Abstract
Objectives
To assess in the Italian general adult population the trends of blood pressure (BP) and prevalence of raised BP (RBP), hypertension and its control in order to evaluate population health and care, and the achievement of an RBP 25% relative reduction as recommended by the WHO at population level.
Design
Results comparison of health examination surveys, cross-sectional observational studies based on health examination of randomly selected age and sex stratified samples including residents aged 35–74 years. Data of the 2018/2019 survey were compared with the previous ones collected in 1998/2002 and 2008/2012.
Setting
Health examination surveys conducted in Italy within the CUORE Project following standardised methodologies.
Participants
2985 men and 2955 women examined in 1998/2002, 2218 men and 2204 women examined in 2008/2012 and 1031 men and 1066 women examined in 2018/2019.
Primary and secondary outcome measures
Age-standardised mean of BP, prevalence of RBP (systolic BP and/or diastolic BP ≥140/90 mm Hg), hypertension (presenting or being treated for RBP) and its awareness and control, according to sex, age class and educational level.
Results
In 2018/2019, a significant reduction was observed in systolic BP and diastolic BP in men (1998/2002: 136/86 mm Hg; 2008/2012: 132/84 mm Hg; and 2018/2019: 132/78 mm Hg) and women (132/82 mm Hg, 126/78 mm Hg and 122/73 mm Hg), and in the prevalence of RBP (50%, 40% and 30% in men and 39%, 25% and 16% in women) and of hypertension (54%, 49% and 44% in men and 45%, 35% and 32% in women). Trends were consistent by age and education attainment. In 2018/2019, hypertensive men and women with controlled BP were only 27% and 41%, but a significant favourable trend was observed.
Conclusions
Data from 2018/2019 underlined that RBP is still commonly observed in the Italian population aged 35–74 years, however, the WHO RBP target at that time may be considered met.
Keywords: Epidemiology, Hypertension, PUBLIC HEALTH
Strengths and limitations of this study.
Use of blood pressure measurements to estimate mean of blood pressure and the prevalence of raised blood pressure and hypertension.
Recruitment of randomly selected age and sex specific samples of residents in 10 Italian regions with coverage of the Northern, Central and Southern Italian territory.
Adoption of standardised procedures and methods to collect data in the three health examination surveys.
Assessment of blood pressure indicators by sex, age-classes and educational levels.
Inadequacy of blood pressure measurement in a single day for the diagnosis of raised blood pressure and hypertension.
Introduction
Raised blood pressure (RBP) is a condition constituting a leading cause of premature death and disability worldwide, since it significantly increases the risk of heart attack, stroke, kidney failure, dementia and blindness.1 The main contributors to RBP are unhealthy eating behaviours—among which sodium excess—physical inactivity, excess of weight, smoking habit, harmful use of alcohol and exposure to persistent stress.2
The value of BP, in particular of systolic BP (SBP), is included in the risk charts for estimating the probability of incurring or dying from a cardiovascular event, both for the strong aetiological significance and for its simplicity and low cost.3–5
To combat global mortality from non-communicable diseases (NCDs), at the Sixty-sixth World Health Assembly in 2013 Member States developed a Global Plan of Action, for 2013–2020 setting global targets that include achieving a 25% relative reduction in the prevalence of RBP or contain the prevalence of RBP, according to national circumstances by 2025, proposed to leading a 33% of the relative reduction by 2030, using 2010 as a baseline.6 7 The WHO is supporting countries to meet this global target and to reduce hypertension as part of WHO’s Thirteenth General Programme of Work (2019–2023), which focuses on measurable impacts on people’s health at country level.
In the Italian adult population, within regional studies using several methodologies and definitions, high prevalence of RBP was found since the 1970s and the 1980s when it resulted just over 50% for those aged 35–69 years.8–12
Integrated NCDs programmes implemented through a primary healthcare approach are an affordable and sustainable way for countries to tackle hypertension. In Italy, the prevention of NCDs is supported by the ‘Gaining Health: making healthy choices easy’ Programme and the National Preventive Plans (NPPs), which were implemented in a context in which NCDs were estimated to account for 91% of all deaths in the period 2000–2016,13 with a decreasing trend of premature death from 2000 to 2016 for both men and women aged between 30 and 70 years.
WHO recommended improving country-level surveillance and monitoring as a top priority in the fight against NCDs, also providing data disaggregated by age, gender and socioeconomic groups.14 15 Monitoring should provide internationally comparable assessments of the trends in NCDs and related risk factors over time, help to benchmark the situation in individual countries versus others in the same region or development category and provide a foundation for advocacy, policy development and coordinated action.14 Age-standardised prevalence of RBP among adults and mean SBP are among the 25 indicators suggested by the WHO in order to monitor global and national progress in the prevention and control of NCDs.15
This study aimed to assess temporal trends for mean values of BP and heart rate measurements, and for prevalence of RBP, hypertension, awareness and control of hypertension in the Italian population aged 35–74 years, according to sex, age class, educational level and region using data measured within the CUORE Project national health examination surveys (HESs) 1998–2002, 2008–2012 and 2018–2019.
Methods
Study design
Three HESs were conducted in Italy within the CUORE Project. The first survey was conducted from May 1998 to December 2002 in all Italian regions, enrolling a random sample of 100 men and 100 women aged 35–74 years for every 1.5 million inhabitants (participation rate 50%). The second survey was conducted from March 2008 to July 2012, investigating a random sample of 110 men and 110 women aged 35–79 years for every 1.5 million residents in all Italian regions (participation rate 53%). The third survey was conducted from April 2018 to December 2019, in 10 regions (out of 20) chosen in the Northern, Central and Southern Italy, using a random sample of 100 men and 100 women aged 35–74 years in each examined region (participation rate 40%). Within the three HESs, probability samples included persons randomly selected from resident registries through stratification by sex and age group (35–44, 45–54, 55–64, 65–74, 75–79).
The three HESs were conducted by the Italian National Institute of Health (Istituto Superiore di Sanità); the first and second surveys in collaboration with the national scientific association of hospital cardiologists (ANMCO - Associazione Nazionale Medici Cardiologi Ospedalieri) and its foundation (Fondazione per il Tuo cuore - Heart Care Foundation). Survey details were published elsewhere.16–19 The three HESs are recognised within the Italian National Statistical Program. The second and third surveys were also recognised within the European HES collaboration.20 21
Study procedures and methods
The CUORE Project HESs used international standardised procedures and methods for the data collection and measurements.16–19
BP measurements were performed applying the appropriate cuff to the right arm, while the participant was in a sitting position after 5 min at rest. During the 1998–2002 and 2008–2012 HES, SBP and diastolic BP (DBP) were identified at the beginning of the first and fifth phase of the Korotkoff sounds using a mercury sphygmomanometer; during the 2018–2019 HES an oscillometric device (Omron HEM-907) was used. Two consecutive readings were recorded in the first survey and three consecutive readings were recorded in the second and third surveys, 1 min apart. Heart rate was measured at the wrist between the first and the second measurements; it was measured at the right wrist by placing the middle fingers of the left hand on it to locate the radial artery—when a pulse was found, the number of beats felt within a 1-min period was counted using a stopwatch as time references. The presence of a previous diagnosis of hypertension was collected by a standardised questionnaire, as well as information on pharmacological treatment; the first was investigated by asking if any doctor or other healthcare operator had previously indicated that the BP was high, the second by asking if in the last 2 weeks they had taken medications prescribed by a doctor to lower BP and by checking the boxes of the drugs being used.
Patient and public involvement
It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research.
Statistical analysis
The statistical comparison of the 1998–2002, 2008–2012 and 2018–2019 CUORE Project HESs data included 35–74 years old residents in 10 regions, distributed in Northern, Central and Southern Italy, involved in all the surveys: Piedmont, Lombardy, Liguria, Emilia Romagna, Tuscany, Lazio, Abruzzo, Basilicata, Calabria and Sicily.
The average of the first and second BP measurement was used for the statistical analysis. As suggested by the WHO, RBP was defined as SBP ≥140 mm Hg and/or DBP ≥90 mm Hg.6 15 Hypertensives were defined as those with SBP ≥140 mm Hg and/or DBP ≥90 mm Hg or under specific pharmacological treatment and were divided into groups of ‘undiagnosed’, ‘diagnosed but untreated’, ‘uncontrolled’ (treated and SBP ≥140 mm Hg and/or DBP ≥90 mm Hg) and ‘controlled’ (treated and SBP <140 mm Hg and DBP <90 mm Hg). The European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) also consider these cut-off values of RBP and hypertension.22
Educational level was selected as a proxy of socioeconomic level; social class was dichotomised as those with primary/middle school attainment (≤8 years, lower education) and high school/university degree (>8 years, higher education).
Mean, SD and 95% CI of SBP, DBP (in all participants and in those not under treatment for hypertension) and heart rate, as well as prevalence and 95% CI of RBP, hypertension and its awareness and control were assessed by sex, age group (35–44, 45–54, 55–64 and 65–74 years) and periods and, for those with available information, by educational level.
Following the suggestion reported in the WHO Global NCDs Action Plan 2013–2020,6 10 indicators, where appropriate, were age standardised using the direct method, referring to the age-specific and sex-specific distributions of the Italian adult population in 2000, 2010 and 2019 (Italian National Institute of Statistics - ISTAT), for the 1998–2002, 2008–2012 and 2018–2019 HESs, respectively.23 Data were also age standardised using the European Standard Population 2013 for international comparisons.24
Indicators assessed in the most recent period, 2018–2019, were compared with those of previous periods, 1998–2002 and 2008–2012. The associations between indicators and age class and educational level were also assessed within periods. Regarding continuous indicators, a t-test was used to compare indicators means between periods, and analysis of variance was used to compare them within periods by age class and educational level. Regarding categorical indicators, the χ2 test was used to compare prevalence indicators between periods and, within periods, by age class and educational level. Comparisons of indicators between periods were also conducted, adjusting by age and educational level, using linear (for continuous indicators) and logistic (for categorical indicators) regression models, considering indicators as dependent variables, and period (2018–2019/1998–2002 or 2018–2019/2008–2012), age (35–54/55–74 years) and educational level (high/low) as independent variables; the statistical significance of the period was reported in tables. Two-sided p values<0.05 were considered statistically significant. Statistical analyses were performed using SAS software, release 9.4.
Results
After the exclusions of persons with missing data for SBP or DBP or use of specific drug treatments (8 persons in 1998, 18 in 2008 and 9 in 2018), 2985 men and 2955 women (mean age±SD: men 55±11 and women 54±11), 2218 men and 2204 women (mean age±SD: men 55±11 and women 55±11) and 1031 men and 1066 women (mean age±SD: men 55±11 and women 55±11) were included in the analysis of the 1998–2002, 2008–2012 and 2018–2019 HESs, respectively (online supplemental table S1).
bmjopen-2022-064270supp001.pdf (3.4MB, pdf)
BP and heart rate measurements
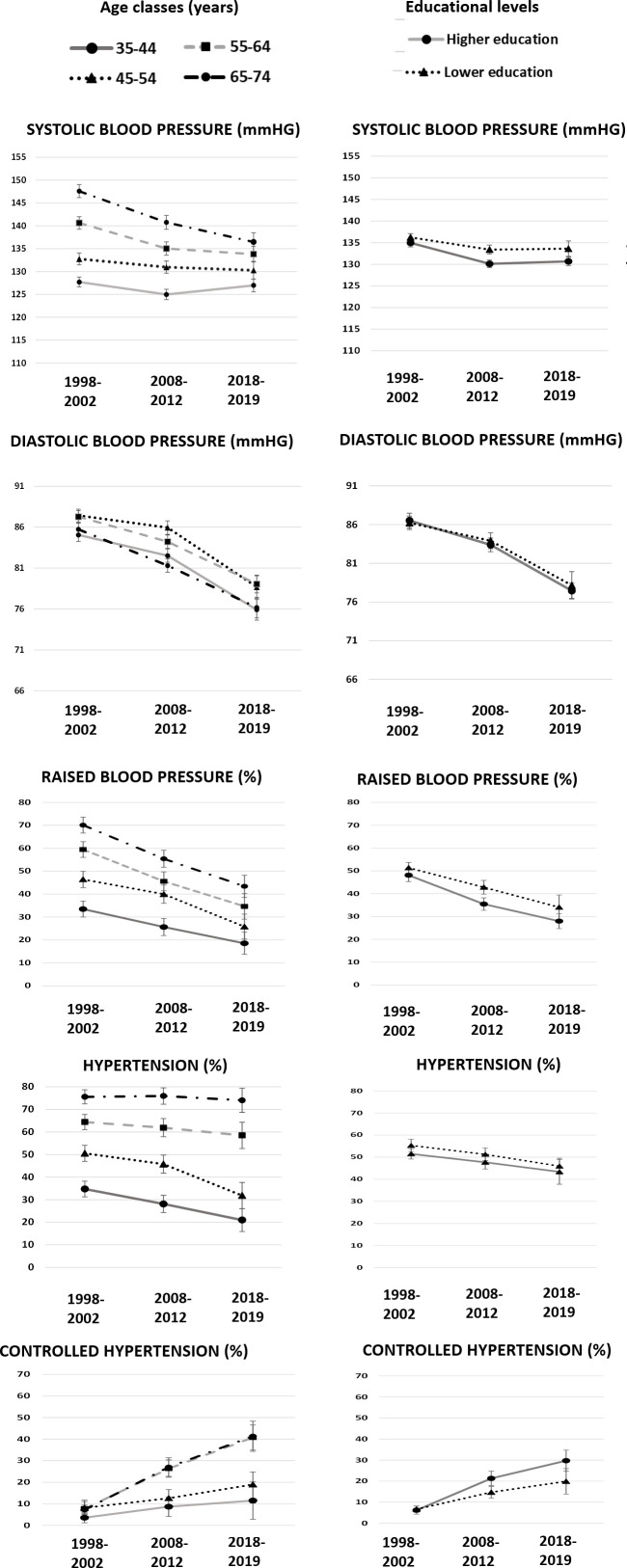
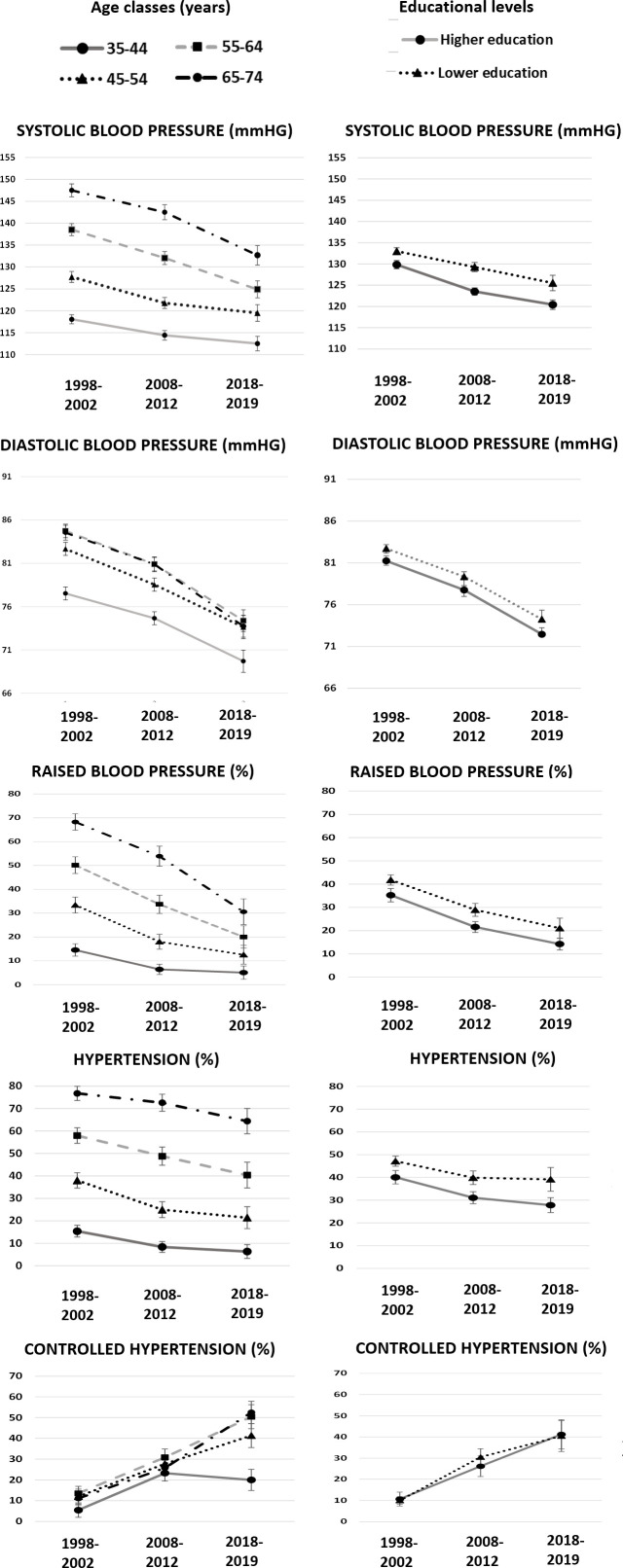
The evaluation of the temporal trend of the mean BP shows in the period 2018–2019 as compared with 20 years before a significant reduction in SBP and DBP in both men (132/78 mm Hg in 2018–2019 with a 3% of reduction for SBP and 10% of reduction for DBP) and women (122/73 mm Hg, with a reduction of 7% and 11%, respectively), while in the period 2018–2019 compared with 10 years earlier, a reduction in mean SBP is observed only in women (3%), being stable in men, and in mean DBP both in men and women (7%) (table 1). Similar trends are also observed for those not under antihypertensive drugs, and by age groups and education level (table 1, online supplemental tables S2–S5, figures 1 and 2).
Table 1.
Age-standardised blood pressure and heart rate measurements and prevalence of blood pressure treatment, raised blood pressure, hypertension and state of hypertension control by sex and period. Men and women residing in Italy aged 35–74 years, the CUORE Project Surveys 1998–2002, 2008–2012 and 2018–2019
| Men | ||||||||||||||||||
| 1998–2002 | 2008–2012 | 2018–2019 | 2018–2019 vs 1998–2002 | 2018–2019 vs 2008–2012 | ||||||||||||||
| n=2985 | n=2218 | n=1031 | ||||||||||||||||
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Diff | T-test sign* | Regression sign† | Diff | T-test sign* | Regression sign† | ||||
| SBP (mm Hg) | 136 | 18 | 135 | 136 | 132 | 16 | 131 | 132 | 132 | 14 | 131 | 132 | −4 | *** | *** | −0.3 | ns | ns |
| DBP (mm Hg) | 86 | 11 | 86 | 87 | 84 | 10 | 83 | 84 | 78 | 10 | 77 | 78 | −9 | *** | *** | −6 | *** | *** |
| SBP not under drug treatment (mm Hg) | 134 | 17 | 133 | 134 | 130 | 15 | 129 | 131 | 131 | 14 | 130 | 132 | −3 | *** | ** | 1 | ns | ns |
| DBP not under drug treatment (mm Hg) | 85 | 10 | 85 | 86 | 83 | 10 | 83 | 84 | 77 | 10 | 76 | 78 | −9 | *** | *** | −6 | *** | *** |
| Heart rate (beats per minute) | 66 | 11 | 66 | 66 | 68 | 10 | 68 | 69 | 72 | 12 | 71 | 72 | 6 | *** | *** | 3 | *** | *** |
| % | 95% CI | % | 95% CI | % | 95% CI | Diff | χ2 sign | Logistic sign | Diff | χ2 sign | Logistic sign | |||||||
| Blood pressure drug treatment | 19 | 17 | 20 | 24 | 22 | 26 | 25 | 23 | 28 | 7 | *** | *** | 1 | ns | ns | |||
| Raised blood pressure | 50 | 48 | 52 | 40 | 38 | 42 | 30 | 27 | 32 | −20 | *** | *** | −10 | *** | *** | |||
| Hypertension | 54 | 52 | 55 | 49 | 47 | 52 | 44 | 41 | 47 | −9 | *** | *** | −5 | ** | ** | |||
| Hypertension | ||||||||||||||||||
| Undiagnosed | 53 | 51 | 56 | 40 | 37 | 42 | 36 | 32 | 41 | −17 | *** | *** | −3 | ns | ns | |||
| Diagnosed but untreated | 15 | 14 | 17 | 19 | 16 | 21 | 14 | 11 | 18 | −1 | ns | ns | −4 | * | ns | |||
| Uncontrolled | 25 | 23 | 27 | 25 | 22 | 27 | 22 | 19 | 26 | −2 | ns | ** | −2 | ns | * | |||
| Controlled | 6 | 5 | 8 | 17 | 15 | 19 | 27 | 23 | 31 | 20 | *** | *** | 10 | *** | *** | |||
| Women | ||||||||||||||||||
| 1998–2002 | 2008–2012 | 2018–2019 | 2018–2019 vs 1998–2002 | 2018–2019 vs 2008–2012 | ||||||||||||||
| n=2955 | n=2204 | n=1066 | ||||||||||||||||
| Mean | SD | 95% CI | Mean | SD | 95% CI | Mean | SD | 95% CI | Diff | T-test sign* | Regression sign† | Diff | T-test sign | Regression sign | ||||
| SBP (mm Hg) | 132 | 18 | 131 | 132 | 126 | 16 | 125 | 127 | 122 | 16 | 121 | 123 | −10 | *** | *** | −4 | *** | *** |
| DBP (mm Hg) | 82 | 10 | 82 | 82 | 78 | 9 | 78 | 79 | 73 | 11 | 72 | 74 | −9 | *** | *** | −6 | *** | *** |
| SBP not under drug treatment (mm Hg) | 129 | 16 | 128 | 129 | 124 | 15 | 123 | 124 | 120 | 15 | 119 | 121 | −9 | *** | *** | −4 | *** | *** |
| DBP not under drug treatment (mm Hg) | 81 | 10 | 80 | 81 | 78 | 9 | 77 | 78 | 72 | 10 | 71 | 73 | −9 | *** | *** | −6 | *** | *** |
| Heart rate (beats per minute) | 70 | 11 | 69 | 70 | 71 | 9 | 71 | 71 | 73 | 10 | 72 | 73 | 3 | *** | *** | 2 | *** | *** |
| % | 95% CI | % | 95% CI | % | 95% CI | Diff | χ2 sign | Logistic sign | Diff | χ2 sign | Logistic sign | |||||||
| Blood pressure drug treatment | 22 | 20 | 23 | 22 | 20 | 24 | 23 | 20 | 25 | 1 | ns | ** | 1 | ns | ns | |||
| Raised blood pressure | 39 | 38 | 41 | 25 | 24 | 27 | 16 | 14 | 19 | −23 | *** | *** | −9 | *** | *** | |||
| Hypertension | 45 | 43 | 46 | 35 | 33 | 37 | 32 | 29 | 34 | −13 | *** | *** | −4 | * | ns | |||
| Hypertension | ||||||||||||||||||
| Undiagnosed | 44 | 42 | 47 | 32 | 28 | 35 | 28 | 23 | 32 | −17 | *** | *** | −4 | ns | ** | |||
| Diagnosed but untreated | 16 | 14 | 18 | 16 | 13 | 18 | 15 | 12 | 19 | −0.4 | ns | ** | −0.4 | ns | ns | |||
| Uncontrolled | 30 | 27 | 32 | 26 | 23 | 29 | 16 | 13 | 20 | −13 | *** | *** | −10 | ** | ** | |||
| Controlled | 10 | 9 | 12 | 27 | 24 | 30 | 41 | 36 | 46 | 31 | *** | *** | 14 | *** | *** | |||
Diff: mean or percentage difference between 2018–2019 and 1998–2002 or 2018–2019 and 2008–2012; the values are approximated taking into account the first decimal of means or prevalence.
Means, SDs and prevalence were age-standardised by Italian National Institute of Statistics - ISTAT Italian population 2000, 2010, and 2019, respectively.
*T-test to compare mean values between periods; χ2 test to compare prevalence between periods.
†Linear regression and logistic models were assessed considering indicators as dependent variable and period (2018–2019/1998–2002 or 2018–2019/2008–2012), age (35–54/55–74 years) and educational level (high/low) as independent variables; the statistical significance of the period was reported.
*p<0.05; **p<0.01; ***p<0.0001; ns, not significant p value.
Raised blood pressure: SBP ≥140 mm Hg or DBP ≥90 mm Hg. Hypertension: SBP ≥140 mm Hg or DBP ≥90 mm Hg and/or under specific pharmacological treatment. Hypertension is divided into ‘undiagnosed, ‘diagnosed but untreated’, ‘uncontrolled’ (treated and SBP ≥140 mm Hg or DBP ≥90 mm Hg) and ‘controlled’ (treated and SBP <140 mmHg and DBP <90 mmHg).
Pool of the following Italian regions: Piedmont, Lombardy, Liguria, Emilia Romagna, Tuscany, Lazio, Abruzzo, Basilicata, Calabria and Sicily.
DBP, diastolic blood pressure; SBP, systolic blood pressure.
Figure 1.
Mean of blood pressure and prevalence of raised blood pressure, hypertension and controlled hypertension based on measurements, by age class, educational level and period. Italian resident men aged 35–74 years, the CUORE Project Surveys 1998–2002, 2008–2012 and 2018–2019. Bars refer to 95% CIs. Statistics by educational level were age-standardised by Italian National Institute of Statistics - ISTAT Italian population 2000, 2010 and 2019, respectively. Higher education—high school or college; lower education—primary or middle school. Raised blood pressure: systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg. Hypertension: systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or under specific pharmacological treatment. Controlled hypertension: under drug treatment for hypertension with systolic blood pressure <140 mm Hg and diastolic blood pressure <90 mm Hg. Pool of the following Italian Regions: Piedmont, Lombardy, Liguria, Emilia Romagna, Tuscany, Lazio, Abruzzo, Basilicata, Calabria and Sicily.
Figure 2.
Mean of blood pressure and prevalence of raised blood pressure, hypertension and controlled hypertension based on measurements, by age class, educational level and period. Italian resident women aged 35–74 years, the CUORE Project Surveys 1998–2002, 2008–2012 and 2018–2019. Bars refer to 95% CIs. Statistics by educational level were age-standardised by Italian National Institute of Statistics - ISTAT Italian population 2000, 2010 and 2019, respectively. Higher education—high school or college; lower education—primary or middle school. Raised blood pressure: systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg. Hypertension: systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or under specific pharmacological treatment. Controlled hypertension: under drug treatment for hypertension with systolic blood pressure <140 mm Hg and diastolic blood pressure <90 mm Hg. Pool of the following Italian Regions: Piedmont, Lombardy, Liguria, Emilia Romagna, Tuscany, Lazio, Abruzzo, Basilicata, Calabria and Sicily.
Within the 1998, 2008 and 2018 periods, mean SBP and DBP was higher in men than in women, regardless of antihypertensive drug treatment use, class of age and educational level, although not always statistically significant, especially in the 1998–2002 period considering that the difference increased progressively over time, passing from 3% in 1998–2002 to 4% in 2008–2012 until it reached 8% in 2018–2019 (table 1, online supplemental tables S2–S5, figures 1 and 2). Within those periods, in both men and women, mean SBP and DBP, regardless of antihypertensive drug treatment use, progressively increased by age group and was tendentially higher in those with a lower level of education, except DBP in men (online supplemental tables S2–S5). The mean SBP difference between educational levels increased progressively in the 1998, 2008 and 2018 periods in both men and women (men: 2%, 3% and 4% and women: 7%, 8% and 12%) (online supplemental tables S4, S5, figures 1 and 2).
The mean heart rate was progressively increasing in the three survey periods, both in men and women, in all age groups and education levels, remaining between 66 and 74 beats per minute. Within the 1998, 2008 and 2018 periods, no significant differences are observed in the mean heart rate by age group, with the exception of women in 1998–2002 for whom it decreases starting from 55 years; there are no differences between levels of education with the exception of men in 2018–2019 for whom there is an average level of heart rate higher in the lowest level of education.
Hypertension drug treatment, RBP and hypertension
The prevalence of antihypertensive drug treatment use in men showed a significant increase by 7% in 2018–2019 compared with 20 years earlier, it remained stable for men compared with 10 years earlier and for women in the three survey periods (table 1), however a significant increase was observed in 2018–2019 compared with 20 years earlier in men aged 55 years and over and women aged 65 years and over (online supplemental tables S6, S7). The general increase in the use of antihypertensive drug treatment in men was especially observed among those with higher education level; in women, a generally stable prevalence was observed regardless of education level (online supplemental tables S8, S9). Antihypertensive drug treatment use was higher in men than in women in 1998–2002, and reached more similar values between men (25%) and women (23%) in 2018–2019.
The prevalence of RBP was 30% in men and 16% in women in 2018–2019, significantly decreased compared with 20 and 10 years earlier: in men it decreased by 20% and 10%, respectively, and in women 23% and 9%, respectively (table 1). The decreasing trend of RBP was progressively higher by age classes, reaching, in 2018–2019 compared with 1998–2002, the 27% in men and 38% in women aged 65–74 years, while it was similar between educational levels both in men and women (online supplemental tables S6–S9, figures 1 and 2).
The prevalence of hypertension was 44% in men and 32% in women in the 2018–2019, significantly decreased compared with 20 and 10 years earlier: in men it decreased by 9% and 5%, respectively, and in women 13% and 4%, respectively (table 1); in men the decrease was observed among those aged 35 to 54 years both compared with 20 and 10 years earlier, in women in all age groups compared with 20 years earlier, while from 55 to 74 years of age compared with the previous 10 years; similar decreasing trend was observed between educational levels with a more favourable trend among more educated women (online supplemental tables S6–S9, figures 1 and 2).
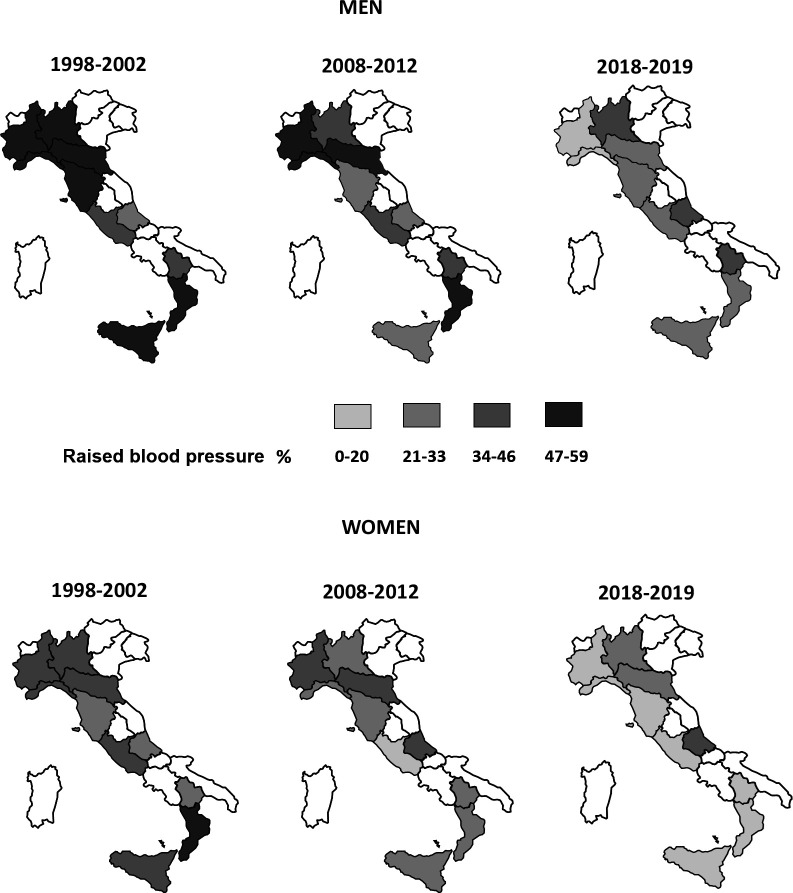
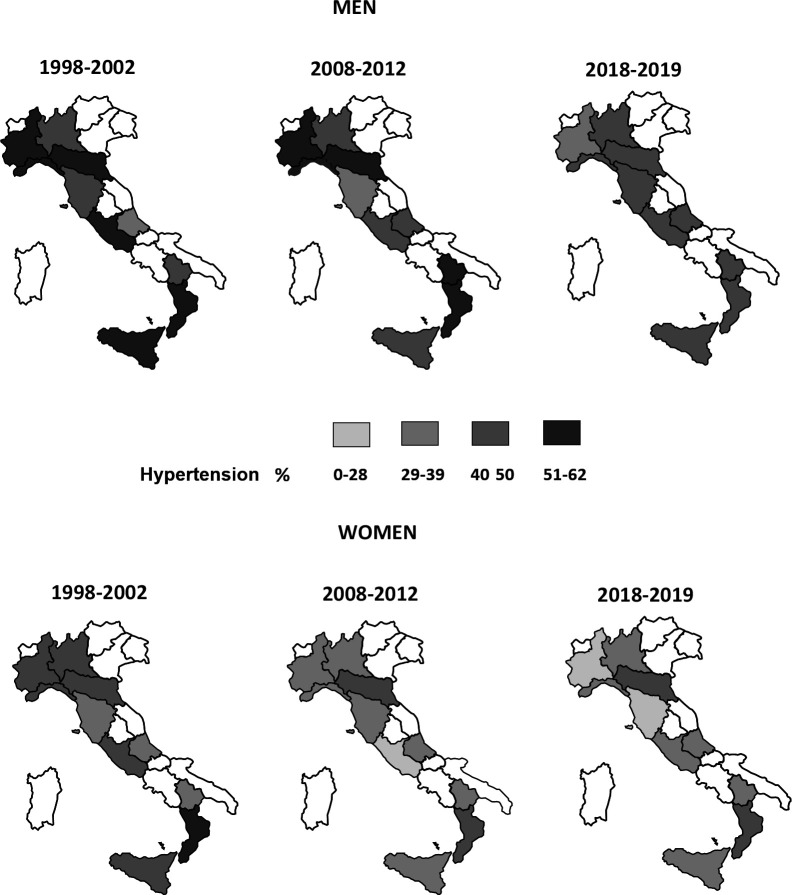
As expected, within periods, both in men and women, prevalence of RBP and hypertension significantly increased by age group and was tendentially higher in those with a lower level of education (online supplemental tables S6–S9, figures 1 and 2). Prevalence of RBP and hypertension decreased or remained stable in all Italian regions both in men and women (figures 3 and 4, and online supplemental table S10).
Figure 3.
Prevalence of raised blood pressure based on measurements, by sex, regions and period. Italian resident men and women aged 35–74 years, the CUORE Project Surveys 1998–2002, 2008–2012 and 2018–2019. Italian regions: Piedmont, Lombardy, Liguria, Emilia Romagna, Tuscany, Lazio, Abruzzo, Basilicata, Calabria and Sicily. Prevalences were age-standardised by Italian National Institute of Statistics - ISTAT Italian population 2000, 2010 and 2019, respectively. Raised blood pressure: systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg.
Figure 4.
Prevalence of hypertension based on measurements, by sex, regions and period. Italian resident men and women aged 35–74 years, the CUORE Project Surveys 1998–2002, 2008–2012 and 2018–2019. Italian regions: Piedmont, Lombardy, Liguria, Emilia Romagna, Tuscany, Lazio, Abruzzo, Basilicata, Calabria and Sicily. Prevalences were age-standardised by Italian National Institute of Statistics - ISTAT Italian population 2000, 2010 and 2019, respectively. Hypertension: systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg and/or under specific pharmacological treatment.
Awareness and control of hypertension
In 2018–2019, prevalence of undiagnosed hypertension resulted in 36% and 28% of hypertensive men and women, with a decreasing trend of 17% in comparison with 20 years earlier both in men and women and 3–4% in comparison with 10 years earlier (table 1); these trends were found in particular in those aged 45 years and over and were similar by educational level, with some advantage in women with higher education (online supplemental tables S6–S9). Within periods, both in men and women, prevalence of undiagnosed hypertension was higher among younger men and women but similar between educational levels (online supplemental tables S6–S9).
Prevalence of not controlled hypertension was found to be halved in women, from 30% of 1998–2002 to 16% in 2018–2019 (table 1); favourable, but much more contained, trend was found in men with a reduction of 2% (table 1). Within periods, both in men and women, prevalence of uncontrolled hypertension was found increasing by age classes and tendentially higher in those with lower educational level (online supplemental tables S6–S9).
Although in 2018–2019 only 27% of hypertensive men and 41% of hypertensive women had their BP under control, a positive growth trend of hypertension under control was observed both in men and women, with an increase in 2018–2019, compared with 20 years earlier, of 20% in men and 31% in women (10% and 14%, respectively, compared with 10 years earlier) (table 1). An important increase was observed in men from the age of 55 years and in women in all age groups; similar trend for more or less educated men, while a more favourable trend is observed among more educated women (online supplemental tables S6–S9, figures 1 and 2). In 2008–2012 and 2018–2019, in men, prevalence of controlled hypertension increased by age classes (in women only in the last survey), and in the latter two surveys it is higher in men with higher education levels (online supplemental tables S6–S9).
Results, age standardised according to the European standard population 2013, are available in online supplemental tables S11–S15.
Discussion
Data of measured BP in random samples of the general Italian population aged 35–74 years during three HESs conducted in 1998–2002, 2008–2012 and 2018–2019, showed a significant reduction, in 2018–2019 compared with 20 years earlier, of SBP and DBP mean levels and prevalence of RBP and hypertension. The reductions were consistent with respect to sex, age classes and education level and were detected to different extents in almost all Italian regions. This favourable decline in mean BP and in the prevalence of RBP and hypertension was observed in 2018–2019 even when compared with 10 years earlier, except for mean SBP in men which was stable. Although around 7 out of 10 men and 6 out of 10 women with RBP still in 2018–2019 did not have their BP under control (because it is not diagnosed, diagnosed but not treated or treated but not under control), an important increase in RBP control was observed in 2018–2019 compared with 20 years earlier, for men mostly due to a decrease in the prevalence of undiagnosed high BP and for women also due to a reduction in the prevalence of uncontrolled RBP.
These results, which to our knowledge are based on the most recent national measured data on Italian general adult population, responds to the WHO’s request to provide information on effectiveness of national policies and strategies, showing, in relation to the objective indicated in the Global Action Plan 2013–2020 (25% relative reduction in the prevalence of RBP or containment of the prevalence of RBP by 2025, proposed leading to a 33% of relative reduction by 2030), a significant decline from 1998–2020 to 2018–2019 in the prevalence of RBP, from 50% to 30% in men and from 39% to 16% in women, equal to a relative reduction of 41% and 58%, respectively, and also a significant decline from 2008–2012 to 2018–2019, from 40% to 30% in men and from 25% to 16% in women, equal to a relative reduction of 25% and 36%, respectively.6
Mean values of SBP and DBP, as well as prevalence of RBP trends are consistent with those of other studies conducted in the Italian adult population. NCD Risk Factor Collaboration, that pooled data of population-based studies with measured BP in adults aged 18 years and older from 200 countries, showed that within the 36 Italian surveys (at community, subnational and national levels, including the CUORE Project surveys 1998–2002 and 2008–2012), mean values of SBP and DBP, as well as prevalence of RBP decreased during 1995–2015 period.25 26
In some other European countries, such as UK, Switzerland, Spain, Sweden, Norway, Netherlands, Luxemburg, Ireland, Germany, France, Finland, Belgium and Austria, a decline of BP levels was also observed with various intensities both in men and women, while in other countries, mainly from Eastern Europe, such as Slovenia, Slovakia, Serbia, Romania, Poland, Lithuania, Hungary, Greece, Czech Republic and Portugal, a trend of decline was observed in women and a stable or slightly increasing trend in men; in other countries, such as Moldova, Croatia, Bosnia and Herzegovina and Albania, a stable or an increasing trend is still ongoing both in men and women.25 26
High-income countries have begun to reduce hypertension in their populations through strong public health policies such as the reduction of salt content in processed food and widely available early diagnosis and treatment that tackle hypertension and other risk factors together.2 27 Also in Italy, an explanation of the reasons why a decrease in mean BP and in the prevalence of RBP is observed in the general adult population might be on the one hand the enhancement of its early detection, treatment and control and on the other hand successful national programmes of primary prevention which have led to an increase in the normal weight prevalence and to the reduction of the daily consumption of salt in the general adult population, despite the average levels of daily potassium consumption being not yet adequate.16–18 In the last two decades, the ‘Gaining Health’ Programme and NPPs in Italy were oriented to reduce risk factors associated to the increase of BP, such as physical inactivity, excess of weight and salt consumption, as well as the smoking habit, through intersectional strategies at both population (eg, facilitating the choice of correct lifestyles) and individual levels (eg, motivational counselling and specific therapeutic groups), promoting and supporting national surveillance systems and monitoring studies, and through voluntary agreements for salt reduction in food products, school and workplace programmes, and public awareness campaigns.28 As an example, aimed directly at the diagnosis and control of RBP, in the NPP 2005–2008 the promotion of a multifactorial cardiovascular diseases (CVD) risk assessment, based also on BP measurements, and its monitoring over time in clinical practice has been explicitly included. As well as, NPP 2014–2019 also focused on the early identification and integrated assessment of persons with NCDs risk factors, to be directed towards an adequate systemic management, able to enhance personal resources for the conscious adoption of correct life, or when necessary, towards suitable multidisciplinary therapeutic and assistance paths.
Additional findings of the study, including higher level of BP and RBP/hypertension in men than in women and more severe values in the southern Italy regions and tendentially in people with lower education levels, are consistent with results from other Italian and European studies,25 26 29 and are in line with the association of excess of weight and salt consumption with gender, education level and Italian macro-area.16 17 19 30 31
As far as the favourable trend of increase in hypertension awareness, treatment and control is concerned, it could be due to the greater diffusion and compliance with the guidelines for hypertension in clinical practice that include simplified recommendations. In Italy, over the period of our analysis, the antihypertensive treatment was based on the guidelines drawn up by the ESC/ESH22 32–34 which indicated as threshold for immediate treatment BP ≥180/110 or BP of 140–179/90–109 (depending on CVD risk stratification) after lifestyle modifications, with a treatment target that has changed over time (2003: BP <140/90 mm Hg; 2007: BP <140/90 mm Hg and BP <130/80 mm Hg in high CVD risk; 2013: BP <140/90 mm Hg; 2018: DBP <80 mm Hg for all and SBP 120–129 mm Hg for persons aged <65 years or SBP 130–139 mm Hg for persons aged ≥65 years). The progressively lower thresholds for diagnosing hypertension and the beginning of treatment also may have contributed to this favourable trend based on the threshold of 140/90 mm Hg. In addition, over time, treatment efficacy and control for some patients suffering from smaller side effects of the earliest generations of drugs improved thanks to the availability of newer drugs.35
Early detection and treatment of RBP and other risk factors, as well as public health policies that reduce exposure to behavioural risk factors, have contributed to the gradual decline in mortality due to heart disease and stroke in Italy and other high-income countries over the last three decades.36 37
Strengths and limitations
Major strengths of this study are the following: the use of standardised procedures and methods to assess BP measurements, allowing objective and reliable estimates of SBP, DBP and RBP; the checking of drug boxes to assess the use of specific pharmacological treatments; a good national coverage with the enrolment of study participants from half of the Italian regions distributed in Northern, Central and Southern Italy; the random selection and the sex and age classes stratification of samples from the general population.
Conversely, we acknowledge some study limitations, which should be taken in consideration when interpreting results. First, because of the choice of urban districts for the random selection of the study participants within the surveys, the results may not be representative of the habits of the population living in rural areas. The participation rates in the surveys were lower than desirable, yet consistent, with lower contact rates occurring in more highly urbanised areas and with a decreasing trend of participation observed in HESs in other European countries.38 The cross-sectional design of the study does not allow to assess causality of the associations between SBP, DBP and RBP and educational level. There were differences in the educational level distribution between the three surveys, which is consistent with the increase of secondary and tertiary education assessed in adults from 2008 to 2017 by the Italian National Institute of Statistics.39 The use of mercury sphygmomanometer in the 1998–2002 and 2008–2012 surveys and of an oscillometric device in the 2018–2019 survey (due to the European Union regulation 847/2012 that banned the sale of mercury sphygmomanometers from 10 April 2014 onwards40) may affect comparison among surveys41; however, the oscillometric device used in HES 2018–2019 was certified according to international validation protocol to ensure that the device measures accurately in comparison with the mercury sphygmomanometer; in addition it should prevent the observer’s error due to the use of a mercury sphygmomanometer, and the common standardised protocol based on aspects such as room temperature, disturbing noises, lighting, adequacy of the table and chair for the measurement, interaction between the survey participant and the measurer, availability of different cuffs may minimise variation due to measurement technique.21 42 43 Anyway, with all device types, mercury and aneroid sphygmomanometers, and oscillometric devices, calibration error may bias the results.44 Hypertension diagnosis should be based on several BP readings taken on several occasions (at least two), as recommended by international guidelines22; however, epidemiological studies are based on BP measurement in a single visit, possibly with two or more measurements repeated during the same visit.21 45
Conclusions
BP assessment in three independent surveys on the Italian population aged 35–74 years, carried out in 10 regions approximately 10 years apart from each other, showed a significant reduction of BP mean values and prevalence of RBP and hypertension in 2018–2019 compared with 20 years earlier, with a favourable trend also observed compared with 10 years earlier. This reduction was independent of gender, age and educational level and met the 25% target for reduction/containment of the RBP prevalence indicated in the WHO Global Action Plan 2013–2020 by 2025 with baseline as 2010. Although in 2018–2019 underdiagnoses and non-control of elevated BP was still largely prevalent in Italy, a favourable trend in the control of RBP has been observed.
Although systematic and periodic monitoring are necessary to observe the trend and control of BP in the coming years, also in relation to the direct and indirect effects of the COVID-19 pandemic, these results have major public health implications in so much as they encourage the initiatives undertaken by the Italian Ministry of Health in order to contain risk factors associated to the onset of RBP at individual and population level through the ‘Gaining Health: making healthy choices easy’ Programme and the NPPs. In continuity with the NPP 2014–2019, the NPP 2020–2025 renewed the commitment to the health promotion and the prevention of NCDs by providing preventive and protective interventions according to a life-course approach and aiming at the early identification and management of persons with risk factors.
Prevention and control of RBP involve multistakeholder collaboration, such as governments, academia, the food and beverage industry and civil society. In view of the enormous public health benefits of BP control, some concerted action has been implemented and data demonstrate that the prevention of RBP is today an attainable goal.
Supplementary Material
Acknowledgments
Research Group of Osservatorio Epidemiologico Cardiovascolare/Health Examination Survey (OEC/HES) 1998–2002 and 2008–2012 within the CUORE Project for the National Institute of Health (Istituto Superiore di Sanità) ISS: LP (coordinator), CD (coordinator), Simona Giampaoli (former coordinator), CLN, SV, ADL, Francesco Dima (former). Research group of the CUORE Project OEC/HES 1998–2002 and 2008–2012 for Associazione Nazionale Medici Cardiologi Ospedalieri/Health Care Foundation (ANMCO/HCF): MMG, Furio Colivicchi and Andrea Di Lenarda (coordinators), Diego Vanuzzo (former coordinator), Domenico Gabrielli, Giuseppe Di Pasquale, Aldo Pietro Maggioni, Gian Francesco Mureddu, Carmine Riccio, Marino Scherillo, Stefano Urbinati, Pompilio Faggiano. Research Group of the Health Examination Survey (HES) 2018–2019 within the CUORE Project: CD (coordinator), LP, CLN, ADL, EP, BB, SV, Simona Giampaoli (former coordinator) (Italian National Institute Health - ISS). Local coordinators of the OEC 1998–2002 participating centres: V. Martinelli (Ospedale Civile S.S. Antonio E Biagio, Alessandria); M. Vona, M.A. (Ospedale Generale Regionale, Aosta); M.L. Biorci (Divisione Di Cardiologia, Ospedale La Colletta, Arenzano); G. Gullace, (Ospedale Umberto I, Bellano); F. Tettamanti, (Azienda Ospedaliera Sant’anna, Como); F. Avanzini, (Servizio Di Cardiologia, Ospedale Di Circolo, Desio); D. Mazzoleni, (Ospedali Riuniti, Mozzo); I. Pastine, M N (Asl 4, Rapallo); A. Pizzuti, M.A. (Ospedale Maggiore S.S. Annunziata, Savigliano); G. Cucchi (Ospedale Civile, Sondrio); M.G. Sclavo, (Centro Tramautologico Ortopedico, Torino); R. Pedretti, (Fondazione S. Maugeri Irccs, Tradate); F. Soffiantino, (Fondazione S. Maugeri Irccs, Veruno); D. Girardini, (Ospedale Civile, Ala); A. Pozzati, (Ospedale Di Bentivoglio); S. Boni, (Ospedale Civile San Biagio, Bovolone); G. Candelpergher, (Stabilimento Ospedaliero Castelfranco Veneto); E. Cremaschi, (Ospedale Civile, Guastalla); C.A. Goldoni, (Ospedale S. Agostino, Modena); F. Cioppi, (Ospedale Degli Infermi, Rimini); L. Roncon, (Presidio Ospedaliero, Rovigo); G. Zanata, (Ospedale Civile, Sacile); P. Spolaore, (Ospedale Civile, Vicenza); L. Quattrini, (Ospedale Geriatrico, Ancona); G. Schillaci, (Policlinico Universitario, Corciano); F. Cecchi, (Presidio Ospedaliero Villa Basilewsky, Firenze); C. Pagnotta, (Presidio Ospedaliero, Foligno); G. Micoli, (Ospedale Civile S. Maria Goretti, Latina); L. Iacopetti, (Ospedale Val Di Nievole, Pescia); M. Uguccioni, (Ospedale Cto A. Alesini, Roma); G. Greco, (Ospedale S. Spirito, Roma); L. Robiglio, (Ospedale Tabarracci, Viareggio); G. Chiarandà, (Ospedale Muscatello, Augusta); A.R. Mascolo, (Ospedale Umberto I, Barletta); A. Storelli, (Ospedale A. Di Summa, Brindisi); P. Maxia, (Ospedale San Michele Brotzu, Cagliari); F. Vancheri, (Ospedale S. Elia, Caltanissetta); S. Iacopino (Policlinico, Catanzaro); L. Mantini, (Ospedale Civile Renzetti, Lanciano); G. Di Mauro, (Ospedale Curteri, Mercato S. Severino); M.A. Cauteruccio, Ospedale Civile Minervini, Mormanno); P. Morra, (Azienda Ospedaliera V. Monaldi, Napoli); F. Clemenza, (Ospedale G.F. Ingrassia, Palermo); A. Lopizzo, (Ospedale Regionale San Carlo, Potenza); P. Russo, (Ospedale Santa Maria Delle Grazie, Pozzuoli); G. Neri, (Ospedali Riuniti G. Melacrino E F. Bianchi, Reggio Calabria); C. De Matteis, (Ospedale Ave, Gratia Plena, San Felice A Cangello); S. Pede, (Ospedale N. Melli, S. Pietro Vernotico); P. Furgi, (Fondazione S. Maugeri, Telese Terme); D. Staniscia, (Ospedale San Timoteo, Termoli). Local coordinators of the OEC/HES 2008-2012 participating centers: Diego Vanuzzo (Centro di Prevenzione Cardiovascolare ASS 4 “Medio Friuli”, Udine); Licia Iacoviello (Centro di ricerca e formazione ad alta tecnologia nelle scienze biomediche Giovanni Paolo II, Università Cattolica, Campobasso); Federico Vancheri (Ospedale S. Elia, Caltanissetta); Carlo Alberto Goldoni (Dipartimento di sanità pubblica, Azienda USL, Modena); Carmelo Antonio Caserta (Associazione calabrese di epatologia, Cittanova - Reggio Calabria); Antonio Lopizzo (Ospedale San Carlo, Potenza); Natalino Meloni (USL 4, Loceri - Nuoro); Marinella Gattone (Fondazione S. Maugeri, Veruno - Novara); Giuseppe Salamina (SC Centro controllo malattia, ASL TO1, Torino); Alessandro Boccanelli (Ospedale San Giovanni Addolorata, Roma); Roberto Amici (Ospedale Santa Maria della Pietà, Camerino -Macerata); Gianfranco Alunni (Ospedale SantaMaria della Misericordia, Azienda Ospedaliera, Perugia); Giuseppe Favretto (Ospedale rabilitativo di alta specializzazione, Motta di Livenza - Treviso); Mariapiera Vettori (Azienda ULSS 13 del Veneto, Noale - Venezia); Marino Scherillo (Azienda Ospedaliera G. Rummo, Benevento); Pompilio Faggiano (Azienda Ospedaliera Spedali Civili, Brescia); Maria Teresa La Rovere (Fondazione Salvatore Maugeri, Istituto di riabilitazione, Montescano - Pavia); Maria Luisa Biorci (ASL 3 Genovese- PO “La Colletta”, Arenzano - Genova); Pasquale Caldarola (Cardiologia, Ospedale di Terlizzi, Centro servizi territoriali della città, Bitonto - Bari); Giovanni Menegoni (Azienda provincial per i servizi sanitari di Trento, Presidio ospedaliero, Borgo Valsugana - Trento); Rosa Maria Teresa Cristaudo (Azienda USL della Valle d’Aosta, Aosta); Andrea Zipoli (Azienda USL 11, Ospedale San Giuseppe, Empoli - Firenze); Paolo Michele Accettura (Laboratorio analisi, Ospedale San Camillo, Atessa - Chieti). Local referents of HES 2018-2019 partecipating centers: Luigi Dell’Orso and Alessandro Grimaldi (Ospedale San Salvatore, L’Aquila); Nicola Giordano (ASL - Azienda Sanitaria Locale di Potenza, Potenza); Carmelo Caserta (Centro di Medicina Solidale – Associazione Calabrese di Epatologia, Reggio Calabria); Alessandra Fabbri (Casa della Salute AUSL RE, Montecchio Emilia); Fabrizio Ciaralli (Casa della Salute S. Caterina della Rosa, Rome); Fiorella Bagnasco (Municipality of Arenzano, Arenzano - Genova); Giuliana Rocca (ATS Bergamo); Giuseppe Salamina (ASL Città di Torino, Torino); Pietro Modesti (Università di Firenze, Florence); Federico Vancheri and Giulio Geraci (Ospedale S. Elia, Caltanissetta). Also we would to thank for HES 2018-2019: Anna Rita Ciccaglione, Cinzia Marcantonio, Roberto Bruni (ISS), Emanuele Bottosso and Anna Acampora (as trainee medical doctor at ISS), Giulia Cairella (ASL Roma 2, SINU) and Municipality of Potenza. Administrative staff of the ANMCO/HCF: Giulia Salone, Angela Petrucci, Monica Nottoli; and to Laura Bellicini and to L Bellicini, consultant lawyer of the ANMCO-HCF. Fondazione IRCCS, Istituto nazionale dei tumori, Milano: Vittorio Krogh, Sara Grioni. Research Group MINISAL-GIRCSI and MENO SALE PIU’ SALUTE: Pasquale Strazzullo, Ornella Russo, Lanfranco D’Elia, Roberto Iacone, Renato Ippolito, Enrico Agabiti-Rosei, Angelo Campanozzi, Marina Carcea, Ferruccio Galletti, Licia Iacoviello, Luca Scalfi, Alfonso Siani, Daniela Galeone, Chiara Donfrancesco, Simona Giampaoli. CARHES Research Group: Luca De Nicola, Chiara Donfrancesco, Roberto Minutolo, Cinzia Lo Noce, Luigi Palmieri, Amalia De Curtis, Licia Iacoviello, Carmine Zoccali, Loreto Gesualdo, Giuseppe Conte, Diego Vanuzzo, Simona Giampaoli. Italian Ministry of Health: Daniela Galeone, Paolo Bellisario, Giovanna Laurendi, Bianca Maria Polizzi. European Health Examination Survey, Reference Centre: Hanna Tolonen, Kari Kuulasmaa, Paivikki Koponen, Johan Heldan, Susanna Conti, Georg Alfthan. Administrative staff of the ISS: Claudia Meduri, Tiziana Grisetti, Matilde Bocci, Gabriella Martelli, Valerio Occhiodoro, Maria Grazia Carella, Francesca Meduri. We acknowledge all persons who decided to participate to the 1998–2002, 2008–2012 and 2018– 2019 surveys. A grateful thanks to Simona Giampaoli, research manager of the ISS, who founded the CUORE Project and coordinated with dedication the research activities until her retirement in 2018.
Footnotes
Contributors: Guarantor: CD. Conceptualisation: CD and LP. Methodology: CD, CLN and LP. Software: FV. Formal analysis: CD. Investigation: CD, CLN, ADL, EP and BB. Resources: CD, DG, PB, LP and MMG. Data curation: CD, CLN and LP. Writing—original draft preparation: CD. Writing—review and editing: CD, ADL, CLN, EP, BB, FV, SV, FG, GO, MMG, DG, PB, and LP. Visualisation: CD. Supervision: CD, LP and GO. Project administration: CD. Funding acquisition: CD, LP and MMG. All authors have read and agreed to the published version of the manuscript.
Funding: The Osservatorio Epidemiologico Cardiovascolare (OEC) 1998–2002 and the Osservatorio Epidemiologico Cardiovascolare/Health Examination Survey (OEC/HES) 2008–2012 within the CUORE Project were funded by the Italian Ministry of Health (MoH), by the Associazione Nazionale Medici Cardiologi Ospedalieri (ANMCO), by the Fondazione per il Tuo cuore onlus (Heart Care Foundation – HCF) and OEC/HES 2008–2012 also by the Joint Action of the European Health Examination Survey. The Health Examination Survey (HES) 2018–2019 within the CUORE Project was promoted and funded by the MoH-CCM for activities related to the CCM 2017 project—Central Actions Area—entitled ‘Monitoring of the average daily consumption of sodium in the Italian population’. The OEC 1998–2002, OEC/HES 2008–2012 and HES 2018–2019 were also funded by the Italian National Institute of Health (Istituto Superiore di Sanità - ISS) through permanent staff salary and some travel refunds.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographical or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: Italian Ministry of Health defined the needs and the use of data for evidence based policymaking and collaborated in the interpretation of results for health promotion and prevention activities and planning health services. Associazione Nazionale Medici Cardiologi Ospedalieri (ANMCO) and the Fondazione per il Tuo cuore onlus (Heart Care Foundation - HCF) had a role a role in the choice of collaborating centres, in the management of funding for the support of local centres and in the interpretation of results.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. The data are not publicly available due to ethical and legal restrictions on data sharing.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
CUORE Project health examination surveys were approved by the Ethical Committee of the Italian National Institute of Health on 11 March 2008 (Prot. PRE/150/08), 11 November 2009 (Prot. PRE/569/09) and 14 March 2018 (Prot. PRE 1176/18); all invited persons received an informative note and signed an informed consent to participate, Participants gave informed consent to participate in the study before taking part.
References
- 1.Olsen MH, Angell SY, Asma S, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet 2016;388:2665–712. 10.1016/S0140-6736(16)31134-5 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Improving hypertension control in 3 million people: country experiences of programme development and implementation, 2020. Available: https://www.who.int/publications/i/item/improving-hypertension-control-in-3-million-people-country-experiences-of-programme-development-and-implementation [Accessed 22 Feb 2022].
- 3.WHO CVD Risk Chart Working Group . World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health 2019;7:e1332–45. 10.1016/S2214-109X(19)30318-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Visseren FLJ, Mach F, Smulders YM. ESC national cardiac societies; ESC scientific document group. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021;42:3227–337. [DOI] [PubMed] [Google Scholar]
- 5.Giampaoli S, Palmieri L, et al. , on behalf of The CUORE Project Research Group . Cardiovascular risk assessment in Italy: the CUORE project risk score and risk chart. Italian Journal of Public Health 2007;4:102–9. [Google Scholar]
- 6.WHO . Global action plan for the prevention and control of noncommunicable diseases 2013-2020, 2013. [Google Scholar]
- 7.WHO Discussion Paper For The Regional Expert Consultations . Development of an implementation roadmap 2023–2030 for the global action plan for the prevention and control of NCDS 2013–2030. Available: https://www.who.int/publications/m/item/implementation-roadmap-2023-2030-for-the-who-global-action-plan-for-the-prevention-and-control-of-ncds-2023-2030 [Accessed 22 Feb 2022].
- 8.Menotti A, Seccareccia F, Lanti M, et al. Mean levels and distributions of some cardiovascular risk factors in Italy in the 1970's and the 1980's. The Italian rifle pooling project. risk factors and life expectancy. G Ital Cardiol 1995;25:1539–72. [PubMed] [Google Scholar]
- 9.Salvetti M, Muiesan ML, Rizzoni D, et al. Night time blood pressure and cardiovascular structure in a middle-aged general population in northern Italy: the Vobarno study. J Hum Hypertens 2001;15:879–85. 10.1038/sj.jhh.1001286 [DOI] [PubMed] [Google Scholar]
- 10.Bombelli M, Toso E, Peronio M, et al. The Pamela study: main findings and perspectives. Curr Hypertens Rep 2013;15:238–43. 10.1007/s11906-013-0348-1 [DOI] [PubMed] [Google Scholar]
- 11.Mancia G, Bombelli M, Lanzarotti A, et al. Systolic vs diastolic blood pressure control in the hypertensive patients of the PAMELA population. Pressioni Arteriose Monitorate E Loro Associazioni. Arch Intern Med 2002;162:582–6. 10.1001/archinte.162.5.582 [DOI] [PubMed] [Google Scholar]
- 12.Cirillo M, Terradura-Vagnarelli O, Mancini M, et al. Cohort profile: the Gubbio population study. Int J Epidemiol 2014;43:713–20. 10.1093/ije/dyt025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . Noncommunicable diseases country profiles, 2018. Available: https://apps.who.int/iris/handle/10665/274512 [Accessed 22 Feb 2022].
- 14.A Comprehensive Global Monitoring Framework . Including indicators, and a set of voluntary global targets for the prevention and control of Noncommunicabale diseases who, 2012. Available: https://www.who.int/nmh/events/2012/discussion_paper2_20120322.pdf [Accessed 22 Feb 2022].
- 15.Noncommunicable Diseases Global Monitoring Framework . Indicator definitions and specifications (WHO 2014). Available: https://www.who.int/publications/i/item/ncd-gmf-indicator-definitions-and-specifications [Accessed 22 Feb 2022].
- 16.Donfrancesco C, Profumo E, Lo Noce C, et al. Trends of overweight, obesity and anthropometric measurements among the adult population in Italy: the CUORE project health examination surveys 1998, 2008, and 2018. PLoS One 2022;17:e0264778. 10.1371/journal.pone.0264778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donfrancesco C, Lo Noce C, Russo O, et al. Trend of salt intake measured by 24-h urine collection in the Italian adult population between the 2008 and 2018 CUORE project surveys. Nutr Metab Cardiovasc Dis 2021;31:802–13. 10.1016/j.numecd.2020.10.017 [DOI] [PubMed] [Google Scholar]
- 18.Donfrancesco C, Lo Noce C, Russo O, et al. Trend in potassium intake and Na/K ratio in the Italian adult population between the 2008 and 2018 CUORE project surveys. Nutr Metab Cardiovasc Dis 2021;31:814–26. 10.1016/j.numecd.2020.11.015 [DOI] [PubMed] [Google Scholar]
- 19.Giampaoli S, Palmieri L, Donfrancesco C, et al. Cardiovascular health in Italy. ten-year surveillance of cardiovascular diseases and risk factors: Osservatorio Epidemiologico Cardiovascolare/Health examination survey 1998-2012. Eur J Prev Cardiol 2015;22:9–37. 10.1177/2047487315589011 [DOI] [PubMed] [Google Scholar]
- 20.European Health Examination Survey (EHES) . Measuring the health of Europeans. Available: http://www.ehes.info/national/national_hes_status.htm [Accessed 22 Feb 2022].
- 21.Tolonen H, Koponen P, Naska A, et al. Challenges in standardization of blood pressure measurement at the population level. BMC Med Res Methodol 2015;15:33. 10.1186/s12874-015-0020-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Williams B, Mancia G, Spiering W. ESC scientific document group. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021–104. [DOI] [PubMed] [Google Scholar]
- 23.National Institute of Statistics . Resident population 1991-2019. Available: http://dati.istat.it/Index.aspx?DataSetCode=DCIS_RICPOPRES2011 [Accessed 22 Feb 2022].
- 24.Revision of the European Standard Population . Report of Eurostat’s task force - 2013 edition. Available: https://ec.europa.eu/eurostat/documents/3859598/5926869/KS-RA-13-028-EN.PDF/e713fa79-1add-44e8-b23d-5e8fa09b3f8f [Accessed 22 Feb 2022].
- 25.NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021;398:957–80. 10.1016/S0140-6736(21)01330-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NCD Risk Factor Collaboration (NCD-RisC). Available: https://ncdrisc.org/obesity-prevalence-ranking.html
- 27.WHO . High blood pressure - country experiences and effective interventions utilized across the European Region, 2013. Available: https://www.euro.who.int/__data/assets/pdf_file/0008/185903/e96816.pdf [Accessed 22 Feb 2022].
- 28.Strazzullo P, Cairella G, Campanozzi A, et al. Population based strategy for dietary salt intake reduction: Italian initiatives in the European framework. Nutr Metab Cardiovasc Dis 2012;22:161–6. 10.1016/j.numecd.2011.10.004 [DOI] [PubMed] [Google Scholar]
- 29.Bann D, Fluharty M, Hardy R, et al. Socioeconomic inequalities in blood pressure: co-ordinated analysis of 147,775 participants from repeated birth cohort and cross-sectional datasets, 1989 to 2016. BMC Med 2020;18:338. 10.1186/s12916-020-01800-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.CUOREDATA platform - The CUORE Project. Available: http://www.cuore.iss.it/eng/survey/cuoredata
- 31.Venezia A, Barba G, Russo O, et al. Dietary sodium intake in a sample of adult male population in southern Italy: results of the Olivetti heart study. Eur J Clin Nutr 2010;64:518–24. 10.1038/ejcn.2010.22 [DOI] [PubMed] [Google Scholar]
- 32.European Society of Hypertension-European Society of Cardiology Guidelines Committee . 2003 European Society of Hypertension-European Society of cardiology guidelines for the management of arterial hypertension. J Hypertens 2003;21:1011–53. 10.1097/00004872-200306000-00001 [DOI] [PubMed] [Google Scholar]
- 33.Mansia G, De Backer G, Dominiczak A, et al. 2007 ESH-ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of hypertension (ESH) and of the European Society of cardiology (ESC). Blood Press 2007;16:135–232. 10.1080/08037050701461084 [DOI] [PubMed] [Google Scholar]
- 34.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of hypertension (ESH) and of the European Society of cardiology (ESC). J Hypertens 2013;31:1281–357. 10.1097/01.hjh.0000431740.32696.cc [DOI] [PubMed] [Google Scholar]
- 35.Wing LM, Reid CM, Ryan P. Second Australian National blood pressure Study Group. A comparison of outcomes with angiotensin-converting-enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 2003;348:583–92. [DOI] [PubMed] [Google Scholar]
- 36.Palmieri L, Bennett K, Giampaoli S, et al. Explaining the decrease in coronary heart disease mortality in Italy between 1980 and 2000. Am J Public Health 2010;100:684–92. 10.2105/AJPH.2008.147173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ogata S, Nishimura K, Guzman-Castillo M, et al. Explaining the decline in coronary heart disease mortality rates in Japan: contributions of changes in risk factors and evidence-based treatments between 1980 and 2012. Int J Cardiol 2019;291:183–8. 10.1016/j.ijcard.2019.02.022 [DOI] [PubMed] [Google Scholar]
- 38.Mindell JS, Giampaoli S, Goesswald A, et al. Sample selection, recruitment and participation rates in health examination surveys in Europe--experience from seven national surveys. BMC Med Res Methodol 2015;15:78. 10.1186/s12874-015-0072-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Italian National Institute of Statistics . Population education levels and occupational returns: the main indicators, 2017. Available: https://www.istat.it/it/files/2018/07/Indicatori-dellistruzione.pdf [Accessed 22 Feb 2022].
- 40.European Commission . Commission regulation (EU) NO 847/2012 on 19 September 2012 amending Annex XVII to regulation (EC) NO 1907/2006 of the European Parliament and of the Council on the registration, evaluation, authorisation and restriction of chemicals (reach) as regards mercury. in 847/2012. edited by European Commission. Off J Eur Union 2012;L253. [Google Scholar]
- 41.Ostchega Y, Zhang G, Sorlie P. Blood pressure randomized methodology study comparing automatic oscillometric and mercury sphygmomanometer devices: National health and nutrition examination survey, 2009–2010. Natl Health Stat Report 2012;59:1–15. [PubMed] [Google Scholar]
- 42.Chen Z, Wang X, Wang Z, et al. Assessing the validity of oscillometric device for blood pressure measurement in a large population-based epidemiologic study. J Am Soc Hypertens 2017;11:730–6. 10.1016/j.jash.2017.09.004 [DOI] [PubMed] [Google Scholar]
- 43.El Assaad MA, Topouchian JA, Darné BM, et al. Validation of the Omron HEM-907 device for blood pressure measurement. Blood Press Monit 2002;7:237–41. 10.1097/00126097-200208000-00006 [DOI] [PubMed] [Google Scholar]
- 44.de Greeff A, Lorde I, Wilton A, et al. Calibration accuracy of hospital-based non-invasive blood pressure measuring devices. J Hum Hypertens 2010;24:58–63. 10.1038/jhh.2009.29 [DOI] [PubMed] [Google Scholar]
- 45.Wolf HK, Tuomilehto J, Kuulasmaa K, et al. Blood pressure levels in the 41 populations of the who MONICA project. J Hum Hypertens 1997;11:733–42. 10.1038/sj.jhh.1000531 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-064270supp001.pdf (3.4MB, pdf)
Data Availability Statement
No data are available. The data are not publicly available due to ethical and legal restrictions on data sharing.