Abstract
Trust in government is considered a prominent factor for enhancing public compliance with government policies and instructions. The Coronavirus pandemic demonstrates the crucial role public compliance with governmentally issued health guidelines has in mitigating the pandemic. However, the mechanism explaining the trust-compliance association, particularly in regard to health-behavior compliance, is unclear. This article develops a new theoretical model, the Mediated Trust Model (MTM), for explaining the relationship between trust in government and public compliance with health instructions. The model extends the classic Health Belief Model for predicting health behavior by claiming that the perceptions regarding the instructions' costs, benefits and one's ability to perform them are affected by trust in government and mediate the trust-compliance association. The MTM was tested in four cross-sectional studies performed during the first 20 months of the Coronavirus pandemic in Israel on 3732 participants, for various health instructions. Implications for public health literature, policy compliance theory and policy makers are discussed.
Keywords: Trust in government, Compliance, Health behavior, The Mediated Trust Model, COVID-19
Introduction
Trust in government, or interchangeably termed, political trust (Zmerli & van der Meer, 2017), refers to citizens' attitudes regarding the performance and intentions of political actors and institutions, and their consequential confidence in these actors to fairly achieve optimal outcomes (Davies et al., 2021; Levi & Stoker, 2000; Lissitsa, 2021; A. H. Miller, 1974; Norris, 1999; Yap, 2019). It is considered an essential factor for assuring the stability of democratic systems and for enabling better governance and policy implementation, by enhancing public compliance with government policies, which are governmentally issued and promoted behavioral guidelines (Almond & Verba, 1963; Dalton, 2004; Goren et al., 2022; X. Han & Baird, 2022; Levi & Stoker, 2000; Weible et al., 2020; Zmerli & van der Meer, 2017).
Policy compliance is an innate part in policy sciences (Attwell et al., 2021). The association between policy compliance and trust in government was mostly investigated and supported in the context of tax compliance (e.g., Cook & Gronke, 2005; Kirchler et al., 2008; Levi, 1988; Scholz & Lubell, 1998). However, it has also been found in other contexts, such as safe-driving (Tyler, 1990), environment protection (Bruno et al., 2022; Caferra et al., 2021), and health behaviors (e.g., Blair et al., 2017; Q. Han et al., 2021; C. Lee et al., 2016). Nonetheless, the mechanisms explaining the trust-compliance associations are much less clear (e.g., Thomassen et al., 2017). The theoretical tenets that have tried to explain this relationship focused mainly on the government's legitimacy (Hough et al., 2010; Levi & Stoker, 2000; Zmerli & van der Meer, 2017). Specifically, it is argued that political trust affects the levels of legitimacy citizens attribute to their government and their feelings of cooperation and obligation, which in turn, determine their compliance with government policies (Citrin & Stoker, 2018; May, 2005; Murphy, 2004; Norris, 2017; Tyler, 1990). Yet, the assumption within these theoretical strands is that legitimacy explains the trust-compliance relationship regardless of the behavioral context and does not consider that the underlying trust-compliance mechanism may vary from one behavioral (or policy) domain to another. Such variation is especially likely since decision-making processes differ depending on their context and discipline (Chapman, 2004; Kahneman & Tversky, 1979; Morgado et al., 2015; Redelmeier & Tversky, 1990, 1992; Thomadsen et al., 2018). The unique and personal implications of health behaviors and decisions on one's body, health and physiological state, which refer to humans' most basic set of considerations and needs (Maslow, 1943), suggest that health behavior decision processes are likely to be different than other types of behaviors, such as tax-compliance or pro-environmental behavior. Indeed, while classic policy compliance and law obedience scholarships stress the role of perceived legitimacy of the government or sense of moral duty or obligation in compiling with governmentally desired behavior (Fine & van Rooij, 2021; Levi, 1988; Murphy, 2004; Scholz & Lubell, 1998; Thomassen et al., 2017; Tyler, 1990), health behavior theories highlight a complex set of cognitive perceptions and evaluations regarding the promoted behaviors, as behavioral determinants (Green, 1974; Hayden, 2022; Irwig et al., 2008; Janz & Becker, 1984; Prochaska & DiClemente, 1982; Rosenstock, 1974). This emphasizes the likelihood that decision-making processes regarding health-behavior-related instructions are different than those operated in other domains.
Given the seminal role political and democratic theories attribute to trust in government in shaping numerus aspects of our lives and for democratic societies (Hardin, 1999; Warren, 2018), understanding if and why trust in government and civic compliance are related in different contexts is of great importance. Moreover, such understandings are likely to have a significant contribution for times in which civic (non)compliance has life-threatening consequences, such as in public health crises, in which health-behavior-related instructions are likely to be issued.
The recent COVID-19 pandemic highlighted issues of compliance with governmentally issued health instructions at a global scale and stressed the theoretical gap regarding the obscurity of the political trust-compliance relationship in the context of health behaviors (Devine et al., 2021). Yet, many of the studies that aimed to address this gap harnessed various behavioral models and frameworks that seem to misfit the specific context of health behavior (e.g., W. Liu & Huang, 2021; Mizrahi et al., 2022; Saechang et al., 2021; Sata Shanka & Moges Menebo, 2021). Though some of these studies applied health-behavior frameworks in an attempt to explain the political trust-compliance relationship, these investigations either applied these frameworks in a partial manner (e.g., Yuan, 2022), did not focus on governmentally issued instructions and guidelines, but rather on general recommendations regarding protective behaviors issued by various non-governmental organizations (e.g., the World Health Organization; Sarwar et al., 2022), or confined their examination to trust in a specific branch of the government (e.g., trust in the healthcare system; Bord et al., 2021). Furthermore, the relationship between trust in government and compliance with health instructions has recently been challenged altogether with some studies reporting moderate, null and even negative associations between the two concepts (e.g., Clark et al., 2020; Goren et al., 2021, 2022; Jones et al., 2021; Kim & Tandoc, 2021; Pak et al., 2021; Parfenova, 2020; Radu, 2021; Travaglino & Moon, 2021). These inconsistencies stress the complexity of this association and the need for a theoretical model that can explain the political trust-compliance association, specifically in the context of health behaviors.
This study aims to do so by suggesting a model that highlights the mediating role of health-behavior-related factors in the relationship between trust in government and health-behavior compliance. Our model extends a prominent health behavior model, the Health Belief Model (HBM; Janz & Becker, 1984; Rosenstock, 1974), which is the most robust and popular model for predicting health behavior of various types (Mesch & Schwirian, 2015; Shmueli, 2021; Weston et al., 2020). In addition, this study aims to respond to a previous call made by Weible et al. (2020) regarding the need to further investigate factors and conditions that may affect civic response and policy compliance in times in which health instructions are issued (pp. 237–238).
The MTM is based on previous research regarding the potential effects of political trust on health behavior decision-making processes. Its formulization derives from the combination of persuasion theory and health behavior theory. While the first stresses the effect of trusted sources of information on cognitive appraisals of promoted actions (Chaiken, 1980; Chetioui et al., 2021; P. Liu et al., 2019; O’Keefe, 2015; Petty & Cacioppo, 1986; Thaker et al., 2017; Visschers et al., 2011; Wallace et al., 2020), the latter, as mentioned above, and particularly the HBM, focus on cognitive appraisals of actions and their outcomes as a prominent factor in determining health behavior (Green, 1974; Hayden, 2022; Irwig et al., 2008; Janz & Becker, 1984; Prochaska & DiClemente, 1982; Rosenstock, 1974).
The MTM integrates these notions and postulates that when it comes to governmentally instructed health behaviors, trust in government affects compliance by shaping the way citizens appraise and perceive the benefits and costs of governmentally advocated behavior, as well as their ability to carry it out. More specifically, the suggested MTM posits that the association between trust in government and compliance is explained by the main (but not all) appraisal-oriented concepts of the HBM (Janz & Becker, 1984; Rosenstock, 1974). These are perceptions about (1) ones' ability or self-efficacy to perform the promoted behavior; the (2) benefits and the (3) barriers for preforming these actions (see Fig. 1).
Fig. 1.
The Mediated Trust Model and the Health Belief Model
Aiming to test the MTM, we conducted 4 cross-sectional studies, two of which are survey-experiments, across the first 20 months of the Coronavirus pandemic in Israel (April 2020 to November 2021), with a total number of 3732 participants. These studies were performed as a deductive exercise, each of which testing the MTM under slightly different conditions and features. The studies measured compliance intentions of the adult Israeli population with various simulated governmentally issued health guidelines, in different points in time, representing varying duration and severity of the pandemic. The factors of the HBM were measured in all studies, and a path analysis was performed.
This research has the potential to make several important contributions. First, it may enhance public policy literature as it suggests a model that explains the relationship between political trust and compliance with government health instructions, which is not explained by existing political theories. By doing so, this work meets one of the main goals of the policy literature, set by Harold D. Lasswell, which is to provide "insights into unfolding phenomena" (Weible et al., 2020, p. 225), as civic compliance with health instructions is a unique phenomenon, and the mechanism explaining the effects of trust in government on such phenomena is understudied. Second, it stresses variances in the effect of political trust on different types of cognitive perceptions. Specifically, this work demonstrates that political trust is more likely to affect ones' perceptions regarding a governmentally promoted behavior (i.e., costs, benefits, and self-efficacy), but less likely to impact perceptions regarding the situation and circumstances that may justify it (i.e., risk perception). This suggests that political theory should address this complexity and further examine the effects of political trust. Third, this work may contribute to public health literature, as it suggests political trust as an important antecedent of health-behavior-related factors of the HBM and thus, should be taken into consideration as a basic factor in future research on health compliance studies. Lastly, from a practical perspective, this study can provide policy makers with understandings regarding the direct and indirect ways to increase compliance rates with health guidelines and facilitate a quicker control over public health issues or crises. Hence, the current research provides insights for both policy sciences scholars and policy practitioners, regarding the role of trust in government, and additional mediating factors, in the potential levels of public adoption of health-related policies (i.e., behaviors) and the consequential potential achievement of policy goals (Howlett, 2009).
Literature review and hypotheses development
Trust in government
Trust in government is a multilayered concept which can be defined in various ways (Norris, 2017). We adopt a rationalist evaluative approach (Rieger & Wang, 2022) and refer to trust in government as the degree of confidence citizens have in their government, and the extent in which they view it as fair, credible, competent and trustworthy (Davies et al., 2021; Levi & Stoker, 2000; A. H. Miller, 1974). Trust in government, or political trust (Zmerli & van der Meer, 2017), is a deep-rooted trait-like perception (Sønderskov & Dinesen, 2016; Yap, 2019), which develops over time, through early political socialization experiences of individuals (Grimes, 2006; Hooghe & Wilkenfeld, 2008; Schoon & Cheng, 2011; Yap, 2019). Political theory views political trust as "the glue that keeps the [democratic] system together and as the oil that lubricates the policy machine" (Zmerli & van der Meer, 2017, p. 1). Although the relationship between political trust and compliance is not fully explained (Devine et al., 2021; Rothstein` & Stolle, 2008; Thomassen et al., 2017), this view stems from the convention that posits that public's trust in government is essential for public legitimacy of the government's decisions and actions, which not only assures the stability of democratic systems, but also enables better governance and policy implementation, by enhancing public compliance with government policies (Almond & Verba, 1963; Dalton, 2004; Levi & Stoker, 2000; Zmerli & van der Meer, 2017). That is, political trust affects the levels of legitimacy citizens attribute to their government, as well as their feelings of cooperation, and obligation to obey regulations, which in turn, trigger and determine their compliance with government policies (Citrin & Stoker, 2018; Murphy, 2004; Norris, 2017; Tyler, 1990). However, this explanation is challenged by some scholars who argue that the perceived legitimacy of the government does not necessarily derive from political trust, but rather is a type of an independent moral judgment, a sense of duty to comply with authoritative instructions, which may affect compliance, in a separate route from political trust (Gilley, 2006; Peter, 2010). Other scholars posit that legitimacy and political trust comprise the concept of political support (Easton, 1965; Norris, 2017), which is then argued to be the main determinant of compliance (Thomassen et al., 2017).
Differences of opinion regarding the explaining mechanism of the trust-compliance association may not only derive from differences in philosophical viewpoints, but also from variance in policy domains. This is because different behaviors in different context may trigger different decision-making processes (Kahneman & Tversky, 1979; Morgado et al., 2015; Thomadsen et al., 2018). Specifically, evidence shows that decisions regarding health outcomes demonstrate different patterns than those of other domains, such as financially oriented ones (Chapman, 2004; Redelmeier & Tversky, 1990, 1992). Since ones' health decisions impact ones’ physical wellbeing, which is the most basic human motivation (Maslow, 1943), health behaviors may be driven by a stronger intrinsic motivation and be affected by different factors, compared to other types of behavior (Gardiner & Bryan, 2017; Promberger & Marteau, 2013).
Furthermore, as will be elaborated in the next section, prominent theories on health behavior set their main focus on cognitive mechanisms of appraisal of the behavior of interest, at the heart of the health behavior decision-making process (Green, 1974; Hayden, 2022; Irwig et al., 2008; Janz & Becker, 1984; Prochaska & DiClemente, 1982; Rosenstock, 1974). This differs from classic political and law obedience literature, which, as mentioned above, points at a different set of considerations when deciding to comply with laws and regulations in other realms, namely legitimacy and a sense of obligation and duty to comply (Fine & van Rooij, 2021; Levi, 1988; Murphy, 2004; Scholz & Lubell, 1998; Thomassen et al., 2017; Tyler, 1990). In this latter body of literature, cognitive evaluations of the potential outcomes of the desired behaviors are not considered. In fact, the only outcomes that are assessed and weighed are those of non-compliance, i.e., the likelihood of one being caught, punished and the severity of the punishment, in case of non-compliance (Fine & van Rooij, 2021; Kirchler et al., 2008; Tyler, 1990). In other words, according to this scholarship, law obedience and compliance do not depend on citizen's perceptions of the instructed behaviors, but rather on perceptions regarding the government (or the regulating authorities), feelings of obligation to comply and fear of being punished. This detachment, so to speak, of utility considerations regarding the actual behavior/instruction, is supported in some cases of non-health-related contexts, such as tax-compliance, as compliance was found to be unassociated with perceptions regarding the costs and benefits of the instructed behavior (e.g., Scholz & Lubell, 1998). As such detachment is not likely when considering health behavior compliance, it is likely that political trust and compliance with health-related instructions may be associated through a different mechanism than those involved in other types of behaviors and domains, such as tax-compliance or pro-environmental behavior.
Compliance with health instructions
In this study, compliance refers to citizens' willingness to perform and/or the actual performance of specific health behaviors in response to governmentally issued instructions or requirements (Sata Shanka & Moges Menebo, 2021). Health behavior is defined as "any activity undertaken by a person believing himself to be healthy, for the purpose of preventing disease or detecting it in an asymptomatic stage" (Kasl & Cobb, 1966, p. 246). The public health literature applies various theories and models for explaining individuals' choices for taking-up preventive health behaviors (Armitage & Conner, 2000; Hayden, 2022). Some of these models and theories are general behavior-related decision-making theories that were adopted by health behavior researchers, such as the Social Cognitive Theory (SCT; Bandura, 1986), the Theory of Reasoned Action (TRA; Ajzen & Fishbein, 1980; Fishbein & Ajzen, 1975), its extension as the Theory of Planned Behavior (TPB; Ajzen, 1985), and The Protection Motivation Theory (PMT; Rogers, 1975). Other commonly used theoretical strands in health behavior literature were specifically developed for predicting health-behavior-related decision-making processes, mainly in regard to adherence with a medical professional's advice or taking up a healthy lifestyle (Champion & Skinner, 2008; Weston et al., 2020), such as the PRECEDE-PROCEED Model (PPM; Green, 1974), the Common-Sense Model of self-regulation (CSM; Leventhal et al., 1980) and the Transtheoretical Model of behavior change (TM; Prochaska & DiClemente, 1982).
The conceptual prism of these models is similar to a large extent. Though some of them consider emotions as an important component of individual‐level decision processes for health behavior (e,g,. CSM; Hayden, 2022; Magnan et al., 2017), most of these theoretical strands are cognitively based and associate a decision to engage in a health behavior with one's perceptions and appraisals of the behavior and its outcomes (e.g., SCT, TRA, TPB, PMT). Specifically, they attribute human behavior to a cognitive process, which includes an inherent phase of assessing the pros and cons of the behavior (or of not behaving in the recommended manner) and its outcomes led by the "economic" motivation to maximize one's benefits and reduce one's costs (Montoya et al., 2000; Simons-Morton et al., 2012). These costs and benefits are not only material or physical of various types, such as emotional and moral (Bobek et al., 2007; Simons-Morton et al., 2012; Sun, 2020). The appraisal of the costs and benefits is not purely logical and may be affected by various psychological biases (Kahneman & Tversky, 1972), but this appraisal is a pivotal stage in the decision-making process.
The most popular and robust model for predicting health behavior is the HBM (Janz & Becker, 1984; Mesch & Schwirian, 2015; Rosenstock, 1974; Shmueli, 2021; Weston et al., 2020). The HBM too builds upon the cognitive and utilitarian prism and was originally developed for the US public health service in order to explain citizens' uptake of public health services, such as screening tests (Davis et al., 2013; Janz & Becker, 1984). Considering the dominance of this model in the health behavior literature and the fact that it was specifically developed for predicting health behavior within a public service environment, we find it to be the most suitable model for the context of compliance with governmentally instructed health behaviors. The next paragraphs will describe the HBM and theoretical grounds for the suggested MTM and its hypotheses.
The HBM posits that individuals will adopt health behaviors when they perceive them to be doable and when their benefits for dealing with the perceived threats posed by the health condition outweigh their costs. The model is composed of six concepts: (1) Perceived benefits—beliefs in the efficacy of the suggested health behavior in reducing one's risk to experience the disease or the condition, or reducing its impact; (2) Perceived barriers—beliefs in the potential costs and disadvantages of the suggested behavior (e.g., pain, discomfort, expenses, stress, time); (3) Perceived severity and (4) Perceived susceptibility that refer to the seriousness of the disease or the health condition's implications and beliefs regarding the chances of being inflicted by it. These two concepts are often referred to as a single construct representing risk or threat perceptions (e.g., Bish et al., 2011; Zampetakis & Melas, 2021); (5) Self-efficacy—the belief in one's ability to perform the behavior; and (6) Cues to action—strategies and triggers for creating awareness for the advantages of behavior and the need to perform it (such as information provided by the media or a conversation with friends or a physician). The HBM postulates that while higher perceived benefits, self-efficacy, severity and susceptibility, and stronger cues to action increase the chances of a person to perform the suggested behavior, higher perceived barriers will decrease these chances (see Fig. 1).
Much empirical evidence supports the HBM and its principals in the context of civic compliance with governmentally issued guidelines. However, these studies do not consider political trust as a factor that may antecede the HBM components (e.g., Clark et al., 2020; Goren et al., 2021; Matute et al., 2021; Paredes et al., 2021). Nonetheless, as the following paragraphs demonstrate, there is a strong theoretical background to suggest that political trust may be related to at least some of the HBM components, which in turn, determine compliance.
Factors explaining the trust–health behavior compliance relationship
As described above, health behavior theory stresses the effect of one's cognitive appraisals, i.e., beliefs and perceptions regarding the promoted behavior, as a predominant determinant of the adoption of a health behavior (Green, 1974; Hayden, 2022; Irwig et al., 2008; Janz & Becker, 1984; Prochaska & DiClemente, 1982; Rosenstock, 1974). Such perceptions seem to be particularly relevant for health behavior compliance, and not to other types of behavior in the context of compliance with state authorities (Fine & van Rooij, 2021; Levi, 1988; Murphy, 2004; Scholz & Lubell, 1998; Thomassen et al., 2017; Tyler, 1990). Persuasion theory provides a plausible explanation for the potential effect of political trust on such appraisals. Persuasion, in its broader sense, shares some significant similarities with the concept of civic compliance, as it is defined as a change in one's attitudes or behaviors following the instruction of another (O’Keefe, 2004). In the context of this study, the government which issues and promotes the health guidelines is the persuader and the members of the public, which are expected to comply with them, are the persuadees.
Persuasion theory emphasizes the significance of one's perceptions regarding the conveyer or the source of information advocating for the adoption of a specific behavior for determining the likelihood of one's compliance (M. D. Miller & Levine, 2019). The perceived trustworthiness of the source of information is a key element in the recipient's appraisal and determinant of the latter's acceptance of the information and consequent change of attitudes and behavior (e.g., Chaiken, 1980; O’Keefe, 2015; Petty & Cacioppo, 1986; Wallace et al., 2020). Trustworthiness is ones' assessment regarding the likelihood of another person to do what the former trusts him/her to do (Hardin, 2002). Therefore, the trustworthiness of a source of information is a fundamental antecedent for the generation of trust and predicts the level of trust we place on it (Hardin, 2002; Mayer et al., 1995). In other words, if a person trusts someone or something, it is because he/she finds them trustworthy. Given the interdependence between these two concepts, and inspired by previous work (e.g., Somera et al., 2016), we relate to the trustworthiness of the source of information and the trust in it as synonymous.
Dual-process models of persuasion, such as the Elaboration Likelihood Model (ELM; Petty & Cacioppo, 1986) and the Heuristic-Systematic Processing Model (HSM; Chaiken, 1980), posit that trust in a source of information is a cognitive shortcut, a "peripheral" characteristic of the persuasive situation or a decision heuristic, that may facilitate persuasion mainly under low motivation and/or low processing ability conditions (Wallace et al., 2020). That is, when the target of the persuasion is not motivated to process the conveyed information, due to lack of interest (relevance) or because he/she is unable to process it, due to lack of knowledge or time (ability), perceptions regarding the qualities of the source of information, trustworthiness being such, may impact the target's primary cognition, and determine its persuasion and attitudes toward the message (Champion & Skinner, 2008; Petty & Cacioppo, 1986). Nonetheless, trust in the source of information affects one' attitudes and perceptions also when the recipient is highly motivated and able to process the information, though to a lesser extent (Petty & Cacioppo, 1986). Simply put, according to persuasion theory, when a trusted persuader promotes a specific action or subject, we are likely to appraise this behavior in a more favorable manner than when promoted by a less trusted source. Indeed, evidence supports the effect of trust and trusted sources of information in determining audiences attitudes and cognitive appraisals in various situations that are not related to compliance with government instructions (Chetioui et al., 2021; P. Liu et al., 2019; Thaker et al., 2017; Visschers et al., 2011).
Considering the above-mentioned notions of persuasion theory and the evidence regarding trust's effect on cognitive appraisals, we hypothesize that trust in government will affect some of the HBM components that reflect one's cognitive-appraisal of the advocated behavior, i.e., perceptions regarding the benefits and costs of governmentally promoted health behaviors. For example, when the government promotes vaccine uptake, one's high levels of trust in the government may "pink-color" the government's message and enhance the way the person perceives the protective benefits of vaccination. Simultaneously, they may reduce the salience of prospected side-effects or inconvenience that may be caused by getting the shot. Specifically, we predict that (H1) trust in government will be positively related with the perceived benefits of governmentally promoted health behaviors and that (H2) trust in government will be negatively related with the perceived barriers of governmentally promoted health behaviors.
Furthermore, cognitive appraisals regarding a behavior do not relate solely to the pros and cons of the behavior, but also to one's assessment of his/her ability to perform it (Tam et al., 2021). Hence, trust in the source of information that promotes desired health actions may also affect one's perceptions of efficacy to carry out these actions. This effect may be highlighted particularly in a stressful situation, such as a public health threat, in which health guidelines are instructed. A threatening situation may cause an increase in one's level of anxiety, which may undermine perceptions regarding self-efficacy to perform a protective behavior (Bandura, 1997). Nonetheless, people are likely to feel less anxious if a trusted authority provides the instructions regarding health behaviors (Hall et al., 2001; Y. Y. Lee & Lin, 2009). For example, given that the COVID-19 pandemic was found to increase anxiety among the general population (Vindegaard & Benros, 2020), this anxiety may hamper citizens perceptions of their capability to carry out preventive health behaviors, such as adhering to mask wearing or getting fully vaccinated. However, if a trusted figure instructs or recommends this behavior, it may be perceived as more doable. This notion is further strengthen given the bilateral and reciprocal nature of trust (Wang et al., 2020), which may lead one to feel that if a trusted figure issues instructions, the latter trusts one's ability to perform it. This, in turn, may boost one's appraisals and perceptions regarding their self-efficacy to do so. Hence, we predict that (H3) trust in government will be positively associated with one's perceptions regarding their self-efficacy to perfume the advised behavior.
It is important to note that although we build the MTM on the HBM, our model does not include all of the HBM's conceptual factors. Specifically, despite some studies reporting a significant association between trust in government and risk perceptions (e.g., Schneider et al., 2021; Xu, 2021), we do not predict that the political trust-compliance association will be mediated by risk perceptions. This is since, risk perception literature suggests that one's assessment of risk, particularly in health contexts, is determined by a wide range of references, which develop over a lifetime (Brown, 2014). For example, risk perception has been shown to be shaped by multiple social and cultural factors (Kwok et al., 2020; Malecki et al., 2021). More specifically, research indicates that social identity and its consequential "cultural cognition," that is the matching of one's opinions to those in the social groups they relate with, plays a leading part in shaping risk perceptions (Brown, 2014; Cruwys et al., 2020). This assumption is also supported in Dryhurst et al.'s (2020) recent mid-COVID multinational study, which indicated that risk perception was associated with trust in government in only 2 out of 10 examined countries.
The suggested MTM is based upon the combination of the presented above hypotheses and the basic postulations of the HBM. More specifically, we hypothesize that the mechanism explaining the trust–health behavior compliance relationship relies upon cognitive appraisals which are the main concepts of the HBM, while persuasion theory provides the rational for the association between political trust and these concepts. In other words, we predict that trust in government will affect perceptions regarding the advised health behavior's benefits, costs, and individuals' ability to perform them, but not their risk perceptions regarding the threat/hazard. These will consequently affect individuals' compliance intentions with the guidelines, in accordance with the HBM. Hence, we hypothesized that:
H4: Perceptions regarding the benefits of the advocated health behavior will mediate the relationship between trust in government and compliance intentions.
H5: Perceptions regarding the barriers for performing the advocated health behavior will mediate the relationship between trust in government and compliance intentions.
H6: Perceptions regarding one's self-efficacy to perform the advocated health behavior will mediate the relationship between trust in government and compliance intentions.
Method
Given procedural similarities between the studies which will be described in the procedure and measures sections, this section will be presented jointly for all four studies. However, considering the variance in their applied measures, their results will be reported separately. Following the approval of the ethics committee of the Social Sciences faculty of the University of Haifa (#112/20 and #292/20), using 5 local panel survey companies, we performed four studies: two on-line surveys and two on-line survey-experiments with a total of 3732 Israeli adult participants, during April 2020 (Study 1; N = 1005), October 2020 (Study 2; N = 614), December 2020 (Study 3; N = 1184) and November 2021 (Study 4; N = 929), which encompass a total of 20 months into the COVID-19 pandemic.
Though our hypothesized model was not specifically designed to address a crisis situation, a public health crisis, such as the COVID-19 pandemic, is a scenario in which health-behavior-related instructions are likely to be issued (Kotz Crego & Kontanidis, 2020; Pak et al., 2021), making it a natural environment for our examination. In order to control, to some extent, for the potential impact of the crisis environment, our studies were spread across 4 points in time, which represent different levels of the pandemic severity based on the number of severely ill individuals at the onset of each study, as published by the Israeli Ministry of health1 (see Fig. 2).
Fig. 2.
Dates of data collection onset of our studies and numbers of severely ill patients in Israel, Data: the Israeli Ministry of health's web site
Sample
All the studies included samples of the three main social groups in Israel (Goren et al., 2021): the general Jewish majority, the Arab community and the Ultra-Orthodox community. Each sub-sample was aimed to be stratified by age and gender. However, considering the known difficulty in sampling minority groups in Israel and particularly recruiting members of the Ultra-Orthodox community for internet-based surveys (Gordoni & Schmidt, 2010; Kalagy, 2020), representative samples in these groups were not fully achieved in all the surveys (see descriptive demographic features of the samples in Table 1). Nonetheless, we believe that the obtained samples fairly represent the adult Israeli population, and our analysis considers and controls for variables that may impact the extent to which the sample is representative.
Table 1.
Means and standard deviations of the demographic variables by social group in the four studies
| General | Arab | Ultra-Orthodox | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Std | N | Mean | Std | N | Mean | Std | ||
| Study 1 | Gender1 | 321 | .57 | .496 | 361 | .39 | .489 | 323 | .48 | .500 |
| Age2 | 321 | 43.56 | 16.619 | 361 | 35.24 | 10.974 | 323 | 28.40 | 7.157 | |
| Education3 | 321 | 1.59 | .493 | 353 | 1.67 | .472 | 323 | 1.50 | .501 | |
| Children4 | 321 | 1.78 | 1.724 | 361 | 1.50 | 1.446 | 323 | 2.17 | 2.418 | |
| Income5 | 283 | 2.4594 | 1.21498 | 344 | 1.8895 | 1.08233 | 283 | 1.9011 | 1.03353 | |
| Study 2 | Gender | 218 | .53 | .500 | 202 | .52 | .501 | 194 | .51 | .501 |
| Age | 218 | 46.83 | 18.831 | 202 | 32.83 | 14.504 | 194 | 35.81 | 15.044 | |
| Education6 | 218 | 3.33 | 1.580 | 202 | 3.96 | 1.225 | 194 | 3.57 | 1.478 | |
| Parenthood7 | 218 | .59 | .493 | 202 | .29 | .456 | 194 | .58 | .495 | |
| Income | 213 | 2.62 | 1.332 | 200 | 1.68 | 1.042 | 194 | 2.11 | 1.206 | |
| Study 3 | Gender | 617 | .51 | .500 | 265 | .30 | .460 | 302 | .49 | .501 |
| Age | 617 | 39.57 | 14.544 | 265 | 34.55 | 12.242 | 302 | 34.90 | 12.339 | |
| Education6 | 617 | 4.08 | 1.304 | 263 | 4.10 | 1.371 | 301 | 4.13 | 1.281 | |
| Parenthood | 580 | .42 | .494 | 255 | .44 | .498 | 288 | .69 | .464 | |
| Income | 550 | 2.81 | 1.254 | 221 | 1.86 | 1.057 | 260 | 1.95 | 1.124 | |
| Study 4 | Gender | 755 | .49 | .500 | 107 | .42 | .496 | 55 | .44 | .501 |
| Age | 757 | 40.46 | 14.255 | 108 | 35.63 | 11.897 | 55 | 33.27 | 12.409 | |
| Education6 | 753 | 4.11 | 1.330 | 104 | 4.27 | 1.192 | 54 | 3.56 | 1.341 | |
| Parenthood | 751 | .41 | .492 | 104 | .48 | .502 | 54 | .70 | .461 | |
| Income5 | 681 | 2.54 | 1.138 | 103 | 1.75 | 1.064 | 50 | 1.74 | .853 | |
1Gender: 1 = male, 0 = female; 2Age by years; 31—less than an academic degree, 2—academic degree and above; 4the number of children; 5Income level: relative to average household income: ranging from 1 = "much lower" to 5 = "much higher"; 6Education was measured on a 6-point scale ranging from elementary school = 1 to a masters' degree and beyond = 6; 7Parenthood: 1 = "has children," 0 = "does not have children"
Procedure
Following an informed consent, participants were presented with simulated newly governmentally issued health instructions (one per participant). Each study presented different instruction/s: Study 1: A daily body temperature screening and a report to the Ministry of Health if it exceeded 38°C (100.4°F)2; Studies 2 and 3 were of an experimental nature and included two instructions that were randomly presented to the participants: (1) a mandatory use of an eye protector in addition to a face mask in public places; OR (2) a stay-at-home instruction during a week-long general lockdown that will begin in three days; Study 4: a periodical vaccination against COVID-19 every 6 months. This variance in instructions is relevant also for other studies that are reported elsewhere. After the instruction was introduced, participants were asked to report their intentions to comply with it. We chose to explore compliance intentions with simulated instructions and not self-reported actual behavior for two main reasons. First, we wanted to examine acceptance of new health directives. Second, we wanted to avoid social desirability effects, which are particularly strong when participants are asked to state whether they comply with existing normative laws and rules (Bradburn et al., 1978; Gonzalez-Ocantos et al., 2012). In addition, we measured other psychological and political variables, including trust in government, and concluded the surveys with a battery of demographic questions and a debriefing that stressed the presented instruction was bogus.
Measures
Dependent variable
In all the experiments, the Compliance intentions were measured using the protocol for measuring behavioral intentions in a medical context (Francis et al., 2004), which is composed of three five-point items, each presenting a different verb regarding intentions. For example, in study 4 the three items were "I expect/ want/ intend to get vaccinated against COVID-19 every six months"; (1 = "strongly disagree" to 5 = "strongly agree"). An average score of the three items was calculated following an inner reliability check (α > 0.9 in all studies) and constituted our intention to comply variable.
Independent and control variables
Given variances in the measured variables and the measurement tools applied in each study, and due to space limitations, this section will only list the measures used in each study. For their full description, see appendix A.
Study 1: Trust in government; Perceived benefits of the instructed behavior; Risk perception; Technical ability to comply; Stress; Knowledge about the disease; Demographics.
Study 2: Trust in government; Perceived benefits and barriers (psychological, physical and logistic ones) of the instructed behavior; Risk perception; Self-efficacy to comply; Knowledge about the disease and Demographics. The type of instruction (eye protector/lockdown) was controlled for as well.
Study 3: Trust in government; Perceived benefits and barriers (psychological, physical and logistic ones) of the instructed behavior; Risk perception; Self-efficacy to comply; Social norms and Demographics. The type of instruction (eye protector/ lockdown) was controlled for as well.
Study 4: Trust in government; Perceived benefits and barriers (psychological, physical, logistic and safety ones) of the instructed behavior; Risk perception; Self-efficacy to perform the instruction; Perceived social norms of adopting the instructed behavior; Previous vaccination against COVID-19 and Demographics.
Statistical analysis
Considering the variance in applied measures in our studies, we analyzed each study separately. First, we performed descriptive analyses. Next, in studies 2 and 3 we conducted a T-test, of compliance intentions between the experimental groups. Then, in each of the studies, we performed a parallel mediation analysis using PROCESS macro for SPSS (Hayes, 2017), where the dependent variable was compliance intentions, the independent variable was trust in government, and the mediating variables were the main factors of the HBM. All models also included control variables: stress (in study 1), knowledge about the disease (in studies 1 and 2), type of instruction (in studies 2 and 3), social norms in regard to abiding with the presented health instruction (in studies 3 and 4), past vaccination against COVID-19 (in study 4) and demographic variables (in all studies). Finally, in order to show the fit of the data to our proposed model, we conducted a series of post hoc "reversed" mediation tests in all four studies, in which trust in government was the mediator and the hypothesized mediators were the independent variables, to rule out alternative models.
Results
A general overview of compliance intentions scores in all four studies
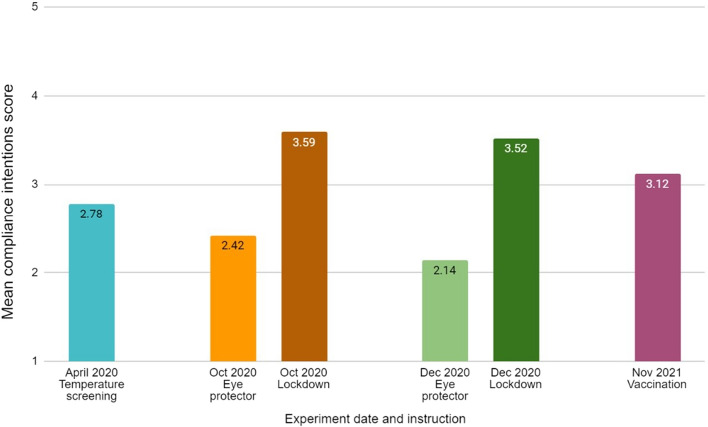
In all four studies, the mean compliance intentions scores were medium, ranging from 2.14 to 3.59 (on a 1–5 scale; see Fig. 3). The highest scores were observed during studies 2 and 3, and they relate to the lockdown instruction. An independent samples T-test in each of these studies indicated that the compliance intentions scores with the lockdown instruction were significantly higher than those of the eye-protector instruction (study 2: t(612) = 9.602, p < 0.001; study 3: t(1,182) = 19.187, p < 0.001). While we cannot statistically determine that the Israeli population will more likely comply with one instruction over the other, these results do indicate a stable medium-level willingness to comply with various newly introduced health instructions, even in varying levels of a public health crisis.
Fig. 3.
Mean compliance intentions scores by survey and instruction
Mediators of the trust and compliance intentions relationship
Study 1
In study 1, the mediators were the perceived benefits of the instruction, and the perceived risk posed by the disease. As Table 2 and Fig. 4 show, there was no direct effect of trust in government on compliance intentions. However, trust in government was positively associated with both perceived benefits and perceived risk, which were also positively associated with compliance intentions, making trust's indirect effect on compliance intentions through these variables significant (benefits: b = 0.0044, CI[0.002,0.0068]; risk: b = 0.0006; CI[0.001,0.0012]. Hence, H1 and H4, which regard the role of the perceived benefits, were supported in this study, but our postulation regarding the lack of association between trust and risk perception was not confirmed. As this study's simulated instruction was to take one's temperature and report it only if it exceeded 38°C (100.4°F), we assumed self-efficacy to comply with the simulated instruction would not vary and that there would not be perceived barriers to conduct behavior. Thus, H2, H3, H5 and H6 were not examined in this study.
Table 2.
Results of a parallel mediation analysis of perceived benefits and risk perception in study 1
| Path | Effect | SE | 95% LCI | 95%UCI |
|---|---|---|---|---|
| Total effect | ||||
| Trust ➞ Comp. intentions | .007*** | .0021 | .0029 | .0111 |
| Direct effect | ||||
| Trust ➞ Comp. intentions | .0021 | .0017 | -.0013 | .0055 |
| Trust ➞ Benefits | .0072*** | .0019 | .0035 | .0109 |
| Trust ➞ Risk perception | .0028* | .0012 | .0004 | .0053 |
| Benefits ➞ Comp. intentions | .611*** | .0516 | .545 | .677 |
| Risk perception➞ Comp. intentions | .1995*** | .0516 | .0983 | .3008 |
| Specific indirect effect | ||||
| Trust ➞ Benefits ➞ Comp. intentions | .0044* | .0013 | .002 | .0068 |
| Trust ➞ Risk perception ➞ Comp. intentions | .0006* | .0003 | 0.001 | .0012 |
N = 736; *p < 0.05; **p < 0.01; ***p < 0.001; Trust = trust in government; Covariates in the model: Gender, Age, Number of children, Education, Income, Sector (Ultra-Orthodox/ Arab/ General Jewish), Political ideology, Having a thermometer at home, knowledge about COVID, Stress
Fig. 4.

An empirical model of the indirect effects in study 1, *p < 0.05; **p < 0.01; ***p < 0.001
Study 2
In study 2, we examined the mediation effect of all of the HBM factors, i.e., the perceived benefits, perceived risk, self-efficacy to comply with the instruction and three types of perceived barriers for complying with the promoted behavior: physical, psychological and logistic, which are commonly measured in similar studies, in crisis and routine times (e.g., Champion, 1984; Sung et al., 2008; Trent et al., 2021a, 2021b). As indicated in Table 3 and Fig. 5, similar to study 1, there was no direct effect of trust in government on compliance intentions. However, trust in government was positively associated with perceived benefits, and self-efficacy and negatively associated with physical barriers. Hence, supporting H1-3. Moreover, trust was indirectly associated with compliance intentions, and therefore, supporting H4-6 (through perceived benefits (b = 0.002, CI[0.0009,0.0031]), self-efficacy (b = 0.0055, CI[0.0027,0.0084]) and physical barriers (b = 0.0004, CI[0.0001,0.0010])). Interestingly, trust was not associated with psychological and logistic barriers, which were also unrelated to compliance intentions. In addition, in this study as well, trust was significantly associated with risk perceptions, therefore contradicting our postulation regarding the lack of this association.
Table 3.
Results of a parallel mediation analysis of perceived benefits, risk perception, barriers and self-efficacy in study 2
| Path | Effect | SE | 95% LCI | 95% UCI |
|---|---|---|---|---|
| Total effect | ||||
| Trust ➞ Comp. intentions | .0088*** | .0021 | .0046 | .0129 |
| Direct effect | ||||
| Trust ➞ Comp. intentions | .001 | .0012 | −.0014 | .0033 |
| Trust ➞ Benefits | .0088*** | .0022 | .0045 | .0131 |
| Trust ➞ Risk perception | .0027* | .0014 | .0001 | .0054 |
| Trust ➞ Self-efficacy | .0091*** | .0023 | .0045 | .0136 |
| Trust ➞ Physical barriers | −.012** | .0046 | −.0121 | −.0029 |
| Trust ➞ Psychological barriers | −.0064 | .0053 | −.0168 | .004 |
| Trust ➞ Logistic barriers | −.0038 | .0053 | −.0143 | .0067 |
| Benefits ➞ Comp. intentions | .2229*** | .0277 | .1685 | .2774 |
| Risk perception ➞ Comp. intentions | −.0059 | .0363 | −.0773 | .0655 |
| Self-efficacy ➞ Comp. intentions | .6033*** | .0269 | .5504 | .6561 |
| Physical barriers ➞ Comp. intentions | −.0335** | .0124 | −.0579 | −.009 |
| Psychological barriers ➞ Comp. intentions | .0122 | .011 | −.0094 | .0338 |
| Logistic barriers ➞ Comp. intentions | −.016 | .0099 | −.0354 | .0034 |
| Specific indirect effect | ||||
| Trust ➞ Benefits ➞ Comp. intentions | .002* | .0006 | .0009 | .0031 |
| Trust ➞ Risk perception ➞ Comp. intentions | 0 | .0001 | −.0003 | .0002 |
| Trust ➞ Self-efficacy ➞ Comp. intentions | .0055* | .0015 | .0027 | .0084 |
| Trust ➞ Physical barriers ➞ Comp. intentions | .0004* | .0002 | .0001 | .001 |
| Trust ➞ Psychological barriers ➞ Comp. intentions | −.0001 | .0001 | −.0004 | .0001 |
| Trust ➞ Logistic barriers ➞ Comp. intentions | .0001 | .0001 | −.0001 | .0003 |
N = 571; *p < 0.05; **p < 0.01; ***p < 0.001; Trust = trust in government; Covariates in the model: Gender, Age, parenthood, Education, Income, Sector (Ultra-Orthodox/ Arab/ General Jewish), instruction type, knowledge about COVID; Note: we did not include stress and political ideology in this model as we did in study 1, due to their insignificant effect on compliance intentions. Knowledge was also insignificant but included in the analysis due to its prominent role in some behavioral theories
Fig. 5.

An empirical model of the indirect effects in study 2, *p < 0.05; **p < 0.01; ***p < 0.001
Study 3
In study 3, we examined the mediating effects of the same variables (and the same barriers) as in study 2, this time during a lower level of crisis severity (based on number of severely ill patients in the country). In this case too, trust in government was not directly associated with compliance intentions. Of the HBM factors, trust was positively associated with perceived benefits, and negatively associated with physical and psychological barriers. However, trust was not associated with self-efficacy (hence, supporting H1 and H2 and rejecting H3 and A6). Aside from psychological barriers, these variables had similar associations with compliance intentions. The effect of trust in government on compliance intentions was mediated by perceived benefits (b = 0.0018, CI[0.0007,0.0029] and physical barriers (b = 0.0003, CI[0.0001,0.0008]) and consequently supporting H4 and H5 (for physical barriers only), and supporting our postulation regarding the lack of association between trust and risk perception (See Table 4 and Fig. 6). It is interesting to note that psychological barriers were not associated with compliance intentions, however, perceptions of risk and self-efficacy were.
Table 4.
Results of a parallel mediation analysis of perceived benefits, risk perception, barriers and self-efficacy in study 3
| Path | Effect | SE | 95% LCI | 95% UCI |
|---|---|---|---|---|
| Total effect | ||||
| Trust ➞ Comp. intentions | .0039** | .0013 | .0013 | .0065 |
| Direct effect | ||||
| Trust ➞ Comp. intentions | .0016 | .0012 | −.0007 | .0038 |
| Trust ➞ Benefits | .0045** | .0015 | .0016 | .0074 |
| Trust ➞ Risk perception | .0008 | .0011 | −.0014 | .003 |
| Trust ➞ Self-efficacy | .0012 | .0012 | −.0011 | .0034 |
| Trust ➞ Physical barriers | −.0109** | .0039 | −.0186 | −.0031 |
| Trust ➞ Psychological barriers | −.0092* | .0043 | −.0176 | −.0008 |
| Trust ➞ Logistic barriers | −.0014 | .0044 | −.01 | .0072 |
| Benefits ➞ Comp. intentions | .389*** | .0258 | .3387 | .4401 |
| Risk perception ➞ Comp. intentions | .0683* | .0338 | .0019 | .1346 |
| Self-efficacy ➞ Comp. intentions | .1035** | .0322 | .0404 | .1667 |
| Physical barriers ➞ Comp. intentions | −.0313** | .0112 | −.0532 | −.0093 |
| Psychological barriers ➞ Comp. intentions | .0016 | .0106 | −.0192 | .0223 |
| Logistic barriers ➞ Comp. intentions | −.0287*** | .0086 | −.0456 | −.0119 |
| Specific indirect effect | ||||
| Trust ➞ Benefits ➞ Comp. intentions | .0018* | .0006 | .0007 | .0029 |
| Trust ➞ Risk perception ➞ Comp. intentions | .0001 | .0001 | −.001 | .0003 |
| Trust ➞ Self-efficacy ➞ Comp. intentions | .0001 | .0001 | −.001 | .0004 |
| Trust ➞ Physical barriers ➞ Comp. intentions | .0003* | .0002 | 0.001 | .0008 |
| Trust ➞ Psychological barriers ➞ Comp. intentions | 0 | .0001 | −.0003 | .0002 |
| Trust ➞ Logistic barriers ➞ Comp. intentions | 0 | .0001 | −.0002 | .0003 |
N = 997; *p < 0.05; **p < 0.01; ***p < 0.001; Trust = trust in government; Covariates in the model: Gender, Age, parenthood, Education, Income, Sector (Ultra-Orthodox/ Arab/ General Jewish), instruction type, social norms regarding the instructed behavior; Note: although social norms (i.e., what people expect others to do) are a key factor in predicting compliance (Cialdini & Trost, 1998), they were not measured in studies 1 & 2. This is due to the slow-evolving nature of social norms regarding abidance with new laws and rules (Andrighetto et al., 2013; Cooter, 1998), which our studies simulate, and hence, cannot capture authentic social norms regarding our simulated instructions. However, as the pandemic and our research continued, new evidence regarding the agility of social norms during the COVID-19 pandemic emerged (e.g., Casoria et al., 2021), and we decided to add this measure to the questionnaire and to the analysis of studies 3 & 4 (See appendix A).; We did not include knowledge about COVID-19 in this model as we did in study 1 & 2, due to its insignificant effect on compliance intentions in both of them and given the long duration of the pandemic, which we assumed contributed to high and non-variant levels of knowledge on the matter
Fig. 6.

An empirical model of the indirect effects in study 3, *p < 0.05; **p < 0.01; ***p < 0.001
Study 4
In study 4, we measured 4 types of barriers (physical, psychological, logistic and additional safety barriers, which are particularly relevant and common for vaccination (Paredes et al., 2021)) and the perceived risk posed by the disease was measured by the two basic concepts of perceived severity (of the disease) and susceptibility (to contract it). Aside from these variables, the mediation model included the other two factors of the HBM: perceived benefits and self-efficacy to comply. As Table 5 and Fig. 7 show, unlike the previous studies, the association between trust in government and compliance intentions was direct and significant (b = 0.0027, SE = 0.0013, p < 0.05). Trust was also associated (in the expected direction) with all the HBM factors except for the two variables representing risk/threat perceptions. Hence, our preliminary postulation and H1-3 were supported. These factors were similarly associated with compliance intentions (in the barriers factor, only safety barriers demonstrated a significant correlation). Consequently, the effect of trust on compliance intentions was significant and indirect through perceived benefits (b = 0.0029, CI[0.0016,0.0043]), safety barriers (b = 0.0029, CI[0.0016,0.0044]) and self-efficacy (b = 0.0007, CI[0.0001,0.0014]). Therefore, H4-6 were supported. A post hoc analysis indicated that the mediation effects of benefits and the safety barriers explain the same variance in the model. This suggests that the perceived benefits and safety (risks) of the behavior examined in this study counter-weigh each other in their effect on the intention to adopt the promoted behavior (a periodical vaccination against COVID-19).
Table 5.
Results of a parallel mediation analysis of perceived benefits, risk perception, barriers and self-efficacy in study 4
| Path | Effect | SE | 95% LCI | 95% UCI |
|---|---|---|---|---|
| Total effect | ||||
| Trust ➞ Comp. intentions | .0098*** | .0017 | .0065 | .0131 |
| Direct effect | ||||
| Trust ➞ Comp. intentions | .0027* | .0013 | .0002 | .0052 |
| Trust ➞ Benefits | .0078*** | .0016 | .0047 | .0109 |
| Trust ➞ Severity | .0004 | .0014 | −.0023 | .0031 |
| Trust ➞ Susceptibility | .0023 | .0013 | −.0003 | .005 |
| Trust ➞ Self-efficacy | .0059*** | .0015 | .003 | .0087 |
| Trust ➞ Safety barriers | −.0081*** | .0016 | −.0112 | −.0051 |
| Trust ➞ Physical barriers | −.0018*** | .0018 | −.0117 | −.0045 |
| Trust ➞ Psychological barriers | −.0053*** | .0015 | −.0083 | −.0023 |
| Trust ➞ Logistic barriers | −.0028* | .0014 | −.0055 | −.0001 |
| Benefits ➞ Comp. intentions | .3725*** | .0333 | .3072 | .4379 |
| Severity ➞ Comp. intentions | .053 | .039 | −.0236 | .1295 |
| Susceptibility ➞ Comp. intentions | .05 | .04 | −.0286 | .1286 |
| Self-efficacy ➞ Comp. intentions | .1124** | .0401 | .0336 | .1912 |
| Safety barriers ➞ Comp. intentions | −.3626*** | .037 | −.4351 | −.29 |
| Physical barriers ➞ Comp. intentions | −.0077 | .0317 | −.07 | .0545 |
| Psychological barriers ➞ Comp. intentions | −.059 | .0393 | −.1361 | .0181 |
| Logistic barriers ➞ Comp. intentions | −.0161 | .0378 | −.0904 | .0582 |
| Specific indirect effect | ||||
| Trust ➞ Benefits ➞ Comp. intentions | .0029* | .0007 | 0016 | .0043 |
| Trust ➞ Severity ➞ Comp. intentions | 0 | .0001 | −.0002 | .0003 |
| Trust ➞ Susceptibility ➞ Comp. intentions | .0001 | .0001 | −.0001 | .0004 |
| Trust ➞ Self-efficacy ➞ Comp. intentions | .0007* | .0003 | .0001 | .0014 |
| Trust ➞ Safety barriers ➞ Comp. intentions | .0029* | .0007 | .0016 | .0044 |
| Trust ➞ Physical barriers ➞ Comp. intentions | .0001 | .0003 | −.0005 | .0006 |
| Trust ➞ Psychological barriers ➞ Comp. intentions | .0003 | .0003 | −.0001 | .0009 |
| Trust ➞ Logistic barriers ➞ Comp. intentions | 0 | .0001 | −.0002 | .0003 |
N = 802; *p < 0.05; **p < 0.01; ***p < 0.001; Trust = trust in government; Covariates in the model: Gender, Age, Parenthood, Education, Income, Sector (Ultra-Orthodox/ Arab/ General Jewish), Political ideology, Social norms regarding the instructed behavior, Past vaccination against COVID-19. Note: Past vaccination was included in the analysis due to its relevance for general acceptance of the COVID-19 vaccine. Political ideology was included in the analysis given previous studies suggesting a close association between vaccine acceptance and political ideology
Fig. 7.

An empirical model of the indirect effects in study 4, *p < 0.05; **p < 0.01; ***p < 0.001
Summary of results from all four studies
Table 6 summarizes our hypotheses examination results in all 4 studies. It shows that perceived benefits and barriers of the behavior were associated with trust in government and mediated the latter's association with compliance intentions in all the studies. However, self-efficacy mediated this relationship only in studies 2 and 4 (two out of the three studies in which it was measured).
Table 6.
Hypotheses support/rejection in four experiments
| Hypothesis | Path description | S1 | S2 | S3 | S4 |
|---|---|---|---|---|---|
| H1 | Trust ➞ Perceived benefits | V | V | V | V |
| H2 | Trust ➞ Perceived barriers | – | V | V | V |
| H3 | Trust ➞ Perceived self-efficacy | – | V | X | V |
| H4 | Trust ➞ Perceived benefits ➞ Comp. intentions | V | V | V | V |
| H5 | Trust ➞ Perceived barriers ➞ Comp. intentions | – | V | V | V |
| H6 | Trust ➞ Perceived self-efficacy ➞ Comp. intentions | – | V | X | V |
S = study; V = significant effect; X = insignificant effect; '–' = the factor was not measured
Discussion
Our findings reveal several important insights. First, as indicated from the mean score of compliance intentions in all the studies, it seems that citizens are willing to comply with various health instructions, that are newly issued by the government to a stable medium extent, regardless of the duration or the severity of the public health crisis they face (i.e., the COVID-19 pandemic). This seems not to be aligned with previous findings regarding "pandemic fatigue," which attests to a decrease in compliance levels as the crisis perseveres (e.g., Yadete et al., 2021). However, these previous studies refer mostly to long-term adherence with "old" guidelines that were issued in the past, while our studies focused on the willingness to adopt newly instructed behaviors. Though this may not necessarily predict long-term adherence with new guidelines, our findings indicate a persistent and long-lasting public willingness and openness toward new policies and measures, even in long-term crises.
Second, our analysis shows that the direct association between trust in government and compliance intentions with health instructions is unstable. In fact, in three out of the four studies, the direct trust-compliance intentions association was not significant. While this may contradict a large body of empirical evidence (e.g., Blair et al., 2017; Trent et al., 2021a, 2021b), our findings are not the first to report the absence or a weakening of this direct relationship, particularly during the Covid-19 pandemic (Clark et al., 2020; Goren et al., 2021; Pak et al., 2021; Prati et al., 2011; Travaglino & Moon, 2021). These somewhat unintuitive findings highlight the intricate relationship between the two concepts, at least in regards to health behavior. These inconsistencies can be explained by methodological differences, such as the type of trust that was measured (e.g., institutional, political or trust in the government's management of the crisis), the examined health behavior (e.g., mask wearing, social distancing, vaccination) and the type of compliance measured (e.g., reported, intended, with actual or simulated instructions). Additional explanation for these discrepancies could be the public health crisis context, during which these studies were conducted. The unprecedented global magnitude of the Covid-19 pandemic compared to other public health crises and routine times, and particularly the similarities in mitigating policies applied by different governments, during the pandemic. Simply put, it is possible that when citizens realize that due to a unique situation millions of people around the world are instructed by their governments to take similar measures as their own government advises them, their trust in their government may indirectly, and not directly, affect their decision to adopt these measures or not. Since certain preventive behaviors seem universally inevitable during such crises, trust in government may affect the way citizens interpret and appraise these behaviors, which consequently may shape their decision to adopt them and not directly affect their behavior. As will be further elaborated in the next paragraph, the fact that the indirect effect of trust on compliance intentions was significant even when trust was not directly related with compliance intentions (studies 1–3), indicates the innate role of trust in government in effecting compliance intentions.
Third, despite the absence of a consistent direct association between trust and compliance intentions, our findings show that trust was indirectly associated with compliance intentions through different perceived barriers, particularly physical and safety barriers, and through perceived self-efficacy to perform the advocated behavior (in 2 out of 3 of the studies that measured this factor). However, the most prominent factor through which trust in government affected compliance intentions in all the studies was the perceived benefits of the behavior. That is, the higher the levels of trust in government, the more beneficial the advocated health behavior was perceived to be, and this in turn led to stronger intentions to adopt it. Simply put, all four studies indicated that when citizens trust their government, they perceive its instructed behaviors to be more beneficial, less "costly" in terms of barriers and disadvantages and more doable, and therefore, are more lenient to comply with them. These results coincide with our hypotheses, which were derived from persuasion theory and supporting evidence regarding the tie between the trust in a source of information and cognitive appraisals and perceptions regarding the subject of the information (Chaiken, 1980; Chetioui et al., 2021; P. Liu et al., 2019; O’Keefe, 2015; Petty & Cacioppo, 1986; Thaker et al., 2017; Visschers et al., 2011; Wallace et al., 2020), as well as scholarship on the plausible effect of trust in a source of information and one's perceptions regarding their efficacy to perform the advocated behaviors (Bandura, 1997; Hall et al., 2001; Y. Y. Lee & Lin, 2009; Wang et al., 2020). These results also align with health behavior theory, and particularly with the HBM, as they indicate that cognitive appraisals of the advocated health behavior and its outcomes determine behavioral intentions (Ajzen, 1985; Ajzen & Fishbein, 1980; Bandura, 1986; Fishbein & Ajzen, 1975; Janz & Becker, 1984; Rogers, 1975; Rosenstock, 1974). Thus, our results support the MTM. Specifically, they reveal that cognitive appraisals regarding the pros and cons of instructed behaviors and one's ability to perform them mediate the effect of trust in government on one's willingness to comply with these instructions.
Importantly, our findings indicate that not all types of cognitive appraisal mediate the trust-compliance relationship. Specifically, as expected, risk perceptions do not mediate this effect, suggesting that such perceptions are less relevant for the trust-compliance relationship. Nonetheless, it should be noted that in the first study risk perceptions did mediate this relationship. Furthermore, contrary to our predictions, and to previous work that challenges the effect of political trust on cognitive appraisals of risk perceptions (Brown, 2014; Cruwys et al., 2020; Dryhurst et al., 2020), trust in government was associated with risk perceptions in the first and second studies. However, this may be explained by the timing in which these studies were conducted, as these surveys took place about a month and 7 months after the initial outbreak of the pandemic in Israel (while the other surveys took place later into the pandemic). This may suggest that as a situation in which health instructions are being issued prolongs (i.e., an ongoing public health crisis), the effect of trust in government on risk perceptions decreases. It is possible that at the initial stages of a large-scale public health crisis, citizens depend on their perceptions regarding their government in order to assess the risks posed by the crisis, due to its novelty and their unfamiliarity with its features. However, as the crisis continues and becomes "the new normal" routine (Michaels et al., 2022), it is possible that the anchors and references citizens use in order to make risk assessments change and are derived from various sources and factors that are known to affect health-related risk perceptions, such as one's cultural or social group (Brown, 2014; Cruwys et al., 2020), or other and competing sources of information—not necessarily formal and valid ones, including personal experience and acquaintance with the crisis (or the disease), international regulators, traditional and social media. These alternative references may crowd their perceptions regarding their government's trustworthiness out of their risk assessment system.
Fourth, the results of this study indicate that the HBM, in its classic form, may not be an optimal framework for predicting compliance with health guidelines, at least during an ongoing public health crisis. As our findings show, contrary to one of the core hypotheses of the HBM, risk perceptions were not associated with compliance intentions in all of our studies (see Table 7). Although these results contradict some recent evidence that support the risk perception-compliance relationship (e.g., Limbu et al., 2022; Shmueli, 2021), other studies demonstrate similar results to ours, such that this relationship is insignificant, partial or applies only to specific health behaviors but not to others (e.g., Al-Sabbagh et al., 2021; Coe et al., 2012; Tong et al., 2020; Wong et al., 2020). This may be explained by the fact that the HBM was originally developed for explaining voluntary health behaviors, such as screening tests, recommended by healthcare professionals, and not governmentally issued instructions (Davis et al., 2013; Janz & Becker, 1984). It is possible that risk perceptions are crucial for making health-related decisions regarding the worthwhileness of health measures when health instructions and recommendations come from medical professionals but not when health behaviors are instructed by the government or its official agencies.
Table 7.
The HBM factors and trust in government and their association with compliance intentions in the study
| Factor | Study1 | Study2 | Study3 | Study4 |
|---|---|---|---|---|
| Perceived Benefits | V | V | V | V |
| Perceived Barriers | – | V Physical | V Physical & Logistic | V Safety |
| Perceived Self-efficacy | – | V | V | V |
| Perceived Risk | V | X | V | X Neither severity nor susceptibility |
| Trust in government | X | X | X | V |
V = significant effect; X = insignificant effect; '–' = the factor was not measured
Furthermore, our findings indicate that not all types of barriers for adopting a health behavior indeed effect the intentions to do so. We suggest that this variance depends on the type of health instruction being advised. While physical and logistic barriers were negatively associated with compliance intentions with regards to the eye-protector and the lockdown instructions, they were not associated with compliance intentions regarding vaccination. The willingness to get vaccinated, on the other hand, was affected only by safety barriers. The latter finding matches previous studies that stress the dominance of safety considerations in vaccination decision making (e.g., Paredes et al., 2021). The effect of physical and logistic barriers on compliance intentions with behaviors of a more physical (eye-protector) or lifestyle change (stay-at-home) nature seems logical and intuitive.
Interestingly, psychological barriers, i.e., concerns that preforming the advocated behavior may induce feelings of stress, embarrassment and anxiety, were not associated with compliance intentions with neither of the examined behaviors and in neither of the studies. This may suggest that psychological barriers for health behaviors are less relevant when the behavioral instructions apply to the general population and not to a specific person or a risk group. For example, if mask wearing in public places is mandatory for all citizens, the effect of embarrassment on the decision to wear it is likely to be weak, since all the other citizens will be in a similar situation. Furthermore, previous studies that identified an effect of psychological barriers on adoption of health behaviors mostly referred to screening tests for sever diseases, such as cancer (Huang et al., 2021). In these cases, the psychological barriers referred to the concerns that the tests cause, while the patients anxiously wait for their results. Though this issue should be further explored, on the face of it, it seems that psychological barriers are less relevant for predicting compliance intentions when health guidelines are uniform and refer to the public as a whole.
Finally, while our findings stress the notion that political trust may effect cognitive appraisal and utility perceptions of one's actions, situational appraisals may be less susceptible to this effect, as perceptions regarding the risks and threats posed by the medical situation (i.e., a pandemic) were found to be associated with political trust only in our first two studies. As mentioned above, this unstable effect of political trust on risk perceptions coincides with the recent work of Dryhurst et al.'s (2020), and further stress the need to deepen the examination of trust effects on cognitive appraisals.
Limitations
This research has several limitations. First, the included studies and the MTM were performed and tested during a public health crisis (the COVID-19 pandemic), which may hamper their validity to times of routine or general health behavior compliance in response to governmentally issued instructions. However, governments usually issue health instructions during public health crises (Kotz Crego & Kontanidis, 2020; Pak et al., 2021). This makes the COVID-19 pandemic a natural and a suitable environment for testing the MTM. Furthermore, our research expanded across a period of 20 months from the initial outbreak and included data collection in 4 points in time at varying levels of crisis severity. Given that our results were similar across all these levels, we can cautiously infer that crisis severity does not affect the validity of the MTM. In addition, in some behavioral disciplines, it is a common and desired practice to explore a model under extreme conditions in order to infer its robustness or to gain new insights on the examined phenomenon in less harsh or routine environments (Bamberger & Pratt, 2010; Sterman, 2002). Therefore, we believe that this work and its conclusions can apply to situations in which governments issue health guidelines, regardless of the situational context. Nonetheless, the MTM should be further examined in future studies under non-crisis conditions. Similarly, despite the postulated theoretical differences in the decision-making process of compliance with health behaviors and other domains, the MTM was tested solely for health behaviors. Hence, the compatibility of our suggested model should be examined in other behavioral domains as well, in order to shed light on its relevance to other contexts.
A second limitation of this work is its single state examination, i.e., Israel. Despite the fact that levels of political trust in Israel are similar to the average of OECD countries (OECD, 2022), and although studies on political trust often consider Israel as a representative case of other democratic countries (e.g., Katz & Gidron, 2022), Israel is characterized with a highly diverse citizenry, and a historic national divide which may impact the effects of political trust on political participation and civic behavior (e.g., Goren et al., 2021; Superti & Gidron, 2021). Some comparative studies support this notion and attest to the exceptionalities in the effects of political trust on civic behavior in Israel (e.g., Norris, 2005). Furthermore, at the time this research was performed, Israel had experienced an unprecedented political crisis, expressed in four consecutive election campaigns within 30 months (instead of one elections every four years), due to the elected parties' inability to form a stable coalition.3 These conditions may have affected the relationship between trust in government and other examined and unexamined variables in this work. Hence, it is possible that under different political conditions our findings would have been different. Nonetheless, it is possible that the political conditions under which our research was conducted may have challenged our model, and that under more serene political times the relationship between political trust and compliance, and its mediating factors would have been even stronger. Therefore, until the MTM is examined in different countries and diverse political contexts, we caution against inferring that our conclusions fully represent other political conditions. Third, the use of behavioral intentions, as an indicator of compliance, may not fully predict actual behavior. However, robust behavioral theories, as well as many health behavior acceptance-focused studies, consider behavior intentions as a good indicator of future behavior(Ajzen, 1985; Bults et al., 2011; Freimuth et al., 2017; Hagger & Hamilton, 2021; Head et al., 2020; Persad & Emanuel, 2020). Fourth, this work is based on four separate studies with several methodological differences, which prevent inter-study statistical analyses and comparisons. Nonetheless, the repeating and accumulating findings, despite these differences, attest to the robustness and validity of our results.
An additional limitation lies in the fact that our main analyses and findings focus on mediation analysis of variables that were measured simultaneously. In other words, our measurements do not reflect any temporal relativity between the "affecting" and the "affected" variables. However, these mediation effects are supported both theoretically and statistically: Theoretically, trust in government is viewed as a deep-rooted trait-like perception (Sønderskov & Dinesen, 2016; Yap, 2019), making it stable and precedent to other perceptions and opinions that may be triggered and measured in surveys. Statistically, a series of post hoc "reversed" mediation tests in all four studies, in which trust in government was the mediator and the hypothesized mediators were the independent variables, were all insignificant. Both of these arguments support our cross-sectional non-temporal approach.
Conclusions
This study sheds light on the mechanism through which trust in government affects compliance intentions with health guidelines, by introducing the MTM. It indicates that trust in government may not have a direct effect on health-related compliance intentions but rather affect the willingness to comply with such instructions through specific types of cognitive appraisals, which are known to affect health behavior, i.e., perceived benefits of the behavior, perceived self-efficacy to perform the behavior and various perceived barriers and shortcomings of these actions. This study also demonstrates that political trust does not necessarily affect compliance intentions through all types of cognitive appraisals that are related to health behavior, as risk perceptions did not mediate this effect. This suggests that while political trust may have a significant effect on the way we perceive our actions and their outcomes, it does not necessarily determine the way we appraise the situational factors we face and that such perceptions may not be relevant for the trust-compliance relationship.
The fact that political trust was not directly associated with health behavior compliance intentions, but only indirectly related to them, does not diminish its relevance for public cooperation with health guidelines, but rather stresses its crucial encompassing impact on public compliance, as it shapes cognitive perceptions which are at the heart of the health-behavior decision-making process. This emphasizes the effect of our relationship with the government in forming the way we evaluate and plan our behaviors, particularly in times of public health crisis, where governmentally issued health instructions are usually published, and public compliance with such instructions is crucial for the management of the crisis and for the prevention of loss of lives.
Despite its limitations, our work may contribute to the public health literature, policy sciences literature and to political theory, as it suggests a new and theoretically adjusted model that explains public compliance with governmentally issued health instructions, while highlighting both the overarching role of political trust alongside its potential limitations. By doing so, our work may provide its readers with theoretical and practical insights with regards to the paths for enhancing public compliance in times in which compliance with health behavior instructions is critical. Future work should consider cultural, situational and personality factors as well.
Acknowledgements
Talia Goren was supported by IDIT - PhD Program for Outstanding Social Sciences Researchers, The Herta & Paul Amir Faculty of Social Sciences, University of Haifa.
Appendix A: Measures applied in the studies
| Measuresa/Study | Study 1 | Study 2 | Study 3 | Study 4 |
|---|---|---|---|---|
| Compliance intentions | An averaged scale of three items (Francis et al., 2004): "I expect/ want/ intend to [the examined health behavior]….". | |||
| α = 0.941 | α = 0.923 | α = 0.914 | α = 0.942 | |
| Trust in GOV | An averaged scale of 5 items (Kang & Van Ryzin, 2019; Miller, 1974). E.g.,: “How much of the time do you think you can trust the government to do the right thing?” (0 = "never" to 100 = "always"). | |||
| α = 0.891 | α = 0.874 | α = 0.885 | α = 0.895 | |
| Benefits | “To what extent do you assume that complying with the directive of the Ministry of Health will help the fight against the coronavirus?” | “To what extent do you assume that using an eye protector/ staying at home during the lockdown will reduce the chances of you being harmed by the Coronavirus?” |
An averaged scale of two items (Chen et al., 2020; Lin et al., 2020): (1) "Getting vaccinated against COVID-19 every 6 months is a good idea because it makes me feel less worried about catching COVID-19"; (2) "Getting vaccinated against COVID-19 every 6 months will reduce may chances of catching COVID-19" r = 0.853; p < 0.01 |
|
| Risk perception |
An averaged scale of three items (Bults et al., 2011; Freimuth et al., 2017; Shim & You, 2015): (1) “How likely do you think it is that you would become sick with coronavirus?”; (2) “How severe would your condition be if you did become sick with coronavirus?”; (3) “To what extent are you worried about the possibility of becoming sick with Coronavirus?” An inter-item reliability check, indicated a relatively low, yet acceptable values (Taber, 2018; van Griethuijsen et al., 2015). |
Perceived severity and susceptibility were each measured by three items (Lin et al., 2020): Severity (α = 0.71), e.g.,: "Complications from COVID-19 are serious"; Susceptibility (α = 0.743), e.g., "the chance of getting COVID-19 in the next few months is great". |
||
| α = 0.654 | α = 0.536 | α = 0.685 | ||
| Barriers | – | Physical, psychological and logistic barriers. Each type was measured by a single item asking participants to rate the extent to which physical, psychological and logistic difficulties may inhibit them from performing the presented instructions. E.g.,: "to which extent will using an eye protector/ staying at home during lockdown will cause you emotional distress, such as embarrassment, stress and anxiety?" Possible answers range from 1 = "to very little extent" to 10 = "to very large extent". |
Safety barriers (Gerend et al., 2013)—2 items: e.g., "I have concerns about the safely of getting the COVID-19 vaccination every 6 months" (r = 0.74; p < 0.01) Psychological barriers (Ampofo et al., 2020;—3 items Champion, 1984): e.g., "getting the COVID-19 vaccination every 6 months will cause me embarrassment/ stress/ anxiety" (α = 0.859) Logistic barriers (Gerend et al., 2013)—2 items: e.g., "I don’t have the time to get vaccinated against COVID-19 every 6 months" (r = 0.678; p < 0.01) Physical barriers — 2 items measuring the level of concern of the predicted pain and discomfort that may be caused by getting vaccinated every 6 months (r = 0.845; p < 0.01). |
|
| Self-efficacy | – | A single item (Barclay et al., 2007; de Vries et al., 2012): "Do you believe you could [perform the presented instruction]?" | An averaged scale of three items (Farooq et al., 2020): e.g., “I am able to take avoidant measures against COVID-19 if I want to” | An averaged scale of three items (Chen et al., 2020; Farooq et al., 2020): e.g., "I am able to get vaccinated against COVID-19 every 6 months if I want to” |
| – | (α = 0.638) | (α = 0.827) | ||
| Technical ability to comply | A single yes/no (1/0) question asked the participants whether they had a working thermometer at home. | – | – | – |
| Knowledge | A summed scale of six items inspired by the 2009 H1N1 influenza knowledge measure (Jhummon-Mahadnac et al., 2012). The questions focused on familiarity with symptoms, modes of transmission, incubation period and preventive measures. Correct answers were summed to a maximum of 20 points. | A summed scale of six statements based on Huang and Zhao (2020) COVID-19 knowledge scale. Respondents, stated whether each statement is correct/ incorrect or "don’t know." E.g., "Inhalation of droplets from sneezing, coughing, or talking to an infected person could cause infection." Each correct answer received a point and the scores were summed to range from 0 to 6. | – | – |
| Stress | A summed scale of fourteen 5-point items of the Perceived Stress Scale (Cohen et al., 1983). E.g.,: "In the last month, how often have you felt nervous and stressed?” (1-never to 5-very often). Scores ranged from 14 (low stress) to 70 (high stress). | – | – | – |
| Instruction type | – | 0—Lockdown; 1- Eye protector | – | |
| Social norms | – | – | A single item (Scholz & Brook, 1998): "Please assess the rate to which your close friends and relatives will …[comply with the presented instruction]?" (0 = "no one" to 100 = "everyone"). | |
| Past COVID vaccination | – | – | – |
1 = Got vaccinated against COVID 0 = Did not get vaccinated against COVID |
| Gender | 1 = Male, 0 = Female; | |||
| Age | In years | |||
| N of children/ parenthood | Number of children | Parenthood: 1 = "has children," 0 = "does not have children" | ||
| Education |
0 = Less than academic degree 1 = Academic degree and above |
A 6-point scale ranging from elementary school = 1 to a masters' degree and beyond = 6; | ||
| Income | A 5-point scale, relative to average household income: 1 = "much lower" to 5 = "much higher" | |||
| Sector | Participants were asked for their sectorial affiliation (Ultra-orthodox / Arab/ General Jewish) | |||
| Political ideology | 3-point ideological spectrum: 1= right; 2 = center; 3= left | – | – | 11-point spectrum: 0=Radical right to 10=Radical left |
aUnless mentioned otherwise, all items were measured on five-point 1–5 scales, representing low to high levels of agreement with statements or extent of behavior.
Funding
This study was funded by the Ministry of Science & Technology, Israel, grant #16914 and the Israel National Institute for Health Policy and Health Services Research, Grant #2020/400R.
Declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Footnotes
At the time the survey was conducted, body temperature monitoring was mandatory in Israel prior to entering public places. Furthermore, citizens were asked to report any changes in their health to their general physician. Our simulated instruction combined these two elements, making it plausible.
The Knesset (the Israeli parliament) website: https://m.knesset.gov.il/EN/About/History/Pages/Lobby.aspx retrieved on August 28th 2022.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Talia Goren, Email: taliagoren@gmail.com.
Dana R. Vashdi, Email: dvashdi@poli.haifa.ac.il
Itai Beeri, Email: itaibeeri@poli.haifa.ac.il.
References
- Ajzen I. From intentions to actions: A theory of planned behavior. In: Kuhl J, Beckmann J, editors. Action control: From cognition to behavior. Springer-Verlag; 1985. pp. 11–39. [Google Scholar]
- Ajzen I, Fishbein M. Attitudes and predicting social behavior: Attitudes, intentions, and perceived behavioral control. Prentice Hall; 1980. [Google Scholar]
- Almond, G. A., & Verba, S. (1963). The civic culture: Political attitudes and democracy in five nations. In The Civic Culture: Political Attitudes and Democracy in Five Nations. Princeton University Press.
- Al-Sabbagh MQ, Al-Ani A, Mafrachi B, Siyam A, Isleem U, Massad FI, Alsabbagh Q, Abufaraj M. Predictors of adherence with home quarantine during COVID-19 crisis: The case of health belief model. Psychology, Health and Medicine. 2021;27(1):215–227. doi: 10.1080/13548506.2021.1871770. [DOI] [PubMed] [Google Scholar]
- Ampofo AG, Adumatta AD, Owusu E, Awuviry-newton K. A cross-sectional study of barriers to cervical cancer screening uptake in Ghana: An application of the health belief model. PLoS ONE. 2020 doi: 10.1371/journal.pone.0231459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrighetto, G., Castelfranchi, C., Mayor, E., McBreen, J., Lopez-Sanchez, M., & Parsons, S. (2013). (Social) Norm Dynamics. In Normative Multi-Agent Systems (Vol. 4).
- Armitage CJ, Conner M. Social cognition models and health behaviour: A structured review. Psychology and Health. 2000;15(2):173–189. doi: 10.1080/08870440008400299. [DOI] [Google Scholar]
- Attwell K, Harper T, Rizzi M, Taylor J, Casigliani V, Quattrone F, Lopalco P. Inaction, under-reaction action and incapacity: Communication breakdown in Italy’s vaccination governance. Policy Sciences. 2021;54:457–475. doi: 10.1007/s11077-021-09427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamberger PA, Pratt M. Moving forward by looking back: Reclaiming unconventional research contexts and samples in ogranizational scholarship. Academy of Management Journal. 2010;53(4):665–671. doi: 10.5465/amj.2010.52814357. [DOI] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice-Hall; 1986. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. Freeman; 1997. [Google Scholar]
- Barclay TR, Hinkin CH, Castellon SA, Mason KI, Reinhard MJ, Marion SD, Levine AJ, Durvasula RS. Age-associated predictors of medication adherence in HIV-positive adults: Health beliefs, self-efficacy, and neurocognitive status. Health Psychology. 2007;26(1):40–49. doi: 10.1037/0278-6133.26.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bish A, Yardley L, Nicoll A, Michie S. Factors associated with uptake of vaccination against pandemic influenza: A systematic review. Vaccine. 2011;29(38):6472–6484. doi: 10.1016/j.vaccine.2011.06.107. [DOI] [PubMed] [Google Scholar]
- Blair RA, Morse BS, Tsai LL. Public health and public trust: Survey evidence from the Ebola Virus Disease epidemic in Liberia. Social Science and Medicine. 2017;172:89–97. doi: 10.1016/j.socscimed.2016.11.016. [DOI] [PubMed] [Google Scholar]
- Bobek DD, Hatfield RC, Wentzel K. An investigation of why taxpayers prefer refunds: A theory of planned behavior approach. Journal of the American Taxation Association. 2007;29(1):93–111. doi: 10.1521/jata.2007.29.1.93. [DOI] [Google Scholar]
- Bord S, Schor A, Satran C, Saleh OA, Inchi L, Halperin D. Distancing adherence and negative emotions among the israeli elderly population during the covid-19 pandemic. International Journal of Environmental Research and Public Health. 2021 doi: 10.3390/ijerph18168770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradburn NM, Sudman S, Blair E, Stocking C. Question threat and response bias. Public Opinion Quarterly. 1978;42(2):221–234. doi: 10.1086/268444. [DOI] [Google Scholar]
- Brown VJ. Risk perception: It’s personal. Environmental Health Perspectives. 2014;122(10):A276–A279. doi: 10.4324/9780203712979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruno JM, Bianchi EC, Sánchez C. Determinants of household recycling intention: The acceptance of public policy moderated by habits, social influence, and perceived time risk. Environmental Science and Policy. 2022;136(November 2021):1–8. doi: 10.1016/j.envsci.2022.05.010. [DOI] [Google Scholar]
- Bults M, Beaujean DJMA, Zwart OD, Kok G, Empelen PV. Perceived risk, anxiety, and behavioural responses of the general public during the early phase of the Influenza A (H1N1) pandemic in the Netherlands: Results of three consecutive online surveys. BMC Public Health. 2011;11(2):1–13. doi: 10.1186/1471-2458-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caferra R, Colasante A, Morone A. The less you burn, the more we earn: The role of social and political trust on energy-saving behaviour in Europe. Energy Research and Social Science. 2021;71(October 2020):101812. doi: 10.1016/j.erss.2020.101812. [DOI] [Google Scholar]
- Casoria F, Galeotti F, Villeval MC. Perceived social norm and behavior quickly adjusted to legal changes during the COVID-19 pandemic. Journal of Economic Behavior and Organization. 2021;190(August):54–65. doi: 10.1016/j.jebo.2021.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaiken S. Heuristic versus systematic information processing and the use of source versus message cues in persuasion. Journal of Personality and Social Psychology. 1980;39(5):752–766. doi: 10.1037//0022-3514.39.5.752. [DOI] [Google Scholar]
- Champion, V. L., & Skinner, C. S. (2008). The Health Belief Model. In: Glanz, K., Rimer, B. K., & Viswanath, K. (Eds.), Health Behavior and Health education (4th ed., pp. 45–66). Jossey-Bass.
- Champion VL. Instrument development for health belief model constructs. Advances in Nursing Science. 1984;6(3):73–85. doi: 10.1097/00012272-198404000-00011. [DOI] [PubMed] [Google Scholar]
- Chapman GB. The psychology of medical decision making. In: Koehler DJ, Harvey N, editors. Blackwell handbook of judgment and decision making. Blackwell Publishing Ltd; 2004. pp. 585–603. [Google Scholar]
- Chen, Y., Zhou, R., Chen, B., Chen, H., Li, Y., & Chen, Z. (2020). Knowledge , Perceived Beliefs , and Preventive Behaviors Related to COVID-19 Among Chinese Older Adults : Cross-Sectional Corresponding Author : Background : Journal of Medical Internet Research, 22(12), e23729. 10.2196/23729. [DOI] [PMC free article] [PubMed]
- Chetioui Y, Lebdaoui H, Chetioui H. Factors influencing consumer attitudes toward online shopping: The mediating effect of trust. EuroMed Journal of Business. 2021;16(4):544–563. doi: 10.1108/EMJB-05-2020-0046. [DOI] [Google Scholar]
- Cialdini RB, Trost MR. Social influence: Social norms, conformity and compliance. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. McGraw-Hill; 1998. pp. 151–192. [Google Scholar]
- Citrin J, Stoker L. Political Trust in a Cynical Age. Annual Review of Political Science. 2018;21:49–70. doi: 10.1146/annurev-polisci-050316-092550. [DOI] [Google Scholar]
- Clark C, Davila A, Regis M, Kraus S. Predictors of COVID-19 voluntary compliance behaviors: An international investigation. Global Transitions. 2020;2:76–82. doi: 10.1016/j.glt.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coe, A. B., Gatewood, S. B. S., Moczygemba, L. R., & Goode, J.-V. “Kelly” R. (2012). The use of the health belief model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. INNOVATIONS in Pharmacy, 3(2), 1–11. 10.24926/iip.v3i2.257. [DOI] [PMC free article] [PubMed]
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A Global Measure of Perceived Stress. In Source: Journal of Health and Social Behavior (Vol. 24, Issue 4). [PubMed]
- Cook TE, Gronke P. The skeptical American: Revisiting the meanings of trust in government and confidence in institutions. Journal of Politics. 2005;67(3):784–803. doi: 10.1111/j.1468-2508.2005.00339.x. [DOI] [Google Scholar]
- Cooter R. Expressive law and economics. Journal of Legal Studies. 1998;27(2):585–608. doi: 10.1086/468036. [DOI] [Google Scholar]
- Cruwys T, Stevens M, Greenaway KH. A social identity perspective on COVID-19: Health risk is affected by shared group membership. British Journal of Social Psychology. 2020;59:584–593. doi: 10.1111/bjso.12391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton RJ. Democratic challenges, democratic choices: The erosion of political support in advanced industrial democracies. Oxford University Press; 2004. [Google Scholar]
- Davies B, Lalot F, Peitz L, Heering MS, Ozkececi H, Babaian J, Davies Hayon K, Broadwood J, Abrams D, Hayon KD, Broadwood J, Abrams D. Changes in political trust in Britain during the COVID-19 pandemic in 2020: Integrated public opinion evidence and implications. Humanities and Social Sciences Communications. 2021;8(1):1–9. doi: 10.1057/s41599-021-00850-6. [DOI] [Google Scholar]
- Davis JL, Buchanan KL, Lee Green B. Racial/ethnic differences in cancer prevention beliefs: Applying the health belief model framework. American Journal of Health Promotion. 2013;27(6):384–389. doi: 10.4278/ajhp.120113-QUAN-15. [DOI] [PubMed] [Google Scholar]
- de Vries H, van Osch L, Eijmael K, Smerecnik C, Candel M. The role of risk perception in explaining parental sunscreen use. Psychology and Health. 2012;27(11):1342–1358. doi: 10.1080/08870446.2012.684059. [DOI] [PubMed] [Google Scholar]
- Devine D, Gaskell J, Jennings W, Stoker G. Trust and the coronavirus pandemic: What are the consequences of and for trust? An early review of the literature. Political Studies Review. 2021;19(2):274–285. doi: 10.1177/1478929920948684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dryhurst S, Schneider CR, Kerr J, Freeman ALJ, Recchia G, van der Bles AM, Spiegelhalter D, van der Linden S. Risk perceptions of COVID-19 around the world. Journal of Risk Research. 2020;23(7–8):994–1006. doi: 10.1080/13669877.2020.1758193. [DOI] [Google Scholar]
- Easton D. A systems analysis of political life. Wiley; 1965. [Google Scholar]
- Farooq A, Laato S, Najmul Islam AKM. Impact of online information on self-isolation intention during the COVID-19 Pandemic: Cross-Sectional study. Journal of Medical Internet Research. 2020;22(5):1–15. doi: 10.2196/19128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine AD, van Rooij B. Legal socialization: Understanding the obligation to obey the law. Journal of Social Issues. 2021;77(2):367–391. doi: 10.1111/josi.12440. [DOI] [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intentions and behavior: An introduction to theory and research. Addison-Wesley; 1975. [Google Scholar]
- Francis, J., Eccles, M. P., Johnston, M., Walker, A. E., Grimshaw, J. M., Foy, R., Kaner, E. F. S., Smith, L., & Bonetti, D. (2004). Constructing questionnaires based on the theory of planned behavior. A manual for health services researcher. In Centre for Health Services Research, University of Newcastle upon Tyne.
- Freimuth VS, Jamison A, Hancock G, Musa D, Hilyard K, Quinn SC. The role of risk perception in flu vaccine behavior among African-American and white adults in the United States. Risk Analysis. 2017;37(11):2150–2163. doi: 10.1111/risa.12790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardiner CK, Bryan AD. Monetary incentive interventions can enhance psychological factors related to fruit and vegetable consumption. Annals of Behavioral Medicine. 2017;51:599–609. doi: 10.1007/s12160-017-9882-4. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Shepherd MA, Shepherd JE. The multidimensional nature of perceived barriers: Global versus practical barriers to HPV vaccination. Health Psychology. 2013;32(4):361–369. doi: 10.1037/a0026248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilley B. The meaning and measure of state legitimacy: Results for 72 countries. European Journal of Political Research. 2006;45(3):499–525. doi: 10.1111/j.1475-6765.2006.00307.x. [DOI] [Google Scholar]
- Gonzalez-Ocantos E, de Jonge CK, Meléndez C, Osorio J, Nickerson DW. Vote buying and social desirability bias: Experimental evidence from Nicaragua. American Journal of Political Science. 2012;56(1):202–217. doi: 10.1111/j.1540-5907.2011.00540.x. [DOI] [Google Scholar]
- Gordoni G, Schmidt P. The decision to participate in social surveys: The case of the arab minority in Israel—An application of the theory of reasoned action. International Journal of Public Opinion Research. 2010;22(3):364–391. doi: 10.1093/ijpor/edq022. [DOI] [Google Scholar]
- Goren T, Beeri I, Vashdi DR. Framing policies to mobilize citizens’ behavior during a crisis: Examining the effects of positive and negative vaccination incentivizing policies. Regulation & Governance. 2022 doi: 10.1111/rego.12478. [DOI] [Google Scholar]
- Goren T, Vashdi DR, Beeri I. “Apples and Oranges”: Examining different social groups’ compliance with government health instructions during the COVID-19 pandemic. International Journal of Health Policy and Management. 2021 doi: 10.34172/ijhpm.2021.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green LW. Toward cost-benefit evaluations of health education: Some concepts, methods, and examples. Health Education Monographs. 1974;2(1_suppl):34–64. doi: 10.1177/10901981740020s106. [DOI] [Google Scholar]
- Grimes M. Organizing consent: The role of procedural fairness in political trust and compliance. European Journal of Political Research. 2006;45:285–315. doi: 10.1111/j.1475-6765.2006.00299.x. [DOI] [Google Scholar]
- Hagger MS, Hamilton K. Effects of socio-structural variables in the theory of planned behavior: A mediation model in multiple samples and behaviors. Psychology and Health. 2021;36(3):307–333. doi: 10.1080/08870446.2020.1784420. [DOI] [PubMed] [Google Scholar]
- Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: What Is it, can it be measured, and does it matter? Milbank Quarterly. 2001;79(4):613–639. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Q, Zheng B, Cristea M, Agostini M, Bélanger JJ, Gützkow B, Kreienkamp J, Leander NP. Trust in government regarding COVID-19 and its associations with preventive health behaviour and prosocial behaviour during the pandemic: A cross-sectional and longitudinal study. Psychological Medicine. 2021 doi: 10.1017/S0033291721001306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X, Baird C. Government crisis messaging on social media, citizen online engagement and compliance with policies. Public Management Review. 2022 doi: 10.1080/14719037.2022.2103843. [DOI] [Google Scholar]
- Hardin, R. (1999). Do we want trust in government? In: Warren, M. E. (Ed.), Democracy and Trust (pp. 22–41). Cambridge University Press. 10.1017/cbo9780511659959.002.
- Hardin R. Trust and trustworthiness. Russell Sage Foundation; 2002. [Google Scholar]
- Hayden J. Introduction to health behavior theory. 4. Jones & Bartlett Learning; 2022. [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis. 2. Guilford Publications; 2017. [Google Scholar]
- Head KJ, Kasting ML, Sturm LA, Hartsock JA, Zimet GD. A national survey assessing SARS-CoV-2 vaccination intentions: Implications for future public health communication efforts. Science Communication. 2020;42(5):698–723. doi: 10.1177/1075547020960463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooghe M, Wilkenfeld B. The stability of political attitudes and behaviors across adolescence and early adulthood: A comparison of survey data on adolescents and young adults in eight countries. Journal of Youth and Adolescence. 2008;37(2):155–167. doi: 10.1007/s10964-007-9199-x. [DOI] [Google Scholar]
- Hough M, Jackson J, Bradford B, Myhill A, Quinton P. Procedural justice, trust, and institutional legitimacy. Policing. 2010;4(3):203–210. doi: 10.1093/police/paq027. [DOI] [Google Scholar]
- Howlett M. Governance modes, policy regimes and operational plans: A multi-level nested model of policy instrument choice and policy design. Policy Sciences. 2009;42(1):73–89. doi: 10.1007/s11077-009-9079-1. [DOI] [Google Scholar]
- Huang J, Choi P, Pang TWY, Chen X, Wang J, Ding H, Jin Y, Zheng ZJ, Wong MCS. Factors associated with participation in colorectal cancer screening: A population-based study of 7200 individuals. European Journal of Cancer Care. 2021;30(2):1–15. doi: 10.1111/ecc.13369. [DOI] [PubMed] [Google Scholar]
- Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research. 2020;288(March):112954. doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwig L, Irwin J, Trevena L, Sweet M. Smart health choices: Making sense of health advice. Hamershmith Press; 2008. [PubMed] [Google Scholar]
- Janz NK, Becker MH. The health belief model: A decade later. Health Education & Behavior. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Jhummon-Mahadnac ND, Knott J, Marshall C. A cross-sectional study of pandemic influenza health literacy and the effect of a public health campaign. BMC Research Notes. 2012 doi: 10.1186/1756-0500-5-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones P, Menon A, Hicken A, Rozek LS. Global adoption of personal and social mitigation behaviors during COVID-19: The role of trust & confidence. PLoS ONE. 2021;16(9):1–16. doi: 10.1371/journal.pone.0256159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahneman D, Tversky A. Subjective probability: A judgment of representativeness. Cognitive Psychology. 1972;3(3):430–454. doi: 10.1016/0010-0285(72)90016-3. [DOI] [Google Scholar]
- Kahneman D, Tversky A. Prospect theory: An analysis of decision under risk. Econometrica. 1979;47(2):263–292. doi: 10.2307/1914185. [DOI] [Google Scholar]
- Kalagy T. “Enclave in transition”: Ways of coping of academics from ultra-orthodox (haredim) minority group with challenges of integration into the workforce. International Journal of Environmental Research and Public Health. 2020;17(7):1–14. doi: 10.3390/ijerph17072373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S, Van Ryzin GG. Coproduction and trust in government: Evidence from survey experiments. Public Management Review. 2019;21(11):1646–1664. doi: 10.1080/14719037.2019.1619812. [DOI] [Google Scholar]
- Kasl SV, Cobb S. Health behavior, illness behavior, and sick role behavior. I. Health and illness behavior. Archives of Environmental Health. 1966;12(2):246–266. doi: 10.1080/00039896.1966.10664365. [DOI] [PubMed] [Google Scholar]
- Katz, H., & Gidron, B. (2022). Civil Society Encroachment in Nonliberal Democracies: The Case of Israel . In: Hoelscher, M., List, R. A., Ruser, A., & Toepler, S. (Eds.), Civil Society: Concepts, Challenges, Contexts (pp. 309–322).
- Kim HK, Tandoc ECJ. Wear or not to wear a mask? Recommendation inconsistency, government trust and the adoption of protection behaviors in cross-lagged TPB models. Health Communication. 2021 doi: 10.1080/10410236.2020.1871170. [DOI] [PubMed] [Google Scholar]
- Kirchler E, Hoelzl E, Wahl I. Enforced versus voluntary tax compliance: The “slippery slope” framework. Journal of Economic Psychology. 2008;29(2):210–225. doi: 10.1016/j.joep.2007.05.004. [DOI] [Google Scholar]
- Kotz Crego, M., & Kontanidis, S. (2020). States of emergency in response to the coronavirus crisis: Situation in certain Member States. In: European Parliamentary Research Service (EPRS) (Issue December).
- Kwok KO, Li KK, Chan HHH, Yi YY, Tang A, Wei WI, Wong SYS. Community responses during the early phase of the COVID-19 epidemic in Hong Kong: Risk perception, information exposure and preventive measures. Emerging Infectious Diseases. 2020;26(7):1575–1579. doi: 10.1101/2020.02.26.20028217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C, Whetten K, Omer S, Pan W, Salmon D. Hurdles to herd immunity: Distrust of government and vaccine refusal in the US, 2002–2003. Vaccine. 2016;34(34):3972–3978. doi: 10.1016/j.vaccine.2016.06.048. [DOI] [PubMed] [Google Scholar]
- Lee YY, Lin JL. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Social Science and Medicine. 2009;68(6):1060–1068. doi: 10.1016/j.socscimed.2008.12.033. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Meyer D, Nerenz D. The common sense model of illness danger. In: Rachman S, editor. Medical psychology. Pergamon Press; 1980. pp. 7–30. [Google Scholar]
- Levi M. Of rule and revenue. University of California Press; 1988. [Google Scholar]
- Levi M, Stoker L. Political trust and trustworthiness. Annual Review of Political Science. 2000;3(1992):475–507. doi: 10.1146/annurev.polisci.3.1.475. [DOI] [Google Scholar]
- Limbu YB, Gautam RK, Pham L. The health belief model applied to COVID-19 vaccine hesitancy: A systematic review. Vaccines. 2022;10(6):1–13. doi: 10.3390/vaccines10060973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y, Hu Z, Zhao Q, Alias H, Id MD, Id PW, Danaee M, Wong LP, Id MD, Id PW. Understanding COVID-19 vaccine demand and hesitancy: A nationwide online survey in China. PLOS Neglected Tropical Diseases. 2020;28(12):e0008961. doi: 10.1371/journal.pntd.0008961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lissitsa S. Effects of digital use on trust in political institutions among ethnic minority and hegemonic group—A case study. Technology in Society. 2021;66(June):101633. doi: 10.1016/j.techsoc.2021.101633. [DOI] [Google Scholar]
- Liu P, Yang R, Xu Z. Public acceptance of fully automated driving: Effects of social trust and risk/benefit perceptions. Risk Analysis. 2019;39(2):326–341. doi: 10.1111/risa.13143. [DOI] [PubMed] [Google Scholar]
- Liu W, Huang Y. Does relationship matter during a health crisis: Examining the role of local government- public relationship in the public acceptance of COVID-19 vaccines. Health Communication. 2021 doi: 10.1080/10410236.2021.1993586. [DOI] [PubMed] [Google Scholar]
- Magnan RE, Shorey Fennell BR, Brady JM. Health decision making and behavior The role of affect-laden constructs. Soc Personal Psychol Compass. 2017;11:e12333. doi: 10.1111/spc3.12333ARTICL. [DOI] [Google Scholar]
- Malecki KMC, Keating JA, Safdar N. Crisis communication and public perception of COVID-19 risk in the era of social media. Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of America. 2021;72(4):697–702. doi: 10.1093/cid/ciaa758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslow AH. A theory of human motivation. Psychological Review. 1943;50(4):370–396. doi: 10.1037/h0054346. [DOI] [Google Scholar]
- Matute J, Palau-Saumell R, Meyer J, Derqui B, Jiménez-Asenjo N. Are you getting it? Integrating theories to explain intentions to get vaccinated against COVID-19 in Spain. Journal of Risk Research. 2021 doi: 10.1080/13669877.2021.1958044. [DOI] [Google Scholar]
- May PJ. Regulation and compliance motivations: Examining different approaches. Public Administration Review. 2005;65(1):31–44. doi: 10.1111/j.1540-6210.2005.00428.x. [DOI] [Google Scholar]
- Mayer RC, Davis JH, Schoorman FD. An integrative model of organizational trust. Academy of Management Review. 1995;20(3):709–734. doi: 10.2307/258792. [DOI] [Google Scholar]
- Mesch GS, Schwirian KP. Social and political determinants of vaccine hesitancy: Lessons learned from the H1N1 pandemic of 2009–2010. American Journal of Infection Control. 2015;43(11):1161–1165. doi: 10.1016/j.ajic.2015.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaels D, Emanuel EJ, Bright RA. A national strategy for COVID-19: Testing, surveillance, and mitigation strategies. JAMA - Journal of the American Medical Association. 2022;327(3):213–214. doi: 10.1001/jama.2021.24168. [DOI] [PubMed] [Google Scholar]
- Miller, M. D., & Levine, T. R. (2019). Persuasion. In: Stacks, D. W., Salwen, M. B., & Eichhorn, K. C. (Eds.), An integrated approach to communication theory and research (3rd ed., pp. 261–276). Routledge.
- Miller AH. Political issues and trust in government: 1964–1970. The American Political Science Review. 1974;68(3):951–972. doi: 10.2307/1959140. [DOI] [Google Scholar]
- Mizrahi S, Cohen N, Vigoda-Gadot E, Krup DN. Compliance with government policies during emergencies: Trust, participation and protective actions. Governance. 2022 doi: 10.1111/gove.12716. [DOI] [Google Scholar]
- Montoya ID, Atkinson JS, Trevino RA. Economics as a factor in models of behavioral motivation and change. Substance Use and Misuse. 2000;35(3):329–346. doi: 10.3109/10826080009147700. [DOI] [PubMed] [Google Scholar]
- Morgado P, Sousa N, Cerqueira JJ. The impact of stress in decision making in the context of uncertainty. Journal of Neuroscience Research. 2015;93(6):839–847. doi: 10.1002/jnr.23521. [DOI] [PubMed] [Google Scholar]
- Murphy K. The role of trust in nurturing compliance: A study of accused tax avoiders. Law and Human Behavior. 2004;28(2):187–209. doi: 10.1023/B:LAHU.0000022322.94776.ca. [DOI] [PubMed] [Google Scholar]
- Norris, P. (2017). The conceptual framework of political support. In: Zmerli, S. & van der Meer, T. W. G. (Eds.), Handbook on Political Trust (pp. 19–32). Edward Elgar. 10.4337/9781782545118.
- Norris P. Critical citizens: Global support for democratic government. Oxford University Press; 1999. [Google Scholar]
- Norris P. Radical right: Voters and parties in the electoral market. Cambridge University Press; 2005. [Google Scholar]
- O’Keefe, D. J. (2004). Trends and Prospects in Persuasion Theory and Research. In Readings in persuasion, social influence, and compliance gaining (3rd ed., pp. 31–43). Pearson/Allyn and Bacon.
- O’Keefe DJ. Persuasion: Theory and research. 3. Sage; 2015. [Google Scholar]
- OECD. (2022). Trust in government (indicator). 10.1787/1de9675e-en.
- Pak A, McBryde E, Adegboye OA. Does high public trust amplify compliance with stringent COVID-19 government health guidelines? A multi-country analysis using data from 102,627 individuals. Risk Management and Healthcare Policy. 2021;14:293–302. doi: 10.2147/RMHP.S278774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paredes MR, Apaolaza V, Marcos A, Hartmann P. Predicting COVID-19 vaccination intention: The roles of institutional trust, perceived vaccine safety, and interdependent self-construal. Health Communication. 2021;00(00):1–12. doi: 10.1080/10410236.2021.1996685. [DOI] [PubMed] [Google Scholar]
- Parfenova A. Will you shake my hand? Factors of noncompliance with COVID-19 behavioral rules in the framework of enforced social isolation in Russia. The International Journal of Sociology and Social Policy. 2020;40(9/10):1221–1235. doi: 10.1108/IJSSP-06-2020-0246. [DOI] [Google Scholar]
- Persad G, Emanuel EJ. Fair allocation of scarce medical resources in the time of covid-19. JAMA. 2020;323(22):2241–2242. doi: 10.1056/nejmsb2005114. [DOI] [PubMed] [Google Scholar]
- Peter, F. (2010). Political Legitimacy. Stanford Encyclopedia of Philosophy Archive. https://stanford.library.sydney.edu.au/archives/sum2021/entries/legitimacy/.
- Petty, R. E., & Cacioppo, J. T. (1986). The elaboration likelihood model of persuasion. Communication and persuasion (pp. 1–24). Springer. 10.1007/978-1-4612-4964-1_1.
- Prati G, Pietrantoni L, Zani B. Compliance with recommendations for pandemic influenza H1N1 2009: The role of trust and personal beliefs. Health Education Research. 2011;26(5):761–769. doi: 10.1093/her/cyr035. [DOI] [PubMed] [Google Scholar]
- Prochaska, J. O., & DiClemente, C. C. (1982). Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy: Theory, Research and Practice, 19(3), 276–288. 10.1037/h0088437.
- Promberger M, Marteau TM. When do financial incentives reduce intrinsic motivation ? Comparing behaviors studied in psychological and economic literatures. Health Psychology. 2013;32(9):950–957. doi: 10.1037/a0032727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radu, B. (2021). Trust in public institutions and compliance with measures against the COVID-19 pandemic. Case study on the metropolitan area of Cluj, Romania. Transylvanian Review of Administrative Sciences, 17(63), 128–150. 10.24193/tras.63E.7.
- Redelmeier DA, Tversky A. Discrepancy between medical decisions for individual patients and for groups. The New England Journal of Medicine. 1990;322:1162–1164. doi: 10.1056/NEJM199004193221620. [DOI] [PubMed] [Google Scholar]
- Redelmeier DA, Tversky A. On the framing of multiple prospects. Psychological Science. 1992;3(3):191–193. doi: 10.1111/j.1467-9280.1992.tb00025.x. [DOI] [Google Scholar]
- Rieger MO, Wang M. Trust in government actions during the COVID-19 Crisis. Social Indicators Research. 2022;159(3):967–989. doi: 10.1007/s11205-021-02772-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers RW. A protection motivation theory of fear appeals and attitude change1. The Journal of Psychology. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. Historical origins of the health belief model. Health Education Monographs. 1974;2(4):328–335. doi: 10.1177/109019817400200403. [DOI] [PubMed] [Google Scholar]
- Rothstein B, Stolle D. The state and social capital: An institutional theory of generalized trust. Comparative Politics. 2008;40(4):441–459. doi: 10.5129/001041508x12911362383354. [DOI] [Google Scholar]
- Saechang O, Yu J, Li Y. Public trust and policy compliance during the COVID-19 Pandemic: The role of professional trust. Healthcare. 2021 doi: 10.3390/healthcare9020151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarwar F, Imam H, Jameel HT, Panatik SA, Brannen DE. Unravelling the relationship between trust in government and voluntary adoption of preventative behaviour through health belief model: A cross-culture study. Kybernetes. 2022 doi: 10.1108/K-05-2022-0667. [DOI] [Google Scholar]
- Sata Shanka M, Moges Menebo M. When and how trust in government leads to compliance towards COVID-19 precautionary measures. Journal of Business Research. 2021;139(October 2021):1275–1283. doi: 10.1016/j.jbusres.2021.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider CR, Dryhurst S, Kerr J, Freeman ALJ, Recchia G, Spiegelhalter D, van der Linden S. COVID-19 risk perception: A longitudinal analysis of its predictors and associations with health protective behaviours in the United Kingdom. Journal of Risk Research. 2021;24(3–4):294–313. doi: 10.1080/13669877.2021.1890637. [DOI] [Google Scholar]
- Scholz JT, Lubell M. Trust and taxpaying: Testing the heuristic approach to collective action. American Journal of Political Science. 1998;42(2):398–417. doi: 10.2307/2991764. [DOI] [Google Scholar]
- Schoon I, Cheng H. Determinants of political trust: A lifetime learning model. Developmental Psychology. 2011;47(3):619–631. doi: 10.1037/a0021817. [DOI] [PubMed] [Google Scholar]
- Shim M, You M. Cognitive and affective risk perceptions toward food safety outbreaks: Mediating the relation between news use and food consumption intention. Asian Journal of Communication. 2015;25(1):48–64. doi: 10.1080/01292986.2014.989242. [DOI] [Google Scholar]
- Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):804. doi: 10.1186/s12889-021-10816-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons-Morton, B., McLeroy, K., & Wendel, M. (2012). Behavior Theory in Health Promotion Practice and Research. Jones & Bartlett Learning.
- Somera LP, Lee H, Badowski G, Cassel K, Somera LP, Lee H, Badowski G, Cassel K, Somera LP, Lee H, Badowski G, Cassel K. Health information seeking, source trust, and culture : A comparative analysis of health information trends and needs between guam and the United States health information seeking, source trust, and culture : A comparative analysis of health informati. Journal of Health Communication. 2016;21(4):469–478. doi: 10.1080/10810730.2015.1095822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sønderskov KM, Dinesen PT. Trusting the state, trusting each other? The effect of institutional trust on social trust. Political Behavior. 2016;38:179–202. doi: 10.1007/s11109-015-9322-8. [DOI] [Google Scholar]
- Sterman, J. D. (2002). System Dynamics: Systems Thinking and Modeling for a Complex World (ESD-WP-2003–01.13).
- Sun W. Toward a theory of ethical consumer intention formation: Re-extending the theory of planned behavior. AMS Review. 2020;10(3–4):260–278. doi: 10.1007/s13162-019-00156-6. [DOI] [Google Scholar]
- Sung JJY, Choi SYP, Chan FKL, Ching JYL, Lau JTF, Griffiths S. Obstacles to colorectal cancer screening in Chinese: A study based on the Health Belief Model. American Journal of Gastroenterology. 2008;103(4):974–981. doi: 10.1111/j.1572-0241.2007.01649.x. [DOI] [PubMed] [Google Scholar]
- Superti C, Gidron N. Too old to forget: The dynamics of political trust among immigrants. Political Studies. 2021 doi: 10.1177/0032321720980899. [DOI] [Google Scholar]
- Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Research in Science Education. 2018;48(6):1273–1296. doi: 10.1007/s11165-016-9602-2. [DOI] [Google Scholar]
- Tam CC, Li X, Li X, Wang Y, Lin D. Adherence to preventive behaviors among college students during COVID-19 pandemic in China: The role of health beliefs and COVID-19 stressors. Current Psychology. 2021 doi: 10.1007/s12144-021-01942-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thaker J, Zhao X, Leiserowitz A. Media use and public perceptions of global warming in India. Environmental Communication. 2017;11(3):353–369. doi: 10.1080/17524032.2016.1269824. [DOI] [Google Scholar]
- Thomadsen R, Rooderkerk RP, Amir O, Arora N, Bollinger B, Hansen K, John L, Liu W, Sela A, Singh V, Sudhir K, Wood W. How context affects choice. Customer Needs and Solutions. 2018;5(1–2):3–14. doi: 10.1007/s40547-017-0084-9. [DOI] [Google Scholar]
- Thomassen, J., Andeweg, R., & van Ham, C. (2017). Political trust and the decline of legitimacy debate: a theoretical and empirical investigation into their interrelationship. In: Zmerli, S. & van der Meer, T. W. G. (Eds.), Handbook on Political Trust (pp. 509–525). Edward Elgar. 10.4337/9781782545118.
- Tong KK, Chen JH, Yu EW, Wu AMS. Adherence to COVID-19 precautionary measures applying the health belief model. Applied Psychology: Health and Well-Being. 2020;12(4):1205–1223. doi: 10.1111/aphw.12230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglino GA, Moon C. Compliance and self-reporting during the COVID-19 pandemic: A cross-cultural study of trust and self-conscious emotions in the United States, Italy, and South Korea. Frontiers in Psychology. 2021;12:565845. doi: 10.3389/fpsyg.2021.565845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trent M, Salmon DA, MacIntyre CR. Using the health belief model to identify barriers to seasonal influenza vaccination among Australian adults in 2019. Influenza and Other Respiratory Viruses. 2021;15(5):678–687. doi: 10.1111/irv.12843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trent M, Seale H, Chughtai AA, Salmon D, MacIntyre CR. Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: A comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine. 2021 doi: 10.1016/j.vaccine.2021.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler TR. Why people obey law? Contemporary Sociology. 1990 doi: 10.2307/2076193. [DOI] [Google Scholar]
- van Griethuijsen RALF, van Eijck MW, Haste H, den Brok PJ, Skinner NC, Mansour N, Gencer AS, BouJaoude S. Global patterns in students’ views of science and interest in science. Research in Science Education. 2015;45(4):581–603. doi: 10.1007/s11165-014-9438-6. [DOI] [Google Scholar]
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020;89(May):531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visschers VHM, Keller C, Siegrist M. Climate change benefits and energy supply benefits as determinants of acceptance of nuclear power stations: Investigating an explanatory model. Energy Policy. 2011;39(6):3621–3629. doi: 10.1016/j.enpol.2011.03.064. [DOI] [Google Scholar]
- Wallace LE, Wegener DT, Petty RE. When sources honestly provide their biased opinion: Bias as a distinct source perception with independent effects on credibility and persuasion. Personality and Social Psychology Bulletin. 2020;46(3):439–453. doi: 10.1177/0146167219858654. [DOI] [PubMed] [Google Scholar]
- Wang M, Zhang Q, Zhou KZ. The origins of trust asymmetry in international relationships: An institutional view. Journal of International Marketing. 2020;28(2):81–101. doi: 10.1177/1069031X19898492. [DOI] [Google Scholar]
- Warren, M. E. (2018). Trust and democracy. In: The Oxford handbook of social and political trust (pp. 75–94). Oxford University Press.
- Weible CM, Nohrstedt D, Cairney P, Carter DP, Crow DA, Durnová AP, Heikkila T, Ingold K, McConnell A, Stone D. COVID-19 and the policy sciences: Initial reactions and perspectives. Policy Sciences. 2020;53(2):225–241. doi: 10.1007/s11077-020-09381-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weston D, Ip A, Amlôt R. Examining the application of behaviour change theories in the context of infectious disease outbreaks and emergency response: A review of reviews. BMC Public Health. 2020;20(1):1–19. doi: 10.1186/s12889-020-09519-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human Vaccines and Immunotherapeutics. 2020;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu T. Media, trust in government, and risk perception of COVID-19 in the early stage of epidemic: An analysis based on moderating effect. Healthcare. 2021 doi: 10.3390/healthcare9111597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadete T, Batra K, Netski DM, Antonio S, Patros MJ, Bester JC. Assessing acceptability of COVID-19 vaccine booster dose among adult americans: A cross-sectional study. Vaccines. 2021 doi: 10.3390/vaccines9121424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yap OF. How political trust matters in emergent democracies: Evidence from East and Southeast Asia. Journal of Public Policy. 2019;39(2):295–328. doi: 10.1017/S0143814X1800003X. [DOI] [Google Scholar]
- Yuan M. Psychological perceptions and voluntary protective behaviors during COVID-19 pandemic in China: The roles of cultural worldview. Human and Ecological Risk Assessment. 2022;28(1):114–132. doi: 10.1080/10807039.2021.2023316. [DOI] [Google Scholar]
- Zampetakis LA, Melas C. The health belief model predicts vaccination intentions against COVID-19: A survey experiment approach. Applied Psychology: Health and Well-Being. 2021;13(2):469–484. doi: 10.1111/aphw.12262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zmerli, S., & van der Meer, T. W. G. (2017). Handbook on Political Trust, In: Zmerli, S. & van der Meer, T. W. G. (eds.). Edward Elgar. 10.4337/9781782545118.