Abstract
Research has shown threat overestimation is significantly associated with intolerance of uncertainty (IU), and both processes predict higher anxiety and safety behavior usage. However, the extent to which threat overestimation predicts subsequent COVID-19-related distress may vary as a function of IU. The present study examined IU as a moderator of the relationship between COVID-19 threat estimation and subsequent COVID-19 fear and safety behavior use. Between February 27 and March 26, 2020, participants (N = 57) completed a self-report measure of IU and estimated the number of people they believed had died from COVID-19. Four weeks later, participants completed measures of COVID-19 fear and safety behavior use. Results revealed IU significantly predicted subsequent COVID-19 fear and safety behavior use. IU also moderated the effect of threat estimation on COVID-19 fear such that those who underestimated threat and experienced low to moderate levels of IU reported experiencing lower levels of COVID-19 fear 1 month later.
Keywords: Intolerance of uncertainty, COVID-19, Overestimation of threat
On January 21, 2020, the first case of the coronavirus disease 2019 (COVID-19) was confirmed in the USA (U.S.; Centers for Disease Control, 2020). By late January 2020, 74% of Americans reported being “somewhat concerned” to “very concerned” about the illness spreading to the USA (Morning Consult, 2020), and by mid-March 2020, the World Health Organization had declared COVID-19 a global pandemic (WHO, 2020). Early in the pandemic, approximately 25% of the general population reported experiencing moderate to severe levels of anxiety-related symptoms (Qiu et al., 2020; Wang et al., 2020), and symptoms of anxiety and depression have been shown to increase over the course of the COVID-19 pandemic (del-Valle et al., 2022) . Since then, researchers have identified a wide range of adverse anxiety- and stress-related outcomes associated with the pandemic, which have been collectively termed “COVID Stress Syndrome” (Taylor et al., 2020).
The stress associated with the COVID-19 pandemic has indeed cultivated high anxiety and uncertainty about virus transmission and subsequent death. However, it remains unclear who in particular may be at higher risk for elevated COVID-19 fear. Traditional cognitive models posit higher anxiety risk for those with cognitive biases like threat overestimation coupled with the perceived inability to cope with adverse outcomes (Beck et al., 1985). Although threat-related anticipatory responses are generally adaptive in reducing the risk of harm, this process can be maladaptive when risk estimates exceed the true likelihood. This tendency to overestimate threat has been consistently shown to contribute to the development and maintenance of anxious responding (Abramowitz & Blakey, 2020; Mathews & MacLeod, 2002). Individual differences in the overestimation of threat not only contribute to the subjective experience of fear and anxiety, but they also facilitate the use of safety behaviors, which are unnecessary actions taken to minimize, avoid, or escape negative outcomes (Telch & Lancaster, 2012). Although the use of safety behaviors may temporarily temper the anxiety that is evoked by threat overestimation, they have been shown to paradoxically exacerbate symptoms by preventing the correction of mistakenly held anxious beliefs (Helbig-Lang & Petermann, 2010; Salkovskis, 1991).
Individual differences in threat estimation may be an especially relevant process to better understand anxiety- and stress-related outcomes associated with the pandemic, given the high rates of asymptomatic transmission and the novelty of COVID-19. More specifically, the overestimation of threat may be reflected in the beliefs people hold about the perceived probability/certainty of contracting COVID-19 and subsequently dying from the virus. This proposed link between the overestimation of threat and COVID-related fearfulness is consistent with recent research. For example, one study found that perceived threat was the most reliable predictor of concurrent COVID-related emotional reactions and coping behaviors (Cypryańska & Nezlek, 2020). As stated by Bavel et al. (2020), “people are less likely to die from over-reaction than from under-reaction, that is, not responding to signs of danger until it is too late” (p. 462). Although this suggests that the overestimation of threat may be adaptive by motivating people to wash their hands regularly, practice social distancing, and use face masks, there is also some evidence suggesting that the overestimation of COVID-related threat may be maladaptive. For example, one study found that individuals who felt more threatened by COVID-19 stockpiled more toilet paper (Garbe et al., 2020), leading to fear of contagion and contributing to shortages (Taylor, 2021).
Although the overestimation of threat is likely associated with increased COVID-related fearfulness, the specific processes that may influence this association are unclear. One potentially relevant process is intolerance of uncertainty (IU), which refers to a dispositional characteristic that reflects the tendency to react negatively to situations that are uncertain (Obsessive Compulsive Cognitions Working Group, 1997). Research has shown that overestimation of threat is significantly associated with high levels of IU (Dugas et al., 2004; Koerner & Dugas, 2008) and IU has been posited as a factor that influences the estimation of threat (Pepperdine et al., 2018; Sookman & Pinard, 2002). Consistent with this view, results from the lab-based vignettes have shown that high threat and/or explicitly uncertain scenarios lead to increased anxiety and urges to engage in safety behaviors (Reuman et al., 2015). Further, during the 2009 H1N1 pandemic individuals with high IU were more likely to perceive the pandemic as threatening and experienced heightened levels of anxiety compared to individuals with low IU (Taha et al., 2014). During the COVID-19 pandemic, IU has been positively associated with coronavirus fear in particular (Millroth & Frey, 2021; Wheaton et al., 2021) as well as more general psychological distress (Reizer et al., 2021). Higher IU has also been shown to predict greater fear and avoidance of healthcare settings and increased fear of leaving the home (Radell & McGuire, 2021). Together, these findings suggest that overestimation of threat and IU may be synergistic in explaining fearful responding during a pandemic. Indeed, a recent theoretical model, known as the Uncertainty Distress Model, proposed that dispositional IU will moderate the relationship between threat perception and uncertainty-reducing behaviors (i.e., safety behaviors) and distress (Freeston et al., 2020). However, to our knowledge, this model has yet to be tested empirically.
The existing literature suggests that IU may be one process that influences the association between overestimation of threat and COVID-related fearfulness (Sookman & Pinard, 2002; Taha et al., 2014). Accordingly, the present study examined IU as a potential moderator of the relationship between estimation of COVID-19 threat and subsequent COVID-19 fear and safety behavior use. It was hypothesized that estimation of threat at Time 1 would predict increased coronavirus fear and safety behavior use 4 weeks later at Time 2. Similarly, it was hypothesized that high levels of IU at Time 1 would predict increased coronavirus fear and safety behavior use at Time 2. Lastly, it was hypothesized that IU would moderate the relationship between estimation of threat and coronavirus fear and safety behavior use, such that those high in threat overestimation and high in IU would report the highest levels of COVID-19 fear and safety behavior use.
Method
Participants
The present sample (N = 57; 63.4% female) included undergraduate students from a private southeastern university who were recruited from psychology courses and compensated with course credit. The mean age of the sample was 19.86 (SD = 1.23), ranging from 18 to 22. The racial and ethnic composition of the sample was as follows: White (n = 39; 54.9%), African American (n = 6; 8.5%), Asian/Pacific Islander (n = 14; 19.7%), Hispanic/Latino (n = 3; 4.2%), Other (n = 1; 1.4%).
Measures
Overestimation of Threat
The one-item estimation of threat variable was calculated by subtracting the total number of US deaths (Center for Systems Science and Engineering at Johns Hopkins University, 2020) from the participants’ estimated number of US deaths. Time was accounted for in this measure by coding the total number of U.S. deaths to correspond with the data from the day on which each participant completed the Time 1 survey.
Intolerance of Uncertainty Scale-Short Form (IUS-12; Carleton et al., 2007).
The IUS-12 is a self-report measure that assesses participant responses to uncertainty, ambiguous situations, and the future (e.g., “it frustrates me not having all the information I need”). Items are rated on a 5-point Likert scale ranging from 1 (not at all characteristic of me) to 5 (entirely characteristic of me). The IUS-12 demonstrated excellent internal consistency in the present sample (α = 0.90). IUS-12 scores within the present sample (M = 28.28, SD = 9.08) were comparable to IUS-12 scores within Carleton et al. (2007) undergraduate sample (M = 25.85, SD = 9.45).
The Coronavirus Anxiety Inventory (CAI; Cox et al., 2020; Knowles & Olatunji, 2021).
The CAI is a 10-item self-report measure that assesses fear related to COVID-19. This measure was adapted from similar measures used to examine fear in response to Ebola (Blakey et al., 2015) and H1N1 (Wheaton et al., 2012). The CAI asks participants to rate their beliefs (e.g., “to what extent are you concerned about the coronavirus?”) on a 5-point Likert-type scale ranging from 0 (not at all) to 4 (very much). The CAI demonstrated good internal consistency in the present sample (α = 0.85).
The Coronavirus Safety Behaviors Scale (CSBS; Cox et al., 2020; Knowles & Olatunji, 2021).
The CSBS is a 9-item self-report questionnaire that assesses the degree to which individuals engage in coronavirus-related safety behaviors. Participants were asked to rate the frequency in which they engaged in coronavirus-related safety behaviors on an 11-point Likert-type scale ranging from 0 (not at all) to 10 (extreme amount). Examples of safety behaviors on the CSBS are “washing your hands,” “seeking reassurance from friends/family,” and “avoiding certain places.” The CSBS demonstrated good internal consistency in the present sample (α = 0.86).
Procedure
Participants completed the study measures using RedCap at two time points. RedCap is a secure, web-based application designed to assist in data collection for research studies (Harris et al., 2009), hosted by the university and supported by UL1 TR000445 from NCATS/NIH. Between February 27 and March 26, 2020 (Time 1; N = 108), participants completed the IUS and then estimated the number of individuals who had died from COVID-19 in the United States (COVID-19 threat). Four weeks later (Time 2; N = 57), participants completed the CAI and CSBS to measure COVID-19 fear and safety behavior use, respectively. Participants were then debriefed and compensated for their time.
Data Analytic Overview
To examine whether IU moderated the relationship between threat estimation and COVID-19 fear and safety behavior use, moderation models were conducted using the PROCESS macro for SPSS (Hayes, 2013). Within PROCESS, model 1 was selected, the confidence interval was set to 95%, and predictor variables were mean centered. The Johnson-Neyman technique was applied to statistically significant interactions to assess the threshold of significance (Johnson & Neyman, 1936). Simple effects were computed to examine the effect of one independent variable (i.e., threat perception or IU) on one dependent variable (i.e., coronavirus fear or safety behavior use). Interactions were then examined between the independent variables.
Results
Descriptive Statistics and Associations Between Study Variables
Table 1 shows the correlations between study variables. Moderate, positive associations were found between IU and both coronavirus fear and safety behaviors (p’s < 0.01). Further, there was a large, positive correlation between coronavirus fear and coronavirus safety behavior use (p’s < 0.01). Overestimation of threat was not significantly associated with other study variables (p’s > 0.05).1
Table 1.
Descriptive statistics and correlations among study variables
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. Threat estimation | – | |||
| 2. IUS-12 | .11 | – | ||
| 3. CAI | .13 | .40** | – | |
| 4. CSBS | .12 | .34** | .72** | – |
| Mean | –2.46 | 28.28 | 29.35 | 54.42 |
| SD | 233.77 | 9.08 | 6.64 | 6.64 |
| Range | –640–1384 | 12–54 | 0–40 | 4–85 |
Threat estimation, predicted number of US deaths minus reported number of US deaths (negative numbers represent underestimation of threat); IUS-12 Intolerance of Uncertainty Scale, CAI Coronavirus Anxiety Inventory, CSBS Coronavirus Safety Behaviors Scale. ** = ps ≤ .01
Moderated Effects of IU
Coronavirus Fear
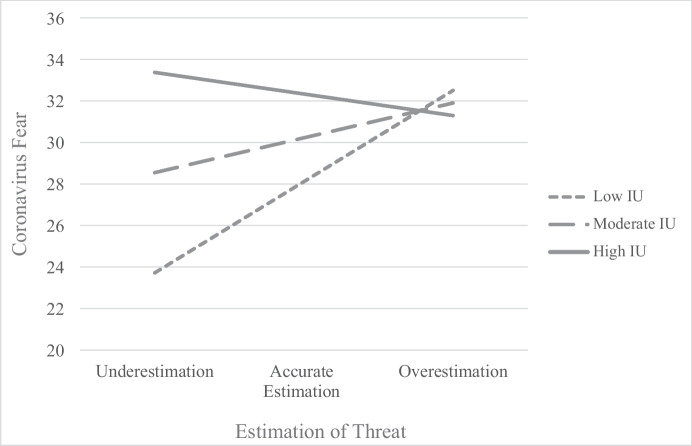
In the model predicting coronavirus fear (see Table 2), there was a significant, simple effect of overestimation of threat, β = 0.04, p = 0.02, 95% CI [0.01, 0.08], on coronavirus fear, suggesting that overestimation of threat is associated with increased coronavirus fear. There was also a significant, simple effect of IU, β = 0.23, p < 0.01, 95% CI [0.09, 0.37], on coronavirus fear, suggesting that IU is associated with increased coronavirus fear. Lastly, the interaction between overestimation of threat and IU was significant in predicting coronavirus fear, ΔR2 = 0.07, p = 0.03 (see Fig. 1).2 An analysis using the Johnson-Neyman technique revealed that for IU scores above the mean, there is no effect of overestimation of threat on coronavirus fear. However, for IU scores at or below the mean, coronavirus fear decreases with lower estimations of threat.
Table 2.
Unstandardized model coefficients for intolerance of uncertainty moderation predicting coronavirus fear and safety behaviors
| Outcome | ||||||
|---|---|---|---|---|---|---|
| Y1 (CAI) | Y2 (CSBS) | |||||
| Predictor | Coeff | SE | p | Coeff | SE | p |
| Threat estimation | .04 | .02 | .02* | .08 | .05 | .14 |
| IUS | .23 | .07 | .002* | .55 | .21 | .01* |
| Threat Estimation × IUS-12 | − .001 | .001 | .03* | − .002 | .002 | .16 |
| ΔR2 | .07 | .03* | .03 | .16 | ||
| Constant | 23.75 | 2.14 | < .001 | 40.39 | 6.33 | < .001 |
| R2 = .24 | R2 = .15 | |||||
| F(3, 53) = 5.56, p = .002 | F(3, 53) = 3.21, p = .03 | |||||
Threat estimation predicted number of US deaths minus reported number of US deaths (negative numbers represent underestimation of threat); IUS-12 Intolerance of Uncertainty Scale, CAI Coronavirus Anxiety Inventory, CSBS Coronavirus Safety Behaviors Scale
Fig. 1.
Simple regression slopes of threat levels predicting coronavirus fear at various levels of IU. All values are mean centered, such that low, moderate, and high levels of threat estimation and IU represent ± 1 standard deviation from the mean. IU, intolerance of uncertainty
Coronavirus Safety Behavior Use
In the model predicting coronavirus safety behavior use (Table 2), there was a significant, simple effect of IU on coronavirus safety behavior use, β = 0.55, p = 0.01, 95% CI [0.12, 0.98], suggesting that IU is associated with increased coronavirus safety behavior use. However, there was not a significant simple effect of threat overestimation on coronavirus safety behavior use. Furthermore, there was not a significant interaction between overestimation of threat and IU in predicting coronavirus safety behavior use.
Discussion
The present study hypothesized that individuals with higher overestimation of threat would report greater COVID-19 fear and safety behavior use. The results partially supported these hypotheses, in that overestimation of COVID-19 threat prospectively predicted higher levels of COVID-19 fear but not higher levels of COVID-19 safety behavior use 4 weeks later. Importantly, these results contribute to the understanding of the relationship between overestimation of threat and IU in the context of the COVID-19 pandemic. The finding linking the overestimation of COVID-19 deaths to subsequent fear about COVID-19 is consistent with current conceptualizations of the tendency to overestimate threat as a key cognitive process that plays a role in the maintenance of anxious responding (Abramowitz & Blakey, 2020). Given the highly contagious nature of COVID-19 as well as the rapid spread of the virus, a considerable amount of fear and anxiety has been observed in the general population. Indeed, individuals in the current study reported moderately high levels of anxiety (M = 29.35, range 0–40) related to COVID-19. The present study suggests that this level of fearfulness observed in the general population may be partially explained by the overestimation of threat. This overestimation of threat may take a variety of forms, including the tendency to catastrophically miscalculate the probability of death or misjudging the presumed severity of other adverse outcomes associated with the virus.
Consistent with the study hypotheses, results also showed higher levels of IU predicted greater COVID-19 fear and safety behavior use 4 weeks later. These findings are consistent with previous research linking IU to anxious responding and safety behavior use in the laboratory (Reuman et al., 2015). This finding also complements previous research showing that anxiety in response to the 2009 H1N1 pandemic was linked to higher IU (Taha et al., 2014). More recently, Wheaton et al. (2021) found that concern about COVID-19 was moderately and positively correlated with IU. Furthermore, IU partially accounted for the connections between concern about the spread of COVID-19 and anxiety-related symptoms. Given that a central characteristic of those high in IU is the incapacity to tolerate the aversive response evoked by the perceived absence of salient, key, or sufficient information (Carleton, 2016), the emergence of a novel coronavirus disease would be expected to result in anxious responding. Unlike those low in IU, the unpredictability, novelty, and change associated with COVID-19 may also increase the range of situations in which “degree of danger” is overestimated and “capacity to cope” is underestimated among those high in IU. In fact, Carnahan et al. (2022) recently found that looming cognitive style, an underlying cognitive vulnerability in which individuals interpret ambiguous situations as threatening (Riskind et al., 2000), prospectively predicted subsequent increases in intolerance of uncertainty, avoidant coping, and state anxiety in a serial mediation model. Consistent with the present study, these findings suggest intolerance of uncertainty, coupled with heightened perceptions of threat, may contribute to elevated anxiety during the COVID-19 pandemic. Given that looming cognitive style may be an important antecedent to intolerance of uncertainty (Carnahan et al., 2022), future research should further explore this relationship both within and outside of the pandemic.
It is important to note that although the correlation between overestimation of threat and COVID anxiety was not significant, overestimation of threat was significant in the regression predicting COVID fear which is likely a case of statistical suppression (i.e., variables remove irrelevant variance from other predictors included in a regression model, thereby increasing the predictive validity of the variable). Furthermore, the present study observed a significant interaction between threat estimation and IU, in which individuals with low to moderate IU who underestimated COVID-19 threat reported lower levels of COVID-19 fear compared to individuals with high IU who reported high levels of COVID-19 fear regardless of the accuracy of their threat estimates. These findings provide preliminary empirical support for the Uncertainty Distress Model, which postulates that IU and perception of threat will influence the degree to which an individual experiences distress (Freeston et al., 2020). Additionally, the finding that self-reported COVID-19 fear for those high in IU was significant and relatively independent of threat estimates further supports the robustness of IU in better understanding COVID-19 related fearfulness. That is, for those high in IU there appears to be a (high) ceiling effect on COVID-19 fear 4 weeks later that is unaffected by threat estimation. For those with low to moderate IU, however, increasing estimation of threat did result in increasing levels of COVID-19 fear 4 weeks later. One potential interpretation of these findings is that high IU may be a risk factor that independently increases vulnerability to anxious responding to COVID-19. However, the finding that individuals who experienced low to moderate levels of IU and underestimated threat reported experiencing lower levels of COVID-19 fear 1 month later suggests this interaction could also reveal a resilience factor that protects against some of the negative effects of COVID-19 related stress. The view that low levels of IU and underestimation of threat may be adaptive in minimizing COVID-19 related fearfulness may be informed by previous research on emotion regulation. More specifically, Taha and colleagues (2014) found that during the 2009 H1N1 pandemic, high IU predicted high anxiety and more emotion-focused coping (compared to problem-focused coping). In contrast, individuals who were able to tolerate uncertainty reported higher appraisals of control, which were subsequently related to more adaptive, problem-focused coping strategies and lower levels of H1N1 anxiety. Of note, previous research has shown adaptive emotional regulation strategies also reduce threat overestimation (e.g., Hovasapian & Levine, 2016). Based on the existing literature, one potential interpretation of the present findings is that individuals lower in IU may be able to engage in more effective coping strategies that inhibit the overestimation of threat, resulting in lower levels of COVID-19 related fear.
The present findings suggest that individuals low in IU may have a higher threshold for perceiving situations as threatening, which results in a reduction in fearful responding. Interestingly, although there was a high degree of variability in threat estimation within the present sample, mean estimation of threat was negative, suggesting these undergraduate students on average are underestimating the threat of COVID-19. It is important to consider that such a disposition could also be maladaptive during a global pandemic. That is, underestimation of COVID-19 threat may result in increased risk-taking behavior. For example, in a national sample of college students, 30.1% reported attending class, 14.5% reported attending work, and 13.7% attended social gatherings while experiencing potential symptoms of COVID-19 in Spring 2020 (Cohen et al., 2020). Although those who underestimated the number of COVID-related deaths who were also low in IU did report less fear of COVID-19, it is unclear if the same individuals were also more likely to engage in risk-taking behaviors during the pandemic. It is important to note that the interaction between overestimation of threat and IU in predicting COVID-19 safety behavior use was not statistically significant in the present study. This suggests that while individuals who are low in IU and who perceive COVID-19 as “low threat” may be less likely to be fearful, they do not appear to be less likely to wash their hands, not socially distance, or not wear a mask.
Although the present study highlights how IU and threat estimation relates to fear of COVID-19 and associated safety behaviors using a prospective design, several study limitations should be noted. First, the present study is limited by the exclusive use of an undergraduate sample from a private institution who may have higher socioeconomic status than the general population. Research has shown that students with above-average socioeconomic status are less likely to be psychologically impacted by COVID-19 (Browning et al., 2021). In particular, undergraduate students may have viewed themselves as less vulnerable to disease than the average individual in the U.S., potentially decreasing threat estimates of COVID-19. Accordingly, these preliminary findings require replication in a nationally representative sample. Although a prospective design was employed, the present study is also limited by a fairly small sample and as such, future studies should attempt to replicate these findings in a larger representative sample. Another limitation of the present study is the operationalization of threat estimation using a single item that may not fully capture all the central elements of the cognitive bias. For example, it may be the case that individuals differ in their estimation of perceived threat for themselves compared to others, which could influence threat estimation scores (e.g., overestimating the threat to others, underestimating the threat to self). Future research should employ a more comprehensive assessment of threat estimation in order to more precisely examine its effects, though such a measure has not yet been validated. Lastly, overestimation of threat and IU were assessed only at Time 1, which prevents drawing causal conclusions regarding their interactive effects. Additional research is necessary to temporally examine the relationship between these variables and how they relate to the development of anxious responding. Future research along these lines may facilitate the identification of risk and resilience factors for heightened anxiety responses to COVID-19 as well as anxiety-related disorders that may emerge as a result of this global pandemic.
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
One overestimation of threat score was identified as a potential outlier (score > 2 SD above the mean). However, the inclusion/exclusion of this outlier did not change the significance of study results and as such was included in all study analyses.
The effect size (f2 = .08) for the moderation model was small. This is however unsurprising given previous research that shows the mean observed effect size for tests of moderation is .009 (Aguinis et al., 2005). Based on this small effect size, the power was found to be .55. Notably, the observed power for tests of moderation has been consistently shown to be quite low (McClelland & Judd, 1993). Because this was a post hoc examination, future research should replicate the pattern of results from the present study in a larger sample.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abramowitz JS, Blakey SM. Overestimation of threat. In: Washington DC, editor. Clinical Handbook of Fear and Anxiety: Maintenance Processes and Treatment Mechanisms. American Psychological Association; 2020. pp. 7–25. [Google Scholar]
- Aguinis H, Beaty JC, Boik RJ, Pierce CA. Effect size and power in assessing moderating effects of categorical variables using multiple regression: A 30-year review. Journal of Applied Psychology. 2005;90:94–107. doi: 10.1037/0021-9010.90.1.94. [DOI] [PubMed] [Google Scholar]
- Bavel JJV, Baicker K, Boggio PS, Capraro V, Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nature Human Behaviour. 2020;4:460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: A cognitive perspective. Basic Book; 1985. [Google Scholar]
- Blakey SM, Reuman L, Jacoby RJ, Abramowitz JS. Tracing “Fearbola”: Psychological predictors of anxious responding to the threat of Ebola. Cognitive Therapy and Research. 2015;39:816–825. doi: 10.1007/s10608-015-9701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning, H. E. M., Larson, L. R., Sharaievska, I., Rigolon, A., McAnirlin, O., Mullenbach, L., . . . Hector, O. A. (2021). Psychological impacts from COVID-19 among university students: Risk factors across seven states in the united states. PLoS One, 16(1) 10.1371/journal.pone.0245327 [DOI] [PMC free article] [PubMed]
- Carleton RN. Fear of the unknown: One fear to rule them all? Journal of Anxiety Disorders. 2016;41:5–21. doi: 10.1016/j.j.anxdis.2016.03.011. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Norton PJ, Asmundson GJG. Fearing the unknown: A short version of the Intolerance of Uncertainty Scale. Journal of Anxiety Disorders. 2007;21:105–117. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Carnahan ND, Carter MM, Sbrocco T. Intolerance of uncertainty, looming cognitive style, and avoidant coping as predictors of anxiety and depression during COVID-19: A longitudinal study. International Journal of Cognitive Therapy. 2022;15:1–19. doi: 10.1007/s41811-021-00123-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (January 21, 2020). First travel-related case of 2019 novel coronavirus detected in United States. https://www.cdc.gov/media/releases/2020/p0121-novel-coronavirus-travel-case.html
- Cohen AK, Hoyt LT, Dull B. A descriptive study of COVID-19–related experiences and perspectives of a national sample of college students in spring 2020. Journal of Adolescent Health. 2020;67(3):369–375. doi: 10.1016/j.jadohealth.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox RC, Jessup SC, Luber MJ, Olatunji BO. Pre-pandemic disgust proneness predicts increase coronavirus anxiety and safety behaviors: Evidence for a diathesis-stress model. Journal of Anxiety Disorders. 2020;76:1–7. doi: 10.1016/j.janxdis.2020.102315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cypryańska M, Nezlek JB. Anxiety as a mediator of relationships between perceptions of the threat of COVID-19 and coping behaviors during the onset of the pandemic in Poland. PLoS ONE. 2020;15:e0241464. doi: 10.1371/journal.pone.0241464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- del-Valle, M. V., López-Morales, H., Andrés, M. L., Yerro-Avincetto, M., Gelpi, T. R., Urquijo, S., & Canet-Juric, L. (2022). Intolerance of COVID-19-related uncertainty and depressive and anxiety symptoms during the pandemic: A longitudinal study in Argentina. Journal of Anxiety Disorders10.1016/j.janxdis.2022.102531 [DOI] [PMC free article] [PubMed]
- Dugas MJ, Buhr K, Ladouceur R. The role of intolerance of uncertainty in etiology and maintenance. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorder: Advances in research and practice. New York: Guilford Press.; 2004. [Google Scholar]
- Freeston MH, Tiplady A, Mawn L, Bottesi G, Thwaites S. Towards a model of uncertainty distress in the context of Coronavirus (Covid-19) The Cognitive Behaviour Therapist. 2020;13:e31. doi: 10.1017/S1754470X2000029X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbe L, Rau R, Toppe T. Influence of perceived threat of COVID-19 and HEXACO personality traits on toilet paper stockpiling. PLoS ONE. 2020;15:e0234232. doi: 10.1371/journal.pone.0234232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)- A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Helbig-Lang S, Petermann F. Tolerate or eliminate? A systematic review on the effects of safety behavior use across anxiety disorders. Clinical Psychology Science and Practice. 2010;17:218–233. doi: 10.1111/j.1468-2850.2010.01213.x. [DOI] [Google Scholar]
- Hovasapian A, Levine LJ. Reappraisal mitigates overestimation of remembered pain in anxious individuals. Cognition and Emotion. 2016;30:1222–1231. doi: 10.1080/02699931.2015.1049937. [DOI] [PubMed] [Google Scholar]
- Johnson PO, Neyman J. Tests of certain linear hypotheses and their application to some educational problems. Statistical Research Memoirs. 1936;1:57–93. [Google Scholar]
- Knowles KA, Olatunji BO. Anxiety and safety behavior usage during the COVID-19 pandemic: The prospective role of contamination faer. Journal of Anxiety Disorders. 2021;77:1–5. doi: 10.1016/j.janxdis.2020.102323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koerner N, Dugas MJ. An investigation of appraisals in individuals vulnerable to excessive worry: The role of intolerance of uncertainty. Cognitive Therapy and Research. 2008;32:619–638. doi: 10.1007/s10608-007-9125-2. [DOI] [Google Scholar]
- Mathews A, MacLeod C. Induced processing biases have causal effects on anxiety. Cognition and Emotion. 2002;16:331–354. doi: 10.1080/02699930143000518. [DOI] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM. Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. Journal of Anxiety Disorders. 2020;74:102258. doi: 10.1016/j.janxdis.2020.102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millroth, P., & Frey, R. (2021). Fear and anxiety in the face of COVID-19: negative dispositions towards risk and uncertainty as vulnerability factors. Journal of Anxiety Disorders, 8310.1016/j.janxdis.2021.102454 [DOI] [PMC free article] [PubMed]
- Morning Consult (January 26, 2020). National tracking poll #200164. https://morningconsult.com/wp-content/uploads/2020/01/200164_crosstabs_CORONAVIRUS_Adults_v1.pdf
- Obsessive Compulsive Cognitions Working Group Cognitive assessment of obsessive-compulsive disorder. Behaviour Research and Therapy. 1997;35:667–681. doi: 10.1016/S0005-7967(97)00017-X. [DOI] [PubMed] [Google Scholar]
- Pepperdine E, Lomax C, Freeston MH. Disentangling intolerance of uncertainty and threat appraisal in everyday situations. Journal of Anxiety Disorders. 2018;57:31–38. doi: 10.1016/j.janxdis.2018.04.002. [DOI] [PubMed] [Google Scholar]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33:100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radell, M. L., & McGuire, B. M. (2021). Intolerance of uncertainty predicts fear of healthcare settings but not desire for testing during the novel coronavirus pandemic. Discover Psychology, 1(1). 10.1007/s44202-021-00010-6
- Reizer A, Geffen L, Koslowsky M. Life under the COVID-19 lockdown: On the relationship between intolerance of uncertainty and psychological distress. Psychological Trauma: Theory, Research, Practice, and Policy. 2021;13(4):432–437. doi: 10.1037/tra0001012. [DOI] [PubMed] [Google Scholar]
- Reuman L, Jacoby RJ, Fabricant LE, Herring B, Abramowitz JS. Uncertainty as an anxiety cue at high and low levels of threat. Journal of Behavior Therapy and Experimental Psychiatry. 2015;47:111–119. doi: 10.1016/jbtep.2014.12.002. [DOI] [PubMed] [Google Scholar]
- Riskind JH, Williams NL, Gessner T, Chrosniak LD, Cortina J. The looming maladaptive style: Anxiety, danger, and schematic processing. Journal of Personality and Social Psychology. 2000;79:837–852. doi: 10.1037/0022-3514.79.5.837. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM. The importance of behavior in the maintenance of anxiety and panic: A cognitive account. Behavioural Psychotherapy. 1991;19:6–19. doi: 10.1017/S0141347300011472. [DOI] [Google Scholar]
- Sookman, D., & Pinard, G. (2002). Overestimation of threat and intolerance of uncertainty in obsessive compulsive disorder. R. O. Frost, G. Steketee (Eds.). Cognitive approaches to obsessions and compulsions: Theory, assessment, and treatment (63–89). Oxford: Elsevier.
- Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H1N1 pandemic. British Journal of Health Psychology. 2009;19:592–605. doi: 10.1111/bjhp.12058. [DOI] [PubMed] [Google Scholar]
- Taha, S., Matheson, K., Cronin, T., & Anisman, H. (2014). Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H 1 N 1 pandemic. British Journal of Health Psychology, 19, 592–605. [DOI] [PubMed]
- Taylor S. Understanding and managing pandemic-related panic buying. Journal of Anxiety Disorders. 2021;78:102364. doi: 10.1016/j.janxdis.2021.102364. [DOI] [PubMed] [Google Scholar]
- Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJG. COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety. 2020;37:706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telch, M. J., & Lancaster, C. L. (2012). Is there room for safety behaviors in exposure therapy for anxiety disorders? In P. Neudeck, & H.U. Wittchen (Eds.). Exposure therapy: Rethinking the model- refining the method (313–334). New York: Springer-Verlag. 10.1007/978-1-4614-3342-2_18.
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton MG, Abramowitz JS, Berman NC, Fabricant LE, Olatunji BO. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research. 2012;36:210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- Wheaton MG, Messner GR, Marks JB. Intolerance of uncertainty as a factor linking obsessive-compulsive symptoms, health anxiety and concerns about the spread of the novel coronavirus (COVID-19) in the United States. Journal of Obsessive-Compulsive and Related Disorders. 2021;28:100605. doi: 10.1016/j.jocrd.2020.100605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (April 27, 2020). WHO Timeline- COVID-19. https://www.who.int/news/item/27-04-2020-who-timeline---covid-19
- Zhou Y, MacGeorge EL, Myrick JG. Mental health and its predictors during the early months of the COVID-19 pandemic experience in the United States. International Journal of Environmental Research and Public Health. 2020;17:6315. doi: 10.3390/ijerph17176315. [DOI] [PMC free article] [PubMed] [Google Scholar]