Abstract
Context:
Sedentary time spent with screen media is associated with obesity among children and adults. Obesity has potentially serious health consequences, such as heart disease and diabetes. This Community Guide systematic review examined the effectiveness and economic efficiency of behavioral interventions aimed at reducing recreational (i.e., neither school- nor work-related) sedentary screen time, as measured by screen time, physical activity, diet, and weight-related outcomes.
Evidence acquisition:
For this review, an earlier (“original”) review (search period, 1966 through July 2007) was combined with updated evidence (search period, April 2007 through June 2013) to assess effectiveness of behavioral interventions aimed at reducing recreational sedentary screen time. Existing Community Guide systematic review methods were used. Analyses were conducted in 2013–2014.
Evidence synthesis:
The review included 49 studies. Two types of behavioral interventions were evaluated that either (1) focus on reducing recreational sedentary screen time only (12 studies); or (2) focus equally on reducing recreational sedentary screen time and improving physical activity or diet (37 studies). Most studies targeted children aged ≤13 years. Children’s composite screen time (TV viewing plus other forms of recreational sedentary screen time) decreased 26.4 (interquartile interval= −74.4, −12.0) minutes/day and obesity prevalence decreased 2.3 (interquartile interval= −4.5, −1.2) percentage points versus a comparison group. Improvements in physical activity and diet were reported. Three study arms among adults found composite screen time decreased by 130.2 minutes/day.
Conclusions:
Among children, these interventions demonstrated reduced screen time, increased physical activity, and improved diet- and weight-related outcomes. More research is needed among adolescents and adults.
Context
Obesity prevalence in the U.S. has nearly tripled among children and adolescents over the past 3 decades, with obesity affecting approximately 17% of all U.S. children and adolescents, and more than one third of U.S. adults.1 Obese children are more likely to have risk factors associated with cardiovascular disease2 and Type 2 diabetes,3 and are more likely to become obese adults.4,5 Among adults, obesity is associated with increased risk of heart disease, stroke, some cancers, diabetes, and liver disease.6,7 Healthy People 2020 identifies obesity as a leading health indicator and calls for a reduction in obesity prevalence.8
Longitudinal studies have shown that sedentary screen time, especially TV viewing, increases the risk of children being overweight and obese.9,10 Although cross-sectional studies suggest the relationship may be of little clinical significance during childhood,11 childhood screen time is a risk factor for adult obesity.12 Increased TV viewing among adults is positively associated with overweight and obesity,13,14 cardiovascular disease, Type 2 diabetes, and all-cause mortality.15 In this review, sedentary screen time is defined as recreational (i.e., neither school- nor work-related) time spent with screens, such as TVs, non-active video games, or computers. Several mechanisms by which sedentary screen time may contribute to obesity are hypothesized: displaced physical activity, increased consumption of calories while engaging in screen time, increased exposure to advertisements promoting unhealthy foods, and disturbed sleep patterns.16
The American Academy of Pediatrics recommends no TV or other screen-based entertainment for children aged <2 years, and <2 hours/day with entertainment media for children aged ≥2 years.17 Despite these recommendations, in 2009, U.S. children aged 8–18 years reported 7.2 hours with screen media (4.5 hours watching TV, 1.5 hours using the computer recreationally, and 1.2 hours playing video games); this does not include screen media for school work or cell phone use.18 Although there are no recommendations for adults, in 2013, watching TV was the leisure activity that occupied the most time for adults, about half of their leisure time, or 2.8 hours of TV daily.19
The Guide to Community Preventive Services (Community Guide) serves as a respected source of information about effective community approaches and interventions to address many public health issues, including obesity prevention and control.20 An earlier Community Guide evidence review (“original review”) under the topic of obesity prevention and control found that behavioral interventions aimed at reducing recreational screen time led to a reduction in measured screen time and improvement in weight-related outcomes in children and adolescents; however, the systematic review of published evidence regarding the economics of the intervention only identified two papers.21 The present Community Guide review updates the original evidence and economic reviews by searching for more recent evidence to examine the effectiveness and economic efficiency of behavioral interventions aimed at reducing recreational (i.e., neither school- nor work-related) sedentary screen time, as assessed by screen time, physical activity, diet, and weight-related outcomes.
Evidence Acquisition
Detailed systematic review methods used by the Community Guide are published elsewhere.22,23 The obesity team included subject matter experts in obesity, physical activity, nutrition, and economics from various agencies and institutions together with systematic reviewers from the Community Guide Branch at CDC. The obesity team worked under the oversight of the independent, nonfederal, unpaid Community Preventive Services Task Force. The conceptual approach and methods specific to this systematic review, including intervention selection and outcome determination, are described.
Conceptual Approach and Analytic Framework
Conceptual approach.
The team defined behavioral interventions that aim to reduce recreational (i.e., neither school- nor work-related) sedentary screen time as interventions that teach behavioral self-management skills to initiate or maintain behavior change.
In this review, behavioral screen time interventions were classified into two types: (1) screen-time-only interventions only focus on reducing recreational sedentary screen time; and (2) screen-time-plus interventions focus on reducing recreational sedentary screen time and increasing physical activity or improving diet.
Screen-time-only and screen-time-plus interventions teach behavioral self-management skills through one or more of the following components:
classroom-based education;
tracking and monitoring;
coaching or counseling sessions; or
family-based or peer social support.
Interventions may include one or more additional components: use of an electronic monitoring device to limit screen time (allows users to set time limits for TV, DVD, computer, or video game use), TV Turnoff Challenge (campaign to turn off TV for a specified number of days), screen time contingent on physical activity, or education through mass or small media (e.g., news-letters, brochures, or billboards).
Screen-time-only and screen-time-plus interventions were stratified by intensity. Intensity was based on the presence of an electronic monitoring device to limit screen time and the number of interactions. Interactions could be in person, by phone, or computer-tailored. Personal interactions were conducted by the researcher or other trained professional implementing the intervention. Computer-tailored interactions consisted of computer-generated feedback based on individual input. High-intensity interventions included an electronic monitoring device or at least three interactions. Low-intensity interventions included no more than two interactions.
Analytic framework.
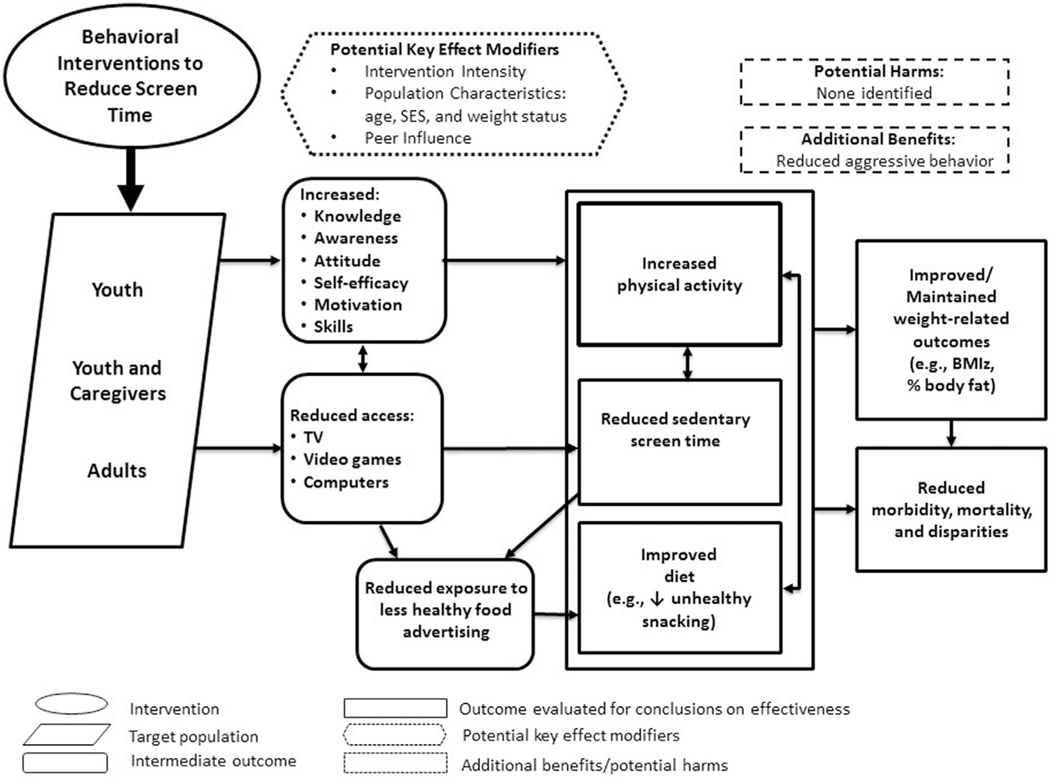
The analytic framework for this review is shown in Figure 1. Behavioral interventions aimed at reducing recreational sedentary screen time may work by changing youth or caregivers’ screen time-related knowledge, awareness, attitudes, motivation, or skills. These interventions might also reduce screen time by changing access to TV, video games, and computers. This approach suggests that reducing screen time may reduce exposure to less-healthful food advertising or reduce snacking during screen time, resulting in an improved diet. In addition, reduced sedentary screen time may increase physical activity and improve diet, which could influence weight-related outcomes. Because of the relationships between screen time, diet, physical activity, and weight, all of these outcomes were considered primary outcomes of interest.
Figure 1.
Analytic framework: hypothesized ways in which reducing screen time can improve diet and activity outcomes.
Search for Evidence
Two searches were conducted, covering the period from 1966 to June 2013 (original review, 1966 through July 2007; updated review, April 2007 through June 2013). The overlap in search periods was to account for delays in database cataloging. Electronic searches were conducted in MEDLINE, CINAHL, EMBASE, PsycINFO, and Cochrane Library databases, which included journal articles, books, and dissertations. Also reviewed were reference lists in retrieved articles. The search combined terms related to recreational screen time (e.g., TV, video games) and weight, physical activity, and diet outcomes. The search terms are available on The Community Guide website (www.thecommunityguide.org/obesity/supportingmaterials/SSscreentime.html).
Inclusion and Exclusion Criteria
Studies were included if they were:
behavioral interventions focused on reducing recreational sedentary screen time;
published in English;
conducted in high- or medium-income nations as classified by The World Bank24;
primary research published in a peer-reviewed journal, technical report, or government report;
primary investigations of interventions rather than guidelines or reviews; or
reporting outcome data on recreational screen time, weight, physical activity, or diet.
Studies were excluded if:
reducing screen time was a minor component (i.e., intervention was primarily directed at physical activity or diet, but mentioned screen time); or
they focused on active video gaming (i.e., interactive video or electronic games that feature player movement, such as would occur in “real-life” exercise participation),25 reducing computer use for school or work, or reducing violent behavior.
Data Abstraction and Quality Assessment
Data from included studies were abstracted and assessed for study design suitability and quality of execution by two reviewers independently. Abstraction and assessment of potential threats to validity were conducted using standardized abstraction forms for Community Guide reviews.23 Discrepancies between reviewers were resolved through discussion. Quality of execution was rated as good (zero to one limitation), fair (two to four), or limited (five or more).22 Limitations were counted in the following nine categories:
description of the study population and intervention;
sampling;
measurement of exposure;
measurement of outcome and independent variables;
confounding bias;
data analysis;
participation;
comparability and bias; and
other biases.23
Studies with good or fair quality of execution, and any level of design suitability, were included in the body of evidence. Analyses were conducted in 2013–2014.
Primary Outcomes of Interest
The primary outcomes of interest for this review were:
screen time behavior assessed by commercial TV viewing and composite screen time (the sum of TV viewing plus at least one other form of screen time, such as sedentary video game playing [sedentary video games are traditional, seated video games] or recreational computer use);
physical activity behavior assessed by accelerometer, pedometer, or self-reported duration;
dietary behavior assessed by intake of total energy, snacks, sugar-sweetened beverages, fruit and vegetables, and meals or snacks with the TV on;
weight-related outcomes assessed by BMI, BMI z-score, body fat percentage; and
This body of evidence includes objective measures, such as accelerometer and height/weight data, and self-reported measures, such as dietary consumption and TV viewing.
Calculation of Effect Estimates for Qualifying Studies
When the adjusted change for an outcome was reported, it was used. When the adjusted change was not provided, effect estimates were calculated. The formula for calculating effect estimates was carried out using three methods, depending on study design and variability of the outcome. The preferred method of calculating effect estimates included a nontreated comparison (C) and intervention (I) study arm, the basic unit for the calculation, with measurements made before and after the intervention. For studies with multiple intervention arms meeting inclusion criteria and a single nontreated comparison arm, effect estimates were calculated using the same comparison arm. For studies with a comparison group, the obesity team used the following formula:
where is the post-test for the arm of participants receiving the intervention (i.e., for the time point closest to the conclusion of the intervention), is the pretest for the arm receiving the intervention, is the post-test for the comparison arm, and is the pretest for the comparison arm.
When studies did not include a comparison arm or included a comparison arm that received an intervention meeting inclusion criteria, the obesity team assumed that in the absence of an intervention, no change would have occurred, that is, ; and the following formula was used:
In addition, when studies used various measures to assess the same outcome, relative percentage change was calculated using the following formula:
For each primary outcome measure, the median of effect estimates from individual studies with the interquartile interval (IQI), which is the interval between the first and third quartiles, was reported.
Economic Review
General methods followed by The Community Guide for the systematic review of economic evidence are available at www.thecommunityguide.org/about/economics.html. Estimates of cost and economic benefit were abstracted from studies meeting the intervention definition and criteria for inclusion. Estimates were then converted to per-capita terms denominated in 2013 U.S. dollars. Determinations were made from the evidence whether the intervention was cost effective (i.e., cost per quality-adjusted life-year [QALY] saved <$50,000)29 or cost beneficial (i.e., economic benefit was greater than intervention cost).
Evidence Synthesis
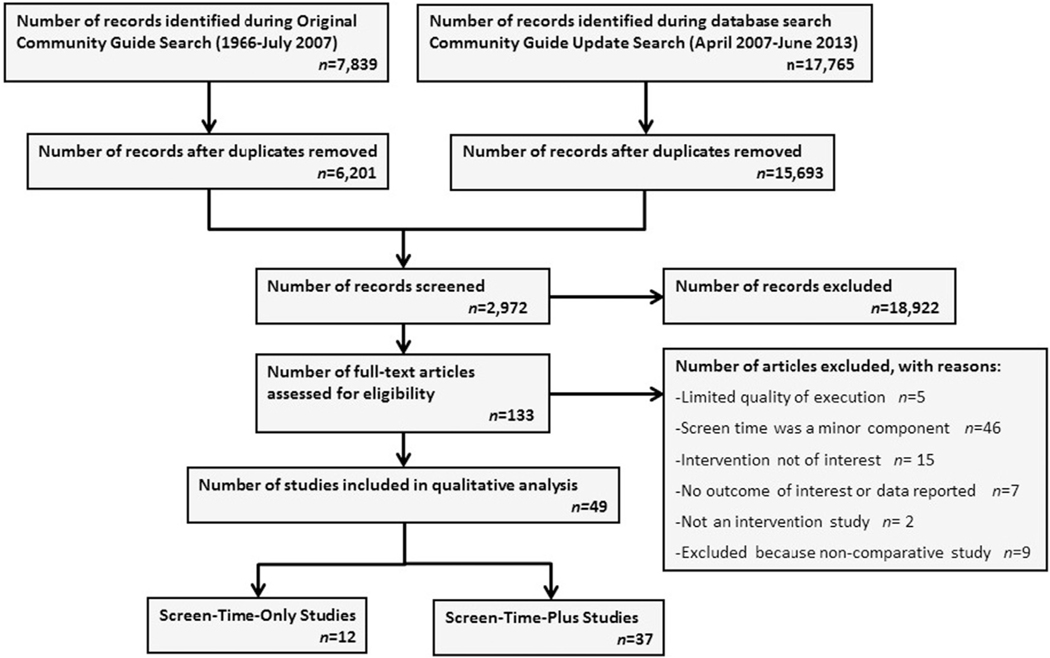
Figure 2 summarizes the search process. The original search (1966 through July 2007) identified 7,839 records. The updated search for evidence (April 2007 through June 2013) identified 17,765 records. After removing duplicates, the titles of 21,894 records were screened independently. Next, the abstracts of 2,972 potentially relevant records were each screened by two reviewers, leaving 133 potentially relevant articles needing full-text assessment for eligibility; these were screened by two reviewers. Five studies30–34 with limited quality of execution were excluded, leaving seven studies from the original review and 42 studies from the updated search. Of these, 12 studies35–46 were screen-time-only and 37 studies47–83 were screen-time-plus interventions.
Figure 2.
Search process showing number of studies identified, reviewed in full text, reasons for exclusion, and total number of included studies.
Study and Intervention Characteristics
Table 1 displays study characteristics including country, setting, degree of urbanization, and intervention components. Most studies (n=32) took place in the U.S. and 20 took place in schools. Additionally, 25 took place in an urban/suburban setting. Family-based social support (e.g., parents given materials to facilitate reducing their child’s screen time) was the most common intervention component. Lastly, more than half of studies reported theoretic underpinnings, with 14 reporting social cognitive theory.
Table 1.
Location and Intervention Characteristics from Included Studies
| Characteristic | Studies, n (%) |
|---|---|
|
| |
| Country | |
| U.S. | 32 (65.3) 36–40,42–47,49,51–53,55,56,58,59,67,68,70–74,77–80,82,83 |
| Australia | 6 (12.2)44,46,56,63,71,72 |
| United Kingdom | 4 (8.2) 57,58,61,77 |
| Canada | 2 (4.1)35,57 |
| Other | 5 (10.0); 1 study each from France64; the Netherlands54; New Zealand41; Sweden66; and Switzerland69 |
| Setting | |
| School | 20 (40.1)42,43,49,51,54,56,58–61,64–66,69,70,75,76,78,80,81 |
| Home | 12 (24.5)36,39,41,44,46,55,57,60,66,81,83 |
| Community | 5 (10.2)37,40,47,62,82 |
| Primary care clinic | 5 (10.2)31,34,63,64,75 |
| Research institute | 4 (8.2)44,48,49,73 |
| Combination of settings | 4 (8.2) 46,59,67,68 |
| Degree of urbanization | |
| Urban/suburban | 25 (51.0)31–34,37–39,43,50–52,54,55,58,61,63,65,66,68,71,72,75,77–79 |
| Mixed urban to rural | 6 (12.2) 36,42,46,56,57,60 |
| Rural only | 1 (2.0)63 |
| Not reported | 17 (34.7)39,44,45,48,49,51–53,57,66,68,71,73,74,77,78,80 |
| Intervention components | |
| Electronic monitoring device | 14 arms from 13 studies (23.0)a,36,38,39,41–44,46,55,57,71,72,74 |
| TV Turnoff Challenge | 11 arms from 10 studies (18.0)a,42,43,51,59,61,63,71,72,75,76 |
| Screen time contingent on physical activity | 2 arms from 2 studies (3.3)a’53,70 |
| Tracking/monitoring | 24 arms from 18 studies (39.3)a,35,41,43,48–50,53,57,59,61,65,67,68,70–73,79 |
| Peer social support | 7 arms from 6 studies (11.5)a,42,43,47,64,65,78 |
| Family social support | 50 arms from 39 studies (82.0)a,31–41,43–45,47–49,51–54,57–70,73,76–78 |
| Coaching/counseling | 29 arms from 22 studies (47.5)a,35,36,38,40,41,44,45,48,49,52,53,55,62,63,67,68,70,77,79,80,82,83 |
| Environmental | 8 arms from 8 studies (13.1)a,50,55,60,63,66,69,71,72 |
| Classroom-based health education | 24 arms from 21 studies (39.3)a’42,43,49,51,54,56,58–61,63–66,69,70,75,76,78,80,81 |
| Mass or small media | 41 arms from 36 studies (67.2)a,31–36,38–41,44–49,51,52,54,56–68,71,75,77,78 |
| Theoretical underpinningb | |
| Social cognitive theory | 14 studies (28.6)37,38,42,43,45,47,52,55,57–59,65,71,72 |
| Behavioral choice theory | 5 studies (10.2)47,57,59,75,83 |
| Self-determination theory | 3 studies (6.1)61,62,70 |
| Transtheoretical model of behavior change | 3 studies (6.1)45,65,82 |
| Other theory reported | 9 studies (18.4)35,53,54,63,65,68,76,80,81 |
| No theory reported | 21 studies (42 9)36,39–41,44,46,48–51,56,60,64,66,67,69,73,74,77–79 |
Percentage calculated using total number of study arms (N=61) as denominator.
Percentages do not add to 100 because some studies reported more than one theory.
Of the screen-time-only studies, seven studies36,39,42–46 were high-intensity, three studies35,37,40 were low-intensity, and two studies38,41 had both a high- and a low-intensity arm, totaling 14 study arms from 12 studies. Of the screen-time-plus studies, 24 studies49–53,55,57–59,61–63,66,68,69,71–76,79,80,83 (33 study arms) were high-intensity, 11 studies47,48,54,56,60,64,65,67,70,78,82 (12 study arms) were low-intensity, and two studies77,81 had both a high- and a low-intensity arm (five study arms), totaling 37 studies and 50 study arms. Appendix Table 1 (available online) lists the studies and study arms stratified by intervention type and intensity. The median duration of the interventions was 6 (IQI=3.8, 15.0) months. Detailed evidence tables are available at www.thecommunityguide.org/obesity/supportingmaterials/SET-screentime.pdf.
Appendix Figure 1 (available online) displays the quality of execution assessment from included studies. The most common limitations were in sampling (n=18) and description (n=12).
Population Characteristics
Most included studies (n=46) targeted children aged ≤13 years,35–45,47–54,56–82 one55 study targeted the whole family, and two46,83 studies targeted only adults. In general, included studies were balanced across genders and the racial distribution was somewhat similar to that of the U.S. population. Nine studies38,40,49,61,71,72,75,76,82 targeted low-income populations. More specifically, three studies38,71,72 targeted low-income African-American children; two studies40,82 targeted Special Supplemental Nutrition Program for Women, Infants, and Children participants; one study49 targeted Head Start participants; and three studies61,75,76 targeted disadvantaged children. Seven studies36,46,52,53,57,67,79 targeted overweight or obese participants.
Outcomes
Table 2 presents summary effect estimates for children for screen time, physical activity, dietary, and weight-related outcomes, stratified by intervention type and intensity. Screen time and weight-related outcomes are described below. Physical activity and dietary outcomes are described in the Appendix (available online). When available, summary effects for adults are presented in the text.
Table 2.
Selected Outcomes for Children Stratified by Intervention Type and Intensity
| Screen-time-onlya | Screen-time-plusb | Combined | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Outcomes | High intensityc | Low intensityd | High and low intensity combined | High intensity | Low intensity | High and low intensity combined | screen-time- only and screen-time- plus | ||
|
| |||||||||
| Recreational sedentary screen time | |||||||||
| Commercial TV viewing (minutes/day) | |||||||||
| No. of study arms | 6 | 3 | 9 | 13 | 5 | 18 | 27 | ||
| Median change | −46.8 (−210.0, −34.8) | −0.6 (−120.6, 0.0) | −45.6 (−162.6, −15.0) | −13.8 (−52.2, 6.0) | −18.0 (−78.0, 0.0) | −16.2 (−70.8, 3.6) | −22.2 (−76.8, −0.60) | ||
| Composite screen time (minutes/day) | |||||||||
| No. of study arms | 7 | 4 | 11 | 17 | 6 | 23 | 34 | ||
| Median change | −82.2 (−117.6, −67.2) | −51.6 (−116.4, −23.4) | −82.2 (−117.6, −37.2) | −21.6 (−44.4, −10.8) | −19.2 (−28.2, 10.8) | −21.6 (−34.2, −9.0) | −26.4 (−74.4, −12.0) | ||
| Physical activity | |||||||||
| Accelerometer counts (counts/day) | |||||||||
| No. of study arms | NR | NR | NR | 7 | NR | 7 | NA | ||
| Median change | 4 arms: 66.0 (40.8, 115.0) Contingente (3 arms): 130.0 (127.8, 150.0) | 4 arms: 66.0 (40.8, 115.0) Contingente (3 arms): 130.0 (127.8, 150.0) | |||||||
| Pedometer steps (steps/day) | |||||||||
| No. of study arms | 2 | 1 | 3 | 4 | 2 | 6 | 9 | ||
| Median change | 679.0 (298, 1,150) | 992.0 | 992.0 (298, 1,150) | 1,359.5 (−258.0, 4,972.0) | −377.0 (−993.0, 239.0) | 310.0 (−441.8, 2,996.4) | 381 (−9.5, 1,743.9) | ||
| Duration of moderate to vigorous physical activity (minutes/day) | |||||||||
| No. of study arms | 2 | 1 | 3 | 9 | 4 | 13 | 16 | ||
| Median change | 27.6 (−2.4, 30.0) | −70.6 | −2.4 (−70.6, 30.0) | 1.2 (−4.5, 20.2) | 5.1 (−2.5, 15.4) | 4.4 (−3.0, 14.7) | 2.3 (−4.2, 16.7) | ||
| Diet | |||||||||
| Total energy intake (kcal/day) | |||||||||
| No. of study arms | 1 | NR | NR | 5 | NR | NR | 6 | ||
| Median change | −75 | − | − | −117.9 (−373.1, 28.5) | − | − | −121.0 (−268.0, 0.59) | ||
| Snack intake (kcal/day) | |||||||||
| No. of study arms | 1 | 1 | 2 | 1 | NR | NR | 3 | ||
| Median change | −233.7 | −123.7 | −178.7 | −281.9 | − | − | −233.7 | ||
| Sugar-sweetened beverage intake (relative percent change) | |||||||||
| No. of study arms | NR | NR | NR | 8 | 6 | 14 | NA | ||
| Median change | − | − | − | −17.2 (−54.7,’ −9.2) | −1.6 (−40.9, 5.4) | −10.9 (−50.0, 3.5) | − | ||
| Fruit and vegetable intake (servings/day) | |||||||||
| No. of study arms | NR | NR | NR | 9 | 5 | 14 | NA | ||
| Median change | − | − | − | 0.16 (−0.25, 0.43) | 0.5 (−0.85, 1.04) | 0.21 (−0.38, 0.53) | − | ||
| Weight-related outcomes | |||||||||
| BMI (kg/m2) | |||||||||
| No. of study arms | 3 | 1 | 4 | 9 | 2 | 11 | 15 | ||
| Median change | −0.44 (−0.45. −0.04) | −0.09 | −0.27 (−0.45, −0.04) | −0.21 (−0.65, 0.07) | 0.13 (0.10, 0.16) | −0.08 (−0.40, 0.10) | −0.09 (−0.44, −0.04) | ||
| BMI z-score | |||||||||
| No. of study arms | 1 | 1 | 2 | 7 | 5 | 12 | 14 | ||
| Median change | −0.20 | 0.01 | −0.11 | −0.11 (−0.19, 0.02) | −0.20 (−0.34, −0.02) | −0.11 (−0.19, 0.05) | −0.13 (−0.23, −0.01) | ||
| Percent body fat (pet pts) | |||||||||
| No. of study arms | l | NR | NR | 5 | 2 | 7 | 8 | ||
| Median change | −2.54 | — | — | −4.9 (−5.9, | −0.38 (−0.83, | −4.5 (−5.5, | −3.5 (−5.4, | ||
| 2.8) | 0.08) | −0.8) | −0.90) | ||||||
| Morbidity | |||||||||
| Obesity prevalence (pet pts) | |||||||||
| No. of study arms | NR | NR | NR | 9 | 4 | 13 | NA | ||
| Median change | − | − | − | −2.0 (−2.8, −1.1) | −4.6 (−7.6, −1.1) | −2.3 (−4.5, −1.2) | − | ||
Note: All medians are followed by interquartile interval if there are ≥5 study arms, range if there are <5 study arms. Not all studies are represented in the table because of inconsistent outcome measures.
Screen-time-only interventions only focus on reducing recreational sedentary screen time.
Screen-time-plus interventions focus on reducing recreational sedentary screen time and increasing physical activity and/or improving diet.
High-intensity interventions must include use of an electronic monitoring device to limit screen time or at least three personal or computer-tailored interactions.
Low-intensity interventions include two or fewer personal or computer-tailored interactions.
Screen time contingent on physical activity.
NA, not applicable; NR, not reported; pet pts, percentage points.
Screen time.
Forty-nine study arms from 39 studies35–39,41–49,51,54–59,61,63,65,67,69–80,82,83 reported duration of commercial TV viewing or composite screen time among children and adults. Among children, 27 study arms from 19 studies37–39,41–43,45,48,55,67,70,72–77,80,82 reported a median decrease of 22.2 (IQI= −76.8, −0.60) minutes/day of commercial TV viewing. In addition, 34 study arms from 32 studies35–38,42–45,47,49,51,54,56–59,61,63,65,69,71,72,74–76,78,79 reported a median decrease in composite screen time of 26.4 (IQI= −74.4, −12.0) minutes/day (Table 2). Among adults, one study55 reported a median decrease in commercial TV viewing of 33.0 minutes/day. Three study arms (in two studies)46,83 reported a median decrease in composite screen time of 130.2 (range = −142.8, −128.4) minutes/day.
Appendix Figure 2 (available online) displays effect estimates and, when available, 95% CIs, for the absolute change in minutes per day of composite screen time among children. For controlled trials, participants receiving screen time interventions were compared with either no screen time intervention or usual care (e.g., usual classroom lessons). There were 11 screen-time-only study arms with a median baseline composite screen time of 156.0 (IQI=114.0, 201.0) minutes/day and a median decrease of 82.2 (IQI= −105.4, −52.1) minutes/day. Removing pre-post study arms, the median decrease was 69.6 (IQI= −99.6, −27.9) minutes/day. Also, 23 screen-time-plus study arms with a median baseline composite screen time of 162.0 (IQI=144.0, 204.0) minutes/day had a decrease of 21.6 (IQI= −38.4, −12.9) minutes/day. Removing the pre-post study arms, the median decrease was 22.8 (IQI= −29.7, −2.3) minutes/day.
Screen-time-only studies had a greater effect on reducing composite screen time, with high-intensity screen-time-only showing the greatest effect. Studies with electronic monitoring devices, which are electronic devices that connect to a TV, DVD player, or video-game console that set time limits, reported greater reductions than those without devices. Six screen-time-only and five screen-time-plus high-intensity studies with an electronic monitoring device reported median composite screen time reductions of 91.8 (IQI= −125.4, −70.8) minutes/day and 52.8 (IQI= −119.4, −19.2) minutes/day, respectively. In addition, one high-intensity screen-time-only study and 11 high-intensity screen-time-plus study arms (from 12 studies) without an electronic monitoring device reported median reductions of 37.1 minutes/day and 17.4 minutes/day (IQI= −28.2 minutes/day, −4.8 minutes/day), respectively.
Physical activity.
Forty-seven study arms from 35 studies36,38,41,42,44,46–49,52,54–63,65,66,68,69,71–80,83 reported physical activity. Additional information is in the Appendix (available online).
Dietary behaviors.
Forty study arms from 32 studies included dietary behaviors as outcomes among children35–38,40–42,44,47–50,54–59,63,65,66,68,70–72,77,79–82 and adults46,83 and adults. Additional information is in the Appendix (available online).
Weight-related.
Thirty-nine study arms from 33 studies35,36,41,42,44,46–57,61,63–69,71–75,78–80 reported weight-related outcomes. Among children, two screen-time-only35,36 and 12 screen-time-plus study arms from 12 studies 48–51,55,63–67,72,78 reported a median decrease in BMI z-score of −0.13 (IQI= −0.23, −0.01) (Table 2). Body fat percentage was assessed by one screen-time-only44 and seven screen-time-plus study arms from five studies,52,53,65,69,78 which found a median decrease of −3.5 (IQI= −5.4, −0.90) percentage points (pct pts). One screen-time only study40 and three screen-time-plus studies49,67,70 measured fat mass by skin-fold thickness in normal weight samples and reported a median decrease of −1.0 (range= −2.5, −0.44) mm. Among adults, two studies46,55 reported BMI decreases of −0.18 kg/m2 and −0.19 kg/m2.
Obesity Prevalence
No screen-time-only studies reported obesity prevalence. Appendix Figure 3 (available online) displays screen-time-plus effect estimates for absolute pct pt change in obesity prevalence among children. Ten high-intensity screen-time-plus study arms with a median obesity prevalence at baseline of 10.3% (IQI=5.4%, 21.5%) reported a median decrease of 2.1 (IQI= −3.9, −1.1) pct pts. Four low-intensity study arms with a median baseline of 12.3% (range=6.0%, 23.7%) reported a median decrease of 4.6 (range= −7.6, −1.1) pct pts. Combining high- and low-intensity study arms (n=14), the median baseline obesity prevalence was 10.3% and the median decrease was 2.3 (IQI= −17.7, −6.0) pct pts, which is a relative reduction of approximately 20%. For the 14 screen-time-plus study arms that reported obesity prevalence, the median reduction in composite screen time was −23.7 (IQI= −28.2, −13.2) minutes/day, which is similar to the median reduction in composite screen time in all screen-time-only and screen-time-plus studies combined (−26.4 [IQI= −74.4, −12.0] minutes/day), but is less than the screen-time-only studies of −82.2 (IQI= −105.4, −52.1) minutes/day. It was not possible to examine physical activity and dietary results, which may have contributed to this reduction in obesity, because of the variety of outcome measures used.
Economic Evidence
Two economic studies84,85 were identified from the search results for the effectiveness review, and from a separate search (1966 through 2014) within specialized databases (available at www.thecommunityguide.org/obesity/supportingmaterials/SSscreentime.html). Detailed evidence tables are available at www.thecommunityguide.org/obesity/supportingmaterials/SET-screentime.pdf. The two studies targeted children and estimated or modeled the:
intervention cost from quantities of labor and materials identified in the intervention descriptions;
number of cases of adult overweight prevented, because cases of overweight were prevented in childhood;
economic benefits as the difference in cost between the additional healthcare resources consumed by overweight adults compared with normal weight adults; and
improved QALYs lived as the difference between the greater number of QALYs lived by normal weight adults compared with overweight adults.
Both studies modeled a screen-time-plus intervention59 under various parameter values and found it to be cost effective based on a conservative threshold of $50,000 per QALY saved. The second study also modeled a screen-time-only intervention42 and found the intervention not to be cost effective.85
Applicability
Findings from this review are applicable to children aged ≤13 years in the U.S. and other high-income countries. Few studies targeted adults46,83 and none targeted adolescents aged >13 years. Most studies in this review included normal-weight participants and seven studies36,46,52,53,57,67,79 targeted overweight or obese participants. Interventions were found to be effective regardless of weight status. More than half of the studies 35,37–43,45–47,49,51,53,56–59,62,67,68,70–72,77–79,82,83 reported race/ethnicity, and nine studies38,40,49,61,71,72,75,76,82 targeted low-income populations. Studies were found to be effective across race/ethnicity and low-income populations.
Five studies36,40,64,69,79 performed a stratified analysis to examine effectiveness on SES disparities. Four of these studies examined the effectiveness on weight-related outcomes (e.g., BMI, obesity prevalence), of which three showed greater reductions in low-income participants compared with high-income participants. One study,40 conducted in Special Supplemental Nutrition Program for Women, Infants, and Children clinics, reported a greater increase in meeting American Academy of Pediatrics recommendations among children whose parents were non-high school graduates compared to parents who were high school graduates.
Discussion
Summary of Findings
There is strong evidence that screen-time-only and screen-time-plus interventions are effective at reducing recreational sedentary screen time, increasing physical activity, improving diet, and improving or maintaining weight status. These findings are applicable to children aged ≤13 years of various races/ethnicities living in various countries and settings. In addition, evidence shows these interventions may reduce obesity prevalence and disparities in weight status between children of high and low SES.
Evidence Gaps
Although evidence shows that behavioral interventions to reduce recreational sedentary screen time are effective, research gaps remain. Future studies should examine which characteristics (e.g., intensity and duration) and components (e.g., family-based social support, electronic monitoring device) are most effective. In addition, follow-up research should examine how long intervention effects are maintained.
Research is needed among adolescents and adults, and by degree of urbanization. Research among adolescents aged >13 years is needed because time spent with screen media increases as children age18 and adolescents have access to many electronic devices.86 More research among adults is needed because only two studies were found.46,83 Studies should also consider degree of urbanization. Most included studies were implemented in urban or suburban settings, and it remains unknown if similar interventions would be successful in rural settings, where the barriers to physical activity are more frequent (e.g., lack of parks or sidewalks).87
It would also be beneficial to consider other outcomes of reduced screen time, such as improved sleep,88 improved family and peer relationships,89 and substitution of other sedentary behaviors. For example, does a reduction in screen time result in the substitution of other sedentary behaviors (e.g., reading for leisure or listening to music)?
Evidence about the effect of more recent mobile devices such as smartphones and tablets was rarely reported in this body of evidence. It is unknown to what extent these devices are associated with weight status, and whether decreases in their use would be associated with outcomes included in this review. Research on screen time interventions should be broadened to include the use of mobile devices and should report the context and duration for the use of multiple electronic devices.
Lastly, only two studies provided economic data, emphasizing the need for more economic evaluations of these interventions. Studies that model economic outcomes for children need to incorporate averted healthcare costs, improved academic productivity, and increased quality of life during the childhood years.
Limitations
This review had several limitations. First, most of the articles were from peer-reviewed literature; thus, there is a potential publication bias. The team attempted to address this by searching gray literature, but only two dissertations met the inclusion criteria. Second, a formal meta-analysis was not possible, owing to varied study designs and few studies reporting CIs or SEs. Additionally, calculating an effect estimate that included all studies reporting a particular outcome was not possible because of heterogeneous measures. In addition, the team reported the data point closest to the conclusion of the intervention because too few studies reported maintenance. Therefore, review results do not reflect maintenance of outcome. Additionally, much of the screen time, dietary, and physical activity data were self-reported, and warrant cautious interpretation of results. Finally, no screen-time-only studies reported obesity prevalence, resulting in an obesity prevalence effect estimate based solely on screen-time-plus studies.
Conclusions
Since the original Community Guide screen time review, the number of studies on behavioral interventions to reduce sedentary screen time has increased greatly, underscoring the importance of recreational sedentary screen time. The interest might be a result of the link between screen time during childhood and childhood obesity or lowered scores for self-esteem and decreased academic achievement,9 or the link between childhood/adolescent TV viewing and overweight, poor fitness, and elevated cholesterol in adulthood.12
A 2014 review of reviews reported on the effectiveness of reducing time in sedentary behaviors and found results similar to those of this review.90 Half of the studies defined sedentary time as recreational screen time, and all found some level of effectiveness at reducing sedentary behavior. The authors report that interventions targeting children aged <6 years may be more effective because of parental control, and that the more effective interventions included family social support, behavioral interventions, and electronic TV monitors.
Supplementary Material
Acknowledgments
The members of the obesity team for this review were Leigh Ramsey Buchanan, Cherie R. Rooks-Peck, Ramona K. C. Finnie, Holly R. Wethington, Charlotte A. Pratt, Janet E. Fulton, Donna B. Johnson, Leila C. Kahwati, Gilbert Ramirez, Randy Elder, Shawna Mercer, and Karen Glanz. All obesity team members contributed to the conceptualization of the review and interpretation of results.
LRB, CRRP, RKCF, HRW abstracted studies, conducted analyses, and drafted the manuscript. CAP, JEF, DBJ, LCK, GR, and KG provided revisions to draft manuscripts. VJ designed and carried out the economic analysis for this review.
We gratefully acknowledge the contributions of Kate W. Harris, Krista H. Cole, and Onnalee Gomez (all from Community Guide Branch, CDC), who provided input on various stages of the review and the development of the manuscript. We are also indebted to the investigators who created the body of literature we examined for this review.
The work of Cherie R. Rooks-Peck and Ramona K. C. Finnie was supported with funds from the Oak Ridge Institute for Science and Education.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC, or the National Heart, Lung and Blood Institute, NIH.
No financial disclosures were reported by the authors of this paper.
Footnotes
Appendix
Supplementary data
Supplementary data associated with this article can be found at http://dx.doi.org/10.1016/j.amepre.2015.09.030.
Names and affiliations of Task Force members can be found at: www.thecommunityguide.org/about/task-force-members.html.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedman DS, Mei Z, Srinivasan SR, Berenson GS, Dietz WH. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(1):12–17. 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- 3.Rosenbloom AL, Joe JR, Young RS, Winter WE. Emerging epidemic of type 2 diabetes in youth. Diabetes Care. 1999;22(2):345–354. 10.2337/diacare.22.2.345. [DOI] [PubMed] [Google Scholar]
- 4.Biro FM, Wien M. Childhood obesity and adult morbidities. Am J Clin Nutr. 2010;91(5):1499s–1505s. 10.3945/ajcn.2010.28701B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22(2):167–177. 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 6.Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NIH. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Vol No. 98–4083. Bethesda, MD; 1998. [PubMed] [Google Scholar]
- 8.U.S. DHHS, Office of Disease Prevention and Health Promotion. Healthy People 2020. www.healthypeople.gov/2020/default. Accessed April 30, 2014.
- 9.Tremblay MS, LeBlanc AG, Kho ME, et al. Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act. 2011;8:98. 10.1186/1479-5868-8-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kimbro RT, Brooks-Gunn J, McLanahan S. Young children in urban areas: links among neighborhood characteristics, weight status, outdoor play, and television watching. Soc Sci Med. 2011;72(5):668–676. 10.1016/j.socscimed.2010.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marshall S, Biddle S, Gorely T, Cameron N, Murdey I. Relationships between media use, body fatness and physical activity in children and youth: a meta-analysis. Int J Obes. 2004;28:1238–1246. 10.1038/sj.ijo.0802706. [DOI] [PubMed] [Google Scholar]
- 12.Hancox R, Milne B, Poulton R. Association between child and adolescent television viewing and adult health: a longitudinal birth cohort study. Lancet. 2004;364:257–262. 10.1016/S0140-6736(04)16675-0. [DOI] [PubMed] [Google Scholar]
- 13.Shuval K, Gabriel KP, Leonard T. TV viewing and BMI by race/ethnicity and socio-economic status. PLoS One. 2013;8(5):e63579. 10.1371/journal.pone.0063579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults: a systematic review of longitudinal studies, 19962011. Am J Prev Med. 2011;41(2):207–215. 10.1016/j.amepre.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Grontved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305(23):2448–2455. 10.1001/jama.2011.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McKetta S, Rich M. The fault, dear viewer, lies not in the screens, but in ourselves: relationships between screen media and childhood overweight/obesity. Pediatr Clin North Am. 2011;58(6):1493–1508, xii. 10.1016/j.pcl.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 17.American Academy of Pediatrics. Children, adolescents, and television. Pediatrics. 2001;107(2):423–426. 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 18.Rideout V, Foehr U, Roberts D. GENERATION M2: Media in the Lives of 8- to 18-year-olds. Menlo Park, CA: The Henry J. Kaiser Family Foundation, 2010. [Google Scholar]
- 19.U.S. Department of Labor. American time use survey summary. 2014. www.bls.gov/news.release/atus.nr0.htm.
- 20.Guide to Community Preventive Services. Obesity prevention andcontrol. 2015; www.thecommunityguide.org/obesity/index.html.
- 21.Guide to Community Preventive Services. Obesity prevention and control: behavioral interventions to reduce screen time. 2008; www.thecommunityguide.org/obesity/communitysettings_archive.html.
- 22.Briss PA, Zaza S, Pappaioanou M, et al. Developing an evidence-based Guide to Community Preventive Services—methods. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18(1 Suppl):35–43. 10.1016/S0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 23.Zaza S, Wright-De Agüero LK, Briss PA, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Am J Prev Med. 2000;18(1 Suppl):44–74. 10.1016/S0749-3797(99)00122-1. [DOI] [PubMed] [Google Scholar]
- 24.The World Bank. Country and lending groups. 2014; data.worldbank.org/about/country-and-lending-groups.
- 25.Bailey BW, McInnis K. Energy cost of exergaming: a comparison of the energy cost of 6 forms of exergaming. Arch Pediatr Adolesc Med. 2011;165(7):597–602. 10.1001/archpediatrics.2011.15. [DOI] [PubMed] [Google Scholar]
- 26.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243. 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. National Center for Health Statistics. Vital Health Stat. 2002;11(246). [PubMed] [Google Scholar]
- 28.Rolland-Cachera MF, Cole TJ, Sempe M, Tichet J, Rossignol C, Charraud A. Body mass index variations: centiles from birth to 87 years. Eur J Clin Nutr. 1991;45(1):13–21. [PubMed] [Google Scholar]
- 29.Eichler H-G, Kong SX, Gerth WC, Mavros P, Jönsson B. Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost-effectiveness thresholds expected to emerge? Value Health. 2004;7(5):518–528. 10.1111/j.1524-4733.2004.75003.x. [DOI] [PubMed] [Google Scholar]
- 30.Kameswararao AA, Bachu A. Survey of childhood diabetes and impact of school level educational interventions in rural schools in Karimnagar district. Int J Diabetes Dev Ctries. 2009;29(2):69–73. 10.4103/0973-3930.53123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Corriveau NL, Gurm R, Smith CA, et al. Middle school wellness program shows lasting impact for lower income community: a report from project healthy schools. Circulation. 2012;126:A18634. [Google Scholar]
- 32.Pelletier JA. Use of stimulus management techniques to reduce sedentary behaviors of overweight children. All Graduate Theses and Dissertations. Paper 58. digitalcommons.usu.edu/etd/58. [Google Scholar]
- 33.Stahl CE, Necheles JW, Mayefsky JH, Wright LK, Rankin KM. 5–4-3–2-1 go! Coordinating pediatric resident education and community health promotion to address the obesity epidemic in children and youth. Clin Pediatr (Phila). 2011;50(3):215–224. 10.1177/0009922810385106. [DOI] [PubMed] [Google Scholar]
- 34.Ribeiro RQDC. Effectiveness evaluation of a school program for obesity prevention. Oral Presentations from the World Congress of Cardiology Scientific Sessions; 2012 April 1821; Dubai, United Arab Emirates. Circulation. 2012;125(19):e72. [Google Scholar]
- 35.Birken CS, Maguire J, Mekky M, et al. Office-based randomized controlled trial to reduce screen time in preschool children. Pediatrics. 2012;130(6):1110–1115. 10.1542/peds.2011-3088. [DOI] [PubMed] [Google Scholar]
- 36.Epstein LH, Roemmich JN, Robinson JL, et al. A randomized trial ofthe effects of reducing television viewing and computer use on body mass index in young children. Arch Pediatr Adolesc Med. 2008;162(3):239–245. 10.1001/archpediatrics.2007.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Escobar-Chaves SL, Markham CM, Addy RC, Greisinger A, Murray NG, Brehm B. The Fun Families Study: intervention to reduce children’s TV viewing. Obesity (Silver Spring). 2010;18(suppl 1):S99–S101. 10.1038/oby.2009.438. [DOI] [PubMed] [Google Scholar]
- 38.Ford BS, McDonald TE, Owens AS, Robinson TN. Primary care interventions to reduce television viewing in African-American children. Am J Prev Med. 2002;22(2):106–109. 10.1016/S0749-3797(01)00410-X. [DOI] [PubMed] [Google Scholar]
- 39.Gorin A, Raynor H, Chula-Maguire K, Wing R. Decreasing household television time: a pilot study of a combined behavioral and environmental intervention. Behav Intervent. 2006;21(4):273–280. 10.1002/bin.221. [DOI] [Google Scholar]
- 40.Johnson DB, Birkett D, Evens C, Pickering S. Statewide intervention to reduce television viewing in WIC clients and staff. Am J Health Promot. 2005;19(6):418–421. 10.4278/0890-1171-19.6.418. [DOI] [PubMed] [Google Scholar]
- 41.Ni Mhurchu C, Roberts V, Maddison R, et al. Effect of electronic time monitors on children’s television watching: pilot trial of a home-based intervention. Prev Med. 2009;49(5):413–417. 10.1016/j.ypmed.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 42.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282(16):1561–1567. 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 43.Robinson TN, Borzekowski DL. Effects of the SMART classroom curriculum to reduce child and family screen time. J Commun. 2006;56(1):1–26. 10.1111/j.1460-2466.2006.00001.x. [DOI] [Google Scholar]
- 44.Todd MK, Reis-Bergan MJ, Sidman CL, et al. Effect of a family-based intervention on electronic media use and body composition among boys aged 8–11 years: a pilot study. J Child Health Care. 2008;12(4):344–358. 10.1177/1367493508097404. [DOI] [PubMed] [Google Scholar]
- 45.Zimmerman FJ, Ortiz SE, Christakis DA, Elkun D. The value of social-cognitive theory to reducing preschool TV viewing: a pilot randomized trial. Prev Med. 2012;54(34):212–218. 10.1016/j.ypmed.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 46.Otten JJ, Jones KE, Littenberg B, Harvey-Berino J. Effects of television viewing reduction on energy intake and expenditure in overweight and obese adults: a randomized controlled trial. Arch Intern Med. 2009;169(22):2109–2115. 10.1001/archinternmed.2009.430. [DOI] [PubMed] [Google Scholar]
- 47.Branscum PW. Designing and evaluating an after-school social cognitive theory based comic book intervention for the prevention of childhood obesity among elementary aged school children. DAI-A. 2012;73(1A):87. [Google Scholar]
- 48.Campbell KJ, Lioret S, McNaughton SA, et al. A parent-focused intervention to reduce infant obesity risk behaviors: a randomized trial. Pediatrics. 2013;131(4):652–660. 10.1542/peds.2012-2576. [DOI] [PubMed] [Google Scholar]
- 49.Davison KK, Jurkowski JM, Li K, Kranz S, Lawson HA. A childhood obesity intervention developed by families for families: results from a pilot study. Int J Behav Nutr Phys Act. 2013;10:3. 10.1186/1479-5868-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr. 2010;91(4):831–840. 10.3945/ajcn.2009.28826. [DOI] [PubMed] [Google Scholar]
- 51.Dennison BA, Russo TJ, Burdick PA, Jenkins PL. An intervention to reduce television viewing by preschool children. Arch Pediatr Adolesc Med. 2004;158(2):170–176. 10.1001/archpedi.158.2.170. [DOI] [PubMed] [Google Scholar]
- 52.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing sedentary behaviors in treating pediatric obesity. Arch Pediatr Adolesc Med. 2000;154(3):220–226. 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 53.Epstein LH, Valoski AM, Vara LS, et al. Effects of decreasing sedentary behavior and increasing activity on weight change in obese children. Health Psychology. 1995;14(2):109–115. 10.1037/0278-6133.14.2.109. [DOI] [PubMed] [Google Scholar]
- 54.Ezendam NP, Brug J, Oenema A. Evaluation of the web-based computer-tailored FATaintPHAT intervention to promote energy balance among adolescents: results from a school cluster randomized trial. Arch Pediatr Adolesc Med. 2012;166(3):248–255. 10.1001/archpediatrics.2011.204. [DOI] [PubMed] [Google Scholar]
- 55.French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: Take Action-a group-randomized trial. Obesity (Silver Spring). 2011;19(10):2082–2088. 10.1038/oby.2010.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gentile DA, Welk G, Eisenmann JC, et al. Evaluation of a multiple ecological level child obesity prevention program: Switch what you Do, View, and Chew. BMC Med. 2009;7:49. 10.1186/1741-7015-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goldfield GS, Mallory R, Parker T, et al. Effects of open-loop feedback on physical activity and television viewing in overweight and obese children: a randomized, controlled trial. Pediatrics. 2006;1:e157–e166. 10.1542/peds.2005-3052. [DOI] [PubMed] [Google Scholar]
- 58.Gortmaker SL, Cheung LWY, Peterson KE, et al. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: eat well and keep moving. Arch Pediatr Adolesc Med. 1999;153(9):975–983. 10.1001/archpedi.153.9.975. [DOI] [PubMed] [Google Scholar]
- 59.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via aschool-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153(4):409–418. 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- 60.Hardy LL, King L, Kelly B, Farrell L, Howlett S. Munch and Move: evaluation of a preschool healthy eating and movement skill program. Int J Behav Nutr Phys Act. 2010;7:80. 10.1186/1479-5868-7-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Harrison M, Burns CF, McGuinness M, Heslin J, Murphy NM. Influence of a health education intervention on physical activity and screen time in primary school children: Switch Off–Get Active. J Sci Med Sport. 2006;9(5):388–394. 10.1016/j.jsams.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 62.Jago R, Sebire SJ, Turner KM, et al. Feasibility trial evaluation of a physical activity and screen-viewing course for parents of 6 to 8 year-old children: Teamplay. Int J Behav Nutr Phys Act. 2013;10:31. 10.1186/1479-5868-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Johnson B, Kremer P, Swinburn B, de Silva-Sanigorski A. Multilevel analysis of the Be Active Eat Well intervention: environmental and behavioural influences on reductions in child obesity risk. Int J Obes (Lond). 2012;36(7):901–907. 10.1038/ijo.2012.23. [DOI] [PubMed] [Google Scholar]
- 64.Jouret B, Ahluwalia N, Dupuy M, et al. Prevention of overweight in preschool children: results of kindergarten-based interventions. Int J Obes (Lond). 2009;33(10):1075–1083. 10.1038/ijo.2009.166. [DOI] [PubMed] [Google Scholar]
- 65.Lloyd JJ, Wyatt KM, Creanor S. Behavioural and weight status outcomes from an exploratory trial of the Healthy Lifestyles Programme (HeLP): a novel school-based obesity prevention programme. BMJ Open. 2012;2(3): 10.1136/bmjopen-2011-000390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Marcus C, Nyberg G, Nordenfelt A, Karpmyr M, Kowalski J, EkelundU. A 4-year, cluster-randomized, controlled childhood obesity prevention study: STOPP. Int J Obes (Lond). 2009;33(4):408–417. 10.1038/ijo.2009.38. [DOI] [PubMed] [Google Scholar]
- 67.O’Connor T, Hilmers A, Watson K, Baranowski T, Giardino A. Feasibility of an obesity intervention for paediatric primary care targeting parenting and children: Helping HAND. Child Care Health Dev. 2013;39(1):141–149. 10.1111/j.1365-2214.2011.01344.x. [DOI] [PubMed] [Google Scholar]
- 68.Patrick K, Calfas KJ, Norman GJ, et al. Randomized controlled trial of a primary care and home-based intervention for physical activity and nutrition behaviors: PACEþ for adolescents. Arch Pediatr Adolesc Med. 2006;160(2):128–136. 10.1001/archpedi.160.2.128. [DOI] [PubMed] [Google Scholar]
- 69.Puder JJ, Marques-Vidal P, Schindler C, et al. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): cluster randomised controlled trial. BMJ. 2011;343:d6195. 10.1136/bmj.d6195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Riggs NR, Sakuma KL, Pentz MA. Preventing risk for obesity by promoting self-regulation and decision-making skills: pilot results from the PATHWAYS to health program (PATHWAYS). Eval Rev. 2007;31(3):287–310. 10.1177/0193841X06297243. [DOI] [PubMed] [Google Scholar]
- 71.Robinson T, Killen J, Kraemer H, Wilson D, Matheson D, Haskell W. Dance and reducing TV to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis. 2003;13:S65–S77. [PubMed] [Google Scholar]
- 72.Robinson TN, Matheson DM, Kraemer HC, et al. A randomized controlled trial of culturally tailored dance and reducing screen time to prevent weight gain in low-income African American girls: Stanford GEMS. Arch Pediatr Adolesc Med. 2010;11:995–1004. 10.1001/archpediatrics.2010.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Roemmich JN, Gurgol CM, Epstein LH. Open-loop feedback increases physical activity of youth. Med Sci Sports Exerc. 2004;36(4):668–673. 10.1249/01.MSS.0000121947.59529.3B. [DOI] [PubMed] [Google Scholar]
- 74.Roemmich JN, Lobarinas CL, Barkley JE, White TM, Paluch R, Epstein LH. Use of an open-loop system to increase physical activity. Pediatr Exerc Sci. 2012;24(3):384–398. [DOI] [PubMed] [Google Scholar]
- 75.Salmon J, Ball K, Hume C, Booth M, Crawford D. Outcomes of a group-randomized trial to prevent excess weight gain, reduce screen behaviours and promote physical activity in 10-year-old children: Switch-play. Int J Obes. 2008;32(4):601–612. 10.1038/sj.ijo.0803805. [DOI] [PubMed] [Google Scholar]
- 76.Salmon J, Jorna M, Hume C, et al. A translational research intervention to reduce screen behaviours and promote physical activity among children: Switch-2-Activity. Health Promot Int. 2011;26(3):311–321. 10.1093/heapro/daq078. [DOI] [PubMed] [Google Scholar]
- 77.Shapiro JR, Bauer S, Hamer RM, Kordy H, Ward D, Bulik CM. Use of text messaging for monitoring sugar-sweetened beverages, physical activity, and screen time in children: a pilot study. J Nutr Educ Behav. 2008;40(6):385–391. 10.1016/j.jneb.2007.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Spruijt-Metz D, Nguyen-Michel ST, Goran MI, Chou CP, Huang TT. Reducing sedentary behavior in minority girls via a theory-based, tailored classroom media intervention. Int J Pediatr Obes. 2008;3(4):240–248. 10.1080/17477160802113415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: the High Five for Kids study. Arch Pediatr Adolesc Med. 2011;165(8):714–722. 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tucker S, Lanningham-Foster L, Murphy J, et al. A school based community partnership for promoting healthy habits for life. J Community Health. 2011;36(3):414–422. 10.1007/s10900-010-9323-9. [DOI] [PubMed] [Google Scholar]
- 81.Warren JM, Henry CJ, Lightowler HJ, Bradshaw SM, Perwaiz S. Evaluation of a pilot school programme aimed at the prevention of obesity in children. Health Promot Int. 2003;18(4):287–296. 10.1093/heapro/dag402. [DOI] [PubMed] [Google Scholar]
- 82.Whaley SE, McGregor S, Jiang L, Gomez J, Harrison G, Jenks E. A WIC-based intervention to prevent early childhood overweight. J Nutr Educ Behav. 2010;42(3 suppl):S47–S51. 10.1016/j.jneb.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 83.Spring B, Schneider K, McFadden HG, et al. Multiple behavior changes in diet and activity: a randomized controlled trial using mobile technology. Arch Intern Med. 2012;172(10):789–796. 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang LY, Yang Q, Lowry R, Wechsler H. Economic analysis of a school-based obesity prevention program. Obes Res. 2003;11(11):1313–1324. 10.1038/oby.2003.178. [DOI] [PubMed] [Google Scholar]
- 85.Dalziel K, Segal L, Mortimer D. Risk Factor Study—How to Reduce the Burden of Harm From Poor Nutrition, Tobacco Smoking, Physical Inactivity and Alcohol Misuse: Cost-Utility Analysis of 9 Multi-Risk Factor Interventions. Melbourne, Australia: Monash University, Centre for Health Economics, 2005. [Google Scholar]
- 86.Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and Technology 2013. Cambridge, MA: Pew Research Center, The Berkman Center for Internet & Society at Harvard University, 2013. [Google Scholar]
- 87.Schwantes T. Using active living principles to promote physical activity in rural communities. 2010. activelivingresearch.org/using-active-living-principles-promote-physical-activity-rural-communities.
- 88.Falbe J, Davison KK, Franckle RL, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. 2015;135(2): e367–e375. 10.1542/peds.2014-2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Richards R, McGee R, Williams SM, Welch D, Hancox RJ. Adolescent screen time and attachment to parents and peers. Arch Pediatr Adolesc Med. 2010;164(3):258–262. 10.1001/archpediatrics.2009.280. [DOI] [PubMed] [Google Scholar]
- 90.Biddle SJH, Petrolini I, Pearson N. Interventions designed to reducesedentary behaviours in young people: a review of reviews. Br J Sports Med. 2014;48:182–186. 10.1136/bjsports-2013-093078. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.