, in a statewide assessment of high school football, the overall SRC rate was 16.0 per 10 000 AEs.2 Separating SRCs occurring in competition versus practice, Kerr et al25 identified a practice SRC rate of 3.5 per 10 000 AEs and a competition SRC rate of 25.7 per 10 000 AEs in high school football during the 2005–2006 through 2013–2014 seasons. Similarly, in an investigation of SRC rates across 20 high school sports during the 2013–2014 through 2017–2018 athletic seasons, competition and practice SRC rates were 35.8 and 5.0 per 10 000 AEs in football, respectively.1 In the current study, the overall estimated rate of SRC was 8.03 per 10 000 AEs, with 30.13 per 10 000 AEs in competition and 3.51 per 10 000 AEs in practice, which aligns with previous literature.1,2,25
We found that the rate of SRC was 8 times higher in competition than in practice. This is in contrast to a recent report by McCrea et al26 that a greater proportion of concussions (72.0%) and head impacts (66.9%) occurred in practices relative to games among a sample of collegiate football players from 6 NCAA Division I programs instrumented with in-helmet sensors. Importantly, not all players participating on a given team were included and epidemiologic data were not collected. In contrast, when accounting for epidemiologic data, including AEs, earlier researchers1 observed a 7.2 times greater rate of SRCs in competition versus practice among high school football players. Higher rates of SRC in competition (3.7 per 1000 AEs) versus practice (1.0 per 1000 AEs) in middle school football and collegiate football (competition = 3.0 per 1000 AEs, practice = 0.4 per 1000 AEs) have also been seen.1,25,27 Despite the higher rates observed in competition, almost 40% of all SRCs in our sample resulted from practice. Moreover, by considering the week of the season when the SRCs occurred, we determined that 40% of all practice-related SRCs happened before the first competition. This was similar to the findings in a recent study of collegiate football athletes, suggesting that 48.5% of SRCs and 66.7% of all head-impact exposures occurred during the preseason.26 Accordingly, these high percentages of SRCs and head-impact exposures, paired with our identification of player-to-player contact as the most common mechanism of injury, provide evidence that SRCs can be mitigated by limiting collision practices, especially during the preseason.
Over the course of the 5 athletic seasons, the MHSAA progressively limited the time allowed for contact practices, with the 2019–2020 season being the most restrictive. We noted a lower estimated rate of SRC in 2019–2020 relative to the 2015–2016 season. Moreover, in the most recent season that specifically targeted the preseason, after collision practices had been limited to no more than 30 minutes per week, we also found a lower estimated rate of preseason practice-related SRC in 2019–2020 relative to the 2018–2019 estimated preseason practice rate. We are not the first to report a protective influence of policy changes in football. In the Ivy League, limiting the number of contact practices combined with the 25-yd line touchback rule and the 40-yd line kickoff rule resulted in 81% fewer SRCs during kickoffs.9 Further, in the high school setting, limiting the number of full-contact practices to 1 hour per week after the second week of games resulted in a 57% reduction of SRCs in practice.10 Among 11- to 15-year-old youth football athletes, a football coaching education program (USA Football: “Heads Up Football”) paired with Pop Warner Football restriction guidelines to limit contact during practice resulted in decreased practice-related SRC rates compared with youth football teams not affiliated with either program.6 Along with decreasing SRCs, policy changes are also suggested to decrease head-impact exposure in high school12 and collegiate28,29 football settings.
Limitations
This study was not without limitations. First, the database did not include the ages of athletes, and therefore, our information was restricted to their grade in school and level of participation; however, each athlete participated at the high school athletic level. In addition, we could not match each SRC to the team of participation, and thus, could not adjust for clustering in our analysis. Based on simulation analyses,30 we expect this would not have biased the relative rate estimates but might have either reduced or increased the precision of the P values and CIs depending on the prevalence of the exposure in a given analysis. Hence our use of robust SEs, in an attempt to be conservative in our conclusions about whether rule changes led to reductions in SRC. Furthermore, a threat to the validity of our conclusions was that temporal trends that we did not account for may have influenced SRC rates over the study period. For example, SRC rates could have increased during the study period if SRC awareness and proper recognition and management of the injury increased. The rising values would then not reflect a true rate increase but rather an increase in the frequency of detection. Indeed, the incidence of diagnosed concussions markedly increased by 115% and 132% in 2017 and 2018, respectively, compared with 2013 according to the electronic health records of a large US health system.31 Also, in the high school athletics setting, schools with AT access exhibited higher rates of SRC than those with no AT access.32,33 Notably, having an AT involved in an initial SRC evaluation was associated with subsequent management practices, including medical facilities at which athletes were cleared for unrestricted return.34 We observed that the proportion of SRC cases with an AT involved in the initial evaluation increased from 78% in 2015–2016 to 83.1% in 2019–2020. This may have created bias toward the null in our estimates, as previous authors32,33 reported increased SRCs in the presence of ATs, attributable to proper recognition and management. Even so, our results indicate that an increase in rule restrictiveness led to a decrease in SRC rates.
Still, other changes to high school football may have occurred that we did not take into account. For example, 1 Michigan high school introduced helmetless tackling in practice during the study period, based on the impression that it might decrease the frequency of head impacts across a season. Although we know of no other instances, training techniques may vary in additional ways, and no system exists for enumerating tackling and training techniques. We are not aware of any systemwide changes during the study period that could account for the SRC reductions that we are attributing to the policy changes at our focus. Moreover, football players have a history of nondisclosure of SRC.35,36 If that hesitation attenuated over the study period, the result would only be bias toward the null in our finding that increasing rule restrictions corresponded with a decrease in SRC rates. Finally, as SRCs occurred, athletes were likely absent from a number of practice and competition events. Our approach to calculating exposure did not account for such time out in the way that athletes would be censored and did not contribute further time to the denominator, as occurs with a survival analysis. This is not a study limitation but rather a feature of our work, which used total possible time exposed as the method for estimating SRCs rates. Other limitations included the lack of multiple comparisons and the lack of an a priori sample-size calculation. Ultimately, the study had considerable strengths, including focusing on high school football only, which provides a homogeneous context for evaluating a rule change, and the large number of high schools that participated in this statewide surveillance system.
CONCLUSIONS
We reported an estimated SRC rate of 8.03 per 10 000 AEs in the regular season (weeks 1 to 11); however, the competition rate (30.13 per 10 000 AEs; 95% CI = 29.28, 31.00) was 8.58 (95% CI = 8.19, 9.00) times greater relative to practice (3.51 per 10 000 AEs; 95% CI = 3.38, 3.65). The primary mechanism of injury was person-to-person contact. Across the 5-year study period, SRC rates during practice decreased in conjunction with the progressive rollout of rules restricting collision practice times. These findings are evidence that rules can effectively protect against SRC by limiting unnecessary collisions between student-athletes. The effect was especially apparent during the preseason, in which we saw lower rates of SRC in the most recent and most restrictive season (ie, 2019–2020) relative to 2018–2019 (RR = 0.78; 95% CI = 0.64, 0.95) and 2017–2018 (RR = 0.81; 95% CI = 0.66, 0.98).
Sport-related concussions remain a common injury in high school football players, but the MHSAA's restrictive collision rules appear effective in reducing practice SRC rates. These results support the movement toward implementing rules targeted at reducing the number of unnecessary collisions in football at multiple competitive levels. Furthermore, these findings can serve as an empirical backing for other state high school athletic associations that are considering implementing such policies.
REFERENCES
- 1.Kerr ZY, Chandran A, Nedimyer AK, Arakkal A, Pierpoint LA, Zuckerman SL. Concussion incidence and trends in 20 high school sports. Pediatrics . 2019;144(5):e20192180. doi: 10.1542/peds.2019-2180. [DOI] [PubMed] [Google Scholar]
- 2.Chun BJ, Furutani T, Oshiro R, Young C, Prentiss G, Murata N. Concussion epidemiology in youth sports: sports study of a statewide high school sports program. Sports Health . 2021;13(1):18–24. doi: 10.1177/1941738120932570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Connor KL, Baker MM, Dalton SL, Dompier TP, Broglio SP, Kerr ZY. Epidemiology of sport-related concussions in high school athletes: National Athletic Treatment, Injury and Outcomes Network (NATION), 2011–2012 through 2013–2014. J Athl Train . 2017;52(3):175–185. doi: 10.4085/1062-6050-52.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartley JH, Murray MF, Kraeutler MJ, et al. Epidemiology of injuries sustained as a result of intentional player contact in high school football, ice hockey, and lacrosse: 2005–2006 through 2015–2016. Orthop J Sports Med . 2017;5(12):2325967117740887. doi: 10.1177/2325967117740887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hammer E, Brooks MA, Hetzel S, Arakkal A, Comstock RD. Epidemiology of injuries sustained in boys' high school contact and collision sports, 2008–2009 through 2012–2013. Orthop J Sports Med . 2020;8(2):2325967120903699. doi: 10.1177/2325967120903699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dompier TP, Kerr ZY, Marshall SW, et al. Incidence of concussion during practice and games in youth, high school, and collegiate American football players. JAMA Pediatr . 2015;169(7):659–665. doi: 10.1001/jamapediatrics.2015.0210. [DOI] [PubMed] [Google Scholar]
- 7.McGuine TA, Hetzel S, McCrea M, Brooks MA. Protective equipment and player characteristics associated with the incidence of sport-related concussion in high school football players: a multifactorial prospective study. Am J Sports Med . 2014;42(10):2470–2478. doi: 10.1177/0363546514541926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Health & safety rules changes NFL Football Operations Web site https://operations.nfl.com/football-ops/nfl-ops-honoring-the-game/health-safety-rules-changes/ Accessed November 15 . 2020.
- 9.Wiebe DJ, D'Alonzo BA, Harris R, Putukian M, Campbell-McGovern C. Association between the experimental kickoff rule and concussion rates in Ivy League football. JAMA . 2018;320(19):2035–2036. doi: 10.1001/jama.2018.14165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pfaller AY, Brooks MA, Hetzel S, McGuine TA. Effect of a new rule limiting full contact practice on the incidence of sport-related concussion in high school football players. Am J Sports Med . 2019;47(10):2294–2299. doi: 10.1177/0363546519860120. [DOI] [PubMed] [Google Scholar]
- 11.Johnson J, Kimmerly G. New football practice policies promote safety as 14–15 sports year begins Michigan High School Athletic Association 2014 Accessed November 15 2020 https://www.mhsaa.com/News/PressReleases/articleType/ArticleView/articleId/3093/New-Football-Practice-Policies-Promote-Safety-as14-15-Sports-Year-Begins .
- 12.Broglio SP, Williams RM, O'Connor KL, Goldstick J. Football players' head-impact exposure after limiting of full-contact practices. J Athl Train . 2016;51(7):511–518. doi: 10.4085/1062-6050-51.7.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bretzin AC, Covassin T, Fox ME, et al. Sex differences in the clinical incidence of concussions, missed school days, and time loss in high school student-athletes: part 1. Am J Sports Med . 2018;46(9):2263–2269. doi: 10.1177/0363546518778251. [DOI] [PubMed] [Google Scholar]
- 14.Covassin T, Petit KM, Savage JL, et al. Sports-related concussion occurrence at various time points during high school athletic events: part 2. Am J Sports Med . 2018;46(9):2270–2276. doi: 10.1177/0363546518780225. [DOI] [PubMed] [Google Scholar]
- 15.Summary report Michigan High School Athletic Association head injury reporting system 2016–2017 school year Michigan High School Athletic Association Accessed October 14. 2021. https://www.mhsaa.com/portals/0/documents/health%20safety/concussionreport1617.pdf .
- 16.Summary report Michigan High School Athletic Association head injury reporting system 2015–2016 school year Michigan High School Athletic Association Accessed October 14. 2021. https://www.mhsaa.com/portals/0/documents/health%20safety/concussionreport1516.pdf .
- 17.Summary report Michigan High School Athletic Association head injury reporting system 2017–2018 school year Michigan High School Athletic Association Accessed October 14. 2021. https://www.mhsaa.com/portals/0/documents/health%20safety/concussionreport1718.pdf .
- 18.Summary report Michigan High School Athletic Association head injury reporting system 2018–2019 school year Michigan High School Athletic Association Accessed October 14. 2021. https://www.mhsaa.com/portals/0/Documents/health%20safety/concussionreport18-19.pdf .
- 19.Summary report Michigan High School Athletic Association head injury reporting system 2019–2020 school year Michigan High School Athletic Association Accessed October 14. 2021. https://www.mhsaa.com/portals/0/Documents/health%20safety/concussionreport19-20.pdf .
- 20.MHSAA 2015–16 calendar. Michigan High School Athletic Association Accessed May 10 2021. https://www.mhsaa.com/portals/0/documents/15-16calendar.pdf .
- 21.MHSAA 2016–17 calendar. Michigan High School Athletic Association Accessed May 5 2021. https://www.mhsaa.com/portals/0/documents/16-17calendar.pdf .
- 22.MHSAA 2017–18 calendar. Michigan High School Athletic Association Accessed May 10 2021. https://www.mhsaa.com/portals/0/documents/17-18calendar.pdf .
- 23.MHSAA 2018–19 calendar. Michigan High School Athletic Association Accessed May 10 2021. https://www.mhsaa.com/portals/0/documents/18-19calendar.pdf .
- 24.MHSAA 2019–20 calendar. Michigan High School Athletic Association Accessed May 10 2021. https://www.mhsaa.com/portals/0/documents/19-20calendar.pdf .
- 25.Kerr ZY, Wilkerson GB, Caswell SV, et al. The first decade of web-based sports injury surveillance: descriptive epidemiology of injuries in United States high school football (2005–2006 through 2013–2014) and National Collegiate Athletic Association football (2004–2005 through 2013–2014) J Athl Train . 2018;53(8):738–751. doi: 10.4085/1062-6050-144-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCrea MA, Shah A, Duma S, et al. Opportunities for prevention of concussion and repetitive head impact exposure in college football players: a Concussion Assessment, Research, and Education (CARE) Consortium study. JAMA Neurol . 2021;78(3):346–350. doi: 10.1001/jamaneurol.2020.5193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kerr ZY, Cortes N, Ambegaonkar JP, et al. The epidemiology of injuries in middle school football, 2015–2017: the Advancing Healthcare Initiatives for Underserved Students project. Am J Sports Med . 2019;47(4):933–941. doi: 10.1177/0363546518825361. [DOI] [PubMed] [Google Scholar]
- 28.Stemper BD, Shah AS, Harezlak J, et al. CARE Consortium Investigators. Repetitive head impact exposure in college football following an NCAA rule change to eliminate two-a-day preseason practices: a study from the NCAA-DoD CARE Consortium. Ann Biomed Eng . 2019;47(10):2073–2085. doi: 10.1007/s10439-019-02335-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stemper BD, Shah AS, Mihalik JP, et al. Head impact exposure in college football after a reduction in preseason practices. Med Sci Sports Exerc . 2020;52(7):1629–1638. doi: 10.1249/MSS.0000000000002283. [DOI] [PubMed] [Google Scholar]
- 30.Ntani G, Inskip H, Osmond C, Coggon D. Consequences of ignoring clustering in linear regression. BMC Med Res Methodol . 2021;21(1):139. doi: 10.1186/s12874-021-01333-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Askow AT, Erickson JL, Jagim AR. Recent trends in youth concussions: a brief report. J Prim Care Community Health . 2020;11:2150132720985058. doi: 10.1177/2150132720985058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McGuine TA, Pfaller AY, Post EG, Hetzel SJ, Brooks A, Broglio SP. The influence of athletic trainers on the incidence and management of concussions in high school athletes. J Athl Train . 2018;53(11):1017–1024. doi: 10.4085/1062-6050-209-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pierpoint LA, LaBella CR, Collins CL, Fields SK, Comstock RD. Injuries in girls' soccer and basketball: a comparison of high schools with and without athletic trainers. Inj Epidemiol . 2018;5(1):29. doi: 10.1186/s40621-018-0159-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bretzin AC, Zynda AJ, Wiebe DJ, Covassin T. Time to authorized clearance from sport-related concussion: the influence of healthcare provider and medical facility. J Athl Train . 2020;56(8):869–878. doi: 10.4085/JAT0159-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kerr ZY, Register-Mihalik JK, Kay MC, DeFreese JD, Marshall SW, Guskiewicz KM. Concussion nondisclosure during professional career among a cohort of former National Football League athletes. Am J Sports Med . 2018;46(1):22–29. doi: 10.1177/0363546517728264. [DOI] [PubMed] [Google Scholar]
- 36.Kerr ZY, Register-Mihalik JK, Kroshus E, Baugh CM, Marshall SW. Motivations associated with nondisclosure of self-reported concussions in former collegiate athletes. Am J Sports Med . 2016;44(1):220–225. doi: 10.1177/0363546515612082. [DOI] [PMC free article] [PubMed] [Google Scholar]


