Abstract
Background:
MRI techniques of the lumbar spine have not provided data on the effect of gravity on the spine and on the relationship of anatomic structures during its action. Because conventional MRI examinations of the spine are usually performed in the supine position these are often exacerbated by standing upright and are not evident in the supine position the loading conditions differ from those known to cause symptoms in patients with lumbar instability. Axial loading imaging may improve diagnostics in the clinical management of LBP and lead to appropriate treatment decisions.
Objective:
The aim of this study is to determine the significance of alMRI in detecting the morphologic changes of the lumbar spine caused by axial loading and to compare it with conventional MRI images of the lumbar spine without loading.
Methods:
The study was conducted as a prospective, descriptive clinical trial. Imaging was performed with a MRI 1.5 T in the head-first supine position. Imaging was performed in two acts: without load and under load. Loading for alMRI was performed with the DynaWell L-Spine device. The onset of loading was 10 minutes before the start of alMRI. The loading continued throughout the imaging procedure. The height of the IV, AP and LL diameters of IV, IV disk surface area, DSCA and width of the IV foraminas before and under load was measured.
Results:
After evaluating the changes in the height and size of the lumbar disks, the size of the DSCA, and the narrowing of the intervertebral foramina significant differences were found between the images before and after axial loading.
Conclusion:
alMRI provides information on morphological changes of all segments of the lumbar spine. This data represents significant information that can lead to more accurate and effective treatment of LBP.
Keywords: Weight-Bearing, Magnetic Resonance Imaging, Low Back Pain, Intervertebral Disc, Spinal Canal, Dural Sac
1. BACKGROUND
Low back pain (LBP) remains a major global health problem that has increased significantly over several decades (1). Chronic LBP is a major health problem because pain, physical harm, and pathology are weakly correlated. Experiencing pain is perceived as suffering, distracts attention, and is disabling for those affected (2).
A meta-analysis by Meucci et al (3) found that the prevalence of chronic LBP was 4.2% in individuals aged 24-39 years and 19.6% in individuals aged 20-59 years.
In addition to pain, work disability due to LBP is frequently reported and remains the leading cause of the number of years of disability (4).
The increasingly frequent occurrence of LBP, the development of chronicity, and the significant impact on work ability indicate the need to improve the system for accurate diagnosis, so that functional changes must be identified in addition to the precise determination of structural changes with standard imaging techniques (5). The high prevalence of degenerative changes in the lumbar spine, the significant disability of patients with chronic pain syndrome, and the low correlation of radiologic and clinical findings require the introduction of new examination techniques into the diagnostic algorithm (6).
To date, magnetic resonance imaging (MRI) techniques of the lumbar spine have not provided data on the effect of gravity on the spine and on the relationship of anatomic structures during its action. Because conventional MRI examinations of the spine are usually performed in the supine position, i.e., at functional rest, the loading conditions differ from those known to cause symptoms in patients with lumbar instability. These are often exacerbated by standing upright and are not evident in the supine position (7).
To simulate the upright position, clinicians and researchers have developed a series of devices that apply axial loading to the spine in the supine position (8).
Axial loading imaging may improve diagnostics in the clinical management of LBP and lead to appropriate treatment decisions (9, 10).
2. OBJECTIVES
The aim of this study is to determine the significance of axial loaded MRI (alMRI) in detecting the morphologic changes of the lumbar spine caused by axial loading and to compare it with conventional MRI images of the lumbar spine without loading.
3. MATERIAL AND METHODS
The study was conducted as a prospective, descriptive clinical trial in the period from January 1, 2017, to June 15, 2018, in the Radiology Clinic of the Clinical Center of the University of Sarajevo, involving 80 adults of both sexes. Study was approved by the Ethics Committee of the Clinical Center of Sarajevo University and by the Ethics Committee of the Faculty of Health Studies of Sarajevo University. Written informed consent for the procedure was obtained prior to the start of imaging. The criteria for inclusion in the study, in addition to written informed consent for the procedure, were that the patient had symptoms of LBP and had not been previously diagnosed with degenerative disease of the spine or lumbar disk.
Also patients who had undergone surgery on any segment of the spine and patients who had undergone hip or knee arthroplasty were also excluded from the study. Patients who experienced pain during alMRI procedure were also excluded, and loading was stopped. Imaging was performed with a Siemens Magnetom Avanto (Erlangen, Germany), 1.5 T in the head-first supine position and using a spine matrix coil. Imaging was performed in two acts: without load and under load, using the following acquisition protocol:
- T2 tse sag: TR 3370 ms, TE 110 ms, FOV 320 mm, slice tickness 4mm, number of slices 11, distance factor 10%;
- T1 tse sag: TR 552 ms, TE 12 ms, FOV 320, slice tickness 4 mm, number of slices 11, distance factor 10%;
- T2 tirm sag: TR 3200 ms, TE 78 ms, TI 160 ms, FOV 320 ms, slice tickness 4 mm, number of slices 11, distance factor 10 %,
- T2 tse cor: TR 5610, TE 180 ms, FOV 320 mm, slice tickness 4 mm, number of slices 19, distance factor 10 %;
- T2 tse tra MSMA: TR 3200-4000 ms, TE 104 ms, FOV 210, number of slabs 3, number of slices per slab 5, slice tickness 4 mm, distance factor 10%.
Loading for alMRI was performed with the DynaWell L-Spine device (DynaWell Int. AB, Billdal, Sweden). The onset of loading was 10 minutes before the start of alMRI. The loading continued throughout the imaging procedure. The spine was subjected to a load of 50% of the patient’s body mass, which was equally distributed among the legs (25% of the patient’s body mass per leg). alMRI was performed according to the following protocol:
- T2 tse sag: TR 3370 ms, TE 110 ms, FOV 320 mm, slice tickness 4mm, number of slices 11, distance factor 10%;
- T2 tse tra MSMA: TR 3200-4000 ms, TE 104 ms, FOV 210, number of slabs 3, number of slices per slab 5, slice tickness 4 mm, distance factor 10%;
After the imaging was completed, measurements were made on the console of the MR machine using the Syngo b13 software.
We measured:
- The height of the intervertebral (IV) disk L3/L4, L4/L5, L5/S1 expressed in millimeters (mm) before and under load (Image 1. a and b).
Image 1. a, b the height of the IV disk before and under load; c, d AP and LL diameters of IV disk before and under load; e, f IV disk surface area before and under load; g, h DSCA before and under load; i, j width of the IV foraminas before and under load.
- Anterio – Posterior (AP) and Latero -Lateral (LL) diameters of IV disk diameter of IV disk L3/L4, L4/L5, L5/S1 expressed in millimeters before and under load (Image 1. c and d).
- IV disk surface area L3/L4, L4/L5, L5/S1 expressed in square millimeters (mm2) before and under load (Image 1. e and f).
- The Dural Sac Cross-Sectional Area (DSCA) at the level of the L3/L4, L4/L5, L5/S1 IV disk before and under load (Image 1. g and h).
- Width of the IV foraminas in area of lumbar disk L3/L4, L4/L5, L5/S1 before and under load (Image 1. i and j).
The measurement data were entered into an individual form and then statistically analyzed. Data were processed using SPSS statistical software version 20.0.
4. RESULTS
After examining 80 respondents who met the criteria for inclusion in the study, it was found that 46 (57.5%) of the respondents were male and 34 (42.5%) of the respondents were female. The median height of the disk at the L3/L4 level before loading was 11 mm (11.3 mm–males, 10.4 mm–females). Loaded, the median height of the L3/L4 disk was 10.0 mm (10.6 mm–men, 9.6 mm–women). The difference without load and loaded was 0.75 mm on average. Using the Wilcoxon test, a significant difference in disk height was found, Z=-6.966; p < 0.001.
The median value of the height of the disk at the L4/L5 level before loading was 10.90 mm (11.25 mm–men, 10.45 mm–women). Loaded, the median height of the L4/L5 disk was 9.80 mm (9.6 mm–men, 9.8 mm–women). The difference without load and loaded was 0.87 mm on average. Using the Wilcoxon test, a significant difference in the height of the intervertebral disk was found (Z=-6.953, p < 0.001).
The median height of the disk at the L5/S1 level before loading was 10 mm (10.1 mm–men, 10.0 mm–women). Loaded, the median height of the L4/L5 disk was 9.0 mm (9.3 mm–men, 8.9 mm–women). The difference without load and loaded was 1 mm on average. Using the Wilcoxon test, a significant statistical difference was found (Z=-7.01, p < 0.001) (Table 1).
Table 1. Analysis of the height of the intervertebral disk.
| Before loading | Loaded | Z | p | |||
|---|---|---|---|---|---|---|
| IV SPACE | Median | IQ range | Median | IQ range | ||
| L3/L4 | 11.0 | 9.95-12.5 | 10.0 | 8.7-11.3 | -6.966 | <0.001 |
| L4/L5 | 10.90 | 9.8-12.3 | 9.8 | 8.75-11.2 | -6.953 | <0.001 |
| L5/S1 | 10.0 | 8.55-12.15 | 9.0 | 7.3-10.7 | -7.01 | 0.001 |
Measurement of the A-P diameter of the disk before loading and under load gave the following results:
At the L3/L4 level, the median length of the A-P diameter before loading was 41.4 mm (men 42.6 mm, women 39.3 mm),under load there was an increase to 42.3 mm (men 43.5 mm , women 39.8 mm). The average increase in A-P diameter was 0.7 mm. Using the Wilcoxon test, a significant difference was found in AP diameter before loading and under load (Z=-7.629; p < 0.001). L4/L5 level before loading, where the median length of the A-P diameter was 43.1 mm (men 45.8 mm, women 39.7 mm) and under load 44.4 mm (men 46.4 mm, women 40.8 mm). The average increase in A-P diameter was 0.90 mm. Using the Wilcoxon test, a significant difference was found in AP diameter before loading and under load (Z=-7.479; p < 0.001). L5/S1 level, where the median length of the A-P diameter before loading was 41.2 mm (men 42.7 mm, women 38.5 mm) and under load was 42.3 mm (men 43.5 mm, women 39.9 mm). The average increase in A-P diameter was 1.45 mm. Using the Wilcoxon test, a significant difference was found in AP diameter before loading and under load (Z=-7.248; p < 0.001) (Table 2).
Table 2. Analysis of the A-P diameter of the intervertebral disk.
| IV SPACE | Before loading | Loaded | Z | p | ||
|---|---|---|---|---|---|---|
| Median | IQ range | Median | IQ range | |||
| L3/L4 | 41,4 | 39,2-44,2 | 42,3 | 39,7-45,1 | -7,629 | <0.001 |
| L4/L5 | 43,1 | 39,8-46,5 | 44,4 | 40,8-47,6 | -7,479 | <0.001 |
| L5/S1 | 41,2 | 37,8-44,2 | 42,3 | 39,6-45,4 | -7,248 | <0.001 |
Measurement of the Latero-Lateral (L-L) diameter of the intervertebral disk before and with loading showed a statistically significant difference at all levels, namely:
At the L3/L4 level, the median IV disk width before loading was 58.0 mm (men 59.6 mm, women 54.6 mm) and loaded was 59.20 mm (men 60.2 mm, women 55.9 mm). The increase in IV disk width averaged 1.2 mm. Using the Wilcoxon test, a significant statistical difference was found (Z=-7.577; p < 0.001). L4/L5 level before loading, where the median disk width was 60.1 mm (men 61.5 mm, women 56.3 mm) and loaded 61.4 mm (men 62.5 mm, women 57.1 mm ). The increase in IV disk width averaged 1.30 mm. Using the Wilcoxon test, a significant statistical difference was found (Z=-7.679; p < 0.001).
L5/S1 level before loading, where the median IV disk width was 57.5 mm (males 58.0 mm, females 55.2 mm) and loaded 58.3 mm (males 59.0 mm, females 56.1 mm). The increase in IV disk width at this level averaged 0.85 mm. Using the Wilcoxon test, a significant statistical difference was found (Z=-7.632; p < 0.001) (Table 3).
Table 3. Analysis of the L-L diameter of the intervertebral disk.
| Before loading | Loaded | Z | p | |||
|---|---|---|---|---|---|---|
| IV SPACE | Median | IQ range | Median | IQ range | ||
| L3/L4 | 58,0 | 55,3-60,7 | 59,2 | 56,1-62,0 | -7,577 | <0.001 |
| L4/L5 | 60,1 | 56,3-62,5 | 61,4 | 57,4-63,5 | -7,679 | <0.001 |
| L5/S1 | 57,5 | 54,3-61,5 | 58,3 | 54,9-62,7 | -7,632 | <0.001 |
Measurement of the surface area of the IV disk also shows statistically significant differences at all levels, namely: at the L3/L4 level, where the median surface area before loading was 204.9 mm2 (men 213.1 mm2, women 180.7 mm2). Under load, the surface area was 211.25 mm2 (men 221.05 mm2, women 185.25 mm2). The increase in disk surface area at the L3/L4 level averaged 6.35 mm2. Using the Wilcoxon test, a significant difference in disk surface area was found at level L3/L4 (Z=-7.588; p < 0.001).
Level L4/L5, where the median surface area before loading was 212.15 mm2 (men 225.10 mm2, women 176.50 mm2). Loaded the median surface area increased to 221.0 mm2 (men 232.8 mm2, women 182.7 mm2). The increase in disk surface area at the L4/L5 level averaged 8.5 mm2. A significant statistical difference was found (Z=-7.588; p < 0.001).
Level L5/S1, where the median IV disk area surface before loading was 185.75 mm2 (men 202.55 mm2, women 164.80 mm2). Loaded, the disk surface area increased to 196.7 mm2 (men 210.2 mm2, women 173.6 mm2). The difference before and after loading averaged 10.95 mm2. A significant statistical difference was found in the surface area of the IV disk (Z=-7.506; p < 0.001) (Table 4).
Table 4. Analysis of the IV disk surface area.
| IV SPACE | Before loading | Loaded | Z | p | ||
|---|---|---|---|---|---|---|
| Median | IQ range | Median | IQ range | |||
| L3/L4 | 204.9 | 183.4-227.95 | 211.25 | 187.4-235.85 | -7.583 | <0.001 |
| L4/L5 | 212.15 | 178.4-236.15 | 221.0 | 182.7-247.45 | -7.588 | <0.001 |
| L5/S1 | 185.75 | 161.95-219.85 | 196.7 | 166.8-226.1 | -7.506 | <0.001 |
DSCA at the level of the intervertebral disks at the L3/L4, L4/L5, and L5/S1 levels is statistically significantly smaller in images acquired with ALMRI technique.
At L3/L4 level before loading the median DSCA was 16.05 mm2 (men 16.74 mm2, women 14.47 mm2), and loaded 13.9 mm2 (men 14.5 mm2, women 12.4 mm2). The reduction in DSCA averaged 2.15 mm2. Using the Wilcoxon test, a significant difference was found between preload and loaded values (Z=-7.772; p < 0.001);
At L4/L5 level before loading the median DSCA was 13.90 mm2 (males 13.45 mm2, females 14.30 mm2), and loaded 10.8 mm2 (males 11.3 mm2, females 10 mm2) The reduction in DSCA averaged 2.8 mm2. Using the Wilcoxon test, a significant statistical difference was found (Z=-7.682; p < 0.001).
At L5/S1 level before loading the median area was 12.7 mm2 (12.6 mm2 males, 13.3 mm2 females), and loaded 11.0 mm2 (10.7 mm2 males, 11.4 mm2 females). The reduction in DSCA averaged 1.7 mm2. A significant statistical difference was determined using the Wilcoxon test (Z=-7.682; p < 0.001) (Table 5).
Table 5. Analysis of the of the DSCA.
| Level of DSCA | Before loading | Loaded | Z | p | ||
|---|---|---|---|---|---|---|
| Median (mm2) | IQ range (mm2) | Median (mm2) |
IQ range (mm2) | |||
| L3/L4 | 16,05 | 11,10-19,15 | 13,9 | 9,9-17,1 | -7.772 | <0.001 |
| L4/L5 | 13,90 | 9,90-17,40 | 10,8 | 7,8-15,5 | -7.388 | <0.001 |
| L5/S1 | 12,7 | 9,4-21,4 | 11,0 | 6,9-18,5 | -7.682 | <0.001 |
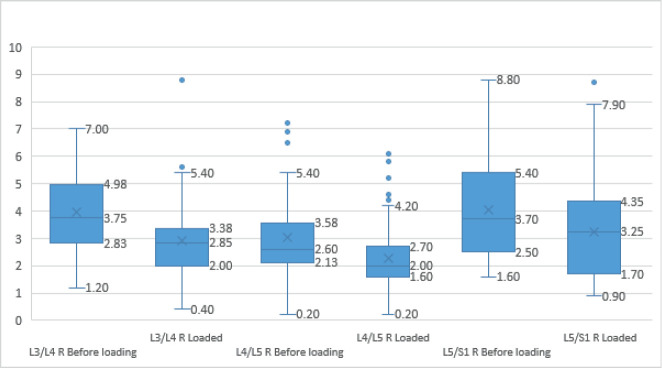
The analysis showed that the width of the right IV foramen at the L3/L4 level decreased under loading, so that the median width of the foramen before loading was 3.75 mm (2.83 mm-4.98 mm), whereas under loading it was 2.85 mm (2.0 mm-3 .38 mm). A significant statistical difference was found (p < 0.001).
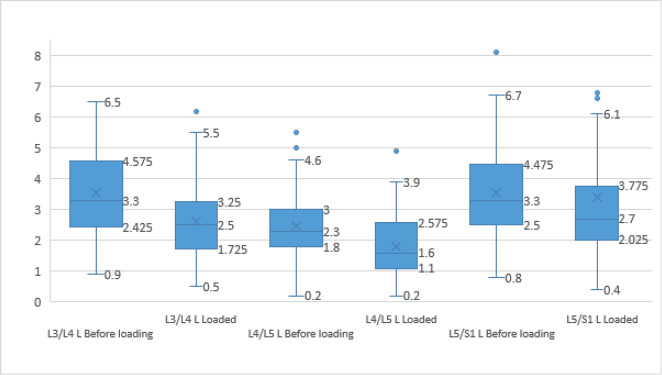
Graph 1. Analysis of the width of the right IV foraminas.
Graph 2. Analysis of the width of the right IV foraminas before and after loading.
The width of the right IV foramen at L4/L5 level had a median value of 2.6 mm (2.2 mm -3.6 mm) before loading and 2.0 mm (1.6 mm-2.7 mm) under loading. A significant statistical difference was found (p < 0.001).
The width of the right IV foramen between L5/S1 had a median value of 3.7 mm (2.5 mm-5.4 mm) before loading, while the width of the IV foramen had a median value of 3.3 mm (1.7 mm-4.3 mm) under loading. A significant statistical difference was found (p < 0.001) (Graph 1).
The analysis showed that the width of the left IV foramen at the L3/L4 level decreased under loading, so that the median width of the foramen before loading was 3.30 mm (2.43 mm–4.58 mm), while under loading it was 2.50 mm (1.73 mm–3 ,25 mm). A significant statistical difference was found (p < 0.001).
The width of the left IV foramen at the L4/L5 level had a median value of 2.30 mm (1.80 mm–3 mm) before loading and 1.6 mm (1.10 mm–2.58 mm) under loading. A significant statistical difference was found (p < 0.001).
The width of the left IV foramen between L5/S1 had a median value of 3.3 mm (2.50 mm–4.48 mm) before loading, while the width of the IV foramen had a median value of 2.70 mm (2.03 mm–3.78 mm) after loading. A significant statistical difference was found (p < 0.001). (Graph 2.).
5. DISCUSSION
MRI is the most widely accepted imaging modality for the evaluation of lumbar spine pathology, especially in patients with low back pain, sciatica, and neurogenic claudication. These symptoms are usually caused by excessive standing or walking, so imaging in a symptomatic position can provide much more information than when the psoas muscle is relaxed in a neutral position. Under ideal conditions, imaging in a standing position would be optimal because of the normal gravitational pressure on the spine. However, this imaging position is impractical because it requires the patient to stand completely motionless for approximately 30 minutes (11).
alMRI of the lumbar spine was introduced to simulate physiologic loading of the spine in the standing position to improve the diagnostic performance of MRI, which is usually performed in the supine position (12).
The biomechanics of the lumbar spine lead to changes in the diameter of the spinal canal during sitting and standing (13).
Evaluation of physiological and biomechanical elements of the lumbar spine shows significant differences between imaging before and after axial loading. Umberto Tarantino et al (14) found a statistical significance of p < 0.01 in the reduction of disk height at all measurement levels. Apart from the fact that we obtained similar results to those authors, and in addition, it should be emphasized that they had oportunity to make imaging in a real standing position (they used a permanent MRI system 0.25T Esaote G- SCAN, which offers the possibility of placing the gantry in a vertical position), and the possibility of measuring the real effect of the gravitational force on the whole body, we found that it is possible to simulate the gravitational force using auxiliary devices, which does not affect the biomechanics of the lumbar spine. By reducing the height of the intervertebral space, the disk surface area increases and DSCA decreases. During alMRI, the loading conditions are different from physiological upright loading, however, the loading applied during alMRI was chosen according to the in vivo disk pressure measurements in the upright, unloaded position. In terms of influences on the intervertebral disk, alMRI has similar effects to physiological spinal loading in the upright position (15)
In our study, there is significant narrowing of the dural sac at all levels. In similar studies, it has been confirmed that the DSCA decreases significantly at all levels when comparing the condition of the lumbar spine before and with axial loading. In the present study, it was shown that the width of facet fluid significantly correlated with the change in DCSA caused by axial loading (16, 17). The cross-sectional areas in alMRI were significantly smaller than those in conventionalMRI (18).
Statistically significant differences were found at all levels when measuring the width of the intervertebral foramina before loading and under loading. Compared with conventional imaging methods, alMRI can result in a reduction in foraminal area, reveal foraminal stenosis that cannot be detected by conventional methods, and accurately assess the severity of foraminal stenosis. It is of clinical value in improving the diagnosis of foraminal stenosis (19).
alMRI of lumbar spine offers a new type of functional imaging and a perspective for studying the physiology and pathophysiology of degenerative processes. This technique allows assessment of almost all structures of the vertebral motor segments and their positional relationship to the anatomical structures of the spinal canal and intervertebral foramen. In addition, this method can be used to identify signs of instability of soft tissue structures of the spine and compression of neural structures during axial loading (20).
MRI with axial loading can provide more information about the alignment of the spine, the height of the intervertebral disks and the width of the spinal canal. This information can explain the patient’s symptomatology and significantly change the treatment plan accordingly. Patients with clinical symptoms that could not be explained by conventional supine MRI may benefit from alMRI, which can provide additional information that may affect the future treatment plan (21).
6. CONCLUSION
alMRI provides information on morphological changes of all segments of the lumbar spine. This data represents significant information that can lead to more accurate and effective treatment of LBP.
Author’s contribution
All authors were involved in writing of this article and they all accepted responsibility for the entire content of this submitted manuscript and approved submission.
Conflict of interest:
The authors report no conflicts of interest.
Financial support and sponsorship:
None.
REFERENCES
- 1.Clark S, Horton R. Low back pain: a major global challenge. Lancet. 2018;391:2302. doi: 10.1016/S0140-6736(18)30725-6. [DOI] [PubMed] [Google Scholar]
- 2.Osborn M, Smith JA. The Personal Experience of Chronic Benign Lower Back Pain: An Interpretative Phenomenological Analysis. British Journal of Pain. 2015;9:65–83. doi: 10.1177/2049463714541642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meucci RD, Fassa AG, Faria NMX. Prevalence of chronic low back pain: systematic review. Revista de Saúde Pública. 2015;49:1. doi: 10.1590/S0034-8910.2015049005874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hurwitz EL, Randhawa K, Yu H, Côté P, Haldeman S. The Global Spine Care Initiative: a summary of the global burden of low back and neck pain studies. Eur Spine J. 2018;27:796–801. doi: 10.1007/s00586-017-5432-9. [DOI] [PubMed] [Google Scholar]
- 5.Drake RL, Vogl WA, Mitchell AWM. Canada: Churchill livingstone elsevier; 2015. Grays anatomy for students, 3th edition. [Google Scholar]
- 6.Bazhin AV, Egorova EA, Novoselova EV, Vasiliev YA, Pakhomov GA, Berkutov ES, Durov AN. Methods of magnetic resonance imaging with axial load for assessment of lumbarspine under normal and degenerative changes. MIA Medical Bulletin. 2015;74:49–54. [Google Scholar]
- 7.Muto M. Update on Spine Imaging. Magn Reson Imaging Clin N Am. 2016;24(3):485–648. doi: 10.1016/j.mric.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Hiwatashi A, Danielson B, Moritani T, et al. Axial loading during MR imaging can influence treatment decision for symptomatic spinal stenosis. AJNR Am J Neuroradiol. 2004;25:170–174. [PMC free article] [PubMed] [Google Scholar]
- 9.Sasani H, Solmaz B, Sasani M, Vural M, Ozer AF. Diagnostic Importance of Axial Loaded Magnetic Resonance Imaging in Patients with Suspected Lumbar Spinal Canal Stenosis. World Neurosurg. 2019;127:e69–e75. doi: 10.1016/j.wneu.2019.02.091. [DOI] [PubMed] [Google Scholar]
- 10.Lorenc T, Palczewski P, Wójcik D, Glinkowski W, Gołębiowski M. Diagnostic Benefits of AxialLoaded Magnetic Resonance Imaging Over Recumbent Magnetic Resonance Imaging in Obese Lower Back Pain Patients. Spine. 2018;43:1146–1153. doi: 10.1097/BRS.0000000000002532. [DOI] [PubMed] [Google Scholar]
- 11.Heba IA, Alaa S. Lumbar spine MRI axial loading in patients with degenerative spine pathologies: Its impact on the Radiological findings and treatment decision. The Egyptian Journal of Radiology and Nuclear Medicine. 2015;46(4):1065–1069. [Google Scholar]
- 12.Lorenc T, Palczewski P, Wójcik D, Glinkowski W, Gołębiowski M. Diagnostic Benefits of Axial-Loaded Magnetic Resonance Imaging Over Recumbent Magnetic Resonance Imaging in Obese Lower Back Pain Patients. SPINE. 2018;43(16):1146–1153. doi: 10.1097/BRS.0000000000002532. [DOI] [PubMed] [Google Scholar]
- 13.Coulier B. Evaluation of lumbar canal stenosis: decubitus imaging methods versus flexion-myelografphy and surface measurements versus the diameter of the dural sac. JBR-BTR. 2000;83(2):61–67. [PubMed] [Google Scholar]
- 14.Tarantino U, Fanucci I, Iundusi R, Celi M, Altobelli S, Gasbarra E, Simonetti G, Mananeti G. Journal orthopaediae and traumatologiae. Vol. 14. Springer; 2013. Lumbar spine in upright position for diagnostic of acute and cronic low back pain:statistical analysis of morphological changes; pp. 15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hebelka H, Brisby H, Hansson , T. Comparison between pain at discography and morphological disc changes at axial loaded MRI in patients with low back pain. European Spine Journal. 2014;23(10):2075–2082. doi: 10.1007/s00586-014-3408-6. [DOI] [PubMed] [Google Scholar]
- 16.Kanno H, Ozawa H, Koizumi Y, Morozumi N, Aizawa T, Itoi , E. Increased Facet Fluid Predicts Dynamic Changes in the Dural Sac Size on Axial-Loaded MRI in Patients with Lumbar Spinal Canal Stenosis. American Journal of Neuroradiology. 2015;37(4):730–735. doi: 10.3174/ajnr.A4582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanno H, Aizawa T, Ozawa H, Koizumi Y, Morozumi N, Itoi , E. An increase in the degree of olisthesis during axial loading reduces the dural sac size and worsens clinical symptoms in patients with degenerative spondylolisthesis. The Spine Journal. 2018;18(5):726–733. doi: 10.1016/j.spinee.2017.08.251. [DOI] [PubMed] [Google Scholar]
- 18.Kanno H, Endo T, Ozawa H, Koizumi Y, Morozumi N, Itoi E, Ishii Y. Axial Loading During Magnetic Resonance Imaging in Patients With Lumbar Spinal Canal Stenosis. Spine. 2012;37(16):E985–E992. doi: 10.1097/BRS.0b013e31821038f2. [DOI] [PubMed] [Google Scholar]
- 19.Liu Q.Y, Liang B.L, Chen J.Y. Effect of axially loaded MSCT on the intervertebral foramina. Chinese Journal of Medical Imaging Technology. 2007;23(9):1382–1385. [Google Scholar]
- 20.Bazhin AV, Egorova EA, Kozlov AE. The use of weight-bearing Magnetic Resonance Imaging in Lumbar Spine Examination. Radiology - practice. 2014;2:6–14. [Google Scholar]
- 21.Bulja D, Strika J, Jusufbegović M, Bečirčić M, Šehić A, Julardžija F, Beganović A, Zukić F, Vegar-Zubović S. Effects of axial loaded magnetic resonance imaging of lumbar spine on dural sac and lateral recesses. JHSCI. 2021;11(3):181–185. [Google Scholar]