Summary
Background
The COVID-19 pandemic and associated responses have induced a host of crises worldwide, including an economic recession and a global mental health crisis. The specific effects of recession on youth mental health are understudied. We aimed to examine the mechanisms by which pandemic-related financial strain may affect mental health in a diverse sample of American adolescents.
Methods
We analyzed data from the Adolescent Brain Cognitive Development Study (ABCD Study®), a large, longitudinal study of diverse US adolescents which collected data before and during the pandemic (N = 9,720, mean age 12.9 years, 18.2% Black). Linear mixed-effects models tested associations of financial strain (parent-reported household wage loss and youth-reported financial stress) with depressive symptomatology over time, covarying for multiple confounders including pre-pandemic socioeconomic status and psychopathology, and pandemic-related environmental factors. Longitudinal mediation analyses examined potential mechanisms leading from wage loss to youth mental health.
Findings
Financial strain was highly prevalent, especially among low-income participants, with >70% of the total sample reporting lost wages. Both wage loss and subjective financial stress were associated with depressive symptomatology over time (Estimate = 0.04, P = 0.014; Estimate = 0.17, P < 0.001; respectively). The association between financial stress and depressive symptomatology was robust to the addition of multiple environmental confounders (Estimate = 0.16, P < 0.001). Both family-level (family conflict) and individual-level (financial stress) factors mediated the relationship between wage loss and depressive symptomatology.
Interpretation
The financial effects of COVID-19 (and worldwide responses to it) have taken a significant toll on youth mental health. In families that lost wages, youth-reported financial stress and familial factors mediated the relationship between wage loss and mental health over time. Findings highlight financial stress as a key driver of youth mental health burden and identify familial factors as critical targets for intervention to mitigate mental health risks in periods of economic crises.
Funding
This study was supported by the National Institute of Mental Health [grant numbers K23MH120437 (RB), R01MH117014 (TMM)]; the Lifespan Brain Institute of Children's Hospital of Philadelphia and Penn Medicine, University of Pennsylvania.
Keywords: COVID-19, Economic crisis, Financial strain, Stress, Child and adolescent mental health, Depression
Research in context.
Evidence before this study
Preliminary evidence, largely in adult populations, suggests that COVID-19-related financial strain is associated with negative mental health outcomes, similar to previous economic recessions. Multiple studies have also explored the impacts of the pandemic, including financial, on disadvantaged families, suggesting vulnerable populations are at greater risk of facing significant pandemic-induced burden. We searched PubMed, Google Scholar, Penn Libraries, and medRxiv on May 15, 2022, for studies published in English since March 1, 2020, that examined the economic impact of COVID-19 on individuals, specifically children and adolescents. We used the search terms “COVID-19”, “children”, “adolescents”, “financial strain”, and related synonyms. Scarce data are available on the relationship between pandemic-related financial strain and youth mental health.
Added value of this study
We investigate the specific association of financial strain with adolescent mental health longitudinally between May 2020 and May 2021 in a diverse sample of 9720 youth. All participants had pre-pandemic data on household income and mental health. To our knowledge, this is the most comprehensive study to prospectively study the relationship of financial strain with youth mental health during the pandemic accounting for pre-pandemic factors. Results provide evidence that financial strain is specifically associated with youth mental health burden and suggest pathways that mediate this link and can be targets for future mental health preventative interventions.
Implications of all the available evidence
The pandemic-related financial strain appears to take a distinct toll on adolescent mental health. Adolescents whose families were disadvantaged prior to the onset of the pandemic face disproportionately greater amounts of financial strain, putting them at greater risk. The financial strain appears to drive youth's mental health symptomatology through their self-reported financial stress and through family conflict. Findings highlight the need to address both youth's perspective of financial strain and family dynamics surrounding financial strain as key factors in mental health risk classification and as potential targets for intervention for mitigating mental health consequences among youth following the pandemic.
Introduction
Socioeconomic disadvantage plays a major role in health and disease,1 and periods of financial uncertainty pose substantial hazards to mental health specifically.2 The rippling effects of financial crises can be devastating to families, particularly to children and adolescents, who depend heavily on the family to provide a context for healthy development.3 Youths whose families endure significant financial strain tend to face both stunted development and behavioural problems,4,5 and are at greater risk to endure health problems, social dysfunction, and socioeconomic disadvantage later in life.6
Amidst its drastic impact on global health and public policy, the COVID-19 pandemic has also fed a global economic crisis which has both exacerbated financial issues in struggling families and introduced newfound financial strain to many others.7 It's been demonstrated in adult populations that both pandemic-resultant income loss and financial stress have distinct associations with depressive symptoms over and above multiple confounders.8, 9, 10 However, the specific impacts of pandemic-related financial strain on adolescent health have not been thoroughly investigated, despite accumulating data suggesting an increased burden of depression and anxiety in youth globally.11 Thus, further research is needed to clarify the relationship between financial strain and youth mental health.
With the growing understanding of the role of social determinants of mental health,12 it's important to dissect how specific social and economic factors influence health outcomes during the pandemic. Preliminary studies in youth populations have identified various factors associated with mental health burden during the pandemic, including social isolation, school closure, and uncertainty about the future.13,14 Research conducted before the pandemic has identified key familial factors through which financial strain may affect adolescents, including parental mental health, parenting quality, and family conflict.15,16 To promote resilience in youth following the pandemic, it is critical to identify mechanisms by which pandemic-related factors drive youth mental health burden and detect potentially modifiable targets for intervention.
In the current study, we aimed to disentangle the specific relationship between pandemic-related financial strain and youth mental health, accounting for pre-pandemic economic and mental health factors. We leveraged data from the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study,17 which has followed a large sample of American youths since prior to the pandemic and administered multiple surveys specifically targeted to characterize the impacts of COVID-19 longitudinally between May 2020 and May 2021. Previous work in the ABCD Study has used data-driven approaches to identify risk and resilience factors for youth mental health during the pandemic,18,19 as well as highlight key disparities on social determinants of health underlying COVID-19 impact.20,21 Building on these works, we aimed to dissect the specific effect of financial strain on youth mental health during the pandemic and identify mechanisms underlying this relationship. We hypothesized that financial strain would drive depressive symptomatology in youth throughout the course of the pandemic and that subjective financial stress and family-level factors will mediate the relationship of pandemic-related wage loss with youth mental health.
Methods
Participants
The ABCD sample included 11,878 children aged 9–10 years at baseline assessment (conducted 2016–2018), recruited through school systems.17 Participants were enrolled at 21 sites across the continental US, the catchment area comprising over 20% of the US population in this age group. We analyzed data from ABCD Study® data release 4.0 (https://abcdstudy.org/), which included a series of seven electronically administered surveys that were sent to participants to characterize the impacts of the COVID-19 pandemic from May 2020 to May 2021. In total, 9720 unique participants participated in at least one of these surveys (mean age 12.9, 47.8% female, 77.6% White). See Supplemental Table S1 for a demographic breakdown of each survey. Pre-pandemic data was included from the 1-year follow-up assessment (conducted 2017–2020; N = 11,235, mean age 10.9 years, 47.7% female, 75.3% White). See Supplemental Table S2 for a demographic breakdown of the 1-year follow-up sample and a comparison of participants who completed at least one COVID-19 survey versus those who did not.
All participants gave assent. Parents/caregivers signed informed consent. The ABCD protocol was approved by the University of California, San Diego Institutional Review Board (IRB), and was exempted from a full review by the University of Pennsylvania IRB.
Measures
All ABCD Study measures used in the current analysis are described in Supplemental Table S3.
Exposure measures
We used two measures of pandemic-related financial strain in our main analyses: (i) parent-reported household wage loss during the pandemic (i.e., objective strain); (ii) youth-reported financial stress (i.e., subjective strain). The parent-reported wage loss measure was binary (yes/no) and probed whether any member of the household had lost wages since January 2020 “due to the impact of coronavirus on employment, business, or the economy.” The youth-reported financial stress measure was a single item which probed, “over the past week, I worried that my family would not have enough money to pay for necessities like clothing or bills,” measured on a Likert scale (from “never” [0] to “very frequently” [4]). To further ensure specificity of the subjective measure to only financial stress, we regressed out a youth-reported item from the financial stress measure that assessed general worry “about coronavirus,” also measured on a Likert scale (from “not at all” [1] to “extremely” [5]).
In sensitivity analyses, we used a measure of experiences of poverty during the pandemic, as well as an item administered to parents to assess whether their children were worried about the “non-health-related consequences of coronavirus (e.g., financial).”
Outcome measures
The ABCD COVID-19 surveys included multiple measures of different domains of mental health. The main outcome measure used in the current study was the sum-score of an 8-item sadness scale that assessed depressive-spectrum symptoms, part of the NIH PhenX Toolkit.22 The items in this scale assessed the presence of symptoms in the past week (feelings of sadness and loneliness, difficulty having fun, feeling “everything in my life went wrong” and “like I couldn't do anything right”), each measured on a Likert scale (from “never” [1] to “almost always” [5]). The COVID-19 surveys also included other mental health measures: (i) a single-question item assessing recent changes in general mental health; (ii) the PhenX Toolkit perceived stress scale; (iii) multiple questions assessing substance use patterns. In the current study, measures of alcohol use, marijuana use, and other drug use (use of cocaine, methamphetamine, heroin, hallucinogens; sniffing liquids, sprays, gases; misuse of prescription drugs) were included.
Covariates
All models covaried for age, sex, race (White, Black, other), Hispanic ethnicity, pre-pandemic household income (ordinal, from below $5000 [1] to above $200,000 [10] annually), and pre-pandemic parental education (mean years). Participants could endorse more than one race in ABCD Study. In our analyses, we considered race as endorsed by participants (e.g., if a participant endorsed Black race, they were considered as Black regardless of whether they also endorsed another race). To address confounding effects of prior mental health burden, a dimensional measure of pre-pandemic psychopathology was introduced as a covariate (P-factor23).
To address confounding effects of non-financial environmental confounders, we further covaried for multiple factors that have been previously linked to mental health outcomes in youth. These factors included both pandemic-specific exposures (COVID-19 infection, school closure, family social isolation behaviours, pandemic-related separation from an important figure) and non-pandemic-specific exposures (family conflict, parental monitoring, weekly screen time, presence of daily routines, frequency of exercise and outdoor play).
Statistical analyses
Analytic design and hypotheses were preregistered in October 2021 (https://osf.io/guzwh/), prior to ABCD data release 4.0. Data analyses were conducted between January and April 2022, using the SPSS 26.0 statistical package and R 4.1.2. Mean (standard deviation [SD]) and frequency (%) were reported for descriptive purposes. Univariate comparisons were made using t-tests for continuous measures and chi-square tests for categorical variables, with false discovery rate (FDR) correction for multiple testing.
To handle the hierarchical and longitudinal nature of the ABCD data, linear mixed-effects models were employed using the lme4 R package to determine the association of financial strain with mental health outcomes over time.24 All models took the 3-level structure of the data into account; survey time points were first nested according to subject ID and then according to family ID. The ABCD COVID-19 surveys were administered online, thus we did not consider random effects of site in main models; instead, we performed sensitivity analyses which considered site-specific effects. Furthermore, we assumed time-associated trends to be similar across subjects and allowed only random intercepts in all models. We employed listwise deletion for observations at any time point with missing values. In all models, multicollinearity among independent variables was acceptable with Variance inflation factor (VIF) scores smaller than 2.
Longitudinal mediation analyses were conducted using the lavaan R package25; for this, we applied bootstrapped mediation with 500 samples.
Univariate comparisons characterizing participants affected by pandemic-related financial strain
To begin to understand the characteristics of families most impacted by pandemic-related financial strain, we compared participants whose families lost wages during the pandemic to those whose families retained wages across a variety of domains. For the purposes of comparison, included data was summarized temporally across all COVID-19 surveys. If a participant's parent reported lost wages at any of the seven surveys, that participant's family was considered to have lost wages. For continuous variables, mean scores were calculated from available data points across all surveys. For binary (yes/no) variables, endorsement at any survey was considered positive endorsement (i.e., yes). For demographic variables (excluding age), data was taken from the 1-year follow-up assessment. To further probe the role of pre-pandemic socioeconomic status in families' resilience to the financial impact of the pandemic, we compared prevalence of parent-reported household wage loss and youth-reported financial stress across quintiles of pre-pandemic household income.
Multivariable models of longitudinal associations between financial strain and depressive symptoms
To determine the association of pandemic-related financial strain with depressive symptoms over the course of the pandemic, we conducted two sets of mixed-effects models – one which used parent-reported household wage loss as the main exposure and one which used youth-reported financial stress as the main exposure. Models covaried for age, sex, race, ethnicity, parental education, and pre-pandemic household income. To address the possibility that pre-pandemic mental health confounded the association, we further included pre-pandemic P-factor as a covariate. To address the possibility that confounding environmental factors may drive associations, we further introduced a variety of pandemic-specific and non-pandemic-specific environmental factors as covariates. The model with financial stress as the main exposure was also run with household wage loss as a covariate.
Longitudinal mediation analyses
To better understand potential mechanisms leading from financial strain to youth mental health, longitudinal mediation analyses were employed to examine the pathway from wage loss at the beginning of data collection (first two surveys; May–June 2020) to depressive symptomatology a year into data collection (last survey; May 2021). To allow temporal separation between variables, mediator data was averaged across the four intermediate surveys (August 2020–March 2021). To enhance the specificity of results, we regressed out sociodemographic data (age, sex, race, ethnicity, pre-pandemic household income) from our main exposure (household wage loss). First, youth-reported financial stress was assessed as a mediator in the pathway between parent-reported household wage loss and youth-reported depressive symptoms. Next, in a separate model, multiple familial factors (family conflict, parental monitoring, and parent-reported conflict between family and workplace responsibilities) were assessed as mediators. Finally, both youth-reported financial stress and familial factors were assessed as mediators in the same model. Due to the temporal separation of data for longitudinal mediation, only participants who provided data on depressive symptoms at the most recent survey were included (n = 4427). We then employed listwise deletion for participants with missing data within this reduced sample.
Sensitivity analyses
To evaluate potential effects of our choice of exposures, main models were run using two alternative parent-reported measures of financial strain: (i) count of poverty experiences during the pandemic and (ii) prevalence of their child's worries about the non-health consequences of the pandemic (e.g., financial) as independent variables. To evaluate the potential effects of our choice of dependent variable as a mental health indicator, we conducted analyses to assess the association between the main exposures and three different mental health outcomes: (i) general mental health; (ii) perceived stress; and (iii) substance use. Additional models were run to account for potential site-specific effects: one in which site was treated as a covariate and one which considered site as a random effect.
Role of funding source
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Results
Characterization of participants affected by pandemic-related financial strain
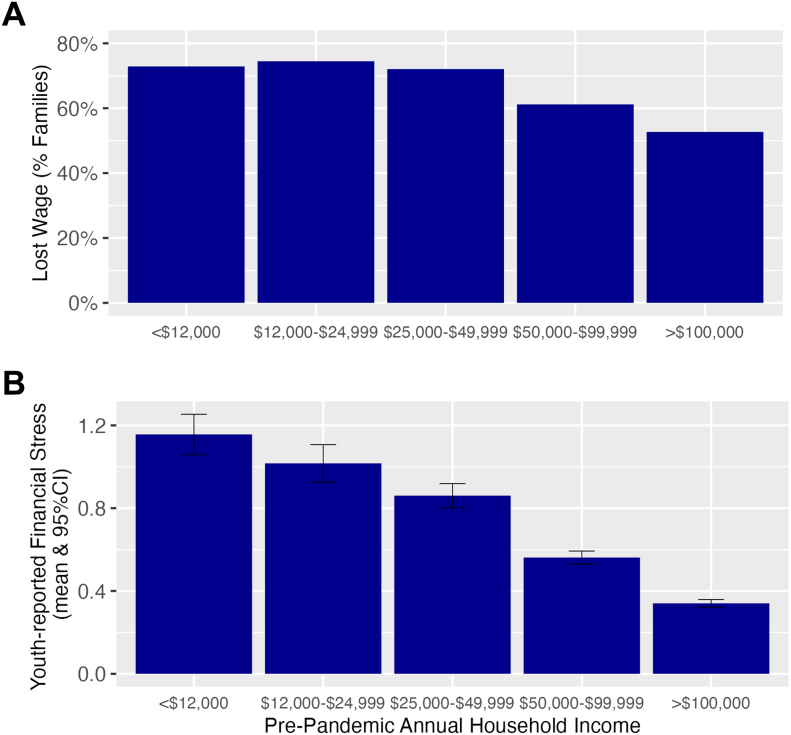
Participants whose families lost wages due to the pandemic were significantly different from those whose families retained wages (Table 1). Those who lost wages were more likely to be Black (19.5% vs 12.2%), Hispanic (22.0% vs 12.9%), and below the poverty line (15.2% vs 4.2%) than those who did not (P's < 0.001). They also endorsed greater levels of stress about the financial impacts of the pandemic (mean [SD] 0.6 [0.8] vs 0.3 [0.5], P < 0.001). Moreover, both pandemic-related wage loss and financial stress were more prevalent among participants with lower pre-pandemic household income (Fig. 1). In terms of mental health, participants from families who lost wages endorsed more symptoms of depression compared to those from families who did not lose wages (mean [SD] 15.3 [6.4] vs 14.8 [5.9], respectively, P = 0.004) and reported experiencing more perceived stress (mean [SD] 7.7 [2.5] vs 7.3 [2.3], respectively, P < 0.001), with no difference in substance use patterns (P = 0.739).
Table 1.
Comparison of participants whose families lost or retained wages as a result of the coronavirus pandemic.
| Total sample |
Lost wages |
Retained wages |
P-valuea | Missing data |
||||
|---|---|---|---|---|---|---|---|---|
| n = 9720 |
n = 5805 |
n = 2123 |
1792 (18.4%) | |||||
| Mean | SD | Mean | SD | Mean | SD | |||
| Age (years) | 12.9 | 0.9 | 12.8 | 0.9 | 12.9 | 0.9 | <0.001 | |
| Parent education (years) | 16.7 | 2.5 | 16.4 | 2.6 | 17.6 | 2.0 | <0.001 | |
| Financial stress (mean score) | 0.6 | 0.8 | 0.6 | 0.8 | 0.3 | 0.5 | <0.001 | 966 (9.9%) |
| Family social isolation (mean score) | 5.9 | 3.0 | 6.2 | 2.9 | 5.8 | 2.7 | <0.001 | |
| Depressive symptoms (mean score) | 15.1 | 6.3 | 15.3 | 6.4 | 14.8 | 5.9 | 0.007 | 1853 (19.1%) |
| Perceived stress (mean score) | 7.6 | 2.5 | 7.7 | 2.5 | 7.3 | 2.3 | <0.001 | 3883 (39.9%) |
| n | % | n | % | n | % | P-valuea | ||
|---|---|---|---|---|---|---|---|---|
| Sex (female) | 4651 | 47.9% | 2727 | 47.0% | 1053 | 49.6% | 0.05 | |
| White race | 7546 | 77.6% | 4392 | 75.7% | 1805 | 85.0% | <0.001 | |
| Black race | 1765 | 18.2% | 1134 | 19.5% | 258 | 12.2% | <0.001 | |
| Hispanic ethnicity | 1849 | 19.3% | 1259 | 22.0% | 272 | 12.9% | <0.001 | |
| Below poverty line | 1033 | 12.0% | 764 | 15.2% | 83 | 4.2% | <0.001 | 1125 (11.6%) |
| COVID-19 infection (child) | 499 | 8.6% | 332 | 9.1% | 124 | 5.9% | <0.001 | 3922 (40.3%) |
| COVID-19 infection (other family member) | 1686 | 19.7% | 1154 | 21.9% | 342 | 16.7% | <0.001 | 1545 (15.9%) |
| School closure | 8364 | 99.9% | 5088 | 100.0% | 1957 | 99.8% | 0.303 | 1806 (18.6%) |
| Any substance use | 648 | 7.5% | 407 | 7.9% | 163 | 8.0% | 0.86 | 1066 (11%) |
When compared across sociodemographic factors, family experiences during the pandemic, and mental health, participants whose families lost wages due to the pandemic were significantly different from participants whose families retained wages during the pandemic.
For the purposes of comparison, variables were collapsed temporally across all seven surveys administered as part of the ABCD COVID-19 assessment. Because not every participant completed every survey, there is substantial missing data; missing data greater than 3% is detailed in the rightmost column.
FDR corrected P-value.
Fig. 1.
Household wage loss (A) and youth-reported financial stress (B) across quintiles of pre-pandemic annual household income. Pandemic-related financial strain was greater in lower income levels. (A) Experiencing wage loss during COVID-19 was less likely with higher pre-COVID annual income (logistic regression of pre-pandemic annual income level predicting income loss Odds ratio = 0.57, P < 0.001). (B) Youth financial stress (measured on a Likert scale from “never” [0] to “very frequently” [4] worrying that family will not have money to pay for necessities) during COVID-19 was lower with higher pre-COVID annual income (linear regression of income level predicting COVID-19 financial stress β = −0.339, P < 0.001).
Longitudinal association of pandemic-related financial strain and youth mental health
Parent-reported household wage loss was significantly associated with youth's depressive symptoms over time when accounting for demographic and pre-pandemic socioeconomic factors (Model 1; Estimate = 0.04, P = 0.014), and when further co-varying for pre-pandemic psychopathology (Model 2; Estimate = 0.04, P = 0.018). This association became nonsignificant upon the introduction of non-financial environmental confounders to the model (Model 3; Table 2).
Table 2.
Association of household wage loss with depressive symptoms over time.
| Model 1 |
Model 2 |
Model 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Estimate | CI | P-value | Estimate | CI | P-value | Estimate | CI | P-value | |
| Wage loss | 0.04 | 0.01–0.07 | 0.014 | 0.04 | 0.01–0.07 | 0.018 | −0.01 | −0.05 to 0.03 | 0.633 |
| Pre-COVID-19 household income | −0.03 | −0.05 to 0.00 | 0.068 | −0.01 | −0.03 to 0.02 | 0.694 | −0.001 | −0.03 to 0.03 | 0.921 |
| Pre-COVID-19 parent education | 0.02 | −0.01 to 0.05 | 0.206 | 0.04 | 0.01–0.06 | 0.008 | 0.04 | 0.01–0.07 | 0.003 |
| Pre-COVID-19 psychopathology | 0.27 | 0.25–0.29 | <0.001 | 0.22 | 0.20–0.24 | <0.001 | |||
| Family conflict | 0.06 | 0.04–0.07 | <0.001 | ||||||
| Parental monitoring | −0.12 | −0.14 to −0.10 | <0.001 | ||||||
| Weekly screen time | 0.03 | 0.01–0.05 | <0.001 | ||||||
| Daily routines | −0.02 | −0.04 to −0.00 | 0.022 | ||||||
| Exercise/outside play | −0.07 | −0.09 to −0.05 | <0.001 | ||||||
| COVID-19 infection (child) | −0.44 | −0.94 to 0.05 | 0.079 | ||||||
| School closure | −0.03 | −0.13 to 0.08 | 0.632 | ||||||
| Family social isolation | 0.02 | 0.00–0.05 | 0.031 | ||||||
| Child separation from someone important due to pandemic | 0.19 | 0.15–0.23 | <0.001 | ||||||
Three linear mixed-effects models were run to disentangle the role of household wage loss (independent variable) from confounding factors in association with depressive symptoms (dependent variable).
Model 1 co-varies for age, sex, race (Black, White, other), Hispanic ethnicity, pre-pandemic household income, pre-pandemic parental education and assessment time-point.
Model 2 builds on Model 1 by adding pre-pandemic psychopathology.
Model 3 builds on Model 2 by adding pandemic-specific and non-pandemic-specific environmental risk and protective factors.
Abbreviation: CI = confidence interval.
Youth-reported financial stress was also significantly associated with youth's depressive symptoms (Table 3). This association was observed when accounting for demographics and pre-pandemic socioeconomic factors (Model 1; Estimate = 0.17, P < 0.001), when further accounting for pre-pandemic psychopathology (Model 2; Estimate = 0.16, P < 0.001), and when accounting for non-financial environmental confounders (Model 3; Estimate = 0.16, P < 0.001) as well as for household wage loss (Model 4; Estimate = 0.16, P < 0.001).
Table 3.
Association of youth-reported financial stress with depressive symptoms over time.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | CI | P-value | Estimate | CI | P-value | Estimate | CI | P-value | Estimate | CI | P-value | |
| Financial stressa | 0.17 | 0.15–0.19 | <0.001 | 0.16 | 0.14–0.17 | <0.001 | 0.16 | 0.14–0.18 | <0.001 | 0.16 | 0.14–0.19 | <0.001 |
| Pre-COVID-19 household income | 0.0007 | −0.03 to 0.03 | 0.955 | 0.02 | −0.01 to 0.04 | 0.15 | 0.02 | −0.00 to 0.05 | 0.089 | 0.02 | −0.01 to 0.05 | 0.108 |
| Pre-COVID-19 parent education | 0.03 | 0.00–0.05 | 0.032 | 0.04 | 0.02–0.07 | 0.001 | 0.06 | 0.03–0.09 | <0.001 | 0.06 | 0.03–0.08 | <0.001 |
| Pre-COVID-19 psychopathology | 0.25 | 0.23–0.27 | <0.001 | 0.21 | 0.18–0.23 | <0.001 | 0.21 | 0.18–0.23 | <0.001 | |||
| Family conflict | 0.05 | 0.03–0.07 | <0.001 | 0.05 | 0.03–0.07 | <0.001 | ||||||
| Parental monitoring | −0.11 | −0.13 to −0.09 | <0.001 | −0.11 | −0.13 to −0.09 | <0.001 | ||||||
| Weekly screen time | 0.04 | 0.02–0.05 | <0.001 | 0.04 | 0.02–0.05 | <0.001 | ||||||
| Daily routines | −0.02 | −0.04 to 0.00 | 0.062 | −0.02 | −0.04 to −0.00 | 0.042 | ||||||
| Exercise/outside play | −0.07 | −0.09 to −0.05 | <0.001 | −0.07 | −0.08 to −0.05 | <0.001 | ||||||
| COVID-19 infection (child) | −0.4 | −0.88 to 0.09 | 0.113 | −0.39 | −0.88 to 0.10 | 0.120 | ||||||
| School closure | −0.02 | −0.13 to 0.08 | 0.651 | −0.02 | −0.13 to 0.08 | 0.664 | ||||||
| Family social isolation | 0.03 | 0.00–0.05 | 0.025 | 0.03 | 0.00–0.05 | 0.021 | ||||||
| Child separation from someone important due to pandemic | 0.19 | 0.15–0.23 | <0.001 | 0.19 | 0.15–0.23 | <0.001 | ||||||
| Wage loss | −0.03 | −0.07 to 0.01 | 0.088 | |||||||||
Four linear mixed-effects models were run to disentangle the role of youth-reported financial stress (independent variable) from confounding factors in association with depressive symptoms (dependent variable).
Model 1 co-varies for age, sex, race (Black, White, other), Hispanic ethnicity, pre-pandemic household income, pre-pandemic parental education, and assessment time-point.
Model 2 builds on Model 1 by adding pre-pandemic psychopathology.
Model 3 builds on Model 2 by adding pandemic-specific and non-pandemic-specific environmental risk and protective factors.
Model 4 builds on Model 3 by adding household wage loss.
Abbreviation: CI = confidence interval.
General worries about coronavirus were regressed out of the financial stress variable.
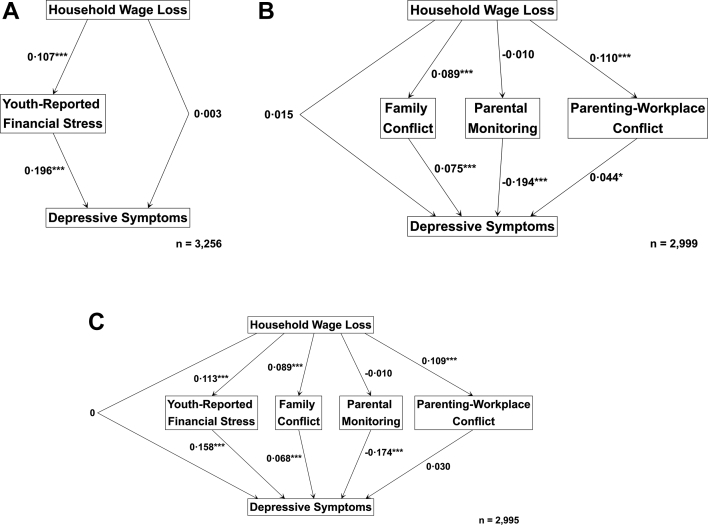
Mediating factors between household wage loss and youth depressive symptoms over time
To better understand potential causal pathways from pandemic-related wage loss to depressive symptoms in youth a year later, we conducted three longitudinal mediation analyses to examine the directionality of effects and test the following potential mediating factors: (i) youth-reported financial stress (Mediation Model 1), (ii) familial factors (Mediation Model 2), and (iii) both youth-reported financial stress and familial factors together (Mediation Model 3).
Mediation Model 1 revealed a significant indirect effect of wage loss on depressive symptoms mediated by youth-reported financial stress (Estimate = 0.021, P < 0.001; Fig. 2A). Mediation Model 2 revealed a significant indirect effect of parent-reported household wage loss on depressive symptoms mediated by family conflict and parent-reported conflict between family and workplace responsibilities, but not parental monitoring (Estimate = 0.013, P = 0.004; Fig. 2B). When tested together in Mediation Model 3, the observed indirect effect from household wage loss on depressive symptoms was driven by youth-reported financial stress and family conflict, but not parental monitoring or parent-reported conflict between family and workplace responsibilities (Estimate = 0.03, P < 0.001; Fig. 2C). No direct effect between wage loss and youth depressive symptoms was observed in any mediation analysis. Full statistics for all mediation models are presented in Supplemental Table S4.
Fig. 2.
Longitudinal Mediation analysis examining the pathway between household wage loss reported in May–June 2020 and youth depressive symptoms reported in May 2021. Three longitudinal mediation analyses were run to examine the pathway from household wage loss (at the beginning of data collection; May–June 2020) to depressive symptoms (a year later; May 2021), using mediator data from intermittent survey data (August 2020–March 2021). (A) Mediation Model 1 examines youth-reported financial stress as a mediator. (B) Mediation Model 2 examines familial factors (family conflict, parental monitoring, and parent-reported conflict between family and workplace responsibilities) as mediators. (C) Mediation Model 3 examines both youth-reported financial stress and familial factors as mediators. Sociodemographic data (age, sex, race, ethnicity, pre-pandemic household income) was regressed out of household wage loss (independent variable). General worries about coronavirus were regressed out of youth-reported financial stress (mediator). ∗ indicates P-value less than 0.05. ∗∗∗ indicates P-value less than 0.001.
Sensitivity analyses
Use of different measures of financial strain than those used in main analyses (parent-reported mid-pandemic poverty experiences and parent-reported youth financial stress) showed similar associations with depressive symptoms (Supplemental Tables S5 and S6). Use of different youth-reported mental health measures instead of depressive symptoms (general mental health, perceived stress, substance use) revealed similar associations with financial strain as main analyses (Supplemental Tables S7–S9). Models accounting for site-specific effects also proved similar in directionality and significance to main models (Supplemental Table S10).
Discussion
Leveraging a large diverse sample of American adolescents, we report specific longitudinal associations between financial strain and youth mental health over the course of a year from mid-2020 to mid-2021. We found that youth's subjective stress about their family's financial situation during the pandemic, as well as family conflict, mediate the relationship between wage loss in the household and youth mental health. The fact that findings were significant when accounting for pre-pandemic household income and pre-pandemic youth psychopathology highlights the relevance of financial strain to youth mental health across socioeconomic levels and regardless of their pre-pandemic mental health. Taken together the current study suggests that the financial consequences of COVID-19 are a major contributing factor to the youth mental health burden, in what has been coined a global youth mental health crisis.11
Our results show that youth's financial strain during the pandemic is a unique driver of negative mental health outcomes. While there is established literature on the relationship between financial stress and mental health of adults, including during the COVID-19 pandemic,8, 9, 10 there is very limited data on youth's financial strain and mental health. A single study in families who entered the child welfare system in the US showed an association between parent-reported financial stress and parent reports of youth internalizing symptoms.26 During the pandemic, a single study from Canada reported associations between COVID-19 financial strain and adverse youth mental health in a sample of 215 youth of whom 65% had pre-COVID psychiatric disorders.27 Our results expand the literature by showing that in a large sample of community youth, which is not enriched for socioeconomic vulnerability nor for psychiatric patients, financial strain is critical in driving youth mental health burden. Notably, the diversity of this study's sample allowed appreciation of the greater burden of financial stress experienced among study participants of lower income and of non-White race families. These finding echo recent ABCD Study analyses highlighting disparities in COVID-19's impact on youth.19,20
A key strength of this work that adds to previous studies is the investigation into mechanisms leading from objective financial hardship in the household (i.e., wage loss) to youth's mental health symptoms in a longitudinal mediation framework. This analysis was made possible given the repeated sampling during the pandemic that allowed for temporal separation between pandemic-related wage loss, the tested mediators, and later depressive symptoms. We found that both individual-level (youth-reported financial stress) and family-level (family conflict) factors mediate the path from “objective” financial hardship to mental health symptom. These findings confirmed our hypotheses and concurred with the literature studying the complex role of financial strain in childhood wellbeing, suggesting that economic hardship impacts children and adolescents through a multitude of indirect pathways.28 These pathways largely involve induced changes in family environment and parental practices,15,16 but also youth's own stress about their financial situations and socioeconomic status.29
This study may have two clinical implications that are critical in light of the current youth mental health crisis.11 First, our results highlight financial strain as a key factor in youth mental health and calls for clinicians' vigilance regarding the financial consequences of the pandemic. This is in line with the growing realization of the role of social determinants in shaping mental health.12 While the current work addressed specificity of financial strain to COVID-19 pandemics' effects, it is likely that financial strain is a broader mental health risk factor for youth that was made more salient during the pandemic but will remain key in youth mental health in times of economic uncertainties. Second, our mediation analyses point to youth's subjective financial stress and to family conflict as potential modifiable factors on the causal pathway from objective financial hardship to youth depressive symptoms. Future interventional studies can now target these two mediators in attempt to mitigate the pandemic related mental health burden.
Our results should be interpreted considering several limitations. First, it's important to acknowledge participant attrition from pre-pandemic assessment to mid-pandemic data collection; out of the 11,235 participants who completed the annual 1-year ABCD Study assessment (the last assessment to be completed before the pandemic), 1505 participants did not respond to any COVID-19 survey. Of these participants, 33.8% were Black, 25.1% were Hispanic, and 29.5% fell below the poverty line, highlighting the loss of a significant portion of the socioeconomically disadvantaged study sample to the “digital divide”.30 In addition, of the 9720 participants who responded to the COVID-19 surveys, 18.4% did not provide data on changes to income during the pandemic. Despite this, the large sample that was included in the current analysis was still racially and ethnically diverse (18.2% Black, 19.3% Hispanic), included a significant number of adolescents whose families were below the poverty line (12.0%) and comprised a significant catchment area across the United States. Taken together, the characteristics of the sample we analyzed support generalizability of findings to families across the US. Nonetheless, generalizability to other countries' populations, in which public health measures and government response to the pandemic differed, may be limited. Second, there are other factors that could potentially confound the relationship between wage loss and financial strain with youth depressive symptoms during the pandemic, these include (among others) parental mental health and access to mental health care that were not assessed in the surveys analyzed in this work. Third, the sample was substantially smaller for the mediation analyses where we only include youth who completed the last sadness scale survey (N = 4427). Another limitation is the use of the NIH PhenX Toolkit22 sadness scale to evaluate depressive symptomatology, which did not include certain symptoms of clinical major depressive disorder (diminished appetite/energy, and suicidality). Indeed, we do not make claims here regarding clinical depression, but rather presence of specific depressive symptoms. Notably, our sensitivity analyses demonstrated consistent longitudinal associations of financial strain with multiple other measures of youth mental health, supporting the validity of main results.
Conclusions
To conclude, this study highlights the pressing burden of the economic fallout related to the COVID-19 pandemic on the mental health of adolescents. Findings identify key contextual factors that should be considered by both clinicians and policymakers to mitigate the youth mental health burden of pandemic-related financial strain, including youth financial stress and familial dynamics. Results should inform healthcare providers and policymakers on key risk factors for youth mental health during economic crises.
Contributors
S.T.A. contributed to study conceptualization, formal analysis, investigation and wrote the first draft of the manuscript. K.T.T. contributed to data curation, formal analysis, investigation, methodology, software and visualization. E.V. contributed to data curation, formal analysis, investigation, methodology, software and visualization. G.E.D. contributed to data curation, project administration, and resources. T.M.M. contributed to formal analysis, investigation, methodology, software and supervision. R.B. contributed to study conceptualization, formal analysis, investigation, funding acquisition, supervision and wrote the first draft of the manuscript with S.T.A. All authors substantially contributed to the final version of the manuscript. S.T.A., K.T.T. and E.V. had direct access to the data. R.B. is responsible for the decision to submit the manuscript.
Data sharing statement
Link to study protocol: https://osf.io/guzwh/. Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development Study (https://abcdstudy.org), held in the National Institute of Mental Health Data Archive.
Declaration of interests
Dr Barzilay serves on the scientific board and receives consulting fees from ‘Taliaz Health’ and ‘Zynerba Pharmaceuticals’ and reports stock ownership in ‘Taliaz Health’, with no conflict of interest relevant to this work. All other authors have no conflicts of interest to disclose.
Acknowledgements
Data used in the preparation of this article were obtained from the Adolescent Brain and Cognitive DevelopmentSM (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9–10 and follow them over 10 years into early adulthood. The ABCD Study® is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041048, U01DA050989, U01DA051016, U01DA041022, U01DA051018, U01DA051037, U01DA050987, U01DA041174, U01DA041106, U01DA041117, U01DA041028, U01DA041134, U01DA050988, U01DA051039, U01DA041156, U01DA041025, U01DA041120, U01DA051038, U01DA041148, U01DA041093, U01DA041089, U24DA041123, U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/consortium_members/. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators.
Funding/support: This study was supported by the National Institute of Mental Health [grant numbers K23MH120437 (R.B.), R01MH117014 (T.M.M.)]; the Lifespan Brain Institute of Children's Hospital of Philadelphia and Penn Medicine, University of Pennsylvania.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2022.100391.
Appendix A. Supplementary data
References
- 1.Adler N.E., Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff. 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 2.Christodoulou N.G., Christodoulou G.N. Financial crises: impact on mental health and suggested responses. Psychother Psychosom. 2013;82:279–284. doi: 10.1159/000351268. [DOI] [PubMed] [Google Scholar]
- 3.Frasquilho D., Matos M.G., Salonna F., et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health. 2016;16:115. doi: 10.1186/s12889-016-2720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mari G., Keizer R. Parental job loss and early child development in the Great Recession. Child Dev. 2021;92(5):1698–1716. doi: 10.1111/cdev.13517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duran C.A.K., Cottone E., Ruzek E.A., Mashburn A.J., Grissmer D.W. Family stress processes and children's self-regulation. Child Dev. 2020;91:577–595. doi: 10.1111/cdev.13202. [DOI] [PubMed] [Google Scholar]
- 6.Santini Z.I., Koyanagi A., Stewart-Brown S., Perry B.D., Marmot M., Koushede V. Cumulative risk of compromised physical, mental and social health in adulthood due to family conflict and financial strain during childhood: a retrospective analysis based on survey data representative of 19 European countries. BMJ Glob Health. 2021;6:1–14. doi: 10.1136/bmjgh-2020-004144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brodeur A., Gray D., Islam A., Bhuiyan S. A literature review of the economics of COVID-19. J Econ Surv. 2021;35(4):1007–1044. doi: 10.1111/joes.12423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hertz-Palmor N., Moore T.M., Gothelf D., et al. Association among income loss, financial strain and depressive symptoms during COVID-19: evidence from two longitudinal studies. J Affect Disord. 2021;291:1–8. doi: 10.1016/j.jad.2021.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yao R., Wu W. Mental disorders associated with COVID-19 related unemployment. Appl Res Qual Life. 2021;17(2):949–970. doi: 10.1007/s11482-021-09950-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Badellino H., Gobbo M.E., Torres E., et al. ‘It's the economy, stupid’: lessons of a longitudinal study of depression in Argentina. Int J Soc Psychiatry. 2022;68:384–391. doi: 10.1177/0020764021999687. [DOI] [PubMed] [Google Scholar]
- 11.Racine N., McArthur B.A., Cooke J.E., Eirich R., Zhu J., Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175(11):1142–1150. doi: 10.1001/jamapediatrics.2021.2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Compton M.T., Shim R.S. The social determinants of mental health. Focus. 2015;13:419–425. doi: 10.1176/appi.focus.20150017. [DOI] [Google Scholar]
- 13.Binagwaho A., Senga J. Children and adolescent mental health in a time of COVID-19: a forgotten priority. Ann Glob Health. 2021;87:1–5. doi: 10.5334/aogh.3330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adegboye D., Williams F., Collishaw S., et al. Understanding why the COVID-19 pandemic-related lockdown increases mental health difficulties in vulnerable young children. JCPP Adv. 2021;1(1):e12005. doi: 10.1111/jcv2.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conger R.D., Conger K.J., Elder G.H., et al. A family process model of economic hardship and adjustment of early adolescent boys. Child Dev. 1992;63:526–541. doi: 10.1111/j.1467-8624.1992.tb01644.x. [DOI] [PubMed] [Google Scholar]
- 16.Neppl T.K., Senia J.M., Donnellan M.B. Effects of economic hardship: testing the family stress model over time. J Fam Psychol. 2016;30:12–21. doi: 10.1037/fam0000168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barch D.M., Albaugh M.D., Avenevoli S., et al. Demographic, physical, and mental health assessments in the adolescent Brain and cognitive development study: rationale and description. Dev Cogn Neurosci. 2018;32:55–66. doi: 10.1016/j.dcn.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kiss O., Alzueta E., Yuksel D., et al. The pandemic's toll on young adolescents: prevention and intervention targets to preserve their mental health. J Adolesc Health. 2022;70:387–395. doi: 10.1016/j.jadohealth.2021.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yip S.W., Jordan A., Kohler R.J., Holmes A., Bzdok D. Multivariate, transgenerational associations of the COVID-19 pandemic across minoritized and marginalized communities. JAMA Psychiatry. 2022;79:350–358. doi: 10.1001/jamapsychiatry.2021.4331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiao Y., Yip P.S., Pathak J., Mann J.J. Association of social determinants of health and vaccinations with child mental health during the COVID-19 pandemic in the US. JAMA Psychiatry. 2022;79(6):610–621. doi: 10.1001/JAMAPSYCHIATRY.2022.0818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shim R.S. Mental health inequities in the context of COVID-19. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.20104. [DOI] [PubMed] [Google Scholar]
- 22.Hamilton C.M., Strader L.C., Pratt J.G., et al. The PhenX toolkit: get the most from your measures. Am J Epidemiol. 2011;174:253–260. doi: 10.1093/aje/kwr193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moore T.M., Visoki E., Argabright S.T., et al. The exposome and its associations with broad mental and physical health measures in early adolescence. medRxiv [pre-print] 2021 doi: 10.1101/2021.08.11.21261918. [DOI] [Google Scholar]
- 24.Venables W., Ripley B. 4th ed. Springer; New York: 2002. Modern applied statistics with S. [DOI] [Google Scholar]
- 25.Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48(2):1–36. [Google Scholar]
- 26.Liu Y., Merritt D.H. Familial financial stress and child internalizing behaviors: the roles of caregivers' maltreating behaviors and social services. Child Abuse Negl. 2018;86:324–335. doi: 10.1016/j.chiabu.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Rizeq J., Korczak D.J., Cost K.T., et al. Vulnerability pathways to mental health outcomes in children and parents during COVID-19. Curr Psychol. 2021;1:1–11. doi: 10.1007/s12144-021-02459-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Main G., Montserrat C., Andresen S., Bradshaw J., Lee B.J. Inequality, material well-being, and subjective well-being: exploring associations for children across 15 diverse countries. Child Youth Serv Rev. 2019;97:3–13. [Google Scholar]
- 29.Rees G., Savahl S., Lee B.J., Casas F. 2020. Children's views on their lives and well-being in 35 countries: a report on the Children's Worlds study, 2016-19. Jerusalem, Israel. [Google Scholar]
- 30.Lai J., Widmar N.O. Revisiting the digital divide in the COVID-19 era. Appl Econ Perspect Policy. 2021;43:458–464. doi: 10.1002/aepp.13104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.