Abstract
Background
Multiple myeloma (MM) accounts for 1% to 2% of all cancers. Exposure to the pesticide Agent Orange (AO) has been established as a potential risk factor for the development of monoclonal gammopathy of undetermined significance (MGUS) and, subsequently, MM in Vietnam War veterans.
Methods
This study explored variation in survival related to AO exposure, transformation from MGUS to MM, and covariates. Vietnam War veterans with MM or MGUS were identified in Veterans Health Administration (VHA) health records data. Cox proportional hazards models analyzed survival as a function of AO, race, ethnicity, body mass index, nicotine dependence, alcohol use disorder, Charlson Comorbidity Index, and treatment. Autologous hematopoietic cell transplantation for MM was defined by procedure codes.
Results
In the VHA 16,366 patients were identified: 11,112 patients diagnosed with MGUS and 7261 with MM during fiscal years 2010 to 2015 were identified; 12% (n = 2007) had both diagnoses. No statistically significant difference in the rate of transformation from MGUS to MM in the AO exposed and AO not exposed groups was found. In survival models, AO exposure was associated with slightly lower mortality. Alcohol use disorder, nicotine dependence, older age, and greater comorbidity burden increased mortality risk. Black race, female sex, obesity/overweight, and hematopoietic cell transplantation for patients with MM were protective factors. AO exposure was associated with decreased mortality for both MM/MGUS groups. Transformation increased mortality risk for patients with MGUS and decreased mortality risk for patients with MM.
Conclusions
Because AO exposure is a nonmodifiable risk factor, focus should be placed on modifiable risk factors (eg, nicotine dependence, alcohol and drug use disorders, underlying comorbid conditions) as these were associated with worse outcomes. Future studies should examine the correlation of AO exposure, cytogenetics, and clinical outcomes in these veterans to best identify their disease course and optimize their care in the latter part of their life.
Multiple myeloma (MM) accounts for 1% to 2% of all cancers and slightly more than 17% of hematologic malignancies in the United States.1 MM is characterized by the neoplastic proliferation of immunoglobulin (Ig)-producing plasma cells with ≥ 10% clonal plasma cells in the bone marrow or biopsy-proven bony or soft tissue plasmacytoma, plus presence of related organ or tissue impairment or presence of a biomarker associated with near-inevitable progression to end-organ damage.2
BACKGROUND
Up to 97% of patients with MM will have a monoclonal (M) protein produced and secreted by the malignant plasma cells, which can be detected by protein electrophoresis of the serum and an aliquot of urine from a 24-hour collection combined with immunofixation of the serum and urine. The M protein in MM usually consists of IgG 50% of the time and light chains 16% of the time. Patients who lack detectable M protein are considered to have nonsecretory myeloma. MM presents with end-organ damage, which includes hypercalcemia, renal dysfunction, anemia, or lytic bone lesions. Patients with MM frequently present with renal insufficiency due to cast nephropathy or light chain deposition disease.3
MM is thought to evolve from monoclonal gammopathy of uncertain significance (MGUS), an asymptomatic premalignant stage of clonal plasma cell proliferation with a risk of progression to active myeloma at 1% per year.4,5 Epidemiologic data suggest that people who develop MM have a genetic predisposition, but risk factors may develop or be acquired, such as age, immunosuppression, and environmental exposures. To better assess what causes transformation from MGUS to MM, it is important to identify agents that may cause this second hit.6
In November 1961, President John F. Kennedy authorized the start of Operation Ranch Hand, the US Air Force’s herbicide program during the Vietnam War. Twenty million gallons of various chemicals were sprayed in Vietnam, eastern Laos, and parts of Cambodia to defoliate rural land, depriving guerillas of their support base. Agent Orange (AO) was one of these chemicals; it is a mixed herbicide with traces of dioxin, a compound that has been associated with major health problems among exposed individuals.7 Several studies have evaluated exposure to AO and its potential harmful repercussions. Studies have assessed the link between AO and MGUS as well as AO to various leukemias, such as chronic lymphocytic leukemia.8,9 Other studies have shown the relationship between AO exposure and worse outcomes in persons with MM.10 To date, only a single abstract from a US Department of Veterans Affairs (VA) medical center has investigated the relationships between AO exposure and MGUS, MM, and the rate of transformation. The VA study of patients seen from 2005 to 2015 in Detroit, Michigan, found that AO exposure led to an increase in cumulative incidence rate of MGUS/MM, suggesting possible changes in disease biology and genetics.11
In this study, we aimed to determine the incidence of transformation of MGUS to MM in patients with and without exposure to AO. We then analyzed survival as a function of AO exposure, transformation, and clinical and sociodemographic variables. We also explored the impact of psychosocial variables and hematopoietic stem cell transplantation (HSCT), a standard of treatment for MM.
METHODS
This retrospective cohort study assembled electronic health record (EHR) data from the Veterans Health Administration Corporate Data Warehouse (CDW). The VA Central Texas Veterans Healthcare System Institutional Review Board granted a waiver of consent for this record review. Eligible patients were Vietnam-era veterans who were in the military during the time that AO was used (1961–1971). Veterans were included if they were being cared for and received a diagnosis for MGUS or MM between October 1, 2009, and September 30, 2015 (all prevalent cases fiscal years 2010–2015). Cases were excluded if there was illogical death data or if age, race, ethnicity, body mass index (BMI), or prior-year diagnostic data were missing.
Measures
Patients were followed through April 2020. Presence of MGUS was defined by the International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code 273.1. MM was identified by ICD-9 diagnosis codes 203.00, 203.01, and 203.02. The study index date was the earliest date of diagnosis of MGUS or MM in fiscal years 2010–2015. It was suspected that some patients with MM may have had a history of MGUS prior to this period. Therefore, for patients with MM, historical diagnosis of MGUS was extracted going back through the earliest data in the CDW (October 1999). Patients diagnosed with both MGUS and MM were considered transformation patients.
Other measures included age at index date, sex, race, ethnicity, VA priority status (a value 1 to 8 summarizing why the veteran qualified for VA care, such as military service-connected disability or very low income), and AO exposure authenticated per VA enrollment files and disability records. Service years were separated into 1961 to 1968 and 1969 to 1971 to match a change in the formulation of AO associated with decreased carcinogenic effect. Comorbidity data from the year prior to first MGUS/MM diagnosis in the observation period were extracted. Lifestyle factors associated with development of MGUS/MM were determined using the following codes: obesity per BMI calculation or diagnosis (ICD-9, 278.0), tobacco use per diagnosis (ICD-9, 305.1, V15.82), and survival from MGUS/ MM diagnosis index date to date of death from any cause. Comorbidity was assessed using ICD-9 diagnosis codes to calculate the Charlson
Comorbidity Index (CCI), which includes cardiovascular diseases, diabetes mellitus, liver and kidney diseases, cancers, and metastatic solid tumors. Cancers were omitted from our adapted CCI to avoid collinearity in the multivariable models. The theoretical maximum CCI score in this study was 25.12,13 Additional conditions known to be associated with variation in outcomes among veterans using the VA were indicated, including major depressive disorder, posttraumatic stress disorder (PTSD), alcohol use disorder (AUD), substance use disorder (SUD), and common chronic disease (hypertension, lipid disorders).14
Treatment with autologous HSCT was defined by Current Procedural Terminology and ICD-9 Clinical Modification procedure codes for bone marrow and autologous HSCT occurring at any time in the CDW (eAppendix available online at doi:10.12788/fp.0303). Days elapsed from MM diagnosis to HSCT were calculated.
Statistical Analysis
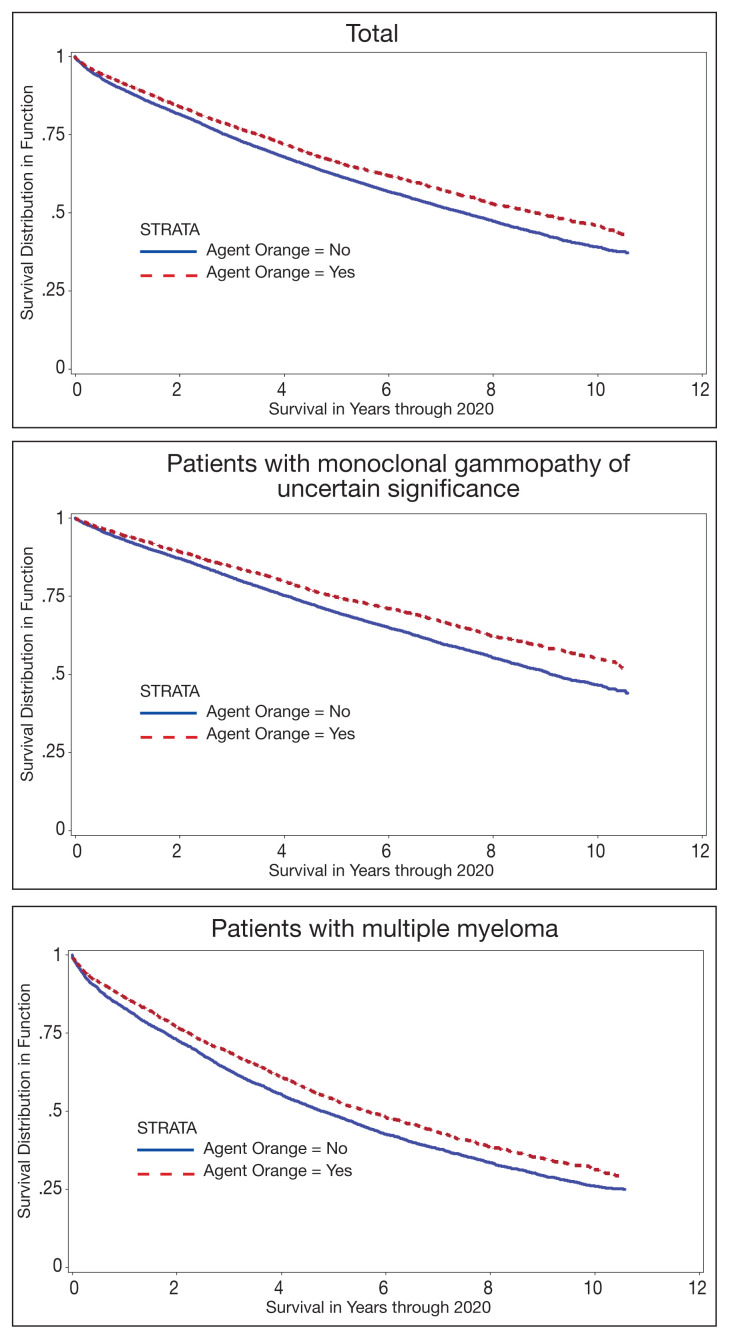
Sample characteristics were represented by frequencies and percentages for categorical variables and means and SDs (or medians and ranges where appropriate) for continuous variables. A χ2 test (or Fisher exact test when cell counts were low) assessed associations in bivariate comparisons. A 2-sample t test (or Wilcoxon rank sum test as appropriate) assessed differences in continuous variables between 2 groups. Kaplan-Meier curves depicted the unadjusted relationship of AO exposure to survival. Cox proportional hazards survival models examined an unadjusted model containing only the AO exposure indicator as a predictor and adjusted models were used for demographic and clinical factors for MGUS and patients with MM separately.
Predictors were age in decades, sex, Hispanic ethnicity, race, nicotine dependence, obesity, overweight, AUD, SUD, major depressive disorder, PTSD, and the adapted CCI. When modeling patients with MM, MGUS was added to the model to identify the transformation group. The interaction of AO with transformation was also analyzed for patients with MM. Results were reported as hazard ratios (HR) with their 95% CI.
RESULTS
We identified 18,215 veterans diagnosed with either MGUS or MM during fiscal years 2010–2015 with 16,366 meeting inclusion criteria. Patients were excluded for missing data on exposure (n = 334), age (n = 12), race (n = 1058), ethnicity (n = 164), diagnosis (n = 47), treatment (n = 56), and BMI (n = 178). All were Vietnam War era veterans; 14 also served in other eras.
The cohort was 98.5% male (Table 1). Twenty-nine percent were Black veterans, 65% were White veterans, and 4% of individuals reported Hispanic ethnicity. Patients had a mean (SD) age of 66.7 (5.9) years (range, 52–96). Most patients were married (58%) or divorced/separated (27%). All were VA priority 1 to 5 (no 6, 7, or 8); 50% were priority 1 with 50% to 100% service-connected disability. Another 29% were eligible for VA care by reason of low income, 17% had 10% to 40% service-connected disability, and 4% were otherwise disabled.
TABLE 1.
Characteristics of Vietnam Veterans With MGUS or MM
| Characteristics | Agent Orange exposed | Not exposed | Total |
|---|---|---|---|
| Age, mean (SD), y | 66.6 (5.0) | 66.8 (6.3) | 66.7 (5.9) [range, 0–14] |
|
| |||
| Charlson Comorbidity Index, omitting cancers, mean (SD) | 1.9 (2.1) | 1.9 (2.1) | 1.9 (2.1) |
|
| |||
| Survival, mean (SD), y | 5.8 (3.1) | 5.5 (3.1) | 5.6 (3.1) [range, 0–10.6] |
|
| |||
| Survived past end of observation (April 1 2020), No. (%) | 8144 (49.7) | ||
|
| |||
| Agent Orange exposure, No. (%) | 5683 (100) | 0 (0) | 5683 (34.7) |
|
| |||
| Female sex, No. (%) | 9 (0.2) | 229 (2.1) | 238 (1.5) |
|
| |||
| Hispanic ethnicity, No. (%) | 260 (4.6) | 430 (4.0) | 690 (4.2) |
|
| |||
| Race, No. (%) | |||
| American Indian/Alaska Native, Hawaiian/Pacific Islander | 349 (6.1) | 653 (6.1) | 1002 (6.1) |
| Black | 1528 (26.9) | 3198 (29.9) | 4726 (28.9) |
| White | 3806 (67.0) | 6832 (64.0) | 10,638 (65.0) |
|
| |||
| Marital status, No. (%) | |||
| Married | 3856 (67.9) | 5667 (53.1) | 9523 (58.2) |
| Divorced/separated | 1281 (22.5) | 3223 (30.2) | 4504 (27.5) |
| Single | 300 (5.3) | 1117 (10.5) | 1417 (8.7) |
| Widow(ed) | 281 (4.9) | 749 (7.0) | 1030 (6.3) |
|
| |||
| VA priority group, No. (%) | |||
| 1: 50%–100% disabled service-connected | 4506 (79.3) | 3734 (35.0) | 8240 (50.4) |
| 2: 30%–40% disabled service-connected | 30 (0.5) | 330 (3.1) | 360 (2.2) |
| 3: 10%–20% disabled service-connected | 572 (10.1) | 1802 (16.9) | 2374 (14.5) |
| 4: catastrophically disabled/homebound | 46 (0.8) | 581 (5.4) | 627 (3.8) |
| 5: very low income | 529 (9.3) | 4236 (39.7) | 4765 (29.1) |
|
| |||
| Comorbidity, No. (%) | |||
| Hypertension | 3957 (69.6) | 7689 (72.0) | 11,646 (71.2) |
| Diabetes mellitus | 2217 (39.0) | 3964 (37.1) | 6181 (37.8) |
| Dyslipidemia | 3301 (58.1) | 6060 (56.7) | 9361 (57.2) |
| Nicotine dependent | 1195 (21.0) | 2390 (22.4) | 3585 (21.9) |
| Major depressive disorder | 861 (15.2) | 1355 (12.7) | 2216 (13.5) |
| Posttraumatic stress disorder | 1301 (22.9) | 767 (7.2) | 2068 (12.6) |
| Alcohol use disorder | 499 (8.8) | 968 (9.1) | 1467 (9.0) |
| Drug use disorder | 249 (4.4) | 604 (5.7) | 853 (5.2) |
| Overweight (body mass index 25–29) | 2019 (35.5) | 3690 (34.6) | 5709 (34.9) |
| Obese (body mass index ≥ 30) | 2505 (44.1) | 4271 (40.0) | 6776 (41.4) |
|
| |||
| MGUS, with or without MM, No. (%) | 3797 (66.8) | 7315 (68.5) | 11,112 (67.9) |
|
| |||
| MM, with or without MGUS, No. (%) | 2581 (45.4) | 1312 (12.3) | 2007 (12.3) |
|
| |||
| Transformation from MGUS to MM, No. (%) | 695 (12.2) | 4680 (43.8) | 7261 (44.4) |
|
| |||
| Hematopoietic stem cell transplantation of 7261 patients with MM, No. (%) | 242 (9.4) | 385 (8.2) | 627 (8.6) |
Abbreviations: MGUS, monoclonal gammopathy of uncertain significance; MM, multiple myeloma; VA, US Department of Veterans Affairs.
During fiscal years 2010 to 2015, 68% of our cohort had a diagnosis of MGUS (n = 11,112; 9105 had MGUS only), 44% had MM (n = 7261; 5254 had MM only), and 12% of these were transformation patients (n = 2007). AO exposure characterized 3102 MGUS-only patients (34%), 1886 MM-only patients (36%), and 695 transformation patients (35%) (χ2 = 4.92, P = .09). Among 5683 AO-exposed patients, 695 (12.2%) underwent MGUS-to-MM transformation. Among 10,683 nonexposed veterans, 1312 (12.3%) experienced transformation.
Comorbidity in the year leading up to the index MGUS/MM date determined using CCI was a mean (SD) of 1.9 (2.1) (range, 0–14). Among disorders not included in the CCI, 71% were diagnosed with hypertension, 57% with lipid disorders, 22% with nicotine dependence, 14% with major depressive disorder, 13% with PTSD, and 9% with AUD. Overweight (BMI 25 to < 30) and obesity (BMI ≥ 30) were common (35% and 41%, respectively). For 98% of patients, weight was measured within 90 days of their index MGUS/MM date. Most of the cohort (70%) were in Vietnam in 1961 to 1968.
HSCT was provided to 632 patients with MM (8.7%), including 441 patients who were treated after their index date and 219 patients treated before their index date. From fiscal years 2010 to 2015, the median (IQR) number of days from MM index date to HSCT receipt was 349 (243–650) days. Historical HSCT occurred a median (IQR) of 857 (353–1592) days before the index date, per data available back to October 1999; this median suggests long histories of MM in this cohort.
The unadjusted survival model found a very small inverse association of mortality with AO exposure in the total sample, meaning patients with documented AO exposure lived longer (HR, 0.85; 95% CI, 0.81–0.89; Table 2; Figure). Among 11,112 MGUS patients, AO was similarly associated with mortality (HR, 0.79; 95% CI, 0.74–0.84). The effect was also seen among 7269 patients with MM (HR, 0.86; 95% CI, 0.81–0.91).
TABLE 2.
Survival Among Vietnam Veterans With MM or MGUS
| Predictor | No. or Mean (SD) | Hazard ratio (95% CI) | P value |
|---|---|---|---|
| Unadjusted models | |||
| Agent Orange exposurea | |||
| MM + MGUS (n = 16,366) | 5683 | 0.85 (0.81–0.89) | < .001 |
| MGUS only (n = 11,112) | 3797 | 0.79 (0.74–0.84) | < .001 |
| MM only (n = 7261) | 2581 | 0.86 (0.81–0.91) | < .001 |
|
| |||
| Adjusted models | |||
| Patients with MGUS (n = 11,112) | |||
| Agent Orange exposurea | 3,797 | 0.85 (0.80–0.91) | < .001 |
| Female sexa | 174 | 0.64 (0.48–0.86) | < .001 |
| Age, ya | 66.8 (5.9) | 1.61 (1.53–1.69) | < .001 |
| Hispanic ethnicity | 457 | 0.9 (0.78–1.04) | .15 |
| Race | |||
| American Indian/Alaska Native, Hawaiian/Pacific Islander | 254 | 0.91 (0.75–1.11) | .34 |
| Blacka | 3430 | 0.78 (0.73–0.83) | < .001 |
| Nicotine dependenta | 2681 | 1.37 (1.28–1.46) | < .001 |
| Alcohol use disordera | 1165 | 1.26 (1.15–1.40) | < .001 |
| Drug use disorder | 663 | 1.1 (0.97–1.25) | .14 |
| Overweight (BMI 25–29)a | 3807 | 0.68 (0.63–0.74) | < .001 |
| Obese (BMI ≥ 30)a | 4786 | 0.61 (0.57–0.66) | < .001 |
| Major depressive disorder | 1648 | 0.98 (0.90–1.07) | .6 |
| Posttraumatic stress disordera | 1563 | 0.83 (0.75–0.91) | < .001 |
| Charlson Comorbidity Index (omits cancers)a | 2.2 (2.2) | 1.23 (1.22–1.25) | < .001 |
| MM (transformation)a | 2007 | 1.76 (1.65–1.88) | < .001 |
|
| |||
| Patients with MM (n = 7261) | |||
| Agent Orange exposurea | 2581 | 0.89 (0.84–0.95) | < .001 |
| Female sexa | 86 | 0.70 (0.52–0.95) | .02 |
| Age, ya | 66.5 (5.8) | 1.32 (1.25–1.39) | < .001 |
| Hispanic ethnicity | 343 | 0.98 (0.85–1.12) | .73 |
| Race | |||
| American Indian/Alaska Native, Hawaiian/Pacific Islander | 180 | 1.03 (0.86–1.23) | .78 |
| Blacka | 2009 | 0.86 (0.80–0.92) | < .001 |
| Nicotine dependencea | 1321 | 1.2 (1.11–1.29) | < .001 |
| Alcohol use disordera | 466 | 1.15 (1.01–1.31) | .03 |
| Drug use disorder | 308 | 1.01 (0.87–1.18) | .89 |
| Overweight (BMI 25–29)a | 2603 | 0.69 (0.64–0.74) | < .01 |
| Obese (BMI ≥ 30)a | 2840 | 0.64 (0.60–0.69) | < .001 |
| Major depressive disorder | 853 | 1.02 (0.93–1.13) | .66 |
| Posttraumatic stress disorder | 801 | 0.92 (0.83–1.02) | .10 |
| Charlson Comorbidity Index (omits cancers)a | 1.6 (1.9) | 1.13 (1.12–1.15) | < .001 |
| MGUS (transformation)a | 2,007 | 0.62 (0.58–0.67) | < .001 |
| Hematopoietic stem cell transplantationa | 627 | 0.87 (0.79–0.97) | .01 |
|
| |||
| Interaction model for patients with MM (n = 7261) | |||
| Agent Orange exposure and MGUSa | 695 | 0.53 (0.48–0.60) | < .001 |
| Agent Orange exposure without MGUSa | 1886 | 0.91 (0.85–0.98) | .01 |
| MGUS without Agent Orange exposurea | 1312 | 0.64 (0.59–0.70) | < .001 |
| Female sexa | 86 | 0.70 (0.52–0.95) | .02 |
| Age, ya | 66.5 (5.8) | 1.32 (1.25–1.39) | < .001 |
| Hispanic ethnicity | 343 | 0.98 (0.85–1.12) | .72 |
| Race | |||
| American Indian/Alaska Native, Hawaiian/Pacific Islander | 180 | 1.03 (0.86–1.23) | .79 |
| Blacka | 2009 | 0.86 (0.80–0.92) | < .001 |
| Nicotine dependencea | 1321 | 1.20 (1.11–1.29) | <.001 |
| Alcohol use disordera | 466 | 1.15 (1.01–1.31) | .03 |
| Substance use disorder | 308 | 1.01 (0.87–1.18) | .89 |
| Overweight (BMI 25–29)a | 2603 | 0.69 (0.64–0.74) | <.001 |
| Obese (BMI ≥ 30)a | 2840 | 0.64 (0.60–0.69) | <.001 |
| Major depressive disorder | 853 | 1.02 (0.93–1.13) | .67 |
| Posttraumatic stress disorder | 801 | 0.92 (0.83–1.02) | .12 |
| Charlson Comorbidity Index (omits cancers)a | 1.6 (1.9) | 1.13 (1.12–1.15) | <.001 |
| Hematopoietic stem cell transplantationa | 627 | 0.88 (0.79–0.97) | .01 |
Abbreviations: BMI, body mass index; MGUS, monoclonal gammopathy of uncertain significance; MM, multiple myeloma.
Significant at P < .05.
FIGURE.
Kaplan-Meier Curves
In the adjusted model of the total sample, the mortality hazard was greater for veterans who were older, with AUD and nicotine dependence, greater comorbidity per the CCI, diagnosis of MM, and transformation from MGUS to MM. Protective effects were noted for AO exposure, female sex, Black race, obesity, overweight, PTSD, and HSCT.
After adjusting for covariates, AO exposure was still associated with lower mortality among 11,112 patients with MGUS (HR, 0.85; 95% CI, 0.80–0.91). Risk factors were older age, nicotine dependence, AUD, the adapted CCI score (HR, 1.23 per point increase in the index; 95% CI, 1.22–1.25), and transformation to MM (HR, 1.76; 95% CI, 1.65–1.88). Additional protective factors were female sex, Black race, obesity, overweight, and PTSD.
After adjusting for covariates and limiting the analytic cohort to MM patients, the effect of AO exposure persisted (HR, 0.89; 95% CI, 0.84–0.95). Mortality risk factors were older age, nicotine dependence, AUD, and higher CCI score. Also protective were female sex, Black race, obesity, overweight, diagnosis of MGUS (transformation), and HSCT.
In the final model on patients with MM, the interaction term of AO exposure with transformation was significant. The combination of AO exposure with MGUS transformation had a greater protective effect than either AO exposure alone or MGUS without prior AO exposure. Additional protective factors were female sex, Black race, obesity, overweight, and HSCT. Older age, AUD, nicotine dependence, and greater comorbidity increased mortality risk.
DISCUSSION
Elucidating the pathophysiology and risk of transformation from MGUS to MM is an ongoing endeavor, even 35 years after the end of US involvement in the Vietnam War. Our study sought to understand a relationship between AO exposure, risk of MGUS transforming to MM, and associated mortality in US Vietnam War veterans. The rate of transformation (MGUS progressing to active MM) is well cited at 1% per year.15 Here, we found 12% of our cohort had undergone this transformation over 10 years.
Vietnam War era veterans who were exposed to AO during the Operation Ranch Hand period had 2.4 times greater risk of developing MGUS compared with veterans not exposed to AO.8 Our study was not designed to look at this association of AO exposure and MGUS/MM as this was a retrospective review to assess the difference in outcomes based on AO exposure. We found that AO exposure is associated with a decrease in mortality in contrast to a prior study showing worse survival with individuals with AO exposure.10 Another single center study found no association between AO exposure and overall survival, but it did identify an increased risk of progression from MGUS to MM.11 Our study did not show increased risk of transformation but did show positive effect on survival.
Black individuals have twice the risk of developing MM compared with White individuals and are diagnosed at a younger age (66 vs 70 years, respectively).16 Interestingly, Black race was a protective factor in our study. Given the length of time (35 years) elapsed since the Vietnam War ended, it is likely that most vulnerable Black veterans did not survive until our observation period.
HSCT, as expected, was a protective factor for veterans undergoing this treatment modality, but it is unclear why such a small number (8%) underwent HSCT as this is a standard of care in the management of MM. Obesity was also found to be a protective factor in a prior study, which was also seen in our study cohort.8
Limitations
This study was limited by its retrospective review of survivors among the Vietnam-era cohort several decades after the exposure of concern. Clinician notes and full historical data, such as date of onset for any disorder, were unavailable. These data also relied on the practitioners caring for the veterans to make the correct diagnosis with the associated code so that the data could be captured. Neither AO exposure nor diagnoses codes were verified against other sources of data; however, validation studies over the years have supported the accuracy of the diagnosis codes recorded in the VA EHR.
CONCLUSIONS
Because AO exposure is a nonmodifiable risk factor, focus should be placed on modifiable risk factors (eg, nicotine dependence, alcohol and substance use disorders, underlying comorbid conditions) as these were associated with worse outcomes. Future studies will look at the correlation of AO exposure, cytogenetics, and clinical outcomes in these veterans to learn how best to identify their disease course and optimize their care in the latter part of their life.
Supplementary Data
eAPPENDIX.
Variable Definitions
| Cohort definition | ICD-9 diagnosis codes/beginnings |
|---|---|
| MGUS | 273.1 |
|
| |
| Multiple myeloma | 203.00, 203.01, 203.02 |
|
| |
| Mental and behavioral disorders | |
| Alcohol use disorder | 303, 305.0 |
| Substance use disorder | 304, 305.2–305.9 |
| Nicotine dependence | 305.1, V15.82 |
| Major depressive disorder | 311, 296.2, 296.3 |
| Posttraumatic stress disorder | 309.81 |
| Schizophrenia or bipolar disorder | 295, 296.0, 296.1, 296.4–296.8 |
| Anxiety | 300.00–300.02 |
| Overweight or obesity | 278.00, 278.01, 278.02 |
|
| |
| Other common conditions | |
| Dyslipidemia | 272 |
| Hypertension | 401–405 |
|
| |
| Charlson Comorbidity Index conditions | |
| Myocardial infarction | 410, 412 |
| Heart failure | 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 425.4–425.5, 425.7–425.9, 428 |
| Peripheral vascular disease | 093.0, 437.3, 440, 441, 443.1, 443.2, 443.8, 443.9, 447.1, 557.1, 557.9, V43.4 |
| Cerebral vascular | 362.34, 430–438 |
| Dementia | 290, 294.1, 331.2 |
| COPD | 416.8, 416.9, 490–496, 500–505, 506.4, 508.1, 508.8 |
| Rheumatic disease | 446.5, 710.0, 710.1–710.4, 714.0–714.2, 714.8, 725 |
| Peptic ulcer disease | 531–534 |
| Cirrhosis of the liver | 070.22, 070.23, 070.32, 070.33, 070.44, 070.54, 070.6, 070.9, 570, 571, 573.3, 573.4, 573.8, 573.9, V42.7 |
| Diabetes mellitus without complications | 250.0–250.3, 250.8–250.9 |
| Diabetes mellitus with complications | 250.4–250.7 |
| Hemiplegia, paraplegia | 334.1, 342, 343, 344.0–344.6, 344.9 |
| Renal disease | 403.01, 403.11, 403.91, 404.02, 404.03, 404.12, 404.13, 404.92, 404.93, 582, 583.0, 583.1, 583.2, 583.4, 583.6, 583.7, 585, 586, 588.0, V42.0, V45.1, V56 |
| Other cancers | 140–172, 174–195, 200–208, 238.6 |
| Liver failure | 456.0–456.2, 572.2–572.4, 572.8 |
| Metastatic solid tumors (omitted from index) | 196–199 |
| HIV/AIDS | 042, 043, 044 |
|
| |
| Procedures (treatment) | |
| HCT: ICD-9 procedure codes | 41.0, 41.00, 41.04, 41.07, 41.09 |
| HCT: ICD-10 procedure codes | 30230Y0, 30233Y0, 30240Y0, 30243Y0, 30230C0, 30233C0, 30240C0, 30243C0 |
| HCT: CPT code | 38241 |
Abbreviations: HCT, hematopoietic cell transplantation; ICD, International Classification of Diseases; MGUS, monoclonal gammopathy of undetermined significance.
Acknowledgments
This research was supported by the Central Texas Veterans Health Care System and Baylor Scott and White Health, both in Temple and Veterans Affairs Central Western Massachusetts Healthcare System, Leeds.
Footnotes
Author affiliations can be found at the end of this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the US Government, or any of its agencies. This article may discuss unlabeled or investigational use of certain drugs. Please review the complete prescribing information for specific drugs or drug combinations—including indications, contraindications, warnings, and adverse effects—before administering pharmacologic therapy to patients.
Ethics and consent
All authors adhered to the ethical principles for medical research involving human and animal subjects outlined in the World Medical Association’s Declaration of Helsinki. This is a database only study and was determined to be exempt by Central Texas Veterans Healthcare System Institutional Review Board.
Author disclosures
The authors report no actual or potential conflicts of interest or outside sources of funding with regard to this article.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30. doi: 10.3322/caac.21442. [DOI] [PubMed] [Google Scholar]
- 2.Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15(12):e538–e548. doi: 10.1016/S1470-2045(14)70442-5. [DOI] [PubMed] [Google Scholar]
- 3.Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21–33. doi: 10.4065/78.1.21. [DOI] [PubMed] [Google Scholar]
- 4.Kyle RA, Therneau TM, Rajkumar SV, et al. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med. 2002;346(8):564–569. doi: 10.1056/NEJMoa01133202. [DOI] [PubMed] [Google Scholar]
- 5.International Myeloma Foundation. [Accessed June 20, 2022];What Are MGUS, smoldering and active myeloma? Updated June 6, 2021. https://www.myeloma.org/what-are-mgus-smm-mm . [Google Scholar]
- 6.Riedel DA, Pottern LM. The epidemiology of multiple myeloma. Hematol Oncol Clin North Am. 1992;6(2):225–247. doi: 10.1016/S0889-8588(18)30341-1. [DOI] [PubMed] [Google Scholar]
- 7.Buckingham WA., Jr . Operation Ranch Hand: The Air Force and herbicides in southeast Asia, 1961–1971. Washington, DC: Office of Air Force History United States Air Force; 1982. [Accessed June 20, 2022]. https://apps.dtic.mil/sti/pdfs/ADA121709.pdf . [Google Scholar]
- 8.Landgren O, Shim YK, Michalek J, et al. Agent Orange exposure and monoclonal gammopathy of undetermined significance: an Operation Ranch Hand veteran cohort study. JAMA Oncol. 2015;1(8):1061–1068. doi: 10.1001/jamaoncol.2015.2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mescher C, Gilbertson D, Randall NM, et al. The impact of Agent Orange exposure on prognosis and management in patients with chronic lymphocytic leukemia: a National Veteran Affairs Tumor Registry Study. Leuk Lymphoma. 2018;59(6):1348–1355. doi: 10.1080/10428194.2017.1375109. [DOI] [PubMed] [Google Scholar]
- 10.Callander NS, Freytes CO, Luo S, Carson KR. Previous Agent Orange exposure is correlated with worse outcome in patients with multiple myeloma (MM) [abstract] Blood. 2015;126(23):4194. doi: 10.1182/blood.V126.23.4194.4194. [DOI] [Google Scholar]
- 11.Bumma N, Nagasaka M, Kim S, Vankayala HM, Ahmed S, Jasti P. Incidence of monoclonal gammopathy of undetermined significance (MGUS) and subsequent transformation to multiple myeloma (MM) and effect of exposure to Agent Orange (AO): a single center experience from VA Detroit [abstract] Blood. 2017;130(suppl 1):5383. doi: 10.1182/blood.V130.Suppl_1.5383.5383. [DOI] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 14.Copeland LA, Zeber JE, Sako EY, et al. Serious mental illnesses associated with receipt of surgery in retrospective analysis of patients in the Veterans Health Administration. BMC Surg. 2015;15:74. doi: 10.1186/s12893-015-0064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Younes MA, Perez JD, Alirhayim Z, Ochoa C, Patel R, Dabak VS. MGUS Transformation into multiple myeloma in patients with solid organ transplantation [Abstract presented at American Society of Hematology Annual Meeting, November 15, 2013] Blood. 2013;122(21):5325. doi: 10.1182/blood.V122.21.5325.5325. [DOI] [Google Scholar]
- 16.Waxman AJ, Mink PJ, Devesa SS, et al. Racial disparities in incidence and outcome in multiple myeloma: a population-based study. Blood. 2010 Dec 16;116(25):5501–5506. doi: 10.1182/blood-2010-07-298760. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAPPENDIX.
Variable Definitions
| Cohort definition | ICD-9 diagnosis codes/beginnings |
|---|---|
| MGUS | 273.1 |
|
| |
| Multiple myeloma | 203.00, 203.01, 203.02 |
|
| |
| Mental and behavioral disorders | |
| Alcohol use disorder | 303, 305.0 |
| Substance use disorder | 304, 305.2–305.9 |
| Nicotine dependence | 305.1, V15.82 |
| Major depressive disorder | 311, 296.2, 296.3 |
| Posttraumatic stress disorder | 309.81 |
| Schizophrenia or bipolar disorder | 295, 296.0, 296.1, 296.4–296.8 |
| Anxiety | 300.00–300.02 |
| Overweight or obesity | 278.00, 278.01, 278.02 |
|
| |
| Other common conditions | |
| Dyslipidemia | 272 |
| Hypertension | 401–405 |
|
| |
| Charlson Comorbidity Index conditions | |
| Myocardial infarction | 410, 412 |
| Heart failure | 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 425.4–425.5, 425.7–425.9, 428 |
| Peripheral vascular disease | 093.0, 437.3, 440, 441, 443.1, 443.2, 443.8, 443.9, 447.1, 557.1, 557.9, V43.4 |
| Cerebral vascular | 362.34, 430–438 |
| Dementia | 290, 294.1, 331.2 |
| COPD | 416.8, 416.9, 490–496, 500–505, 506.4, 508.1, 508.8 |
| Rheumatic disease | 446.5, 710.0, 710.1–710.4, 714.0–714.2, 714.8, 725 |
| Peptic ulcer disease | 531–534 |
| Cirrhosis of the liver | 070.22, 070.23, 070.32, 070.33, 070.44, 070.54, 070.6, 070.9, 570, 571, 573.3, 573.4, 573.8, 573.9, V42.7 |
| Diabetes mellitus without complications | 250.0–250.3, 250.8–250.9 |
| Diabetes mellitus with complications | 250.4–250.7 |
| Hemiplegia, paraplegia | 334.1, 342, 343, 344.0–344.6, 344.9 |
| Renal disease | 403.01, 403.11, 403.91, 404.02, 404.03, 404.12, 404.13, 404.92, 404.93, 582, 583.0, 583.1, 583.2, 583.4, 583.6, 583.7, 585, 586, 588.0, V42.0, V45.1, V56 |
| Other cancers | 140–172, 174–195, 200–208, 238.6 |
| Liver failure | 456.0–456.2, 572.2–572.4, 572.8 |
| Metastatic solid tumors (omitted from index) | 196–199 |
| HIV/AIDS | 042, 043, 044 |
|
| |
| Procedures (treatment) | |
| HCT: ICD-9 procedure codes | 41.0, 41.00, 41.04, 41.07, 41.09 |
| HCT: ICD-10 procedure codes | 30230Y0, 30233Y0, 30240Y0, 30243Y0, 30230C0, 30233C0, 30240C0, 30243C0 |
| HCT: CPT code | 38241 |
Abbreviations: HCT, hematopoietic cell transplantation; ICD, International Classification of Diseases; MGUS, monoclonal gammopathy of undetermined significance.