Abstract
Healthcare is one of the most critical sectors due to its importance in handling public health. With the outbreak of various diseases, more recently during Covid-19, this sector has gained further attention. The pandemic has exposed vulnerabilities in the healthcare supply chain (HSC). Recent advancements like the adoption of various advanced technologies viz. AI and Industry 4.0 in the healthcare supply chain are turning out to be game-changers. This study focuses on identifying critical success factors (CSFs) for AI adoption in HSC in the emerging economy context. Rough SWARA is used for ranking CSFs of AI adoption in HSC. Results indicate that technological (TEC) factors are the most influential factor that impacts the adoption of AI in HSC in the context of emerging economies, followed by institutional or environmental (INT), human (HUM), and organizational (ORG) dimensions.
Keywords: Artificial Intelligence, Healthcare, Supply chain, SWARA
1. Introduction
With the advent of the fourth industrial revolution, businesses have geared towards adopting disruptive technologies such as AI, blockchain, and the internet of things (Rajput and Singh, 2019; Egger and Masood, 2020). This transformation is driving new financial benefits to stakeholder firms (Wu et al., 2017), making intelligent and timely decisions (Wu et al., 2016), and securing the competitiveness of business models (Viswanadham, 2018). Among these technologies, AI is increasingly being recognized as a game-changer across sectors like healthcare (Zhang et al., 2018a, Jain et al., 2020), insurance (Cognizant, , 2017, Toyoda et al., 2017), manufacturing (Zhou et al., 2018), banking (Cocco et al., 2017), digital payments (Gao et al., 2018), energy (Mengelkamp et al., 2018), and education (Fryer et al., 2020). In their study, Belhaldi et al. (2021) suggest that there can be extensive benefits of AI applications in supply chain management. In response to this, more artificial intelligence (AI) based functional supply chain applications have emerged (Riahi et al., 2021), and researchers have explored the transformational impact of AI technology in the supply chain ecosystem (Saberi et al., 2019a). While discussing the issues associated with centralized supply chain systems, Azzi et al. (2019) elaborated on AI’s capability to infuse desired visibility and transparency, leading to greater flexibility in value chains (Kshetri, 2018, Soltanisehat et al., 2020). Further, AI technology can impart energy efficiency (Zhang et al., 2018b), cost reduction (Catalini and Gans, 2016), better inventory management and fraud reduction (Clauson et al., 2018), and security and traceability to the supply chain, thus generating superior performance and better customer and partner trust for businesses (IBM, 2018).
An adequate supply chain reduces cost and risk (Tarei et al., 2022), improves quality, speed, and dependability (Munir et al., 2020), ensures flexibility (Azadegan et al., 2020), and enhances sustainability (Yousefi and Tosarkani, 2022). Although attaining an effective supply chain remains a challenge across industries and businesses (Schuetz and Venkatesh, 2020), the involvement of patient safety and related health outcomes generate greater complexity in the healthcare supply chain (HSC), which gets aggravated by the presence of multiple participants falling under different jurisdictions (Kwon et al., 2016, Gardas, 2022). Operational issues like lead time (Xu et al., 2020) and disruptions like disasters and strikes (Ivanov and Dolgui, 2021) pose risks to the supply chain. Besides these, issues on service interruptions (Kara et al., 2020), shorter product life cycle (World Economic Forum, 2017), and climate variability (Rajagopal et al., 2017) also challenge supply chain efficiency. Epidemic outbreaks like SARS, Ebola, and the most recent COVID-19 also expose the supply chain vulnerabilities (Araz et al., 2020), which further get attenuated due to their lean and globalized structures. A recent report shows that around 94 percent of Fortune 1000 companies have reported supply chain disruptions due to the global outbreak of Covid-19 (Fortune, 2020). The extant studies have discussed the supply chain issues and the importance of AI in addressing these challenges. However, the context-specific insight that can help gain new insights into AI adoption is inadequate and a growing need. As industry characteristics play a distinctive role in technology adoption (Tourajipour et al., 2021), this study examines the factors that can facilitate AI adoption in the healthcare supply chain (HSC).
The Healthcare supply chain refers to an extensive network of processes and components that ensure timely manufacturing, distribution, and provision of medicines and healthcare supplies to patients (Beaulieu and Bentahar, 2021). Since healthcare is a specialized industry that requires preparedness during unexpected and troubled times like the outbreak of a pandemic, biological/ chemical warfare, etc., its management differs from commercial supply chain management. In the context of the healthcare supply chain (HSC), issues like the involvement of patient safety, related health outcomes, and the presence of multiple participants generate even greater complexity (Senna et al., 2021). Owing to the critical flows in these supply chains, operational uncertainties, and the demand for high service levels, it is challenging and complicated to replicate the standard practices in different settings (Aldrighetti et al., 2019). Further, a compromised supply chain in the health care sector is feared to promote transnational trade in counterfeit medicines, create an artificial shortage of medicines and medical devices, and pose a security threat in using connected medical devices (Min 2019). Considering the significance of HSC in ensuring the availability of medical products and devices at the right time, maximizing patient care, minimizing inventory wastage, reducing the chances of errors, and improving the coordination among stakeholders (Senna et al., 2021), it is imperative to strengthen our understanding of this subject for overcoming the unique challenges that HSC encounters. While the existing literature discusses the benefits of AI-integrated HSCs, the focus on enablers for AI adoption in HSCs is inadequate. The HSC industry is experiencing rising demand, growing costs, shifting customer needs, increased competition, and growing interdependencies (Gartner 2022). Following the immense benefits of AI technology in addressing HSC issues, and the pressing need to ensure continuity in HSC operations during situations like a pandemic, this study provides insights that can facilitate the adoption of AI by HSC managers.
A significant body of extant HSC literature deliberates on the benefits accruing to multiple stakeholders (Laroiya et al. 2020) and aspects like improvement in healthcare delivery, automating procurement contracts, traceability, and improvement in firm performance (Beaulieu and Bentahar, 2021, Ageron et al., 2020). Few studies have also explored the technology adoption barriers (Desingh, 2022). Other studies have focused on the benefits and challenges of AI technology in the supply chain (Onik et al., 2019). However, no comprehensive study has investigated the CSFs of AI adoption in HSC. To address this gap, this study proposes a theoretical framework for identifying the CSFs of AI implementation in Indian HSC. In a recent survey of 399 healthcare executives conducted by Accenture (2021), around 73 percent believed that the technology architecture adopted by their organization is critical to the business's overall success. This growing inseparability between business and technology strategies owing to their crucial technological intervention roles in maintaining business competitiveness is the primary motivation of this study. Further, in response to the findings of the report by Gartner (2022), healthcare providers need to work on aspects like effective cost management, ensuring transparency among different stakeholders, and identifying new sources of competitive advantage. The potential of AI technology in meeting these objectives in HSC provides another motivation for the study. Moreover, the recent instance of pandemic-induced supply chain fallouts and subsequent market failures further augments the case for technological integration in healthcare supply chains. This calls for exploring the factors that can guide AI implementation in HSC. The study, therefore, intends to address the following research questions:
RQ1: What are the emerging technologies for managing the healthcare supply chain?
RQ2: What are the critical success factors of AI implementation in the healthcare supply chain?
This study contributes to the existing literature on HSC. Firstly, by examining CSFs for AI implementation in HSC, the study extends the existing literature on technology adoption in HSC. Although Scholars, researchers, health care providers, and governments have started giving attention to the AI applications in HSC (Guan, 2019, Habli et al., 2020), empirical research about the CSFs of AI usage in a supply chain ecosystem, particularly in the health care industry is scant. The study further assimilates the Technology-Organisation-Environment (TOE) framework (Tornatzky and Fleischer 1990) and Human-Organisation-Technology fit (HOT-fit) (Yusof et al. 2008) model and proposes a theoretical model based upon the significant factors facilitating AI adoption in HSC. Serving as an analytical tool for explaining technological innovation adoptions by organizations, the TOE framework has been extensively applied across domains (Bala and Feng, 2019, Chen et al., 2019, Cruz-Jesus et al., 2019), including the health care industry (Gao and Sunyaev, 2019, Sadoughi et al., 2019). With a set of comprehensive dimensions, the HOT fit model concentrates intensively on adopting innovation toward Health Information Systems (HIS) and broadly suggests a greater realization of HIS attributable to better fit amongst human, organization, and technology factors (Yusof et al. 2008). While integrating the mature TOE framework and the recently developed HOT fit model to identify factors crucial for ICT adoption (Arpaci, 2019, Mir and Padma, 2020), extant literature has shown that integrated models give better results (Ahmadi et al., 2017, Yadegaridehkordi et al., 2018). Therefore, the current study explores CSFs based on the integrated approach of using the TOE framework and HOT fit model.
This research has adopted the recent specialized method- Step-wise Assessment Ratio Analysis (SWARA), for weighing criteria according to their priority. This method employs experts’ knowledge, available information, and different experiences from the criteria for evaluating the significance of coefficients. Previous studies (Mardani et al., 2017) have seen extensive applications of the SWARA method in areas like investigating supply chain competitive strategies (Khodadadi et al., 2017) and evaluating the sustainability of third-party logistics providers (Zarbakhshnia et al., 2018).
This study applies CSF originating from the TOE and HOT framework to understand the AI implementation in HSC in the Indian context. Studies have highlighted that prominent research in AI adoption has been conducted in developed countries (Brock and Khan, 2017). The study is relevant for achieving a robust HSC for the world’s second-most populous country, India. Developing countries generally witness skepticism on the shortcomings arising from the usage of conventional supply chain models. This, along with these countries' demographic, epidemiological, and economic transitions, motivates businesses to undertake higher investments in healthcare and improve their HSC. The outcome of this study can help healthcare providers, researchers, consultants, and the government envision the CSFs for the successful implementation of AI in HSC.
The paper is organized as follows. Section two will review the literature on the application of AI across sectors with a focus on HSC and CSFs of AI adoption in HSC. Section three presents the modeling framework. Section four discusses the analysis and results and discusses implications, followed by conclusions with implications in Sections five and six.
2. Literature review
2.1. Scenario of healthcare supply chain (HSC) network
As a unique supply chain, HSC focuses on managing resources, including streamlining supplies and delivering medicines and medical products/services to providers and patients (Govindan et al., 2020). The stakeholders involved in this process include manufacturers, hospitals, providers, insurance companies, regulatory agencies, and patients. Since this supply chain involves upstream and downstream relationships amongst these entities, and each stakeholder is concerned about their interest, HSCs are complex and fragmented (Zamiela et al., 2022). Studies in the HSC domain have suggested supply chain models for different healthcare products like vaccines, medical equipment, etc. (Phares et al., 2021). Few studies have also explored the barriers and enablers for improving HSC performance (Hussain et al., 2018, Srivastava et al., 2021). For example, Yousefli et al. (2017) have identified financial constraints, lack of awareness, inadequate infrastructure, and lack of clarity in government policies as hindering HSC performance. RecentlyHSCs are under tremendous pressure to reduce costs, address alterations in customer needs, improve productivity, provide better healthcare and become as lean as possible (Hussain et al., 2018, Scavarda et al., 2019). However, disruptions like manufacturer consolidation, changes in the economic and political scenario, and climate changes impart difficulty in achieving these objectives (Gartner, 2022). The recent outbreak of COVID-19 exposed HSC drastically and led to a global shortage of medical products. Following this, scholars have highlighted the significance of HSC in predicting, planning, and reacting to disruptions through one or more value chain links (Senna et al., 2021, Zamiela et al., 2022).
2.2. Artificial intelligence (AI) in healthcare supply chain (HSC)
Many industrial applications, including supply chain management, have the potential to be transformed by AI (Gupta et al., 2021, Toorajipour et al., 2021). The benefits of AI applications in supply chains have been observed in areas such as demand forecasting (Bala and Feng, 2019); facility location (Florez et al., 2015); supplier selection (Ferreira and Borenstein, 2012); supply chain risk management (Tsang et al. 2018); inventory replenishment (Sinha et al., 2012); and sustainability in the supply chain (Kazancoglu et al., 2022). According to Toorajipour et al. (2021), most research on AI in the supply chain lack specific industrial contexts, and their limiting insights may not be relevant for other settings. Besides, the AI implementation in HSCs has received little attention in the existing literature and offers scope for new study directions.
A recent report by Grand View (2020) estimates that the global AI market will grow at a CAGR of 57 percent between 2017 and 2025. There is also a surge in the academic literature on the potential of AI across different subjects, healthcare supply chain being one of them (Mitra et al., 2022, Beaulieu and Bentahar, 2021). AI technology is being used for different therapeutic and research purposes in healthcare, and a few include managing chronic disease and drug discovery. In the context of HSC, AI-based HSC can contribute to product delivery, tracking, inventory sharing, and resource pooling among stakeholders (McGhin et al., 2019). It can help validate product legitimacy, track counterfeit products, and authenticate medical devices (Jayaraman et al., 2019). Studies have also discussed the immense potential of AI in verifying and setting producers’ price eligibility (Randall et al. 2017) and improving healthcare data management (Dimitrov, 2019). In their recent study, Damoah et al. (2021) deliberated the applications of AI-enhanced medical in HSCs.
In a nutshell, by integrating disparate procurement, clinical systems, and financial administration throughout the HSC arrangement, AI-based HSC offers a practical solution to the challenges currently experienced by the HSC industry (Degnarain, 2020). Martínez-Pérez et al. (2020) have found AI capable of creating supply chain surplus in healthcare via improvements in operational efficiency and patient quality. Although there is ample support for the positive impact of AI in establishing a robust supply chain, there is no study presenting the CSFs of AI adoption in the healthcare sector. Besides facilitating AI implementation, a thorough analysis of CSFs would enhance healthcare services’ quality.
2.3. Identification of CSFs for AI implementation in HSC
The theoretical framework used in the current study is based upon a four-dimensional model comprising technological, organizational, institutional, and human factors (TOEH) that will facilitate the implementation of AI in HSC (Table 1 ). Besides, CSFs are drawn from the extant literature, expert opinions in IT, supply chain, and strategy domain, and feedback from academicians.
Table 1.
CSFs of AI adoption in HSC.
| Major CSF | Sub-CSF | Description | References |
|---|---|---|---|
| Technological (TEC) | Technology sophistication (TEC1) | It refers to the maturity and diversity of technological hardware and software for addressing issues of latency, security, and throughput | Agrawal et al., 2018, Hoy, 2017, Büyüközkan and Göçer, 2019, Alrahbi et al., 2021 |
| Perceived benefits (TEC2) | It stipulates the anticipated advantages and positive impact accruing from technology adoption | Alrahbi et al., 2021, Dwivedi et al., 2019a, Sun et al., 2020, Yadegaridehkordi et al., 2018 | |
| Sustainable data quality and integrity (TEC3) | Data quality refers to usability in terms of determining the reliability of data, while data integrity refers to the trustworthiness of data in terms of its physical and logical validity | Li et al. (2020), Zhang et al. (2018b); Damoah et al., 2021 | |
| Technological testing and troubleshooting feasibility (TEC4) | It indicates the diverse and well-defined testing activities in terms of validation models, techniques, and tools to identify and overcome errors in software and achieve test requirements | Aboelmaged, 2014, Sun et al., 2020, Gardas, 2022 | |
| Interoperability (TEC5) | Data interoperability refers to the processing and interpretation of received data to facilitate smooth communication between different stakeholders | Wang et al., 2019, Dobrovnik et al., 2018, Orji et al., 2020 | |
| Organizational (ORG) | Organizational leadership and support (ORG1) | It draws an association to the dynamic leadership and support being extended by top management and managers towards the entire process, from commencement to full technology adoption | Gutierrez at al. (2015), Szalavetz, 2019, Singh et al., 2019, Alrahbi et al., 2021, Gardas, 2022 |
| Strategic alignment between business viability and AI adoption (ORG2) | It refers to creating an alignment between business goals, the viability of business, and technology adoption to have better management of risks and opportunities in business | Nguyen et al., 2015, Tallon et al., 2019, Gardas, 2022 | |
| Organizational readiness (ORG3) | It directs to the receptive attitude and preparedness of the business for AI adoption | Yang et al., 2015, Pacchini et al., 2019, Magistretti et al., 2020, Khanijahani et al., 2022 | |
| Firm size and organization structure (ORG4) | It refers to the size and organizational structure of the firm as a reflection of its ability to invest, mobilize human and financial resources and absorb risks while adopting the new business model | Janssen et al., 2020, Mathauer and Hofmann, 2019, Sun et al., 2020, Khanijahani et al., 2022 | |
| Competitive advantage (ORG5) | It pertains to technology adoption due to the existing competitive advantage achieved by firms | Chu et al. (2018); Saberi et al. (2019a), Pan et al., 2020, Beaulieu and Bentahar, 2021 | |
| Organizational culture (ORG6) | It refers to the pattern of shared values and beliefs that provide an understanding of organizational functioning and the norms for acceptable behavior witorganizationnisation | Ghadge et al., 2020, Xia et al., 2019, Khanijahani et al., 2022 | |
| Financial Resources (ORG7) | It refers to the availability of adequate finances to undertake technological adoption | Kiel et al., 2017, Kusi-Sarpong et al., 2019, Gardas, 2022 | |
| Institutional (INT) | Government support and policy framework (INT1) | It indicates government support in terms of credit availability, staff training, technical advice, support infrastructure, and conducive policy framework | Yadav et al., 2020, Tsai et al., 2019, Singh et al., 2019, Alrahbi et al., 2021 |
| Ecosystem management (INT2) | It lays down the approach toward complex interaction and integration amongst several domains and participants | Wong et al., 2020, Santoro et al., 2018, Clohessy and Acton, 2019 | |
| Effective collaboration with partners and stakeholders (INT3) | It ascribes effective collaboration with internal and external stakeholders | Kamble et al., 2019, Luthra et al., 2020; Balasubramanian et a., 2021 | |
| Competitive pressure (INT4) | It refers to the promptness towards adoption of technological innovation arising out of the pressure due to intense rivalry between industry players | Chu et al., 2018, Chang, 2020, Alrahbi et al., 2021 | |
| Demand volatility for health care supply chain sector (INT5) | It engulfs the various factors that impart volatility in demand for the healthcare supply chain | Polater and Demirdogen, 2018, Lawrence et al., 2020 | |
| Human (HUM) | User desirability at the implementation stage (HUM1) | It directs attention to the user's intention and desirability to adopt a new technology | Naszay et al., 2018, Cocosila and Turel, 2019, Roberts et al., 2019, Balasubramanian et al., 2021 |
| Customer acceptance and loyalty (HUM2) | For adoption to be successful, this dimension highlights customer acceptance in terms of continued use (post-adoption) and loyalty towards technology adoption. | Mathauer and Hofmann, 2019, Nysveen et al., 2020 | |
| Human resource team competence and training for AI integration (HUM3) | It refers to the availability of human capital with expertise in technical matters and technology management. It would also take into account the training facilities and opportunities being extended to existing team members | Tortorella et al., 2020, Sivathanu and Pillai, 2018, Gardas, 2022 | |
| Behavioral Intention (HUM4) | It refers to the formulation of conscious plans toward a specified future behavior | Holzmann et al., 2020, Sharma, 2019, Chopdar et al., 2018 | |
| Assurance of job security post-AI adoption (HUM5) | It directs attention to the technological unemployment and security of work as an outcome of AI adoption | Kamble et al. (2019b), Nam, 2019, Wang et al., 2019; |
2.3.1. Technological context
Technological context incorporates technology characteristics and benefits (internal and external), accruing improved productivity and operational efficiency (Ahuja et al. 2020). Technological feasibility for AI implementation is critical as it determines the potential economic viability of technology adoption and provides inputs to technology validation plans (Tseng et al., 2018). The level of technological sophistication is another factor that clarifies the technical community's need to improve the existing state of technology or create/adopt newer versions to settle latency, security, and throughput (Bogart and Rice, 2015). Sustainable data quality and integrity are critical factors for successfully implementing disruptive technologies (Wang et al., 2019). Therefore, overcoming the potential vulnerabilities while having clearly defining security goals in the healthcare system is crucial. Another strategic factor in the technological context is interoperability which would entail smooth communication between users/businesses/ public entities resulting in increased efficiency (Governatori et al., 2018). Perceived benefits from AI adoption in a supply chain may lead to reduced delivery delays and frauds (Rodríguez-Espíndola et al., 2020), enhanced transparency and efficiency (Dwivedi et al., 2019a), cost reduction (Baryannis et al., 2019), and competitive advantage (Webster and Ivanov, 2020).
2.3.2. Organizational context
Apart from the technological context, the organizational dimension comprising varied organizational conditions holds great importance towards successful AI adoption (Bala and Feng, 2019). Organizational leadership and support are crucial for technology adoption (Yang et al., 2015), with past research (Cao et al., 2020) reporting higher adoption benefits as an outcome of solid support. Another factor enhancing the likelihood of AI adoption is the strategic alignment between business and AI adoption, as it is crucial to align the business case of technology adoption with the organization's strategic vision (Shao, 2019). Firms’ readiness can be another critical factor as it would ensure the availability of required resources for AI adoption (Pacchini et al. (2019). Within the organizational context, firm size and organization structure can influence the adoption of disruptive technologies via the availability and access to financial and technical resources (AlBar and Hoque, 2019). In addition to these factors, the competitive advantage generated by companies due to their prompt actions and strategies can be a driver for technology adoption (El-Kassar and Singh, 2019). Further, an organizational culture encouraging experimentation, empowering employees, and creating effective relationships amongst internal members (Horváth and Szabó, 2019) would enable AI implementation. Additionally, the availability of financial resources can be one of the significant factors enabling technology adoption (Mikalef et al., 2020).
2.3.3. Institutional context
The institutional context comprising the environment surrounding the organization like competitors, regulatory bodies, external stakeholders, and demand fluctuations affects technology adoption (Tsai et al. 2019). Government support and policies on compliance, intellectual property, consumer protection, and the like would reduce ambiguity, instill confidence and assist organizations in adopting disruptive technologies (Luthra et al., 2020). The presence and effective management of ecosystems are essential factors enabling AI adoption as they would reduce barriers and initial investments, enabling developers and businesses to undertake innovation while attracting the critical mass of users (Wamba and Queiroz, 2020). Successful adoption of AI in the supply chain would necessitate an effective collaboration with partnering firms, competitors, government, and domain experts (Ashaye and Irani, 2019, Stević et al., 2020). Further, a competitive environment can be a vital influencer for adopting technologies as it would influence firms’ ability to compete in the marketplace (Mero et al., 2020). Due to the changing economic environment, market unpredictability, supply chain risk and uncertainty, political instability, and other factors, supply chains in healthcare suffer from demand volatility, another critical factor influencing technology adoption (Singh et al., 2019).
2.3.4. Human context
Human and behavioral aspects offer another context for technology adoption (Gao and Sunyaev, 2019). Here user desirability is an essential factor as it involves an evaluation of technology adoption by users’ (Tumasjan and Beutel 2019) and extends to their values and ethical perception (Dwivedi et al., 2019b). Customer acceptance and loyalty capture the users’ actions/decisions towards future use as generated by perceived usefulness and ease of use (Lu et al. 2019) and are thus another significant factor influencing technology adoption. Being determined by attitude, norms, and perception of control over the behavior, behavioral intention refers to the formulation of prearranged plans towards a specified future behavior and is another factor influencing AI adoption (Mahardika et al., 2019). Training human resources and developing competence via upgrading technical and analytical skills while developing capabilities for organizational changes would be critical for successful adoption and generating better results from implementing disruptive technologies (Darko et al., 2018). While there is controversy in the literature on disruptive technologies giving rise to technological unemployment or replacing the existing nature of work, assurance of job security post AI adoption can influence the AI usage HSC (Zeng et al. 2020). Table 1 depicts the significant CSFs and sub-CSFs based on the TOEH framework.
2.4. Research gaps and contributions
The healthcare sector was initially hesitant to integrate disruptive technologies or system digitalization, but, with demonstrated potential impact on supply chain activities, AI, blockchain, and big data analytics technologies have found a place in their operational activities (Kumar et al., 2020). Supply chain management activities are critical organizational activities, and AI technologies are thought to improve supply chain activities by eliminating redundant bottlenecks and increasing transparency, resilience, and agility in the supply chain activities. Though the implementation of AI technology benefits the healthcare supply chain, there is a significant acceptance gap in the digitalization of the healthcare sector. There is less evidence in the literature discussing the critical success factors of HSC -AI adoption comprehensively. Table 2 depicts the main studies investigating the digitalization of healthcare.
Table 2.
Summary of research gaps and contribution of our study.
| Authors | Contribution | Methodology | Research Gap | Our Contributions |
|---|---|---|---|---|
| Zhang et al. (2017) | Developed supplier’s CSR capabilities in a pharmaceutical supply chain | Case study | Lack of empirical validation of findings. | As this study expands the literature in the healthcare supply chain, we see a growing need to understand how digitalization enables HSC and how these case studies play a role in AI technology adoption. As AI adoption is in its nascent stage, especially in the context of HSC, it lacks a decision support system framework that uses an integrated theoretical as well as MCDM approach (i.e., TOEH framework and novel rough-SWARA), which can assist various stakeholders in understanding the importance of Key Success Factors (CSFs) for the successful AI adoption in HSC. Therefore, it is of great importance for HSC practitioners to understand the potential of AI adoption. Furthermore, this study partially addresses the need by Nguyen et al. (2021) for future studies on the need for additional empirical investigation of AI adoption in the transition to an HSC. |
| Wang et al. (2018) | Examined intricacies of big data analytics in healthcare organizations | Content analysis | Lack of focus on the human dimension. | |
| Marques et al. (2020) | Conducted meta-synthesis of current research in supply chain management in the healthcare sector | Systematic Literature Review | Addressing network-level analysis of flows | |
| Rehman and Ali (2021) | Prioritized resilience strategies for healthcare supply chains | Fuzzy analytical hierarchy process (AHP) | Conducted in a general perspective. | |
| Beaulieu and Bentahar (2021) | Identified initiatives for the digitalization of HSC | Literature review | Validation of research findings from decision-makers. | |
| Chauhan et al. (2022) | Identified and grouped vital success factors relevant to telemedicine services | DEMATEL, BWM, VIKOR | Absence of interrelations of crucial success factors within each criterion. | |
| Saha et al. (2022) | Investigated the role of emerging technologies on pharmaceutical supply chain performance | Structural Equation Modeling | In this study, the authors addressed the barriers to emerging technologies but lacked a clear framework for critical success factors for technology adoption. |
3. Research methodology
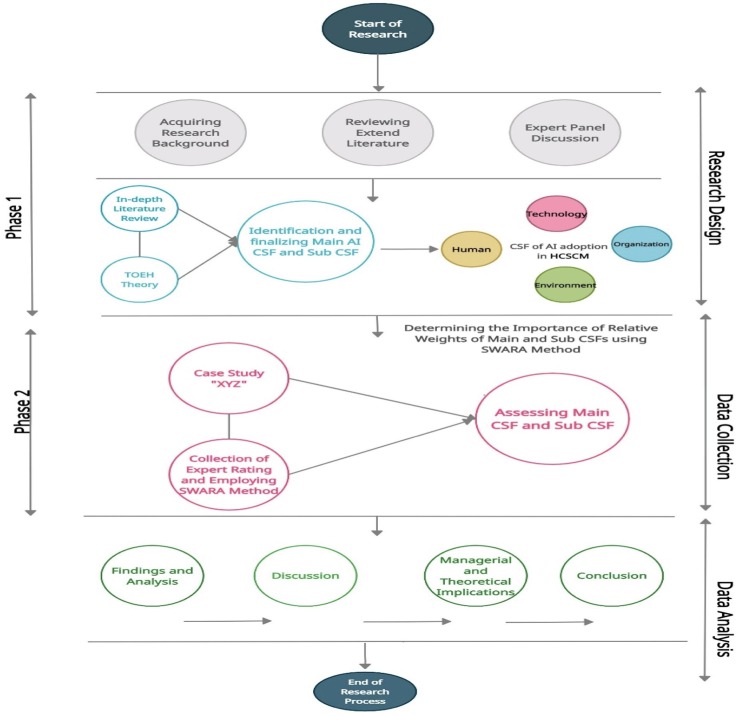
The proposed research framework used in this study for prioritizing CSFs of AI is by determining the importance weight of the health care supply chain in emerging economies especially in the Indian context, using rough SWARA (R-SWARA), as depicted in Fig. 1 .
Fig. 1.
Research Framework.
As discussed in the literature review section, adopting AI and its usability would significantly contribute toward effective and resilient HSC. In this study, comprehensive know-how of the critical factors would facilitate decision-makers to make robust-decision by determining the relative importance of identified CSFs of AI adoption in HSC using R-SWARA. This study is a pioneering attempt to identify CSFs of AI adoption and then categorize them based on TOE and HOT frameworks.
3.1. Rough Step-wise weighted assessment ratio analysis (R-SWARA)
R-SWARA method developed by Zavadskas et al. (2018) is mainly used for determining the relative weights of the attributes by using rough numbers to reduce the subjectivity and uncertainty in complex decision-making problems. In recent times, R-SWARA has gained popularity among researchers and practitioners, and it has been noticed lately that many studies address research problems by applying hybrid frameworks associated with MCDM (multiple criteria decision making) and rough set numbers. For instance, under uncertainty, Zavadskas et al. (2018) used rough SWARA as a novel MCDM approach in the logistics sector. Vasiljević et al. (2018) employed to evaluate the criteria for supplier selection in the textile industry. Sremac et al. (2018) used it to rank third-party logistics providers. Stefanović et al. (2019) used rough SWARA to rank and prioritize the influential safety factors for developing occupational safety and health (OSH) climate. Further, Ulutas (2020) used for the evaluation of selection criteria for logistics service providers. Currently, it is evident in the existing literature that no study has been done focused on analyzing the CSFs of AI adoption in the health care supply chain by utilizing the application of R-SWARA. Compared to popular MCDM techniques like AHP, ANP, and Best-Worst Method, the method R-SWARA is less complex for analyzing domain experts' knowledge and judgment scores to evaluate the relative significance weights of the CSFs (Hashemkhani Zolfani et al., 2018). The benefits of this approach are: Firstly, it calls for much fewer pair-wise comparisons amongst elements while contrasted with different MCDM techniques. Secondly, the SWARA approach is the likelihood of estimating domain experts or vested opinions on the critical factors' significance ratio in the relative weight assessment process (Karabasevic et al., 2016). Additionally, this technique proved decisive for determining the significance ratio of identified decision-making criteria.
The R-SWARA method consists of the following steps (Zavadskas et al., 2018):
Step 1: Define a set of attributes or CSFs that participate or strive for the decision-making process.
Step 2: Establish a team of “k” experts who will rate or rank the attribute according to their relative importance, from the highly significant to the least significant attribute. Next, “Sj” is determined in such a way, starting with the second attribute or criterion, that we can determine how vital criterion C1 is compared to criterion C1-n.
Step 3: In this step, every individual response of each expert (K1, K2 ……. Kn) is converted into a rough matrix (Cj) using equations (1) – (6) mentioned by Zavadskas et al. (2018).
| (7) |
Step 4: In this step, normalization can be done of matrix in order to determine the matrix by using equation (8).
| (8) |
Using equation (9), we can determine the matrix elements of matrix
| (9) |
The first element of matrix , i.e., =, because . For other elements equation (9) can be calculated using equation (10):
| (10) |
Step 5: In this step, calculate the matrix by using equation (11)- (12).
| (11) |
| (12) |
Step 6: In this step, re-calculated matric can be obtained using equation (13), (14).
| (13) |
| (14) |
Step 7: Finally, the relative importance weights matrix are calculated using equation (15).
| (15) |
4. Case study
The Healthcare industry is recognized as one of the largest and fast-growing sectors in most emerging nations and plays a vital role in any nation’s economy. Although, emerging nations are strategic destinations for big investors due to their rapid growth potential (Cook, 2019). Innovations and integration of disruptive technologies (such as artificial intelligence (AI), blockchain technology (BT), the internet of things (IoT), and machine learning (ML)) promise to achieve value-added service in this sector. With its vast inequalities in healthcare operation and supply chain management, it encountered with lack of innovative healthcare infrastructure and low monetary support and investment from authorities. India is one of the top emerging economies having space for adopting innovative, sustainable, and scalable technologies to reduce the risk of healthcare supply chain disruption. However, in a country like India, there is an extensive digital divide, and growing disparities in healthcare access and delivery between urban and rural areas due to large geographical areas and the high population is often a challenge that AI has the potential to alleviate (Ajmera and Jain, 2019). Due to that, AI implementation in HSC is still in its nascent stage. An emerging economy such as India is uniquely positioned to be a leader in adopting AI technologies in HSC that considers local constraint for more affordability (Rao and Clarke, 2020). The adoption of AI technologies can potentially change the future of Indian HSC. However, there are certain factors like organization preparedness, technology understanding, skilled human resource, data standardization, cybersecurity, and most importantly, a legal implication that needs to be focused on prior to implementing AI technologies in their operation and supply chain management; otherwise, no organization may encounter challenges of integrating AI with the healthcare supply chain.
4.1. Participants profile
This study uses the mixed-method (qualitative and quantitative) approach to analyze the CSFs of AI adoption in the Indian healthcare industry. The study involved an extensive literature review and expert opinions for identifying and finalizing various CSFs related to AI adoption in the healthcare supply chain in an emerging economy context. Initially, questionnaires were designed to collect feedback from managers of Indian healthcare companies with a minimum work experience of 10 years in decision making. A team of twenty experts comprised of logistics and supply chain managers, information technology (IT) managers, senior level managers, strategy managers, and academic experts are used for the study. The experts’ information is depicted in Table 3 .
Table 3.
Expert profile information.
| Expert | Expertise /Background | Experience (years) | Sector/Organization Type | Location |
|---|---|---|---|---|
| Expert 1 | Senior level Supply chain manager | 14 | Healthcare company | Delhi |
| Expert 2 | Technology support manager | 13 | Medicare devices company | Delhi |
| Expert 3 | General Manager IT | 15 | Pharmaceutical Industry | Baddi (Himachal Pradesh) |
| Expert 4 | Senior level Logistics manager | 15 | Pharmaceutical Industry | Baddi (Himachal Pradesh) |
| Expert 5 | Senior level Logistics manager | 13 | Medicare devices company | Noida |
| Expert 6 | Deputy Manager IT infrastructure | 12 | Technology Solution Providers | Gurugram |
| Expert 7 | Ph.D. (Health-care Chain Management) | 12 | Academics | Delhi |
| Expert 8 | General manager Strategy | 13 | Healthcare company | Noida |
| Expert 9 | Deputy Manager IT | 15 | Technology Solution Providers | Bangalore |
| Expert 10 | Middle-level logistics manager | 10 | Healthcare equipment supplies company | Noida |
| Expert 11 | Middle-level Logistics manager | 11 | Healthcare equipment supplies company | Noida |
| Expert 12 | Ph.D. (Health-care Chain Management) | 13 | Academics | Delhi |
| Expert 13 | Deputy Manager IT infrastructure | 15 | Technology Solution Providers | Gurugram |
| Expert 14 | Middle level Logistics manager | 12 | Healthcare equipment manufacturer | Noida |
| Expert 15 | Senior level Supply chain manager | 15 | Healthcare equipment manufacturer | Bangalore |
| Expert 16 | Deputy Manager IT infrastructure | 15 | Technology Solution Providers | Bangalore |
| Expert 17 | General manager Strategy | 14 | Pharmaceutical Industry | Baddi (Himachal Pradesh) |
| Expert 18 | General manager Strategy | 14 | Healthcare & Hospital service | Delhi |
| Expert 19 | Ph.D. (Health-care Chain Management) | 13 | Academics | Delhi |
| Expert 20 | General manager Strategy | 14 | Healthcare & Hospital service | Delhi |
4.2. Identification and finalization of CSFs of AI adoption in the healthcare supply chain (HSC)
In this phase, extensive literature review and experts’ judgment were employed to identify and finalize CSFs of AI adoption in HSC. The initial identified list of CSFs has been brought to the experts’ panel for dialogue to peer the relevance of contemporary AI adoption via consensus building. The initial list was further reduced to twenty-two CSFs of AI adoption in HSC after various rounds of deliberation with an experts’ panel. After that, the experts’ panel was asked to group the finalized CSFs into the main dimensions based on the adopted TOEH framework: Technological, Organizational, Environmental, or Institutional, and Human dimensions. Finally, Table 1 depicts the main CSFs and sub-CSFs with a detailed description.
4.3. Calculation of the weight score of the CSFs of AI adoption in HSC using the rough SWARA method
This section used the novel rough-SWARA method to analyze the experts' rating to determine the relative weight and ranking of leading dimension CSFs and sub-dimension CSFs of AI adoption in HSC. The experts' rating was collected through a survey questionnaire and administrated with the help of a prescribed matrix suggested by Yazdani et al., 2018. In this study, twenty experts were requested to determine which main dimension of CSF was the most important and then compare it with others for its significance. The assessment rating given by each expert is presented in Table 4 .
Table 4.
Individual rating of main dimension CSFs of AI adoption by all experts.
| Experts | E1 | E2 | E3 | E4 | E5 | E6 | E7 | E8 | E9 | E10 | E11 | E12 | E13 | E14 | E15 | E16 | E17 | E18 | E19 | E20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TEC | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 3 | 1 |
| ORG | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 3 | 3 | 4 | 4 | 4 | 3 | 4 | 4 | 4 | 3 | 3 | 3 | 3 |
| INT | 2 | 2 | 2 | 2 | 1 | 3 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 3 | 2 | 1 | 2 | 2 | 1 | 2 |
| HUM | 2 | 3 | 3 | 3 | 3 | 3 | 3 | 2 | 2 | 3 | 3 | 3 | 4 | 2 | 3 | 3 | 4 | 3 | 2 | 4 |
Based on the expert assessment, seventeen out of twenty experts identified the technological (TEC) CSF as the critical CSF among other main CSFs of AI adoption in HSC. The organizational CSF (ORG) was recognized as the least important by thirteen experts, while the human factor (HUM) was marked twice as the least essential CSF in the main dimension category. In the next step, we convert all the individual ratings into a rough group matrix based on the above rating using equation (7) presented in Table 5 .
Afterward, the value of normalized rough group matrix is obtained by employing equations (8), (9). In this step, the least CSF has the maximum value per the value derived from the rough group matrix. It is said that the most significant CSF is equal to one, while other CSFs of the same matrix divided them by the maximum value, i.e., = [3.275, 3.797] in this case.
In this step, all the CSFs of the normalized rough group matrix should be added by one except the value of by applying equation (12). The obtained matrix is presented in Table 6 .
Table 5.
Rough group matrix for all major CSFs of AI adoption in HSC.
| [1.220, 1.400] | |
|---|---|
| [1.917, 2.283] | |
| [2.500, 3.250] | |
| [3.360, 3.840] |
Table 6 Represents the values of matrix for all major CSFs of AI adoption in HSC.
Table 6.
Values of RN (Kj)j) Matrix.
| [1.000, 1.000] | |
|---|---|
| [1.500, 1.680] | |
| [1.651, 1.967] | |
| [1.875, 2.142] |
Next, all the values of matrix are recalculated by applying equation (14) to determine the value of matrix . To obtain the value of matrix , we follow the condition mentioned in equation (14) that defines “j – 1” represents the previous attribute in relation to j.
Finally, the relative importance, weight, and ranking of main dimension CSFs are obtained using equation (15), as shown in Table 7 . The calculation of matrix is presented below.
Table 7.
Relative importance weight of main dimension CSFs of AI adoption in HSC.
| Main CSF | Weights |
Crisp | Rank | |
|---|---|---|---|---|
| min | max | |||
| TEC | 0.439 | 0.491 | 0.465 | 1 |
| ORG | 0.062 | 0.105 | 0.084 | 4 |
| INT | 0.259 | 0.326 | 0.293 | 2 |
| HUM | 0.134 | 0.196 | 0.165 | 3 |
Similarly, all the experts were requested to rate the most significant and least significant among sub-dimension CSFs category. Individual responses for all the sub-dimension CSFs by all the experts determine the weight of all sub-dimension categories and are presented in Appendix (Table A1-A4). Finally, the global weight or global ranking of all the main dimensions and sub-dimension CSFs of AI adoption in HSC was calculated using the rating of all the experts with the above calculations, presented in Table 8 .
Table 8.
Final ranking of CSFs of AI adoption in HSC.
| Main CSF | Local weight | Sub-CSF | Local weight | Global weight | Global ranking |
|---|---|---|---|---|---|
| TEC | 0.465 | TEC1 | 0.410 | 0.191 | 1 |
| TEC2 | 0.097 | 0.045 | 9 | ||
| TEC3 | 0.277 | 0.129 | 2 | ||
| TEC4 | 0.049 | 0.023 | 13 | ||
| TEC5 | 0.170 | 0.079 | 5 | ||
| ORG | 0.084 | ORG1 | 0.263 | 0.022 | 14 |
| ORG2 | 0.332 | 0.028 | 12 | ||
| ORG3 | 0.179 | 0.015 | 16 | ||
| ORG4 | 0.064 | 0.005 | 20 | ||
| ORG5 | 0.035 | 0.003 | 21 | ||
| ORG6 | 0.115 | 0.010 | 18 | ||
| ORG7 | 0.017 | 0.001 | 22 | ||
| INT | 0.293 | INT1 | 0.286 | 0.084 | 4 |
| INT2 | 0.050 | 0.015 | 17 | ||
| INT3 | 0.099 | 0.029 | 11 | ||
| INT4 | 0.397 | 0.116 | 3 | ||
| INT5 | 0.176 | 0.052 | 7 | ||
| HUM | 0.165 | HUM1 | 0.179 | 0.029 | 10 |
| HUM2 | 0.405 | 0.067 | 6 | ||
| HUM3 | 0.047 | 0.008 | 19 | ||
| HUM4 | 0.282 | 0.046 | 8 | ||
| HUM5 | 0.094 | 0.016 | 15 |
5. Results and discussion
5.1. Results
In this study, with the help of available literature resources and various rounds of deliberations with industry experts, twenty-two CSFs of AI adoption in the HSC domain were considered for the analysis. The study identifies that the main dimension of CSF technological (TEC) has the highest weightage and is ranked the most influential factor impacting AI adoption of AI in HSC in emerging economies. However, institutional or environmental (INT), human (HUM), and organizational (ORG) dimensions have been found to rank second, third and fourth in the order of obtained weightage as presented in Table 8.
The results indicate that the technological (TEC) dimensions are crucial for AI adoption because it refers to the ability in terms of technology infrastructure and feasibility to implement or adopt AI at an organizational level. The second dimension, institutional (INT), plays a vital role in AI adoption as various external environmental factors like competitive pressure, market dynamics, and explicit and supportive regulatory framework act as driving factors for adopting AI in the healthcare supply chain. The human (HUM) dimension is next in line, which is also very critical CSF because the adoption of AI technologies in the healthcare supply chain is associated with human behavioral intention and acceptance by the customer. Last but not least, the organizational (ORG) dimension refers to the adoption of AI technology in the healthcare supply chain and is influenced by factors such as top management commitment, organizational readiness, culture, and strategic alignment between business viability and AI adoption.
The global ranking of the CSFs of AI adoption in the healthcare supply chain is presented in Table 8. Among sub-dimension CSFs, the top six prominent CSFs include Technology sophistication (TEC1), Sustainable data quality and integrity (TEC3), Government support and policy framework (INT1), Competitive pressure (INT4), Interoperability (TEC5), Customer acceptance and loyalty (HUM2), Demand volatility for health care supply chain sector (INT5), Behavioral Intention (HUM4), Technological testing and troubleshooting feasibility (TEC2) and Customer acceptance and loyalty (HUM2) in the order of their global ranks belong to all the major dimension CSF except organizational dimension considered in the study. Technology sophistication achieves the highest ranking CSF for AI adoption in the healthcare supply chain. Technology sophistication helps to understand the technical feasibility, maturity, and capabilities to address security, latency, and throughput that enable or actualize the adoption objectives (Agrawal and Madaan, 2021). The second highest ranked CSF for AI adoption in HSC is sustainable data quality and integrity. Possessing a higher degree of data quality and integrity enables smooth sharing of data among the supply chain partners from the public data repository (Kwon and Johnson, 2014). The third highly ranked CSF is government support and policy framework and positively impacts and provides enough support to healthcare companies by integrating AI technologies in their operation supply chain activities (Yadav et al., 2020). The fourth highly ranked CSF is under competitive pressure to adopt AI in the healthcare supply chain. In the case of emerging economies, especially in the Indian context, there is immense competition in the healthcare supply chain industry which can pose a severe threat of losing competitive advantage due to the large population and globalization (Saberi et al., 2019b; Pan et al., 2020). Interoperability, ranked fifth in the global ranking list, plays a vital role in AI adoption by determining the best path forward for reducing the number of repetitive administrative tasks at the implementing phase in the technology innovation decision-making process. Technical interoperability refers to the ability of two or more ICT applications to accept data from each other and perform a given task in an appropriately and satisfactorily manner without the need for extra operator intervention. Finally, the sixth-ranked critical success factor is customer acceptance and loyalty, a potential driver for adopting AI technologies in the healthcare supply chain (Roy et al., 2018).
5.2. Discussions of the study
Based on the findings of this study, technological factors are the most important among the other critical success factor for AI adoption in HSC. Technological sophistication (TEC1) is the highest CSF among sub-dimension CSFs. Technological maturity or sophistication is a critical factor within the healthcare supply chain which entails that effective utilization of technological tools can promote the adoption of AI in the supply chain (Agrawal et al., 2018, Khan et al., 2021). Sustainable data quality and data integrity (TEC3) was found to be the second most vital sub-dimension CSFs for AI adoption in the healthcare supply chain. A study by Ko et al. (2011) reported that data consistency and quality of information contribute to the system's reliability and security. Data integrity provides information on goods flow in the supply chain using different devices, including barcodes, inventory serial numbers, and digitally encrypted RFID sensors (Tian, 2016). Therefore, the collection and development of secured data from all sources are significant for the successful implementation of AI. Interoperability (TEC5) ranked third among other technological sub-dimension CSF and held the fifth in the global ranking. Data interoperability refers to the processing and interpreting received data to facilitate smooth communication between different stakeholders such as manufacturers, suppliers, vendors, and customers that can foster smooth adoption of AI in the supply chain (Dobrovnik et al., 2018, Wang et al., 2019). Finally, perceived benefits (TEC2) were critical to raising consciousness on the advantages of AI usability among their target supply chain firms, hence improving the adoption rate (Yadegaridehkordi et al., 2018). Thus, AI should offer healthcare supply chain firms a comprehensive solution that can provide more effective data storage and analytical tools for decision-making in real-time situations.
Institutional (INT) factors hold the second position in the significant CSFs of AI adoption in the health care supply chain (HSC), as presented in Table 8. Under the institutional dimension, the sub- CSFs are prioritized as follows: competitive pressure (INT4) > government support and policy framework (INT1) > demand volatility for health care supply chain sector (INT5) > effective collaboration with partners and stakeholders (INT3) > ecosystem management (INT2). According to the global ranking, competitive pressure (INT4) ranked first among other institutional critical success factors, which is recognized as one of the fundamental driving forces to adopt disruptive technologies to achieve a resilient healthcare supply chain (Chang, 2020). This is in line with the popular institutional theory that a firm would imitate other similar firms’ operations in its operational and strategic decisions (Nilashi et al., 2016). Government support and policy framework (INT1) ranked second on the priority list. Generally, healthcare supply chain (HSC) companies have restricted admittance and control over the compliance structure administered by government agencies. Consequently, appropriate guidelines and adequate financial subsidizing can support the utilization of AI technologies in the healthcare supply chain (Alreemy et al., 2016; Singh et al., 2019). Afterward, demand volatility (INT5) ranked third under institutional factors. To avoid vulnerability and unpredictability of market demand for healthcare supplies, firms must expect to integrate disruptive technologies like AI, machine learning (ML), and data analytics to demonstrate the elevated level of deftness because of erratic vacillations sought after. Finally, effective collaboration with partners and stakeholders (INT3) and ecosystem management (INT2) ranked fourth and fifth in the institutional CSFs category list.
Human factors hold the third rank among AI implementation's major critical success factors in the healthcare supply chain sector. Under the human success factors dimension, sub-CSFs are prioritized in order as follows: customer acceptance and loyalty (HUM2) > behavioral intention (HUM4) > user desirability at implementation stage (HUM1) > assurance of job security post-AI implementation (HUM5) > human resource team competencies for AI integration (HUM3). According to the study, customer acceptance and loyalty (HUM2) earned the highest ranking among other sub-dimension critical success factors. According to a report by Nguyen (2013), healthcare organizations should pay more attention to customer acceptance and loyalty. A study by Kamble et al. (2019) suggested that businesses can be achieved competitive advantages by reaping the maximum benefits of AI implementation in their supply chain activities by reducing demand forecasting errors, improving product traceability, and improved delivery cycles. Behavioral intention (HUM4) ranked second among other human sub-dimension success factors. A recent study by Holzmann et al. (2020) aligned with our findings that the behavioral intentions of healthcare professionals about using AI technologies are the most potent indicator of users’ intention. User desirability at the implementation stage (HUM1) ranked third in the list. This implies that the willingness of the top management typically directs employees' and lead resources' commitment to innovation during AI implementation, resulting in improved or real-time quality planning and leadership strategies to increase firm supply chain efficiency. Assurance of job security post-AI adoption (HUM5) and human resource team competence and training for AI integration (HUM3) ranked fourth and fifth among other human sub-dimension CSFs.
Organizational factors hold the last rank in the main-dimensions critical success factors for adopting AI technologies in the HSC context. As per the analysis, Strategic alignment between business viability and AI adoption (ORG2) has the highest rank. According to Becker and Schmid (2020), aligning business viability and AI adoption strategies is long-term growth and change phase that encompasses not only firm-level strategy and IT strategy but also company infrastructure and processes, as well as AI infrastructure and processes. Findings suggest that the strategic use of IT would allow the company to retain its competitive advantage (Zaki, 2019, Reddy et al., 2021). Secondly, organizational leadership and support (ORG1) can substantially impact AI adoption for articulating an organizational vision and mission, providing sufficient funds, and allocating desirable resources (Gutierrez et al., 2015). Organizational readiness (ORG3) can be another critical factor as it would ensure the availability of required resources for AI adoption (Pacchini et al., 2019). Organizational culture (ORG6) ranked fourth critical success factor among other sub-dimensions CSFs for AI adoption in the healthcare supply chain. Our finding, in line with Horvath and Szabo (2019), suggested that organizational culture facilitates an environment for shared values and beliefs among employees, provides a platform for upgrading skills, encourages experimentation, and enables strong relationships among top management and lower management employees. Within the organizational context, firm size and organization structure (ORG4) can influence the adoption of disruptive technologies via the availability and access to financial and technical resources (AlBar and Hoque 2019).
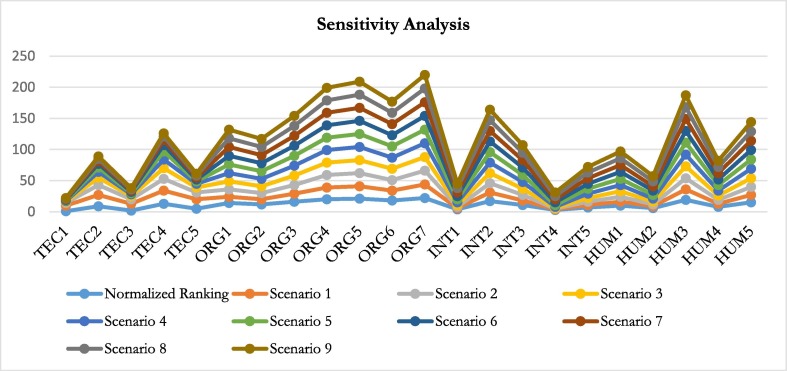
5.3. Sensitivity analysis
The technological component (TEC) is positioned as the most significant among all the critical dimension CSFs category in this investigation using rough-SWARA. In this way, the incremental addition of 0.1 from run 1 to run 9 changes the relative importance weight of technological CSFs (Kumar & Dixit, 2019). As a result, adjustments must be made for other main dimensions CSFs simultaneously. Table 9 lists the relative relevance weights for the other main dimension CSFs utilizing sensitivity analysis. The relative importance weight and rankings of the sub-dimension CSFs are altered due to the incremental addition to the relative weights of the main dimensions CSFs presented in Table 10 . When the weight of the technological factor (TEC) is changed from run 4 to run 9, (TEC1) dominates the sensitivity analysis at that time. Similar to this, when the weight is changed from run 5 to run 9, (TEC3) follows closely behind (TEC5) in holding the third position. (ORG7) contains the last place and is shown in Fig. 2 during different weight adjustments from run 1 to run 9. Therefore, it is generally assumed that while developing short-term strategies for implementing AI technologies in the healthcare supply chain, stakeholders' decision-making processes should prioritize technological CSFs. Therefore, the study's findings can be used for decision-making because they stand up to expert scrutiny.
Table 9.
Sensitivity Analysis of main CSFs dimension.
| CSFs | Normalized | Scenario1 | Scenario 2 | Scenario 3 | Scenario 4 | Scenario 5 | Scenario 6 | Scenario 7 | Scenario 8 | Scenario 9 |
|---|---|---|---|---|---|---|---|---|---|---|
| TEC | 0.465 | 0.100 | 0.200 | 0.300 | 0.400 | 0.500 | 0.600 | 0.700 | 0.800 | 0.900 |
| ORG | 0.084 | 0.141 | 0.125 | 0.110 | 0.094 | 0.079 | 0.063 | 0.048 | 0.032 | 0.017 |
| INT | 0.293 | 0.490 | 0.436 | 0.382 | 0.328 | 0.274 | 0.220 | 0.166 | 0.112 | 0.058 |
| HUM | 0.165 | 0.276 | 0.246 | 0.215 | 0.185 | 0.154 | 0.124 | 0.093 | 0.063 | 0.033 |
Table 10.
Represent the changes in ranking using sensitivity analysis.
| Sub-CSF | Normalized Ranking | Scenario 1 | Scenario 2 | Scenario 3 | Scenario 4 | Scenario 5 | Scenario 6 | Scenario 7 | Scenario 8 | Scenario 9 |
|---|---|---|---|---|---|---|---|---|---|---|
| TEC1 | 1 | 9 | 4 | 2 | 1 | 1 | 1 | 1 | 1 | 1 |
| TEC2 | 9 | 18 | 16 | 12 | 9 | 7 | 6 | 4 | 4 | 4 |
| TEC3 | 2 | 11 | 7 | 5 | 3 | 2 | 2 | 2 | 2 | 2 |
| TEC4 | 13 | 21 | 19 | 17 | 14 | 13 | 10 | 8 | 6 | 5 |
| TEC5 | 5 | 15 | 11 | 8 | 6 | 4 | 3 | 3 | 3 | 3 |
| ORG1 | 14 | 10 | 12 | 13 | 13 | 14 | 14 | 14 | 14 | 14 |
| ORG2 | 12 | 8 | 10 | 11 | 12 | 12 | 13 | 13 | 13 | 13 |
| ORG3 | 16 | 13 | 14 | 15 | 16 | 16 | 16 | 16 | 16 | 16 |
| ORG4 | 20 | 19 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 |
| ORG5 | 21 | 20 | 21 | 21 | 21 | 21 | 21 | 21 | 21 | 21 |
| ORG6 | 18 | 16 | 17 | 18 | 18 | 18 | 18 | 18 | 18 | 18 |
| ORG7 | 22 | 22 | 22 | 22 | 22 | 22 | 22 | 22 | 22 | 22 |
| INT1 | 4 | 2 | 2 | 3 | 4 | 5 | 5 | 6 | 7 | 7 |
| INT2 | 17 | 14 | 15 | 16 | 17 | 17 | 17 | 17 | 17 | 17 |
| INT3 | 11 | 7 | 9 | 10 | 11 | 11 | 12 | 12 | 12 | 12 |
| INT4 | 3 | 1 | 1 | 1 | 2 | 3 | 4 | 5 | 5 | 6 |
| INT5 | 7 | 4 | 5 | 6 | 7 | 8 | 8 | 9 | 9 | 9 |
| HUM1 | 10 | 6 | 8 | 9 | 10 | 10 | 11 | 11 | 11 | 11 |
| HUM2 | 6 | 3 | 3 | 4 | 5 | 6 | 7 | 7 | 8 | 8 |
| HUM3 | 19 | 17 | 18 | 19 | 19 | 19 | 19 | 19 | 19 | 19 |
| HUM4 | 8 | 5 | 6 | 7 | 8 | 9 | 9 | 10 | 10 | 10 |
| HUM5 | 15 | 12 | 13 | 14 | 15 | 15 | 15 | 15 | 15 | 15 |
Fig. 2.
Variation in CSFs.
5.4. Validation of the finding through experts’ feedback
Feedback was gathered from the experts to validate the study's findings. They were chosen randomly (General Manager Strategy, Deputy Manager IT, IT Solution Providers, Healthcare Supply Chain Manager, Logistics Manager). The experts were shown the finished CSFs list and the final aggregated significance weights and associated rankings of the key critical success factors relevant to HSC.
The experts validated the study's findings and emphasized the importance of “technological” parameters CSFs for Adoption in HSC. Technology sophistication (TEC1), Sustainable data quality and integrity (TEC3), and Interoperability (TEC5), in his perspective, are critical. Experts also acknowledged that “government support and policy framework (INT1)” was in line with Luthra et al. (2020) that government assistance and policies on intellectual property, consumer protection, and other related issues would eliminate ambiguity, establish trust, and aid organizations in embracing disruptive technologies in their supply chain. Followed by “competitive environment (INT4)” can have a significant impact on technology adoption since it affects enterprises' capacity to compete in the market (Mero et al., 2020). Overall, the experts considered technological, institutional or environment, and human CSFs equally significant for adopting AI in HSC (Table 8). They noted the low ranking of organizational CSFs contributing towards AI implementation.
6. Implications
6.1. Theoretical contributions
The study aims to investigate CSFs of adopting AI in HSC using R-SWARA. Although previous studies have explored the benefits and challenges of AI adoption in the supply chain (Onik et al. 2019), there is a paucity of academic work undertaken to examine the CSFs of AI implementation in HSC. The present study is the first attempt to identify CSFs of AI adoption by categorizing them based on TOE and HOT frameworks. Our first contribution from theoretical and practical standpoints is that the findings of this study can generate focal points for achieving organizational objectives. In an increasingly competitive marketplace, companies in the HSC domain can better understand the drivers of technological adoption, make robust decisions, and prevent instances of losing their competitive edge.
The findings of this study suggest that technological feasibility, sustainable data quality and integrity, competitive pressure, government support, and policy framework are significant factors that facilitate the implementation of AI technology in HSC. While critically examining the potential application of blockchain technology in supply chain management, Saberi et al. (2019b) mentioned that technological feasibility is one of the prominent barriers hindering technology adoption. A recent study by Wong et al. (2020) on small and medium enterprises in Malaysia suggests that data quality, integrity, and competitive pressure significantly affect the adoption of disruptive technologies. Such an outcome is in alignment with the results of our study. Further, our research underlines the importance of government support and regulatory framework, which has also been identified as a key dimension for technology adoption by Dwivedi et al. (2019a). However, our findings of the relatively low prominence of financial resources as a factor for AI adoption in HSC contradict the results of Kusi-Sarpong et al. (2019). They ranked financial availability for innovation as the most relevant innovation cum adoption criterion. This may be due to higher importance assigned to other organizational factors like management leadership and support and organizational readiness. Also, the financial resources as tangible as against intangible resources like leadership and support, which affect AI adoption in supply chain management. Similarly, the influence of competitive advantage on technology adoption has been documented in earlier studies (Chiu & Yang, 2019). It contrasts with our findings as a competitive advantage has been assigned the second least significant ranking. This may be owing to the increasing body of knowledge that advocates that competitive advantage is not limited to a firm versus another context; instead, it can also be derived from one supply chain competing with the other.
The following contribution of our study is that it has methodically investigated CSFs of AI implementation in the Indian health care industry. Although past studies have reviewed the challenges and drivers of AI adoption in the supply chain, our study is different in approach and context. It amalgamates the TOE and HOT framework- TOEH to assess the CSFs. By reviewing the findings of this study, managers and practitioners in HSC can emphasize the relative prominence assigned to each factor which may reduce the complexities involved in AI adoption.
6.2. Managerial implications
From a managerial perspective, the study reviews the success factors in enhancing effectiveness and gaining cost efficiency in the supply chain by adopting AI technology in the healthcare industry. The paper focuses on four key dimensions- technological, organizational, institutional, and human and thus extends a comprehensive framework to managers in India and other emerging economies in the HSC industry.
Even though the study has adopted the TOEH framework, it recognizes managers’ limitations on extending equal attention and devoting similar resources to all the dimensions and sub-dimensions for AI implementation. Thus, the rankings generated in this paper assign higher importance to the technological dimension, followed by institutional and human, with the least importance assigned to the organizational dimension. Based on this study’s findings, managers can anticipate their weaknesses, so they can easily focus on these areas and try to overcome lacuna in their firm and achieve supply chain sustainability. In addition, managers can review the viability of technology adoption and focus on data quality and integrity to maintain market competitiveness. Also, collectively, managers can persuade the government to extend support in credit availability, technical know-how, coordinating infrastructure, and staff training as government support and policy framework emerged as another significant sub-dimension in this study.
In terms of practical applications, this study shows that an AI-based supply chain has vast potential to disrupt the Indian healthcare industry. From monitoring and tracking the healthcare equipment and vaccine across the supply chain, AI technologies have the potential to solve the complexities of the healthcare supply chain. Additionally, the adoption of AI in the Health care sector enables privacy and security to patient data which is a significant concern to the customer. Furthermore, the findings align with the National Digital Health Mission (NDHM) 2020 of the Government of India (GOI), making the country a digitally advanced nation by establishing cutting-edge healthcare systems to manage essential digital health data and the infrastructure needed for its seamless and agile supply chain.
7. Conclusions
This study applies CSF from the TOE and HOT frameworks to assess the ease of AI adoption in HSC in emerging economies. Businesses in developing countries are reporting fallibilities with the existing conventional supply chain models. Further, there is a greater will and preparedness by businesses in these countries to invest in healthcare and reap the benefits of technological innovations, particularly in supply chain management. Our study is timely as the impact of prevailing supply chain disruptions attributable to the spread of Covid-19 can be minimized by integrating technological innovations with the existing HSCs. This can enable practitioners to augment their competitive advantage while preventing adverse scenarios due to supply chain fallouts and market failures. Our study will likely extend an improved understanding of AI technology and address related issues impacting AI implementation in HSCs.
By incorporating the TOE and HOT framework, this paper suggests a theoretical model based upon the significant factors facilitating AI adoption in HSC. Further, R-SWARA was employed to evaluate the significance of coefficients based on experts’ knowledge, available information, and different experiences from the criteria. Our research findings indicate that technological feasibility, sustainable data quality, integrity, and competitive pressure are the leading sub-dimensions within the TOEH framework to facilitate AI implementation in HSC. The study can help healthcare providers, scholars, researchers, consultants, and government envision CSF for successful implementation of AI in HSC and can thus contribute towards achieving an effective HSC via improved quality, access, safety, and reduced cost.
However, the study has certain limitations. The findings of this study are based on the expert opinion drawn from practitioners in logistics, supply chain, and IT domains and academicians, and the possibility of response biasedness and ambiguity cannot be ruled out. Further, the study is based on a limited number of experts, future studies may involve analysis of critical success factors using statistical tools like structural equation modeling for further validating the results. Future studies can also use causal -effect techniques such as DEMATEL to study the causal effect among various critical success factors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability
The authors do not have permission to share data.
References
- Aboelmaged M.G. Predicting e-readiness at firm-level: An analysis of technological, organizational and environmental (TOE) effects on e-maintenance readiness in manufacturing firms. International Journal of Information Management. 2014;34(5):639–651. [Google Scholar]
- Accenture (2021). Leaders Wanted. Available at: https://www.accenture.com/_acnmedia/PDF-156/Accenture-Digital-Health-Tech-Vision-2021.pdf (accessed on 20 July 2022).
- Ageron B., Bentahar O., Gunasekaran A. Digital supply chain: Challenges and future directions. Supply Chain Forum: An International Journal. 2020;21(3):133–138. [Google Scholar]
- Agrawal, Madaan A structural equation model for big data adoption in the healthcare supply chain. International Journal of Productivity and Performance Management. 2021 doi: 10.1108/IJPPM-12-2020-0667. [DOI] [Google Scholar]
- Agrawal T.K., Sharma A., Kumar V. In: Artificial Intelligence for Fashion Industry in the Big Data Era. Thomassey S., Zeng X., editors. Springer; Singapore: 2018. Blockchain-based secure traceability system for textile and clothing supply chain; pp. 197–208. [Google Scholar]
- Ahmadi H., Nilashi M., Shahmoradi L., Ibrahim O. Hospital Information System adoption: Expert perspectives on an adoption framework for Malaysian public hospitals. Computers in Human Behavior. 2017;67:161–189. [Google Scholar]
- Ahuja R., Sawhney A., Jain M., Arif M., Rakshit S. Factors influencing BIM adoption in emerging markets–the case of India. International Journal of Construction Management. 2020;20(1):65–76. [Google Scholar]
- Ajmera, Jain Modelling the barriers of Health 4.0–the fourth healthcare industrial revolution in India by TISM. Operations Management Research. 2019;12(3):129–145. [Google Scholar]
- AlBar A.M., Hoque M.R. Factors affecting the adoption of information and communication technology in small and medium enterprises: A perspective from rural Saudi Arabia. Information Technology for Development. 2019;25(4):715–738. [Google Scholar]
- Aldrighetti R., Zennaro I., Finco S., Battini D. Healthcare supply chain simulation with disruption considerations: A case study from Northern Italy. Global Journal of Flexible Systems Management. 2019;20(1):81–102. [Google Scholar]
- Alrahbi D., Khan M., Hussain M. Exploring the motivators of technology adoption in healthcare. International Journal of Healthcare Management. 2021;14(1):50–63. [Google Scholar]
- Araz O.M., Choi T.M., Olson D., Salman F.S. Data analytics for operational risk management. Decision Sciences. 2020;51(6):1316–1319. [Google Scholar]
- Arpaci I. A hybrid modeling approach for predicting the educational use of mobile cloud computing services in higher education. Computers in Human Behavior. 2019;90:181–187. [Google Scholar]
- Ashaye O.R., Irani Z. The role of stakeholders in the effective use of e-government resources in public services. International Journal of Information Management. 2019;49:253–270. [Google Scholar]
- Azadegan A., Mellat Parast M., Lucianetti L., Nishant R., Blackhurst J. Supply chain disruptions and business continuity: An empirical assessment. Decision Sciences. 2020;51(1):38–73. [Google Scholar]
- Azzi R., Chamoun R.K., Sokhn M. The power of a blockchain-based supply chain. Computers & industrial engineering. 2019;135:582–592. [Google Scholar]
- Bala H., Feng X. Success of small and medium enterprises in Myanmar: Role of technological, organizational, and environmental factors. Journal of Global Information Technology Management. 2019;22(2):100–119. [Google Scholar]
- Balasubramanian S., Shukla V., Sethi J.S., Islam N., Saloum R. A readiness assessment framework for Blockchain adoption: A healthcare case study. Technological Forecasting and Social Change. 2021;165 [Google Scholar]
- Baryannis G., Validi S., Dani S., Antoniou G. Supply chain risk management and artificial intelligence: State of the art and future research directions. International Journal of Production Research. 2019;57(7):2179–2202. [Google Scholar]
- Beaulieu M., Bentahar O. Digitalization of the healthcare supply chain: A roadmap to generate benefits and effectively support healthcare delivery. Technological forecasting and social change. 2021;167 [Google Scholar]
- Becker W., Schmid O. The right digital strategy for your business: An empirical analysis of the design and implementation of digital strategies in SMEs and LSEs. Business Research. 2020;13:985–1005. [Google Scholar]
- Bogart, S., & Rice, K. (2015). The blockchain report: welcome to the internet of value. Needham Insights.https://needham.bluematrix.com/sellside/EmailDocViewer?encrypt=4aaafaf1-d76e-4ee3-94067d0ad3c0d019&mime=pdf&co=needham&id=sbogart@needhamco.com&source=mail&utm_content=buffer0b432&utm_medium=social&utm_source=twitter.com&utm_campaign=buffer. Accessed 25 March 2020.
- Brock V., Khan H.U. Big data analytics: Does organizational factor matters impact technology acceptance? Journal of Big Data. 2017;4(1):1–28. [Google Scholar]
- Büyüközkan G., Göçer F. A novel approach integrating AHP and COPRAS under Pythagorean fuzzy sets for digital supply chain partner selection. IEEE Transactions on Engineering Management. 2019 doi: 10.1109/TEM.2019.2907673. [DOI] [Google Scholar]
- Cao D., Tao H., Wang Y., Tarhini A., Xia S. Acceptance of automation manufacturing technology in China: an examination of perceived norm and organizational efficacy. Production Planning & Control. 2020;31(8):660–672. [Google Scholar]
- Catalini C., Gans J.S. Some simple economics of the blockchain National Bureau of Economic. Research. 2016;No. w22952 https://www.nber.org/papers/w22952.pdf Accessed March 27 2020. [Google Scholar]
- Chang Y.W. What drives organizations to switch to cloud ERP systems? The impacts of enablers and inhibitors. Journal of Enterprise Information Management. 2020;33(3):600–626. [Google Scholar]
- Chauhan A., Jakhar S.K., Jabbour C.J.C. Implications for sustainable healthcare operations in embracing telemedicine services during a pandemic. Technological Forecasting and Social Change. 2022;176 doi: 10.1016/j.techfore.2021.121462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Kang H., Luna-Reyes L.F. Key determinants of online fiscal transparency: A technology-organization-environment framework. Public Performance & Management Review. 2019;42(3):606–631. [Google Scholar]
- Chiu C.N., Yang C.L. Competitive advantage and simultaneous mutual influences between information technology adoption and service innovation: Moderating effects of environmental factors. Structural Change and Economic Dynamics. 2019;49:192–205. [Google Scholar]
- Chopdar P.K., Korfiatis N., Sivakumar V.J., Lytras M.D. Mobile shopping apps adoption and perceived risks: A cross-country perspective utilizing the Unified Theory of Acceptance and Use of Technology. Computers in Human Behavior. 2018;86:109–128. [Google Scholar]
- Chu Z., Xu J., Lai F., Collins B.J. Institutional theory and environmental pressures: The moderating effect of market uncertainty on innovation and firm performance. IEEE Transactions on Engineering Management. 2018;65(3):392–403. [Google Scholar]
- Clauson K.A., Breeden E.A., Davidson C., Mackey T.K. Leveraging blockchain technology to enhance supply chain management in healthcare: An exploration of challenges and opportunities in the health supply chain. Blockchain in healthcare today. 2018;1(3):1–12. [Google Scholar]
- Clohessy T., Acton T. Investigating the influence of organizational factors on blockchain adoption: An innovation theory perspective. Industrial Management and Data Systems. 2019;119(7):1457–1491. [Google Scholar]
- Cocco L., Pinna A., Marchesi M. Banking on blockchain: Costs savings thanks to the blockchain technology. Future internet. 2017;9(3):25. [Google Scholar]
- Cocosila M., Turel O. Adoption and non-adoption motivational risk beliefs in the use of mobile services for health promotion. Internet Research. 2019;29(4):846–869. [Google Scholar]
- Cognizant (2017). Blockchain: A Potential Game-Changer for Life Insurance. https://www.cognizant.com/whitepapers/blockchain-a-potential-game-changer-for-life-insurance-codex2484.pdf. Accessed 3 April 2020.
- Cook N. Congressional Research Service; Washington, DC: 2019. Ghana: current issues and US relations in brief. [Google Scholar]
- Cruz-Jesus F., Pinheiro A., Oliveira T. Understanding CRM adoption stages: Empirical analysis building on the TOE framework. Computers in Industry. 2019;109:1–13. [Google Scholar]
- Darko A., Chan A.P.C., Yang Y., Shan M., He B.J., Gou Z. Influences of barriers, drivers, and promotion strategies on green building technologies adoption in developing countries: The Ghanaian case. Journal of Cleaner Production. 2018;200:687–703. [Google Scholar]
- Damoah I.S., Ayakwah A., Tingbani I. Artificial intelligence (AI)-enhanced medical drones in the healthcare supply chain (HSC) for sustainability development: A case study. Journal of Cleaner Production. 2021;328 [Google Scholar]
- Degnarain N. “Five Ways Block chain Can Unblock The Coronavirus Medical Supply Chain”, Forbes. 2020. https://www.forbes.com/sites/nishandegnarain/2020/03/22/5-ways-blockchain-can-unblock-the-coronavirus-medical-supply-chain/#1fd97c491380 Accessed 7 April 2020.
- Desingh V. Internet of Things adoption barriers in the Indian healthcare supply chain: An ISM-fuzzy MICMAC approach. The International journal of health planning and management. 2022;37(1):318–351. doi: 10.1002/hpm.3331. [DOI] [PubMed] [Google Scholar]
- Dimitrov D.V. Blockchain applications for healthcare data management. Healthcare Informatics Research. 2019;25(1):51–56. doi: 10.4258/hir.2019.25.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobrovnik M., Herold D.M., Fürst E., Kummer S. Blockchain for and in Logistics: What to Adopt and Where to Start. Logistics. 2018;2(3):18. [Google Scholar]
- Dwivedi Y.K., Hughes L., Ismagilova E., Aarts G., Coombs C., Crick T., et al. Artificial Intelligence (AI): Multidisciplinary perspectives on emerging challenges, opportunities, and agenda for research, practice and policy. International Journal of Information Management. 2019;57 [Google Scholar]
- Dwivedi Y.K., Rana N.P., Jeyaraj A., Clement M., Williams M.D. Re-examining the unified theory of acceptance and use of technology (UTAUT): Towards a revised theoretical model. Information Systems Frontiers. 2019;21(3):719–734. [Google Scholar]
- Egger J., Masood T. Augmented reality in support of intelligent manufacturing–a systematic literature review. Computers & Industrial Engineering. 2020;140 [Google Scholar]
- El-Kassar A.N., Singh S.K. Green innovation and organizational performance: The influence of big data and the moderating role of management commitment and HR practices. Technological Forecasting and Social Change. 2019;144:483–498. [Google Scholar]
- Ferreira L., Borenstein D. A fuzzy-Bayesian model for supplier selection. Expert Systems with Applications. 2012;39(9):7834–7844. [Google Scholar]
- Fortune (2020). 94% of the Fortune 1000 are seeing coronavirus supply chain disruptions: Report. https://fortune.com/2020/02/21/fortune-1000-coronavirus-china-supply-chain-impact/. Accessed 10 March 2020.
- Florez J.V., Lauras M., Okongwu U., Dupont L. A decision support system for robust humanitarian facility location. Engineering Applications of Artificial Intelligence. 2015;46:326–335. [Google Scholar]
- Fryer L.K., Thompson A., Nakao K., Howarth M., Gallacher A. Supporting self-efficacy beliefs and interest as educational inputs and outcomes: Framing AI and Human partnered task experiences. Learning and Individual Differences. 2020;80 [Google Scholar]
- Gao F., Sunyaev A. Context matters: A review of the determinant factors in the decision to adopt cloud computing in healthcare. International Journal of Information Management. 2019;48:120–138. [Google Scholar]
- Gao F., Zhu L., Shen M., Sharif K., Wan Z., Ren K. A blockchain-based privacy-preserving payment mechanism for vehicle-to-grid networks. IEEE network. 2018;32(6):184–192. [Google Scholar]
- Gardas B.B. Organizational hindrances to Healthcare 4.0 adoption: An multi-criteria decision analysis framework. Journal of Multi-Criteria Decision Analysis. 2022;29(1–2):186–195. [Google Scholar]
- Gartner (2022). Managing Healthcare Supply Chains. Available at: https://www.gartner.com/en/supply-chain/insights/healthcare-supply-chain-management.
- Ghadge A., Kara M.E., Moradlou H., Goswami M. The impact of Industry 4.0 implementation on supply chains. Journal of Manufacturing Technology Management. 2020;31(4):669–686. [Google Scholar]
- Governatori G., Idelberger F., Milosevic Z., Riveret R., Sartor G., Xu X. On legal contracts, imperative and declarative smart contracts, and blockchain systems. Artificial Intelligence and Law. 2018;26(4):377–409. [Google Scholar]
- Govindan K., Mina H., Alavi B. A decision support system for demand management in healthcare supply chains considering the epidemic outbreaks: A case study of coronavirus disease 2019 (COVID-19) Transportation Research Part E: Logistics and Transportation Review. 2020;138 doi: 10.1016/j.tre.2020.101967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan J. Artificial intelligence in healthcare and medicine: Promises, ethical challenges and governance. Chinese Medical Sciences Journal. 2019;34(2):76–83. doi: 10.24920/003611. [DOI] [PubMed] [Google Scholar]
- Gupta H., Kumar A., Wasan P. Industry 4.0, cleaner production and circular economy: An integrative framework for evaluating ethical and sustainable business performance of manufacturing organizations. Journal of Cleaner Production. 2021;295 [Google Scholar]
- Gutierrez A., Boukrami E., Lumsden R. Technological, organisational and environmental factors influencing managers’ decision to adopt cloud computing in the UK. Journal of Enterprise Information Management. 2015;28(6):788–807. [Google Scholar]
- Habli I., Lawton T., Porter Z. Artificial intelligence in health care: Accountability and safety. Bulletin of the World Health Organization. 2020;98(4):251. doi: 10.2471/BLT.19.237487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashemkhani Zolfani S., Yazdani M., Zavadskas E.K. An extended stepwise weight assessment ratio analysis (SWARA) method for improving criteria prioritization process. Soft Computing. 2018;22(22):7399–7405. [Google Scholar]
- Holzmann P., Schwarz E.J., Audretsch D.B. Understanding the determinants of novel technology adoption among teachers: The case of 3D printing. The Journal of Technology Transfer. 2020;45(1):259–275. [Google Scholar]
- Horváth D., Szabó R.Z. Driving forces and barriers of Industry 4.0: Do multinational and small and medium-sized companies have equal opportunities? Technological Forecasting and Social Change. 2019;146:119–132. [Google Scholar]
- Hoy M.B. An introduction to the blockchain and its implications for libraries and medicine. Medical reference services quarterly. 2017;36(3):273–279. doi: 10.1080/02763869.2017.1332261. [DOI] [PubMed] [Google Scholar]
- Hussain M., Ajmal M.M., Gunasekaran A., Khan M. Exploration of social sustainability in healthcare supply chain. Journal of Cleaner Production. 2018;203:977–989. [Google Scholar]
- IBM (2018). Blockchain for supply chain. https ://www.ibm.com/block chain /suppl y-chain /. Accessed 14 April 2020.
- Ivanov D., Dolgui A. A digital supply chain twin for managing the disruption risks and resilience in the era of Industry 4.0. Production Planning & Control. 2021;32(9):775–788. [Google Scholar]
- Jain V., Singh N., Pradhan S., Gupta P. Factors Influencing AI Implementation Decision in Indian Healthcare Industry: A Qualitative Inquiry. Springer; Cham: 2020. pp. 635–640. [Google Scholar]
- Janssen M., Weerakkody V., Ismagilova E., Sivarajah U., Irani Z. A framework for analysing blockchain technology adoption: Integrating institutional, market and technical factors. International Journal of Information Management. 2020;50:302–309. [Google Scholar]
- Jayaraman R., Saleh K., King N. Improving Opportunities in healthcare supply chain processes via the Internet of Things and Blockchain Technology. International Journal of Healthcare Information Systems and Informatics. 2019;14(2):49–65. [Google Scholar]
- Kamble S.S., Gunasekaran A., Parekh H., Joshi S. Modeling the internet of things adoption barriers in food retail supply chains. Journal of Retailing and Consumer Services. 2019;48:154–168. [Google Scholar]
- Kara M.E., Fırat S.Ü.O., Ghadge A. A data mining-based framework for supply chain risk management. Computers and Industrial Engineering. 2020;139 [Google Scholar]
- Karabasevic D., Zavadskas E.K., Turskis Z., Stanujkic D. The framework for the selection of personnel based on the SWARA and ARAS methods under uncertainties. Informatica. 2016;27(1):49–65. [Google Scholar]
- Kazancoglu I., Ozbiltekin-Pala M., Mangla S.K., Kumar A., Kazancoglu Y. Using emerging technologies to improve the sustainability and resilience of supply chains in a fuzzy environment in the context of COVID-19. Annals of Operations Research. 2022:1–24. doi: 10.1007/s10479-022-04775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S.A., Kusi-Sarpong S., Gupta H., Arhin F.K., Lawal J.N., Hassan S.M. Critical factors of digital supply chains for organizational performance improvement. IEEE Transactions on Engineering Management. 2021 doi: 10.1109/TEM.2021.3052239. [DOI] [Google Scholar]
- Khanijahani A., Iezadi S., Dudley S., Goettler M., Kroetsch P., Wise J. Organizational, professional, and patient characteristics associated with artificial intelligence adoption in healthcare: A systematic review. Health Policy and Technology. 2022;100602 doi: 10.1016/j.hlpt.2022.100602. [DOI] [Google Scholar]
- Khodadadi M.R., Hashemkhani Zolfani S., Yazdani M., Zavadskas E.K. A hybrid MADM analysis in evaluating process of chemical wastewater purification regarding to advance oxidation processes. Journal of Environmental Engineering and Landscape Management. 2017;25(3):277–288. [Google Scholar]
- Kiel D., Arnold C., Voigt K.I. The influence of the Industrial Internet of Things on business models of established manufacturing companies–A business level perspective. Technovation. 2017;68:4–19. [Google Scholar]
- Ko, et al. (2011). TrustCloud: A framework for accountability and trust in cloud computing. In 2011 IEEE World Congress on Services (pp. 584-588). IEEE.
- Kshetri N. Blockchain’s roles in meeting key supply chain management objectives. International Journal of Information Management. 2018;39:80–89. [Google Scholar]
- Kumar A., Dixit G. A novel hybrid MCDM framework for WEEE recycling partner evaluation on the basis of green competencies. Journal of Cleaner Production. 2019;241 [Google Scholar]
- Kumar S., Raut R.D., Narkhede B.E. A proposed collaborative framework by using artificial intelligence-internet of things (AI-IoT) in COVID-19 pandemic situation for healthcare workers. International Journal of Healthcare Management. 2020;13(4):337–345. [Google Scholar]
- Kusi-Sarpong S., Gupta H., Sarkis J. A supply chain sustainability innovation framework and evaluation methodology. International Journal of Production Research. 2019;57(7):1990–2008. [Google Scholar]
- Kwon J., Johnson M.E. Proactive versus reactive security investments in the healthcare sector. Mis Quarterly. 2014;38(2):451–A3. [Google Scholar]
- Kwon I.W.G., Kim S.H., Martin D.G. Healthcare supply chain management; strategic areas for quality and financial improvement. Technological Forecasting and Social Change. 2016;113:422–428. [Google Scholar]
- Laroiya C., Saxena D., Komalavalli C. Handbook of Research on Blockchain Technology. Academic Press; 2020. Applications of Blockchain Technology; pp. 213–243. [Google Scholar]
- Lawrence J.M., Hossain N.U.I., Jaradat R., Hamilton M. Leveraging a Bayesian network approach to model and analyze supplier vulnerability to severe weather risk: A case study of the US pharmaceutical supply chain following Hurricane Maria. International Journal of Disaster Risk Reduction. 2020;49 doi: 10.1016/j.ijdrr.2020.101607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Jiang P., Chen T., Luo X., Wen Q. A survey on the security of blockchain systems. Future Generation Computer Systems. 2020;107:841–853. [Google Scholar]
- Lu L., Cai R., Gursoy D. Developing and validating a service robot integration willingness scale. International Journal of Hospitality Management. 2019;80:36–51. [Google Scholar]
- Luthra S., Kumar A., Zavadskas E.K., Mangla S.K., Garza-Reyes J.A. Industry 4.0 as an enabler of sustainability diffusion in supply chain: An analysis of influential strength of drivers in an emerging economy. International Journal of Production Research. 2020;58(5):1505–1521. [Google Scholar]
- Magistretti S., Dell'Era C., Verganti R. Searching for the right application: A technology development review and research agenda. Technological Forecasting and Social Change. 2020;151 [Google Scholar]
- Mahardika H., Thomas D., Ewing M.T., Japutra A. Predicting consumers’ trial/adoption of new technology: Revisiting the behavioral expectations–behavioral intentions debate. The International Review of Retail, Distribution and Consumer Research. 2019;29(1):99–117. [Google Scholar]
- Mardani A., Nilashi M., Zakuan N., Loganathan N., Soheilirad S., Saman M.Z.M., et al. A systematic review and meta-Analysis of SWARA and WASPAS methods: Theory and applications with recent fuzzy developments. Applied Soft Computing. 2017;57:265–292. [Google Scholar]
- Marques L., Martins M., Araújo C. The healthcare supply network: Current state of the literature and research opportunities. Production planning & control. 2020;31(7):590–609. [Google Scholar]
- Martínez-Pérez F.E., Nunez-Varela J.I., Castillo-Barrera F.E., Nava-Muñoz S.E., Pérez-González H.G. Artificial intelligence techniques applied to patient care and monitoring. Academic Press; 2020. pp. 439–464. [Google Scholar]
- Mathauer M., Hofmann E. Technology adoption by logistics service providers. International Journal of Physical Distribution & Logistics Management. 2019;49(4):416–434. [Google Scholar]
- McGhin T., Choo K.K.R., Liu C.Z., He D. Blockchain in healthcare applications: Research challenges and opportunities. Journal of Network and Computer Applications. 2019;135:62–75. [Google Scholar]
- Mengelkamp E., Notheisen B., Beer C., Dauer D., Weinhardt C. A blockchain-based smart grid: Towards sustainable local energy markets. Computer Science-Research and Development. 2018;33(1–2):207–214. [Google Scholar]
- Mero J., Tarkiainen A., Tobon J. Effectual and causal reasoning in the adoption of marketing automation. Industrial Marketing Management. 2020;86:212–222. [Google Scholar]
- Mikalef P., Krogstie J., Pappas I.O., Pavlou P. Exploring the relationship between big data analytics capability and competitive performance: The mediating roles of dynamic and operational capabilities. Information & Management. 2020;57(2) [Google Scholar]
- Min H. Blockchain technology for enhancing supply chain resilience. Business Horizons. 2019;62(1):35–45. [Google Scholar]
- Mir S.A., Padma T. Integrated Technology Acceptance Model for the Evaluation of Agricultural Decision Support Systems. Journal of Global Information Technology Management. 2020;23(2):138–164. [Google Scholar]
- Mitra T., Kapoor R., Gupta N. Studying key antecedents of disruptive technology adoption in the digital supply chain: An Indian perspective. International Journal of Emerging Markets. 2022 [Google Scholar]
- Munir M., Jajja M.S.S., Chatha K.A., Farooq S. Supply chain risk management and operational performance: The enabling role of supply chain integration. International Journal of Production Economics. 2020;227 [Google Scholar]
- Nam T. Technology usage, expected job sustainability, and perceived job insecurity. Technological Forecasting and Social Change. 2019;138:155–165. [Google Scholar]
- Naszay M., Stockinger A., Jungwirth D., Haluza D. Digital age and the public ehealth perspective: Prevailing health app use among Austrian Internet users. Informatics for Health and Social Care. 2018;43(4):390–400. doi: 10.1080/17538157.2017.1399131. [DOI] [PubMed] [Google Scholar]
- Nguyen A., Lamouri S., Pellerin R., Tamayo S., Lekens B. Data analytics in pharmaceutical supply chains: State of the art, opportunities, and challenges. International Journal of Production Research. 2021;1–20 [Google Scholar]
- Nguyen T.H., Newby M., Macaulay M.J. Information technology adoption in small business: Confirmation of a proposed framework. Journal of Small Business Management. 2015;53(1):207–227. [Google Scholar]
- Nilashi M., Ahmadi H., Ahani A., Ravangard R., bin Ibrahim O. Determining the importance of hospital information system adoption factors using fuzzy analytic network process (ANP) Technological Forecasting and Social Change. 2016;111:244–264. [Google Scholar]
- Nysveen H., Pedersen P.E., Skard S. Ecosystem adoption of practices over time (EAPT): Toward an alternative view of contemporary technology adoption. Journal of Business Research. 2020;116:542–551. [Google Scholar]
- Onik M.M.H., Aich S., Yang J., Kim C.S., Kim H.C. Big Data Analytics for Intelligent Healthcare Management. Academic Press; 2019. Blockchain in healthcare: Challenges and solutions; pp. 197–226. [Google Scholar]
- Orji I.J., Kusi-Sarpong S., Huang S., Vazquez-Brust D. Evaluating the factors that influence blockchain adoption in the freight logistics industry. Transportation Research Part E: Logistics and Transportation Review. 2020;141 [Google Scholar]
- Pacchini A.P.T., Lucato W.C., Facchini F., Mummolo G. The degree of readiness for the implementation of Industry 4.0. Computers in Industry. 2019;113 [Google Scholar]
- Pan X., Pan X., Song M., Ai B., Ming Y. Blockchain technology and enterprise operational capabilities: An empirical test. International Journal of Information Management. 2020;52 [Google Scholar]
- Phares J., Dobrzykowski D.D., Prohofsky J. How policy is shaping the macro healthcare delivery supply chain: The emergence of a new tier of retail medical clinics. Business Horizons. 2021;64(3):333–345. [Google Scholar]
- Polater A., Demirdogen O. An investigation of healthcare supply chain management and patient responsiveness. International Journal of Pharmaceutical and Healthcare Marketing. 2018;12(3):325–347. [Google Scholar]
- Rajagopal V., Venkatesan S.P., Goh M. Decision-making models for supply chain risk mitigation: A review. Computers & Industrial Engineering. 2017;113:646–682. [Google Scholar]
- Rajput S., Singh S.P. Identifying Industry 4.0 IoT enablers by integrated PCA-ISM-DEMATEL approach. Management Decision. 2019;57(8):1784–1817. [Google Scholar]
- Randall D., Goel P., Abujamra R. Blockchain applications and use cases in health information technology. Journal of Health and Medical Informatics. 2017;8(3):8–11. [Google Scholar]
- Rao A. Ravishankar, Clarke Daniel. Perspectives on emerging directions in using IoT devices in blockchain applications. Internet of Things. 2020;10 [Google Scholar]
- Reddy K.R.K., Gunasekaran A., Kalpana P., Sreedharan V.R., Kumar S.A. Developing a Blockchain Framework for the Automotive Supply Chain: A systematic Review. Computers & Industrial Engineering. 2021;107334 [Google Scholar]
- Riahi Y., Saikouk T., Gunasekaran A., Badraoui I. Artificial intelligence applications in supply chain: A descriptive bibliometric analysis and future research directions. Expert Systems with Applications. 2021;173 [Google Scholar]
- Roberts A.R., De Schutter B., Franks K., Radina M.E. Older adults’ experiences with audiovisual virtual reality: Perceived usefulness and other factors influencing technology acceptance. Clinical gerontologist. 2019;42(1):27–33. doi: 10.1080/07317115.2018.1442380. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Espíndola O., Chowdhury S., Beltagui A., Albores P. The potential of emergent disruptive technologies for humanitarian supply chains: The integration of blockchain, Artificial Intelligence and 3D printing. International Journal of Production Research. 2020;58(15):4610–4630. [Google Scholar]
- Roy S., Das A.K., Chatterjee S., Kumar N., Chattopadhyay S., Rodrigues J.J. Provably secure fine-grained data access control over multiple cloud servers in mobile cloud computing based healthcare applications. IEEE Transactions on Industrial Informatics. 2018;15(1):457–468. [Google Scholar]
- Saberi S., Kouhizadeh M., Sarkis J. Blockchains and the supply chain: Findings from a broad study of practitioners. IEEE Engineering Management Review. 2019 a;47(3):95–103. [Google Scholar]
- Saberi S., Kouhizadeh M., Sarkis J., Shen L. Blockchain technology and its relationships to sustainable supply chain management. International Journal of Production Research. 2019;57(7):2117–2135. [Google Scholar]
- Sadoughi F., Khodaveisi T., Ahmadi H. The used theories for the adoption of electronic health record: A systematic literature review. Health and Technology. 2019;9(4):383–400. [Google Scholar]
- Saha E., Rathore P., Parida R., Rana N.P. The interplay of emerging technologies in pharmaceutical supply chain performance: An empirical investigation for the rise of Pharma 4.0. Technological Forecasting and Social Change. 2022;181 [Google Scholar]
- Santoro G., Vrontis D., Thrassou A., Dezi L. The Internet of Things: Building a knowledge management system for open innovation and knowledge management capacity. Technological Forecasting and Social Change. 2018;136:347–354. [Google Scholar]
- Scavarda A., Daú G.L., Scavarda L.F., Korzenowski A.L. A proposed healthcare supply chain management framework in the emerging economies with the sustainable lenses: The theory, the practice, and the policy. Resources, Conservation and Recycling. 2019;141:418–430. [Google Scholar]
- Schuetz S., Venkatesh V. Blockchain, adoption, and financial inclusion in India: Research opportunities. International Journal of Information Management. 2020;52 [Google Scholar]
- Senna P., Reis A., Dias A., Coelho O., Guimaraes J., Eliana S. Healthcare supply chain resilience framework: Antecedents, mediators, consequents. Production Planning & Control. 2021:1–15. [Google Scholar]
- Shao Z. Interaction effect of strategic leadership behaviors and organizational culture on IS-Business strategic alignment and Enterprise Systems assimilation. International Journal of Information Management. 2019;44:96–108. [Google Scholar]
- Sharma S.K. Integrating cognitive antecedents into TAM to explain mobile banking behavioral intention: A SEM-neural network modeling. Information Systems Frontiers. 2019;21(4):815–827. [Google Scholar]
- Singh S.K., Del Giudice M., Tarba S.Y., De Bernardi P. Top management team shared leadership, market-oriented culture, innovation capability, and firm performance. IEEE Transactions on Engineering Management. 2019 doi: 10.1109/TEM.2019.2946608. [DOI] [Google Scholar]
- Sinha A.K., Zhang W.J., Tiwari M.K. Co-evolutionary immuno-particle swarm optimization with penetrated hyper-mutation for distributed inventory replenishment. Engineering Applications of Artificial Intelligence. 2012;25(8):1628–1643. [Google Scholar]
- Sivathanu B., Pillai R. Smart HR 4.0–how industry 4.0 is disrupting HR. Human Resource Management International Digest. 2018;26(4):7–11. [Google Scholar]
- Soltanisehat L., Alizadeh R., Hao H., Choo K.K.R. Technical, Temporal, and Spatial Research Challenges and Opportunities in Blockchain-Based Healthcare: A Systematic Literature Review. IEEE Transactions on Engineering Management. 2020 doi: 10.1109/TEM.2020.3013507. [DOI] [Google Scholar]
- Srivastava S., Garg D., Agarwal A. A step towards responsive healthcare supply chain management: An overview. Advances in Manufacturing and Industrial Engineering. 2021:431–443. [Google Scholar]
- Stević Ž., Pamučar D., Puška A., Chatterjee P. Sustainable supplier selection in healthcare industries using a new MCDM method: Measurement of alternatives and ranking according to COmpromise solution (MARCOS) Computers & Industrial Engineering. 2020;140 doi: 10.1016/j.cie.2019.106231. [DOI] [Google Scholar]
- Sun S., Hall D.J., Cegielski C.G. Organizational intention to adopt big data in the B2B context: An integrated view. Industrial Marketing Management. 2020;86:109–121. [Google Scholar]
- Szalavetz A. Industry 4.0 and capability development in manufacturing subsidiaries. Technological Forecasting and Social Change. 2019;145:384–395. [Google Scholar]
- Tallon P.P., Queiroz M., Coltman T., Sharma R. Information technology and the search for organizational agility: A systematic review with future research possibilities. The Journal of Strategic Information Systems. 2019;28(2):218–237. [Google Scholar]
- Tarei P.K., Kumar G., Ramkumar M. A Mean-Variance robust model to minimize operational risk and supply chain cost under aleatory uncertainty: A real-life case application in petroleum supply chain. Computers & Industrial Engineering. 2022;166 [Google Scholar]
- Tian, F. (2016, June). An agri-food supply chain traceability system for China based on RFID & blockchain technology. In 2016 13th international conference on service systems and service management (ICSSSM) (pp. 1-6). IEEE.
- Toorajipour R., Sohrabpour V., Nazarpour A., Oghazi P., Fischl M. Artificial intelligence in supply chain management: A systematic literature review. Journal of Business Research. 2021;122:502–517. [Google Scholar]
- Tornatzky L., Fleischer M. Lexington Books; Lexington, MA: 1990. The process of technology innovation; p. 165. [Google Scholar]
- Tortorella G.L., Vergara A.M.C., Garza-Reyes J.A., Sawhney R. Organizational learning paths based upon industry 4.0 adoption: An empirical study with Brazilian manufacturers. International Journal of Production Economics. 2020;219:284–294. [Google Scholar]
- Toyoda K., Mathiopoulos P.T., Sasase I., Ohtsuki T. A novel blockchain-based product ownership management system (POMS) for anti-counterfeits in the post supply chain. IEEE Access. 2017;5:17465–17477. [Google Scholar]
- Tsai J.M., Cheng M.J., Tsai H.H., Hung S.W., Chen Y.L. Acceptance and resistance of telehealth: The perspective of dual-factor concepts in technology adoption. International Journal of Information Management. 2019;49:34–44. [Google Scholar]
- Tsang Y.P., Choy K.L., Wu C.H., Ho G.T., Lam C.H., Koo P.S. An Internet of Things (IoT)-based risk monitoring system for managing cold supply chain risks. Industrial Management & Data Systems. 2018;118(7):1432–1462. [Google Scholar]
- Tseng J.H., Liao Y.C., Chong B., Liao S.W. Governance on the drug supply chain via gcoin blockchain. International journal of environmental research and public health. 2018;15(6):1055. doi: 10.3390/ijerph15061055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumasjan A., Beutel T. Business transformation through blockchain. Palgrave Macmillan; Cham: 2019. Blockchain-based decentralized business models in the sharing economy: A technology adoption perspective; pp. 77–120. [Google Scholar]
- Viswanadham N. Performance analysis and design of competitive business models. International Journal of Production Research. 2018;56(1–2):983–999. [Google Scholar]
- Wamba S.F., Queiroz M.M. Blockchain in the operations and supply chain management: Benefits, challenges and future research opportunities. International Journal of Information Management. 2020;49 [Google Scholar]
- Wang Y., Kung L., Byrd T.A. Big data analytics: Understanding its capabilities and potential benefits for healthcare organizations. Technological forecasting and social change. 2018;126:3–13. [Google Scholar]
- Wang Y., Singgih M., Wang J., Rit M. Making sense of blockchain technology: How will it transform supply chains? International Journal of Production Economics. 2019;211:221–236. [Google Scholar]
- Webster C., Ivanov S. Digital Transformation in Business and Society. Palgrave Macmillan; Cham: 2020. Robotics, artificial intelligence, and the evolving nature of work; pp. 127–143. [Google Scholar]
- Wong L.W., Leong L.Y., Hew J.J., Tan G.W.H., Ooi K.B. Time to seize the digital evolution: Adoption of blockchain in operations and supply chain management among Malaysian SMEs. International Journal of Information Management. 2020;52 [Google Scholar]
- World Economic Forum (2017). The Global Risks Report 2017. World Economic Forum (weforum.org).
- Wu H., Li Z., King B., Ben Miled Z., Wassick J., Tazelaar J. A distributed ledger for supply chain physical distribution visibility. Information. 2017;8(4):137. [Google Scholar]
- Wu L., Yue X., Jin A., Yen D.C. Smart supply chain management: A review and implications for future research. The International Journal of Logistics Management. 2016;27(2):395–417. [Google Scholar]
- Xia D., Zhang M., Yu Q., Tu Y. Developing a framework to identify barriers of Green technology adoption for enterprises. Resources, Conservation and Recycling. 2019;143:99–110. [Google Scholar]
- Xu S., Zhang X., Feng L., Yang W. Disruption risks in supply chain management: A literature review based on bibliometric analysis. International Journal of Production Research. 2020;58(11):3508–3526. [Google Scholar]
- Yadav V.S., Singh A.R., Raut R.D., Govindarajan U.H. Blockchain technology adoption barriers in the Indian agricultural supply chain: An integrated approach. Resources, Conservation and Recycling. 2020;161 [Google Scholar]
- Yadegaridehkordi E., Nilashi M., Nasir M.H.N.B.M., Ibrahim O. Predicting determinants of hotel success and development using Structural Equation Modelling (SEM)-ANFIS method. Tourism Management. 2018;66:364–386. [Google Scholar]
- Yang Z., Sun J., Zhang Y., Wang Y. Understanding SaaS adoption from the perspective of organizational users: A tripod readiness model. Computers in Human Behavior. 2015;45:254–264. [Google Scholar]
- Yazdani M., Chatterjee P., Zavadskas E.K., Streimikiene D. A novel integrated decision-making approach for the evaluation and selection of renewable energy technologies. Clean Technologies and Environmental Policy. 2018;20(2):403–420. [Google Scholar]
- Yousefi S., Tosarkani B.M. An analytical approach for evaluating the impact of blockchain technology on sustainable supply chain performance. International Journal of Production Economics. 2022;246 [Google Scholar]
- Yusof M.M., Kuljis J., Papazafeiropoulou A., Stergioulas L.K. An evaluation framework for Health Information Systems: Human, organization and technology-fit factors (HOT-fit) International journal of medical informatics. 2008;77(6):386–398. doi: 10.1016/j.ijmedinf.2007.08.011. [DOI] [PubMed] [Google Scholar]
- Zaki M. Digital transformation: Harnessing digital technologies for the next generation of services. Journal of Services Marketing. 2019;33(4):429–435. [Google Scholar]
- Zamiela C., Hossain N.U.I., Jaradat R. Enablers of resilience in the healthcare supply chain: A case study of US healthcare industry during COVID-19 pandemic. Research in Transportation Economics. 2022;93 [Google Scholar]
- Zarbakhshnia N., Soleimani H., Ghaderi H. Sustainable third-party reverse logistics provider evaluation and selection using fuzzy SWARA and developed fuzzy COPRAS in the presence of risk criteria. Applied Soft Computing. 2018;65:307–319. [Google Scholar]
- Zeng Z., Chen P.J., Lew A.A. From high-touch to high-tech: COVID-19 drives robotics adoption. Tourism Geographies. 2020;22(3):724–734. [Google Scholar]
- Zhang K., Leng S., He Y., Maharjan S., Zhang Y. Mobile edge computing and networking for green and low-latency Internet of Things. IEEE Communications Magazine. 2018;56(5):39–45. [Google Scholar]
- Zhang C., Wu J., Zhou Y., Cheng M., Long C. Peer-to-Peer energy trading in a Microgrid. Applied Energy. 2018;220:1–12. [Google Scholar]
- Zhang M., Pawar K.S., Bhardwaj S. Improving supply chain social responsibility through supplier development. Production Planning & Control. 2017;28(6–8):500–511. [Google Scholar]
- Zavadskas E.K., Stević Ž., Tanackov I., Prentkovskis O. A novel multicriteria approach–rough step-wise weight assessment ratio analysis method (R-SWARA) and its application in logistics. Studies in Informatics and Control. 2018;27(1):97–106. [Google Scholar]
- Zhou J., Li P., Zhou Y., Wang B., Zang J., Meng L. Toward new-generation intelligent manufacturing. Engineering. 2018;4(1):11–20. [Google Scholar]
Further reading
- Belhadi A., Mani V., Kamble S.S., Khan S.A.R., Verma S. Artificial intelligence-driven innovation for enhancing supply chain resilience and performance under the effect of supply chain dynamism: An empirical investigation. Annals of Operations Research. 2021:1–26. doi: 10.1007/s10479-021-03956-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Z., Lumineau F. Revisiting the interplay between contractual and relational governance: A qualitative and meta-analytic investigation. Journal of Operations Management. 2015;33:15–42. [Google Scholar]
- Fathollahi-Fard A.M., Govindan K., Hajiaghaei-Keshteli M., Ahmadi A. A green home health care supply chain: New modified simulated annealing algorithms. Journal of Cleaner Production. 2019;240 [Google Scholar]
- Grand Review (2020). The potential of AI in Healthcare supply chain. https://www.supplychainbrain.com/blogs/1-think-tank/post/30899-realizing-the-potential-of-ai-in-the-healthcare-supply-chain.
- Hajipour V., Niaki S.T.A., Akhgar M., Ansari M. The healthcare supply chain network design with traceability: A novel algorithm. Computers & Industrial Engineering. 2021;161 [Google Scholar]
- Hossain M.I., Yusof A.F., Sadiq A.S. Factors influencing adoption model of continuous glucose monitoring devices for internet of things healthcare. Internet of Things. 2021;15 [Google Scholar]
- Jayaraman P.P., Forkan A.R.M., Morshed A., Haghighi P.D., Kang Y.B. Healthcare 4.0: A review of frontiers in digital health. Wiley Interdisciplinary Reviews. Data Mining and Knowledge Discovery. 2020;10(2):e1350. [Google Scholar]
- Kamble S., Gunasekaran A., Arha H. Understanding the Blockchain technology adoption in supply chains-Indian context. International Journal of Production Research. 2019;57(7):2009–2033. [Google Scholar]
- Keršuliene V., Zavadskas E.K., Turskis Z. Selection of rational dispute resolution method by applying new step-wise weight assessment ratio analysis (SWARA) Journal of business economics and management. 2010;11(2):243–258. [Google Scholar]
- Singh R.K., Luthra S., Mangla S.K., Uniyal S. Applications of information and communication technology for sustainable growth of SMEs in India food industry. Resources, Conservation and Recycling. 2019;147:10–18. [Google Scholar]
- Supeekit T., Somboonwiwat T., Kritchanchai D. DEMATEL-modified ANP to evaluate internal hospital supply chain performance. Computers & Industrial Engineering. 2016;102:318–330. [Google Scholar]
- ur Rehman, O., & Ali, Y. (2021). Enhancing healthcare supply chain resilience: decision-making in a fuzzy environment. The International Journal of Logistics Management.
- Yousefi S., Soltani R., Saen R.F., Pishvaee M.S. A robust fuzzy possibilistic programming for a new network GP-DEA model to evaluate sustainable supply chains. Journal of Cleaner Production. 2017;166:537–549. [Google Scholar]
- Yue X., Wang H., Jin D., Li M., Jiang W. Healthcare data gateways: Found healthcare intelligence on blockchain with novel privacy risk control. Journal of medical systems. 2016;40(10):218. doi: 10.1007/s10916-016-0574-6. [DOI] [PubMed] [Google Scholar]
- Zhang P., White J., Schmidt D.C., Lenz G., Rosenbloom S.T. FHIRChain: Applying blockchain to securely and scalably share clinical data. Computational and Structural Biotechnology Journal. 2018;16:267–278. doi: 10.1016/j.csbj.2018.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.