Abstract
Background
Family and other unpaid caregivers play an active role in the recovery of individuals with pancreatic and periampullary cancer after pancreatectomy. However, little is known about caregivers’ experiences and how to better support them.
Methods
Caregivers accompanying patients to 1-month postpancreatectomy visits at 3 hospitals completed an electronic survey between November 2018 and February 2020. We examine measures of absenteeism and work productivity loss among the subset of caregivers who reported working for pay and comparatively assess caregiver experiences by employment status. All analyses were performed as 2-sided tests.
Results
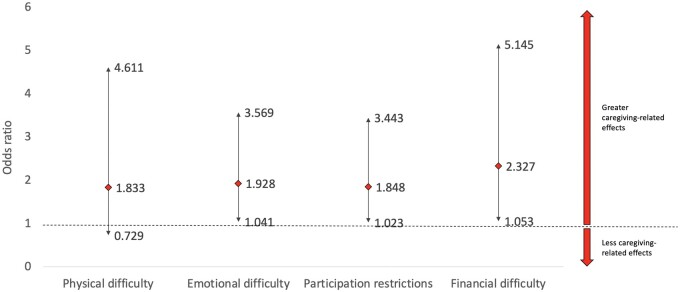
Of 265 caregivers approached for study participation, 240 (90.6%) enrolled. Caregivers were primarily female (70.8% female, 29.2% male) and spouses (58.3%) or adult children (25.8%) of patients, with a median age of 60 years. Of the 240 caregivers included in the study, 107 (44.6%) worked for pay. Nearly half (44.4%) of working caregivers reported being absent from work because of caregiving amounting to a 14% loss in work hours. While at work, 58.9% of working caregivers reported increased work difficulty as a result of caregiving. Taken together, an estimated 59.7% loss in work productivity was experienced because of caregiving in the month following pancreatectomy. After adjustment for sociodemographic factors, working (vs nonworking) caregivers reported increased financial (odds ratio [OR] = 2.32; P = .04) and emotional (OR = 1.93; P = .04) difficulties and daily activity restrictions (OR = 1.85; P = .048).
Conclusions
Working caregivers of patients with pancreatic and periampullary cancer experience negative impacts on work and productivity, and caregiving-related financial and emotional difficulties may be amplified. This study highlights the need for workplace policies to support unpaid cancer caregiving.
With the aging of the population, family members and unpaid caregivers who provide help for their relatives and friends represent an important but overlooked aspect of long-term care support. In 2016, it was estimated that approximately 18 million Americans are family caregivers to older adults with disabilities (1). The focus on family caregiving has historically been directed at policy on long-term services and supports. There is growing recognition that the role has expanded to encompass complex medical and nursing tasks as care is increasingly provided in the community (2). However, caregivers are often poorly prepared for tasks that they are expected to assume, and little is known about their experiences and preparedness within specific clinical contexts (3). Efforts are underway that provide data on caregivers for older adults with dementia or disabilities to inform interventions and policies that can support a patient- and caregiver-centric care delivery model (3,4). However, these efforts are lacking for patients with solid organ tumors.
Pancreatic cancer is the third leading cause of cancer deaths in the United States with 48 220 deaths projected for 2021 (5). Surgical resection is the only treatment option that affords patients the possibility of long-term survival. Given the advanced age and frailty of pancreatic and periampullary cancer patients at the time of diagnosis, these patients experience substantial distress and often rely on family caregivers for support and assistance (6,7). Additionally, pancreatectomy is associated with clinically significant morbidity, including high complication and readmission rates (8-10), changes in bowel habits, diabetes, and pancreatic exocrine insufficiency manifesting as malabsorption requiring daily enzyme replacement therapy (11–14). These issues make it especially challenging for caregivers who often assume this role.
Despite these challenges, family caregivers for patients after pancreatectomy are not systematically identified or routinely assessed. Little is known about caregivers’ experiences and how to support them. The primary aim of this study is to assess the caregiving-related effects experienced by caregivers of patients with pancreatic and periampullary cancer who have had a pancreatectomy. This includes effects on physical and emotional well-being, financial difficulties, work productivity, and ability to perform daily activities. As a secondary aim, this study also examines the differential impact of caregiving on caregivers who work for pay and those who do not, given that prior studies have reported increased caregiving difficulty among working caregivers (15).
Methods
Study Design
This was a cross-sectional study conducted at 3 academic medical centers (Johns Hopkins Hospital, Massachusetts General Hospital, and Thomas Jefferson University Hospital) from January 2019 to January 2020. The study was approved by the institutional review boards of all 3 institutions. The reporting of the study design and results were performed in concordance with the Checklist for Reporting of Survey Studies (see Supplementary Material, available online) (16). Caregivers were defined as persons aged older than18 years who accompanied a patient with pancreatic or periampullary cancer who had undergone surgical resection to their postoperative visit. Patients were identified from clinic appointment schedules at their 1-month postoperative clinic visit and were screened for eligibility the week before their postoperative visit by the clinics’ charge nurse. Eligible patients were met by research staff before their scheduled appointment to be introduced to the study and its procedures and invited to participate. The patients’ primary caregiver was identified and recruited upon the agreement of the patient. Informed consent was obtained from both the patient and caregiver. The caregiver was then given an iPad device to complete the survey on a REDCap platform in a private room separate from the patient (17). Caregivers were also offered the option of completing an online version of the survey at a later time at their convenience. The treating physician was not informed of the patients’ participation or lack thereof unless the patient chose to share that information. The study excluded caregivers of patients who remained in the hospital beyond the first 30 days postoperatively, who therefore could not attend clinic for follow-up (n = 39).
Instrument and Data Sources
An instrument was developed that included measures of caregiver demographics, caregiving circumstances, and experiences that drew heavily on widely tested and validated measures of caregiver experiences from the National Study of Caregiving (18-20). The Work Productivity and Activity Impairment Questionnaire for Informal Caregivers of Chronically Ill Older Patients—an instrument that assesses the caregiver’s working status and provides a quantitative estimate of absenteeism, presenteeism, and overall work productivity loss—was also used (21). Paid work status was assessed by determining if the caregiver worked for pay in the last week. Absenteeism denotes the amount of time caregivers were absent from work because of caregiving-related responsibilities. Presenteeism represents productivity loss while physically at work. Overall work productivity loss is a composite measure that integrates absenteeism and presenteeism. These terms are defined by the following formulas (21,22): absenteeism (%) = hours missed from work/(hours missed from work + hours actually worked) × 100; presenteeism (%) = affected productivity while at work (measured on 1-10 scale) × 100; productivity loss (%) = absenteeism + (% of time worked × presenteeism) × 100. The final collated questionnaire is presented in the Supplementary Material (available online).
Caregivers’ general health was assessed on a visual analogue scale anchored at 0 (poor) and 5 (excellent). Respite care was defined as paid services for patient assistance so that the caregiver could take time off. Paid help was defined as services to perform household chores and personal care. Financial, emotional, and physical difficulty were first assessed as binary yes or no variables. If present, degree of difficulty was assessed on a 1 (a little difficult) to 5 (very difficult) Likert-type scale. Participation restriction was assessed on a 0 (a little) to 10 (a great deal) visual analogue scale and defined as the extent to which caregiving affected the caregivers’ ability to perform their regular daily activities (eg, work around the house, shopping, childcare, exercising, studying)
Patients’ medical record numbers were recorded and linked to their respective institutional National Surgical Quality Improvement Program database to obtain patient-level and postoperative outcome variables. The National Surgical Quality Improvement Program is the most prominent surgical quality improvement effort initiated by the American College of Surgeons (23). The program provides participating hospitals with regular reports on risk-adjusted operative outcomes, allowing for benchmarking against other participating hospitals and identification of areas in need of improvement. For patients’ and caregivers’ race, the “other” category includes patients who do not identify their race as White, African American, African descent, or Black.
Statistical Analysis
All statistical analyses were performed using Intercooled Stata software, version 15.1 (StataCorp, College Station, TX, USA). Categorical variables were expressed in frequency percentages and compared across groups with the χ2 test. Continuous variables were expressed in median and interquartile ranges and compared across groups with the Kruskal-Wallis test. Bivariate analyses were performed between caregivers who reported working for pay and those who did not. Multilevel mixed-effects models were used for the logistic and linear regressions to adjust for potential confounders. Fixed effects were assigned to caregiver-level predictors and random effects to individual hospitals to account for intraclass correlation for patients and caregivers nested within the same hospital. Variables used in the regression models were selected based on their significance on univariate analysis and clinical validity and include caregiver’s age, health status, health literacy, relationship to patient, having children at home, living situation with the patient, and the use of respite care services. Tests of statistical significance are 2-sided, and statistical significance was accepted at a P value less than .05.
Results
In the recruitment phase of approaching patients for study participation, there were no patient refusals. A total of 265 caregivers were approached, of whom 9 caregivers refused participation and 16 did not respond to the survey, resulting in a study cohort of 240 caregivers (response rate of 90.6%). Of the 240 caregivers included in the study, 107 (44.6%) worked for pay.
Caregiver Demographics
The median age of all caregivers was 60 (interquartile range [IQR] = 50.0-68.0) years. Those working for pay were younger than those who did not (53.0 years vs 66.0 years; P < .001). There were no statistically significant differences in sex or race between the working-for-pay and the not working-for-pay groups. The working-for-pay group had higher education attainment (36.4% reporting having a postgraduate or professional degree vs 26.3% in the nonworking group; P = .04). Those working for pay reported better general health than those who did not (74.0 vs 67.0 on a 0-100 scale; P = .001). They were more likely to be the patient’s daughter or son (43.0% vs 12.0% in the nonworking group; P < .001) and more likely to have a child aged younger than 18 years in their household (33.6% vs 12.8% in the nonworking group; P < .001). For the 29.2% of caregivers who did not live with patients, the majority drove motor vehicles (83.0%) and had a median traveling time of 15 minutes (IQR = 5.0-60.0), and there were no differences between working and nonworking groups (Table 1).
Table 1.
Demographics of caregivers of patients with pancreatic cancer who have undergone a pancreatectomy (n = 240)
| Variables | Caregivers not working for pay (n = 133) | Caregivers working for pay (n = 107) | P a |
|---|---|---|---|
| Age, median (IQR), y | 66.0 (58.0-73.0) | 53.0 (44.0-61.0) | <.001 |
| Sex, No. (%) | |||
| Female | 92 (69.2) | 78 (72.9) | .53 |
| Male | 41 (31.8) | 29 (27.1) | |
| Race, No. (%) | >.9 | ||
| African American, African descent, or Black | 12 (9.0) | 10 (9.3) | |
| Otherb | 9 (6.9) | 8 (7.4) | |
| White | 112 (84.2) | 89 (83.2) | |
| Marital status, No. (%) | .08 | ||
| Married | 111 (83.5) | 79 (73.8) | |
| Single, widowed, or divorced | 22 (16.5) | 27 (25.3) | |
| Education attainment, No. (%) | .04 | ||
| High school graduate (grade 12 or GED) or less | 26 (19.6) | 10 (9.3) | |
| Some college or technical or vocational school | 44 (33.1) | 27 (25.2) | |
| College graduate (BS, BA) | 28 (21.1) | 31 (29.0) | |
| Postgraduate or professional degree | 35 (26.3) | 39 (36.4) | |
| Adults aged 18 years or older in the household, median (IQR) | 2.0 (1.0-2.0) | 2.0 (1.0-2.0) | .16 |
| Child aged younger than 18 years in the household, No. (%) | 17 (12.8) | 36 (33.6) | <.001 |
| Hours of caregiving provided per week | 30 (15-70) | 35 (15-60) | .63 |
| Relationship to patient, No. (%) | <.001 | ||
| Spouse | 92 (69.2) | 48 (44.9) | |
| Daughter or son | 16 (12.0) | 46 (43.0) | |
| Other relative | 25 (18.8) | 13 (12.1) | |
| Live with patient, No. (%) | 103 (77.4) | 67 (62.6) | .01 |
| Traveling time, median (IQR), min | 22.5 (5.0-90.0) | 13.5 (5.0-60.0) | .73 |
| Friends and family emotional support, No. (%) | 127 (96.2) | 102 (97.1) | .37 |
| Friends and family caregiving support, No. (%) | 101 (76.5) | 83 (79.0) | .43 |
| Support group participation, No. (%) | 4 (3.0) | 4 (3.8) | .43 |
| Respite care, No. (%) | 10 (7.6) | 18 (17.1) | .05 |
| Paid helper, No. (%) | 14 (10.6) | 12 (11.4) | .66 |
| Log into MyChart/Patient Gateway, No. (%) | 52 (39.1) | 49 (45.8) | .35 |
| Log-in account, No. (%) | .58 | ||
| My own log-in | 4 (8) | 4 (8) | |
| Patients log-in | 48 (92) | 44 (90) | |
| Have discussed personal values, life goals and preferences regarding future medical care, No. (%) | 118 (88.7) | 95 (88.8) | .71 |
Student t test and χ2 tests were used to calculate the P values for continuous and categorical variables respectively, and all tests were performed as 2-sided tests. IQR = interquartile range.
Includes patients who do not identify their race as White, African American, African descent, or Black.
Social Support and Service Use
Caregivers reported high rates of receiving both emotional (96.6%) and caregiving (77.6%) support from friends and family. There were no differences in the receipt of emotional and caregiving support between working-for-pay and nonworking groups. A total of 3.4% of caregivers reported participating in a support group, and 11% used respite care or a paid helper in both groups. Use of respite care was higher for working-for-pay caregivers vs nonworking caregivers (17.1% vs 7.6%; P = .05). A total of 42.1% of caregivers reported using the MyChart/Patient Gateway electronic medical record portal, and 91.1% of these used the patient’s log-in (Table 1).
Patient Demographics
The median age (63.8 years) of patients cared for by working-for-pay caregivers was younger than the nonworking group (70.8 years; P = .006). A total of 42.9% of patients were female, whereas 57.1% were male. When assessing patients’ race, 87.1% were White patients, 6.3% were African American patients, and 3.3% were Asian patients. When examining the pathology of the patient’s cancer, 69.2% had pancreatic adenocarcinoma, for which 81.1% underwent a pancreatoduodenectomy. The median length of hospital stay was 6 (IQR = 5.0-9.0) days, and the 30-day readmission rate was 19.8%. A lower proportion of patients in the working-for-pay caregiver group received preoperative chemotherapy (25.7% vs 46.4% in the nonworking group; P = .002), and similar proportions received preoperative radiation (22.8% vs 33.0%; P = .10). There was also a higher proportion of patients in the working-for-pay caregiver group who had a postoperative intra-abdominal abscess (23.4%) when compared with the nonworking group (12.0%; P = .02; Table 2).
Table 2.
Demographic of patients with pancreatic cancer who undergone a pancreatectomy
| Variables | Caregivers not working for pay (n = 133) | Caregivers working for pay (n = 107) | P a |
|---|---|---|---|
| Sex, No. (%) | |||
| Female | 48 (41.4) | 45 (44.6) | .64 |
| Male | 85 (58.6) | 62 (45.4) | |
| Age at time of surgery, median (IQR), y | 70.8 (63.8-75.8) | 63.8 (58.8-73.0) | .006 |
| Race, No. (%) | .88 | ||
| African American, African descent, or Black | 9 (7.8) | 6 (5.9) | |
| Otherb | 23 (17.3) | 13 (12.1) | |
| White | 101 (87.1) | 88 (87.1) | |
| BMI, median (IQR,) kg/m2 | 24.9 (23.8-27.5) | 25.1 (21.3-28.5) | .47 |
| ASA class 3-4, No. (%) | 78 (67.3) | 73 (72.3) | .68 |
| Pathology, No. (%) | .11 | ||
| Pancreatic adenocarcinoma | 93 (69.9) | 73 (68.2) | |
| Pancreatic IPMN | 6 (4.5) | 6 (5.6) | |
| Ampullary adenocarcinoma | 3 (2.3) | 7 (6.5) | |
| Distal cholangiocarcinoma | 1 (0.8) | 5 (4.7) | |
| Duodenal adenocarcinoma | 1 (0.8) | 2 (1.9) | |
| Other | 29 (21.8) | 14 (13.1) | |
| Hospital length of stay, median (IQR) | 6.0 (5.0-9.5) | 6.0 (5.0-8.0) | .93 |
| Hospital discharge to home, No. (%) | 114 (98.3) | 95 (94.1) | .10 |
| 30-day readmission, No. (%) | 18 (15.5) | 25 (24.8) | .09 |
| Unplanned return to OR, No. (%) | 5 (4.4) | 1 (1.0) | .13 |
| Pre-op chemotherapy, No. (%) | 52 (46.4) | 26 (25.7) | .002 |
| Pre-op radiation therapy, No. (%) | 37 (33.0) | 23 (22.8) | .09 |
| Operation, No. (%) | .98 | ||
| Pancreatoduodenectomy | 94 (81.0) | 82 (81.2) | |
| Distal pancreatectomy | 22 (19.0) | 19 (18.8) | |
| Postoperative intraabdominal abscess, No. (%) | 16 (12.0) | 25 (23.4) | .02 |
| Postoperative delayed gastric emptying, No. (%) | 9 (8.0) | 7 (7.0) | .05 |
Student t test and χ2 tests were used to calculate the P values for continuous and categorical variables respectively, and all tests were performed as 2-sided tests. ASA = American Society of Anesthesiologists; BMI = body mass index; IPMN = intraductal papillary mucinous neoplasm; IQR = interquartile range; OR, operating room; POD = postoperative day.
Includes patients who do not identify their race as White, African American, African descent, or Black.
Impact on Caregivers’ Work Productivity
The 107 caregivers who worked for pay reported 40 (IQR = 22.0-44.0) median hours worked per week. Of the 107 working caregivers, 78 (72.2%) were female, and they worked a median of 36 (IQR = 20.0-40.0) hours per week; male caregivers worked 40 (IQR = 30.0-50.0; P = .01 when compared with female caregivers) hours per week. Of working caregivers, 44% reported being absent from their jobs in the preceding month, with both female and male working caregivers similarly missing a median of 40 (IQR = 24.0-72.0) hours throughout the month. Overall, there was a 14.3% loss in work hours because of caregiving-related absenteeism (female working caregivers reporting 15.8%, male working caregivers reporting 13.0%; P = .34). Additionally, 58.9% reported reduced productivity while being physically present at work because of caregiving-related presenteeism (female working caregivers reporting 60.3%, male working caregivers reporting 56.7%; P = .76). When presenteeism was assessed on a 0-100 scale, the median reported difficulty score was 50.0 (female working caregivers reporting 50.0, male working caregivers reporting 25.5; P = .03). Taken together, the overall work productivity loss due to caregiving was 59.7% (IQR = 51.0%-94.8%; female working caregivers reporting 63.0, male working caregivers reporting 43.0; P = .02; Table 3).
Table 3.
Impact of caregiving for patients with pancreatic cancer who have undergone a pancreatectomy on caregivers’ work productivity (n = 107)
| Work productivity metrics | Female (n = 78) | Male (n = 29) | P a |
|---|---|---|---|
| Median hours worked per week | 36 | 40 | .66 |
| Caregivers reporting being absent from work due to caregiving, % | 47.4 | 36.7 | .54 |
| Median work hours missed per week | 40 | 40 | .57 |
| Overall caregiving-related absenteeism, % | 15.8 | 13 | .29 |
| Caregivers reporting increased work difficulty due to caregiving, % | 60.3 | 56.7 | |
| Overall caregiving-related presenteeism, % | 50 | 25.5 | .03 |
| Overall work productivity loss because of caregiving, % | 63 | 43 | .03 |
Student t test and χ2 tests were used to calculate the P values for continuous and categorical variables respectively, and all tests were performed as 2-sided tests.
Caregiving-Related Difficulties and Participation Effects
The prevalence of emotional, financial, and physical difficulty in caregivers was 49.8%, 24.3%, and 15.9%, respectively. Working-for-pay caregivers were statistically significantly more likely to report emotional difficulty when compared with the nonworking group (62.6% vs 39.4%, respectively; P = .02; Table 4). Working-for-pay caregivers were twice as likely to report financial difficulty compared with the nonworking group (35.5% vs 15.2%, respectively; P < .001). Of caregivers in both groups who reported financial difficulty, the working-for-pay group reported a greater degree of financial difficulty on a 1-5 Likert scale. There were no differences in physical difficulty reported by the working-for-pay caregivers (18.7%) and the nonworking group (13.6%; P = .15). When assessing effect on participation on a visual analogue scale of 0-100, working-for-pay caregivers reported higher degrees of participation restrictions (median = 50.0, IQR = 25.0-67.0) compared with the nonworking group (median = 36.0, IQR = 17.0-62.0; P = .04).
Table 4.
Caregiving-related difficulties and participation effects of caring for patients with pancreatic cancer at 1-month after having undergone a pancreatectomya
| Variables | Caregivers not working for pay | Caregivers working for pay | P b |
|---|---|---|---|
| Total No. | 133 | 107 | |
| Financial difficulty, No. (%) | 20 (15.2) | 38 (35.5) | <.001 |
| Financial degree of difficulty, No. (%) | .04 | ||
| Some (1-2) | 7 (35) | 14 (37) | |
| Substantial (3-5) | 13 (65) | 24 (64) | |
| Emotional difficulty | 52 (39.4) | 67 (62.6) | .002 |
| Emotional degree of difficulty, No. (%) | .42 | ||
| Some (1-2) | 21 (40) | 23 (34) | |
| Substantial (3-5) | 31 (60) | 44 (65) | |
| Physical difficulty | 18 (13.6) | 20 (18.7) | .15 |
| Physical degree of difficulty, No. (%) | .53 | ||
| Some (1-2) | 8 (45) | 7 (35) | |
| Substantial (3-5) | 10 (55) | 13 (65) | |
| Caregiving effects on regular activities, median (IQR) | 36.0 (17.0-62.0) | 50.0 (25.0-67.0) | .04 |
Caregiving-related degree of difficulties measured on a Likert scale anchored at 0 (least) and 5 (most). IQR = interquartile range.
Student t test and χ2 tests were used to calculate the P values for continuous and categorical variables respectively, and all tests were performed as 2-sided tests.
In multilevel logistic regression analyses that adjusted for caregiver and patient characteristics and social services used, working for pay was independently associated with financial (odds ratio [OR] = 2.33, 95% confidence interval [CI] = 1.05 to 5.15; P = .04) and emotional (OR = 1.93, 95% CI = 1.04 to 3.57; P = .04) difficulty but not physical (OR = 1.83, 95% CI = 0.73 to 4.61; P = .20) difficulty. Linear regression performed to assess the independent impact of working for pay on participation restrictions demonstrated a statistically significant difference (+1.85, 95% CI = 1.02 to 3.44; P = .048; Figure 1). Notably, the use of respite care was associated with less financial difficulty (OR = 0.21, 95% CI = 0.07 to 0.51; P = .01), better physical outcomes (OR = 0.14, 95% CI = 0.07 to 0.52; P = .01), and less participation restriction (coefficient = −15.85, 95% CI = −27.33 to −4.38; P = .01).
Figure 1.
Forest plot depicting the logistic regression results for the association between working-for-pay and caregiving-related effects. The dotted lines represent the odds ratio base reference of 1; the diamond represents the odds ratio; the downward arrow represents the lower bound of the 95% confidence interval; the upward arrow represents the upper bound of the 95% confidence interval.
Discussion
This study found that 45% of caregivers of patients with pancreatic cancer who underwent a pancreatectomy were working for pay. Caregivers who worked for pay missed a median of 40 hours of work during the first postoperative month and, even when not absent, had a twofold increase in work difficulty. Taken together, there was an overall caregiving-related work productivity loss of close to 80%. Working caregivers experienced more financial and emotional difficulty and higher degrees of participation restrictions than their nonworking counterparts despite caring for younger patients, with greater medical literacy, and higher use of respite care. To our knowledge, this is the first assessment of the impact of caring for patients with resected pancreatic cancer on caregivers. The results have important implications on how health systems can better deliver patient- and caregiver-centric care.
Presently, little is known about the impact of caregiving for patients with solid organ tumors who have high rates of cancer- and procedure-related morbidity and mortality. Treating pancreatic cancer requires resection, which carries a complication rate approaching 40% at even the highest-volume centers (8,10). Providing this care might be expected to affect caregivers because of changes in the patient’s bowel habits, diabetes, and exocrine insufficiency, which require careful assessment and medication management that are well documented in the literature (11,12,14). This study attempts to fill this knowledge gap and provides data on the substantial financial, emotional, and physical burdens associated with caregiving for these patients.
This study also demonstrated that caring for pancreatic cancer patients in the immediate period after pancreatectomy reduced the overall productivity of working caregivers by 60% in the month following the operation. This substantial impact is likely because of the acuity of the postoperative recovery following a morbid operation; it is more than twofold higher than the impact experienced by caregivers caring for elders with chronic diseases (21), adolescents with cystic fibrosis (24), patients with β-thalassemia (25), and advanced cancer on systemic therapy (26,27). The added burden on productivity observed in the postoperative setting more closely mirrors the impact observed in caregivers of patients after experiencing traumatic orthopedic injury (57% reporting workplace interference) (28). Although this is evidence that patients who experience physical injury either secondary to an operation or trauma are associated with added detriment to caregivers’ work performances, more research is needed to better understand how to address the needs of working caregivers in the context of serious illness.
This study’s findings also speak to the importance of policies to support family and other unpaid caregivers who work, such as the federal Family and Medical Leave Act. The Pew Research Center reported that 1 in 6 US workers in 2016 needed to take medical leave, but more than 70% were unable to do so because of not being able to afford lost salary (29). Presently, only 9 states in the United States have paid family leave laws, and an estimated 13% of workers have access to paid family leave (30). Moreover, one study found that among those who were eligible, only 55% used the benefit, largely out of fear of penalties to their career growth (31). As many as 1 in 3 caregivers caring for cancer survivors have been reported to experience the phenomenon of “job lock” (staying at one’s job to maintain employment-based health insurance) that negatively impacts career trajectory and well-being (32). The substantially reduced work productivity found in our study, along with the employer cost associated with talent lost, staff turnover, and institutional knowledge loss from caregiving-related employee attrition supports the need for the reform and modernization of Family and Medical Leave Act policies that will benefit workers and employers.
This study also sheds light on potential individual-level strategies that could mitigate caregiver difficulties. In this study, 42% of caregivers reported utilizing online patient portals, and 92% did not have their own log-in to the electronic medical record. This finding suggests a potential role for video- and multimedia-based interventions to better prepare patients and caregivers for pancreatic surgery (33–36). Although respite care for caregivers is associated with less financial and physical difficulties as well as participation restriction, only 11.8% of our respondents used such services, which may be because of a lack of awareness of the service. Better information and education on postpancreatectomy expectations and patient care needs are needed; the caregiving-related difficulties demonstrated in this study could be secondary to caregivers’ lack of access to information about patients’ health and treatment plans as demonstrated in the literature (37–39).
The results should be interpreted within the context of its study design. The 3 institutions participating in this study are high-volume, tertiary referral centers for patients with pancreatic cancer. The study’s findings may reflect a more affluent patient population and may have underestimated the burden of caregiving. Similarly, our study population represents predominantly White caregivers, highlighting the need for future study of the perspective of underrepresented racial minorities who may have different degrees of caregiving burden and perspectives. The survey also assesses work-for-pay status by determining if caregivers did so in the preceding 1 week. There is a possibility that caregivers may have stopped working more than a week before the administration of the survey and been misclassified. Our findings would then represent an underestimate of the true impact of caregiving on working caregivers. Additionally, this misclassification of working caregivers in the nonworking group could explain the findings that they have less financial difficulty when compared with the working group, as those who can afford leave would be less stressed. Caregivers’ perspectives may also be influenced by whether patients experienced postoperative complications or had a difficult physical recovery (40). The study population also represents a surgically resected cohort; it would be important to similarly assess the impact of caring for patients who did not undergo an operation secondary to personal preferences or advanced stage of presentation. Finally, this analysis is a cross-sectional assessment of caregiving burden within a single, early postoperative time frame. As the treatment of pancreatic cancer has moved toward more upfront neoadjuvant chemotherapy and chemoradiation prior to surgical resection, caregiving burden will need to be assessed during these treatment phases in a longitudinal fashion to more accurately capture the caregiver’s experience. This is especially important given that patients often struggle with chemotherapy- and radiation-related toxicities, as well as biliary stent–related complications (41,42).
In conclusion, in this prospective multisite trial, almost half of caregivers of patients with pancreatic cancer who had undergone pancreatectomy were working for pay. These caregivers experienced statistically significantly more financial and emotional difficulties, as well as participation restrictions when compared with caregivers who were not working for pay. Working caregivers reported substantial work absenteeism, and even when they were at work, they had more difficulties on the job and reported lost productivity because of their caregiving role. This study supports the need for policies to support cancer caregivers, such as family leave policies to support unpaid cancer caregiving. It also identifies potential interventions at the patient- and caregiver-level that could alleviate difficulties associated with caregiving.
Funding
This work was supported by the National Cancer Institute of the National Institute of Health under the award number: F32CA217455 and the Andrew L Warshaw, MD Institute for Pancreatic Cancer Research Grant under award number: 0004852948.
Notes
Role of the funder: The funders had no role in the conduct of the research.
Disclosures: The authors have no disclosures.
Author contributions: Conceptualization: ZF, MJW, JLW, AWW. Data curation: ZF, JT, DR, TPY. Formal Analysis: ZF, DCC, JLW, TPY. Funding acquisition: ZVF, DCC, MJW, CLW, CFC, JLW, AWW, TPY. Investigation: ZF, HL, CJY, TPY, CLW, KDL, FMJ, JBG, JLW, AWW. Methodology: ZF, JT, MJW, HL, MQ, FMJ, CRF, DCC, CJY, CLW, ALW, KDL, CFC, JLW, AWW, TPY. Project administration: ZF, JT, DR. Resources: ALW, CLW, MJW, CFC, KDL. Software: ZF, DCC, JT, MJW, CLW. Supervision: MJW, HL, MQ, CRF, CLW, ALW, KDL, CFC, JLW, AWW, TPY. Validation: MJW, HL, MQ, CRF, CLW, ALW, KDL, CFC, JLW, AWW, TPY. Visualization: ZF, JLW, AWW, TPY. Writing—original draft: ZF. Writing—review & editing: JT, MJW, HL, MQ, FMJ, CRF, DCC, CJY, CLW, ALW, KDL, CFC, JLW, AWW, TPY.
Prior presentations: Parts of this work were presented as an oral presentation at the 2021 Americas Hepato-Pancreato-Biliary Association Annual Meeting, August 2-5, 2021, Miami, FL.
Supplementary Material
Contributor Information
Zhi Ven Fong, Department of Surgery, Massachusetts General Hospital, Boston, MA, USA.
Jonathan Teinor, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, USA.
Theresa P Yeo, Department of Surgery, Thomas Jefferson University, Philadelphia, PA, USA.
Dee Rinaldi, Department of Surgery, Thomas Jefferson University, Philadelphia, PA, USA.
Jonathan B Greer, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Harish Lavu, Department of Surgery, Thomas Jefferson University, Philadelphia, PA, USA.
Motaz Qadan, Department of Surgery, Massachusetts General Hospital, Boston, MA, USA.
Fabian M Johnston, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
Cristina R Ferrone, Department of Surgery, Massachusetts General Hospital, Boston, MA, USA.
David C Chang, Department of Surgery, Massachusetts General Hospital, Boston, MA, USA.
Charles J Yeo, Department of Surgery, Thomas Jefferson University, Philadelphia, PA, USA.
Christopher L Wolfgang, Department of Surgery, New York University, New York, NY, USA.
Andrew L Warshaw, Department of Surgery, Massachusetts General Hospital, Boston, MA, USA.
Keith D Lillemoe, Department of Surgery, Massachusetts General Hospital, Boston, MA, USA.
Carlos Fernandez-del Castillo, Department of Surgery, Massachusetts General Hospital, Boston, MA, USA.
Matthew J Weiss, Department of Surgery, Northwell Health University Hospital, Manhasset, NY, USA.
Jennifer L Wolff, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA; Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
Albert W Wu, Department of Surgery, Johns Hopkins University School of Medicine, Baltimore, MD, USA; Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
Data Availability
The raw data were generated at Massachusetts General Hospital. Derived, deidentified data supporting the findings of this study are available on the data sharing platform, Open Science Framework, at the following link: https://osf.io/7bame/?view_only=d5815e8d31284d638aa3de738dc41f68.
References
- 1. Wolff JL, Feder J, Schulz R.. Supporting family caregivers of older Americans. N Engl J Med. 2016;375(26):2513-2515. [DOI] [PubMed] [Google Scholar]
- 2. Coe NB, Werner RM.. Informal caregivers provide considerable front-line support in residential care facilities and nursing homes. Health Aff (Millwood). 2022;41(1):105-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. National Academy of Medicine. Families caring for an aging America. https://nam.edu/families-caring-for-an-aging-america/. Published 2016. Accessed July 20, 2021.
- 4. Wolff JL, Spillman BC, Freedman VA, et al. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med. 2016;176(3):372-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021. CA A Cancer J Clin. 2021;71(1):7-33. [DOI] [PubMed] [Google Scholar]
- 6. Yeo TP, Fogg RW, Shimada A, et al. The imperative of assessing quality of life in patients presenting to a pancreaticobiliary surgery clinic. Ann Surg. 2021. doi: 10.1097/sla.0000000000005049. [DOI] [PubMed] [Google Scholar]
- 7. Fong ZV, Lim P-W, Hendrix R, et al. Patient and caregiver considerations and priorities when selecting hospitals for complex cancer care. Ann Surg Oncol. 2021;28(8):4183-4192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fernández-del Castillo C, Morales-Oyarvide V, McGrath D, et al. Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery. 2012;152(3 suppl 1):S56-S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fong ZV, Ferrone CR, Thayer SP, et al. Understanding hospital readmissions after pancreaticoduodenectomy: can we prevent them?: a 10-year contemporary experience with 1,173 patients at the Massachusetts General Hospital. J Gastrointest Surg. 2014;18(1):137-144. discussion 144-145. [DOI] [PubMed] [Google Scholar]
- 10. Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: a single-institution experience. J Gastrointest Surg. 2006;10(9):1199-1210. discussion 1210-1211. [DOI] [PubMed] [Google Scholar]
- 11. Allen CJ, Yakoub D, Macedo FI, et al. Long-term quality of life and gastrointestinal functional outcomes after pancreaticoduodenectomy. Ann Surg. 2018;268(4):657-664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fong ZV, Alvino DM, Castillo CF-D, et al. Health-related quality of life and functional outcomes in 5-year survivors after pancreaticoduodenectomy. Ann Surg. 2017;266(4):685-692. [DOI] [PubMed] [Google Scholar]
- 13. Fong ZV, Sekigami Y, Qadan M, et al. Assessment of the long-term impact of pancreatoduodenectomy on health-related quality of life using the EORTC QLQ-PAN26 module. Ann Surg Oncol. 2021;28(8):4216-4224. [DOI] [PubMed] [Google Scholar]
- 14. Lim P-W, Dinh KH, Sullivan M, et al. Thirty-day outcomes underestimate endocrine and exocrine insufficiency after pancreatic resection. HPB (Oxford). 2016;18(4):360-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ko JY, Aycock DM, Clark PC.. A comparison of working versus nonworking family caregivers of stroke survivors. J Neurosci Nurs. 2007;39(4):217-225. [DOI] [PubMed] [Google Scholar]
- 16. Sharma A, Minh Duc NT, Luu Lam Thang T, et al. A consensus-based checklist for reporting of survey studies (CROSS). J Gen Intern Med. 2021;36(10):3179-3187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Health and Aging Trends Study. National Study of Caregiving (NSOC). https://www.nhats.org/researcher/nsoc. Accessed July 20, 2021.
- 19. Freedman VA, Kasper JD, Cornman JC, et al. Validation of new measures of disability and functioning in the National Health and Aging Trends Study. J Gerontol A Biol Sci Med Sci. 2011;66(9):1013-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Freedman VA, Agree EM, Cornman JC, et al. Reliability and validity of self-care and mobility accommodations measures in the National Health and Aging Trends Study. Gerontologist. 2014;54(6):944-951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Giovannetti ER, Wolff JL, Frick KD, et al. Construct validity of the Work Productivity and Activity Impairment questionnaire across informal caregivers of chronically ill older patients. Value Health. 2009;12(6):1011-1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wolff JL. Calculating Work Productivity Loss in the National Study of Caregiving. National Health and Aging Trends Study (NHATS) Technical Paper. https://www.nhats.org/sites/default/files/2021-01/Work_Productivity_Loss_in_NSOC_Technical_Paper_Aug2019_1.pdf. Updated August 27, 2019. Accessed April 27, 2022.
- 23. American College of Surgeons. National Surgical Quality Improvement Program. https://www.facs.org/quality-programs/acs-nsqip. Accessed July 20, 2021.
- 24. Neri L, Lucidi V, Catastini P, et al. ; for the LINFA Study Group. Caregiver burden and vocational participation among parents of adolescents with CF. Pediatr Pulmonol. 2016;51(3):243-252. [DOI] [PubMed] [Google Scholar]
- 25. Shah F, Telfer P, Velangi M, et al. Routine management, healthcare resource use and patient and career‐reported outcomes of patients with transfusion‐dependent β‐thalassaemia in the United Kingdom: a mixed methods observational study. eJHaem. 2021;2(4):738-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mazanec SR, Daly BJ, Douglas SL, et al. Work productivity and health of informal caregivers of persons with advanced cancer. Res Nurs Health. 2011;34(6):483-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Xiao H, Bertwistle D, Khela K, et al. Patient and caregiver socioeconomic burden of first-line systemic therapy for advanced gastroesophageal adenocarcinoma. Future Oncol. 2022. doi: 10.2217/fon-2021-1449. [DOI] [PubMed] [Google Scholar]
- 28. Ziran BH, Barrette-Grischow M-K, Hull T.. Hidden burdens of orthopedic injury care: the lost providers. J Trauma. 2009;66(2):536-549. [DOI] [PubMed] [Google Scholar]
- 29. Horowitz JM. Americans Widely Support Paid Family and Medical Leave. Pew Research Center; 2017. https://www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/. Accessed July 26, 2021.
- 30.US Bureau of Labor Statistics. Employee Benefits Survey. https://www.bls.gov/ncs/ebs/benefits/2017/. Published 2018. Accessed July 26, 2021.
- 31.Fuller JB, M Raman. The Caring Company: how employers can cut cost and boost productivity by helping employees manage caregiving needs. Harvard Business School; 2019. https://www.hbs.edu/managing-the-future-of-work/research/Pages/the-caring-company.aspx. Accessed July 26, 2021.
- 32. Kent EE, de Moor JS, Zhao J, et al. Staying at one’s job to maintain employer-based health insurance among cancer survivors and their spouses/partners. JAMA Oncol. 2020;6(6):929-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Steves SL, Scafide KN.. Multimedia in preoperative patient education for adults undergoing cancer surgery: a systematic review. Eur J Oncol Nurs. 2021;52:101981. [DOI] [PubMed] [Google Scholar]
- 34. Sun V, Raz DJ, Ruel N, et al. A multimedia self-management intervention to prepare cancer patients and family caregivers for lung surgery and postoperative recovery. Clin Lung Cancer. 2017;18(3):e151-e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Sun V, Raz DJ, Erhunmwunsee L, et al. Improving family caregiver and patient outcomes in lung cancer surgery: study protocol for a randomized trial of the multimedia self-management (MSM) intervention. Contemp Clin Trials. 2019;83:88-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. O’Connor K, La Bruno D, Rudderow J, et al. Preparedness for surgery: analyzing a quality improvement project in a population of patients undergoing hepato-pancreatico-biliary surgery. Clin J Oncol Nurs. 2020;24(5):E65-E70. [DOI] [PubMed] [Google Scholar]
- 37. Zulman DM, Piette JD, Jenchura EC, et al. Facilitating out-of-home caregiving through health information technology: survey of informal caregivers’ current practices, interests, and perceived barriers. J Med Internet Res. 2013;15(7):e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Swan BA. A nurse learns firsthand that you may fend for yourself after a hospital stay. Health Aff (Millwood). 2012;31(11):2579-2582. [DOI] [PubMed] [Google Scholar]
- 39. Sarkar U, Bates DW.. Care partners and online patient portals. JAMA. 2014;311(4):357-358. [DOI] [PubMed] [Google Scholar]
- 40. Hue JJ, Ocuin LM, Kyasaram RK, et al. Weight tracking as a novel prognostic marker after pancreatectomy. Ann Surg Oncol. 2022;29(6):3450-3459. [DOI] [PubMed] [Google Scholar]
- 41. Kirkpatrick S, Gillies G, Underwood P, et al. Biliary intervention rates during neoadjuvant therapy for adenocarcinoma of the pancreatic head. HPB (Oxford). 2021;23(8):1196-1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Murphy JE, Wo JY, Ryan DP, et al. Total neoadjuvant therapy with FOLFIRINOX in combination with losartan followed by chemoradiotherapy for locally advanced pancreatic cancer: a phase 2 clinical trial. JAMA Oncol. 2019;5(7):1020-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data were generated at Massachusetts General Hospital. Derived, deidentified data supporting the findings of this study are available on the data sharing platform, Open Science Framework, at the following link: https://osf.io/7bame/?view_only=d5815e8d31284d638aa3de738dc41f68.