CASE REPORT
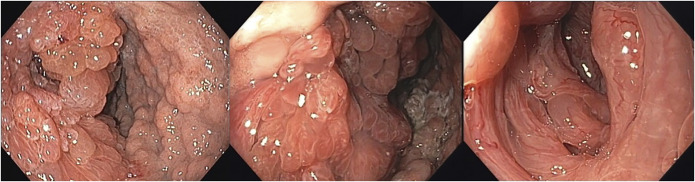
A 61-year-old woman with a medical history of ulcerative colitis had an esophagogastroduodenoscopy performed in 2015. The gastric mucosa revealed multiple polypoid lesions (Figure 1). Biopsies were compatible with hyperplastic polyps. In the same year, because of ulcerative colitis therapy refractoriness, a total proctocolectomy was performed.
Figure 1.
Gastric mucosa with multiple polypoid lesions.
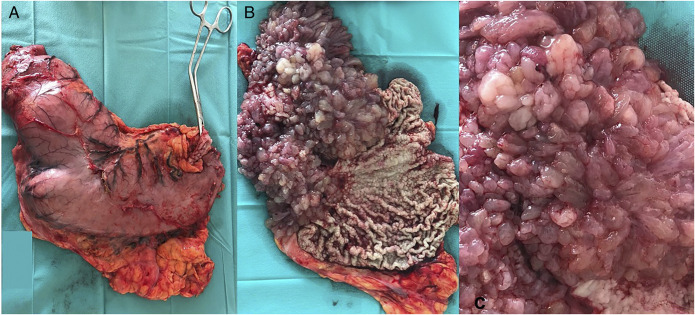
In June 2020, the patient presented with recurrent vomiting. An esophagogastroduodenoscopy revealed the previously described lesions, causing stenosis of the antrum (Figure 2). Given the gastric outlet obstruction, a total gastrectomy was performed (Figure 3). Pathological evaluation of the lesions showed hamartomatous polyps with hyperplastic features and cystic crypt dilation (Figure 4).
Figure 2.
Gastric antrum with luminal stenosis caused by obstructing polypoid lesions.
Figure 3.
(A) Gastrectomy specimen. (B and C) Diffuse infiltration with polypoid lesions is seen in the luminal aspect of the gastric wall, mainly in the antrum.
Figure 4.
(A) Hamartomatous polyp in hematoxylin-eosin (HE). (B and C) Close-ups of hyperplastic features of foveolar epithelium with crypt dilatation, lamina propia oedema, and superficial erosion (HE ×16)
A complete panel of mutations commonly associated with polyposis syndromes came out negative. Even though, given the diffuse infiltration of the stomach wall with hamartomatous polyps, juvenile polyposis syndrome was assumed. Because the patient already had a proctocolectomy, the oncologic risk was considered negligible.
Juvenile polyposis syndrome is a rare autosomal dominant disease. The term juvenile refers to the histopathological features, which include a dense stroma, inflammatory infiltrate, and dilated cystic glands filled with mucus in the lamina propria.1
The diagnosis requires at least 5 juvenile polyps in the colorectum, juvenile polyps in other parts of the gastrointestinal tract, or a family history of the syndrome plus any number of juvenile polyps.1–3 Hemorrhage, anemia, and intestinal obstruction are common presentations.4 Germline mutations of SMAD4 or BMPR1A are present in 50%–60%.3–5 The risk of colorectal cancer and upper gastrointestinal malignancies is 38%–68% and 21%, respectively.5 Polyps in this syndrome are usually removed by endoscopic polypectomy, but if there are too many, too big, or symptomatic, surgery may be indicated.5
DISCLOSURES
Author contributions: All authors contributed to the writing of this paper.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Contributor Information
Pedro Currais, Email: pedro_currais@live.com.pt.
Ana Craciun, Email: aanacraciun@gmail.com.
Margarida Sobral Dias, Email: margarida.dias@chln.min-saude.pt.
João Lopes, Email: joaocpslopes@gmail.com.
Teresa Cabral Braga, Email: teresacabralbraga@gmail.com.
Hélder Matos, Email: helderssmatos@gmail.com.
José Paulo Freire, Email: freire20@sapo.pt.
Ana Berta Almeida, Email: anaalmeida@chln.min-saude.pt.
Bárbara Pena, Email: baba373moon@hotmail.com.
Cristina Ferreira, Email: cristina.ferreira@chln.min-saude.pt.
Luís Carrilho Ribeiro, Email: luis.carrilho@chln.min-saude.pt.
Rui Tato Marinho, Email: ruitatomarinho@sapo.pt.
REFERENCES
- 1.Hussain T, Church JM. Juvenile polyposis syndrome. Clin Case Rep. 2020;8(1):92–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brosens LAA, Langeveld D, van Hattem WA, et al. Juvenile polyposis syndrome. World J Gastroenterol. 2011;17(44):4839–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Latchford AR, Neale K, Phillips RKS, Clark SK. Juvenile polyposis syndrome: A study of genotype, phenotype, and long-term outcome. Dis Colon Rectum. 2012;55(10):1038–43. [DOI] [PubMed] [Google Scholar]
- 4.Gao XH, Li J, Zhao ZY, et al. Juvenile polyposis syndrome might be misdiagnosed as familial adenomatous polyposis: A case report and literature review. BMC Gastroenterol. 2020;20(167):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW. HHS public access. Am J Gastroenterol. 2015;110(2):223–63. [DOI] [PMC free article] [PubMed] [Google Scholar]