Introduction
COVID-19 pandemic has unmasked unmet needs of people with Parkinson disease (PWP). There have been increasing reports of major detrimental effects of COVID-19 in PWP, including worsening of PD [1, 2], disruption in care [3], and increased complications in motor, non-motor, and mental health (MH) domains, as well as the recently described long COVID syndrome.[4–6] Though the inadequate preparedness of health systems has been previously recognized in the area of MH needs and wellness in PWP[7], the devastating impact of the pandemic has further deepened this chasm of care. In particular, the pandemic has magnified chronic issues of social disconnection, loneliness, economic hardship, and barriers to accessing care, especially in people of minority ethnic populations. For many PWP and their caregivers, this has spiraled into a mental health crisis and diminished quality of life.[3, 8] To meet these challenges, we created The Parkinson Wellness and Mental Health Consortium, a group of global experts in movement disorders from multi-disciplinary backgrounds along with PWP and other stake holder voices. We endeavor to create a framework for systematically and proactively addressing the mental health and social needs of this vulnerable population during the pandemic and beyond. Specifically, we focus here on approaches to mitigate the disparities in care among communities of both high- and low-income nations, to optimize health care system infrastructure for PWP, to increase accessibility of multidisciplinary care-team models, and circulate awareness of wellness-enhancing approaches. Our recommendations are developed through a review of 90 common-sense model interviews of key stakeholders and thought-leaders.
A. Barriers to Mental Health in PD
There are many barriers to achieving mental health (Figure 1) and here we discuss common ones.
Figure 1:
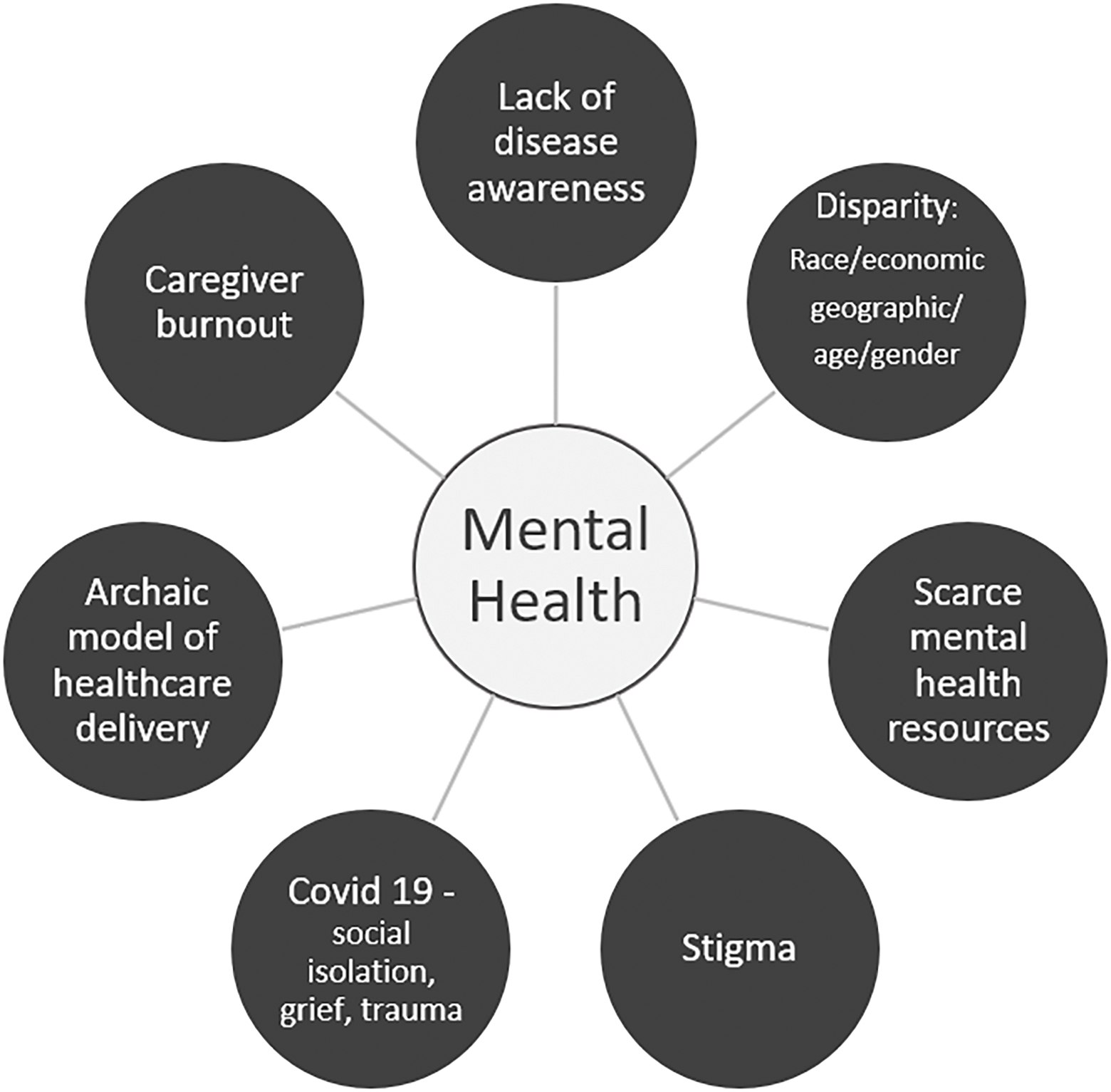
Barriers to Mental Health and Wellness in PD- Pre-existing barriers related to systemic and disease specific issues as well as those uncovered by COVID-19.
1. Lack of Disease Awareness:
Lack of Awareness of PD: Parkinson disease (PD) is a neurodegenerative condition that affects a wide range of age groups, diverse ethnic backgrounds, men and women.[9] However, for many clinicians, the image of the old white man with gray hair and a bent posture leaning on a cane that they learned about in medical school has stuck with them throughout their career. This image is propagated by the continued focus on this population in trials and has done a disservice to many other PWP whose diagnoses were delayed due to the lack of awareness that this disease can present in a young black mom in her 30’s or an Asian actress in her 40’s. [10] Accuracy of PD diagnosis is reduced in communities with poor access to specialist care. In fact, in some rural places, 83% of PWP go entirely undiagnosed.[11]
Lack of Awareness of Non-motor issues in PD: PD is commonly characterized as a movement disorder with focus placed only motor symptoms.[12] It has taken until very recently to raise awareness—even among PD clinical specialists and the scientific community—of the importance of non-motor issues such as constipation and bladder issues in PD and their devastating effects on quality of life and disability. [13, 14]
Lack of Awareness of Mental Health Issues in PD: A previous survey of PWP responded that “doctors were not sensitive enough about PD-related issues in MH treatment” as a barrier to care in 59% of responders. [15] Psychological symptoms in PD can be as disabling as motor symptoms and their severity are a key predictor of quality of life. [16, 17]MH issues faced by PWP can be barriers for their ability to seek care in the first place. For example, PWP experiencing apathy or depression may lack the motivation to seek help. Furthermore, many patients and their caregivers do not know that apathy, depression or anxiety may even be related to PD. [18] [19]
It is essential to educate both providers and the public about the full spectrum of PD symptoms including non-motor symptoms and mental health issues. Public service announcements illustrating the diversity of patient types and presentations are critical.
2. Disparity- Race, Gender, Age, Geographic, Disability:
There are disparities in the care of PWP, with specialty centers and advanced therapies being disproportionately accessible to affluent, married, urban-dwelling, Caucasians. [20]
Race: The COVID vaccination campaign has revealed that issues of mistrust and inequality are deep-seated and are pervasive amongst even healthcare providers of color. [21]Black and Latinx patients experience tremendous barriers that lead them to distrust providers or avoid care altogether.[22] They may not have equal access to interventions such as deep brain stimulation (DBS) surgery, which is offered less often to black women than other populations with PD. Less than 1% of all DBS in the USA was performed in African Americans. [20, 23] There is a lack of inclusion and diversity in trials of PWP. A recent meta-analysis reported on 63 trials with a total of 7,973 patient in which only 11 (17.5%) reported race/ethnicity. Of studies reporting this data, 5 African American (0.2%), 16 Hispanics (0.64%), and 539 Asians (21.44%) were enrolled.[24]
Gender: Women with PD are another underserved population with specific MH needs that must be addressed with customized strategies. [25] Many women have issues with guilt, inadequacy, and low self-esteem in society and this is compounded by a diagnosis of PD. The burdens of caring for ailing parents, homeschooling children, being separated from grandchildren, and balancing work stresses have all impacted women disproportionately during the pandemic.[26]
Age: Young-onset PD are another unique group of PWP with stressors such as the impacts of diagnosis on romantic relationships, family dynamics, and employment.[27] An intersectional framework may also help providers understand how other aspects of identity may compound the impact of a PD diagnosis on overall quality of life. For example, a young, black, mom facing economic hardship or a Latinx migrant farm worker who does not speak English are a few examples of persons who face unique challenges that must be proactively addressed in the context of PD.
Geographic: In the current model of care, most movement disorders specialists (MDS) working within multidisciplinary teams that include mental health support are in urban settings.[28] In fact, in the USA, most Centers of Excellence in the Veterans Administration (PADRECCs) and with Parkinson Foundations are located in large cities. [28] Broadly similar issues and structures are in place in most countries with an established MDS service. [7] This places additional practical burdens (e.g., coordinating and affording travel) on PWP from rural communities that may be intolerable when combined with a background of MH challenges. Lack of transportation (including parking, inability to drive, afford transportation) was identified by 30–40% of PWP surveyed as a barrier to mental health care. [15]
Disability: As patients become more disabled, they have increasing difficulty accessing care in the urban office setting related to travel, reliance on public transport as well as stress of moving from remote residences to busy urban centers. Motor issues with disability from PD have been identified as significant barriers to seeking mental health care by at least 40% of patients surveyed. [15] Clearly, this exemplifies a flaw in our healthcare delivery model. Patients with mental health conditions can be helped in the community setting where they are living, but such support is lacking.[28]
3. Scarce Resources:
There is a shortage of MDS and neurologists worldwide. The deficit of MH specialty care for PWP is even greater.[28] A 2018 report by the All Party Parliamentary Group (APPG) in the UK emphasized a paucity of specialist mental health services for PWP compared to other neurological conditions and that people can wait months or years to get help. The prevalence of PD is increasing with life expectancy, with numbers expected to double by 2040, bringing an impact that will be felt in developing as well as MENASA (Middle Eastern, North African, South Asian countries).[29] Resultant demands on mental health support resources related to this vast projected increase in PD are likely to be considerable and the demand will outstrip capacity.[30] This shortage will only worsen as we are not training enough specialists to meet these needs.[28] [31] Haiti and some African nations may not have more than one general neurologist for the whole country and hence, lack even one MDS for the population. [31] These shortages are associated with potentially dangerous consequences due to undertraining and poor prescription practices. For example, many of the medications given to patients with MH issues (such as dopamine-blocking agents like antipsychotics) can dramatically worsen PD symptoms or are not well-tolerated in PWP (such as benzodiazepines).
Many of the most at-risk PWP cannot afford a computer, smart-phone, or quality internet access.[32] Out of pocket cost of MH care has been identified as a barrier in 64% of respondents in a survey of PWP. [15] Some PWP may not be literate with this technology and need assistance to connect to these platforms. This barrier excludes the most vulnerable populations from the remote care models and social prescription strategies that have been relied upon during the pandemic. [33]
4. Stigma:
Social stigma represents a huge barrier to mental health care that affects populations across the globe, especially people of color.[34] Mistrust is cited as a barrier to mental health care in 20% of a survey of predominantly Caucasian PWP,[15] but discrimination can further exacerbate this in Black, some South Asian, and Latinx communities. [35] PWP are often embarrassed by issues with their MH and do not disclose these issues unless specifically queried, as has been highlighted by Hurt et al. [12] Most PWP will not come forward to their provider and complain about impulse control issues, loneliness, or apathy. Importantly, PWP may be more willing to treat their mental health issues if they can be identified as related to PD itself or a chemical imbalance of the PD.[36] Stigma also affects seeking care from a mental health professional even when mental health issues are linked to PD. [37, 38]Most patients (and many if not most clinicians) see the mind and the body as two separate entities. They would much rather see a neurologist than a psychiatrist or a psychologist.[39]
5. Pandemic Related Issues:
Currently, due to the pandemic, MH providers are overstretched and the wait times even with good insurance or ability to pay out of pocket is months to year to access a provider. This is complicated further by the inability of some to engage with electronics and others for simply not having the resources to fund appropriate laptop and web-cameras. Loss of employment due to the pandemic further can compound issues of cost-prohibitive MH care.
COVID has unmasked the mental health crisis and is compounding the effects of earlier traumas, including Adverse Childhood Experiences (ACES) and their consequences, such as Post-traumatic stress disorder (PTSD). [40]Inter-generational trauma especially in communities of color and women should also be considered. There has been little if no study or attention paid to the effects of trauma on PD. [41] More attention needs to be paid to the ominous effects of COVID as an ongoing societal or mass trauma that is causing a concerning burden of lingering residual mental and physical health consequences. Many PWP have had loved ones pass due to the virus and not had the chance to grieve properly due to social distancing. Some PWP have themselves had COVID and are dealing with the after-effects of the virus on their brains and bodies in Long-COVID syndrome.[6]
6. Caregiver Burnout:
Resources addressing unmet needs in PD have largely focused on the PWP. Caregiver mental health and burnout is a major issue as well. Social distancing and isolation, has increased the burden on caregivers who have not been able to get respite for over a year of the pandemic. Surveys of caregivers in neurological disease involving cognitive issues have revealed the tremendous hardship this responsibility creates. [42]Specifically, caregiver worries included the risk of contagion and death, hyperarousal symptoms (e.g., irritability, hypervigilance) and avoidance behavior (e.g., denial of the meanings and consequences of the pandemic). [43] Addressing the needs of caregivers is fundamental to any mental health support plan of PWP and a gap in research including caregivers input in constructing models of care has been identified. [44–46]
7. Archaic model of health care delivery:
The current model of health care delivery has led to a lack of focus and time to address mental health issues in PD.[28] Especially in the US, a fee-for-service model for healthcare leads to little or no incentive to pursue patient-centered care. Much of care tends to be reactionary rather than emphasizing prevention. Most physicians see PD patients every 6 months for about 15–30 minutes. [47] There is simply not enough time to address all of the issues in the motor and non-motor domains in this timeframe [47]. In the subset of non- motor symptoms in PD, mental health awareness is even less of a focus. 38.5% of responders identified that a specific referral was not given for a mental health complaint as a barrier to mental health care. [15]During the pandemic, reduced in-person contact and mask use (which obscures facial expressions) complicate the identification of disordered mental states.
Since MDS are the ones at the helm of research, advocacy and PD leadership, motor disability is often over-emphasized and non-motor disability is under-represented. Neurologists spend most of the visit adjusting medications for PD motor impairment, while mental health issues are often unrecognized until they become a crisis. Once the calamity is averted, the approach is to put out the fire and move on with the baseline care until the next disaster presents. These erratic time points for accessing mental health resources leads to a relationship with mental health providers that is associated only with times of crises. Hence, understandably, PWP may hesitate to follow-up or consult with mental health specialists rather than developing long-term rapport and coping strategies to reenforce emotional well-being.[48]
B. Strategies to Promote Wellness in PD: A New model
We have outlined important gaps and barriers to achieving better mental health for PWP, we now propose wellness as a key solution. Wellness has been defined as “The active pursuit of activities, choices and lifestyles that lead to a state of holistic health”.[49] Several solutions for more holistic health delivery in PWP have been proposed and implemented throughout the world emphasizing multidisciplinary team approaches and novel models of healthcare delivery. However, these models have focused on motor issues. Examples such as Parkinson Allied Team Training (Parkinson’s Foundation, Global), ParkinsonNet (Netherlands), Hamburg Parkinson Day Clinic (Germany), have been reviewed recently. [46] Our model of a wellness solution is illustrated in Figure 2 and starts with education and empowerment with the long-term goal of wellness which is improved self- efficacy for PWP and their caregivers. Self-efficacy has been shown to improve quality of life. [45, 50, 51] A recent review stated that the ultimate goal of health in PD is to support people with Parkinson’s disease in their ability to participate in activities that are meaningful to them and to support them in self-management. [52]There has been a new focus on the role of the patient participation in their own health including adopting a healthy lifestyle that involves regular exercise and an appropriate diet and involving the PWP in medical decisions based on education and physician guidance. [53]This review further stated that PWP want there to be more of a focus on clinical care and research around lifestyle choices. [53]
Figure 2:
Wellness Strategies: Emphasizing lifestyle choices, education, social support, and self-agency.
1. Education: Including disease awareness
To address the global health needs of PWP worldwide, core educational resources in mental health and wellness should be created in different forms for different audiences. Patient- and provider-facing resources should be created in the form of paper materials that can be handed out directly to patients as well as internet-based materials that can be downloaded. Core educational videos for patients and providers to increase awareness of PD, non-motor issues in PD and mental health issues should be made available and translated widely.
2. Empowerment through teachable lifestyle choices:
Wellness strategies to support holistic health including resilience training, enhancing a positive attitude, perseverance, and empowering patients by giving them a sense of agency. These are all important tools that should be available to all PWP, but there has been a lack of study historically in this area.[54] A number of self-management strategies are promising but need to include the caregiver and peer support in their adoption. [45] Historically, there has been a disproportionate focus on pharmacological interventions in treating mental health issues in PWP. Many patients would like an alternative to adding another pill. [55]Patients want free (or affordable), transportable, and understandable wellness strategies and ways that they can empower themselves to take control of their own health. Counselling and education on modifiable lifestyle choices including sleep, diet, multi modal exercise based strategies (including dance), mind- body and social connection should be available to all PWP from diagnosis. [56]It has been proposed that there should be an emphasis on early assessment to allow for effective psychosocial management from the point of diagnosis longitudinally through to palliative care.[18] [48]
3. Realigned Health Care Team Model:
Novel strategies such as the following have been proposed by PWP and should be considered:
A “mental health check-in buddy” who could be a friend or paired PWP that is assigned to check in about how the PWP are doing through a weekly phone call.
Peer-to-peer mentoring where an older or more seasoned PWP may guide a patient through their disease trajectory.
Health coaches may have expertise to guide certain wellness strategies or exercise classes (e.g. Bounce Back program in Canada uses online coaching and a workbook to help guide patients).
Community health/link workers who form vital connections by referral from the health care system to connect patients with social support that emulates models from other parts of the world (e.g. National Health Service in the UK)[57] need to be explored with an open mind.
Matching lower-level psychotherapists to serve more numbers of less severe patients and to decrease wait times (Improving Access to Psychological Therapy- IAPT by the National Health Service)[58].
4. Proactive Outreach/Global Dissemination:
Anticipating the growing needs of PWP emerging from the pandemic and beyond, there needs to be proactive outreach to any and all partners willing to collaborate on this endeavor including all communities that having suffered from disparate care. By leveraging the knowledge base of the scarce subspecialty providers base for the greatest good for all PWP worldwide, we can provide a virtual platform to share vetted resources and strategies. Geriatricians, primary care doctors, nurses, social workers, caregivers and all who can be engaged to care about PWP should be trained and have access to core resources to support PWP and their mental health needs. [59] Basic knowledge of PD medications and safety issues should be known to all health care providers in all settings.
5. Social Prescribing:
There is evidence that social isolation and loneliness can magnify non-motor issues in PWP and are associated with poor quality of life. [60]Social prescribing strategies in which vulnerable patients can be identified proactively and prescribed social support need to be explored in PWP. [57] “Social Prescribing” is when health professionals refer patients to support in their community in order to improve their health and wellbeing. This strategy has gained traction in the National Health Service [57]in the UK and has been slowly adopted in other countries e.g. The Veteran Administration Compassionate Contact Corps initiative[60]. These strategies would utilize possible novel community outreach liaisons such as link-workers, mentors, coaches or support group leaders.
6. Self-agency:
The ultimate goal of any wellness strategy it to help the patient feel in control of their own health by making lifestyle choices that will help them to achieve a better quality of life and higher level of functioning.
The COVID-19 pandemic has inflicted a historic crisis on nearly all communities around the globe, severely disrupting the lives of PWP and their care partners. While inadequate preparedness of health systems and practices existed and have been recognized in the area of mental health needs and wellness of PWP before, the disastrous impact of the COVID-19 pandemic has wrought the mental health gaps dramatically wider. As we reel from the unspeakable tragedies in the wake of this global crisis, we have an obligation to seize the opportunity to create major reform in approaching disparities in care both in higher- and lower-income countries. As we rebuild and move forward from the pandemic, we can use this opportunity to truly realign the health care model to include a more holistic multidisciplinary approach to mental health and wellness in PWP.
Footnotes
Declarations of interest:
IS: Consultation for Acadia and Acorda Therapeutics
JTH: None
KRC: Serves on advisory boards for: AbbVie, UCB, GKC, Bial, Cynapsus, Lobsor, Stada, Medtronic, Zambon, Profile, Sunovion, Roche, Therevance, Scion, Britannia, Acadia, 4D. Received honoraria for lectures to: AbbVie, Britannia, UCB, Zambon, Novartis, Boeringer Ingelheim, Bial, Kyowa Kirin, SK Pharma. Grants (Investigator Initiated): Britania Pharmaceuticals, AbbVie, UCB, GKC, Bial, Aacdemic grants: EU, IMI EU, Horizon 2020, Parkinson’s UK, NIHR, PDNMG, EU (Horizon 2020), Kirby Laing Foundation, NPF, MRC, Wellcome Trust.
ZM: CME honoraria from Cleveland Clinic and the Movement Disorder Society. Editorial honorarium from Elsevier (assoc. editor for PRD). Advisory fees from Global Kinetics Corporation. Consulting honoraria from: Reckner Health, m-Panels, Amneal, Acadia, Abbvie, Sanofi Genzyme, GB Sciences, and Kyowa Kirin.
HF: Research support from Alkahest, Amneal, Biogen, Michael J. Fox Foundation, NIH/NINDS, Parkinson’s Foundation, Parkinson Study Group, but has no owner interest in any pharmaceutical company. Honoraria from Cleveland Clinic as a speaker in CME events; other honoraria from Bial Neurology, Biopas, Cerevel, CNS Ratings, Covance, Kyowa Hakko Kirin, Partners Healthcare System, Parkinson Study Group, Sun Pharmaceutical Industries (5), Sunovion Research and Development Trust as a consultant. HF receives a stipend from Elsevier as the Editor-In-Chief of Parkinsonism and Related Disorders Journal. He has received royalty payments from Demos Publishing and Springer for serving as a book author/editor.
GP: Consultation for Acadia Pharmaceuticals, Concert Pharmaceuticals, and Cerevance.
References
- [1].Baschi R, Luca A, Nicoletti A, Caccamo M, Cicero CE, D’Agate C, Di Giorgi L, La Bianca G, Lo Castro T, Zappia M, Monastero R, Changes in Motor, Cognitive, and Behavioral Symptoms in Parkinson’s Disease and Mild Cognitive Impairment During the COVID-19 Lockdown, Front Psychiatry 11 (2020) 590134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Zhai H, Lv Y, Xu Y, Wu Y, Zeng W, Wang T, Cao X, Xu Y, Characteristic of Parkinson’s disease with severe COVID-19: a study of 10 cases from Wuhan, J Neural Transm (Vienna) 128(1) (2021) 37–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Brown EG, Chahine LM, Goldman SM, Korell M, Mann E, Kinel DR, Arnedo V, Marek KL, Tanner CM, The Effect of the COVID-19 Pandemic on People with Parkinson’s Disease, J Parkinsons Dis 10(4) (2020) 1365–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Antonini A, Leta V, Teo J, Chaudhuri KR, Outcome of Parkinson’s Disease Patients Affected by COVID-19, Mov Disord 35(6) (2020) 905–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Feeney MP, Xu Y, Surface M, Shah H, Vanegas-Arroyave N, Chan AK, Delaney E, Przedborski S, Beck JC, Alcalay RN, The impact of COVID-19 and social distancing on people with Parkinson’s disease: a survey study, NPJ Parkinsons Dis 7(1) (2021) 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Leta V, Rodriguez-Violante M, Abundes A, Rukavina K, Teo JT, Falup-Pecurariu C, Irincu L, Rota S, Bhidayasiri R, Storch A, Odin P, Antonini A, Chaudhuri KR, Parkinson’s disease and Post-COVID-19 syndrome: The Parkinson’s Long-COVID spectrum, Mov Disord (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bhidayasiri R, Panyakaew P, Trenkwalder C, Jeon B, Hattori N, Jagota P, Wu YR, Moro E, Lim SY, Shang H, Rosales R, Lee JY, Thit WM, Tan EK, Lim TT, Tran NT, Binh NT, Phoumindr A, Boonmongkol T, Phokaewvarangkul O, Thongchuam Y, Vorachit S, Plengsri R, Chokpatcharavate M, Fernandez HH, Delivering patient-centered care in Parkinson’s disease: Challenges and consensus from an international panel, Parkinsonism Relat Disord 72 (2020) 82–87. [DOI] [PubMed] [Google Scholar]
- [8].Helmich RC, Bloem BR, The Impact of the COVID-19 Pandemic on Parkinson’s Disease: Hidden Sorrows and Emerging Opportunities, J Parkinsons Dis 10(2) (2020) 351–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hirsch L, Jette N, Frolkis A, Steeves T, Pringsheim T, The Incidence of Parkinson’s Disease: A Systematic Review and Meta-Analysis, Neuroepidemiology 46(4) (2016) 292–300. [DOI] [PubMed] [Google Scholar]
- [10].Armstrong MJ, Okun MS, Time for a New Image of Parkinson Disease, JAMA Neurol (2020). [DOI] [PubMed] [Google Scholar]
- [11].Kis B, Schrag A, Ben-Shlomo Y, Klein C, Gasperi A, Spoegler F, Schoenhuber R, Pramstaller PP, Novel three-stage ascertainment method: prevalence of PD and parkinsonism in South Tyrol, Italy, Neurology 58(12) (2002) 1820–5. [DOI] [PubMed] [Google Scholar]
- [12].Hurt CS, Rixon L, Chaudhuri KR, Moss-Morris R, Samuel M, Brown RG, Barriers to reporting non-motor symptoms to health-care providers in people with Parkinson’s, Parkinsonism Relat Disord 64 (2019) 220–225. [DOI] [PubMed] [Google Scholar]
- [13].Schapira AHV, Chaudhuri KR, Jenner P, Non-motor features of Parkinson disease, Nat Rev Neurosci 18(8) (2017) 509. [DOI] [PubMed] [Google Scholar]
- [14].Pontone GM, Bakker CC, Chen S, Mari Z, Marsh L, Rabins PV, Williams JR, Bassett SS, The longitudinal impact of depression on disability in Parkinson disease, Int J Geriatr Psychiatry 31(5) (2016) 458–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Dobkin RD, Rubino JT, Friedman J, Allen LA, Gara MA, Menza M, Barriers to mental health care utilization in Parkinson’s disease, J Geriatr Psychiatry Neurol 26(2) (2013) 105–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Soh SE, Morris ME, McGinley JL, Determinants of health-related quality of life in Parkinson’s disease: a systematic review, Parkinsonism Relat Disord 17(1) (2011) 1–9. [DOI] [PubMed] [Google Scholar]
- [17].Leroi I, McDonald K, Pantula H, Harbishettar V, Cognitive impairment in Parkinson disease: impact on quality of life, disability, and caregiver burden, J Geriatr Psychiatry Neurol 25(4) (2012) 208–14. [DOI] [PubMed] [Google Scholar]
- [18].Shulman LM, Taback RL, Rabinstein AA, Weiner WJ, Non-recognition of depression and other non-motor symptoms in Parkinson’s disease, Parkinsonism Relat Disord 8(3) (2002) 193–7. [DOI] [PubMed] [Google Scholar]
- [19].Kua ZJ, Pachana NA, Byrne GJ, O’Sullivan JD, Marsh R, Torbey E, Silburn PA, Mellick GD, Dissanayaka NNW, How Well Do Caregivers Detect Depression and Anxiety in Patients With Parkinson Disease?, J Geriatr Psychiatry Neurol 31(5) (2018) 227–236. [DOI] [PubMed] [Google Scholar]
- [20].Ojukwu DI, Andruska KM, Halpern CH, Lessons From George Floyd: Racial Inequalities in the Treatment of Parkinson’s Disease, Mov Disord (2020). [DOI] [PubMed] [Google Scholar]
- [21].Shekhar R, Sheikh AB, Upadhyay S, Singh M, Kottewar S, Mir H, Barrett E, Pal S, COVID-19 Vaccine Acceptance among Health Care Workers in the United States, Vaccines (Basel) 9(2) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Dahodwala N, Willis AW, Li P, Doshi JA, Prevalence and Correlates of Anti-Parkinson Drug Use in a Nationally Representative Sample, Mov Disord Clin Pract 4(3) (2017) 335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Eskandar EN, Flaherty A, Cosgrove GR, Shinobu LA, Barker FG, 2nd, Surgery for Parkinson disease in the United States, 1996 to 2000: practice patterns, short-term outcomes, and hospital charges in a nationwide sample, J Neurosurg 99(5) (2003) 863–71. [DOI] [PubMed] [Google Scholar]
- [24].Di Luca DG, Sambursky JA, Margolesky J, Cordeiro JG, Diaz A, Shpiner DS, Moore HP, Singer C, Luca C, Minority Enrollment in Parkinson’s Disease Clinical Trials: Meta-Analysis and Systematic Review of Studies Evaluating Treatment of Neuropsychiatric Symptoms, J Parkinsons Dis 10(4) (2020) 1709–1716. [DOI] [PubMed] [Google Scholar]
- [25].Dahodwala N, Shah K, He Y, Wu SS, Schmidt P, Cubillos F, Willis AW, Sex disparities in access to caregiving in Parkinson disease, Neurology 90(1) (2018) e48–e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Del Boca D, Oggero N, Profeta P, Rossi M, Women’s and men’s work, housework and childcare, before and during COVID-19, Rev Econ Househ (2020) 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Calne SM, Lidstone SC, Kumar A, Psychosocial issues in young-onset Parkinson’s disease: current research and challenges, Parkinsonism Relat Disord 14(2) (2008) 143–50. [DOI] [PubMed] [Google Scholar]
- [28].Pontone GM, Dissanayaka N, Dobkin RD, Mari L, Marsh L, Vernaleo BA, Weintraub D, Mari Z, Integration and Extension of Specialty Mental Healthcare Services to Community Practice in Parkinson Disease, Am J Geriatr Psychiatry 27(7) (2019) 712–719. [DOI] [PubMed] [Google Scholar]
- [29].Global, regional, and national burden of Parkinson’s disease, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016, Lancet Neurol 17(11) (2018) 939–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Dorsey ER, Glidden AM, Holloway MR, Birbeck GL, Schwamm LH, Teleneurology and mobile technologies: the future of neurological care, Nat Rev Neurol 14(5) (2018) 285–297. [DOI] [PubMed] [Google Scholar]
- [31].Dorsey R, Ending Parkinson’s disease : a prescription for action, PublicAffairs, New York, 2020. [Google Scholar]
- [32].Spear KL, Auinger P, Simone R, Dorsey ER, Francis J, Patient Views on Telemedicine for Parkinson Disease, J Parkinsons Dis 9(2) (2019) 401–404. [DOI] [PubMed] [Google Scholar]
- [33].Cubo E, Hassan A, Bloem BR, Mari Z, Group MD-TS, Implementation of Telemedicine for Urgent and Ongoing Healthcare for Patients with Parkinson’s Disease During the COVID-19 Pandemic: New Expectations for the Future, J Parkinsons Dis 10(3) (2020) 911–913. [DOI] [PubMed] [Google Scholar]
- [34].Krill Williston S, Martinez JH, Abdullah T, Mental health stigma among people of color: An examination of the impact of racial discrimination, Int J Soc Psychiatry 65(6) (2019) 458–467. [DOI] [PubMed] [Google Scholar]
- [35].Alang SM, Mental health care among blacks in America: Confronting racism and constructing solutions, Health Serv Res 54(2) (2019) 346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Weiss HD, Pontone GM, “Pseudo-syndromes” associated with Parkinson disease, dementia, apathy, anxiety, and depression, Neurol Clin Pract 9(4) (2019) 354–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Salazar RD, Weizenbaum E, Ellis TD, Earhart GM, Ford MP, Dibble LE, Cronin-Golomb A, Predictors of self-perceived stigma in Parkinson’s disease, Parkinsonism Relat Disord 60 (2019) 76–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Oehlberg K, Barg FK, Brown GK, Taraborelli D, Stern MB, Weintraub D, Attitudes regarding the etiology and treatment of depression in Parkinson’s disease: a qualitative study, J Geriatr Psychiatry Neurol 21(2) (2008) 123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Ventriglio A, Bhugra D, Descartes’ dogma and damage to Western psychiatry, Epidemiol Psychiatr Sci 24(5) (2015) 368–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Vindegaard N, Benros ME, COVID-19 pandemic and mental health consequences: Systematic review of the current evidence, Brain Behav Immun 89 (2020) 531–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Sarkar T, Patro N, Patro IK, Cumulative multiple early life hits- a potent threat leading to neurological disorders, Brain Res Bull 147 (2019) 58–68. [DOI] [PubMed] [Google Scholar]
- [42].Canevelli M, Valletta M, Toccaceli Blasi M, Remoli G, Sarti G, Nuti F, Sciancalepore F, Ruberti E, Cesari M, Bruno G, Facing Dementia During the COVID-19 Outbreak, J Am Geriatr Soc 68(8) (2020) 1673–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Alexopoulos P, Soldatos R, Kontogianni E, Frouda M, Loanna Aligianni S, Skondra M, Passa M, Konstantopoulou G, Stamouli E, Katirtzoglou E, Politis A, Economou P, Alexaki M, Siarkos K, Politis A, COVID-19 Crisis Effects on Caregiver Distress in Neurocognitive Disorder, J Alzheimers Dis 79(1) (2021) 459–466. [DOI] [PubMed] [Google Scholar]
- [44].Mosley PE, Moodie R, Dissanayaka N, Caregiver Burden in Parkinson Disease: A Critical Review of Recent Literature, J Geriatr Psychiatry Neurol 30(5) (2017) 235–252. [DOI] [PubMed] [Google Scholar]
- [45].Kessler D, Liddy C, Self-management support programs for persons with Parkinson’s disease: An integrative review, Patient Educ Couns 100(10) (2017) 1787–1795. [DOI] [PubMed] [Google Scholar]
- [46].Lidstone SC, Bayley M, Lang AE, The evidence for multidisciplinary care in Parkinson’s disease, Expert Rev Neurother 20(6) (2020) 539–549. [DOI] [PubMed] [Google Scholar]
- [47].Dorsey ER, George BP, Leff B, Willis AW, The coming crisis: obtaining care for the growing burden of neurodegenerative conditions, Neurology 80(21) (2013) 1989–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Bender MW, T., The need for psychotherapeutic services for people with Parkinson’s disease., Psychologist’s Special Interest Group Working With Older People Newsletter, 2005, pp. 17–23. [Google Scholar]
- [49].Stoewen DL, Health and wellness, Can Vet J 56(9) (2015) 983–4. [PMC free article] [PubMed] [Google Scholar]
- [50].Shimbo T, Goto M, Morimoto T, Hira K, Takemura M, Matsui K, Yoshida A, Fukui T, Association between patient education and health-related quality of life in patients with Parkinson’s disease, Qual Life Res 13(1) (2004) 81–9. [DOI] [PubMed] [Google Scholar]
- [51].van der Eijk M, Nijhuis FA, Faber MJ, Bloem BR, Moving from physician-centered care towards patient-centered care for Parkinson’s disease patients, Parkinsonism Relat Disord 19(11) (2013) 923–7. [DOI] [PubMed] [Google Scholar]
- [52].Huber M, Knottnerus JA, Green L, van der Horst H, Jadad AR, Kromhout D, Leonard B, Lorig K, Loureiro MI, van der Meer JW, Schnabel P, Smith R, van Weel C, Smid H, How should we define health?, BMJ 343 (2011) d4163. [DOI] [PubMed] [Google Scholar]
- [53].Bloem BR, Okun MS, Klein C, Parkinson’s disease, Lancet (2021). [DOI] [PubMed] [Google Scholar]
- [54].Zarotti N, Eccles FJR, Foley JA, Paget A, Gunn S, Leroi I, Simpson J, Psychological interventions for people with Parkinson’s disease in the early 2020s: Where do we stand?, Psychol Psychother (2020). [DOI] [PubMed] [Google Scholar]
- [55].Bega D, Zadikoff C, Complementary & alternative management of Parkinson’s disease: an evidence-based review of eastern influenced practices, J Mov Disord 7(2) (2014) 57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Subramanian I, Complementary and Alternative Medicine and Exercise in Nonmotor Symptoms of Parkinson’s Disease, Int Rev Neurobiol 134 (2017) 1163–1188. [DOI] [PubMed] [Google Scholar]
- [57].Roland M, Everington S, Marshall M, Social Prescribing - Transforming the Relationship between Physicians and Their Patients, N Engl J Med 383(2) (2020) 97–99. [DOI] [PubMed] [Google Scholar]
- [58].Clark DM, Canvin L, Green J, Layard R, Pilling S, Janecka M, Transparency about the outcomes of mental health services (IAPT approach): an analysis of public data, Lancet 391(10121) (2018) 679–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Aye YM, Liew S, Neo SX, Li W, Ng HL, Chua ST, Zhou WT, Au WL, Tan EK, Tay KY, Tan LC, Xu Z, Patient-Centric Care for Parkinson’s Disease: From Hospital to the Community, Front Neurol 11 (2020) 502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Subramanian I, Farahnik J, Mischley LK, Synergy of pandemics-social isolation is associated with worsened Parkinson severity and quality of life, NPJ Parkinsons Dis 6 (2020) 28. [DOI] [PMC free article] [PubMed] [Google Scholar]



