Abstract
Background:
Retinitis pigmentosa (RP) is a set of inherited rod-cone degenerative diseases that clinically presents with similar signs and symptoms. Mutations in one of more than 70 genes are involved. Patients will commonly present with bone-spicule pigment formation, waxy optic nerve pallor, and attenuated blood vessels in the posterior pole.Symptoms often begin with progressive night blindness, mid-peripheral visual field defects, and eventual tunnel vision. Central vision loss will ultimately occur following loss of rod function. Complete blindness is uncommon.
Objective:
The aim of this article is to present two cases of retinitis pigmentosa (mother and daughter) trough optalmologic exams in our clinic. The next aim it to show how to menage a low vision service and to treat cystoid macular oedema as a complication of retinitis pigmentosa.
Methods:
All medical reports are shown in this article. Every diagnostic tool as well as report is a part from our archived history of the patients and has been throughly analysed. We also reviewed available literature using the key words retinitis pigmentosa, cystoid macular oedema, gene therapy.
Case presentation:
A 38 year old female patient for a low vision consultation. The patient was legally blind secondary to retinitis pigmentosa, which was diagnosed in her late 20s. She reported gradually progressive hazy central vision and decreasing peripheral vision in both eyes as well as severe night blindness. Other than the diagnosis of retinitis pigmentosa in both eyes,the patient had no other remarkable ocular conditions. Findings at that visit included unaided distance visual acuities VOD: 0,04 VOS: 0,06. Pupils were round with brisk responses. Extraocular muscle motility was full in both eyes. Confrontation methode visual fields were noted as temporal loss in the right eye and superior and temporal loss in the left eye. The perimetry test could not be performed due to the lack of correspondece of the patient even after a couple repetitions of the perimetry. She had normal ocular adnexa and quiet lids, conjunctiva, and sclera in both eyes. Corneas in both eyes were noted as clear epithelium, clear stroma, and clear endothelium. Anterior chambers had normal depth, iris with no pathological findings in both eyes; lens incipient sclerotic. Intraocular pressures were noted as 22 mmHg in both eyes with Icare, 21mmHg and 19 mmHg with aplanation tonometry; pahimetry corretional factor was +1 on both eyes. The vitreous was clear in both eyes. Both optic nerves were measured as 0.4 cup-to-disc ratios with no disc edema, disc hemorrhages, notching, or thinning noted.Waxy disc pallor and attenuated blood vessels were observed in both eyes. The macula in both eyes had retinal pigment epithelium (RPE) changes with no edema or hemorrhages. Bone spicule changes were noted 360 in the periphery of both eyes with no holes or tears(Figure 1a+1b+1c+1d),
Conclusion:
We presented two cases of retinitis pigmentosa – the mother with diagnosed RP more than 15 years ago in need for low vision rehabilitation service and the daughter that got diagnosed after our initial examination and with complications in visual impairment through cystoid macular oedema.
Keywords: Optical Coherence Tomography (OCT) Diagnostic of Retinitis Pigmentosa
1. BACKGROUND
Retinitis pigmentosa (RP) is a set of inherited rod-cone degenerative diseases that clinically presents with similar signs and symptoms. Mutations in one of more than 70 genes are involved. Patients will commonly present with bone-spicule pigment formation, waxy optic nerve pallor, and attenuated blood vessels in the posterior pole.Symptoms often begin with progressive night blindness, mid-peripheral visual field defects, and eventual tunnel vision. Central vision loss will ultimately occur following loss of rod function. Complete blindness is uncommon. There is currently no cure for RP. Treatment is primarily aimed at slowing progression of the disease that include interventions for secondary complications, retinal prosthesis implants, and gene therapy. RP is one of the most common causes of severe vision impairments and can significantly affect daily life, impacting activities such as driving, reading, and mobility. Low vision rehabilitation services are available to improvevisual function through devices, to assess safe mobility, and to connect patients with resources to maintain levels of independence (1).
2. OBJECTIVE
The aim of this article is to present two cases of retinitis pigmentosa (mother and daughter) trough optalmologic exams in our clinic. The next aim it to show how to menage a low vision service and to treat cystoid macular oedema as a complication of retinitis pigmentosa.
3. MATERIAL AND METHODS
All medical reports are shown in this article. Every diagnostic tool as well as report is a part from our archived history of the patients and has been throughly analysed. We also reviewed available literature using the key words retinitis pigmentosa, cystoid macular oedema, gene therapy.
4. CASE PRESENTATION
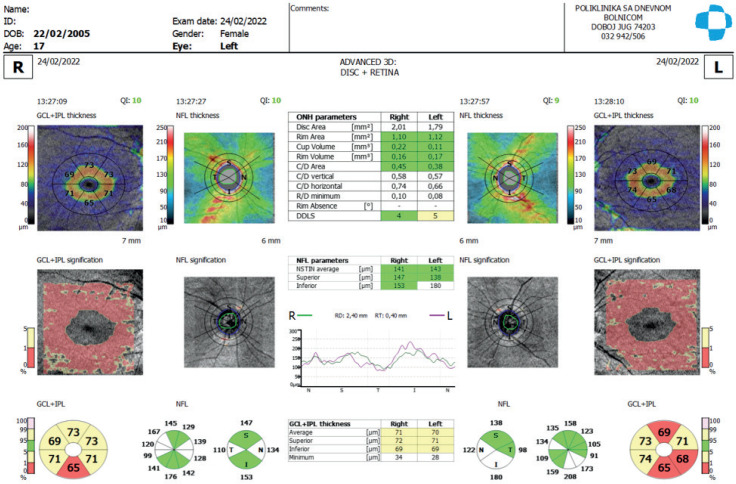
An optical coherence tomography (OCT) scan showed an ischaemic macula and no evidence of macular edema or subretinal fluid in both eyes(Figure 2). The OCT of the optic disc showed thining of the GCL+IPL (Figure no 3). The patient reported a history of testing in her late 20s in Russia when she was diagnosed with retinitis pigmentosa (amamnestic informations with no documentations). She did not recall the name of the test or doctor who performed the test. From her description, an electroretinogram (ERG) was most likely performed, which she reported resulted in positive findings for retinitis pigmentosa. The patiens was also mentioned recieving injections in Russia „in the eye“ that were as explained for treatment of the condition. The patient’s younger daughter accompanied her to the low vision consultation. Knowing that this is a hereditary disease, she is also interested in an exam. The mother regarded herself as a very independent woman and reported living alone with no husband and taking care of the daughter. She was fully aware of the condition and her main goal for low vision rehabilitation was reading and a desire to be fit with a stronger reading prescription. She also wants to show her daughter that it is in fact possible to maintain an everyday life with handing all the daily tasks with no big help. She was currently using several different pairs of reading glasses, all of which she found unhelpful. At the low vision examination, entering unaided distance visual acuities were 0,04 in the right eye and 0,06 in the left eye. Near visual acuities with her preferred +2.50 diopter(D) readers in both measured with single letters at 15 centimeters(cm). The patient was allowed to hold the near chart at any distance to evaluate her preferred working distance. With both eyes open using the +2.50D readers, the patient read with difficulty. The patient initially reported that she preferred using the +2.50D readers combined with an addition +2.00 D for reading. However, when tested with this, the patient was unable to hold the material at the correct distance and struggled to read. A trial frame refraction did not result in an improvement in visual acuity in the left eye but did result in an objective and subjective improvement in the right eye to 0,1 with +2.0 -1.50 x 075. Full-time wear of single vision distance glasses with polycarbonate lenses were recommended for improved clarity of vision and protection. A prescription for glasses was released to the patient. The daughter mentioned seing her falling from the stairs and hitting object while walking, therefor orientation and mobility training was discussed and strongly advised to the patient for safe navigation, and a possibility of using a cone while walking. The patient was receptive to the recommendation as she was aware of her limitations due to reduced peripheral and central vision. Private orientation and mobility instructors were also discussed, but financially difficult for the patient to pursue. We also decided to test the mother for the RPE65-mediated retinal dystrophy so she could be treated with Luxturna, but after the genetic testing performed in „Sveti duh“ clinic in Zagreb, the mother was a heterozygous for PRPF3 c.1481>T,p.(Thr495Met),which is patogenic and a heterozygous for PROM1 c.2401G>T,p.(Ala801Ser) which is a variant of uncertain significance (VUS), and not a candidate for the above mentioned treatment. Findings for the patients daughter at the examination: VOD:1,0 cc -1,0 dsph -0,75 dcyl axis 75, VOS: 0,7 cc -1,0 dsoh -1,0 dcyl axis 87; Pupils were round with brisk responses. Extraocular muscle motility was full in both eyes, optic disc round with no visible oedema but seemingly waxy C/D 0,4, macular field with visible foveal reflex, thining of the retinal perphery with low pigmented atrophic zones especially visible in the mid periphery (Figure 4a+4b+4c+4d). We decided to send the patient for an ERG where a retinal cell demage was detected, which is reflected in the reduction of amlitude and duration of the b wave especially pronounced in the late adapted 3.0 flicker response. After reviewing the OCT images of the patient’s macula and finding that there was cystoid macular edema in the outer plexiform layer, we decided to apply Triamcinolone acetate subtenonialy with a positive response subjectivly and clinicaly (Figure 5, Figure 6). After reviewing the OCT of the optic dics (Figure 7) and aplanation tonometry (TOD 23mmHg TOS 20 mmHg with no pachymetry correcting factor) we prescribed brinzolamide solution and educated the young patient about the proper application. We put an emphasis on the proper education of the daughter and mental health, as well as the importance of regular follow ups.
Figure 2. OCT scans of the macula patient No 1 (mother) -Optopol Revo nx130.
Figure 4a, 4b, 4c and 4d. Foto Fundus + autoflurescence of the patient No 2 (daughter)–Centrevue Eidon FA.
Figure 5. OCT macula of the patient No 2 (daughter) at the first examination.
Figure 6. OCT macula of the patient No 2 after applyinf Triamcinolone acetate subtenonialy.
Figure 7. OCT of the optic disc of the patient No 2 (daughter)–Optopol Revo nx 130.
Figures 1a, 1b, 1c, and 1d. Foto fundus + autofluescence of the patient no 1. (Centervue Eidon FA).
Figure 3. OCT of the patient no 1 (mother)–Optopol Revo nx 130.
5. DISCUSSION
Retinitis pigmentosa (RP) is a disease that affects to rod photoreceptors and subsequent loss of cone function in both eyes. There are more than 3,000 genetic mutations in approximately 70 known genes that are associated with RP. (2) This condition can present as an autosomal dominant, autosomal recessive, X-linked, or unknown pattern inheritance. Approximately 2.5 million people worldwide are affected by RP. There was no significant gender predilection found in literature. The pathophysiology of RP begins with rod photoreceptor degenerationand leads to cone photoreceptor degeneration as well. Mutations can occur in many processes involving the rod photoreceptors, ranging from rod visual transduction to metabolism and RNA processing. Patients with RP initially present with nyctalopia as rod photoreceptors primarily involve vision in dim illumination. Symptoms are initially noticed in dim light settings and commonly begin during adolescence. In advanced disease, patient will have central vision loss in daylight as the cones degenerate further. Eventually, all photoreceptors will be lost, leading to complete blindness. Fortunately, complete blindness was found to be rare in past studies.However, most patients with RP are classified as legally blind (20/200 or worse in the better seeing eye or 20 degrees field or less in the better seeing eye) by the age of 40.(3) One common cause of vision loss is cystoid macular edema(CME). The mechanism of CME in RP is incompletely understood with several theories proposed. One hypothesis suggests that because RP is associated with an increased prevalence of anti-retinal antibodies, CME is the result of an autoimmune reaction. This autoimmune phenomenon may explain the efficacy of steroids in the treatment of CME (4) An alternative hypothesis proposes that dysfunction of the outer blood-retinal barrier at the RPE, perifoveal capillary plexus, or both increases vascular permeability causing fluid leakage in the macula. Carbonic anhydrase inhibitors may treat CME by enhancing the pumping mechanism at the level of the RPE.(5) In addition to its anti-inflammatory properties, steroids may also work at the level of the blood-retinal barrier in RP as it has been shown experimentally to reduce breakdown of the blood-retinal barrier in diabetic retinopathy.
Diagnosis of RP is often based upon characteristic appearances, but ancillary testing can also be performed. A full-field or multifocalelectroretinogram(ERG)is often performed to confirm diagnosis. The scotopic a-and b-wave amplitudes measuring mainly rod function are reduced in all types of RP and photopic (cone) b-wave amplitudes are gradually reduced as well. Gene therapy for retinal degenerations has been an area of great research. Luxturna, voretigene neparvovec (AAV2-hRPE65v2),is the first U.S. FDA-approved gene therapy for RPE65-mediatedretinal dystrophy. Positive outcomes have included improved light sensitivity, visual fields, and mobility in dim lighting. It carries an adeno-associated virus vector containing the human RPE65 complementary DNA that is injected subretinally. Inclusion criteria consist of patients with visual acuity 20/60or worse or visual field less than 20 degrees.(6) Patients also need a confirmed genetic diagnosis of biallelic RPE65gene mutationsasthe cause of RP.Unfortunately, RP associated with RPE65 mutation has been found to be rare, approximately 2% of autosomal recessive RP.(6). Low vision rehabilitation services are crucial for patients in all stages of RP. In early stages, proper education about the disease symptoms and prognosis is critical. Keeping patients independent with low vision rehabilitation helps maintain confidence levels, emotional health, and satisfaction with life.
6. CONCLUSION
We presented two cases of retinitis pigmentosa – the mother with diagnosed RP more than 15 years ago in need for low vision rehabilitation service and the daughter that got diagnosed after our initial examination and with complications in visual impairment through cystoid macular oedema. The aim of the review was to emphasize the obligatory eduation of the patient for the now and in the future possible treatments as well as helping the patient to maintain a full and independend lifestyle.
Authors contribution:
All authors were involved in all steps of preparation this article. Finalproofreading was made by the first author.
Conflict of interest statement:
The authors report no potential conflicts of interest in the development and publication of this article.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Jaissle GB, May CA, Van De Pavert SA, et al. Bone spicule pigment formation in retinitis pigmentosa: Insights from a mouse model. Graefe’s Arch Clin Exp Ophthalmol. 2010;248(8):1063–1070. doi: 10.1007/s00417-009-1253-9. [DOI] [PubMed] [Google Scholar]
- 2.Dias MF, Joo K, Kemp JA, et al. Molecular genetics and emerging therapies for retinitis pigmentosa: Basic research and clinical perspectives. Prog Retin Eye Res. 2017 doi: 10.1016/j.preteyeres.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Wright AF, Chakarova CF, Abd El-Aziz MM, Bhattacharya SS. Photoreceptor degeneration: Genetic and mechanistic dissection of a complex trait. Nat Rev Genet. 2010;11(4):273–284. doi: 10.1038/nrg2717. [DOI] [PubMed] [Google Scholar]
- 4.Hakan O, Murat K, Serra K. Intravitreal triamcinolone acetonide for treatment of cystic macular edema in patients with retinitis pigmentosa. Acta Ophthalmol Scand. 2005;83:248–251. doi: 10.1111/j.1600-0420.2005.00395.x. [DOI] [PubMed] [Google Scholar]
- 5.Fishman GA, Gilbert LD, Fiscella RG, et al. Acetazolamide for treatment of chronic macular edema in retinitis pigmentosa. Arch Ophthalmol. 1989;107:1445–1452. doi: 10.1001/archopht.1989.01070020519031. [DOI] [PubMed] [Google Scholar]
- 6.Luxturna [package insert]. Spark Therapeutics. 2017 [Google Scholar]