Abstract
The use of portable ultrasound (US) devices is increasing, due to its accessibility, versatility, non-invasiveness, and its significant support in the patient management, extending the traditional physical examination through the POCUS (point-of-care ultrasound). The pocket-size or handheld ultrasound devices (HUDs) can easily perform focused exams, not aiming to substitute for the high-end US systems (gold standard), since the HUDs usually have more limited functions. The HUDs are promising tools for the diagnosis, prognosis, and monitoring of the COVID-19 infection and its related disorders. In conclusion, the routine use of HUDs may ameliorate the management of COVID-19 pandemic, according to the guidelines for the POCUS approach and the procedures for the protection of the patients and the professionals.
Keywords: Portable ultrasound, Point-of-Care ultrasound, COVID-19, Echoscopy
Introduction
Evidence in the literature has recently increased about the extending use of the so-called POCUS (point-of-care ultrasound) by portable US devices, improving the timely medical decision-making process, in all the different acute patients’ settings, outside (as at home and/or in ambulance) or inside the healthcare facilities and hospitals (as in emergency rooms and wards) [1–24].
Since its appearance in 2019, the COrona VIrus Disease 19 (COVID-19) infection required major efforts to protect the patients, because of the high risk of mortality, particularly in comorbidity (as in elderly people) and in not protected subjects [25–29]. The advantages of the expanding use of POCUS in the COVID-19 pandemic scenario may involve the resuscitative (related to an acute resuscitation), the diagnostic (enabling the early diagnosis and implementing the diagnostic capacity), the symptom/sign-based (used in a specific clinical pathway), the procedure guidance (guiding a specific medical procedure), and the therapeutic/monitoring activities (monitoring the follow-up of diseases and therapies) [30]. At the same time, the US examination should integrate the clinical physical examination with high-impact images, without replacing it.
A miniaturized hand-held US scanner was developed as early as 1978, with a limited imaging performance and a weight of about 1.5 kg [31, 32]. Nowadays, technological advances have led to small devices, no larger than a mobile phone (referred to as pocket-size or handheld ultrasound devices, HUD), which can be easily used to perform partial, focused exams, not aiming to substitute for the high-end US systems (gold standard).
As matter of fact, the high-end US systems have the full range of standard echo modalities and measurements: mono-dimensional or M-mode (MM); two-dimensional (2-D) or bi-dimensional (B-mode); three-dimensional (3D); color Doppler (Color); continuous Doppler (CW); pulsed wave Doppler (PW); tissue velocity imaging (TVI); transesophageal modality (TEE); and contrast echo (Contrast) modality. The HUDs usually have more limited functions, such as MM, 2D, Color, PW, measurement packages, and imaging optimization (SonoCT real-time compound, XRES adaptive, Tissue Harmonic Imaging) [33–40]. Many HUDs have an included display, such as Vscan and Vscan Extend (GE), C Scan and Optigo (Philips), Acuson (Siemens), iViz and NanoMaxx and iLook (Sonosite), uSmart (Terason) and Sonimage (Konica Minolta), and EvoTouch (Quantel Medical). Other HUD beam images to tablet/smartphone are Vscan Air (GE), Lumify (Philips), Sonoeye (Chison), Butterfly (iQ), Clarius (Clarius Mobile Health), SonoQue C4PL (Sonoque), and Cerbero.3 (ATL).
Methods
The Study USinMED was approved on the role of the bedside ultrasound in our Hospital, by the Ethical Committee of Sapienza University of Rome (RIF. CE 6583_2021).
We searched online medical literature database (PubMed) from 2019 to 2022, covering the 3-year period that marked the COVID-19 appearance and pandemic diffusion, using the search strategy to address the following: (1) problem (COVID-19 disease); (2) intervention (hand-held or portable US); comparisons (POCUS versus conventional imaging); (3) outcome (accuracy); (4) article type (experimental studies); and (5) study design (any).
The following string was used in searching the PubMed database: (hand held ultrasound [Title/Abstract] OR portable ultrasound [Title/Abstract] AND point of care ultrasound [Title/Abstract] AND COVID-19 [Title/Abstract].
Our predetermined list of exclusions included the following: non-English study; impossible to obtain the full-text; article type (e.g., opinion of experts, editorials, tutorials, case reports, abstract, commentary, book chapters, reviews or systematic reviews); no comparison of hand-held US with other imaging method (e.g., X-ray, conventional US, computed tomography; magnetic resonance imaging); US not performed in adult (study in child); US performed by non-doctor (e.g., medical student, nurse); and study not applied to human subject (veterinary study).
The articles’ selection involved a two-step screening process by two independent researchers: in the first step, the studies were screened for relevancy to hand-held US in COVID-19, and, in the second step, the full texts were screened for inclusion. Any disagreement was resolved by the intervention of a third independent reviewer, if necessary.
Results
We retrieved n.334 articles, and 5 studies were evaluated (Fig. 1; Table 1) [41–45]. We initially excluded n.2 books, n.6 systematic reviews and meta-analyses, n.38 reviews, n.23 case reports, n.39 studies in child, n.21 studies in other animals, n.9 tutorials, and n.1 editorial. Then, we excluded n.166 studies not related to COVID-19, n.19 papers not related to US, n.2 studies with not available full text, n.2 no comparison with other imaging method, and n.2 not specified US devices.
Fig. 1.
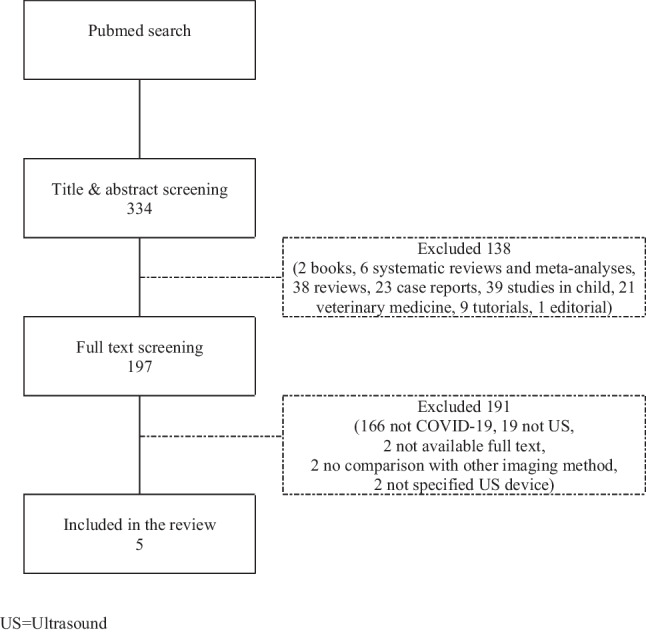
Flowchart of the literature screening
Table 1.
Characteristics of the reviewed studies
| Study, year [Ref.] | Location | Sign or disease/organ | Device | Comparator test |
|---|---|---|---|---|
| Falgarone et al., 2020 [41] | Paris, Marseille/France | Pneumonia/lung | EvoTouch Quantel Medical | CT scan |
| Jalilet al., 2020 [42] | Waxahachie/TX, USA | Pneumonia/lung | Vscan ExtendGE | Chest X-ray (8% CT scan) |
| Gibbonset al., 2021 [43] | Philadelphia/PA, USA | Pneumonia/lung | Butterfly iQ | Chest X-ray, CT scan |
| Abd Wahab et al., 2022 [44] | Kuala Lumpur, Selangor Darul Ehsan, Kelantan/Malaysia | Pneumonia/lung | Lumify Philips,BenQ T3300 | Chest X-ray |
| Dadon et al., 2022 [45] | Jerusalem/Israel | Cardiovascular disease, pneumonia/heart, lung | Vscan ExtendGE | Chest X-ray |
CT computed tomography
Falgarone et al. evaluated n.50 inpatients by lung US (LUS) to predict lung damage at CT scan and oxygen requirement: US was 89% sensitive and 100% specific in predicting CT chest scan abnormalities and 95% sensitive and 67% specific in detecting oxygen requirements [41].
Jalil et al. studied n.69 patients within the first 24 h of hospitalization by LUS for the evaluation of various acute pathologies: a high sensitivity (91%) and specificity (86%) were reported for COVID-19 pneumonia [42].
Gibbons et al. examined n.110 subjects of an urban university emergency department to compare LUS and chest X-ray for detecting viral/atypical pneumonia (CT scan gold standard): LUS sensitivity and specificity were 98% and 33% (versus 70% and 44% for chest X-ray) [43].
Abd Wahab et al. recruited n.261 subjects in out-of-hospital setting, and subsequently, chest X-rays were taken after being admitted to the healthcare facilities: LUS detected pulmonary changes in more subjects than X-ray (97% versus 45%) among subjects with normal LUS but reported abnormal chest X-ray; only 1 subject had pulmonary infiltrate changes (there was no agreement as the Cohen’s kappa coefficient was 0.08) [44].
Dadon et al. evaluated n.103 patients within 48 h of admission to the hospital by echocardiogram and LUS evaluation: a substantial agreement (kappa = 0.612, p < 0.001) was demonstrated between the operator and the echocardiographer for left ventricular ejection fraction (LVEF); chest X-ray demonstrated lung infiltrates in 74% of cases [45].
Discussion
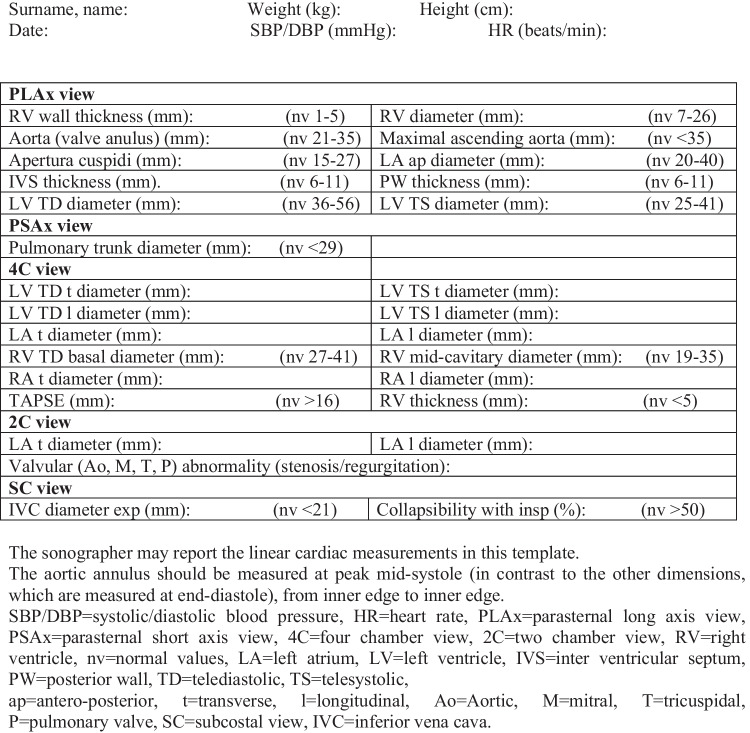
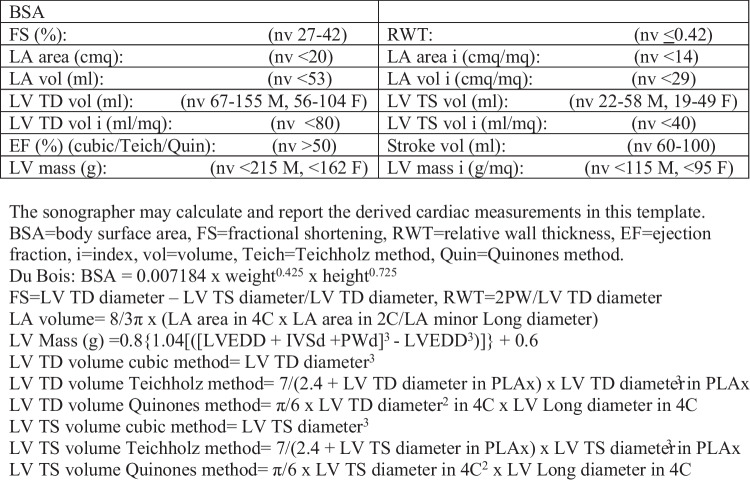
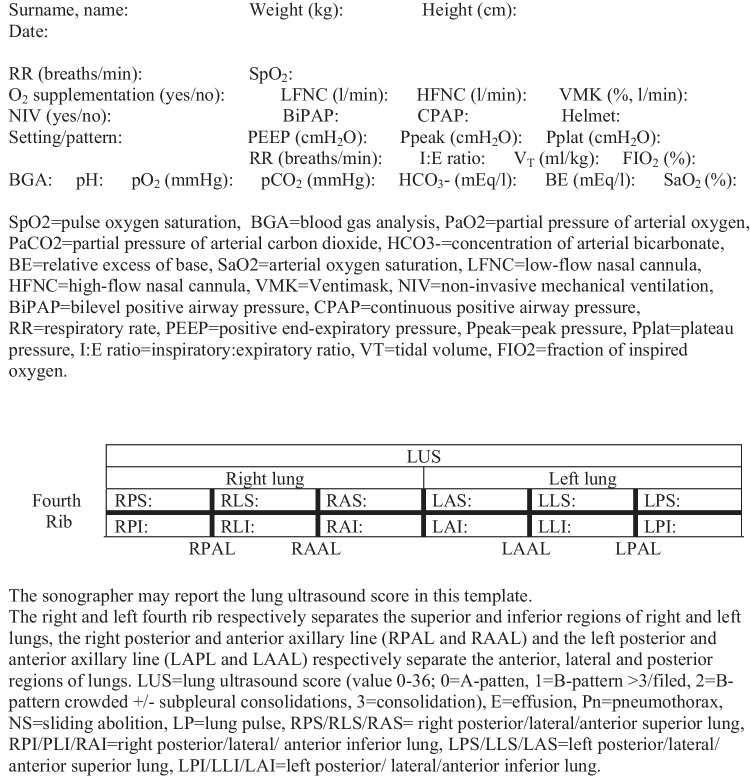
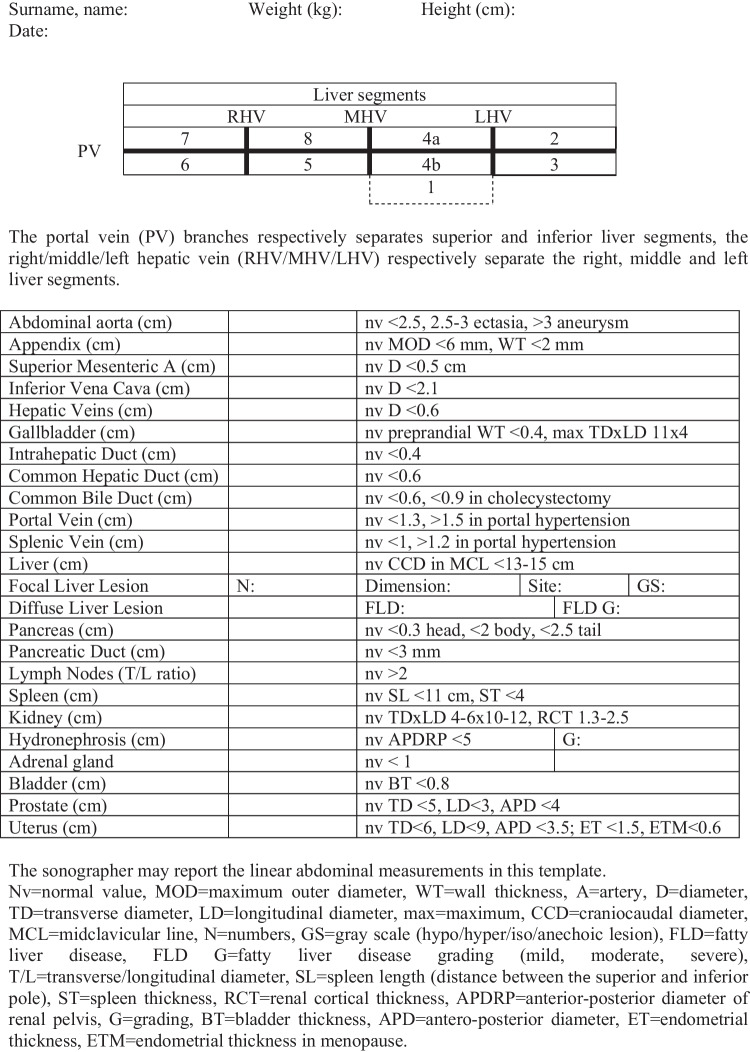
The technical characteristics of HUDs allow to evaluate the main aspects of the heart, lungs, and/or abdominal organs, and they are very useful in patients with a significant comorbidity and polypharmacy (respectively, an average of 7 diseases and 8 drugs) [25, 46]. Previous studies in the literature focused to the left/right ventricular functions, valve regurgitation (by Color option), B-line for lung score, intracavitary (pleural, pericardial, intra-abdominal) effusions, inferior vena cava collapsibility, biliary/urinary tract disorders, aortic diameters, and deep vein thrombosis [23, 35, 47–57]. We proposed three main reports for the echoscopy in Figs. 2, 3, 4, and 5.
Fig. 2.
Bedside heart echoscopy report
Fig. 3.
Derived heart echoscopy measurements
Fig. 4.
Bedside lung echoscopy report
Fig. 5.
Bedside abdomen echoscopy report
The HUDs may be widely used by general medicine practitioners, emergency medicine specialists, internists, geriatricians, and students in teaching schools, with proper training and education of users [36, 58–65]. A tailored training program model for HUD users was proposed for echocardiography: an in-hospital period of 60 days (3 days per week) with visual assessment of at least 150 exams [66]. For emergency US, the trainees should complete a benchmark of 150–300 total exams depending on the number of applications being utilized, as suggested by the American College of Emergency Physicians [23].
The US studies on COVID-19 evaluated by this review were conducted in out-of-hospital [42] and in-hospital settings, and, in particular, in the emergency department [43], in designated medical wards [45], in the department of infectious diseases [41], and within the first 24 h of hospitalization [42]. In lung US protocol, the patients were examined, respectively: in the supine position, with 4 bilateral scanning areas (3 anterior upper, mid, and lower lung zones and the posterolateral costophrenic recess on each hemi thorax) [42]; sitting position with 12 windows (anterior superior, anterior inferior, lateral superior, lateral inferior, posterior superior and posterior inferior bilateral window) and a lung score ranged from 0 to 36 (0 = none, 1–7 = mild; 8–18 = moderate, and 19–36 = severe score) [44, 45] or sitting position with 8 windows (bilaterally anterior upper and middle, posterior middle and lower lobe) [42]; and not limited position (lying, sitting and standing), with 6 locations for each hemithorax (2 anterior, 3 side, and 1 posterior location) [41].
The studies showed high sensitivity (91–95%) and lower specificity (33–100%) for identifying COVID-19 disease by using lung POCUS by HUDs [41–44].
Gibbons et al. pointed out that congestive heart failure (CHF) and interstitial lung disease (ILD) have similar findings as COVID-19 pneumonia on LUS (with three or more B-lines or the presence of a single confluent B-line encompassing a third or more of the visualized intercostal space) [43]. The analysis of the different lung regions may increase the specificity of the test.
Examining the evidence in the literature, a quick guide recently proposed a 12-point lung exam (6 points on each lung), in order to increase the sensitivity in the detection of COVID-19 findings [67], whereas other studies suggested the 6 or 10 point exam [68–70].
As described in the literature, US has highest levels of sensitivity and specificity comparable to CT with regard to the detection of pleural (respectively range 92–100% and 93–100%, US versus CT), pericardial (range 87–94% and 92–96%), and intra-abdominal (range 73–76% and 97–98%) effusions [71–74].
Two studies reported that the ultrasound examination was performed within 1–5 days from symptom/admission [42, 45]. The detectable extent of the lung lesions may be related to the time elapsed before the US examination and may increase the sensitivity of the test.
The severity of the COVID-19 infection is related to the development of a severe pulmonary insufficiency and complications, like superinfections, coagulation disorders (deep vein thrombosis, pulmonary embolism), cardiovascular diseases (myocarditis, pericarditis, atrial fibrillation and/or acute hearth failure, Takotsubo cardiomyopathy, shock), cytokine release syndrome, acute kidney and liver injury, and brain damage [25, 75]. The HUDs are promising tools for the diagnosis, prognosis, and monitoring of COVID-19-related disorders, and POCUS is increasingly being used, as recently reported [68, 76–84]. The heart and the lung are the most investigated sites by US in COVID-9 patients, with particular attention to the left/right systolic function, valvular pathology, inferior vena cava collapsibility, intracavitary effusions, lung B-lines, and subpleural consolidations/lung hepatization (for the lung score) [69, 75, 81–83, 85–89].
In the study of Falgarone et al. [41], the authors demonstrated that the lung US was a good screening test for oxygen requirements (≥ 0.5 l/min), with 95% sensitivity and 67% specificity, and a severity index threshold for oxygen therapy of 0.32 (about 11/36 of the lung score).
It has been reported that the handheld US predicted the composite end point of in-hospital death, mechanical ventilation, shock, and acute decompensated heart failure [68, 90]. Abnormal echocardiogram (defined as left or right ventricular dysfunction or enlargement or moderate/severe valvular regurgitation/stenosis) at the echocardiographic study by HUDs was associated with the need for advanced ventilatory support, acute decompensated heart failure (ADHF), myocardial injury, acute kidney injury (AKI), death, and the composite end point (in-hospital death, mechanical ventilation, shock, and ADHF) with an unadjusted odds ratio (OR) of 7.29 [68]. The lung score (mean 3.7, range 0–20, by the means of a 10-location assessment) was associated with the advanced ventilatory support, anti-COVID-19 medication use, myocardial injury, hospital length of stay, mechanical ventilation, ADHF, in-hospital death, and the composite end point with an unadjusted OR of 1.44 [68].
The survival time of COVID-19 on dry inanimate surfaces is up to 72 h [76, 91]. Therefore, the cleaning of the instruments and the protection of the healthcare workers and patients are key points in the COVID-19 infection management. In patients with suspected/confirmed COVID-19, the US scans are safely conducted with personal protection equipment (clothing, aprons, gowns, shoe covers, double gloving, masks, goggles, face shields) [92]. The ease of HUD decontamination is an unquestioned advantage [93], whereas the high-end US machines need major efforts in terms of time and costs, due to the greater surface area and the additional components (columns, wheels, keyboards, cords, printers, etc.). As matter of fact, the HUDs may be used with the protective covers and the specific cleaning (for the devices and the probes, as well as the dedicated smartphones) [94–102]. The system and transducers must be cleaned and disinfected after each exam. The COVID-19 units may have dedicated devices (that do not leave the ward), which can be disinfected after each scan (for examples, with disposable wipes) and at the end of each day (with ultraviolet irradiation or plasma circulation air sterilizer) [100, 103, 104]. The reporting room should be periodically cleaned, too.
It is noteworthy that other types of diagnostic radiology exams (CT scans and X-rays) require the transportation of the patient to the radiology department, exactly on the contrary of the POCUS approach, increasing the risk of contamination. Moreover, the HUDs are less expensive than standard POCUS systems, and therefore, a hospital could purchase more HUD units, readily available during times of high patient volume and resource-limited settings.
Conclusion
Even if the CT scan remains the gold standard for the assessment of lung involvement extent in COVID-19 infection [105], the cardio-pulmonary US may be very useful in the viral scenario for additional reasons, such as to avoid irradiation (in pregnancy), to perform serial examinations (limiting X-ray and CT scan use), to predict the need for advanced therapy (mechanical ventilation), to prevent the severe complications, and to ameliorate the multiple end-points.
In conclusion, the routine use of HUDs may ameliorate the management of COVID-19 pandemic, when the specific guidelines for the POCUS approach and the specific procedures for the protection of the patients and professionals from the COVID-19 infection are applied.
Author Contribution
All authors contributed to the review conception and design. The first draft of the manuscript was commented by all authors, and they read and approved the final manuscript.
Data Availability
Not applicable.
Code Availability
Not applicable.
Declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
The authors declare no competing interests.
Footnotes
This article is part of the Topical Collection on Covid-19.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baribeau Y, Sharkey A, Chaudhary O, et al. Handheld point-of-care ultrasound probes: the new generation of POCUS. J Cardiothorac Vasc Anesth. 2020;34:3139–3145. doi: 10.1053/j.jvca.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Montinari MR, Minelli S. The first 200 years of cardiac auscultation and future perspectives. J Multidisciplinary Healthcare. 2019;1:183–189. doi: 10.2147/JMDH.S193904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michon A, Jammal S, Passeron A, et al. Échographie ultraportable en médecine interne: retour d’expérience et point de vue. Rev Med Interne. 2019;40:220–225. doi: 10.1016/j.revmed.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 4.Gianstefani S, Catibog N, Whittaker AR, et al. Pocket-size imaging device: effectiveness for ward-based transthoracic studies. Eur Heart J Cardiovasc Imaging. 2013;14:1132–1139. doi: 10.1093/ehjci/jet091. [DOI] [PubMed] [Google Scholar]
- 5.Chugh Y, Lohese O, Sorajja P, et al. Adoptability and accuracy of point-of-care ultrasound in screening for valvular heart disease in the primary care setting. J Clin Ultrasound. 2022;50:265–270. doi: 10.1002/jcu.23062. [DOI] [PubMed] [Google Scholar]
- 6.Jenkins S, Alabed S, Swift A, et al. Diagnostic accuracy of handheld cardiac ultrasound device for assessment of left ventricular structure and function: systematic review and meta-analysis. Heart. 2021;107:1826–1834. doi: 10.1136/heartjnl-2021-319561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lisi M, Cameli M, Mondillo S, et al. Incremental value of pocket-sized imaging device for bedside diagnosis of unilateral pleural effusions and ultrasound-guided thoracentesis. Interact Cardiovasc Thorac Surg. 2012;5:596–601. doi: 10.1093/icvts/ivs223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 9.Lee L, DeCara JM. Point-of-care ultrasound. Curr Cardiol Rep. 2020;22:149. doi: 10.1007/s11886-020-01394-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morbach C, Buck T, Rost C, et al. Point-of-care B-type natriuretic peptide and portable echocardiography for assessment of patients with suspected heart failure in primary care: rationale and design of the three-part Handheld-BNP program and results of the training study. Clin Res Cardiol. 2018;107:95–107. doi: 10.1007/s00392-017-1181-3. [DOI] [PubMed] [Google Scholar]
- 11.Costello C, Yastrebov K, Yang Y, et al. Pocket-sized point-of-care cardiac ultrasound devices. Role in the emergency department. Minimum standards for ultrasound equipment in intensive care. Recommendations from CICM Ultrasound Special Interest Group. Australasian J Ultrasound Med. 2017;20:41–6. doi: 10.1002/ajum.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The College of Emergency Medicine. Core (level 1) ultrasound curriculum. 2009;1–71. Website https://rcem.ac.uk/wp-content/uploads/2021/10/1.14.5-RCEM-EMUS-booklet-3.pdf. Accessed 02 May 2022.
- 13.Sforza A, Mancusi C, Carlino MV, et al. Diagnostic performance of multi-organ ultrasound with pocket-sized device in the management of acute dyspnea. Cardiovasc Ultrasound. 2017;1:16. doi: 10.1186/s12947-017-0105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dietrich CF, Goudie A, Chiorean L, et al. Point of care ultrasound: a WFUMB position paper. Ultrasound Med Biol. 2017;43:49–58. doi: 10.1016/j.ultrasmedbio.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 15.Lancellotti P, Price S, Edvardsen T, et al. The use of echocardiography in acute cardiovascular care: recommendations of the European Association of Cardiovascular Imaging and the Acute Cardiovascular Care Association. Eur Heart J Cardiovasc Imaging. 2015;16:119–146. doi: 10.1093/ehjci/jeu210. [DOI] [PubMed] [Google Scholar]
- 16.Cardim N, Dalen H, Voigt JU, et al. The use of handheld ultrasound devices: a position statement of the European Association of Cardiovascular Imaging (2018 update) Eur Heart J Cardiovasc Imaging. 2019;20:245–252. doi: 10.1093/ehjci/jey145. [DOI] [PubMed] [Google Scholar]
- 17.Galderisi M, Santoro A, Versiero M, et al. Improved cardiovascular diagnostic accuracy by pocket size imaging device in non-cardiologic outpatients: the NaUSiCa (Naples Ultrasound Stethoscope in Cardiology) study. Cardiovasc Ultrasound. 2010;8:51. doi: 10.1186/1476-7120-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Modesti PA, Boddi M, Galanti G. Cardiac ultrasound at the bedside: the power of videos in medical education. Intern Emerg Med. 2016;11:723–725. doi: 10.1007/s11739-016-1432-8. [DOI] [PubMed] [Google Scholar]
- 19.Ruddox V, Norum IB, Stokke TM, et al. Focused cardiac ultrasound by unselected residents-the challenges. BMC Med Imaging. 2017;17:22. doi: 10.1186/s12880-017-0191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spencer KT. Focused cardiac ultrasound: where do we stand? Curr Cardiol Rep. 2015;3:567. doi: 10.1007/s11886-015-0567-y. [DOI] [PubMed] [Google Scholar]
- 21.Scalea TM, Rodriguez A, Chiu WC, et al. Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Trauma. 1999;46:466–472. doi: 10.1097/00005373-199903000-00022. [DOI] [PubMed] [Google Scholar]
- 22.Montoya J, Stawicki SP, Evans DC, et al. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg. 2016;42:119–126. doi: 10.1007/s00068-015-0512-1. [DOI] [PubMed] [Google Scholar]
- 23.Narula J, Chandrashekhar Y, Braunwald E. Time to add a fifth pillar to bedside physical examination. Inspection, palpation, percussion, auscultation, and insonation. JAMA Cardiol. 2018;3:346–50. doi: 10.1001/jamacardio.2018.0001. [DOI] [PubMed] [Google Scholar]
- 24.Peteiro J. Echocardiography at the primary care physician setting: Ready? J Clin Ultrasound. 2022;50:271–272. doi: 10.1002/jcu.23144. [DOI] [PubMed] [Google Scholar]
- 25.Martocchia A, Spuntarelli V, Aiello F, et al. Using INTERCheck® to evaluate the incidence of adverse events and drug-drug interactions in out- and inpatients exposed to polypharmacy. Drugs Real World Outcomes. 2020;7:243–249. doi: 10.1007/s40801-020-00193-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rahman S, Singh K, Dhingra S, et al. The double burden of the COVID-19 pandemic and polypharmacy on geriatric population - public health implications. Ther Clin Risk Manag. 2020;16:1007–1022. doi: 10.2147/TCRM.S272908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Polidori MC, Sies H, Ferrucci L, et al. COVID-19 mortality as a fingerprint of biological age. Ageing Res Rev. 2021;67:101308. doi: 10.1016/j.arr.2021.101308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang JJ, Dong X, Liu GH et al. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol 2022;1–18. 10.1007/s12016-022-08921-5 [DOI] [PMC free article] [PubMed]
- 30.American College of Emergency Physicians. Emergency ultrasound guidelines. https://www.acep.org/Clinical-Practice-Management/Ultrasound/. 2015. Accessed 02 May 2022
- 31.Ligtvoet CM, Rijsterborgh H, Kappen L, et al. Real time ultrasound imaging with a hand-held scanner. Part I - technical description. Ultrasound Med Biol. 1978;4:91–2. doi: 10.1016/0301-5629(78)90033-9. [DOI] [PubMed] [Google Scholar]
- 32.Maeda K. History of medical ultrasound. Donald School J Ultrasound Obstet Gynecol. 2017;2:91–100. [Google Scholar]
- 33.Sicari R, Galderisi M, Voigt JU, et al. The use of pocket-size imaging devices: a position statement of the European Association of Echocardiography. Eur J Echocardiogr. 2011;12:85–87. doi: 10.1093/ejechocard/jeq184. [DOI] [PubMed] [Google Scholar]
- 34.Acheampong B, Parra DA, Aliyu MH, et al. Smartphone interfaced handheld echocardiography for focused assessment of ventricular function and structure in children: a pilot study. Echocardiography. 2020;37:96–103. doi: 10.1111/echo.14575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barreiros AP, Dong Y, Ignee A, et al. EchoScopy in scanning abdominal diseases; a prospective single center study. Med Ultrason. 2019;21:8–15. doi: 10.11152/mu-1907. [DOI] [PubMed] [Google Scholar]
- 36.Cardim N, Fernandez Golfin C, Ferreira D, et al. Usefulness of a new miniaturized echocardiographic system in outpatient cardiology consultations as an extension of physical examination. J Am Soc Echocardiogr. 2011;24:117–124. doi: 10.1016/j.echo.2010.09.017. [DOI] [PubMed] [Google Scholar]
- 37.Choi BG, Mukherjee M, Dala P, et al. Interpretation of remotely downloaded pocket-size cardiac ultrasound images on a web-enabled smartphone: validation against workstation evaluation. J Am Soc Echocardiogr. 2011;24:1325–1330. doi: 10.1016/j.echo.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 38.Colclough A, Nihoyannopoulos P. Pocket-sized point-of-care cardiac ultrasound devices. Role in the emergency department. Herz. 2017;42:255–261. doi: 10.1007/s00059-016-4531-4. [DOI] [PubMed] [Google Scholar]
- 39.Chamsi-Pasha MA, Sengupta PP, Zoghbi WA. Handheld echocardiography: current state and future perspectives. Circulation. 2017;136:2178–2188. doi: 10.1161/CIRCULATIONAHA.117.026622. [DOI] [PubMed] [Google Scholar]
- 40.Roelandt JRTC. A personal ultrasound imager (ultrasound stethoscope). A revolution in the physical cardiac diagnosis! Eur Heart J. 2002;23:523–7. doi: 10.1053/euhj.2001.2800. [DOI] [PubMed] [Google Scholar]
- 41.Falgarone G, Pamoukdjian F, Cailhol J, et al. Lung ultrasound is a reliable diagnostic technique to predict abnormal CT chest scan and to detect oxygen requirements in COVID-19 pneumonia. Aging (Albany NY) 2020;12:19945–19953. doi: 10.18632/aging.104150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jalil BA, Khan A, Kugasia IR, et al. Lung ultrasound in early SARS-CoV-2 pneumonia and the LUS-CoV criteria. Proc (Bayl Univ Med Cent) 2020;34:1–4. doi: 10.1080/08998280.2020.1834658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gibbons RC, Magee M, Goett H, et al. Lung ultrasound vs. chest X-Ray study for the radiographic diagnosis of COVID-19 pneumonia in a high-prevalence population. J Emerg Med. 2021;60:615–625. doi: 10.1016/j.jemermed.2021.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abd Wahab M, Eddie EA, Ibrahim Ahmad UQA, et al. Lung ultrasonography for COVID-19 patients in out of hospital settings. J Ultrasound. 2022;25:475–482. doi: 10.1007/s40477-021-00609-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dadon Z, Levi N, Alpert EA, et al. The quality, safety, feasibility, and interpretive accuracy of echocardiographic and lung ultrasound assessment of COVID-19 patients using a hand-held ultrasound. Echocardiography. 2022;39:886–894. doi: 10.1111/echo.15372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Institute for Health and Care Excellence (NICE) Multimorbidity and polypharmacy. Key therapeutic topic (KTT18). 2017, last updated 2019. Accessed 02 May 2022
- 47.Geria RN, Raio CC, Tayal V. Point-of-care ultrasound: not a stethoscope-a separate clinical entity. J Ultrasound Med. 2015;34:172–173. doi: 10.7863/ultra.34.1.172. [DOI] [PubMed] [Google Scholar]
- 48.Tse KH, Luk WH, Lam MC. Pocket-sized versus standard ultrasound machines in abdominal imaging. Singapore Med J. 2014;55:325–333. doi: 10.11622/smedj.2014078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Andersen GN, Haugen BO, Graven T, et al. Feasibility and reliability of point-of-care pocket-sized echocardiography. Eur J Echocardiogr. 2011;12:665–670. doi: 10.1093/ejechocard/jer108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Erbel R, Eggebrecht H. Aortic dimensions and the risk of dissection. Heart. 2006;92:137–142. doi: 10.1136/hrt.2004.055111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barreiros AP, Cui XW, Ignee A, et al. EchoScopy in scanning abdominal diseases: initial clinical experience. Z Gastroenterol. 2014;52:269–275. doi: 10.1055/s-0033-1350114. [DOI] [PubMed] [Google Scholar]
- 52.Fröhlich E, Beller K, Muller R, et al. Point of care ultrasound in geriatric patients: prospective evaluation of a portable handheld ultrasound device. Ultraschall Med. 2020;41:308–316. doi: 10.1055/a-0889-8070. [DOI] [PubMed] [Google Scholar]
- 53.Williams C, Mateescu A, Rees E, et al. Point-of-care echocardiographic screening for left-sided valve heart disease: high yield and affordable cost in an elderly cohort recruited in primary practice. Echo Res Pract. 2019;6:71–79. doi: 10.1530/ERP-19-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Esposito R, Ilardi F, Schiano Lomoriello V, et al. Identification of the main determinants of abdominal aorta size: a screening by pocket size imaging device. Cardiovasc Ultrasound. 2017;15:2. doi: 10.1186/s12947-016-0094-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dalen H, Gundersen GH, Skjetne K, et al. Feasibility and reliability of pocket-size ultrasound examinations of the pleural cavities and vena cava inferior performed by nurses in an outpatient heart failure clinic. Eur J Cardiovasc Nurs. 2015;14:286–293. doi: 10.1177/1474515114547651. [DOI] [PubMed] [Google Scholar]
- 56.Gulicˇ TG, Makuc J, Prosen G, et al. Pocket-size imaging device as a screening tool for aortic stenosis. Wien Klin Wochenschr. 2016;128:348–353. doi: 10.1007/s00508-015-0904-6. [DOI] [PubMed] [Google Scholar]
- 57.Khandwalla RM, Birkeland KT, Zimmer R, et al. Usefulness of serial measurements of inferior vena cava diameter by VscanTM to identify patients with heart failure at high risk of hospitalization. Am J Cardiol. 2017;119:1631–1636. doi: 10.1016/j.amjcard.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 58.Martocchia A, Ialungo S, Dulcetti A, et al. The evaluation of the intracavitary effusions by a beside ultrasound examination. Clin Hemorheol Microcirc. 2022;81(3):233. doi: 10.3233/CH-221402. [DOI] [PubMed] [Google Scholar]
- 59.Andersen GN, Viset A, Mjølstad OC, et al. Feasibility and accuracy of point-of-care pocket-size ultrasonography performed by medical students. BMC Med Educ. 2014;14:156. doi: 10.1186/1472-6920-14-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Arienti V, Di Giulio R, Cogliati C, et al. Bedside ultrasonography (US), Echoscopy and US point of care as a new kind of stethoscope for internal medicine departments: the training program of the Italian Internal Medicine Society (SIMI) Intern Emerg Med. 2014;9:805–814. doi: 10.1007/s11739-014-1113-4. [DOI] [PubMed] [Google Scholar]
- 61.Galusko V, Khanji MY, Bodger O, et al. Hand-held ultrasound scanners in medical education: a systematic review. J Cardiovasc Ultrasound. 2017;25:75–83. doi: 10.4250/jcu.2017.25.3.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Seraphim A, Paschou SA, Grapsa J, et al. Pocket-sized echocardiography devices: one stop shop service? J Cardiovasc Ultrasound. 2016;24:1–6. doi: 10.4250/jcu.2016.24.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mjølstad OC, Andersen GN, Dalen H, et al. Feasibility and reliability of point-of-care pocket-size echocardiography performed by medical residents. Eur Heart J Cardiovasc Imaging. 2013;14:1195–1202. doi: 10.1093/ehjci/jet062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chambers JB, Rajani R, Short N, et al. Point-of-care cardiac ultrasound in acute internal medicine: how can it be delivered? Clin Med (Lond) 2015;15:403–404. doi: 10.7861/clinmedicine.15-4-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ruddox V, Stokke TM, Edvardsen T, et al. The diagnostic accuracy of pocket-size cardiac ultrasound performed by unselected residents with minimal training. Int J Cardiovasc Imaging. 2013;29:1749–1757. doi: 10.1007/s10554-013-0278-7. [DOI] [PubMed] [Google Scholar]
- 66.Galderisi M, Santoro A, Versiero M, et al. Improved cardiovascular diagnostic accuracy by pocket size imaging device in non-cardiologic outpatients: the NaUSiCa (Naples Ultrasound Stethoscope in Cardiology) study. Cardiovasc Ultrasound. 2010;8:51. doi: 10.1186/1476-7120-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fujifilm Sonosite. Lung ultrasound for COVID-19. Quick guide. EDU20830 12/2020. www.secure.sonosite.com/covid-19. Accessed 02 May 2022.
- 68.Dadon Z, Levi N, Orlev A, et al. The utility of handheld cardiac and lung ultrasound in predicting outcomes of hospitalised patients with COVID-19. Can J Cardiol. 2022;38:338–346. doi: 10.1016/j.cjca.2021.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Szekely Y, Lichter Y, Taieb P, et al. Spectrum of cardiac manifestations in COVID-19: a systematic echocardiographic study. Circulation. 2020;142:342–353. doi: 10.1161/CIRCULATIONAHA.120.047971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kiamanesh O, Harper L, Wiskar K, et al. Lung ultrasound for cardiologists in the time of COVID-19. Can J Cardiol. 2020;36:1144–1147. doi: 10.1016/j.cjca.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Soni NJ, Franco R, Velez MI, et al. Ultrasound in the diagnosis and management of pleural effusions. J Hosp Med. 2015;12:811–816. doi: 10.1002/jhm.2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Netherton S, Milenkovic V, Taylor M, et al. Diagnostic accuracy of eFAST in the trauma patient: a systematic review and meta-analysis. CJEM. 2019;21:727–728. doi: 10.1017/cem.2019.381. [DOI] [PubMed] [Google Scholar]
- 73.Lichtenstein D, Goldstein I, Mourgeon E, et al. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100:9–15. doi: 10.1097/00000542-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 74.Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 75.Dweck MR, Bularga A, Hahn RT, et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21:949–958. doi: 10.1093/ehjci/jeaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gibson LE, Bittner EA, Chang MG. Handheld ultrasound devices: an emerging technology to reduce viral spread during the Covid-19 pandemic. Am J Infect Control. 2020;48:968–969. doi: 10.1016/j.ajic.2020.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Medhane F, Kirkpatrick JN. Echocardiography in the era of COVID-19: lessons for the future. Curr Cardiol Rep. 2021;23:178. doi: 10.1007/s11886-021-01610-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang L, Wang B, Zhou J, et al. Bedside focused cardiac ultrasound in COVID-19 from the Wuhan epicenter: the role of cardiac point-of-care ultrasound, limited transthoracic echocardiography, and critical care echocardiography. J Am Soc Echocardiogr. 2020;33:676–682. doi: 10.1016/j.echo.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Johri AM, Galen B, Kirkpatrick JN, et al. ASE statement on point-of-care ultrasound during the 2019 novel coronavirus pandemic. J Am Soc Echocardiogr. 2020;33:670–673. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Huang G, Vengerovsky A, Morris A, et al. Development of a COVID-19 point-of-care ultrasound protocol. J Am Soc Echocardiogr. 2020;33:903–905. doi: 10.1016/j.echo.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Khanji MY, Ricci F, Patel RS, et al. Special article - The role of hand-held ultrasound for cardiopulmonary assessment during a pandemic. Prog Cardiovasc Dis. 2020;63:690–695. doi: 10.1016/j.pcad.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Iyengar-Kapuganti RL, Patel N, Anastasius M, et al. Point-of-care ultrasound findings and clinical outcomes in patients with COVID-19. J Am Soc Echocardiogr. 2020;33:1416–1417. doi: 10.1016/j.echo.2020.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jenkins S, Garg P. Prime time for handheld echocardiography in COVID-19 pandemic. Clin Med. 2020;20:e132. doi: 10.7861/clinmed.Let.20.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Naderi H, Robinson S, Swaans MJ, et al. Adapting the role of handheld echocardiography during the COVID-19 pandemic: a practical guide. Perfusion. 2021;36:547–558. doi: 10.1177/0267659120986532. [DOI] [PubMed] [Google Scholar]
- 85.Jain SS, Liu Q, Raikhelkar J, et al. Indications for and findings on transthoracic echocardiography in COVID-19. J Am Soc Echocardiogr. 2020;33:1278–1284. doi: 10.1016/j.echo.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.van den Heuvel FMA, Vos JL, Koop Y, et al. Cardiac function in relation to myocardial injury in hospitalised patients with COVID-19. Neth Heart J. 2020;28:410–417. doi: 10.1007/s12471-020-01458-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mahmoud-Elsayed HM, Moody WE, Bradlow WM, et al. Echocardiographic findings in patients with COVID-19 pneumonia. Can J Cardiol. 2020;36:1203–1207. doi: 10.1016/j.cjca.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Barman HA, Atici A, Tekin EA, et al. Echocardiographic features of patients with COVID-19 infection: a cross-sectional study. Int J Cardiovasc Imaging. 2021;37:825–834. doi: 10.1007/s10554-020-02051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ross DW, Hasan Z. Role of Point of Care Ultrasonography in patients with COVID-19 associated acute kidney injury. POCUS J. 2022;7:59–64. doi: 10.24908/pocus.v7iKidney.15344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Karagodin I, Carvalho Singulane C, et al. Echocardiographic correlates of in-hospital death in patients with acute COVID-19 infection: the World Alliance Societies of Echocardiography (WASE-COVID) Study. J Am Soc Echocardiogr. 2021;34:819–830. doi: 10.1016/j.echo.2021.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.World Health Organization (WHO). Technical specifications of personal protective equipment for COVID-19. 2020. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-PPE_specifications-2020.1. Accessed 02 May 2022.
- 93.Fujifilm Sonosite. COVID-19 Point-of-care ultrasound guide. P29241–01. www.secure. sonosite.com/covid-19. Accessed 02 May 2022.
- 94.Wahi S, Thomas L, Stanton T, et al. CSANZ imaging council position statement on echocardiography services during the COVID-19 Pandemic. Heart Lung Circ. 2020;29:e78–e83. doi: 10.1016/j.hlc.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Civco. Ultrasound infection control in management of COVID-19. https://www.civco.com/ covid-19. Accessed 02 May 2022.
- 96.Protek Medical Products, Inc. Probe covers. http://www.protekmedical.com/Covers/ Storage.html. Accessed 02 May 2022.
- 97.Sheathes. https://www.sheathes.com. Accessed 02 May 2022.
- 98.https://www.parkerlabs.com/protex-JUM.asp. Accessed 02 May 2022.
- 99.Samsung. Keep your Galaxy devices clean. https://www.samsung.com/us/support/answer/ ANS00086342. Accessed 02 May 2022.
- 100.Apple Inc. Cleaning your iPhone. https://support.apple.com/en-us/HT207123. Accessed 02 May 2022.
- 101.List of hard-surface disinfectants for use against coronavirus (COVID-19) - Canada.ca. https:// www.canada.ca/en/health-canada/services/drugs-health-products/disinfectants/covid-19/list.html. Accessed 02 May 2022.
- 102.Sonosite. Cleaners and disinfectants tool. www.sonosite.com/sales-support/cleaners-disinfectants. Accessed 02 May 2022.
- 103.Cheng Y, Hu J, Chen H, et al. Effects of different methods of air disinfection of computed tomography rooms dedicated to COVID-19 Cases. Biomed Res Int. 2020;22:5302910. doi: 10.1155/2020/5302910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.American College of Emergency Physicians. Ultrasound machine cleaning process for COVID-19. 2020. Available at: http://www.acep.org/globalassets/images/acep-us-machine-cleaning-covid-19.pdf. Accessed 02 May 2022.
- 105.Quarato CMI, Venuti M, Lacedonia D, et al. The role of transthoracic ultrasound in the novel Coronavirus Disease (COVID-19): a reappraisal. information and disinformation: is there still place for a scientific debate? Front Med (Lausanne) 2020;7:271. doi: 10.3389/fmed.2020.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.