Abstract
Background/Introduction:
Food allergy (FA) management involves avoiding allergenic foods to prevent an adverse reaction. Affected individuals spend substantial amounts of time thinking about food and the impact it has on their bodies. As such, we posit sustained awareness of food choices may contribute to distorted body image and disordered eating. We performed a narrative review to glean insight into associations between FA, body image and eating disorders.
Methods:
A literature search of Scopus, PsycINFO, PubMed and Google Scholar was conducted connecting terms for “food allergy” with terms for “body image” and “eating disorders”. Title and abstract screening were independently performed by two reviewers, with relevant abstracts carried forward to full text screening.
Results:
159 articles were eligible for full text screening and a total of 12 publications were ultimately included in this narrative review, and 1 article from the grey literature. Adolescents and adults both reported feeling as though their bodies were “defective” and were found to have integrated their FA as a stable facet of their identities. In addition, FA was overwhelmingly associated with prevalence of eating disorders and eating disorder-like symptoms. Disturbed body image was found to be a mediating variable for the development of disordered patterns of eating in food allergic individuals.
Limitations:
Few studies appeared to consider comorbidities as confounders. Also, many studies employed convenience sampling, which does limit generalizability of conclusions.
Discussion/Conclusion:
Based on a small body of literature, there appears to be a potential association between FA and distorted body image and disordered eating.
Keywords: Allergies, Anorexia nervosa, Avoidant/restrictive food intake disorder, Body image, Bulimia nervosa, Eating disorder, Food allergy
1. Introduction
With an estimated prevalence of 6–8% in Western countries (Clarke et al., 2020), the number of people affected by food allergy (FA) is at an all-time high. FA is an umbrella term used to describe an adverse immune response to the ingestion of foods (Johansson et al., 2004). There exists a broad spectrum of disease, characterized by mechanism of reactivity and severity of immunologic response, ranging from mild (involving the skin or upper airways) to severe and potentially fatal (Johansson et al., 2004).
FA is a chronic condition that necessitates major lifestyle changes, such as strict avoidance of offending allergens, and a perpetual awareness of all foods consumed. Previous research has shown that a diagnosis of, or suspected FA can be very difficult to cope with and may hinder quality of life (Protudjer et al., 2016; Thörnqvist et al., 2019). In recent years, more consideration has been given to identifying the ways FA can impact an individual. For example, from a nutritional perspective over 90% of Immunoglobulin E (IgE)-mediated food allergies are caused by eight common allergens: eggs, peanuts, cow’s milk, soy, tree nuts, shellfish, fish, or wheat, it is quite plausible that nutrition is impacted (Sicherer & Sampson, 2018). Notably, these are also common foods, and as such, those with FA may be at increased risk of specific macronutrient deficiencies (Hildebrand et al., 2019) insufficient energy intake (Venter et al., 2008; Mehta et al., 2013), and impaired growth indices (Meyer et al., 2019).
In addition to the physical consequences of allergic reactions, FA may also have social and emotional consequences, (Patel et al., 2017) including anxiety and depression (Polloni & Muraro, 2020; Singer et al., 2020). Food allergic individuals and their caregivers regularly report decreased quality of life and increased feelings of anxiety, often due to the constant vigilance surrounding food choice (An Update on the Impact of Food Allergy on Anxiety and Quality of Life, 2017). Although these behaviours mandate that affected individuals must always consider food choices, the intersection of these behaviours with disturbed eating and body image disturbance is incompletely understood.
Disturbed attitudes towards diet and eating in a non-food allergic population have been extensively explored (de Portela Santana et al., 2012). Published in 2013, the updated Diagnostic and Statistical Manual of Mental Disorders (DSM-5) characterizes feeding and eating disorders as a “persistent disturbance of eating or eating-related behaviours that results in altered consumption or absorption of food and that significantly impairs physical health of psychosocial functioning” (American Psychiatric Association, 2013). Diagnostic criteria have been provided for classical eating disorders such as anorexia nervosa and bulimia nervosa in addition to recognizing several new disorders, such as Avoidant/Restrictive Food Intake Disorder, Binge Eating Disorder and Unspecified Feeding or Eating Disorder. A systematic review published in 2019 estimates a lifetime prevalence of eating disorders to be 8.4% for woman and 2.2% for men, with a peak incidence in adolescence (Galmiche et al., 2019). One further consideration is that the hallmark of many eating disorders is the presence of body image disturbance. Body image, which can be defined as “the picture we have in our minds of the size, shape and form of our bodies and our feelings concerning these characteristics” (Slade, 1994) has been shown to influence many areas of life, including self-esteem and mood. Body image disturbance is a core psychopathological symptom in the DSM-5 for the diagnosis of anorexia nervosa but may be present in any of the eating disorders (American Psychiatric Association, 2013). As such, body image disturbance can negatively alter the way one thinks, feels, and behaves in their social or occupational lives; and is one proposed mechanism for the development of clinical and subclinical patterns of dietary restriction or eating disorders (Alexi et al., 2019).
Amongst both adolescents and adults, patterns of dietary restriction in general are strongly associated with an increased incidence of eating disorders including anorexia nervosa and bulimia nervosa (Keski-R-ahkonen & Mustelin, 2016; Kaye et al., 2000). In fact, a significant diagnostic feature of these eating disorders is the existence of restricted patterns of eating. Given that the cornerstone of FA management is this very type of diet modification, it is difficult to ignore the potential for an increased risk of dietary pathology. The aim of this narrative review is to examine the existing literature on the possible association between food allergies and eating disorders or body image disturbance.
2. Methods
2.1. Search Strategy and Inclusion Criteria
For this narrative review, we searched the literature for publications in four databases – Scopus, PsycINFO, PubMed and Google Scholar. Student investigators also scanned the first 10 pages of 6 relevant grey literature sites – Canadian Paediatric Society, American Academy of Pediatrics, Australian Pediatric Society, American Academy of Asthma, Allergies and Immunology and The Canadian Society of Allergy and Clinical Immunology. Our search strategy included the terms “food allergies” or “food hypersensitivity” connected with the terms for “body image” and/or “eating disorders”. Publications were included if they were published in English and considered the association between FA and the development of disordered eating and/or body image disturbance in human subjects. We imposed no restrictions on country of publication, study design or age of participants.
Publications identified through this search process were imported into the citation manager Mendeley and deduplicated before they were exported into Rayyan.qrci. After reviewer calibration, two student investigators (SJ, TLF) independently screened for relevance based on title/abstract. Publications deemed relevant were advanced to full text screening, likewise, independently performed by the same two student investigators. Conflicts resulting from full text screening were managed by these student investigators and the senior author.
2.2. Data Extraction
Data from publications deemed to be relevant subsequent to full text screening were independently extracted by the two student investigators. Specifically, they extracted the titles and year of publication, names of authors and journal, demographic data on the study population, study aim, and definitions of body image, disordered eating and FA, as well as directions for future research/gaps in the literature.
3. Results
Through our search, as represented in Fig. 1 and Table 1 - we identified 3033 potentially relevant articles following de-duplication, which underwent title and abstract screening. Of these, 2990 were excluded for reasons including failure to mention body image/disordered eating, inappropriate directionality of the relationship being studied, or did not meet goals of the review. Thus, a total of 159 articles were eligible for full-text screening. Of these, 9 were excluded because investigators were unable to obtain the full text (Ackerman, 2009; Bartek, 1988; De Asis & Simon, 2009; DunnGalvin et al., 2015; Herbert, 2012; Markus, 2019; Miller, 1995; Molloy and Hourihane, 2008; Health-Related Quality of Life in Children with Food Allergy and Their Parents: A Systematic Review of the Literature, 2014; Reading, 2009; Saperstein, 2010). An additional 130 were further excluded due to irrelevance of reported outcomes or failure to meet goals of the review. This left a total of 12 publications that were ultimately included in this narrative review, and 1 article from the grey literature. Of these 13 articles, 7 mentioned FA and body image, and 6 addressed the relationship between FA and eating disorders. 3 of the studies described subjects with IgE-mediated food allergies, 2 described subjects with eosinophilic esophagitis managed by dietary restriction, and 8 described subjects with either self-reported or physician diagnosed adverse reaction after ingestion of a specific food.
Fig. 1.
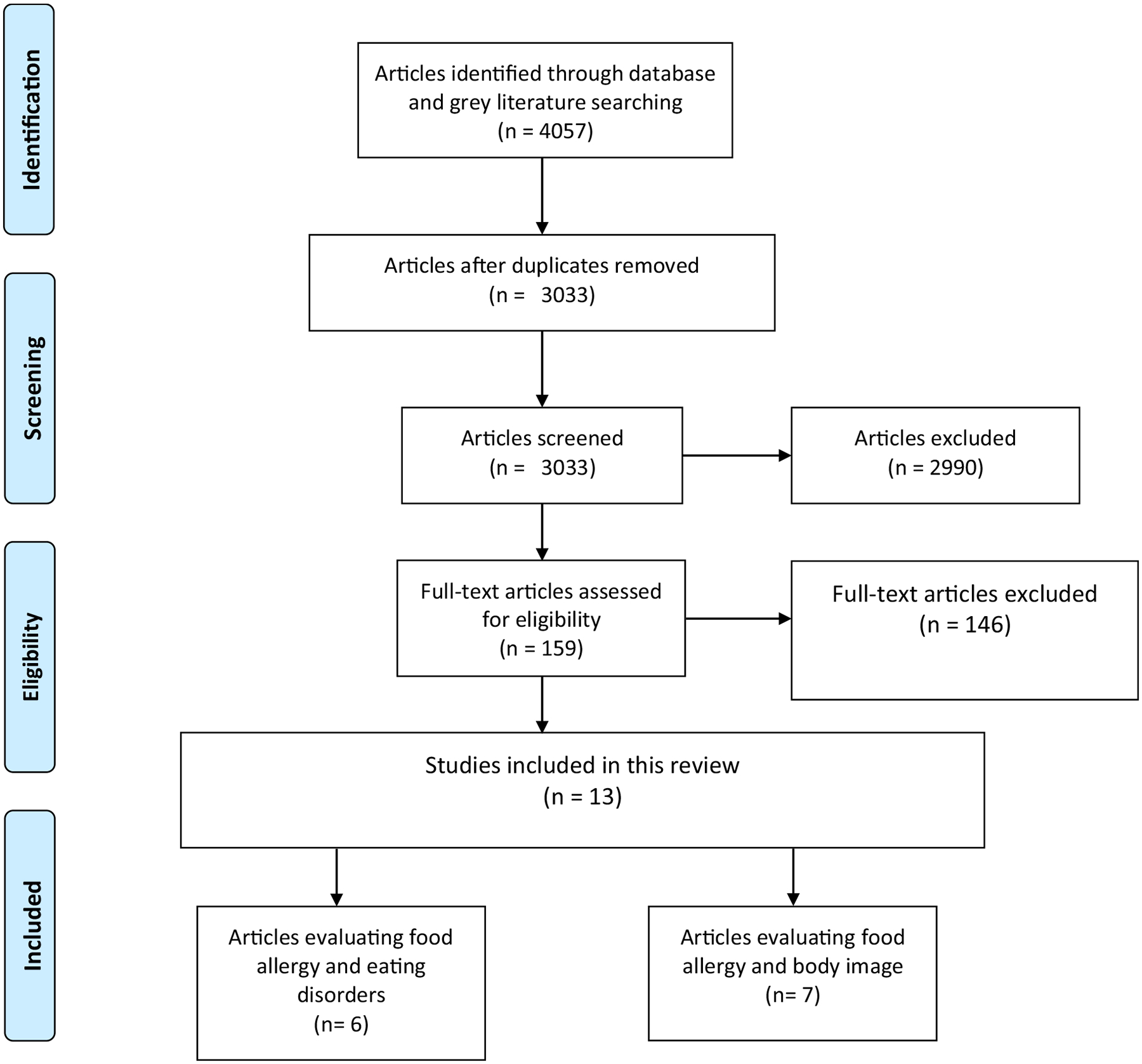
Prisma Flowchart Detailing Identification, Screening and Selection of Eligible Papers Included in This Narrative Review
Table 1.
Summary of Included Papers Reporting on FA, and Body Image or Eating Disorders.
| Body Image | ||||||||
|---|---|---|---|---|---|---|---|---|
| First Author (Year) | Country or Continent | Primary Objective | Design | Sample Size (n) | Demographic Characteristics | Outcomes relevant to Food Allergy | Evidence of Association with Food Allergy | |
| 1 | Marklund (2007) | Sweden | Illuminate adolescents’ experiences of being food hypersensitive | Qualitative | 17 | Adolescents (14–18) 10 Females 7 Males |
Adolescents expressed that they felt “something was wrong with their bodies” and did not consider themselves as having a disease. Their condition had become a constructive part of their identity and felt themselves a bother in relation to others. | yes |
| 2 | Sommer (2014) | United Kingdom | Gain insight into the food choice behaviour of food-allergic teenagers, from their own perspective | Qualitative | 25 | Adolescents | All teenagers from both groups had substantial knowledge of healthy foods and considered healthy eating to be important for well-being and positive body image. Teenagers with food allergies did not show a different attitude towards healthy eating than their non-allergic peers. Teenagers with food allergies found it more difficult to be adventurous with new foods than non-food allergic teenagers. Almost all teenagers liked to eat meals in the company of others should they feel comfortable with them. This was primarily true for food-allergic teenagers who did not want attention drawn to their allergy in front of other people. | yes |
| 3 | Evans (2012) | United Kingdom | 1. Parental experience of having a young child with severe food allergy 2. Perceptions of the effect that food allergy has on the family relationships 3. Managing the challenges associated with food allergy |
Qualitative | 8 | Participants were reluctant to let their child be defined by their allergy, and felt they had a pivotal role in the formation of the child’s positive self concept. Though safety was important, this had to be balanced with other aspects of the child’s identity | yes | |
| 4 | Flokstra-de Blok et al. (2010) | Netherlands | To compare generic HRQL of food allergic patients with the general population and other diseases. | Comparative | 225 | Children (79) Adolescents (74) Adults (72) |
Adolescents with DM scored significantly higher on to the scale(s) ‘self-esteem’ (SE) (P = 0.014) than those with food allergy, indicating poorer HRQL for food allergic adolescents than diabetic adolescents food allergic patients reported poorer HRQL than the general population and that the generic HRQL impact of food allergy is intermediate in magnitude between DM and RA, asthma and IBS. | yes |
| 5 | Östblom (2008) | Sweden | Study the impact of food hypersensitivity in children on health related quality of life | Nested Case Control Study | 1378 | 9 year old children with food allergy (n = 212) and without food allergy (n = 802) | The subscales concerning behaviour (BE), self esteem (SE) (Satisfaction with school, athletic ability, appearance, ability to get along with others), parental impact - time (PT) and family activities (FA) were not influenced by FHS | No |
| 6 | Peniama (2014) | New Zealand | Identify and better understand the issues that affect the quality of life of food-allergic adults and to identify strategies to improve their quality of life. | Qualitative | 29 | Male = 6 Female = 23 |
A majority of the participants discussed the effects of having a food allergy on self-image in terms of feeling isolated, embarrassed, or defective. | Yes |
| 7 | Wróblewska (2018) | Poland | compare the prevalence of symptoms of ED in underage patients with immunologically confirmed, long- duration FA and in healthy peers, as well as to assess which of the additional sociodemographic, environmental and biological variables can have an influence on this phenomenon. | Comparative | 89 | Mean age: 5.9 SES Unknown/Unreported Female = 55.6% |
These findings suggest that participants with FA especially struggling with lack of confidence in FA issues and those following an uncontrolled, restrictive elimination diet are more prone to food aversion and ED than their healthy peers. Applied procedures are necessary, and their neglect is associated with FA deterioration; however, the possibility of ED and biopsychosocial implications development should not be underestimated. | Yes |
| 6 | Peniama (2014) | New Zealand | identify and better understand the issues that affect the quality of life of food-allergic adults and to identify strategies to improve their quality of life. | Qualitative | 29 | A majority of the participants discussed the effects of having a food allergy on self-image in terms of feeling isolated, embarrassed, or defective. | Yes | |
| 7 | Wróblewska (2018) | Poland | Compare the prevalence of symptoms of ED in underage patients with immunologically confirmed, long- duration FA and in healthy peers, as well as to assess which of the additional sociodemographic, environmental and biological variables can have an influence on this phenomenon. | Comparative | 89 | Mean age: 5.9 Female = 55.6% |
These findings suggest that participants with FA especially struggling with lack of confidence in FA issues and those following an uncontrolled, restrictive elimination diet are more prone to food aversion and ED than their healthy peers. Applied procedures are necessary, and their neglect is associated with FA deterioration; however, the possibility of ED and biopsychosocial implications development should not be underestimated. | Yes |
| Eating Disorders | ||||||||
|---|---|---|---|---|---|---|---|---|
| First Author (Year) | Country or Continent | Primary Objective | Design | Sample Size (n) | Demographic Characteristics | Outcomes | Association with Food Allergy | |
| 1 | Shanahan (2014) | USA | Determine whether adolescents with food allergies are at increased risk for psychopathology—concurrently and over time | Cross Sectional | 1420 | Adolescents and Parents | Cross- sectionnally, food allergies were associated with more symptoms of anorexia nervosa. Food allergies were not, however, associated with a higher likelihood of meeting diagnostic criteria for a psychiatric disorder. On average, youth with food allergies had one more symptom of any psychopathology compared with those without food allergies controlling for comorbidity (i.e., other psychopathology symptom scales), separation anxiety and anorexia symptoms continued to be associated with food allergies at p < .05. | Yes |
| 2 | Robson (2019) | USA | Report two cases of disordered eating associated with EoE therapy | Case Study | 2 | children age 3, and 13, both male gender SES unreported | Abruptly changing food content and diversity in children with EoE, particularly those with a history of severe symptoms, feeding difficulties or mental health disease, may have untoward consequences | Yes |
| 3 | Lieberman (2019) | Canada | Examine the medical and psychological characteristics of children under the age of 13 years with avoidant restrictive food intake disorder (ARFID) and anorexia nervosa (AN) from a Canadian tertiary care pediatric eating disorders program | Comparative | 106 | Children (8–13 years old) Male = 24.1% Female = 75.9% SES not reported |
Patients with avoidant restrictive food intake disorder (ARFID) were more likely to have allergies (4.1%) compared to those with Anorexia Nervosa. The number of patients diagnosed with food allergies was 12.3% (n = 13), which is higher than the prevalence observed in the general child population No significant differences were found in diagnosed food allergies between children with ARFID and AN. |
Yes |
| 4 | Fitzgerald (2017) | Australia | Provide preliminary data on the prevalence and nature of food avoidance and restriction in an adult population, and to explore the reasons for this behaviour. | Descriptive Cross Sectional | 102 | Adults (aged 18–79) Male = 31 Female = 70 |
The fear of aversive conse- quences, especially perceived food intolerance and allergy, are significant reasons for this disordered eating. These motivations are particularly significant within certain populations, specifically patients attending a general immunology clinic and females. |
Yes |
| 5 | Presnell (2020) | USA | To determine a potential link between ARFID and food allergy | Qualitative Interview and Chart Review | 54 | Parents of Children with Food Allergy | Avoidant-Restrictive Food Intake Disorder (ARFID) could be a comorbidity associated with food allergy. | Yes |
3.1. Studies considering FA and Body Image
Of the seven included studies on FA and body image, four employed qualitative methods; primarily semi-structured interviews and/or focus groups. Three studies used quantitative methods, including one case-control study (Östblom et al., 2008), and two comparative studies (Flokstra-de Blok et al., 2010; Wróblewska et al., n.d.). All seven studies were published between 2007 and 2019. Five of the studies were conducted on children or adolescents, and two were conducted on an adult population, however a notable difference is that one of the adult studies involved mothers of food allergic children, rather than adults who were food allergic themselves (Evans & Rouf, 2014). All studies were conducted in either European countries or New Zealand.
A qualitative study comparing food allergic individuals to healthy controls revealed that adolescents with FA, as well as non-food allergic adolescents “considered healthy eating to be important for well-being and positive body image”(Sommer et al., 2014).
In the course of this work, we were able to find that all studies employing qualitative interviews demonstrated one unmistakable theme: individuals with FA had integrated their chronic illness into part of their identity (Marklund et al., 2007), and often reported feeling inadequate or insufficient as a result (Peniamina et al., 2014). One study using both focus groups and individual interviews uncovered that adolescents felt as though there was ““something wrong” with their body, [and] did not consider themselves as having a disease”. Instead, adolescents believed their allergies were the result of intrinsic defects rather than external illness: “The body is insufficient: The adolescents believed that the food-hypersensitive body was insufficient. Something was missing, or there was a deformity, often explained as being genetic. Words like “defect”, “short-circuit”, “misinterpretation” and “mistake” were used to explain the insufficiency” (Marklund et al., 2007). This finding was mirrored in the adult study, where participants also discussed the effects of having a FA on self-image in terms of “feeling isolated, embarrassed, or defective” (Peniamina et al., 2014).
Another finding came from a comparative study in which health-related quality of life (HRQL) responses were measured from a survey taken by individuals with FA as well as cohorts of individuals afflicted with diabetes mellitus, asthma, irritable bowel syndrome, and rheumatoid arthritis (Fitzgerald & Frankum, 2017). In this study, adolescents with type 2 diabetes mellitus scored significantly higher on to the scale for ‘self-esteem’ (p=0.014) than those with FA, indicating poorer HRQL for adolescents with FA than adolescents with diabetes. Another qualitative investigation determined that a mother’s experience of her child’s allergy may also mediate the development of body image disturbance (Rouf et al., 2012). In this study, mothers were “reluctant to let their child be defined by their allergy, and felt they had a pivotal role in the formation of the child’s positive self-concept”.
Despite most publications suggesting a clear association between FA and body image disturbance, there was one case control study that did not describe this trend. Parents of 1378 nine-year-old children, 212 with reported food hypersensitivity - completed a questionnaire designed to elucidate the impact of food hypersensitivity on HRQL. In this study, parents of children with food hypersensitivity filled out a generic questionnaire with 13 subscales (Child Health Questionnaire Parental Form 28 – CHQ-PF28) that had been supplemented with questions that were disease-specific for food allergy. Children with FA scored lower on subscales of self-esteem than children without food hypersensitivity, but this difference was not significant. Therefore, self-esteem (including satisfaction with appearance) was not influenced by food hypersensitivity in this study (Östblom et al., 2008).
3.2. Studies Considering FA and Eating Disorders
Six articles, all published between 1996 and 2019, considering food allergies and eating disorders were identified. Of these, 2 were qualitative, including a case study (Robson et al., 2019) and a descriptive cross-sectional study (Michael Fitzgerald & Frankum, 2017) and 3 were quantitative, including one cross sectional study (Shanahan et al., 2014), one comparative study (Lieberman et al., 2019) and one quantitative survey (Polloni et al., 2013). A news release was also identified through our grey literature search and included in this review (Presnell, 2020). Countries of publication included Italy, United Kingdom, Canada, and the United States of America.
Four studies found maladaptive or disordered dietary behaviours adopted in food allergic cohorts which evolved as a mechanism of avoiding undesirable consequences (Robson et al., 2019; Shanahan et al., 2014; Lieberman et al., 2019; Polloni et al., 2013). In a cross-sectional study (Michael Fitzgerald & Frankum, 2017) of adults being followed in either an immunology clinic or a general practice clinic, rates of food avoidance/restriction did not significantly differ between the two groups (p=0.242) although they were comparatively higher (84% vs. 74%). The most common reasons for food avoidance or restriction in both cohorts were related to fear of aversive consequences (intolerance, allergy) followed by avoidance based on sensory characteristics (taste, smell, or texture). Explicit avoidance due to FA was reported in 25% of total respondents and was reported at similar rates between male and female participants (p=0.936). 26% of respondents reporting some degree of food avoidance/restriction felt their patterns of eating impacted their life such as difficulty going out to restaurants, or weight loss. This “life impact” was reported more often by respondents from the immunology clinic (36%) compared to the general practice clinic (10%).
A key finding of this review was that incidence of psychiatric comorbidities including but not limited to: anorexia nervosa, bulimia nervosa, and avoidant/restrictive food intake disorder was correlated with presence of FA (Lieberman et al., 2019; Robson et al., 2019; Shanahan et al., 2014; Presnell, 2020). Notable records include a case study wherein avoidant/restrictive food intake disorder was diagnosed in two children who had previously been on specific food elimination diets to manage their “remitted Eosinophilic Esophagitis” (Robson et al., 2019) and a comparative study of children with eating disorders, which found more patients with avoidant/restrictive food intake disorder (13.8%) were comorbidly diagnosed with FA than those with anorexia nervosa (11.7%) (Lieberman et al., 2019). Also included is a cross-sectional study that demonstrated food allergies were associated with symptoms of anorexia nervosa, even after controlling for psychopathological co-morbidity (Shanahan et al., 2014). In this same study, adolescents with FA were at increased risk for eating disorders symptoms “even beyond ‘just’ being underweight”.
3.3. Studies Considering FA, Disturbed Body Image and Eating Disorders
One comparative study from Poland, published in 2018, looked at the prevalence of eating disorders as an implication of FA (Wróblewska et al., n.d.). This study demonstrated that patients with FA, and who struggle with confidence, or those following an uncontrolled, restrictive elimination diet were more prone to food aversion and eating disorders than their healthy peers.
4. Discussion
In this narrative review of FA, body image and eating disorders, the collective literature points toward a strong association between FA and body image disturbance, as well as FA and development of eating disorders. These associations were seen across different age groups, although studies on children/adolescents were disproportionately represented.
In six of 7 studies, associations between FA and body image disturbance were related to healthy eating habits (Sommer et al., 2014), integration of FA as a stable aspect of identity (Marklund et al., 2007), or influence of caregivers; mothers in particular (Rouf et al., 2012). Interestingly, this finding was more exaggerated in individuals with FA than those with other chronic conditions such as diabetes (Flokstra-de Blok et al., 2009), thus suggesting that FA might possibly be a mediating factor in the development of body image disturbance. The data collected suggest that suffering related to body image could favor, together with FA, the onset of a clinical or subclinical eating disorder. In other words, FA could trigger an eating disorder vulnerability, by means of the interplay with body image. Only one of the 7 studies on FA and body image provided evidence to the contrary, although therein (Östblom et al., 2008), body image was a small component of larger HRQL measurements.
In the six included studies on FA and eating disorders, individuals with FA were overrepresented in cohorts of patients with all types of psychiatric co-morbidity. Interestingly, we found that studies mentioned anorexia nervosa and avoidant/restrictive food intake disorder more than bulimia nervosa or binge eating disorder. This may indicate that FA is associated with anorexia nervosa or avoidant/restrictive food intake disorder to a greater extent than other eating disorders. Taking into account the scant literature available on bulimia nervosa or binge eating disorder and FA, we feel further studies are needed to determine whether FA is associated with certain eating disorders more than others.
Going forward, future research may want to address limitations and minimize other potential confounders by conducting quantitative research, studying adult populations and using longitudinal designs. Further expansion to regions outside of Oceania and Europe may be necessary in order to confidently apply findings to countries in North America. Additional confounding dimensions to take into consideration include gender, household income, ethnicity, individual food allergies, and type and severity of allergies. In addition, it may be reasonable to examine eating disorders that have not yet been studied extensively in the literature, including avoidant/restrictive food intake disorder, bulimia nervosa or binge eating disorder. Control or review of these variables would allow researchers to uncover specific mediating variables beyond those reported in this review and elicit specific relationships that are impossible to determine as of now. Lastly, use of randomized or stratified samples in lieu of convenience samples in order to accurately reflect primary findings and minimize bias, may also want to be considered.
Clinically, routine surveillance of individuals with FA for development of maladaptive behaviors is warranted, with referral to appropriate mental health services if necessary. Language used to discuss diet with individuals with FA and their caregivers may benefit from an adjustment from “what foods to avoid” to “what foods can be safely enjoyed”.
Due to the prevalence of this chronic illness and the evidence that FA has a significantly larger impact on quality of life than other chronic illnesses, it is interesting that there does not exist sufficient consideration for the ways the healthcare system or government programs can raise awareness for and address this concern to prevent damaging psychopathologies. Policy makers must advocate for development of mental health services geared towards individuals with FA and consider the possibility that individuals with FA who develop patterns of disordered eating are followed in clinics that may escape the scope of practice of eating disorder specialists. Education regarding the presentation and symptomology of these eating disorders, as well as increased awareness of the tendency of this vulnerable population to develop maladaptive eating behaviours may improve outcomes for individuals with FA by providing earlier diagnosis and intervention.
5. Limitations
Given the paucity of quantitative data available, and the availability of qualitative data, we performed a narrative review rather than a systematic review. Whereas a narrative review may be considered less rigorous, it provided a means by which to include qualitative data that would not have been possible with a systematic review. Other limitations to this review include acknowledgment that few studies appeared to sufficiently consider comorbidities as potential confounders. There is significant co-morbidity between eating disorder, body image disturbance and psychopathologies such as generalized anxiety, and there also exists a high degree of association between FA and anxiety. This overlap makes it difficult to tease out whether our findings can be attributed to FA associated anxiety or to a more generalized anxiety that would exist in a non-food allergic individual. In addition, many of the included studies employed convenience sampling which does not allow for generalizability to the population as a whole and introduces the possibility of bias due to the reasons why individuals choose to take part in these types of studies. As most of the articles reporting FA and body image were published in European, Oceanic or North American countries these results may not be generalizable to non-western societies. Only one study successfully reported socioeconomic status of participants in addition to gender and/or age (Peniamina et al., 2014). This variable, in addition to race/ethnicity are known to be potential confounders in healthcare research and as such, results of this study may again not be generalizable to all populations.
6. Conclusions
There is evidence to suggest a possible association between body image disturbance in a food allergic individual and increased likelihood of development of subsequent eating disorders. This is summarized in Fig. 2. The association between FA and eating disorders has been explored more than FA and body image, however associations may only accurately reflect anorexia nervosa and avoidant/restrictive food intake disorder as there is more information in the literature regarding those eating disorders. There is evidence to suggest bulimia nervosa may be associated with FA, however it is limited.
Fig. 2.
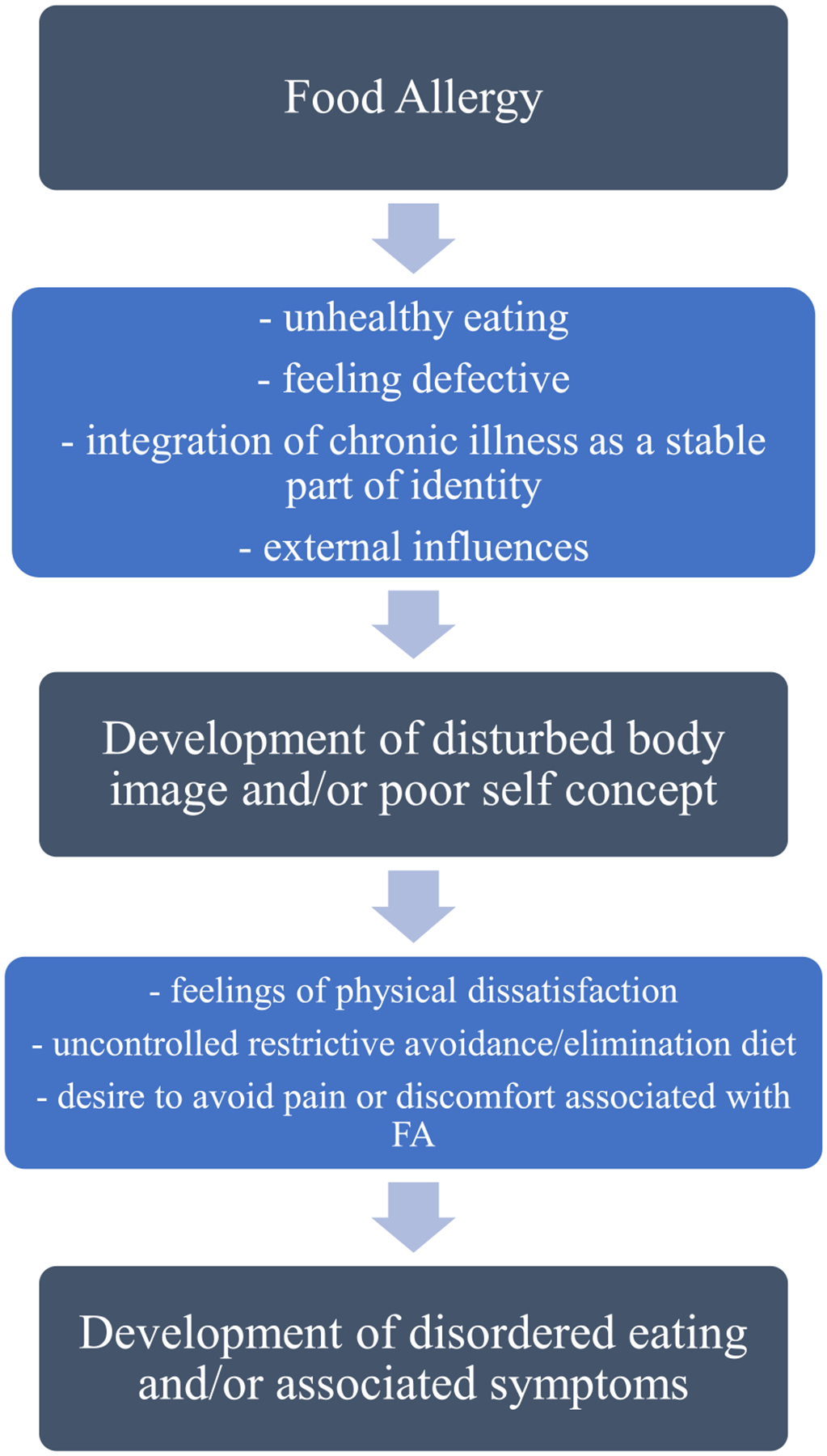
Proposed Mechanism for Development of Eating Disorders Mediated by Body Image Disturbance as A Result of Food Allergy
Role of Funding Sources
This project was supported by a BSc(med) student stipend, from the College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, awarded to SJ, under the supervision of JP. Additional funding sources included National Institutes of Health K24 AI106822 (WP); Allergy Asthma Awareness Initiative, Inc (WP); National Institutes of Health K23 AI143962 (LB); and JP’s start-up funds from the Department of Pediatrics and Child Health, University of Manitoba, and the Children’s Hospital Research Institute of Manitoba. None of these funders were involved in the project design or interpretation of the results.
Abbreviations:
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders
- IgE
Immunoglobulin E
- FA
Food allergy
- HRQL
Health-related quality of life
Footnotes
Declaration of Competing Interest
SJ none
TF none
TB none
WB none
LB none
JP is the Section Head of Allied Health for the Canadian Society of Allergy and Clinical Immunology; and sits on the steering committee of Canada’s National Food Allergy Action Plan.
Author Statement Contributions
SJ co-designed the review, co-performed the literature review and data extraction, and drafted the manuscript.
TF co-performed the literature review and data extraction, and critically reviewed the manuscript.
TB provided critical insight on the manuscript and aided in data interpretation.
WP provided critical insight on the manuscript and aided in data interpretation.
LB provided critical insight on the manuscript and aided in data interpretation.
JP co-designed the review, oversaw the drafting of the manuscript, and supervised SJ and TF on this project.
Submission Declaration
This manuscript has not been previously published, is not under consideration for publication elsewhere, has been approved by all authors and will not be published anywhere else in the same form in any language, including electronically, without the written consent of the copyright holder.
REFERENCES
- Ackerman CS, 2009. Parenting children with food allergy: Stress, anxiety, and parenting style. Dissertation Abstracts International: Section B: The Sciences and Engineering 69 (11-B), 7127. [Google Scholar]
- Alexi J, Palermo R, Rieger E, Bell J, 2019. Evidence for a perceptual mechanism relating body size misperception and eating disorder symptoms. Eating and Weight Disorders 24 (4), 615–621. 10.1007/s40519-019-00653-4. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- Bartek RP, 1988. A descriptive study of the subjective experience of psychological symptoms and food allergies. Dissertation Abstracts International Section A: Humanities and Social Sciences 49 (6-A), 1371. [Google Scholar]
- Clarke AE, Elliott SJ, St. Pierre Y, Soller L, La Vieille S, Ben-Shoshan M, 2020. Temporal trends in prevalence of food allergy in Canada. Journal of Allergy and Clinical Immunology: In Practice 8 (4), 1428–1430. 10.1016/j.jaip.2019.10.021 e5. [DOI] [PubMed] [Google Scholar]
- De Asis LB, Simon RA, 2009. Food Allergy: Psychological Considerations. Food Allergy: Adverse Reactions to Foods and Food Additives, Fourth Edition. 10.1002/9781444300062.ch44. [DOI] [Google Scholar]
- de Portela Santana ML, da Costa Ribeiro H, Mora Giral M, Raich RM, 2012. Epidemiology and risk factors of eating disorder in adolescence; a review. Nutricion Hospitalaria 27 (2), 391–401. 10.1590/S0212-16112012000200008. [DOI] [PubMed] [Google Scholar]
- DunnGalvin A, Dubois AEJ, Flokstra-de Blok BMJ, Hourihane JOB, 2015. The effects of food allergy on quality of life. Chemical Immunology and Allergy 101 (235–52). 10.1159/000375106. [DOI] [PubMed] [Google Scholar]
- Evans K, Rouf K, 2014. Living with severe food allergy. Psychologist 27 (5), 334–337. [Google Scholar]
- Fitzgerald M, Frankum B, 2017. Food avoidance and restriction in adults: A cross-sectional pilot study comparing patients from an immunology clinic to a general practice. Journal of Eating Disorders 5 (1), 30. 10.1186/s40337-017-0160-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flokstra-de Blok BMJ, Dubois AEJ, Vlieg-Boerstra BJ, Oude Elberink JNG, Raat H, DunnGalvin A, Hourihane JOB, Duiverman EJ, 2010. Health-related quality of life of food allergic patients: Comparison with the general population and other diseases. Allergy: European Journal of Allergy and Clinical Immunology 65 (2), 238–244. 10.1111/j.1398-9995.2009.02121.x. [DOI] [PubMed] [Google Scholar]
- Flokstra-de Blok BMJ, Oude Elberink JNG, Vlieg-Boerstra BJ, Duiverman EJ, Dubois AEJ, 2009. Measuring health-related quality of life: Fundamental methodological issues. Clinical and Experimental Allergy : Journal of the British Society for Allergy and Clinical Immunology 39 (11). 10.1111/j.1365-2222.2009.03376.x. [DOI] [PubMed] [Google Scholar]
- Galmiche M, Déchelotte P, Lambert G, Tavolacci MP, 2019. Prevalence of eating disorders over the 2000–2018 period: A systematic literature review. American Journal of Clinical Nutrition 109 (Issue 5), 1402–1413. 10.1093/ajcn/nqy342. Oxford University Press. [DOI] [PubMed] [Google Scholar]
- Herbert LJ, 2012. Mothers’ psychosocial functioning, parenting, and medical decision making related to children’s food allergies and food challenges. Dissertation Abstracts International: Section B: The Sciences and Engineering 72 (12-B), 7742. [Google Scholar]
- Hildebrand H, Simons E, Kozyrskyj AL, Becker AB, Protudjer JLP, 2019. Calcium intake in children with eczema and/or food allergy: A prospective cohort study. Nutrients 11 (12). 10.3390/nu11123039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson SGO, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, Motala C, Ortega Martell JA, Platts-Mills TAE, Ring J, Thien F, Van Cauwenberge P, Williams HC, 2004. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. Journal of Allergy and Clinical Immunology 113 (5), 832–836. 10.1016/j.jaci.2003.12.591. [DOI] [PubMed] [Google Scholar]
- Kaye WH, Klump KL, Frank GKW, Strober M, 2000. Anorexia and Bulimia Nervosa. Annual Review of Medicine 51 (1), 299–313. 10.1146/annurev.med.51.1.299. [DOI] [PubMed] [Google Scholar]
- Keski-Rahkonen A, Mustelin L, 2016. Epidemiology of eating disorders in Europe. Current Opinion in Psychiatry 29 (6), 340–345. 10.1097/YCO.0000000000000278. [DOI] [PubMed] [Google Scholar]
- Lieberman M, Houser MEME, Voyer A-PA-P, Grady S, Katzman DK, 2019. Children with avoidant/restrictive food intake disorder and anorexia nervosa in a tertiary care pediatric eating disorder program: A comparative study. International Journal of Eating Disorders 52 (3). 10.1002/eat.23027. [DOI] [PubMed] [Google Scholar]
- Marklund B, Wilde-Larsson B, Ahlstedt S, Nordström G, 2007. Adolescents’ experiences of being food-hypersensitive: A qualitative study. BMC Nursing 6. 10.1186/1472-6955-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markus LN, 2019. Battle against food allergy isolation: A quantitative exploration of self-perspective in children with food allergies. Dissertation Abstracts International: Section B: The Sciences and Engineering 80 (8–B(E)). No-Specified. [Google Scholar]
- Mehta H, Groetch M, Wang J, 2013. Growth and nutritional concerns in children with food allergy. Current Opinion in Allergy and Clinical Immunology 13 (Issue 3), 275–279. 10.1097/ACI.0b013e328360949d. NIH Public Access. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K, 1995. Psychoneurological aspects of food allergy. Stress, the Immune System and Psychiatry 185–206. [Google Scholar]
- Molloy JDF, Hourihane JB, 2008. Diet and food allergies in children. 24 Journal of Investigational Allergology and Clinical Immunology 382 (2014). [Google Scholar]
- Östblom E, Egmar A, Gardulf A, Lilja G, Wickman M, 2008. The impact of food hypersensitivity reported in 9-year-old children by their parents on health-related quality of life. Allergy,, 2nd63. Wiley Online Library. 10.1111/j.1398-9995.2007.01559.x. [DOI] [PubMed] [Google Scholar]
- Patel N, Herbert L, Green TD, 2017. The emotional, social, and financial burden of food allergies on children and their families. Allergy and Asthma Proceedings 38 (2), 88–91. 10.2500/aap.2017.38.4028. [DOI] [PubMed] [Google Scholar]
- Peniamina RL, Bremer P, Conner TS, Mirosa M, 2014. Understanding the needs of food-allergic adults. Qualitative Health Research 24 (7), 933–945. 10.1177/1049732314539733. [DOI] [PubMed] [Google Scholar]
- Polloni L, Muraro A, 2020. Anxiety and food allergy: A review of the last two decades. Clinical and Experimental Allergy 50 (4), 420–441. 10.1111/cea.13548. [DOI] [PubMed] [Google Scholar]
- Polloni L, Toniolo A, Lazzarotto F, Baldi I, Foltran F, Gregori D, Muraro A, 2013. Nutritional behavior and attitudes in food allergic children and their mothers. Clinical and Translational Allergy 3 (1), 1–6. 10.1186/2045-7022-3-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presnell A (2020, March 19). Food Allergies & Avoidant-Restrictive Food Intake Disorder. https://www.aaaai.org/about-aaaai/newsroom/news-releases/susceptible.
- Protudjer JLP, Jansson S-A, Middelveld R, Östblom E, Dahlén S-E, Arnlind MH, Bengtsson U, Kallström-Bengtsson I, Marklund B, Rentzos G, Sundqvist A-C, Åkerström J, Ahlstedt S, 2016. Impaired health-related quality of life in adolescents with allergy to staple foods. Clinical and Translational Allergy 6 (1), 37. 10.1186/s13601-016-0128-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reading D (2009). The Reality of Food Allergy: The Patients’ Perspective. In Management of Food Allergens. 10.1002/9781444309911.ch1. [DOI] [Google Scholar]
- Robson J, Laborda T, Fitzgerald S, Andersen J, Peterson K, O’Gorman M, Guthery S, Bennett-Murphy L, 2019. Avoidant/Restrictive Food Intake Disorder in Diet-treated Children With Eosinophilic Esophagitis. Journal of Pediatric Gastroenterology and Nutrition 69 (1), 57–60. 10.1097/MPG.0000000000002323. [DOI] [PubMed] [Google Scholar]
- Rouf K, White L, Evans K, 2012. A qualitative investigation into the maternal experience of having a young child with severe food allergy. Clinical Child Psychology and Psychiatry 17 (1), 49–64. 10.1177/1359104511415636. [DOI] [PubMed] [Google Scholar]
- Saperstein TL, 2010. Effect of eliminating food-related activities on academic performance for grade 4 classrooms. Dissertation Abstracts International Section A: Humanities and Social Sciences 71 (3-A), 836. [Google Scholar]
- Shaker MS, Schwartz J, Ferguson M, 2017. An update on the impact of food allergy on anxiety and quality of life. Current Opinion in Pediatrics 29 (4), 497–502. 10.1097/MOP.0000000000000509. [DOI] [PubMed] [Google Scholar]
- W. C.-J. of, 2014, undefined Shanahan L, Zucker N, Copeland WE, Costello EJ, Angold A, …, Copeland WEWE, Costello EJJ, Angold A, 2014. Are children and adolescents with food allergies at increased risk for psychopathology?. Journal of Psychosomatic Research 77 (6), 468–473. 10.1016/j.jpsychores.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sicherer SH, Sampson HA, 2018. Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. Journal of Allergy and Clinical Immunology 141 (1), 41–58. 10.1016/j.jaci.2017.11.003. [DOI] [PubMed] [Google Scholar]
- Singer AG, Kosowan L, Soller L, Chan ES, Nankissoor NN, Phung RR, Abrams EM, 2020. Prevalence of Physician-Reported Food Allergy in Canadian Children. Journal of Allergy and Clinical Immunology: In Practice. 10.1016/j.jaip.2020.07.039. [DOI] [PubMed] [Google Scholar]
- Slade PD, 1994. What is body image? Behaviour Research and Therapy 32 (5), 497–502. 10.1016/0005-7967(94)90136-8. [DOI] [PubMed] [Google Scholar]
- Sommer I, Mackenzie H, Venter C, Dean T, 2014. An exploratory investigation of food choice behavior of teenagers with and without food allergies. Annals of Allergy, Asthma and Immunology 112 (5), 446–452. 10.1016/j.anai.2014.02.009. [DOI] [PubMed] [Google Scholar]
- Thörnqvist V, Middelveld R, Wai HM, Ballardini N, Nilsson E, Strömquist J, Ahlstedt S, Nilsson LJ, Protudjer JLP, 2019. Health-related quality of life worsens by school age amongst children with food allergy. Clinical and Translational Allergy 9 (1). 10.1186/s13601-019-0244-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venter C, Pereira B, Voigt K, Grundy J, Clayton CB, Higgins B, Arshad SH, Dean T, 2008. Prevalence and cumulative incidence of food hypersensitivity in the first 3 years of life. Allergy: European Journal of Allergy and Clinical Immunology 63 (3), 354–359. 10.1111/j.1398-9995.2007.01570.x. [DOI] [PubMed] [Google Scholar]
- Wróblewska B, Szyc A, Markiewicz LH, Zakrzewska M, Romaszko E, 2021. Increased prevalence of eating disorders as a biopsychosocial implication of food allergy. PLoS One 13 (6). 10.1371/journal.pone.0198607. [DOI] [PMC free article] [PubMed] [Google Scholar]


