Background:
Pilonidal sinus is a common disease in the sacrococcygeal region. Although many treatments have been described in recent years, the recurrence of each method remains high. Surgeons did not reach a consensus on the preferred approach for pilonidal sinus. We carried out a meta-analysis of controlled clinical trials comparing the outcomes of endoscopic treatment versus conventional treatment for pilonidal sinus disease in this study.
Methods:
We performed a systematic literature search, and we used electronic databases such as PubMed/Medline, Embase, and the Cochrane library to search for the relevant literature comparing endoscopic management to other conventional treatments for pilonidal sinus disease. The primary outcome parameters were operative time, recurrence, postoperative complications and pain, and total healing time.
Results:
Six studies were included in the review. Endoscopic pilonidal sinus treatment had a lower overall complication rate than the conventional surgery group (risk ratio = 0.33 [0.19–0.58], P = .0001) and lower pain score with a weighted mean difference of −2.44 (95% confidence interval: (−3.96) to (−0.92), I2 = 99%, P = .002). There was no significant difference in recurrence (risk ratio = 0.75, 95% confidence interval [0.30–1.90],P = .55). Compared to the excision followed by the primary closure technique, the operation time, time to complete wound healing, and satisfaction were similar.
Conclusions:
Endoscopic pilonidal sinus treatment is a unique and potential method of sacrococcygeal pilonidal disease treatment. The foremost benefits of this technique are mild postoperative pain, lower complications rate, and return to routine for a shorter time. However, due to the limited number of articles, we need to conduct more rigorous large-sample prospective randomized controlled trials to clarify the efficiency of endoscopic treatment for pilonidal cysts.
Keywords: endoscopic treatment, pilonidal sinus, VAAPS
1. Introduction
Pilonidal sinus disease (PSD) is a widely known inflammatory condition of the gluteal region, with a population incidence of 26 per 100,000. It primarily afflicted males 4 times more than females and it mainly troubled young adults of working age.[1,2] This disease can manifest as an acute pointing abscess or a chronic sinus with intermittent drainage in patients. Whatever the presentation, the infected pilonidal sinus is usually followed by one or more pits in the midline.[3] For symptomatic patients, the onset of the disease can cause significant distress to them. In addition, after surgical excision, a high rate of wound complications leads to prolonged healing time and, as a result, a more extended return to regular activities.[4]
According to the studies, surgical resection is the primary treatment of pilonidal disease, and it is the key to preventing the recurrence of PSD. With the development of medical technology, various techniques have been reported to deal with this problem, such as excision with lay open, primary closure after excision, Karydakis procedure, Bascom cleft lift, and Limberg flap. Recurrent disease with its concomitant morbidity remains a concern, and no single therapeutic option has acquired general acceptability.[5–12]
In recent years, people are more and more inclined to minimally invasive surgery. Minero et al[13] introduced a more minimally invasive approach for sacrococcygeal pilonidal disease named Endoscopic Pilonidal Sinus Treatment in 2013 (EPSiT). The authors employed the same video-assisted anal fistula treatment device and technology to treat primary and recurrent pilonidal disease. The idea behind endoscopic pilonidal sinus treatment (EPSiT) is to use a Futuroscope to remove all damaged tissues through a small circular incision endoscopically. It will bring down the surgical morbidity associated with more wide-ranging flap reconstruction.
In this study, we conducted a meta-analysis of controlled clinical trials comparing the outcomes of Endoscopic treatment versus conventional treatment for PSD.
2. Materials and methods
2.1. Search strategy
From inception until February 2022, a comprehensive search of electronic databases such as PubMed, Embase, and the Cochrane library was conducted. We adopted the search terms: (pilonidal sinus) and (endoscopic OR VAAPS OR EPSiT OR minimally invasive). Two reviewers carried out a literature search and review of the articles. In addition, all of the retrieved publications’ reference lists were manually reviewed.
2.2. Eligibility criteria
All studies, whether randomized or nonrandomized that compare the endoscopic versus conventional surgery for the treatment of pilonidal sinus were qualified for inclusion. As for language, we have no restrictions.
We excluded extraneous articles, editorials, letters, cases reports, reviews, single-arm studies, and meta-analyses. We also excluded the articles that did not explicitly report the main results of this review. We included studies with the most comprehensive data for similar literature.[14,15]
2.3. Data extraction
Both investigators did data extraction separately, and the data extraction between them was double-blind. The data extraction of each study was extracted using a unified, standardized statistical table. We extracted the data from each study, including the type, duration, and country of the study; patient characteristics such as age, gender distribution, and comorbidities; technical details of the procedure; operation time; VAS pain scores; incidence of recurrence of sacrococcygeal pilonidal disease; complications rate; full healing time, time to everyday life, and length of follow-up.
2.4. Evaluation of literature quality
The modified Jadad scoring system (total score of 7 points, including randomization, double-blind, and follow-up) evaluated the included RCTs’ methodological quality. 1 to 3 points were considered low quality, and 4 to 7 points to high quality. The methodological quality of the non-RCT studies was evaluated using the MINORS scale. Scores ≥ 18 were high-quality clinical trials.
2.5. Statistical analysis
Statistical analysis was performed using RevMan version 5.3 software. The risk ratio (RR) and 95% confidence interval (CI) were calculated for each trial result. Heterogeneity between studies was assessed. We defined I2 < 50% as less heterogeneity, and I2 ≥ 50% considered more significant heterogeneity among studies. If I2 < 50%, we used the fixed model. Otherwise, a random model was used. We used the funnel plot method to evaluate the publication bias of the included literature. The asymmetry of the funnel plot indicated the situation of publication bias, and the more significant the asymmetry, the greater the degree of bias. A P-value less than .05 was considered significant.
3. Results
3.1. Patient and study characteristics
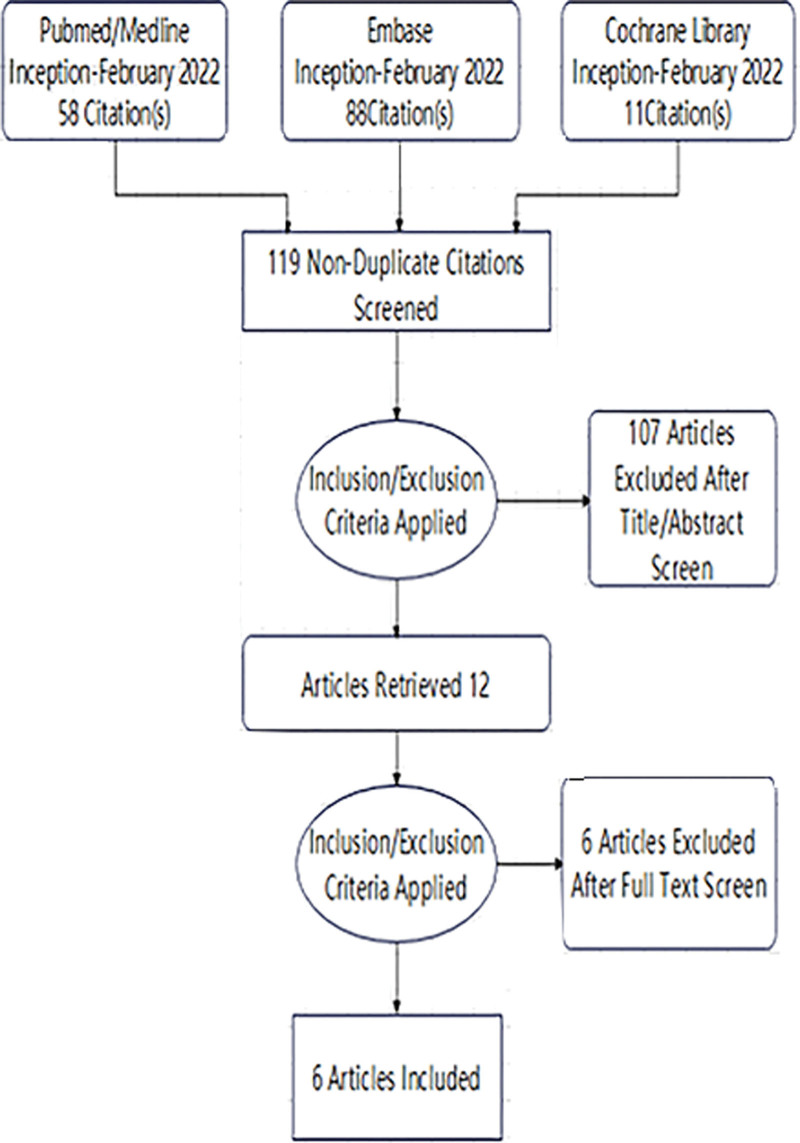
Six studies[14,16–20] were available after the initial screening and were included in the review (Fig. 1). Two studies were carried out in Italy, 1 in the UK, 1 in Poland, 1 in Portugal, and another in Spain. Three prospective studies, 2 retrospective series, and 1 randomized controlled trial were included. The publication bias of the studies was assessed by using the Review Manager program (Rev Manager 5.3) according to the Cochrane tool (Fig. 2). The characteristics of the literature and the outcome of quality appraisal of the trials are shown in Table 1.
Figure 1.
Flow diagram of the search strategy and study selection.
Figure 2.
Summary of review authors’ assessments of risk of bias for each Cochrane item and each included study.
Table 1.
Characteristics of included studies.
| Study | Country | Duration | Type | Type of sinus (primary/recurrent/acute) | Endoscopic technique | Conventional surgery | Follow-up (mo) | Study quality |
|---|---|---|---|---|---|---|---|---|
| Javed et al | UK | January 2015 to April 2016. | Retrospective | Acute | EPAT(n = 20) | Conventional incision(n = 20) | 3-6 | 15 |
| Milone et al | Italy | March 2011 to August 2013 | Prospective | Chronic non-recurrent | VAAPS (n = 40) | Sinusectomy (n = 40) |
60 | 21 |
| Romaniszyn et al | Poland. | 2013 to 2018 | Prospective | Recurrent | EPSiT (n = 26) | Limberg (n = 34) | 27 | 20 |
| Milone et al | Italy | January 2012 to December 2013. | RCT | Chronic nonrecurrent | VAAPS (n = 76) | Bascom cleft lift treatment (n = 69) | 60 | 5 |
| Sequeira et al | Portugal | January through December 2015 for conventionally treated patients January through December 2016 for EPSiT |
Retrospective | Chronic recurrent or nonrecurrent | PEPSiT (n = 21) | Excision followed by primary closure (EPC) (n = 63) |
11.9 (EPSiT) 24.7 (EPC) |
17 |
| Pérez-Bertólez et al | Spain | January to December 2019 | Prospective | PEPSiT (n = 14) | EHSI (n = 23), EPC (n = 12) |
14.8 | 19 |
EHSI = en-bloc excision and healing by secondary intention, EPSiT = endoscopic pilonidal sinus treatment, RCT = randomized controlled trial.
This study included 458 patients, 195 of whom received endoscopic treatment, and the remaining patients were treated using other surgical methods. Table 2 shows the specific demographic characteristics and results.
Table 2.
Patient’s demographic characteristics and results.
| Study | Age (yr) | Male (%)/M:F | Operating time(min) | VAS pain scores | Time of healing (d) | Complications | Recurrence | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| E | C | E | C | E | C | E | C | E | C | E | C | E | C | |||||
| Javed et al | 24 | 24 | NA | NA | 38.5 (29–47) | 13.5 (11–15) | 1 (1–2) | 2 (1–3) | 16 (14–24) | 35 (24.5–42) | NA | NA | 0 | 3 | ||||
| Milone et al | 26.49 ± 5.53 | 25.22 ± 6.04 | 82.5 | 75 | 44.39 ± 7.76 | 30.38 ± 6.23 | 1.4 ± 0.41 | 1.53 ± 0.3 | NA | NA | 5 | 12 | 3 | 10 | ||||
| Romaniszyn et al | 29.03 (20–47) | 28.55 (17–60) | 24:2 | 28:6 | 60 (25–80) | 67 (35–95) | NA | NA | 42 (31–77) | 21 (10–24) | 3 | 9 | 7 | 2 | ||||
| Milone et al 2020 | 25.5 ± 5.9 | 25.7 ± 5.3 | 78.9 | 78.3 | 42.9 ± 9.8 | 26.5 ± 8.7 | 1.65 ± 2.9 | 4.15 ± 4.9 | NA | NA | 4 | 7 | 18 | 16 | ||||
| Sequeira et al | 15.9 | 16.3 | 76.2 | 71.4 | 30 (20–90) | 38 (17–105) | NA | NA | 28 (15–270) | 37.5 (11–203) | 2 | 17 | 2 | 13 | ||||
| Pérez-Bertólez et al | 15.35 (13.73-16.56) |
EHSI n = 23 |
EPC n = 12 |
35.7 | 57.14 | NA | NA | 0.5 ± 0.8 | EHSI | EPC | EHSI (Weeks) | EPC (Weeks) |
0 | 16 | 7 | 0 | 0 | |
| 15.86 | 16.17 | 7.3 ± 2.4 | 7 ± 2.0 | 3.1 ± 0.8 | 14.9 ± 10.5 | 6.1 ± 4.6 | ||||||||||||
Data for the 3 articles (Javed et al/Romaniszyn et al/Sequeira et al) are presented as median, the rest as mean (SD). E = experimental group; C = controlled group; NA = not available; EHSI = en-bloc excision and healing by secondary intention; EPC = excision and primary closure.
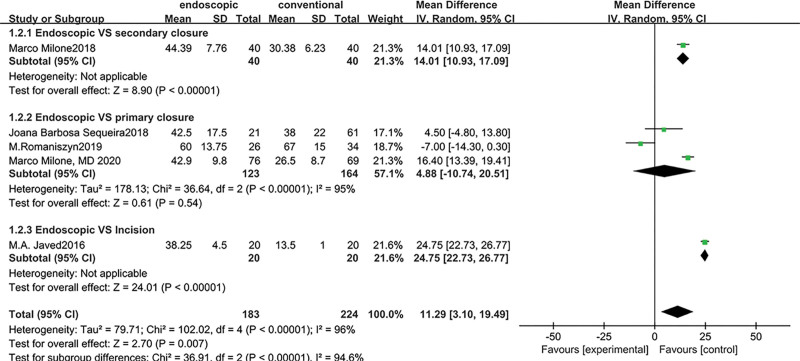
3.2. Operation time
Data on operative time was given in 5 studies. The EPSiT had a considerably longer operation time than conventional surgery, with a weighted mean difference of 11.29 (95 % CI: 3.10 to 19.49, I2 = 96%, P = .007). We divided it into 3 subgroups based on the surgical approaches. There was no significant difference between the EPSiT and the excision followed by the primary closure technique (including the flap technique) (P = .54) (Fig. 3).
Figure 3.
Forest plots of operative time in subgroup analysis by different surgical methods using a random-effect model. Each square represents the individual study’s mean score with a 95% CI indicated by the horizontal line. CI = confidence interval.
3.3. Disease recurrence
All trials included details on illness recurrence. The meta-analysis revealed a tendency toward a decreased incidence of recurrent conditions with endoscopic therapy, with a RR of 0.75, although this was not statistically significant (P = .55, 95 %CI [0.30–1.90]). Milone[21] advocated that a follow-up period of at least 5 years is the gold standard for assessing the effective recurrence rate of pilonidal sinus. So we ran a subgroup analysis based on follow-up time; both categories with endoscopic treatment had decreased recurrence rates, but the difference was not statistically significant. (follow-up = 5 years: RR = 0.62, 95%CI: 0.19–2.04, I2 = 69%, P = .43; follow-up < 5 years: RR = 0.84, 95%CI: 0.12–5.83, I2 = 71%, P = .86) (Fig. 4).
Figure 4.
Forest plots of recurrent rate in subgroup analysis by the length of follow-up using a random-effect model. Each square represents the individual study’s mean score with a 95% CI indicated by the horizontal line. CI = confidence interval.
3.4. Complications
Common complications after both procedures included wound infection (5.14% after EPSiT vs 12.03% after conventional surgery), wound dehiscence (0 vs 4.98%), seroma (0 vs 2.49%), hematoma (1.71 vs 0.83%), bleeding (0 vs 2.49%), granutoma (0 vs 2.07%), infection and dehiscence (0 vs 2.90%), and infection and bleeding (0 vs 0.41%). The EPSiT group had a considerably reduced overall rate of complications than the traditional surgery group (RR = 0.33 [0.19-0.58], P < .0001), according to the meta-analysis (Fig. 5).
Figure 5.
Forest plots of complications using a fixed-effect model. Each square represents the individual study’s mean score with a 95% CI indicated by the horizontal line. CI = confidence interval.
3.5. Postoperative pain
Four studies covered data on postoperative pain scores. Meta-analysis revealed that the EPSiT had a significantly lower pain score than conventional surgery, with a weighted mean difference of −2.44 (95%CI: (−3.96) to (−0.92), I2 = 99%, P = .002) (Fig. 6).
Figure 6.
Forest plots of postoperative pain score using a random-effect model. Each square represents the individual study’s mean score with a 95% CI indicated by the horizontal line. CI = confidence interval.
3.6. Full healing time
The study demonstrated no difference between the 2 bunches with a standard mean benefit of −0.57[(−2.55) to 1.41] (P = .57). We also performed subgroup analyses, but the results did not change (Fig. 7).
Figure 7.
Forest plots of full healing time in subgroup analysis by different surgical methods using a random-effect model. Each square represents the individual study’s mean score with a 95% CI indicated by the horizontal line. CI = confidence interval.
3.7. Quality of life and patient satisfaction
Only 2 studies reported patient satisfaction, and there was no difference between the 2 procedures (Fig. 8).
Figure 8.
Forest plots of satisfaction using a random-effect model. Each square represents the individual study’s mean score with a 95% CI indicated by the horizontal line. CI = confidence interval.
3.8. Cost
Only one experiment from Italy reported cost data, and endoscopic treatment was less expensive than other conventional procedures. Most other healthcare systems may not be able to use this finding.
3.9. Study bias
Funnel plots appeared to be no proof of publication inclination in this meta-analysis.
4. Discussion
Pilonidal sinus is a complex disorder that often occurs in young men. Not only does it cause discomfort to the patient, but it also imposes an economic burden on society. In recent years, various methods have been described demonstrating the complexity of treating pilonidal sinus. As for pilonidal abscess, the most effective emergency management is simple incision and drainage. However, surgical treatment of chronic and recurrent diseases remains disputable. Many studies suggested advocating one treatment over another, but the absence of comparison groups or short-term follow-up weakened the studies’ credibility. In addition, it reported that the long-term recurrence rates of recurrent pilonidal sinus varied from 10% to 30% after operative intervention.[22,23] It is still a challenge for surgeons. In the last few years, investigators have begun looking for more minimally invasive ways to treat the pilonidal sinus. In 2013, Meinero et al first proposed the endoscopic treatment of pilonidal sinus. Since then, many researchers have conducted prospective or retrospective studies on endoscopic treatment for pilonidal sinus. These studies[24–41] showed that endoscopic therapy was a safe, minimally invasive, and less complicated treatment method, but most were single-arm experiments. Therefore, we need more prospective randomized trials with adequate long-term follow-up to improve the body of evidence.
This study reviewed the outcomes of controlled clinical trials that compared endoscopic treatment to conventional treatment for PSD. The results of this study confirmed that endoscopic treatment provided some benefits indeed.
The most significant benefits of endoscopic therapy were minimal postoperative pain, a lower rate of complications, and return to routine for a shorter time. In our outcomes, only 5.14% of patients who accepted the endoscopic treatment suffered from wound infection, and the rate was lower than other conventional treatments. Thus, the postoperative healing time might be shortened. The findings agreed that endoscopic treatment was associated with a lower occurrence rate in terms of other complications. Other studies have shown a significant difference in infection rates between endoscopic treatment and conventional therapies. Endoscopic treatments may be a promising intervention based on our findings, as they showed lower rates of complications.
Nowadays, many surgeons recommend using off-midline primary closure with different flap techniques because they are more likely to improve patient outcomes. Based on this point, we performed the subgroup analysis according to the different techniques and compared the outcomes of endoscopic therapy with the primary closure technique (including the flap technique). In our results, the operative time was shorter in conventional techniques. However, we found no significant difference in operative time when the subgroup analysis was performed. We discovered no substantial difference between endoscopic treatment and conventional surgery in terms of recurrences, but there was a tendency toward fewer recurrences in favor of endoscopic treatment. Only 6 comparative studies cannot demonstrate the advantages of endoscopic therapy. Due to the lack of randomized prospective studies comparing the endoscopic technique to conventional treatment, it is impossible to rule in favor of any of these surgical methods.
Patients who had EPSiT could return to work faster than those who received primary closure or the open laying approach. This procedure also resulted in lower pain scores than previous methods. It also reduced the number of dressings required following surgery. Extrapolating, we can assume that sick leave expenses are lower in the case of endoscopy than in the case of other treatments. It could be beneficial to the general public’s health.
4.1. The limitations in our study
Although the quality of the literature included in this paper is high, the total number of literature is 6, and the number of literature and the sample size of some literature is small, which limits the strength of the demonstration of the results of this systematic review. More trials, particularly randomized trials, comparing endoscopic pilonidal sinus therapy to other conventional techniques are needed to assess surgical results with adequate follow-up. Moreover, to make more valid conclusions about the EPSiT’s effectiveness and safety.
5. Conclusions
Endoscopic pilonidal sinus treatment is a unique and potential method of SPD treatment. The foremost benefits of this technique are slight postoperative pain, lower complications rate, and return to routine for a shorter time. However, due to the limited number of articles, we need to conduct more rigorous large-sample prospective randomized controlled trials to clarify the efficiency of endoscopic treatment for pilonidal cysts.
Author contributions
Conceptualization: Guangyao Dai, Wen Chen, Mingxiang Wang.
Data curation: Sihan Chen, Xian Zhao, Jie Zhang, Chengpeng Yang.
Formal analysis: Sihan Chen, Peng Liu, Xin Xu.
Methodology: Sihan Chen, Guangyao Dai, Peng Liu, Liwei Wang.
Project administration: Guangyao Dai.
Resources: Guangyao Dai.
Software: Sihan Chen, Xian Zhao, Chengpeng Yang.
Supervision: Guangyao Dai.
Validation: Guangyao Dai.
Visualization: Sihan Chen.
Writing – original draft: Sihan Chen, Peng Liu, Dian Zhang.
Writing – review & editing: Peng Liu, Sihan Chen.
Abbreviations:
- CI =
- confidence interval
- EHSI =
- en-bloc excision and healing by secondary intention
- EPC =
- excision and primary closure
- EPSiT =
- endoscopic pilonidal sinus treatment
- ERAS =
- enhanced recovery after surgery
- NA =
- Not available
- PSD =
- pilonidal sinus disease
- RCT =
- randomized controlled trial
- RR =
- risk ratio
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
The authors have no conflicts of interest to disclose.
This work was supported by financial grants from the S & T Program of Shijiazhuang (211460493). The funder had no role in data curation, formal analysis, or writing of the report.
How to cite this article: Chen S, Dai G, Liu P, Zhao X, Zhang J, Yang C, Xu X, Wang L, Chen W, Wang M, Zhang D. Comparative analysis on the effect of the endoscopic versus conventional treatment for pilonidal sinus: A meta-analysis of controlled clinical trials. Medicine 2022;101:45(e31767).
Contributor Information
Sihan Chen, Email: 17603119182@163.com.
Peng Liu, Email: liupeng4287@126.com.
Xian Zhao, Email: 940815560@qq.com.
Jie Zhang, Email: 18832001136@163.com.
Chengpeng Yang, Email: yangchengpeng@163.com.
Xin Xu, Email: 387785864@qq.com.
Liwei Wang, Email: 89631847@qq.com.
Wen Chen, Email: 17603119182@163.com.
Mingxiang Wang, Email: 89631847@qq.com.
Dian Zhang, Email: 18832001136@163.com.
References
- [1].McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008;336:868–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Luedi MM, Schober P, Stauffer VK, et al. Global gender differences in pilonidal sinus disease: a random-effects meta-analysis. World J Surg. 2020;44:3702–9. [DOI] [PubMed] [Google Scholar]
- [3].de Parades V, Bouchard D, Janier M, et al. Pilonidal sinus disease. J Visc Surg. 2013;150:237–47. [DOI] [PubMed] [Google Scholar]
- [4].Pronk AA, Smakman N, Furnee E. Short-term outcomes of radical excision vs. phenolisation of the sinus tract in primary sacrococcygeal pilonidal sinus disease: a randomized-controlled trial. Tech Coloproctol. 2019;23:665–73. [DOI] [PubMed] [Google Scholar]
- [5].Mahmood F, Hussain A, Akingboye A. Pilonidal sinus disease: review of current practice and prospects for endoscopic treatment. Ann Med Surg (Lond). 2020;57:212–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Berthier C, Bérard E, Meresse T, Grolleau JL, et al. A comparison of flap reconstruction vs the laying open technique or excision and direct suture for pilonidal sinus disease: a meta-analysis of randomised studies. Int Wound J. 2019;16:1119–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Yang YP, Yu LY, Wang YZ, et al. Comparative analysis on the effect of Z-plasty versus conventional simple excision for the treatment of sacrococcygeal pilonidal sinus: a retrospective randomised clinical study. Int Wound J. 2020;17:555–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Hatch Q, Marenco C, Lammers D, et al. Postoperative outcomes of Bascom cleft lift for pilonidal disease: a single-center experience. Am J Surg. 2020;219:737–40. [DOI] [PubMed] [Google Scholar]
- [9].Prassas D, Rolfs TM, Schumacher FJ, et al. Karydakis flap reconstruction versus Limberg flap transposition for pilonidal sinus disease: a meta-analysis of randomized controlled trials. Langenbecks Arch Surg. 2018;403:547–54. [DOI] [PubMed] [Google Scholar]
- [10].Sinnott CJ, Glickman LT. Limberg flap reconstruction for sacrococcygeal pilonidal sinus disease with and without acute abscess: our experience and a review of the literature. Arch Plast Surg. 2019;46:235–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Immerman SC. The Bascom cleft lift as a solution for all presentations of pilonidal disease. Cureus. 2021;13:e13053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].el-Khadrawy O, Hashish M, Ismail K, et al. Outcome of the rhomboid flap for recurrent pilonidal disease. World J Surg. 2009;33:1064–8. [DOI] [PubMed] [Google Scholar]
- [13].Meinero P, Mori L, Gasloli G. Endoscopic pilonidal sinus treatment (E.P.Si.T.). Tech Coloproctol. 2014;18:389–92. [DOI] [PubMed] [Google Scholar]
- [14].Milone M, Velotti N, Manigrasso M, et al. Long-term results of a randomized clinical trial comparing endoscopic versus conventional treatment of pilonidal sinus. Int J Surg. 2020;74:81–5. [DOI] [PubMed] [Google Scholar]
- [15].Milone M, Fernandez LM, Musella M, et al. Safety and efficacy of minimally invasive video-assisted ablation of pilonidal sinus: a randomized clinical trial. JAMA Surg. 2016;151:547–53. [DOI] [PubMed] [Google Scholar]
- [16].Pérez-Bertólez S, Martín-Solé O, Moraleda I, et al. Advantages of endoscopic pilonidal sinus treatment. Cir Pediatr. 2021;34:191–9. [PubMed] [Google Scholar]
- [17].Javed MA, Fowler H, Jain Y, et al. Comparison of conventional incision and drainage for pilonidal abscess versus novel endoscopic pilonidal abscess treatment (EPAT). Tech Coloproctol. 2016;20:871–3. [DOI] [PubMed] [Google Scholar]
- [18].Sequeira JB, Coelho A, Marinho AS, et al. Endoscopic pilonidal sinus treatment versus total excision with primary closure for sacrococcygeal pilonidal sinus disease in the pediatric population. J Pediatr Surg. 2018;53:2003–7. [DOI] [PubMed] [Google Scholar]
- [19].Romaniszyn M, Swirta JS, Walega PJ. Long-term results of endoscopic pilonidal sinus treatment vs Limberg flap for treatment of difficult cases of complicated pilonidal disease: a prospective, nonrandomized study. Colorectal Dis. 2020;22:319–24. [DOI] [PubMed] [Google Scholar]
- [20].Milone M, Velotti N, Manigrasso M, et al. Video-assisted ablation of pilonidal sinus (VAAPS) versus sinusectomy for treatment of chronic pilonidal sinus disease: a comparative study. Updates Surg. 2019;71:179–83. [DOI] [PubMed] [Google Scholar]
- [21].Milone M, Velotti N, Manigrasso M, et al. Long-term follow-up for pilonidal sinus surgery: a review of literature with metanalysis. Surgeon. 2018;16:315–20. [DOI] [PubMed] [Google Scholar]
- [22].Doll D, Krueger CM, Schrank S, et al. Timeline of recurrence after primary and secondary pilonidal sinus surgery. Dis Colon Rectum. 2007;50:1928–34. [DOI] [PubMed] [Google Scholar]
- [23].Halleran DR, Lopez JJ, Lawrence AE, et al. Recurrence of pilonidal disease: our best is not good enough. J Surg Res. 2018;232:430–6. [DOI] [PubMed] [Google Scholar]
- [24].Foti N, Passannanti D, Libia A, et al. A minimally invasive approach to pilonidal disease with endoscopic pilonidal sinus treatment (EPSiT): a single-center case series with long-term results. Tech Coloproctol. 2021;25:1045–54. [DOI] [PubMed] [Google Scholar]
- [25].Giordano P, Schembari E, Keshishian K, et al. Negative pressure-assisted endoscopic pilonidal sinus treatment. Tech Coloproctol. 2021;25:739–43. [DOI] [PubMed] [Google Scholar]
- [26].Azhough R, Azari Y, Taher S, et al. Endoscopic pilonidal sinus treatment: a minimally invasive surgical technique. Asian J Endosc Surg. 2021;14:458–63. [DOI] [PubMed] [Google Scholar]
- [27].Kalaiselvan R, Liyanage A, Rajaganeshan R. Short-term outcomes of endoscopic pilonidal sinus treatment. Ann R Coll Surg Engl. 2020;102:94–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Probst M, Mezera V, Turnovský P, et al. Endoscopic pilonidal sinus treatment (E.P.Si.T.) - first experiences and results. Rozhl Chir. 2020;99:266–70. [DOI] [PubMed] [Google Scholar]
- [29].Gökbuget ZM, Özcan R, Karagöz A, et al. Endoscopic pilonidal sinus treatment (EPSiT) in the pediatric age group: Short-term results. Ulus Travma Acil Cerrahi Derg. 2021;27:443–8. [DOI] [PubMed] [Google Scholar]
- [30].Giarratano G, Toscana C, Shalaby M, et al. Endoscopic pilonidal sinus treatment: long-term results of a prospective series. JSLS. 2017;21:e2017.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Gulcu B, Ozturk E. Endoscopic pilonidal sinus treatment: rapid recovery, satisfactory success, and high quality of life. Surg Laparosc Endosc Percutan Tech. 2021;31:711–5. [DOI] [PubMed] [Google Scholar]
- [32].Gecim IE, Goktug UU, Celasin H. Endoscopic pilonidal sinus treatment combined with crystalized phenol application may prevent recurrence. Dis Colon Rectum. 2017;60:405–7. [DOI] [PubMed] [Google Scholar]
- [33].Manigrasso M, Velotti N, Sosa Fernandez LM, et al. Endoscopic approach to recurrent pilonidal sinus: a retrospective analysis. J Laparoendosc Adv Surg Tech A. 2021;31:1–5. [DOI] [PubMed] [Google Scholar]
- [34].Eastment J, Slater K. Outcomes of minimally invasive endoscopic pilonidal sinus surgery. Asian J Endosc Surg. 2020;13:324–8. [DOI] [PubMed] [Google Scholar]
- [35].Meinero P, Stazi A, Carbone A, et al. Endoscopic pilonidal sinus treatment: a prospective multicentre trial. Colorectal Dis. 2016;18:O164–70. [DOI] [PubMed] [Google Scholar]
- [36].Khafagy A, Al Haddad E, AlSabah S. The endoscopic treatment of pilonidal sinus disease: a short-term case-series study. Ann Saudi Med. 2019;39:192–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Meinero P, La Torre M, Lisi G, et al. Endoscopic pilonidal sinus treatment (EPSiT) in recurrent pilonidal disease: a prospective international multicenter study. Int J Colorectal Dis. 2019;34:741–6. [DOI] [PubMed] [Google Scholar]
- [38].Jain Y, Javed MA, Singh S, et al. Endoscopic pilonidal abscess treatment: a novel approach for the treatment of pilonidal abscess. Ann R Coll Surg Engl. 2017;99:134–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Mendes C, Ferreira L, Salim L. Brazilian and argentinean multicentric study in the surgical minimally invasive treatment of pilonidal cyst. Arq Bras Cir Dig. 2019;32:e1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Milone M, Musella M, Di Spiezio Sardo A, et al. Video-assisted ablation of pilonidal sinus: a new minimally invasive treatment--a pilot study. Surgery. 2014;155:562–6. [DOI] [PubMed] [Google Scholar]
- [41].Kalaiselvan R, Bathla S, Allen W, et al. Minimally invasive techniques in the management of pilonidal disease. Int J Colorectal Dis. 2019;34:561–8. [DOI] [PubMed] [Google Scholar]