Abstract
Background
Insomnia is a prevailing health problem among older adults. Tai Chi, a popular mind-body exercise practiced by older people in various oriental communities, has been shown to improve sleep. However, Tai Chi has not been directly compared to cognitive behavioral therapy for insomnia (CBT-I), which is the first-line non-pharmacological treatment for insomnia in older adults. This study aims to examine whether Tai Chi is non-inferior to CBT-I as a treatment for insomnia in older adults.
Methods
This is a single-center, assessor-blinded, non-inferiority randomized controlled trial comparing Tai Chi and CBT-I in 180 older adults aged ≥50 years with chronic insomnia according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Participants will be randomly assigned to either the Tai Chi or CBT-I group. Interventions will last for 3 months with a 12-month follow-up. The primary outcome is self-perceived insomnia severity measured by Insomnia Severity Index (ISI) at 3 months and at 15 months. The secondary outcomes include the remission rate of chronic insomnia, insomnia treatment response, subjective sleep quantity and quality, 7-day actigraphy, 7-day sleep diary, sleep medication, health-related quality of life, mental health, body balance and lower extremity function, adverse events, habitual physical activity, and dietary intake. Measurements will be conducted at baseline, 3 months, and 15 months by outcome assessors who are blinded to the group allocation.
Discussion
This will be the first non-inferiority randomized controlled trial to compare the efficacy and long-term outcomes of Tai Chi versus CBT-I for treating insomnia in older adults. This study will be of clinical importance as it supports the use of Tai Chi as an alternative non-pharmacological approach for insomnia treatment and sustainable management.
Keywords: Chronic insomnia, Cognitive behavioral therapy for insomnia (CBT-I), Non-inferiority trial, Tai Chi
1. Introduction
Insomnia is a common sleep disorder in older adults. Over 50% of the older population worldwide have sleep complaints, and 20%–40% of them present with insomnia.1 In Hong Kong, approximately 40% of adults have insomnia.2 These figures are alarming because persistent sleep disturbance and insomnia increase morbidity (e.g., mood disorders, cardiovascular diseases) and prospectively increase mortality.3 Moreover, insomnia negatively affects cognition.4 As the worldwide population continues to age, insomnia in older adults will increasingly lead to immense economic burdens on healthcare systems and on society.
In older patients with insomnia, the use of pharmacological treatments is a concern, because they can cause adverse effects such as drug dependence and abuse, cognitive impairment, and increase the risk of falls and hip fractures.5 On the other hand, through addressing sleep-related physiological and cognitive arousal, and behavioral and cognitive factors that perpetuate insomnia,6 cognitive behavioral therapy for insomnia (CBT-I) is a more appropriate treatment for insomnia in older adults, because it has been consistently shown to be effective with fewer side effects.7 Nonetheless, accessibility to CBT-I is limited due to the associated high costs and availability of trained therapists, preventing its wider use in the community. Due to its limited availability, CBT-I hardly meets the demands of the increasing number of older adults with insomnia. In addition, a local study conducted in Hong Kong reported that 60% of adults do not seek timely clinical consultation and treatment for insomnia.8 Given that the prevalence of insomnia in the older population is already high and continues to increase, there is a pressing need to explore alternative effective therapeutic modalities for insomnia that are both acceptable and accessible.
Tai Chi is widely practiced in the Chinese communities and is increasingly popular in western countries.9 According to the National Health Interview Surveys in the United States, the practice of Tai Chi and other mind-body exercise modalities increased from 5.8% in 2002 to 14.5% in 2017.10 Tai Chi is safe and has been reported to have high levels of adherence and enjoyment. It is well acknowledged to be a suitable exercise modality for older adults, even among those who are inactive or unfit.11, 12, 13 Compared to CBT-I, Tai Chi is a convenient and inexpensive exercise, and hence, more amenable in older adults, which will facilitate its large-scale adoption in the older population. The promising sleep-promoting effects of Tai Chi in older adults have been well demonstrated by randomized controlled trials and meta-analyses.6,14, 15, 16, 17, 18, 19 Our previous work showed that 12-week Tai Chi intervention significantly improved both the subjective and objective sleep in older adults with chronic insomnia, and the improvements were sustainably maintained over 24 months.15 The underlying mechanisms that mediating the sleep-promoting effects of Tai Chi were preliminarily reported.20, 21, 22 It was found that long-term Tai Chi practice decreased the homogeneity of anterior cingulate cortex,21 and the mindfulness component of Tai Chi might increase the volume of hippocampus and the grey matter concentration in orbital frontal cortex.22,23 In addition, Tai Chi has also been shown to have various health benefits, including preventing falls, improving cardiorespiratory and musculoskeletal fitness, psychological well-being and mental health.24, 25, 26 Therefore, Tai Chi may be a suitable exercise modality for treating insomnia in older adults, as it also confers additional health benefits.
Despite the positive effects of Tai Chi on improving sleep, no studies have compared Tai Chi with CBT-I as a treatment for chronic insomnia in older adults. Using a randomized non-inferiority trial approach, Tai Chi was shown to be non-inferior to CBT-I in treating insomnia in breast cancer survivors.6 However, it is worth noting that the risk factors (i.e., cancer stage and history of lumpectomy and chemotherapy) and clinical characteristics (i.e., increased levels of depression, anxiety and fatigue after the breast cancer diagnosis and treatments) of breast cancer survivors with chronic insomnia cannot be applied to individuals with chronic insomnia but no breast cancer history.27,28 Therefore, it is reasonable to postulate that the findings of this study on the clinical efficacy of Tai Chi in treating insomnia in breast cancer survivors might not be generalizable to the older population with chronic insomnia.
Although studies have compared Tai Chi with sleep education and CBT-I in older adults with insomnia, the study designs were flawed as they lacked appropriate non-inferiority evaluations and mood enhancement was included in the CBT-I protocol, which is not a typical CBT-I component.14,29 Therefore, an adequately powered randomized non-inferiority trial is needed to examine whether Tai Chi is non-inferior to CBT-I for treating insomnia in older adults. As chronic insomnia is characterized by cycles of relapse and remission, treatments that have long-term efficacy and help patients better manage their insomnia symptoms are preferred.30 A previous study demonstrated that the clinical response and remission rates could be maintained over a 12-month period after the Tai Chi and CBT-I interventions in breast cancer survivors with chronic insomnia, but the long-term efficacy of these interventions in improving sleep quality in older adults with chronic insomnia remains unknown.6 One of the primary aims of this study is to examine whether Tai Chi is non-inferior to CBT-I in maintaining sleep quality over the 12-month follow-up period.
2. Aims and hypotheses
This study aims to examine: 1) whether 3 months of Tai Chi (experimental) is non-inferior to 3 months of CBT-I (the first-line non-pharmacological treatment for insomnia) in treating insomnia in older adults, and 2) whether Tai Chi is non-inferior to CBT-I in sustaining the improvements on sleep quality for 12 months after the end of the interventions.
We hypothesize that Tai Chi will be non-inferior to CBT-I for treating insomnia in older adults and for sustaining the sleep quality improvements for 12 months post-intervention.
3. Methods
The current trial protocol has been designed and reported according to The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT),31 and The Consolidated Standards of Reporting Trials (CONSORT) and SPIRIT Extension for RCTs Revised in Extenuating Circumstances (CONSERVE).32
3.1. Trial design
This interventional study will be a single-center, parallel, assessor-blinded, non-inferiority randomized controlled trial. Participants will be allocated to the Tai Chi group or CBT-I group in a 1:1 ratio. The intervention will last for 3 months, and the follow-up period will last for 12 months. The total duration of the study will be 15 months. Assessments will be conducted at baseline, 3 months (post-intervention), and 15 months (12-month follow-up). The study was approved by the University of Hong Kong/Hospital Authority Hong Kong West Institutional Review Board (IRB approval number: UW 18–621). The study was registered in ClinicalTrials.gov (register number: NCT04384822, dated May 12, 2020). An independent committee was formed to review data and safety of study during the IRB application. Details were recorded in the IRB application form. The study will be conducted in accordance with the appropriate data protection legislation and the Declaration of Helsinki.33
3.2. Eligibility
Older adults with chronic insomnia will be recruited to the study. Inclusion criteria include: 1) aged ≥50 years, 2) ethnic Chinese, and 3) diagnosis of chronic insomnia (including difficulty in initiating sleep, maintaining sleep or early morning awakening, complaints of impaired daytime functioning and sleep difficulty occurring at least three nights per week and lasting for at least 3 months) according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).34 Both males and females will be included to enhance generalizability. Participants using sleep medications will also be included to widen the coverage and enhance the practical value of this study. Detailed medication information including drug name, type, dose, and weekly frequency will be recorded as a secondary outcome, which will provide additional practical measures for evaluating the intervention effects. As people with mental disorders can also benefit from the interventions, participants with comorbid mental disorders (e.g., depression and anxiety) will also be included.
Exclusion criteria include: 1) cannot walk without an assistive device (e.g., cane), 2) somatic conditions that limit Tai Chi participation (e.g., limb loss), 3) regular participation in moderate-intensity aerobic exercise or mind-body training such as Tai Chi, yoga, qigong, or meditation (>3 times weekly for >60 min per session), 4) chronic diseases that can affect sleep (e.g., pain disorders, cancer, and benign prostatic hyperplasia), 5) receiving treatments or drugs that can affect sleep (e.g., cancer chemotherapy), 6) dementia or receiving dementia treatments, 7) untreated sleep disorder including obstructive sleep apnea, periodic leg movement disorder and narcolepsy, 8) current or past CBT-I treatment, and 9) shift-worker. Participants who may be disruptive during the group sessions, such as those exhibiting uncontrolled violence or psychotic symptoms, will also be excluded.
3.3. Trial setting
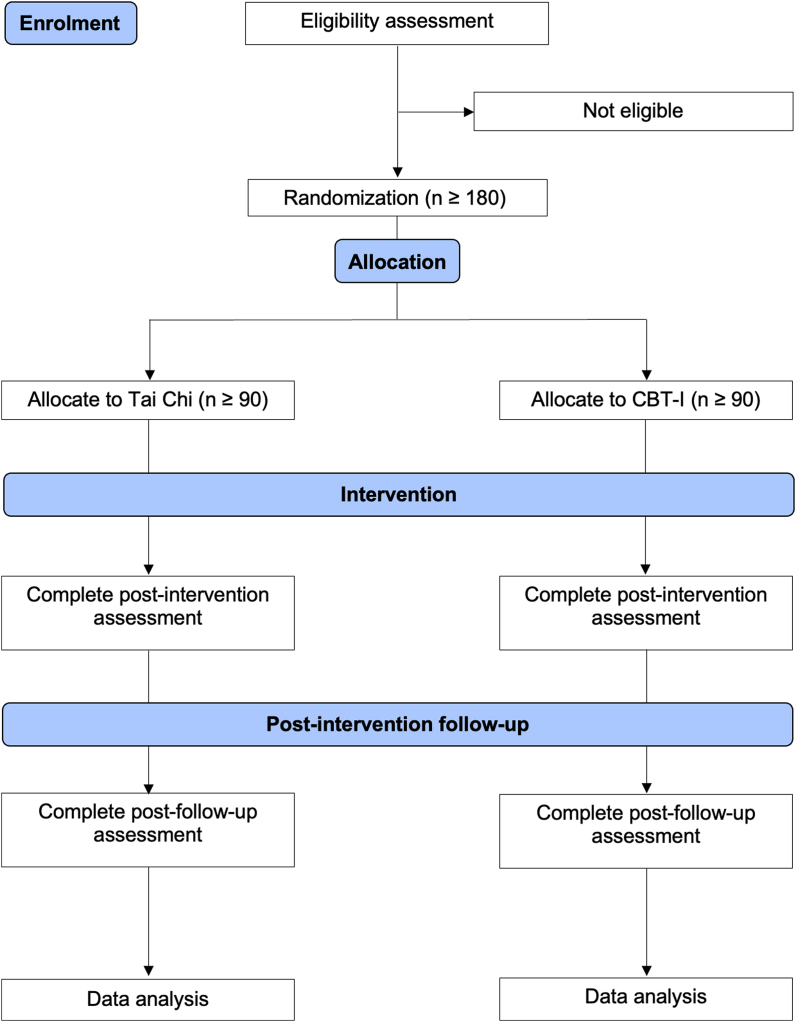
We will approach potential participants in the community via advertisements. Interested individuals will be invited to a preliminary visit to confirm eligibility. Verbal and written information on the study will be provided and written informed consent will be obtained before baseline outcome assessments. Validated instruments/devices will be used to assess the outcome measures. After the baseline assessments, participants will be randomized to either CBT-I or Tai Chi group in a 1:1 ratio. Fig. 1 shows a schematic representation of participants in the screening, randomization, and interventions.
Fig. 1.
Schematic representation of participants in the screening, randomization, and interventions.
3.4. Interventions
3.4.1. Cognitive behavioral therapy for insomnia (CBT-I)
Participants will take part in a conventional CBT-I program conducted in a group setting (8–12 participants per group) delivered by trained therapists. The CBT-I protocol, which has been adopted in previous studies, covers typical CBT-I components including: 1) sleep hygiene education, 2) stimulus control, 3) sleep restriction, 4) relaxation training, and 5) cognitive therapy, but does not include a mood enhancement component, as this is not usually part of CBT-I.6 The CBT-I program aims to address sleep-related physiological and cognitive arousal, and behavioral and cognitive factors that perpetuate insomnia.6 The 3-month CBT-I intervention will consist of two 1-h sessions weekly for a total of 24 sessions. The five therapeutic components will be administrated in the first 2 months followed by an additional month of consolidation. The extra month of treatment exposure provides skill consolidation and relapse prevention. Using a manualized approach, each session will include set objectives, learning skills, and class activities. Course materials will be distributed to the participants in the CBT-I group during the intervention. After the 3-month intervention, all course materials will also be distributed to participants via smartphone messages, Google Drive, and storage media to ensure accessibility during the follow-up period. Details of the manualized CBT-I intervention are listed in the Supplementary Material Table 1.
3.4.2. Tai Chi
Participants will take part in a Tai Chi program conducted in a group setting (8–12 participants per group) delivered by certified Tai Chi instructors. The Tai Chi intervention will be prescribed as a 3-month program with two 1-h sessions weekly for a total of 24 sessions, which is the same duration as the CBT-I intervention. The Tai Chi program will adopt the 24-form simplified Yang style, which is the most popular simplified form of Tai Chi and can be easy learnt in about 2–3 months.35 This form of Tai Chi was first promoted to the public as a fitness exercise by the Chinese Government in 1956.25 The Tai Chi intervention will be delivered in the first 2 months followed by 1 month of consolidation. The instructors will discuss safety issues, proper training principles, and introduce the skills in the first class to minimize any avoidable adverse events due to improper skills/practice. Each Tai Chi session consists of 10 min of breathing and relaxation as warm-up exercises, followed by 45 min of Tai Chi practice, and then 5 min of cool-down exercises. After the intervention, all course materials including videos of the breathing exercises, relaxation exercises, and the 24 forms of Tai Chi will be distributed to the participants via smartphone messages, Google Drive, and storage media to ensure accessibility during the follow-up period. The details of the Tai Chi intervention are listed in the Supplementary Material Table 2.
3.5. Primary outcome measures
3.5.1. Insomnia severity
The primary outcome will be the perceived insomnia severity measured by Insomnia Severity Index (ISI) at 3 months and 15 months. The ISI includes seven items assessing: 1) sleep onset, 2) sleep maintenance difficulties, 3) satisfaction with the current sleep pattern, 4) interference with daily functioning, 5) noticeable impairment due to sleep problems, 6) degree of distress, and 7) concerns caused by sleep problems. Each item is rated on a “0–4” Likert scale, with a higher score indicating more perceived severe insomnia. The Chinese version of the ISI has been shown to have a satisfactory content validity index of 0.94 and high internal consistency with a Cronbach's alpha of 0.81.36
3.6. Secondary outcome measures
Secondary outcomes of this study include remission of chronic insomnia, insomnia treatment response, subjective sleep quantity and quality, 7-day actigraphy, 7-day sleep diary, sleep medications, health-related quality of life, mental health, body balance and lower extremity function, adverse events, and habitual physical activity and dietary intake. The details of these secondary outcome measurements are described in the supplementary material list 1.
Outcome assessments will be conducted at baseline, 3 months, and 15 months by outcome assessors who will be blinded to the group allocation. Interventions will begin within 4 weeks after baseline measurements to ensure data validity. Similarly, outcome assessments will be conducted within 4 weeks after completion of the 3-month intervention and the 12-month follow-up. To minimize the acute effects of Tai Chi or CBT-I on the outcomes, the post-intervention assessments will be conducted at least 24 h after the last session of the interventions. All outcome measurements and data will be collected on the same day except data from the 7-day actigraphy, 7-day sleep diary, and the 3-day food diary, which will be collected one week later. The outcome measurements will be administered in the following order: 1) sleep-related outcomes including diagnosis of chronic insomnia, ISI, Pittsburgh Sleep Quality Index (PSQI), and sleep medication record; 2) other outcomes including the Short Form (SF) 12-item version 2 (SF12v2), the Hospital Anxiety and Depression Scale (HADS), the International Physical Activity Questionnaire (IPAQ), the Short Physical Performance Battery (SPPB), body weight and height; and 3) 7-day actigraphy, 7-day sleep diary, and 3-day food diary. The detailed timeframe of the outcome assessments and other major logistics of the trial are listed in the Supplementary Material Table 3.
3.7. Intervention quality monitoring
The CBT-I will be conducted by two qualified instructors to avoid intervention delivery bias due to individual differences in the teaching style/skill. The instructors will be supervised to ensure that they closely follow and administer the CBT-I protocol. Similarly, the Tai Chi interventions will be conducted by two qualified instructors according to the Tai Chi protocol. Additional measurements will be conducted to monitor the quality of the interventions. Details of these monitoring assessments are listed in the Supplementary Material Table 4.
3.8. Follow-up period
The post-intervention follow-up period will be 12 months. Standardized manualized procedures will be applied in both the Tai Chi and CBT-I groups to encourage and facilitate the participants in continuing to practice Tai Chi and CBT-I during the follow-up period, respectively. The details of the procedures implemented during the follow-up period are listed in the Supplementary Material Table 5.
3.9. Sample size estimation
The sample size calculation for detecting non-inferiority using a two-sample t-test between Tai Chi and CBT-I interventions was conducted using POWER in SAS OnDemand for Academics (SAS Institute). The sample size estimation is based on a primary comparison of insomnia severity by ISI between groups, using a 95% power and 0.05/2 = 0.025 maximum chance of committing false type I errors to account for multiplicity. We will adopt a threshold of 4 points in the ISI as the margin of non-inferiority to assess if Tai Chi is non-inferior to CBT-I. This value is commonly accepted as 50% of the reported minimally important difference (MID) in ISI (reported as 8 points).37, 38, 39 A margin of 4 points in ISI has also been previously adopted in several non-inferiority trials in the chronic insomniac population.6,40 Our pilot study indicated that there was a mean change of −5.05 in the Tai Chi group from the baseline ISI. Assuming the CBT-I group has similar effects on ISI with the standard deviation conservatively taken as 6.5, 70 participants per group will be required. Allowing for 20% dropout, we will recruit 90 participants (rounded up from 88) for each of the Tai Chi and CBT-I interventions, giving an overall study sample of 180 participants.
3.10. Randomization
3.10.1. Sequence generation
Sequence randomization will be generated by an independent researcher using an online random generator (https://www.sealedenvelope.com/) with block sizes of 4–6. The researcher will not interact with the participants during the recruitment or interventions to avoid potential allocation bias.
3.10.2. Allocation concealment
The computer-generated randomized allocation sequence will be securely kept in sealed opaque envelopes by an independent researcher who will not interact with the participants during the recruitment or interventions. Research personnel will contact the independent researcher to retrieve the allocation sequence before the start of the interventions.
3.11. Blinding
Participants cannot be blinded to the group allocation due to the nature of the Tai Chi and CBT-I interventions. The personnel delivering the CBT-I and Tai Chi also cannot be blinded to the group allocation and will not be involved in the outcome assessments. Outcome assessors will be blinded to the group allocation and will not be involved in group allocation and intervention implementation. Participants will be instructed not to disclose their group allocation to research personnel conducting the outcome assessments.
3.12. Statistical methods
Data will be presented as the mean ± standard deviation. Intention-to-treat principle will be adopted to include all randomized participants in the analyses. Missing data will be handled by multiple imputation, as previously adopted.41, 42, 43 Per-protocol analysis will also be used to examine completer-only data to provide a more conservative and stringent non-inferiority comparison. A non-inferiority analysis will be performed on the primary outcome by comparing the differences in the changes of the ISI scores between the two groups at post-intervention and follow-up assessments. Generalized estimating equations (GEE) will be used to examine the treatment effects on the quantitative secondary outcomes, adjusting for baseline values. Other baseline characteristics will be added as additional covariates in the GEE model to control for potential confounding effects using sensitivity analyses. Logistic regression will be performed to analyze the remission of insomnia. Linear contrasts of the respective statistical models will be used to estimate the treatment effects at 3 and 15 months. The level of significance will be set at P < 0.05 and all estimates will be accompanied by 95% confidence intervals.
4. Data management plan
A detailed data management plan is provided in the supplementary material appendix 1.
5. Brief discussion
This will be the first non-inferiority randomized controlled trial to compare the treatment efficacy and long-term efficacy of Tai Chi and CBT-I in older adults with chronic insomnia. Considering the limited accessibility and high cost of CBT-I, there is a pressing need to further validate the therapeutic efficacy of Tai Chi compared to CBT-I to support the use of Tai Chi as an alternative non-pharmacological treatment for chronic insomnia. The study conducted by Irwin and co-workers compared the effects of Tai Chi and CBT-I on improving sleep quality in breast cancer survivors with chronic insomnia. They demonstrated that a 3-month Tai Chi intervention was non-inferior to CBT-I on improving sleep at post-intervention.6 However, it is unclear whether these results can extend to the general older population. No study has directly compared the efficacy of Tai Chi to CBT-I in treating insomnia in older adults. The present study will examine whether a 3-month Tai Chi intervention is non-inferior to CBT-I for improving subjective sleep quality in older adults with chronic insomnia as measured by ISI. This is of clinical importance as it addresses the unmet needs of an insomnia treatment that is accessible and amenable for older adults, while also reducing the associated burdens on healthcare systems and society.
Longitudinal studies have reported that the median duration of chronic insomnia is 3 years, with 56%–74% of chronic insomnia patients experiencing persistent symptoms within the past year.44, 45, 46, 47 More alarmingly, 27% of treated patients relapsed post-remission.47 It is therefore essential to develop treatments that have long-term efficacy to help patients manage their chronic insomnia symptoms and improve their quality of life.30,48 Although CBT-I has been reported to have sustained sleep-promoting effects, a meta-analysis conducted by Zweerde and colleagues showed that these effects can decline over time, with the sleep improvements lasting for only 12 months post-treatment.49 In one of our previous studies, we showed the beneficial effects of Tai Chi on sleep were sustained for 24 months.15 No study has directly compared the long-term efficacy of Tai Chi and CBT-I on improving sleep in older adults with chronic insomnia. Therefore, another primary aim of this study is to monitor the change in insomnia severity as measured by ISI after the 12-month follow-up period to assess the long-term efficacy of both interventions. Evaluation of the long-term efficacy of Tai Chi compared to CBT-I will provide critical evidence to support the use of Tai Chi as an accessible and affordable non-pharmacological treatment for the long-term management of chronic insomnia.
The full-length of the discussion is provided in the supplementary material appendix 2.
Protocol version
Protocol version: 20221017-002; date: October 17, 2022.
List of secondary outcomes
The details of secondary outcome measurements are described in the supplementary material list 1.
List of abbreviation and full form
A list of abbreviation and full form is provided in the supplementary material list 2.
Ethics approval and consent to participate
The study was approved by the University of Hong Kong/Hospital Authority Hong Kong West Institutional Review Board (IRB approval number: UW 18–621). Interested individuals will be invited to a preliminary visit to confirm eligibility. Verbal and written information on the study will be provided and written informed consent will be obtained before baseline outcome assessments.
Consent for publication
Not applicable. This manuscript does not contain data from any individual person.
Availability of data and materials
Data collected for this study is available upon request.
Funding
This study is supported by General Research Fund of Research Grants Council (RGC), Hong Kong University Grants Committee (project number: 17112819) and Seed Fund for Basic Research of the University of Hong Kong. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Authors' contributions
PMS, SXL, DYF, DKCC, SSH, KFC, JW, CW and MRI conceived the study, formulated the research question, and sought funding support for this study. DJY and APY coordinated the intervention arrangement and outcome assessments. SXL, RNYC, APY and DJY supported the interventions. APY and DYF supported the statistical analyses. DJY and PMS drafted the initial version of the manuscript. All authors revised the manuscript for important intellectual content and approved the final version of the manuscript.
Trial status
The study was prospectively registered at ClinicalTrials.gov (NCT04384822) on May 12, 2020. The first participant was recruited on May 18, 2020, and the trial is estimated to be completed by September 30, 2023.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jesf.2022.10.012.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Schubert C.R., Cruickshanks K.J., Dalton D.S., Klein B.E., Klein R., Nondahl D.M. Prevalence of sleep problems and quality of life in an older population. Sleep. 2002;25:48–52. [PubMed] [Google Scholar]
- 2.Wong W.S., Fielding R. Prevalence of insomnia among Chinese adults in Hong Kong: a population-based study. J Sleep Res. 2011;20:117–126. doi: 10.1111/j.1365-2869.2010.00822.x. [DOI] [PubMed] [Google Scholar]
- 3.Stewart R., Besset A., Bebbington P., et al. Insomnia comorbidity and impact and hypnotic use by age group in a national survey population aged 16 to 74 years. Sleep. 2006;29:1391–1397. doi: 10.1093/sleep/29.11.1391. [DOI] [PubMed] [Google Scholar]
- 4.Fortier-Brochu É., Beaulieu-Bonneau S., Ivers H., Morin C.M. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev. 2012;16:83–94. doi: 10.1016/j.smrv.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Sasai T., Inoue Y., Komada Y., Nomura T., Matsuura M., Matsushima E. Effects of insomnia and sleep medication on health-related quality of life. Sleep Med. 2010;11:452–457. doi: 10.1016/j.sleep.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 6.Irwin M.R., Olmstead R., Carrillo C., et al. Tai Chi Chih compared with cognitive behavioral therapy for the treatment of insomnia in survivors of breast cancer: a randomized, partially blinded, noninferiority trial. J Clin Oncol. 2017;35:2656. doi: 10.1200/JCO.2016.71.0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trauer J.M., Qian M.Y., Doyle J.S., Rajaratnam S.M., Cunnington D. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med. 2015;163:191–204. doi: 10.7326/M14-2841. [DOI] [PubMed] [Google Scholar]
- 8.Liu Y., Zhang J., Lam S.P., et al. Help-seeking behaviors for insomnia in Hong Kong Chinese: a community-based study. Sleep Med. 2016;21:106–113. doi: 10.1016/j.sleep.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Yang G.-Y., Sabag A., Hao W.-L., et al. Tai Chi for health and well-being: a bibliometric analysis of published clinical studies between 2010 and 2020. Compl Ther Med. 2021;60 doi: 10.1016/j.ctim.2021.102748. [DOI] [PubMed] [Google Scholar]
- 10.Wang C., Li K., Choudhury A., Gaylord S. Trends in yoga, Tai Chi, and Qigong use among US adults. Am J Publ Health. 2019;109:755–761. doi: 10.2105/AJPH.2019.304998. 2002–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li J., Hong Y., Chan K. Tai chi: physiological characteristics and beneficial effects on health. Br J Sports Med. 2001;35:148–156. doi: 10.1136/bjsm.35.3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wayne P.M., Berkowitz D.L., Litrownik D.E., Buring J.E., Yeh G.Y. What do we really know about the safety of tai chi?: a systematic review of adverse event reports in randomized trials. Arch Phys Med Rehabil. 2014;95:2470–2483. doi: 10.1016/j.apmr.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han A., Judd M., Welch V., Wu T., Tugwell P., Wells G.A. Tai chi for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2004;(3):1465–1858. doi: 10.1002/14651858.CD004849. [DOI] [PubMed] [Google Scholar]
- 14.Irwin M.R., Olmstead R., Carrillo C., et al. Cognitive behavioral therapy vs. Tai Chi for late life insomnia and inflammatory risk: a randomized controlled comparative efficacy trial. Sleep. 2014;37:1543–1552. doi: 10.5665/sleep.4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siu P.M., Angus P.Y., Tam B.T., et al. Effects of tai chi or exercise on sleep in older adults with insomnia: a randomized clinical trial. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.37199. e2037199-e2037199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li H., Chen J., Xu G., et al. The effect of Tai Chi for improving sleep quality: a systematic review and meta-analysis. J Affect Disord. 2020;274:1102–1112. doi: 10.1016/j.jad.2020.05.076. [DOI] [PubMed] [Google Scholar]
- 17.Wang X., Li P., Pan C., Dai L., Wu Y., Deng Y. The effect of mind-body therapies on insomnia: a systematic review and meta-analysis. Evid. Based Complement. Alternat. Med. 2019;2019 doi: 10.1155/2019/9359807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hosseini H., Esfirizi M.F., Marandi S.M., Rezaei A. The effect of Ti Chi exercise on the sleep quality of the elderly residents in Isfahan, Sadeghieh elderly home. Iran J Nurs Midwifery Res. 2011;16:55. [PMC free article] [PubMed] [Google Scholar]
- 19.Raman G., Zhang Y., Minichiello V.J., D'Ambrosio C.M., Wang C. Tai Chi improves sleep quality in healthy adults and patients with chronic conditions: a systematic review and meta-analysis. J Sleep Disord Ther. 2013;2 doi: 10.4172/2167-0277.1000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu A.P., Tam B.T., Lai C.W., et al. Revealing the neural mechanisms underlying the beneficial effects of Tai Chi: a neuroimaging perspective. Am J Chin Med. 2018;46:231–259. doi: 10.1142/S0192415X18500131. [DOI] [PubMed] [Google Scholar]
- 21.Wei G.-X., Dong H.-M., Yang Z., Luo J., Zuo X.-N. Tai Chi Chuan optimizes the functional organization of the intrinsic human brain architecture in older adults. Front Aging Neurosci. 2014:74. doi: 10.3389/fnagi.2014.00074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luders E., Toga A.W., Lepore N., Gaser C. The underlying anatomical correlates of long-term meditation: larger hippocampal and frontal volumes of gray matter. Neuroimage. 2009;45:672–678. doi: 10.1016/j.neuroimage.2008.12.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hölzel B.K., Carmody J., Vangel M., et al. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res Neuroimaging. 2011;191:36–43. doi: 10.1016/j.pscychresns.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang C., Collet J.P., Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164:493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 25.Wayne P.M., Fuerst M. Shambhala Publications; 2013. The Harvard Medical School Guide to Tai Chi: 12 Weeks to a Healthy Body, Strong Heart, and Sharp Mind. [Google Scholar]
- 26.Wang C., Bannuru R., Ramel J., Kupelnick B., Scott T., Schmid C.H. Tai Chi on psychological well-being: systematic review and meta-analysis. BMC Compl Alternative Med. 2010;10:1–16. doi: 10.1186/1472-6882-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Savard J., Simard S., Blanchet J., Ivers H., Morin C.M. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001;24:583–590. doi: 10.1093/sleep/24.5.583. [DOI] [PubMed] [Google Scholar]
- 28.Fiorentino L., Ancoli-Israel S. Insomnia and its treatment in women with breast cancer. Sleep Med Rev. 2006;10:419–429. doi: 10.1016/j.smrv.2006.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edinger J.D., Arnedt J.T., Bertisch S.M., et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021;17:255–262. doi: 10.5664/jcsm.8986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cunnington D., Junge M.F., Fernando A.T. Insomnia: prevalence, consequences and effective treatment. Med J Aust. 2013;199:S36–S40. doi: 10.5694/mja13.10718. [DOI] [PubMed] [Google Scholar]
- 31.Chan A.-W., Tetzlaff J.M., Altman D.G., et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158:200–207. doi: 10.7326/0003-4819-158-3-201302050-00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Orkin A.M., Gill P.J., Ghersi D., et al. Guidelines for reporting trial protocols and completed trials modified due to the COVID-19 pandemic and other extenuating circumstances: the CONSERVE 2021 statement. JAMA. 2021;326:257–265. doi: 10.1001/jama.2021.9941. [DOI] [PubMed] [Google Scholar]
- 33.Williams J.R. The Declaration of Helsinki and public health. Bull World Health Organ. 2008;86:650–652. doi: 10.2471/BLT.08.050955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Psychiatric Association D., Association A.P. American psychiatric association; Washington, DC: 2013. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. [Google Scholar]
- 35.Yang G.-Y., Wang L.-Q., Ren J., et al. Evidence base of clinical studies on Tai Chi: a bibliometric analysis. PLoS One. 2015;10 doi: 10.1371/journal.pone.0120655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yu D.S. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66:2350–2359. doi: 10.1111/j.1365-2648.2010.05394.x. [DOI] [PubMed] [Google Scholar]
- 37.Siu P. 2015. Efficacy of Tai Chi Training to Alleviate Insomnia in Older Adults. [Google Scholar]
- 38.Morin C.M., Belleville G., Bélanger L., Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–608. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Julious S.A. Sample sizes for clinical trials with normal data. Stat Med. 2004;23:1921–1986. doi: 10.1002/sim.1783. [DOI] [PubMed] [Google Scholar]
- 40.Garland S.N., Carlson L.E., Stephens A.J., Antle M.C., Samuels C., Campbell T.S. Mindfulness-based stress reduction compared with cognitive behavioral therapy for the treatment of insomnia comorbid with cancer: a randomized, partially blinded, noninferiority trial. J Clin Oncol. 2014;32:449–457. doi: 10.1200/JCO.2012.47.7265. [DOI] [PubMed] [Google Scholar]
- 41.Wang C., Schmid C.H., Fielding R.A., et al. Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ. 2018:360. doi: 10.1136/bmj.k851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Siu P.M., Angus P.Y., Benzie I.F., Woo J. Effects of 1-year yoga on cardiovascular risk factors in middle-aged and older adults with metabolic syndrome: a randomized trial. Diabetol Metab Syndrome. 2015;7:1–12. doi: 10.1186/s13098-015-0034-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siu P.M., Yu A.P., Chin E.C., et al. Effects of tai chi or conventional exercise on central obesity in middle-aged and older adults: a three-group randomized controlled trial. Ann Intern Med. 2021;174:1050–1057. doi: 10.7326/M20-7014. [DOI] [PubMed] [Google Scholar]
- 44.Morin C.M., Drake C.L., Harvey A.G., et al. Insomnia disorder. Nat Rev Dis Prim. 2015;1:1–18. doi: 10.1038/nrdp.2015.26. [DOI] [PubMed] [Google Scholar]
- 45.Pillai V., Roth T., Drake C.L. The nature of stable insomnia phenotypes. Sleep. 2015;38:127–138. doi: 10.5665/sleep.4338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Morphy H., Dunn K.M., Lewis M., Boardman H.F., Croft P.R. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30:274–280. [PubMed] [Google Scholar]
- 47.Morin C.M., Bélanger L., LeBlanc M., et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009;169:447–453. doi: 10.1001/archinternmed.2008.610. [DOI] [PubMed] [Google Scholar]
- 48.Morin C.M., Benca R. Chronic insomnia. Lancet. 2012;379:1129–1141. doi: 10.1016/S0140-6736(11)60750-2. [DOI] [PubMed] [Google Scholar]
- 49.van der Zweerde T., Bisdounis L., Kyle S.D., Lancee J., van Straten A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med Rev. 2019;48 doi: 10.1016/j.smrv.2019.08.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data collected for this study is available upon request.