Abstract
Objective
To assess the effects of using an animated local language educational video to counsel postpartum adolescents on the benefits and use of long-acting reversible contraception (LARC).
Materials and methods
A two-stage, single group, experimental study was conducted. A total of 124 female adolescents aged < 20 years who had given birth within the last six weeks participated in the study. An educational video and a questionnaire were developed and validated. Participants were asked to fill out a questionnaire on basic demographic data, contraception preferences, and 10 true/false statements to test general contraceptive knowledge, after which they were shown an educational video in a private room. Following this, participants completed the second part of the questionnaire that assessed their knowledge using the same true/false statements and contraception preferences administered earlier.
Results
The mean age (standard deviation) of participants was 18.1 (1.5) years. Participants’ mean age (SD) at the time of their first sexual intercourse was 16.2 (1.6) years. Among the 124 participants, 31 (25%) indicated that they would use LARC before viewing the educational video. After viewing the educational video, this number increased to 48 (38.7%). The participants’ knowledge score was independently associated with their preference to select LARC (adjusted odds ratio 1.46, 95% confidence interval 1.09- 1.97).
Conclusion
This study demonstrated that counseling tools such as animated local language educational video might effectively improve contraceptive knowledge and the preference for LARC in postpartum adolescents. An educational video regarding LARC could be used as a counseling tool for postpartum adolescents.
Keywords: Teenage pregnancies, Long-acting reversible contraception (LARC), Counseling, Educational video, Postpartum adolescents
Introduction
Unintended pregnancy in teenagers is a major problem worldwide. Each year, at least 10 million unintended pregnancies occur among adolescent girls aged 15–19 in developing regions [1]. Pre-term labor, low birth weight, and unsafe abortion in teenage pregnancies contribute to high rates of maternal and child morbidity and mortality [2]. The World Health Organization (WHO) reported that an estimated 3.9 million unsafe abortions occur in girls aged 15–19 years annually [1]. These pregnancies may stem from not using or using less effective contraception. Evidence shows that comprehensive contraceptive counseling can affect young women's decisions on long-acting reversible contraception (LARC) initiation, a cost-saving strategy for preventing unintended pregnancy [3–5]. The American College of Obstetricians and Gynecologists (ACOG) recommends LARC as a first-line contraceptive for adolescents [6], while another study found that effective counseling could improve contraceptive use [7]. Social media has also been used as an adjunct to traditional, in-office counseling and was shown to improve the patients’ contraceptive knowledge as well as preference for LARC [8]. However, there is limited data regarding the implementation of an educational video as a counseling tool [9]. The primary objective of this study was to assess the effectiveness of an educational video in helping sexually active postpartum adolescents select the most appropriate contraceptive method based on their preferences. The secondary objective was to assess the factors associated with the preference for LARC in sexually active postpartum adolescents. The benefits of using educational videos are that they are easier to use, consistently reproducible, have no variations as seen in traditional, in-office counseling, and can be used in almost any setting with low-cost electronic devices. We hypothesized that viewing an animated educational video would give postpartum adolescent mothers contraceptive knowledge, encouraging them to select highly effective contraception [10].
Materials and methods
Study design
This was a two-stage, single-group, experimental study conducted at the Family Planning and Reproductive Health Clinic of the King Chulalongkorn Memorial Hospital. During the study period, LARC, including contraceptive implant(s) and copper intrauterine devices (IUDs), became freely available through the national health care program for all adolescents. We recruited women aged < 20 years who had given birth within the last six weeks and were fluent in Thai. Women who had an absolute contraindication for one of the following contraceptives were excluded: combined/progestin oral contraceptive pills, depot medroxyprogesterone acetate (DMPA), contraceptive implant (s), and copper IUDs. Based on these criteria, a total of 124 female adolescents participated in the study.
Ethical approval
This study was conducted in accordance with the principles of the Declaration of Helsinki. This study was approved by the Ethics and Institutional Research Committees of the Faculty of Medicine (IRB No.135/57) and registered in the Thai Clinical Trials Registry (TCTR) #: TCTR20150715001. Written informed consent was obtained in Thai from participants before starting any procedures.
Study protocol and data collection
An animated 10-min Thai language educational video was developed according to the WHO's family planning handbook [11]. The contents of the educational video provided the following information: 1) outcomes and morbidities of teenage pregnancies, such as pre-term labor and low-birth weight; 2) types of contraception available, including tubal resection and short- and long-acting reversible contraception; 3) pros, cons, and failure rates of each contraceptive method; 4) LARC insertion procedures; and 5) the average cost per month for each contraceptive method. We provided participants with information regarding freely available LARC through the national health care program for all adolescents. The contraceptive methods covered in the educational video were as follows: combined/progestin oral contraceptive pills, DMPA, male condoms, contraceptive implant(s), and copper IUDs. The questionnaire used in this study was divided into two parts. The first part of the questionnaire was administered before the educational video was viewed in a private room. Basic demographic data and characteristics of the participants were collected, including their age, educational level, income, and marital status. The questionnaire also asked about participants’ contraceptive preferences and history of contraceptive use. An additional 10 true/false statements were used to assess participants’ general contraceptive knowledge. Answers were given a score of 1 for correct, 0 for incorrect. The possible lowest-to-highest knowledge scores ranged from 0–10. The second part of the questionnaire was administered after the educational video was viewed. The same 10 true/false statements from the first part of the questionnaire were repeated. Participants were also asked which contraceptive method they would like to use after viewing the educational video. The educational video and questionnaires were validated by two independent family planning experts (SS and UJ).
The sample size was calculated based on a pilot study of 30 postpartum adolescents conducted at the same institution. To achieve 80% power at a 5% significance level, a sample size of 124 participants was required.
Statistical analysis
Data analysis was performed using the IBM SPSS for Windows (version 17.0; IBM Corporation, Armonk, NY). Means, standard deviations (SDs), and percentages were used to describe the demographic characteristics. McNemar’s test was used to compare the selection of LARC before and after viewing the educational video. Multivariable models were analyzed, which included variables that were potential confounders based on both previous literature and univariate analysis (p ≤ 0.2) [12, 13]. Odds ratios (ORs), adjusted odds ratios (aORs), p-values, and 95% confidence intervals (CIs) were calculated to estimate factors that were independently associated with preference to select LARC. Statistical significance was set at p < 0.05.
Results
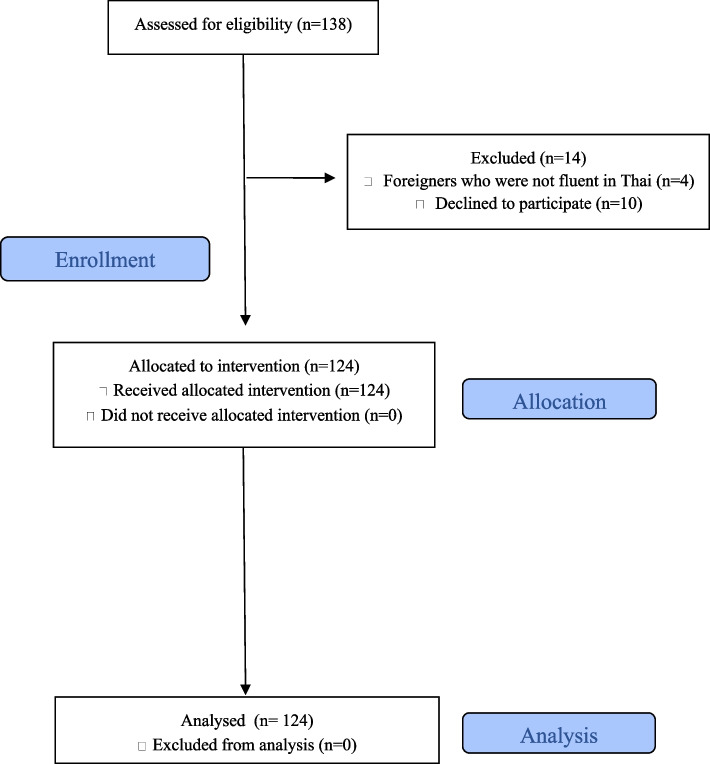
A total of 124 female adolescents were enrolled in the study. The study flow is shown in Fig. 1. The sociodemographic and obstetric characteristics are described in Table 1. The mean age (SD) of the postpartum adolescents who participated in the study was 18.1 (1.5) years. Participants’ mean age (SD) at the time of their first sexual intercourse was 16.2 (1.6) years. Thirty-five percent of the participants had their first sexual intercourse at age ≤ 15 years. Approximately three-quarters (92/124, 74.2%) of the participants had not completed their high school education. The majority of participants (52/124, 41.9%) were students. Half of the participants’ (63/124, 50.8%) parents were either separated or dead. More than half of the participants (85/124, 68.5%) used contraception during their first sexual intercourse. Of these, the following contraceptive methods were used: 61.2% (52/85) used combined oral contraceptive pills, 28.8% (15/52) used emergency pills, and 28.8% (15/52) used male condoms. Twenty-four participants (24/124, 19.3%) had more than one child and 54% (13/24) of them were pregnant within two years of the previous birth.
Fig. 1.
Study flow
Table 1.
Socio-demographic and obstetric characteristics of the post-partum adolescent mothers at the King Chulalongkorn Memorial Hospital (N = 124)
| Characteristics | Number (%) |
|---|---|
| Highest educational level attained | |
| Primary school | 16 (12.9) |
| Lower secondary school | 76 (61.3) |
| Upper secondary school | 21 (16.6) |
| Vocational/ Diploma | 11 (8.9) |
| Occupation | |
| Student | 52 (41.9) |
| Employee | 46 (37.1) |
| Housewife | 21 (16.9) |
| Business | 5 (4) |
| Income (US dollars per month) | |
| 0–300 | 101 (81.5) |
| > 300 | 23 (18.5) |
| Source of income | |
| Family | 81 (65.3) |
| Work | 43 (34.7) |
| Contraception use at first sexual intercourse | |
| Yes | 85 (68.5) |
| No | 39 (31.5) |
| Number of children | |
| 1 | 100 (80.6) |
| 2 | 23 (18.5) |
| 3 | 1 (0.8) |
| Pregnancy intention | |
| Intentional | 47 (37.9) |
| Unintentional | 77 (62.1) |
| Reason for unintended pregnancy | |
| Contraceptive failure | 32 (41.6) |
| No contraceptive use | 45 (58.4) |
| Health insurance | |
| Yes | 87 (70.2) |
| No | 37 (29.8) |
Approximately 75% (93/124) of the participants initially selected non-LARC, but after viewing the educational video, 21.5% (20/93) changed their minds and reported they would prefer to use LARC.. However, three participants (3/31, 9.6%) who initially said they would prefer to use LARC before viewing the educational video later changed their preference to a non-LARC method because they were afraid of the pain associated with the procedure. The mean (SD) contraceptive knowledge scores increased from 6.8 (1.2) points to 7.9 (1.4) points after viewing the educational video. Participants who selected LARC after viewing the educational video said they had changed their opinion due to benefits such as effectiveness (35/48, 72.9%) and the need for long-term contraception (28/48, 58.3%). Half of the participants (40/76, 52.6%) who did not select LARC stated that they were afraid of pain associated with the procedure. Approximately 35% (27/76) of the participants stated that they had some concerns about the side effects of LARC.
Univariable analysis showed that knowledge score after counseling/viewing the educational video was significantly associated with the preference to use LARC (Yes) (OR 1.42, 95% CI 1.07—1.88, p = 0.02) as described in Table 2. When confounding variables were adjusted in the multivariable model, the knowledge score after viewing the educational video was still significantly associated with the preference to use LARC (Yes) (aOR 1.46, 95% CI 1.09—1.97, p = 0.01).
Table 2.
Logistic regression analysis of factors associated with the preference to use the LARC method after viewing an educational videoa (N = 124)
| Variables | Unadjusted models | Adjusted modelsb | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p-value | Adjusted odds ratiob | 95% CI | p-value | |
| Age | 0.80 | 0.64–1.03 | 0.07 | 0.86 | 0.66–1.13 | 0.28 |
|
Source of income - Family vs. Work |
0.57 | 0.26–1.25 | 0.16 | 0.51 | 0.20–1.27 | 0.15 |
|
Health insurance support - No vs. Yes |
0.57 | 0.25–1.30 | 0.18 | 0.45 | 0.19–1.12 | 0.09 |
|
Pregnancy intention - Intentional vs. Unintentional |
1.86 | 0.86–4.03 | 0.11 | 1.55 | 0.67–3.60 | 0.30 |
| Knowledge scores after viewing the educational video | 1.42 | 1.07–1.88 | 0.02 | 1.46 | 1.08–1.97 | 0.01 |
aDependent variable—the preference to use LARC method vs. non LARC method
bAdjusted for age, source of income, health insurance support, pregnancy intention
Discussion
Our study shows that the use of an animated 10-min Thai language educational video as an adjunct to the traditional in-office counseling method can significantly increase the knowledge about LARC and contribute to the subsequent preference for LARC methods. This finding is consistent with the results of a randomized controlled clinical trial conducted by Burapasikarin et al., which showed that an educational video on LARC can increase its utilization during the postpartum period [9], Another study showed that reading the information on LARC out loud to the participants and giving them a written document on LARC did not increase their preference for LARC [14]. Likewise, the use of an educational script on the intrauterine device and contraceptive implant did not increase the preference for LARC postpartum [14]. This indicates that providing information on LARC without using other educational techniques may not affect the preference for LARC. Additional techniques, such as educational videos, can significantly affect the preference for LARC as it can help the viewers concentrate more on the knowledge content and be more engaged in the topic.
The results of the multivariable analysis showed that participants’ general contraceptive knowledge regarding LARC might have affected their preference for LARC. Providing more information on LARC in layman’s terms may help increase the preference for selecting this contraceptive method. This finding corroborates previous reports that improved knowledge of LARC is associated with its increased use [15–17].
Our analysis shows that sources of income and health insurance were not associated with LARC selection. One possible explanation is that LARC is free of charge in our setting. This result may not be generalizable as the cost can be a barrier in other locations and could decrease the preference for LARC [18]. The results of our study are most applicable to postpartum adolescents in comparable settings in Southeast Asian countries. Generalizable to other groups of different ages, educational attainment, and cultural contexts may be limited. These factors might affect clients' health literacy, contributing to their decision to initiate contraception. Another limitation is that our analysis was restricted to participants’ preferences for using LARC. However, information regarding LARC initiation was not available, as most participants preferred to delay contraceptive initiation until the postpartum follow-up visit.
Conclusion
This study successfully demonstrated the effectiveness of using an animated 10-min Thai language educational video as a counseling tool to significantly increase the preference for LARC among postpartum mothers. Additional studies with longer follow-up periods are necessary to evaluate how this educational video subsequently affects patient decision-making to choose LARC over other methods of contraception.
Acknowledgements
The authors would like to thank Ms. Chalalai Amatayakul, Ms. Nantana Thongrod, and Ms. Kangsadal Amatayakul for their research assistance.
Authors’ contributions
“I declare that I participated in the literature review, study concept design, statistical analysis, manuscript editing and revision for intellectual content and that I have seen and approved the final version.”
Somsook Santibenchakul, MD PhD MPH.
“I declare that I participated in the literature review, data acquisition, statistical analysis, primary manuscript drafting and that I have seen and approved the final version.”
Kittithorn Thanativakul MD.
“I declare that I participated in the study concept design and that I have seen and approved the final version.”
Unnop Jaisamrarn, MD MHS.
Funding
This study was sponsored by Family Planning and Reproductive Health Unit, Department of Obstetrics and Gynecology, Faculty of Medicine, Chulalongkorn University.
Availability of data and materials
The data and material that support the findings of this study are available upon request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the principles of the Declaration of Helsinki. This study was approved by the Ethics and Institutional Research Committees of the Faculty of Medicine (IRB No.135/57) and registered in the Thai Clinical Trials Registry (TCTR) #: TCTR20150715001. Written informed consent was obtained in Thai from participants before starting any procedures.
Consent for publication
Not applicable.
Competing interests
All authors certify that there are no conflicts of interest with any financial organization or other reasons regarding the material discussed in the manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Darroch J, Woog V, Bankole A, Ashford LS. Adding it up: Costs and benefits of meeting the contraceptive needs of adolescents. New York: Guttmacher Institute; 2016. [Google Scholar]
- 2.Ganchimeg T, Ota E, Morisaki N, Laopaiboon M, Lumbiganon P, Zhang J, et al. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG. 2014;121(Suppl 1):40–48. doi: 10.1111/1471-0528.12630. [DOI] [PubMed] [Google Scholar]
- 3.Emtell Iwarsson K, Envall N, Bizjak I, Bring J, Kopp Kallner H, Gemzell-Danielsson K. Increasing uptake of long-acting reversible contraception with structured contraceptive counselling: cluster randomised controlled trial (the LOWE trial) BJOG. 2021;128(9):1546–1554. doi: 10.1111/1471-0528.16754. [DOI] [PubMed] [Google Scholar]
- 4.Zapata LB, Pazol K, Dehlendorf C, Curtis KM, Malcolm NM, Rosmarin RB, et al. Contraceptive Counseling in Clinical Settings: An Updated Systematic Review. Am J Prev Med. 2018;55(5):677–690. doi: 10.1016/j.amepre.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madden T, Barker AR, Huntzberry K, Secura GM, Peipert JF, McBride TD. Medicaid savings from the Contraceptive CHOICE Project: a cost-savings analysis. Am J Obstet Gynecol. 2018;219(6):595.e1-.e11. doi: 10.1016/j.ajog.2018.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Committee Opinion No. 710: Counseling Adolescents About Contraception. Obstet Gynecol 2017 (Reaffirmed 2019); 130: e74-e80. [cited 24 Feb 2022]; Available from: https://www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-opinion/articles/2017/08/counseling-adolescents-about-contraception.pdf. [DOI] [PubMed]
- 7.Coleman-Minahan K, Potter JE. Quality of postpartum contraceptive counseling and changes in contraceptive method preferences. Contraception. 2019100(6):492–497. 10.1016/j.contraception.2019.08.011. Epub 2019 Sep 4. PMID: 31491380; PMCID: PMC6893140. [DOI] [PMC free article] [PubMed]
- 8.Kofinas JD, Varrey A, Sapra KJ, Kanj RV, Chervenak FA, Asfaw T. Adjunctive social media for more effective contraceptive counseling: a randomized controlled trial. Obstet Gynecol. 2014;123:763–770. doi: 10.1097/AOG.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 9.Burapasikarin C, Manonai J, Wattanayingcharoenchai R. The effect of an educational video on long-acting reversible contraception (LARC) utilization at 6–8 weeks postpartum period: a randomized controlled trial. Arch Gynecol Obstet. 2020;302(6):1503–1509. doi: 10.1007/s00404-020-05710-3. [DOI] [PubMed] [Google Scholar]
- 10.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Family planning: a global handbook for providers. 2012. [Cited 2013, Jul 14]; Available from: http://www.who.int/reproductivehealth/publications/family_planning/9780978856304/en/.
- 12.Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santibenchakul S, Tschann M, Carlson ADP, L Hurwitz E, Salcedo J. Promotion of Long-Acting Reversible Contraception Among Adolescents and Young Adults. J Midwifery Womens Health. 2019;64(2):194–200. doi:10.1111/jmwh.12934. [DOI] [PMC free article] [PubMed]
- 14.Tang JH, Dominik RC, Zerden ML, Verbiest SB, Brody SC, Stuart GS. Effect of an educational script on postpartum contraceptive use: a randomized controlled trial. Contraception. 2014;90(2):162–167. doi: 10.1016/j.contraception.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 15.Bolarinwa OA, Olagunju OS. Knowledge and factors influencing long-acting reversible contraceptives use among women of reproductive age in Nigeria. Gates Open Res. 2020;3:7. Published 2020 May 20. 10.12688/gatesopenres.12902.3. [DOI] [PMC free article] [PubMed]
- 16.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203(2):115.e1–115.e1157. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dempsey AR, Billingsley CC, Savage AH, Korte JE. Predictors of long-acting reversible contraception use among unmarried young adults. Am J Obstet Gynecol. 2012;206(6):526.e1–526.e5265. doi: 10.1016/j.ajog.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 18.Birgisson NE, Zhao Q, Secura GM, Madden T, Peipert JF. Preventing Unintended Pregnancy: The Contraceptive CHOICE Project in Review. J Womens Health (Larchmt) 2015;24(5):349–353. doi: 10.1089/jwh.2015.5191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data and material that support the findings of this study are available upon request.