Background:
Headache disorders are common diseases that cause a social burden. This systematic review and meta-analysis aimed to evaluate the effects of various non-pharmacological treatments to address or prevent acute headaches, including neuromodulation, acupuncture, and aerobic exercises in patients with episodic migraine and tension-type headache (TTH).
Methods:
We performed a systematic search of the electronic databases PubMed, Cochrane Library, Embase, China National Knowledge Infrastructure, WANFANG MEDICINE ONLINE, and Chinese Medical Journal database using Stata/SE 14.0 to obtain weighted mean differences (WMDs). The outcomes included monthly headache days, headache intensity, headache duration, days per month of acute medication use, and the Medical Outcomes Study 36-Item Short-Form Health Survey.
Results:
Of 872 identified articles, 27 were included in the meta-analysis. Neuromodulation was associated with reduced headache days (WMD: −1.274, 95% CI [−1.914, −0.634], P < .001), duration (WMD: −2.2, 95% CI [−3.32, −0.107], P < .001) and medication consumption (WMD: −1.808, 95% CI [−2.546, −1.071], P < .001) in cases of migraine. Acupuncture was associated with the alleviation of headache days (WMD: −0.677, 95% CI [−0.932, −0.422], P < .001) and intensity (WMD: −0.893, 95% CI [−1.573, −0.212], P = .01) in cases of migraine and acute medication use (WMD: −3.29, 95% CI [−4.86, −1.72], P < .001) in cases of TTH. Aerobic exercise was associated with reduced headache duration (WMD: −5.1, 95% CI [−8.97, −1.22], P = .01) in cases of TTH. The risk of bias for included articles was moderate.
Conclusions:
There is low- and moderate-quality evidence that neuromodulation, acupuncture, and aerobic exercises are associated with attenuated headache symptoms in patients with episodic migraine or TTH. However, high-quality studies are needed to draw more detailed conclusions.
Keywords: acupuncture, aerobic exercises, migraine, neuromodulation, tension-type headache
1. Introduction
Almost 50% of adults have suffered from a headache during the last year, and 90% experience at least 1 headache in their lifetime.[1,2] A study that evaluated the prevalence among more than 100,000 people reported that 38% of the population was affected by tension-type headaches and that migraines – the top cause of disability among 15 to 49 year-olds and responsible for 5.6% of all years lived with disability[3] – affected 12% population.[4] Further, tension-type headache (TTH) and migraine are reportedly major contributors to the social burden for young and middle-aged adults.[5]
The National Institution for Health and Care Excellence (NICE) guidelines for the management of headaches in young people and adults focus primarily on pharmacological treatment.[6] However, certain populations, such as pregnant or lactating individuals, may be reluctant to use medication. Additionally, patients with headaches are at risk of developing medication-overdose headaches, and 46.5% patients with chronic daily headaches have medication-overuse headache.[7]
The only non-pharmacological therapy that NICE recommends for TTH is acupuncture.[6] The NICE guideline development group mentions that the quality of evidence for non-pharmacological therapy is low or very low because of the poor quality of existing studies.[6] Moreover, the guidelines of the French headache society strongly recommended aerobic excise, neuromodulation, and acupuncture as alternative or supplement to pharmacological prophylaxis.[8] Moreover, the guidelines of Danish headache society labels acupuncture, physiotherapy, and behavioral therapy as beneficial for the alleviation headache symptoms.[9] Recent meta-analyses regarding non-pharmacological therapies, including aerobic exercise,[10] psychological therapy,[11] and physiotherapy,[12] have shown the specific effects of such alternative treatments on headache. However, with the continuous advancement of technology and the development of clinical trials, increasingly more evidence continues to emerge, demanding a further need to generate new level of evidence for treatment. Neuromodulation therapy is an emergent treatment method and many large randomized controlled trials (RCTs) have proved that neuromodulation therapy has a certain effect on migraine treatment recently.[13–16] Some RCT studies have found that acupuncture can improve headache symptoms.[17–19] Moreover, recent preclinical studies have shown that acupuncture has a clear anti-inflammatory effect.[20] Because of the basic experiments evidence, the future evidence level will be improved. Although the effect of aerobic exercise on headache is not so obvious,[21–23] some guidelines[8] 9recommend that patients with headache should exercise regularly because it is beneficial to multiple systems. And aerobic exercise an effective, economic and muti-system beneficial treatment. We think the 3 non-pharmacological therapies are the topmost choices for patients with headache, who ask for non-pharmacological treatment. Therefor the aim of this study was to quantify the effects of neuromodulation, acupuncture, and aerobic exercises in patients with migraine and TTH.
2. Materials and methods
This literature review was conducted following the guidelines published by the Cochrane Handbook and reported by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.[24]
2.1. Study-search strategy and study-selection
Three electronic databases were searched to identify eligible studies published from 1/1/2000 to 6/30/2022: PubMed, the Cochrane Central Register of Controlled Trials, Embase, and Chinese database China National Knowledge Infrastructure, WANFANG MEDICINE ONLINE, and Chinese Medical Journal database to extend our literature. Medical subject heading terms and natural language terms were combined in the search strategy.
Search words included “headache,” “TTH OR migraine” combined with “exercise,” “exercises,” “neuromodulation,” “acupuncture,” “remote electrical neuromodulation,” “transcranial magnetic stimulation,” “noninvasive vagus nerve stimulation,” “transcutaneous occipital nerve stimulation,” “transcutaneous supraorbital stimulation” or “external trigeminal nerve stimulation.” The included articles investigated migraine or TTH. The interventions that they reported included neuromodulation, acupuncture, and aerobic exercise. And aerobic exercise was defined as a target heat rate reaching to 70% of the HRmax.[25]
Inclusion criterion: P: population was comprised of adult patients with episodic migraine or TTH; I: studies evaluated neuromodulation, aerobic exercise, or acupuncture; C: control group involved usual care, wait list, routine care, sham stimulation/acupuncture, or no treatment; O: studies included outcomes of interest; S: the studies were RCTs; articles were written in English or Chinese. We also ensured that each study’s definition of migraine and TTH matched the International Classification of Headache Disorders, 2nd or 3rd.[2,26] Additionally, article references were used to broaden the search. The titles and abstracts of all articles were screened by 2 reviewers (PCH and LYL) to exclude irrelevant studies respectively. Two reviewers then checked the entire texts according to predefined inclusion and exclusion criteria (Table 1) respectively. Then the results are put together. If the results are different, the 2 reviewers discuss which result should be adopted. In case of a disagreement between the 2 reviewers that was not resolved by discussion, a third reviewer (YSY) decided whether the article should be included.
Table 1.
The inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Patients (P) | Adults diagnosed episodic migraine or TTH by ICHD criteria | Children or adolescent subjects, other types of headache, migraine or TTH with MOH |
| Intervention (I) | Aerobic exercises, neuromodulation therapy, acupuncture | Medication as stand-alone treatment, other non- pharmacological therapy |
| Control (C) | Usual care, waitlist, routine care, sham stimulation/acupuncture, or no treatment | - |
| Outcomes (O) | Monthly headache days, headache intensity, headache duration, monthly consumption of acute medication, SF-36 | - |
| Studies design (S) | Random clinical trials | Cohort studies, case reports, reviews |
ICHD = International Classification of Headache Disorders; MOH = medication-overuse headache; SF-36 = Medical Outcomes Study 36-Item Short-Form Health Survey; TTH = tension-type headache.
2.2. Data extraction
The reports were searched for the following variables: country of publication, headache type, experimental intervention, intervention in the control group, number of participants included in the experimental and control groups, gender, age, the headache days per month, headache duration and headache intensity in baseline, duration of intervention, outcome measures, and time points of measurements. A data extraction method was developed to extract the reported information. Data were manually extracted from the articles by 2 independent researchers (PCH and LYL) respectively. An additional researcher reviewed the data extraction and resolved conflicts.
2.3. Risk of bias in individual studies and level of evidence
The risk of bias assessment for the selected articles was performed using the Cochrane risk of bias (ROB) tool for RCTs.[27] Two reviewers (PCH and LYL) independently evaluated the included articles.
The overall level of evidence was evaluated using the Grading of Recommendations Assessment, Development and Evaluation (GRADE)[28] to formulate an overall conclusion on the level of evidence based on the methodological quality of the included trials.[28] Two reviewers (PCH and LYL) independently evaluated the outcomes. The inter-rater reliability was determined using a Kappa coefficient (>0.7 indicated a high level of agreement between assessors, between 0.5 and 0.7 a moderate level of agreement and <0.5 a low level of agreement).
2.4. Data synthesis and statistical analysis
The software used for the meta-analyses was Stata/SE 14.0 for Mac (StataCorp LP, College Station, TX). The mean values and standard deviations for post-intervention effects were entered into the meta-analysis. If these were not reported, the mean values were calculated from changes over time, and the standard deviations were determined from confidence intervals (CIs) or standard errors from the equations provided in the Cochrane Handbook.[24] Trials that included 2 active interventions were compared to the control group, respectively. The pooled efficacy measure was assessed as the weighted mean difference (WMD) with a 95% CI using a random effect model. Statistical significance was set to the 2-sided P-value of <0.05. The ROB and GRADE were determined using RevMan 5.3.3 (The Nordic Cochrane Center; The Cochrane Collaboration, Ottawa, ON, Canada).
Heterogeneity among the studies included in the meta-analysis was tested using the I2 statistic, where an I2 value higher than 50% was considered indicative of meaningful heterogeneity. If I2 > 50% or P < .05, sensitivity analyses were performed by excluding studies 1 by 1 from the meta-analysis to test the robustness of the effects of a single study on the overall estimate and find the source of the heterogeneity.
To define the effect of different types of interventions for migraine and TTH, intervention sub-analyses were conducted.
2.5. Ethics statement
Because all the data in the study were retrieved from public databases, this study did not require ethical approval or patient consent.
3. Results
3.1. Study selection
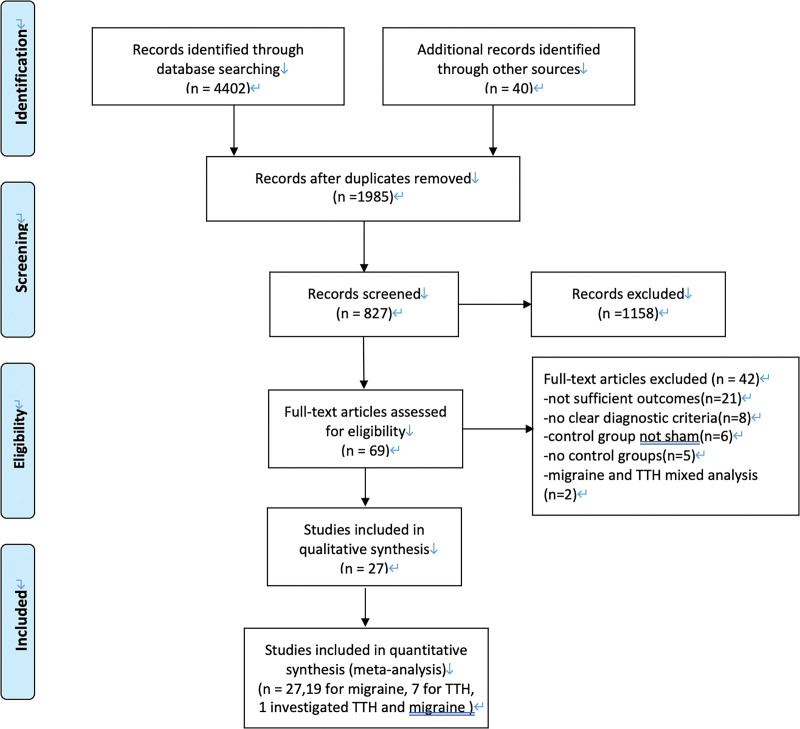
The search strategy yielded 1269 results in PubMed, 469 in the Cochrane library, 943 in Embase, 716 in the China National Knowledge Infrastructure, 557 in the WANFANG MEDICINE ONLINE and 448 in the Chinese Medical Journal database. After removing duplicates, 872 articles were screened for relevant titles and abstracts. After title and abstract screening, 69 studies were retrieved as full text articles. The full text screening identified 27 studies that met the inclusion criteria. A flow diagram of the selection of research articles in the meta-analysis and the reasons for exclusion is shown in Figure 1.
Figure 1.
Flow chart of studies selection.
3.2. Study characteristics
Of the twenty-seven included studies, nineteen investigated the effect of interventions for migraine[13–19,21,29–37] and 7 for TTH.[23,38–42] One study[22] investigated both TTH and migraine using separate data analyses. Fourteen studies focused on acupuncture,[17–19,32,33,37–42] 9 on neuromodulation therapy,[13–16,30,31,35,36,42] and 4 on aerobic exercise.[21–23,34] The specific characteristics of the selected studies are described in Table 2.
Table 2.
Summary of characteristics of included studies.
| Author | Year | Country | Title | Headache type | Criteria | Trial: gender | Control: gender | Trial: age | Control: age | Trial: headache days | Control: trial: headache days | Trial: headache intensity | Control: trial: headache intensity | Trial: headache duration | Control: trial: headache duration | Trial intervention (n) | Control intervention (n) | Measurement time | Test time | Outcome measure |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mekhail NA | 2016 | USA | Safety and efficacy of occipital nerves stimulation for the treatment of chronic migraines: randomized, double-blind, controlled single-center experience | Migraine | ICHD3 | 33 (79%) | 15 (75%) | 44.9 ± 11.0 | 44.6 ± 12.6 | 17.04 ± 8.73 | 16.95 ± 9.56 | 5.09 ± 1.79 | 5.99 ± 2.34 | 21.6 ± 7.1 | 18.5 ± 15.1 | Occipital nerve stimulation (14) | No stimulation (6) | 12 wk | After treatment | Headache days, headache intensity |
| Antal A | 2011 | Germany | Cathodal transcranial direct current stimulation of the visual cortex in the prophylactic treatment of migraine | Migraine | ICHD2 | 12 (85.7%) | 11 (78.5%) | 33.2 ± 10.4 | 32.3 ± 12.3 | 16.5 ± 3.2 | 15.0 ± 4.2 | 5.5 ± 0.5 | 5 ± 0.25 | 15.3 ± 12.1 | 12.0 ± 8.9 | Transcranial direct current stimulation (14) | Sham stimulation (14) | 6 wk | 8 wk follow-up | Headache days, headache duration, headache intensity |
| Liu Y | 2017 | China | Migraine prevention using different frequencies of transcutaneous occipital nerve stimulation: a randomized controlled trial | Migraine | ICHD3 | 18 (81.8%) | 18 (81.8%) | 39.45 ± 10.99 | 44.27 ± 8.32 | / | / | 6.87 ± 1.53 | 6.79 ± 1.05 | 11.11 ± 6.16 | 9.96 ± 5.20 | Transcutaneous occipital nerve stimulation (22) | Sham tONS intervention (22) | 4 wk | 3 mo follow-up | Frequency, intensity, duration, medications consumption |
| Chou DE | 2018 | USA | Acute migraine therapy with external trigeminal neurostimulation (ACME): a randomized controlled trial | Migraine | ICHD3 | 43 (83%) | 49 (91%) | 39.71 ± 13.62 | 40.09 ± 12.65 | / | / | 5.92 ± 1.68 | 6.17 ± 1.81 | 7.00 ± 0.59 | 6.00 ± 1.19 | External trigeminal nerve stimulation (52) | Sham stimulation (54) | 56 min | After treatment 1, 2, 24 h | Headache intensity |
| Hokenek NM | 2020 | Turkey | Treatment of migraine attacks by transcutaneous electrical nerve stimulation in emergency department: a randomize controlled trial | Migraine | ICHD3 | 24 (61.5%) | 24 (61.5%) | 35.62 ± 8.77 | 33.62 ± 10.20 | 5 ± 1.48 | 4 ± 2.22 | / | / | / | / | Transcutaneous Electrical Nerve Stimulation (39) | Sham stimulation (39) | 20 min | After treatment 20, 120 min | Headache intensity |
| Misra UK | 2013 | India | High-rate repetitive transcranial magnetic stimulation in migraine prophylaxis: a randomized, placebo-controlled studye | Migraine | ICHD2 | 44 (88%) | 44 (88%) | 35.62 ± 10.07 | 35.06 ± 10.38 | 20.84 ± 9.45 | 17.04 ± 10.30 | 3 ± 1.2 | 3 ± 1.4 | 11.19 ± 7.41 | 9.75 ± 7.17 | High-rate repetitive transcranial magnetic stimulation (50) | Sham stimulation (50) | 3 times, 412 s every time | 1 mo | Headache days, medication consumption |
| Jiang L | 2019 | China | Combination of flunarizine and transcutaneous supraorbital neurostimulation improves migraine prophylaxis | Migraine | ICHD3 | 38 (74%) | 39 (75%) | 29.67 ± 9.24 | 30.96 ± 9.40 | 5.92 ± 1.04 | 5.68 ± 2.51 | 6.75 ± 1.35 | 6.98 ± 1.10 | 6.21 ± 4.80 | 5.12 ± 4.03 | Combination of flunarizine and transcutaneous supraorbital neurostimulation (51) | Flunarizine (52) | 3 mo | 3 mo | Headache days, intensity and rescue medication consumption |
| Li Y | 2012 | China | Acupuncture for migraine prophylaxis: a randomized controlled trial | Migraine | ICHD2 | 92 (78.0%) | 103 (87.3%) | 36.8 ± 13.0 | 37.5 ± 12.1 | 6.1 ± 1.26 | 5.5 ± 1.04 | 5.4 ± 0.44 | 5.5 ± 0.43 | Acupuncture (121) | Sham acupuncture (118) | 4 wk | 4 wk follow-up | Headache days, headache intensity | ||
| Li Y | 2009 | China | Acupuncture for treating acute attacks of migraine: a randomized controlled trial | Migraine | ICHD2 | 33 (56.9%) | 33 (55.0%) | 41.84 ± 14.21 | 39.65 ± 12.83 | / | / | 5.0 ± 1.26 | 5.0 ± 2.07 | / | / | Acupuncture (54) | Sham acupuncture (55) | 1 session | After treatment 1, 2, 4 h | Headache intensity, medication consumption |
| Farahmand S | 2018 | Iran | Pain management using acupuncture method in migraine headache patients; a single blinded randomized clinical trial | Migraine | ICHD3 | 50 (83.3%) | 50 (83.3%) | 31.4 ± 7.6 | 31.4 ± 7.6 | / | / | / | / | / | / | Acupuncture (30) | Sham acupuncture (30) | 30 min | After treatment 15, 30, 45, and 60 min | Headache intensity |
| Wang LP | 2012 | China | Efficacy of acupuncture for acute migraine attack: a multicenter single blinded, randomized controlled trial | Migraine | ICHD2 | 67 (89.3%) | 63 (84.0%) | 37.8 ± 10.6 | 38.6 ± 12.6 | / | / | 5.7 ± 1.4 | 5.4 ± 1.3 | / | / | Acupuncture (75) | Sham acupuncture (75) | 30 min | 3 d follow-up | Headache intensity |
| Diener HC | 2006 | Germany | Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomized controlled clinical trial | Migraine | ICHD2 | 247 (85%) | 257 (81%) | 37.1 ± 10.5 | 38.3 ± 10.4 | 6.0 ± 3.2 | 5.8 ± 3.2 | 73.7 ± 13.3 | 73.8 ± 13.3 | / | / | Acupuncture (290) | Sham acupuncture (317) | 6 wk | 23 wk follow-up | Headache days |
| Hanssen H | 2018 | Switzerland | Effects of different endurance exercise modalities on migraine days and cerebrovascular health in episodic migraineurs: a randomized controlled trial | Migraine | ICHD3 | 10 (76.9%) | 10 (83.3%) | 36.2 ± 10.7 | 37.3 ± 11.9 | 3.8 ± 3.0 | 3.2 ± 2.4 | / | / | / | / | Intensity interval training group (13) | Daily physical activity (12) | 12-wk | Posttreatment | Headache days |
| Varkey E | 2011 | Swedish | Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls | Migraine | ICHD2 | 25 (83) | 28 (93) | 47.0 ± 10.8 | 41.5 ± 11.4 | 7.0 ± 3.8 | 7.6 ± 3.8 | 5 ± 2.81 | 3.9 ± 2.15 | / | / | Aerobic exercise (30) | Relaxation (30) | 12-wk | 3 and 6 mo follow-up | Headache days, headache intensity |
| Krøll LS | 2018 | Denmark | The effects of aerobic exercise for persons with migraine and co-existing tension-type headache and neck pain. A randomized, controlled, clinical trial | Migraine | ICHD3 | 23 (88%) | 23 (88%) | 42 ± 10.9 | 36 ± 10.1 | 9.2 ± 5.2 | 8.3 ± 4.0 | 5.6 ± 1.8 | 5.7 ± 1.8 | 104.9 ± 83.6 | 90.3 ± 67.5 | Aerobic exercise (24) | No exercise (26) | 3 mo | 3 mo follow-up | Headache days, headache intensity and duration, medication consumption |
| Leahu P | 2022 | Germany | Increased migraine-free intervals with multifocal repetitive transcranial magnetic stimulation | Migraine | ICHD3 | 29 (87%) | 23 (92%) | 39.7 ± 11.53 | 39.8 ± 11.7 | 7.63 ± 3.91 | 6.22 ± 2.69 | 6.37 ± 1.61 | 6.32 ± 1.62 | / | / | rTMS (33) | Sham stimulation (27) | 4 wk | 3 mo | Headache days |
| Najib U | 2022 | USA | Noninvasive vagus nerve stimulation for prevention of migraine: the multicenter, randomized, double-blind, sham-controlled PREMIUM II trial | Migraine | ICHD3 | 49 (87.5%) | 44 (77.2%) | 40.3 ± 13.9 | 44.6 ± 10.7 | 9.2 ± 4.6 | 9.9 ± 3.5 | / | / | / | / | nVNS (77) | Sham stimulation (78) | 12-wk | Posttreatment | Headache days, and acute medication days |
| Zhang Y | 2021 | China | Regulatory effects of acupuncture on emotional disorders in patients with menstrual migraine without aura: a resting-state fMRI study | Migraine | ICHD3 | / | / | 33:04 ± 6:43 | 35:30 ± 9:43 | 3.76 ± 2.35 | 3.29 ± 1.59 | 6.40 ± 1.55 | 5.60 ± 1.57 | / | / | Acupuncture (24) | Sham acupuncture (20) | 3 mo | 3 mo | Headache days, headache intensity |
| Zhang J | 2020 | China | The effect of acupuncture and moxibustion on 64 cases of migraine | Migraine | ICHD3 | / | / | / | / | / | / | 4.01 ± 1.24 | 4.02 ± 1.25 | / | / | Acupuncture (34) | Sham acupuncture (34) | 30 d | Posttreatment | Headache intensity |
| Zhao Z | 2021 | China | Clinical observation on 34 cases of vestibular migraine of Qi and blood deficiency type treated with warm acupuncture | Migraine | ICHD3 | 19 (44.1%) | 20 (46.5%) | 48.9 ± 8.3 | 47.8 ± 8.9 | / | / | 7.41 ± 0.78 | 7.50 ± 0.83 | / | / | Acupuncture (32) | Sham acupuncture (32) | 8 wk | Posttreatment | Headache intensity |
| Chen X | 2006 | China | Evaluation of the effect of acupuncture on episodic tension-type headache | TTH | ICHD2 | 65 (73%) | 60 (72%) | 35 ± 1.7 | 34 ± 1.9 | 16 | 14 | / | / | / | / | Acupuncture (89) | Sham acupuncture (83) | 1 mo | Posttreatment | Headache days |
| Krøll LS | 2018 | Denmark | The effects of aerobic exercise for persons with migraine and co-existing tension-type headache and neck pain. A randomized, controlled, clinical trial | TTH | ICHD3 | 23 (88%) | 23 (88%) | 42 ± 10.9 | 36 ± 10.1 | 7.6 ± 6.5 | 7.9 ± 5.9 | 2.8 ± 1.2 | 3.1 ± 1.6 | 90.3 ± 112.9 | 94.2 ± 103.8 | Aerobic exercise (26) | Exercise (26) | 3 mo | 3 mo follow-up | Headache days, headache intensity and duration, medication consumption |
| Fernando Prieto Peres M | 2018 | Brazil | Non-pharmacological treatment for primary headaches prevention and lifestyle changes in a low-income community of Brazil: a randomized clinical trial | TTH | ICHD3 | 20 (80) | 21 (84) | 41.8 ± 19.7 | 41.1 ± 16.4 | 15.4 ± 11.0 | 13.3 ± 8.6 | 2.5 ± 0.7 | 3.0 ± 0.9 | 28.4 ± 23.9 | 27.6 ± 23.5 | Aerobic exercise (25) | Relaxion (25) | 3 times/wk for 6 mo | Posttreatment | Headache days, headache duration, headache intensity |
| Melchart D | 2005 | Germany | Acupuncture in patients with tension-type headache: randomized controlled trial | TTH | ICHD2 | 53 (88%) | 49 (80%) | 43.5 ± 9.4 | 44.4 ± 9.8 | 7.0 ± 6.3 | 5.3 ± 3.1 | / | / | / | / | Acupuncture (132) | Sham acupuncture (63) or waitlist (75) | 8 wk | 12 wk follow-up | Headache days |
| Endres HG | 2007 | Germany | Acupuncture for tension-type headache: a multicentre, sham-controlled, patient and observer-blinded, randomized trial | TTH | ICHD2 | 163 (78%) | 158 (79%) | 38.9 ± 12.2 | 39.2 ± 11.4 | 14 ± 4.4 | 14 ± 2.96 | 68.3 ± 12.2 | 67.5 ± 12.5 | / | / | Acupuncture (209) | Sham acupuncture (200) | 6 wk | 3 mo, 6 mo follow-up | Headache days, intensity, SF-36 |
| Karst M | 2001 | Germany | Needle acupuncture in tension-type headache: a randomized, placebo-controlled study | TTH | ICHD | 21 (60%) | 17 (50%) | 47.9 ± 13.8 | 48.2 ± 14.6 | 21.1 ± 10.2 | 20.5 ± 10.3 | 4.6 ± 1.8 | 4.4 ± 1.3 | / | / | Acupuncture (34) | Placebo needle (35) | 6 wk | 6 wk follow-up | Headache days, pain intensity, consumption of medication, duration of headache |
| Melchart D | 2005 | Germany | The acupuncture randomized trial (ART) for tension-type headachedetails of the treatment | TTH | ICHD2 | 18 (43%) | 18 (43%) | 42 ± 9.6 | 42 ± 9 | 17.5 ± 6.9 | 17.3 ± 6.9 | / | / | / | / | Acupuncture (132) | Sham acupuncture (63) or waitlist (75) | 8 wk | 12 wk follow-up | Headache days, consumption of medication, SF-36 |
| White AR | 2000 | UK | Acupuncture for episodic tension-type headache: a multicentre randomized controlled trial | TTH | ICHD | / | / | 49.8 ± 2.9 | 48.2 ± 2.9 | 4.3 ± 2.1 | 3.6 ± 1.7 | 38.6 ± 15.4 | 42.1 ± 10.4 | 48.8 ± 56.1 | 39.8 ± 29.7 | Acupuncture (15) | Sham acupuncture (19) | 6 wk | 1, 2 mo follow-up | Headache days, duration, intensity, mediaction consumed |
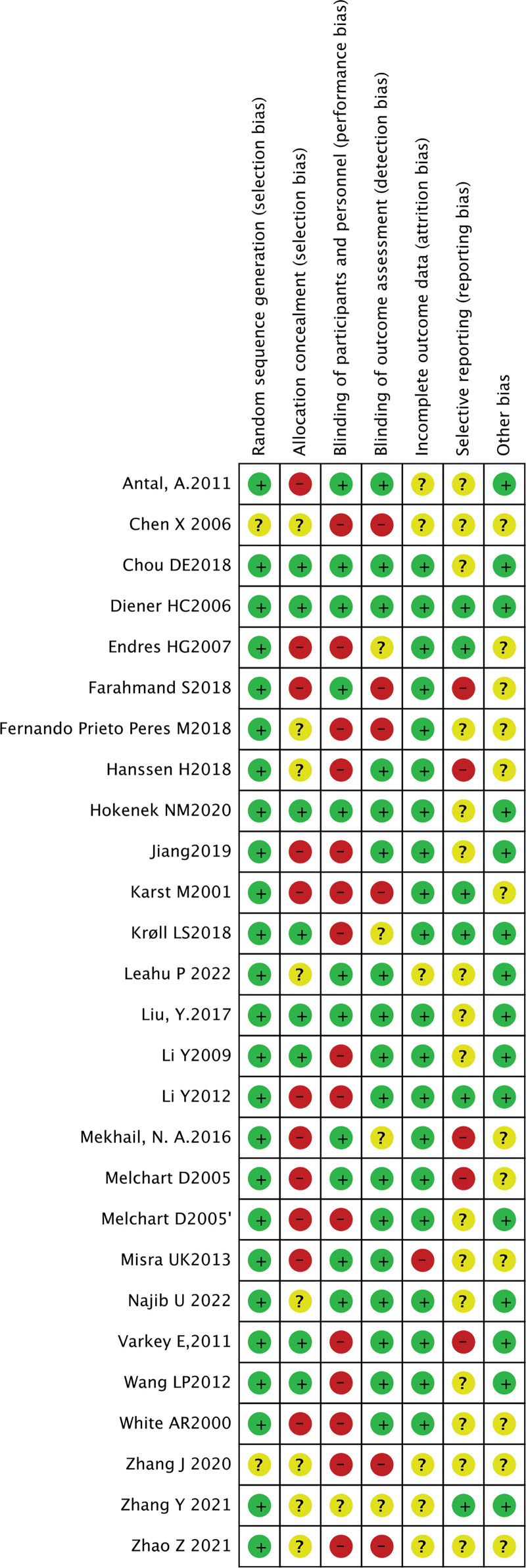
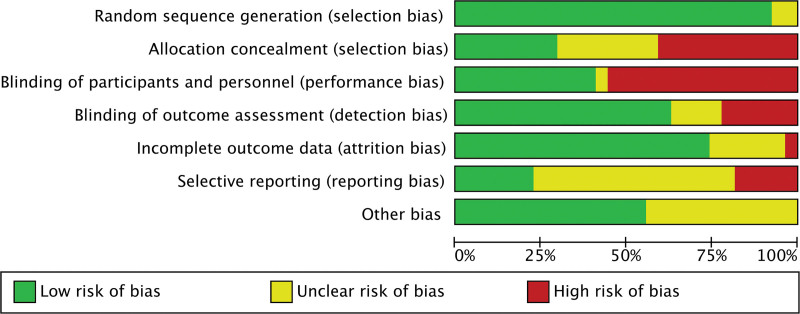
3.3. Risk of bias and level of evidence
Overall, a moderate ROB was present in all the included studies. The ROB assessment resulted in a considerable number of “‘unclear’” ratings. Most of the unclear ratings were due to the unavailability of a study protocol; hence, unclear selective outcome reporting was a source of bias.[13–17,19,23,30,31,35,36,38,42] The unclear risk of bias was also attributed to “other bias”: the lack of sufficient evidence for judging the other risk of bias.[18,23,29,30,34,39–42] The ROB most frequently rated as “high” was “blinding of participants and personnel.”[17,19,21–23,31,32,34,37,39–42] In some trials, such as those on aerobic exercises and waitlist, it was impossible to implement blinded methods. Another source of high risk of bias was the concealment of allocation protocol.[13,17,18,29–31,35–42] Some trials were open to random allocation and some were alternate enrollment.[18,31,32,34] The Kappa coefficient was 0.63 (P < .001), indicating moderate agreement on the bias analysis between the 2 analysts (PCH and LYL). The ROB summary and graph are shown in Figures 2 and 3.
Figure 2.
Risk of bias summary of researches included in this meta-analysis.
Figure 3.
Risk of bias graph of researches include in this meta-analysis.
3.4. Synthesis of the results
3.4.1. Intervention effects on migraine.
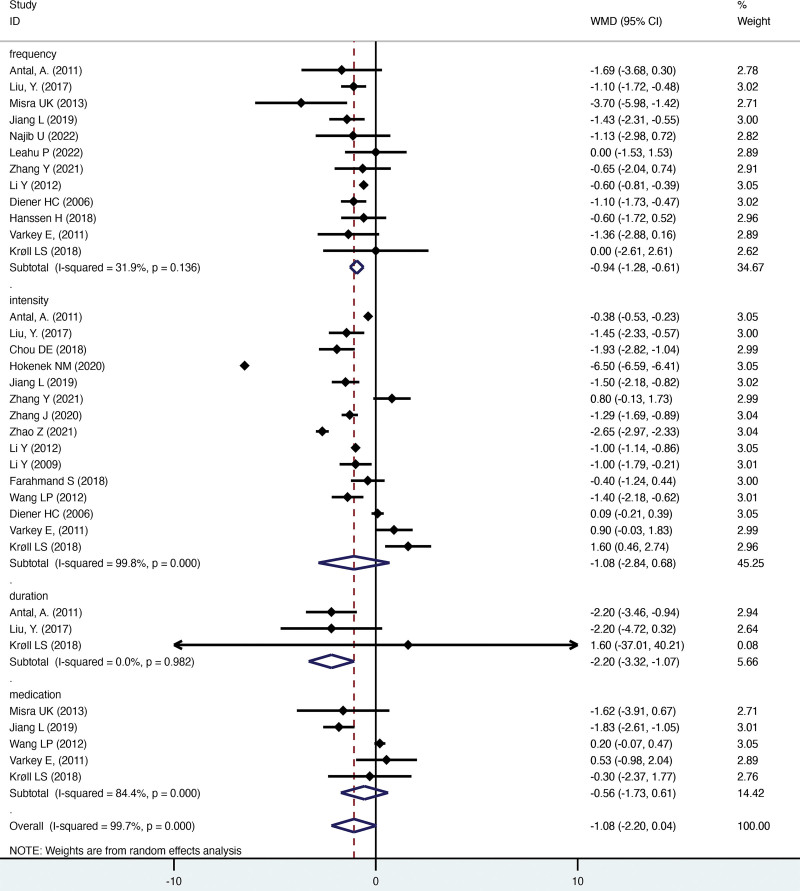
Nineteen studies that evaluated the effects of different types of treatment were included in the meta-analysis. The combined results indicated statistically significant results for headache days and duration (Fig. 4). The sub-analysis showed that neuromodulation therapy was significantly associated with reduced headache days, headache duration, and medication usage. Acupuncture was associated with an obvious reduction in headache days and intensity.
Figure 4.
Pooled data comparing intervention and control group of migraine.
3.4.1.1. Headache days.
12 trials included the number of days of headache per month as an outcome variable. There was a significant reduction in headache days per month (−0.943; 95% CI [−1.275, −0.611], P < .001) between the intervention treatment and control groups. The heterogeneity analysis showed that the studies included in the analysis were moderately heterogeneous (I2 = 31.9%, P = .0851). The sub-analysis showed a significant mean difference of −1.274 (95% CI [−1.914, −0.634], P < .001) between the neuromodulation therapy and control groups. Moreover, we observed a mean difference of −0.677 (95% CI [−0.932, −0.422], P < .001) between the control and acupuncture groups.
3.4.1.2. Headache intensity.
Headache intensity was evaluated in 15 studies. Pain reduction after the intervention was −1.082 (95% CI [−2.845, 0.68], P = .229) on a 0 to 10 scale, indicating a nonsignificant change between the treatment and control groups. The heterogeneity analysis showed that the included studies were significantly heterogeneous (I2 = 99.8%, P < .001). The sensitivity analysis showed that Hokenek et al[16] significantly affected the combined results. After removing the study, the combined results were significant (WMD: −0.748, 95% CI [−1.212, −0.285], P = .002). The combined I2 was still 95.1%, indicating that the heterogeneity came from the difference between the 3 groups. In the subgroup analysis, the overall result demonstrated a significant mean difference of −0.893 (95% CI [−1.573, −0.212], P = .01) between the acupuncture and control groups.
3.4.1.3. Duration.
Three studies that included the duration of headaches were included in the meta-analysis. The reduction in headache hours per month was −2.19 (95% CI [−3.324, −1.070], P < .001), indicating a significant difference between the treatment and control groups. There was no heterogeneity among the included studies (I2 = 0%, P = .982). In the subgroup analysis, we found a significant mean difference of −2.2 (95% CI [−3.32, −0.107], P < .001) between the neuromodulation and control groups.
3.4.1.4. Medication usage.
Five studies compared the consumption of acute care medicine. There was a slight decline in medication consumption in the treatment groups compared with the control group, but the difference was not significant (WMD = −0.563, 95% CI [−1.732, 0.607], P = 0346). There was significant heterogeneity among the included studies (I2 = 84.4%, P < .001). In the sensitivity analysis, after excluding Jiang et al,[31] the I2 became 0%, but the combined result was still nonsignificant (WMD: 0.178, 95% CI [−0.086, 0.442], P = .187). The subgroup analysis showed that there was a significant mean difference between neuromodulation and control groups of −1.808 (95% CI [−2.546, −1.071], P < .001).
3.4.2. Intervention effects on TTH.
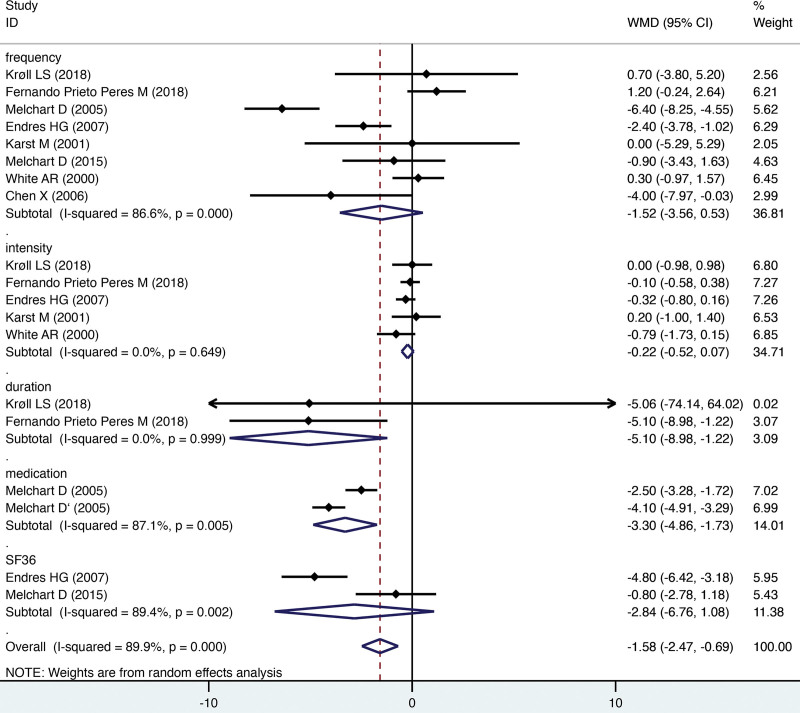
Seven studies evaluated the effectiveness of interventions compared to the control groups in patients with TTH. The combined mean effect was statistically significant for the duration of headache and consumption of acute medication (Fig. 5). The sub-analysis demonstrated that acupuncture was associated with a significant reduction in consumption of acute medicine. Moreover, aerobic exercise was associated with alleviated headache duration.
Figure 5.
Pooled data comparing intervention and control group of TTH. TTH = tension-type headache.
3.4.2.1. Headache days.
Eight trials focused on the number of headache days. The reduction was −1.515 (95% CI [−3.556, 0.526], P = .146), showing that the patients had fewer headache days per month; however, the difference was nonsignificant. The heterogeneity analysis demonstrated that the studies included in the analysis were significantly heterogeneous (I2 = 86.6%%, P < .001). In the sensitivity analysis, after excluding Melchart et al[41] and Endres et al,[39] the I2 became 27.7% and combined result was still not significant (WMD: 0.098, 95% CI [−1.039, 1.235], P = .866). The subgroup analysis demonstrated that there was no significant difference between the different types of intervention.
3.4.2.2. Headache intensity.
Five studies with headache intensity were included in the analysis. The pain intensity difference was −0.223 (95% CI [−0.516, 0.071], P = .137), indicating that the intervention resulted in a nonsignificant reduction in headache intensity. There was no heterogeneity among the studies (I2 = 0%, P = .649). The subgroup analysis demonstrated that there was no significant difference between the different types of intervention.
3.4.2.3. Duration.
Two studies that included the duration of headaches were included in the meta-analysis. The reduction in headache hours per month was −5.1 (95% CI [−8.97, −1.22], P = .01), indicating a significant difference between the treatment and control groups. There was no heterogeneity among the included studies (I2 = 0%, P = .999). Because there were only 2 studies, the sub-analysis could not be conducted.
3.4.2.4. Medication usage.
Two studies that included medication usage as a variable were included in the analysis. The reduction in medication consumption in the intervention group was −3.29 (95% CI [−4.86, −1.72], P < .001) days per month. The heterogeneity analysis showed that the included studies were significantly heterogeneous (I2 = 87.1%, P = .005). Because there were only 2 studies, the sensitivity analysis and sub-analysis could not be performed.
3.4.2.5. SF-36.
Two studies evaluated the SF-35 scores were included in the analysis. There was no significant difference in physical health (mean difference, −2.84; 95% CI [−6.67, 1.07], P = .155). There was no heterogeneity among the studies (I2 = 89.4%, P = .002). Because there were only 2 studies, the sensitivity analysis and sub-analysis could not be conducted.
3.5. Qualitive analysis
Using the GRADE application, data regarding the SF-36 were graded as “moderate-quality” evidence. The overall quality evidence was rated as “low” for data concerning the headache days, self-reported headache intensity, headache duration, and consumption of medication, indicating that the results were uncertain and could be changed. The Kappa coefficient was 0.662 (P < .001), which means that there was moderate agreement in the bias analysis between 2 analysts (PCH and LYL).
4. Discussion
The present study performed a meta-analysis of 27 studies to determine the effects of neuromodulation therapy, acupuncture, and aerobic exercises on episodic migraine and TTH. We found that neuromodulation therapy, acupuncture, and aerobic exercises were associated with the alleviation of headache symptoms. According to our results, neuromodulation therapy could alleviate the headache days, duration, and usage of acute medication for migraines. Acupuncture may result in a significant reduction in headache days and intensity in migraine, as well as acute medication consumption, in patients with TTH. Moreover, aerobic exercises could reduce headache intensity of migraine and headache duration in patients with TTH. Additionally, from our manuscript, we could guide the neurologist to recommend patients with different therapies: the patients with more headache days are more suitable for neuromodulation therapy and patients with more severe headaches intensity may be suitable for acupuncture treatment. Therefore, these results could be significant, especially to some certain population with contraindications to medication, such as pregnant women and breastfeeding women.
Neuromodulation devices are an emergent means of treating migraine, and randomized clinical trials have demonstrated their tolerability and efficacy with significant therapeutic gains in acute and preventive treatment.[44] A systematic review by Moisset et al[45] indicated that neuromodulation methods may have a positive effect on migraine management. Our system review confirms the conclusion that neuromodulation plays a role in reducing headache symptoms. The neuromodulation approach is based on the concept that migraines can be aborted or prevented by the stimulation of peripheral or central nerves.[46] Central nervous stimulation includes transcranial magnetic stimulation (TMS) and transcranial direct stimulation (TENS). Occipital TENS, assessed by the stimulation of the occipital nerve, has been shown to modify thalamocortical dysrhythmia.[47] The possible mechanism of TMS involves using a brief magnetic pulse to interrupt a pattern of neuronal firing that is believed to be associated with migraine.[48] The mechanism of remote electrical neuromodulation is based upon the tendency that pain inhibits pain, an innate mechanism to inhibit perception of pain in other remote body part.[48] Several neuromodulation devices have been shown to be effective for acute or preventive migraine treatment and have been approved by the United States Federal Drug Administration. These include TMS, TENS, noninvasive vagus nerve stimulation, external trigeminal nerve stimulation for the acute and prophylactic treatment of migraine, and remote electrical neuromodulation for acute treatment of migraine.[49] Neuromodulation therapy should be considered for migraines, but the cost and lack of insurance coverage are barriers for their administration to patients.
Based on our meta-analysis, acupuncture seems to have a significant effect on reducing headache days and intensity in cases of migraine and acute medication consumption in patients with TTH. The previous meta-analysis showed that acupuncture is effective for migraine and TTH,[50,51] although the quality of evidence is moderate or low. While only a minimal effect following active treatment was found when compared to the effects of sham treatment.[51] However, Liu et al[20] found that electroacupuncture stimulation at the hindlimb ST36 acupoint could activate the vagal-adrenal anti-inflammatory axis in mice. The mechanism of acupuncture treatment of headache may also involve the anti-inflammatory effect of acupuncture at specific acupoints. More rigorous random control trials that compare the effects of acupuncture with other treatments are needed.
Recent mate-analyses provide moderate-quality evidence that aerobic exercises could decrease the number of headache days in patients with migraine.[10,52,53] Our review also supports evidence that aerobic exercises are effective in reducing headache intensity in migraine and headache duration in patients with TTH. Aerobic exercises are recommended as a means of managing and preventing headaches by the American Academy of Neurology, American College of Physicians, and American Headache Society.[54] The French Headache Society strongly encourage patients with migraine to exercise weekly.[8] Moreover, aerobic exercise has also shown beneficial effects in patients with depression and anxiety.[55,56] The therapeutic effect of aerobic exercises may not only mediate cardiopulmonary, inflammatory, and neurovascular processes, but also enhance sociocognitive factors, such as self-efficacy beliefs.[57] Indeed, the effectiveness of aerobic exercise in mitigating the symptoms of other common disorders, including cardiovascular disease, has been broadly shown, aerobic exercise may be reasonably recommended to patients with headache. Considering the clinically meaningful effects in the context of time, effort, cost of treatment, and systemic effect, aerobic exercise may be a promising treatment approach.
Headache, especially migraine, is a common cause of lost work, disrupted family relationships, and reduced quality of life.[58] Although pharmacological management remains the first choice for headaches worldwide, it does not always achieve the maximal benefit of therapy. For example, delayed use of an acute treatment may cause reduced effects. Further, preventive drugs may be poorly tolerated, and there may be low adherence rates due to common adverse and “wear off” effects.[46] By contrast, non-pharmacological therapies provide acute treatment and prophylactic management with few clinically significant adverse effects.
It is worth noting that non-pharmacological management should be considered based on accurate diagnosis, headache days, the severity of the attack, response to medication, and coexisting conditions. Based on the individuals’ symptoms, doctors can recommend optimal therapeutic strategies for patients. The choice between pharmacological and non-pharmacological treatment of headache depends on the patient’s preference, tolerability, and contraindications in different patient groups. According to our results, there are different types of methods suitable according to the type of headache. For example, neuromodulation may be warranted for patients with migraines but less so for those with TTH. The time, effort, and cost of treatment should also be considered for each patient to determine whether a given treatment is clinically or practically appropriate.
4.1. Limitations
Although our results are promising, there are some limitations to the interpretation of the presently reported outcomes. There was a diversity of treatments used and heterogeneity in the outcome measures reported between studies that influenced the statistical analysis. We performed a subgroup analysis according to the types of treatment. However, within a subgroup in which the same method and outcome were tested, the parameters could be quite different in terms of stimulation intensity and number of sessions, confounding a cohesive consideration of the data.
We do not have data on the long-term effects of interventions. Because the studies included varied time of follow-up periods, we could not synthesize these outcomes in the review. Moreover, we adopted the WMD meta-analysis model recommended by the Cochrane Handbook. However, caution is needed when interpreting the combined results because WMD cannot be directly translated into clinical meaning. Further, there are many non-pharmacological therapies that were not included in the meta-analysis: e.g., manual therapy, which has proven to be effective in treating migraine.[59,60]
Although non-pharmacological therapy seems beneficial for alleviating headache symptoms without evident clinical adverse effects, the overall quality of published non-pharmacological therapies remains moderate or low according to the GRADE.[28] Further, more RCTs of high quality and standard measuring indexes are required to guide the appropriate use of non-pharmacological therapy in clinical practice. We recommend that future RCTs use unified outcome measures and design trials that explore convenient and low-cost non-pharmacological therapies.
4.2. Conclusion
According to our results, neuromodulation, aerobic exercises, and acupuncture are effective in treating patients with migraine or TTH. However, the level of evidence is moderate or low. Future research should use standardized outcome measures to gather high-quality evidence.
Author contributions
Study concept and design: PC and SY. Acquisition of data: SY, PC, and LY Data curation: SY, TW, and LL Analysis of data: PC. Interpretation of data: YX. Drafting of the manuscript: PC. Modifying the manuscript: SY and LY. All authors read and approved the final manuscript.
Conceptualization: Chenghui Pi, Shengyuan Yu.
Data curation: Chenghui Pi, Yinglu Liu, Lingling Li, Wenjing Tang.
Formal analysis: Chenghui Pi, Xin Yan.
Funding acquisition: Shengyuan Yu.
Investigation: Chenghui Pi, Yinglu Liu.
Methodology: Chenghui Pi, Yinglu Liu.
Software: Chenghui Pi.
Supervision: Shengyuan Yu.
Writing – original draft: Chenghui Pi.
Writing – review & editing: Shengyuan Yu.
Abbreviations:
- CI =
- confidence interval
- GRADE =
- Grading of Recommendations Assessment, Development and Evaluation
- NICE =
- National Institution for Health and Care Excellence
- RCTs =
- randomized controlled trials
- ROB =
- risk of bias
- TENS =
- transcranial direct stimulation
- TMS =
- transcranial magnetic stimulation
- TTH =
- tension-type headache
- WMD =
- weighted mean difference
This work was supported by the Beijing Natural Science Foundation Essential Research Project Z170002 and the National Natural Science Foundation of China (grants 81671077, 81771180, 81771200, 81901134, 81901145, and 82071226).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Pi C, Liu Y, Li L, Tang W, Yan X, Yu S. Effects on neuromodulation, acupuncture, and aerobic exercises on migraine and tension-type headache outcomes: A systematic review and meta-analysis. Medicine 2022;101:45(e30530).
Contributor Information
Chenghui Pi, Email: m13521765304@163.com.
Yinglu Liu, Email: lyl.jane@163.com.
Lingling Li, Email: lll18222752817@163.com.
Wenjing Tang, Email: tangwj592@126.com.
Xin Yan, Email: karenyan0919@163.com.
References
- [1].Steiner TJ, Stovner LJ, Katsarava Z, et al. The impact of headache in Europe: principal results of the Eurolight project. J Headache Pain. 2014;15:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders, 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160. [DOI] [PubMed] [Google Scholar]
- [3].Steiner TJ, Stovner LJ, Vos T, et al. Migraine is first cause of disability in under 50s: will health politicians now take notice? J Headache Pain. 2018;19:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Robbins MS. Diagnosis and management of headache: a review. JAMA. 2021;325:1874–85. [DOI] [PubMed] [Google Scholar]
- [5].Collaborators GBDN. Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:459–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Centre NCG. Headaches: Diagnosis and Management of Headaches in Young People and Adults. London, UK:Royal College of Physicians, 2012. [PubMed] [Google Scholar]
- [7].Laskar S, Kalita J, Misra U. Comparison of chronic daily headache with and without medication overuse headache using ICHD II R and ICHD 3 beta criteria. Clin Neurol Neurosurg. 2019;183:105382. [DOI] [PubMed] [Google Scholar]
- [8].Demarquay G, Mawet J, Guégan-Massardier E, et al. Revised guidelines of the French headache society for the diagnosis and management of migraine in adults. Part 3: non-pharmacological treatment. Rev Neurol (Paris). 2021;177:753–9. [DOI] [PubMed] [Google Scholar]
- [9].Schytz HW, Amin FM, Jensen RH, et al. Reference programme: diagnosis and treatment of headache disorders and facial pain. Danish Headache Society, 3rd edition, 2020. J Headache Pain. 2021;22:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lemmens J, De Pauw J, Van Soom T, et al. The effect of aerobic exercise on the number of migraine days, duration and pain intensity in migraine: a systematic literature review and meta-analysis. J Headache Pain. 2019;20:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lee HJ, Lee JH, Cho EY, et al. Efficacy of psychological treatment for headache disorder: a systematic review and meta-analysis. J Headache Pain. 2019;20:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Luedtke K, Allers A, Schulte LH, et al. Efficacy of interventions used by physiotherapists for patients with headache and migraine-systematic review and meta-analysis. Cephalalgia. 2016;36:474–92. [DOI] [PubMed] [Google Scholar]
- [13].Antal A, Kriener N, Lang N, et al. Cathodal transcranial direct current stimulation of the visual cortex in the prophylactic treatment of migraine. Cephalalgia. 2011;31:820–8. [DOI] [PubMed] [Google Scholar]
- [14].Liu Y, Dong Z, Wang R, et al. Migraine prevention using different frequencies of transcutaneous occipital nerve stimulation: a randomized controlled trial. J Pain. 2017;18:1006–15. [DOI] [PubMed] [Google Scholar]
- [15].Chou DE, Shnayderman Yugrakh M, Winegarner D, et al. Acute migraine therapy with external trigeminal neurostimulation (ACME): a randomized controlled trial. Cephalalgia. 2019;39:3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hokenek NM, Erdogan MO, Hokenek UD, et al. Treatment of migraine attacks by transcutaneous electrical nerve stimulation in emergency department: a randomize controlled trial. Am J Emerg Med. 2021;39:80–5. [DOI] [PubMed] [Google Scholar]
- [17].Li Y, Liang F, Yang X, et al. Acupuncture for treating acute attacks of migraine: a randomized controlled trial. Headache. 2009;49:805–16. [DOI] [PubMed] [Google Scholar]
- [18].Farahmand S, Shafazand S, Alinia E, et al. Pain management using acupuncture method in migraine headache patients; a single blinded randomized clinical trial. Anesth Pain Med. 2018;8:e81688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wang LP, Zhang XZ, Guo J, et al. Efficacy of acupuncture for acute migraine attack: a multicenter single blinded, randomized controlled trial. Pain Med. 2012;13:623–30. [DOI] [PubMed] [Google Scholar]
- [20].Liu S, Wang Z, Su Y, et al. A neuroanatomical basis for electroacupuncture to drive the vagal-adrenal axis. Nature. 2021;598:641–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Varkey E, Cider A, Carlsson J, Linde M. Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. Cephalalgia. 2011;31:1428–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Krøll LS, Hammarlund CS, Linde M, et al. The effects of aerobic exercise for persons with migraine and co-existing tension-type headache and neck pain. A randomized, controlled, clinical trial. Cephalalgia. 2018;38:1805–16. [DOI] [PubMed] [Google Scholar]
- [23].Fernando Prieto PM, Prieto Peres Mercante J, Belitardo de Oliveira A. Non-pharmacological treatment for primary headaches prevention and lifestyle changes in a low-income community of Brazil: a randomized clinical trial. Headache. 2019;59:86–96. [DOI] [PubMed] [Google Scholar]
- [24].Higgins JPT, Thomas J, Chandler J, et al. (editors). Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester, UK:John Wiley & Sons, 2019. [Google Scholar]
- [25].Helgerud J, Høydal K, Wang E, et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Med Sci Sports Exerc. 2007;39:665–71. [DOI] [PubMed] [Google Scholar]
- [26].Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38:1–211. [DOI] [PubMed] [Google Scholar]
- [27].Higgins J, Green SR. Chapter 8: assessing risk of bias in included studies. In Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Chichester, UK: John Wiley & Sons. 2011. [Google Scholar]
- [28].Schunemann HJ, Oxman AD, Brozek J, et al. GRADE: assessing the quality of evidence for diagnostic recommendations. ACP J Club. 2008;149:2. [PubMed] [Google Scholar]
- [29].Mekhail NA, Estemalik E, Azer G, et al. Safety and efficacy of occipital nerves stimulation for the treatment of chronic migraines: randomized, double-blind, controlled single-center experience. Pain Pract. 2017;17:669–77. [DOI] [PubMed] [Google Scholar]
- [30].Misra UK, Kalita J, Bhoi SK. High-rate repetitive transcranial magnetic stimulation in migraine prophylaxis: a randomized, placebo-controlled study. J Neurol. 2013;260:2793–801. [DOI] [PubMed] [Google Scholar]
- [31].Jiang L, Yuan DL, Li M, et al. Combination of flunarizine and transcutaneous supraorbital neurostimulation improves migraine prophylaxis. Acta Neurol Scand. 2019;139:276–83. [DOI] [PubMed] [Google Scholar]
- [32].Li Y, Zheng H, Witt CM, et al. Acupuncture for migraine prophylaxis: a randomized controlled trial. CMAJ. 2012;184:401–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Diener HC, Kronfeld K, Boewing G, et al. Efficacy of acupuncture for the prophylaxis of migraine: a multicentre randomised controlled clinical trial. Lancet Neurol. 2006;5:310–6. [DOI] [PubMed] [Google Scholar]
- [34].Hanssen H, Minghetti A, Magon S, et al. Effects of different endurance exercise modalities on migraine days and cerebrovascular health in episodic migraineurs: a randomized controlled trial. Scand J Med Sci Sports. 2018;28:1103–12. [DOI] [PubMed] [Google Scholar]
- [35].Leahu P, Bange M, Ciolac D, et al. Increased migraine-free intervals with multifocal repetitive transcranial magnetic stimulation. Brain Stimul. 2021;14:1544–52. [DOI] [PubMed] [Google Scholar]
- [36].Najib U, Smith T, Hindiyeh N, et al. Non-invasive vagus nerve stimulation for prevention of migraine: the multicenter, randomized, double-blind, sham-controlled PREMIUM II trial. Cephalalgia. 2022;42:560–9. [DOI] [PubMed] [Google Scholar]
- [37].Zhang Y, Wang Z, Du J, et al. Regulatory effects of acupuncture on emotional disorders in patients with menstrual migraine without Aura: a resting-state fMRI study. Front Neurosci. 2021;15:726505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Melchart D, Streng A, Hoppe A, et al. Acupuncture in patients with tension-type headache: randomised controlled trial. BMJ. 2005;331:376–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Endres HG, Böwing G, Diener HC, et al. Acupuncture for tension-type headache: a multicentre, sham-controlled, patient-and observer-blinded, randomised trial. J Headache Pain. 2007;8:306–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Karst M, Reinhard M, Thum P, et al. Needle acupuncture in tension-type headache: a randomized, placebo-controlled study. Cephalalgia. 2001;21:637–42. [DOI] [PubMed] [Google Scholar]
- [41].Melchart D, Streng A, Hoppe A, et al. The acupuncture randomised trial (ART) for tension-type headache – details of the treatment. Acupunct Med. 2005;23:157–65. [DOI] [PubMed] [Google Scholar]
- [42].White AR, Resch KL, Chan JC, et al. Acupuncture for episodic tension-type headache: a multicentre randomized controlled trial. Cephalalgia. 2000;20:632–7. [DOI] [PubMed] [Google Scholar]
- [43].Cousins S, Ridsdale L, Goldstein LH, et al. A pilot study of cognitive behavioural therapy and relaxation for migraine headache: a randomised controlled trial. J Neurol. 2015;262:2764–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Halker Singh RB, Ailani J, Robbins MS. Neuromodulation for the acute and preventive therapy of migraine and cluster headache. Headache. 2019;59(Suppl 2):33–49. [DOI] [PubMed] [Google Scholar]
- [45].Moisset X, Pereira B, Ciampi de Andrade D, et al. Neuromodulation techniques for acute and preventive migraine treatment: a systematic review and meta-analysis of randomized controlled trials. J Headache Pain. 2020;21:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Charles AM. Migraine. N Engl J Med. 2017;377:553–61. [DOI] [PubMed] [Google Scholar]
- [47].Coppola G, Di Lorenzo C, Serrao M, et al. Pathophysiological targets for non-pharmacological treatment of migraine. Cephalalgia. 2016;36:1103–11. [DOI] [PubMed] [Google Scholar]
- [48].VanderPluym JH, Halker Singh RB, Urtecho M, et al. Acute treatments for episodic migraine in adults: a systematic review and meta-analysis. JAMA. 2021;325:2357–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Dodick DW. Migraine. Lancet. 2018;391:1315–30. [DOI] [PubMed] [Google Scholar]
- [50].Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. 2016;2016:Cd001218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev. 2016;4:Cd007587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Barber M, Pace A. Exercise and migraine prevention: a review of the literature. Curr Pain Headache Rep. 2020;24:39. [DOI] [PubMed] [Google Scholar]
- [53].La Touche R, Fernández Pérez JJ, Proy Acosta A, et al. Is aerobic exercise helpful in patients with migraine? A systematic review and meta-analysis. Scand J Med Sci Sports. 2020;30:965–82. [DOI] [PubMed] [Google Scholar]
- [54].Irby MB, Bond DS, Lipton RB, et al. Aerobic exercise for reducing migraine burden: mechanisms, markers, and models of change processes. Headache. 2016;56:357–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Risling M. Blast induced brain injuries – a grand challenge in TBI research. Front Neurol. 2010;1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Buse DC, Manack A, Serrano D, et al. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatry. 2010;81:428–32. [DOI] [PubMed] [Google Scholar]
- [57].Dishman RK, Berthoud HR, Booth FW, et al. Neurobiology of exercise. Obesity (Silver Spring). 2006;14:345–56. [DOI] [PubMed] [Google Scholar]
- [58].Abu Bakar N, Tanprawate S, Lambru G, et al. Quality of life in primary headache disorders: a review. Cephalalgia. 2016;36:67–91. [DOI] [PubMed] [Google Scholar]
- [59].Gómez E, Inglés M, Serra-Aó P, et al. Effectiveness of a manual therapy protocol based on articulatory techniques in migraine patients: a randomized controlled trial. Musculoskelet Sci Pract. 2021;54:102386. [DOI] [PubMed] [Google Scholar]
- [60].Lendraitiene E, Smilgiene L, Petruseviciene D, et al. Changes and associations between cervical range of motion, pain, temporomandibular joint range of motion and quality of life in individuals with migraine applying physiotherapy: a pilot study. Medicina (Kaunas). 2021;57:630. [DOI] [PMC free article] [PubMed] [Google Scholar]