Abstract
Context/Objective
To describe patient experiences with fracture prevention and management among persons with spinal cord injuries/disorders (SCI/D).
Design
Qualitative data collected via semi-structured telephone interviews.
Setting
Veterans Health Administration (VA) SCI/D System of Care.
Participants
Veterans with SCI/D (n = 32) who had experienced at least one lower-extremity fracture in the prior 18 months.
Interventions
N/A.
Outcome Measures
Interview questions addressed patients’: pre-fracture knowledge of osteoporosis and bone health, diagnosis and management of osteoporosis, history and experiences with fracture treatment, and post-fracture care and experiences.
Results
Participants expressed concerns about bone health and fractures in particular, which for some, limited activities and participation. Participants recalled receiving little information from providers about bone health or osteoporosis and described little knowledge about osteoporosis prevention prior to their fracture. Few participants reported medication management for osteoporosis, however many reported receiving radiographs/scans to confirm a fracture and most reported being managed non-operatively. Some reported preference for surgical treatment and believed their outcomes would have been better had their fracture been managed differently. Many reported not feeling fully included in treatment decision-making. Some described decreased function, independence and/or participation post-fracture.
Conclusion(s)
Our results indicate that persons with SCI/D report lacking substantive knowledge about bone health and/or fracture prevention, and following fracture, feel unable and/or hesitant to resume pre-fracture participation. In addition, our findings indicate that individuals with SCI/D may not feel as engaged as they would like to be in establishing fracture treatment plans. As such, persons with SCI/D may benefit from ongoing discussions with providers about risks and benefits of fracture treatment options and consideration of subsequent function and participation, to ensure patients preferences are considered.
Keywords: Bone health, Lower-extremity fractures, Osteoporosis, Spinal cord injury, Veterans
Introduction
Spinal cord injuries and disorders (SCI/D) are highly prevalent; up to 368,000 individuals in the U.S. are living with a SCI.1 The Veterans Health Administration’s (VA) SCI/D System of Care provides comprehensive, life-long care to over 27,000 Veterans with SCI/D across 25 hub (SCI Centers) and 130 spoke (SCI support clinics) facilities.2 Individuals with SCI/D are often affected by related secondary conditions, which may impact their physical and psychological health.3–5 One such condition is loss of bone mineral density (BMD) below the level of injury6; specifically, an estimated 80% of individuals with SCI/D have osteopenia or osteoporosis,7 putting them at increased risk for fractures and fracture-related consequences (e.g. non-unions/malunions, amputations, mortality).8–10 Of note, risk for osteoporotic fractures is greater among women, including those with SCI/D, as compared to men.11
Lower extremity (LE) fractures are among the most common fractures sustained by individuals with SCI/D.12–14 Importantly, individuals with SCI/D often have no (or significantly reduced) sensation below the level of injury, and as such, may be unable to recognize a LE fracture early on; health care providers may identify LE fractures by presence of erythema and/or edema.15 LE fractures are typically managed nonoperatively among persons with SCI/D,16 although increasingly, operative strategies are being considered.16–18 However, evidence to guide fracture treatment decision-making is scarce. Although it is important to promote bone health and manage fractures when they occur given their attendant morbidity19 and mortality,8 primary prevention of fractures is optimal. In recent years, review articles have summarized key evidence about how to promote bone health in persons with SCI.20 Very little exists, however, in the way of standardized guidelines to help clinicians manage osteoporosis and mitigate fracture risk in the SCI/D population.21 This is due in part to a lack of evidence concerning efficacy of fracture prevention strategies in this population.22
Moreover, patient perspectives on bone health management have not been examined. To optimize patient engagement in preventive and management practices, it is imperative to understand the experiences and opinions of individuals with SCI/D who have had a LE fracture. Our objective was to describe experiences with LE fracture prevention and management among Veterans with SCI/D.
Materials and methods
Design: Qualitative data collected via semi-structured telephone interviews.
Participants: Veterans with SCI/D (n = 32) who had experienced at least one LE fracture in the prior 18 months.
Recruitment: Interview recruitment took place between August 2018 and January 2019. A purposive sample23 of Veterans with SCI/D who utilized VA SCI/D care and who had experienced at least one LE fracture were invited to participate. The sample selection strategy included the patient’s completeness of injury (using ASIA score) and time since LE fracture, identified using VA administrative data (i.e. femur, tibia/fibula, or hip fractures were identified i.e. using ICD-10 codes: S72, S82.0-S82.9). Thirty-two patients were selected from four periods of time-since-fracture (in attempt to gather perspectives of individuals with both immediate and longer-term impact of fracture): 0–120, 121–240, 241–365, and 366–548 days. The sample was evenly split among those with an ASIA A vs. B, C, or D score.
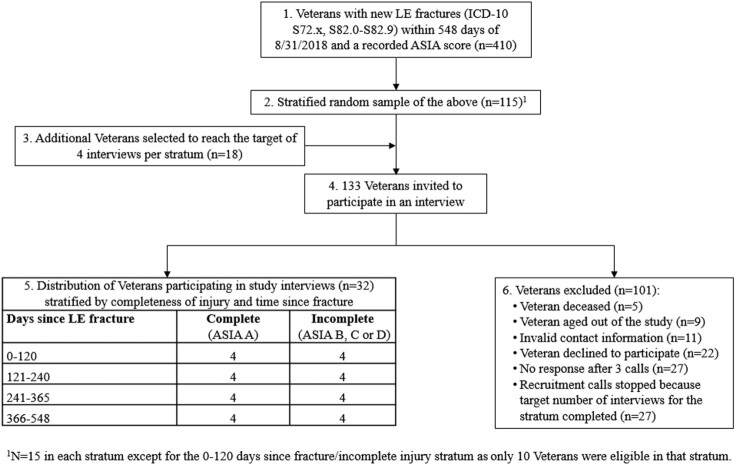
Eligible patients were mailed a letter by a member of our research team inviting them to participate in an interview and asking them to opt out within 2 weeks if they were not interested. A research team member attempted to contact individuals who did not opt out via telephone, up to three times, at least 1 business day apart, to schedule an interview; in total, 133 Veterans were invited to participate (please see Fig. 1). Interviewers obtained verbal consent using a standardized script summarizing that participation was voluntary, data would be confidential and presented only in aggregate form, and the conversation would be audio-recorded for analytic purposes.
Figure 1.
Cohort derivation diagram.
Data Collection/Materials: Interviews were semi-structured following an interview guide (please see Supplementary Appendix A), and were completed by members of the research team with expertise in qualitative methodology. The initial question set was created using expert clinician input, and pilot-tested in interviews with two SCI/D clinicians experienced in LE fracture management and three Veterans with SCI/D who had experienced a LE fracture. The interview guide was refined based on this feedback to optimize the flow of the conversation and the information the questions elicited. The final interview guide included questions designed to elicit information about patients’: pre-fracture knowledge of osteoporosis and bone health, diagnosis and management of osteoporosis, history and experiences with fracture treatment, and post-fracture care and experiences. Interviews were completed by phone to increase access and facilitate national sampling, lasted approximately 30 min, and were audio-recorded and transcribed verbatim for analysis. Upon completion of the interview, participants received a small honorarium in appreciation of their time.
Analyses: An inductive analytic approach was used, wherein codes were developed based on patterns emergent in the data.24 An initial codebook, with a draft list of codes and their operational definitions, was developed alongside the interview guide. The codebook was further refined by 3 research team members experienced in qualitative analysis after they independently coded the same 2 transcripts. Each subsequent transcript was analyzed by two of those same research team members using thematic coding and constant comparison,24,25 wherein each transcript was coded independently, and then two coders met to discuss their codes to establish inter-rater reliability. During these consensus meetings, coders discussed and resolved discrepancies until 100% proportion agreement26–28 was achieved. The codebook was modified during each of these consensus meetings, as needed, until saturation was reached. See Table 1 for a summary of themes, codes and operational definitions, as well as the number of participants who mentioned each and how many times they were mentioned.
Table 1.
Themes and encompassed within-theme sub-codes.
| Theme | Within-theme sub-code | Operational definition | Number of participants code was mentioned by | Number of times code was referenced |
|---|---|---|---|---|
| Knowledge of Osteoporosis | Patients discuss their awareness of osteoporosis and knowledge about bone health promotion | |||
| Knowledge of Bone Health | Description of the extent to which patients know about osteoporosis and how to promote bone health | 27 | 35 | |
| Bone Health Promotion: Physical Activity | To promote bone health, one should move around/exercise | 21 | 28 | |
| Concerned with Bone Health | Patient describes concern about their bone health | 20 | 21 | |
| Bone Health Promotion: Diet | To promote bone health, one should eat healthy/drink milk | 18 | 20 | |
| Bone Health Promotion: Supplements/Medications | To promote bone health, one should take supplements or medications | 15 | 17 | |
| Not Concerned with Bone Health | Patient describes not being concerned about their bone health | 10 | 14 | |
| Activity Limited due to Concerns | Patient describes limiting or restricting certain activities because of concerns about bone health (e.g. falls, fractures) | 6 | 7 | |
| Diagnosis and Management of Osteoporosis | Patients describe how their care providers have diagnosed and managed their osteoporosis | |||
| Supplements | Patient takes supplements that promote bone health (e.g. calcium, vitamin D) | 23 | 30 | |
| Previous Osteoporosis Diagnosis | Patient has been diagnosed with osteoporosis | 19 | 23 | |
| No Medications | Patient does not take medications for bone-health management | 18 | 23 | |
| No Education Provided By Doctor | Patient does not recall care team providing education about bone health management | 16 | 26 | |
| No Osteoporosis Diagnosis | Patient has not been diagnosed with osteoporosis | 15 | 16 | |
| No Previous Pre-Fracture DXA | Patient had not received a DXA prior to their fracture | 15 | 17 | |
| Non-Medication Management | Patient was instructed by their care provider to manage their bone health through non-pharmacological strategies (e.g. physical activity, diet) and/or uses integrative health modalities (i.e. acupuncture) | 13 | 13 | |
| Previous Pre-Fracture DXA | Patient had received a DXA prior to their fracture | 12 | 18 | |
| Barriers to Management: Physical Activity | Patient describes perceiving non-ambulatory or non-weight-bearing status as a barrier to self-management of bone health | 12 | 12 | |
| No Barriers to Management of Bone Health | Patient did not perceive barriers to self-management of bone health | 10 | 11 | |
| Current Medication Management | Patient is currently taking medication for osteoporosis | 6 | 14 | |
| Barriers to Management: Diet | Patient describes perceiving dietary factors as a barrier to self-management of bone health | 5 | 6 | |
| Barriers to Management: Medications | Patient describes perceiving factors related to medication as a barrier to self-management of bone health | 5 | 7 | |
| Previous Medication Management | Patient previously used osteoporosis medication | 5 | 7 | |
| Barriers to Management: Distance to VA or Availability of VA Treatment | Patient describes perceiving living far from the VA or not being able to get treatment at a VA as a barrier to fracture management | 4 | 4 | |
| Barriers to Management: Patient Attitude | Patient describes perceiving aspects of their attitude as a barrier to fracture management | 1 | 1 | |
| Barriers to Management: Sun Exposure | Patient describes perceiving contraindications to sun exposure as a barrier to fracture management | 1 | 1 | |
| Fracture History | Patients describe their lower-extremity fracture history, including location, cause, and treatment | |||
| Location | Where the fracture(s) occurred | 28 | 49 | |
| Realization | Patient describes of how they realized they had broken a bone (e.g. sound, swelling, discoloration, pain) | 27 | 31 | |
| Age At/Time of Fracture | When the fracture(s) occurred/patients’ age at time of fracture | 24 | 32 | |
| Timing of Realization | How long it took for the patient to realize they had broken a bone | 24 | 31 | |
| Symptoms | Symptoms the patient experienced after the fracture | 21 | 25 | |
| Multiple Fractures | Patient describes having multiple lower-extremity fractures | 21 | 43 | |
| Cause – Accident | How the fracture(s) occurred – via an accident | 16 | 20 | |
| Cause – Fall | How the fracture(s) occurred – via a fall | 15 | 19 | |
| Pre-SCI/D Fracture | Whether the patient had a fracture prior to the onset of their SCI/D | 11 | 11 | |
| Cause – Transfer | How the fracture(s) occurred – during a transfer | 7 | 9 | |
| Fracture Treatment | Patient describes how their lower-extremity fracture was managed | |||
| X-Rays/Scans | Patient received a radiograph and/or scan to determine whether or not they had a fracture | 32 | 40 | |
| Medical Management | Patients' fracture was managed medically (e.g. with a brace, cast, etc.) | 26 | 54 | |
| Place of Treatment | Where the patient received post-fracture treatment (e.g. VA SCI Center, VA Medical Center, community-based hospital) | 24 | 37 | |
| Treatment Decision-Making | Patient description of how their fracture treatment plan was decided upon | 21 | 34 | |
| Satisfaction with Treatment | The extent to which the patient was satisfied with their fracture treatment | 20 | 30 | |
| Time to Treatment | How much time passed between when the fracture occurred and when the patient received treatment | 15 | 19 | |
| Location | Location of the patient’s fracture(s) | 8 | 11 | |
| Surgical Management | Patients’ fracture was managed surgically | 6 | 9 | |
| Time to Diagnosis | Patient describes how long it took for their fracture to be diagnosed | 4 | 4 | |
| Equipment | Patient describes equipment they received as part of their fracture treatment | 4 | 4 | |
| Amputation | Patient had an amputation as a result of a fracture | 3 | 4 | |
| Post-Fracture Experience | Patients discuss their post-fracture experiences, including continued treatment and lasting physical/psychosocial impacts, as well as changes in their activities/behaviors after fracture to avoid subsequent fractures | |||
| Physical Therapy | Patient describes receiving (or not receiving) physical therapy following their fracture(s) | 31 | 37 | |
| Functional Impacts | Patient describes changes in function following fracture(s) (e.g. difficulty with transfers) | 30 | 39 | |
| Equipment | Patient received new equipment following a fracture(s) | 25 | 33 | |
| Rehabilitation | Patient describes receiving (or not receiving) inpatient rehabilitation following their fracture(s) | 24 | 25 | |
| Home Assistance | Patient describes receiving [extra] help at home following their fracture(s) | 23 | 25 | |
| Complications | Post-fracture complications (e.g. malunion, infection, pressure ulcer) | 19 | 29 | |
| Participation Impacts | Patient describes changes in participation following fracture(s) | 19 | 21 | |
| Most Helpful in Dealing with a Fracture | Patient describes things that were most helpful to them for dealing with their fracture(s) | 17 | 17 | |
| Physical Impacts | Patient describes changes in physical health following fracture(s) | 9 | 16 | |
| Post-Fracture DXA | Patient did receive a DXA following their fracture(s) | 9 | 11 | |
| No Post-Fracture DXA | Patient did not receive a DXA following their fracture(s) | 8 | 8 | |
| Psychosocial Impacts | Patient describes emotional impacts of fracture(s) | 6 | 8 | |
| Long-Term Care | Patient describes initiating long-term care following their fracture(s) | 1 | 1 |
Analyses were conducted using NVivo Version 12 (QSR International Pty Ltd.). This study was reviewed and approved by the Institutional Review Boards of the Augusta and Hines VA Hospitals.
Results
Sample description (Table 2): Respondents were predominantly male (91%), white (75%) and were about 64 years of age, on average; they represented both traumatic and non-traumatic etiologies. There were no statistically significant differences in fracture characteristics or ASIA score among Veterans invited to participate in an interview who were vs. were not ultimately interviewed.
Table 2.
Sample demographics and injury characteristics (n = 32)a.
| Demographics and injury characteristics | % Unless otherwise indicated |
|---|---|
| Age (n = 31) | |
| Mean | 63.8 |
| Range | 39.0–91.0 |
| Standard Deviation | 11.4 |
| Sex (n = 32) | |
| Male | 90.7 |
| Female | 9.3 |
| Race/Ethnicity (n = 32) | |
| White | 75.0 |
| African American | 12.5 |
| Latino/a | 3.1 |
| Missing | 9.3 |
| Duration of Injuryb (n = 29) | |
| Mean | 28.7 |
| Range | 2.0–73.0 |
| Standard Deviation | 17.7 |
| Travel Time to VA (Minutes) (n = 27) | |
| Mean | 61.3 |
| Range | 12.5–420.0 |
| Standard Deviation | 76.0 |
Row n’s <32 indicate missing values.
Determined by subtracting the number of years between age at time of interview and age at SCI, or, if only the year of SCI was available, subtracting the number of years between the year of interview and year of SCI.
Diagnosis and Management: Among participants who commented on their pre-fracture osteoporosis status, slightly more than half indicated that they had been diagnosed with osteoporosis prior to sustaining their fracture. Slightly less than half reported recalling having received a dual-energy x-ray absorptiometry (DXA) scan before sustaining their fracture. Participants described managing their bone health though a variety of strategies: taking supplements (e.g. calcium, vitamin D); maintaining a healthy diet, with some noting that weight management is also important; and engaging in physical activity (PA). While about half of respondents indicated they did not take prescription medications to manage bone health, just under one-fifth reported taking a medication for osteoporosis (i.e. alendronate, zoledronic acid, denosumab).
Barriers to management: While just under one-third of interviewees indicated no perceived barriers to bone health management, others provided examples of barriers they faced, including: distance from their residence to VA/availability of VA treatment, dietary restrictions (i.e. lactose intolerance), medication-related issues (e.g. remembering to take them, experiencing side effects). Further, Veterans noted PA limitations (i.e. being unable to engage in PA to promote bone strength, desire to engage in adventurous/dangerous activities) as a barrier, as illustrated by one interviewee:
… I had a couple of neighbors that would help me to get in and out of the swimming pool of my apartment and it was about two and a half miles around my neighborhood and I would push myself around that and just basically try to maintain my upper body strength and my posture with my standing frame, but I don’t really get any type of exercise like that now because there's not a lot of area for wheelchair access and there's no [public] transit system. [ASIA C]
Other barriers described among respondents included getting enough Vitamin D naturally (i.e. limited sun exposure), as noted by one interviewee:
[As] a quadriplegic, [I] can’t regulate [my] body temperatures anymore. So, getting out in the sun is kind of limited because when it is really hot … I can have a heat stroke and either die or have a bad stroke because of it. [ASIA A]
Knowledge of osteoporosis: Nearly all (n = 27) interviewees described the extent of their knowledge about osteoporosis and how to promote bone health. Many reported having little knowledge on these topics. Some participants did describe an understanding of osteoporosis and what causes it, including risk factors such as limited mobility status, older age and calcium deficiency, and an understanding that having osteoporosis puts one at greater risk for fracture. As one interviewee discussed:
The bones lose calcium over time. And … paralyzed guys … lose a lot more over time because we are not using our … body much, except to sit. [ASIA A]
Participants also described their knowledge of bone health promotion, including taking their medications and supplements, paying attention to their weight and maintaining a healthy diet that includes calcium and Vitamin D, and engaging in PA as best they can, as described by one interviewee:
… You have to make sure you get plenty of calcium and make sure you get as much exercise as you’re able to do, but I guess that’s about all I know. [ASIA D]
About half of respondents indicated that they did not recall their care team members providing them with education about how to promote bone health/prevent fractures. As one interviewee stated:
They didn’t really explain [any]thing to me. Just told me that I had osteoporosis. [ASIA D]
In addition, while just under one-third of respondents reported not being concerned with their bone health, just under two-thirds conveyed that they were moderately to highly concerned and for some of these Veterans, that concern caused them to be very careful with their activities, limited their participation/activity, or drove other medical decisions. As one Veteran detailed:
I would say that I am concerned … but … I’m doing something about it … I don’t take any chances at all anymore … I have a rule, like if I’m doing anything different at all, I sit there and think about how I’m going to move to do the chore or whatever it is, get out of the chair. [ASIA D]
Further, one interviewee described (along with their care provider) deciding to do an above-the-knee amputation to prevent re-fracturing their leg. Another interviewee reported getting a suprapubic catheter placed post-fracture to limit their number of daily transfers, as their previous fractures had occurred while transferring in the bathroom:
Considering in the last three years I’ve fractured my left leg and my right leg in two places, I would say I’m concerned enough that [after] the last fracture that I had, I went ahead and put in a suprapubic [catheter], even though I could void on my own, just so that I would cut down on my transferring. [ASIA C]
Fracture History: Interviewees described how they sustained their fracture, with several describing having previously sustained multiple fractures. Causes of fracture included falls, transfers, and accidents (e.g. stretching or bending over wrong, getting their foot or leg caught in a footplate/lift, crashing into objects with their wheelchair, motor vehicle accidents).
About three-fourths of interviewees discussed how long it took for them to realize they had broken a bone; some described knowing that they had sustained a fracture immediately, while others indicated not knowing until the next day, a few days later, or even longer. As illustrated by one interviewee:
… I came in the house that evening and [noticed that] I had a real small black and blue mark there. And I just figured I had bumped it … That was Wednesday evening. [On] Friday evening … the whole knee area was black and blue. And my wife … asked me, ‘Well, what do you think?’ And I said, ‘Well, I think it’s broke.’ And she said, ‘Well, we’re going to the VA’. [ASIA A]
Almost all participants also described how they knew they had broken a bone and symptoms they experienced after sustaining the fracture, which in some cases included pain, as one Veteran detailed:
I heard this big, huge pop in my knee and my hip and was immediately in pain throughout my abdomen. And just thought, ‘Okay, no big deal.’ It subsided. [I] woke up in the morning and my knee was … probably four times bigger than what it should have been. [ASIA C]
Additional signals and symptoms detailed by participants included seeing a bone ‘sticking out,’ swelling, fluid build-up, discoloration/bruising, inability to bear weight, hearing the bone break/pop, and the bone being loose or clicking when it was moved, as one Veteran illustrated: “ … when I started manipulating it, it was clicking” [ASIA B].
Fracture Treatment: Veterans discussed where they received fracture treatment including VA SCI Centers, VA Hospitals (non-SCI Centers), and private sector hospitals or primary care providers. Just under half of participants discussed the time interval between sustaining a fracture and when they received treatment, with some participants reporting having gone to the hospital for treatment within the hour of the fracture, while others described not seeking care for one to two days, or even longer.
All interviewees described having received x-rays or other scans to diagnose their fracture. Just over three-fourths of participants described receiving outpatient and/or inpatient (non-surgical) medical management (e.g. stabilizing the bone using a splint, cast or brace, using a bone stimulator, restricting activity, and pain management as appropriate):
It was late in the evening, so I had to go to the emergency room and the doctor, after they took x-rays, they put a cast on me and I was sent up to the medical surgical ward and, but [the] spinal cord [team] knew that I was there. So, the next day, they brought me back down to [the] spinal cord [unit]. And they had a prosthetic[s] person make me a whole new type of brace … So, they took the original cast off and they put the one that they built specifically so that I wouldn’t get any skin breakdown. [ASIA C]
A smaller number (just under one-fifth) of interviewees described having their fracture managed surgically:
They operated the next day with a titanium rod, and I was only in the hospital for about three days and I came back home. [ASIA C]
Some participants (n = 3) indicated their fracture resulted in them having an amputation. Reasons for amputation included prevention of re-fracture or other complications (e.g. nonunion, malunion), and treatment of nonunion (and subsequent pressure injury). As illustrated by one interviewee:
… he said he could pin it up [but it would] … most likely break again. So, that’s when we just decided to go ahead and cut it off above the knee. [ASIA A]
About two-thirds of interviewees described how their fracture treatment plan was decided upon. Among them, some participants described a collaborative decision-making process for managing their fracture:
At that point, we discussed … what the options were and told me they could [not] schedule me for surgery until, I think it was on a Wednesday and this was a Monday. That’s when they put that brace on me and then they sent me home … as bad as it was … I had to have the surgery. But the options were about what they were going to do to until then … . [ASIA A]
Others, however, did not report feeling included in the decision-making process for how to manage their fracture and some reported preference for surgical treatment and believed their outcomes may have been better had their fracture been managed differently:
I’m a young guy with [a] family … I drive, I have kids, I bend over, I’m up, I’m down, I’m in bed … For someone as busy and active as I was, I honestly think the leg stabilization [surgery] would’ve been the ideal route … if it would have been stabilized, I honestly think I would’ve had more confidence in getting things done. [ASIA B]
Just under two-thirds of interviewees discussed the extent to which they were satisfied with their fracture treatment, and among them, many expressed satisfaction with the care that they received:
The VA has been really good to me. I am blessed … they’ve done everything in the world. They bend over backwards to help me. [ASIA A]
Post-fracture experiences: Almost all interviewees (n = 31) indicated whether or not they had received physical therapy and/or rehabilitation (n = 24) following their fracture. Just over three-fourths described receiving new equipment (e.g. lifts, shower chairs, different wheelchairs) or equipment modifications (e.g. additional safety belts added to their wheelchair). Just over a quarter of interviewees mentioned receiving a DXA after sustaining their fracture. Post-fracture complications described by participants included fracture nonunion, pressure injury, autonomic dysreflexia, and/or amputation.
Veterans also described the impact of the fracture on their lives. While some did not experience any long-lasting impacts following their fracture, others discussed challenging impacts in areas such as function, participation, and physical and/or psychological well-being. As one interviewee described:
When I [first] fell and I hurt myself … I still … did a lot of things. I swam. I went to wheelchair games. I skied … This last fracture … has slowed me down … I don’t feel as confident doing things that I used to do … So, it’s put a kink in my lifestyle. [ASIA C]
And another interviewee detailed:
I also had to take this semester off of school to make sure that I was attending all these doctor appointments … but now I’m scared to death to go to school on my own … sometimes I feel like a shut-in … I think that … the people around you that you love want me to be happy and okay when I’m not happy and okay. [ASIA C]
Discussion
This study is among the first to describe perspectives of patients with SCI/D on fracture prevention and management. Our data revealed a range of knowledge about osteoporosis, awareness of when a fracture occurred, and the long-term implications of sustaining a fracture. Participants voiced the desire to feel more included in collaborative decision-making with their physicians for fracture treatment, which several respondents felt was lacking. These data suggest that individuals with SCI/D may benefit from education about bone health and fracture prevention, and how to safely resume pre-fracture participation following LE fracture. Guidelines for inpatient, outpatient and community-based settings on fracture prevention and management are currently under development and may facilitate future creation of such evidence-informed education.
Although few participants reported receiving a pharmacological intervention for prevention or management of osteoporosis, most were aware of the need for adequate calcium and vitamin D intake. These findings are in accordance with previous studies of Veterans with SCI, where pharmacological treatment for osteoporosis was found to be rare,13,29,30 although calcium and vitamin D supplementation is common. Further, many participants recognized the importance of PA to promote bone health, however, others described lacking viable ways to get that activity; providing persons with SCI/D with safe options to facilitate PA (that may also positively impact BMD) could be beneficial.
Causes of fractures ranged from seemingly little to no trauma (e.g. transfers, fragility fractures) to high-impact traumatic fractures (e.g. motor vehicle accidents). In accordance with previous reports, some of our participants reported knowing immediately they had sustained a fracture, whereas others were unaware of the fracture until symptoms/signs such as swelling or bruising were obvious.31
Fracture-related complications in SCI/D are more frequent and significant than the general population,13,28 including nonunion/malunion, pressure injury, and autonomic dysreflexia.10,32–34 Consistent with previous literature, a number of participants in our study reported fracture-related complications. Fracture-related complications like nonunion or malunion can have substantial implications including chronic pain and loss of mobility, functional independence and participation.35–37 Accordingly, many participants in our study conveyed the negative impact of fracture-related complications on their function, participation and quality of life (QOL).
In regard to fracture treatment, some participants reported operative management of fractures, while others had their fracture managed non-operatively. This is consistent with recent literature, which indicates that operative fracture treatment is increasingly used among persons with SCI/D34 and may result in preferable outcomes (e.g. pressure injuries may be more common in patients with SCI/D who sustained a femur fracture following non-operative vs. operative management).38 Moreover, surgical fracture management among individuals who use wheelchairs for mobility (including those with SCI/D) may result in a return to pre-fracture function, maintenance of independence, and improved QOL.39,40
Some participants indicated a preference for operative treatment, but did not feel fully included in the decision-making process for how their fracture was managed. Further study is needed to determine optimal fracture management for persons with SCI/D to minimize complications, maintain QOL, and address patient preferences. Engaging patients in the treatment planning process and factoring in their goals and preferences when making treatment decisions is a cornerstone of patient-centered care,41 even when treatment options are limited. Our data cannot address this issue directly, however, we suspect that a collaborative, multidisciplinary, patient-centered approach to fracture management for persons with SCI/D may increase patient confidence in treatment decisions, and possibly optimize post-fracture functioning and QOL. As such, patient-centered approaches to support greater involvement of patients in the treatment decision-making and programs to address important issues related to patient function, participation and QOL should be incorporated into post-fracture management for persons with SCI/D.
Importantly and to that end, several interviewees discussed having experienced loss of confidence following their fracture, and being hesitant to engage in activities that they previously enjoyed. Retraining persons with SCI/D in safe transfers and mobility strategies, and offering approaches for boosting confidence to safely engage in pre-fracture activities, could be incorporated into post-fracture management and may boost participation and function.
Overall, patients could benefit from additional education about bone health promotion and fracture prevention, which could be provided by care team members through discussions during routine appointments (e.g. primary care visits; comprehensive annual physical exams, referred to in the VA SCI/D System of Care as annual evaluations), or using written educational materials (e.g. pamphlets, websites). Fracture prevention and management guidelines (both clinical and consumer guides) could be valuable tools to guide the content of such education.
Limitations: Perspectives from individuals with SCI/D in the general population and women with SCI/D who have experienced a fracture should be incorporated into future work. While the qualitative data used in this study offers rich detail, future studies may employ a mixed-methods approach (including quantitative data collection strategies such as surveys or medical record reviews) to obtain objective as well as subjective information. Additionally, we did not take purposive measures to establish reflexivity, however, each member of our research team has considerable expertise and experience working with Veterans with SCI/D and conducting qualitative research; in addition, literature indicates that assessing reflexivity is an uncommon practice in medical and public health research.42
Conclusions: Our results suggest that persons with SCI/D may lack substantive knowledge about bone health and fracture prevention, and following fracture, feel unable and/or hesitant to resume pre-fracture participation. In addition, our findings indicate that individuals with SCI/D may not feel as engaged as they would like to be in establishing fracture treatment plans. As such, persons with SCI/D may benefit from ongoing discussions with providers about risks and benefits of fracture treatment options and considerations of subsequent function and participation, to ensure patients preferences are considered.
Supplementary Material
Acknowledgements
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the United States government.
Funding Statement
This study was supported by the U.S. Department of Defense: [grant number SCI50092] and US Department of Veterans Affairs, Office of Research and Development, Health Services Research and Development Service: [grant number IIR 15-294].
Disclaimer statements
Conflicts of interest The authors do not have any financial conflicts of interest. Dr. Weaver is an associate editor for the Journal of Spinal Cord Medicine.
References
- 1.National Spinal Cord Injury Statistical Center . Spinal cord injury facts and figures at a glance [document on the Internet]. 2020 [cited 2020 February 24]. Available from: https://www.nscisc.uab.edu/Public/FactsandFigures2020.pdf.
- 2.US Department of Veterans Affairs, Office of Research and Development . VA research on spinal cord injury [document on the Internet]. 2019 [cited 2020 February 24]. Available from: https://www.research.va.gov/topics/sci.cfm.
- 3.Stillman MD, Barber J, Burns S, Williams S, Hoffman JM.. Complications of spinal cord injury over the first year after discharge from inpatient rehabilitation. Arch Phys Med Rehabil 2017;98(9):1800–5. [DOI] [PubMed] [Google Scholar]
- 4.Wahman K, Nilsson Wikmar L, Chlaidze G, Joseph C.. Secondary medical complications after traumatic spinal cord injury in Stockholm, Sweden: towards developing prevention strategies. J Rehabil Med 2019;51(7):513–17. [DOI] [PubMed] [Google Scholar]
- 5.Lim SW, Shiue YL, Ho CH, Yu SC, Kao PH, Wang JJ, et al. . Anxiety and depression in patients with traumatic spinal cord injury: a nationwide population-based cohort study. PLoS One 2017;12(1):e0169623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bauman WA, Cardozo CP.. Osteoporosis in individuals with spinal cord injury. PM R 2015;7(2):188–201. [DOI] [PubMed] [Google Scholar]
- 7.Svircev J. Osteoporosis and Fractures in Persons with SCI: What, Why and How to Manage [document on the Internet]. 2012 [cited 2020 February 24]. Available from: http://sciwashington.edu/info/forums/reports/osteoporosis.asp.
- 8.Carbone LD, Chin AS, Burns SP, Svircev JN, Hoenig H, Heggeness M, et al. . Mortality after lower extremity fractures in men with spinal cord injury. J Bone Miner Res 2014;29(2):432–9. [DOI] [PubMed] [Google Scholar]
- 9.Bethel M, Bailey L, Weaver F, Harmon RL, Priebe MM, Le B, et al. . A historical study of appendicular fractures in veterans with traumatic chronic spinal cord injury: 2002-2007. J Spinal Cord Med 2016;39(6):686–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grassner L, Klein B, Maier D, Buhren V, Vogel M.. Lower extremity fractures in patients with spinal cord injury characteristics, outcome and risk factors for non-unions. J Spinal Cord Med 2018;41(6):676–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bethel M, Weaver FM, Bailey L, Miskevics S, Svircev JN, Burns SP, et al. . Risk factors for osteoporotic fractures in persons with spinal cord injuries and disorders. Osteoporos Int 2016;27(10):3011–21. [DOI] [PubMed] [Google Scholar]
- 12.Frotzler A, Cheikh-Sarraf B, Pourtehrani M, Krebs J, Lippuner K.. Long-bone fractures in persons with spinal cord injury. Spinal Cord 2015;53(9):701–4. [DOI] [PubMed] [Google Scholar]
- 13.Gifre L, Vidal J, Carrasco J, Portell E, Puig J, Monegal A, et al. . Incidence of skeletal fractures after traumatic spinal cord injury: a 10-year follow-up study. Clin Rehabil 2014;28(4):361–9. [DOI] [PubMed] [Google Scholar]
- 14.Anderson SD, Anderson DG, Vaccaro AR.. Skeletal fracture demographics in spinal cord-injured patients. Arch Orthop Trauma Surg 2004;124(3):193–6. [DOI] [PubMed] [Google Scholar]
- 15.Mortimer DS, Chung K. Osteoporosis and fractures after CNS injury [document on the Internet]. 2016 [cited 2021 March 10]. Available from: https://now.aapmr.org/osteoporosis-and-fractures-after-cns-injury/.
- 16.Bishop JA, Suarez P, Diponio L, Ota D, Curtin CM.. Surgical versus nonsurgical treatment of femur fractures in people with spinal cord injury: an administrative analysis of risks. Arch Phys Med Rehabil 2013;94(12):2357–64. [DOI] [PubMed] [Google Scholar]
- 17.Fouasson-Chailloux A, Gross R, Dauty M, Gadbled G, Touchais S, Le Fort M, et al. . Surgical management of lower limb fractures in patients with spinal cord injury less associated with complications than non-operative management: a retrospective series of cases. J Spinal Cord Med 2019;42(1):39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barrera-Ochoa S, Haddad S, Rodríguez-Alabau S, Teixidor J, Tomás J, Molero V.. Should lower limb fractures be treated surgically in patients with chronic spinal injuries? Experience in a reference centre. Rev Esp Cir Ortop Traumatol 2017;61(1):19–27. [DOI] [PubMed] [Google Scholar]
- 19.Carbone LD, Chin AS, Burns SP, Svircev JN, Hoenig H, Heggeness M, et al. . Morbidity following lower extremity fractures in men with spinal cord injury. Osteoporos Int 2013;24(8):2261–7. [DOI] [PubMed] [Google Scholar]
- 20.Ashe MC, Craven C, Eng JJ.. Krassioukov A; the SCIRE research team. prevention and treatment of bone loss after a spinal cord injury: a systematic review. Top Spinal Cord Inj Rehabil 2007;13(1):123–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ragnarsson KT. Bone loss and fractures in limbs paralyzed by spinal cord injury: prevention, diagnosis, and treatment. J Spinal Cord Med 2015;38(1):10–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zleik N, Weaver F, Harmon RL, Le B, Radhakrishnan R, Jirau-Rosaly WD, et al. . Prevention and management of osteoporosis and osteoporotic fractures in persons with a spinal cord injury or disorder: a systematic scoping review. J Spinal Cord Med 2019;42(6):735–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fossey E, Harvey C, McDermott F, Davidson L.. Understanding and evaluating qualitative research. Aust NZJ Psychiatry 2002;36(6):717–32. [DOI] [PubMed] [Google Scholar]
- 24.Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks (CA: ): Sage; 1998. [Google Scholar]
- 25.Strauss A, Corbin J.. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks (CA: ): Sage; 1998. [Google Scholar]
- 26.Gisev N, Bell JS, Chen TF.. Interrater agreement and interrater reliability: key concepts, approaches, and applications. Res Social Adm Pharm 2013;9(3):330–8. [DOI] [PubMed] [Google Scholar]
- 27.Holdford D. Content analysis methods for conducting research in social and administrative pharmacy. Res Social Adm Pharm 2008;4(2):173–81. [DOI] [PubMed] [Google Scholar]
- 28.Guba EG, Lincoln YS.. Fourth generation evaluation. Newbury Park (CA: ): Sage; 1989. [Google Scholar]
- 29.Weaver FM, Le B, Ray C, Miskevics S, Gonzalez B, Carbone LD.. Predicting osteoporosis medication receipt in Veterans with a spinal cord injury: a retrospective cohort study. J Spinal Cord Med 2019;42(6):760–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weaver FM, Etingen B, Guihan M, Ray C, Priebe M, Burns S, et al. . Spinal cord injury providers’ perspectives on managing sublesional osteoporosis. J Spinal Cord Med. 2020;43(4):428–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Akhigbe T, Chin AS, Svircev JN, Hoenig H, Burns SP, Weaver FM, et al. . A retrospective review of lower extremity fracture care in patients with spinal cord injury. J Spinal Cord Med 2015;38(1):2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morse LR, Battaglino RA, Stolzmann KL, Hallett LD, Waddimba A, Gagnon D, et al. . Osteoporotic fractures and hospitalization risk in chronic spinal cord injury. Osteoporos Int 2009;20(3):385–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ragnarsson KT, Sell GH.. Lower extremity fractures after spinal cord injury: a retrospective study. Arch Phys Med Rehabil 1981;62(9):418–23. [PubMed] [Google Scholar]
- 34.Bethel M, Bailey L, Weaver F, Le B, Burns SP, Svircev JN, et al. . Surgical compared with nonsurgical management of fractures in male veterans with chronic spinal cord injury. Spinal Cord 2015;53(5):402–7. [DOI] [PubMed] [Google Scholar]
- 35.Hak DJ, Fitzpatrick D, Bishop JA, Marsh JL, Tilp S, Schnettler R, et al. . Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury 2014;45(Suppl. 2):S3–7. [DOI] [PubMed] [Google Scholar]
- 36.Kanakaris NK, Angoules AG, Nikolaou VS, Kontakis G, Giannoudis PV.. Treatment and outcomes of pelvic malunions and nonunions: a systematic review. Clin Orthop Relat Res 2009;467(8):2112–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cochran T, Bayley J, Smith M.. Lower extremity fractures in paraplegics: pattern, treatment, and functional results. J Spinal Disord 1988;1(3):219–23. [PubMed] [Google Scholar]
- 38.Bishop JA, Suarez P, Diponio L, Ota D, Curtin CM.. Surgical versus nonsurgical treatment of femur fractures in people with spinal cord injury: an administrative analysis of risks. Arch Phys Med Rehabil 2013;94(12):2357–64. [DOI] [PubMed] [Google Scholar]
- 39.Sugi MT, Davidovitch R, Montero N, Nobel T, Egol KA.. Treatment of lower-extremity long-bone fractures in active, nonambulatory, wheelchair-bound patients. Orthopedics 2012;35(9):e1376–82. [DOI] [PubMed] [Google Scholar]
- 40.Bärlehner C, Böhm V, Flieger R, Meiners T.. [Surgery for fractures of the lower extremities in cases of chronic spinal cord injury]. Orthopade 2005;34(2):137–8. 140–3. [DOI] [PubMed] [Google Scholar]
- 41.Barry MJ, Edgman-Levitan S.. Shared decision making–pinnacle of patient-centered care. N Engl J Med 2012;366(9):780–1. [DOI] [PubMed] [Google Scholar]
- 42.Dodgson JE. Reflexivity in qualitative research. J Hum Lact 2019;35(2):220–2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.