Background:
Over the past 30 years, treatments from different disciplines have been applied to spastic cerebral palsy (SCP). However, few bibliometric studies have been conducted to date. This study explored the knowledge base, emerging hotspots, and future trends related to SCP treatment research using bibliometric analysis.
Methods:
Publications on SCP treatment included in the Web of Science Core Collection database between 1990 and 2020 were retrieved, and Medical Subject Headings terms were extracted from PubMed. Online bibliometric analysis website (http://bibliometric.com/), 2 pieces of software called “CiteSpace” and “VOSViewer” were used for quantitative analysis and knowledge map establishment.
Results:
A total of 1668 papers were retrieved from 1990 to 2020. The number of publications has increased annually. Developmental Medicine and Child Neurology is the most productive and the highest co-cited journal. The United States has been the largest contributor. Vrije Universiteit Amsterdam ranked first in the number of papers published among institutions that have conducted correlational research. Becher JG and Graham HK should be considered scholars who have made outstanding contributions. The knowledge base of the SCP treatment research field is thoughtfully constructed to promote understanding of the field.
Conclusion:
This bibliometric study identified global achievements, research hotspots, and trends of SCP treatment. They provide insights into the research field and valuable information for future scientific research and clinical treatment.
Keywords: bibliometrics analysis, research trends, spastic cerebral palsy, treatment, visualization
1. Introduction
Cerebral palsy (CP) is defined as a group of permanent disorders of movement and posture development due to non-progressive disturbances that occur in the developing fetal or infant brain.[1] Recent magnetic resonance imaging (MRI) studies have shown that common abnormalities include periventricular white matter lesions, focal ischemic/hemorrhagic lesions, diffuse encephalopathy, basal ganglia damage, and brain malformations.[2] The average prevalence of CP is 2 to 3 per 1000 live births. These values vary in selected patient groups, depending on the risk factors.[3,4] CP is clinically categorized into spastic, dyskinetic, and ataxic CP depending on the predominant motor disorder. Spastic CP (SCP) accounts for up to 80% of CP cases.[5] Children with SCP are prone to motor disorders, comorbidities, and secondary problems caused by motor disorders that threaten their growth, development, and quality of life.[6,7] The past 30 years since William J. Little first described CP have been the most exciting and productive period in the field of treatment. Patients with SCP and their families seek many forms of treatment, especially modalities that have the potential to improve motor function or sensation, such as pharmacotherapy, functional surgery, basic rehabilitation techniques, physical therapy, speech, and psychotherapy. However, the results show that the evidence of beneficial SCP treatment in recent decades is weak.[8,9] Therefore, a comprehensive review of this area is essential for both newcomers and old stagers who can benefit greatly from it.
Bibliometrics is an indispensable tool for studying the knowledge base in an academic field. It uses mathematical and statistical principles to quantitatively analyze the structure of knowledge, active themes, evolutionary trajectories, and emerging trends in a given field by studying literature systems and metrology characteristics.[10] Compared to traditional review methods, bibliometrics provides a more detailed and objective way of analysis to describe the evolution of a field, and can be used to comprehensively explore the impact of a set of research topics, a group of researchers, and a specific paper within the field and predicts the research trends or hotspots. Bibliometrics has been progressively applied to research in different fields, such as medicine and ecology, and has also played a vital role in formulating policy and clinical guidelines for various diseases.[11]
To the best of our knowledge, only a few bibliometric analyses have been performed in the field of SCP treatment before this study. We extracted bibliometric indicators from the data, including the number of publications, citation frequency, and Hirsch index,[12] and performed a comprehensive analysis to understand the knowledge base of research on SCP treatment and present future global trends.
2. Methods
2.1. Database sources and search strategy
First, Medical Subject Headings terms in the PubMed database were searched to identify search terms. Second, the Web of Science Core Collection (WoSCC) was selected as the original database with a long-standing collection of leading international academic journals that provide detailed publication information, especially references. Therefore, this study evaluated the WoSCC database of over 70.8 million documents. In this study, the searches were limited to articles and reviews, published in English. The literature search was conducted on the same day, October 24, 2021, to avoid bias caused by daily database updates. The detailed search strategy was presented in Table 1.
Table 1.
The topic search queries.
| Set | Search query | Result |
|---|---|---|
| #1 | TS=(Spastic Cerebral Palsy* OR Spastic Diplegia* OR Monoplegic Cerebral Palsy* OR Monoplegic Infantile Cerebral Palsy OR Quadriplegic Infantile Cerebral Palsy OR Diplegic Infantile Cerebral Palsy) | 4259 |
| #2 | TS=(Therapy* OR Treatment* OR disease management*) | 5,000,206 |
| #3 | #1 AND #2 | 1668 |
A total of 1668 documents were obtained (Supplementary material, Supplemental Digital Content, http://links.lww.com/MD/H883), including 30,570 references. We exported the complete records as plain text format files, and the exported records included a list of authors, article titles, publication dates, keywords, abstracts, and citations. Two researchers conducted screening that showed no duplicates. The above data were downloaded from public database, and no ethical issues were involved in the text. Hence, ethical approval was not necessary.
2.2. Statistical analysis
Both CiteSpace and VOSviewer are popular tools used to map scientific knowledge and have been adapted for bibliometric analysis in different disciplinary research areas.[13,14] Therefore, in this study, Citespace V5.8 was applied to analyze the collaborative network of journals, authors, countries, and institutions, as well as the highest cited articles with impact. The VOSviewer 1.6.15, which allows for the visualization of keyword co-occurrence and co-citation clustering, was used to create graphs. Furthermore, an online bibliometric analysis website (http://bibliometric.com/) was also used to visualize the number of publications in different years by country.
3. Result
3.1. Over trend
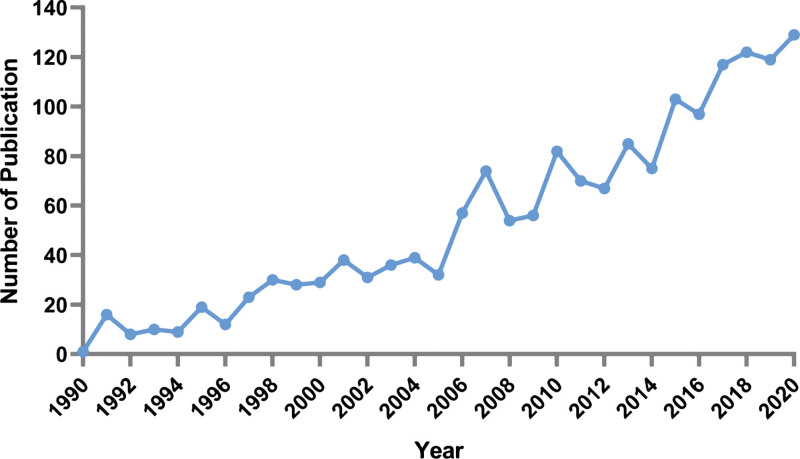
Over the past 30 years, the number of publications on SCP treatment has been steadily increasing annually, demonstrating growing academic interest in this field (Fig. 1). However, there is a noticeable difference between the periods 1990 to 2005 and 2006 to 2020. The first period grew smoothly, accounting for only 21.6% of the total number of publications with an average of 23 publications per year while the second period accounted for 78.4% with an average of 23 publications per year, reaching 129 publications in 2020. By and large, the publication trend over the past 30 years indicates that the treatment of SCP has received the attention of researchers from various disciplines.
Figure 1.
The annual number of publications. Horizontal coordinate: year; vertical coordinate: number of publications; blue line: annual number of publications.
3.2. Country distribution
The 1668 published papers were from 76 countries and regions, and the top 5 countries in the number of publications are the United States, the Netherlands, the United Kingdom, China, and Australia. Centrality is an indicator of node importance in a network; a higher centrality suggests a node with a greater impact. The top 5 countries in centrality (Table 2) are the US (0.59), the UK (0.21), France (0.21), Canada (0.2), and Germany (0.14.) Since 1990, the U.S. has published 33.15% of the total number of publications. We can see the participation and enrichment of more countries in this field of research globally in the 21st century.
Table 2.
Top 10 contributing countries.
| Rank | Country | Publications | Percentage | Centrality | Institution | Publications | Affiliation |
|---|---|---|---|---|---|---|---|
| 1 | USA | 553 | 33.15 | 0.59 | Vrije Universiteit Amsterdam | 59 | Netherlands |
| 2 | Netherlands | 112 | 6.72 | 0.05 | Ku Leuven | 38 | Belgium |
| 3 | England | 99 | 5.94 | 0.21 | University of California | 38 | USA |
| 4 | China | 98 | 5.88 | 0.00 | Nemours Alfred I Dupont Hospital For Children | 32 | USA |
| 5 | Australia | 94 | 5.64 | 0.11 | Royal Children s Hospital Melbourne | 32 | USA |
| 6 | Canada | 89 | 5.34 | 0.20 | Columbia University | 31 | Australia |
| 7 | Germany | 76 | 4.56 | 0.14 | University Hospital Leuven | 31 | Belgium |
| 8 | South Korea | 74 | 4.44 | 0.01 | Washington University Wustl | 31 | USA |
| 9 | Italy | 71 | 4.26 | 0.10 | Harvard University | 28 | USA |
| 10 | Brazil | 63 | 3.78 | 0.01 | Ruprecht Karls University Heidelberg | 27 | Germany |
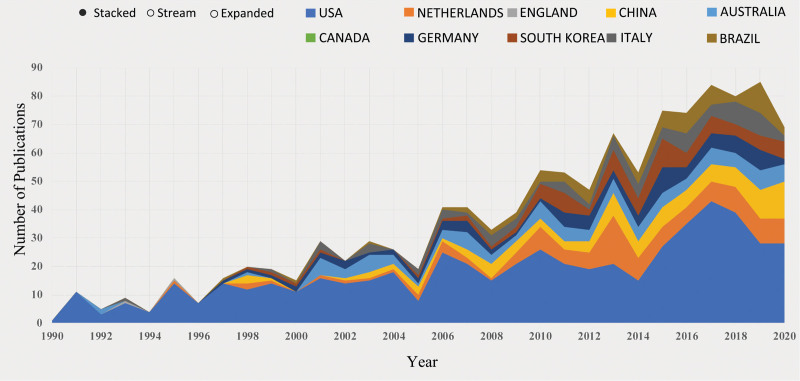
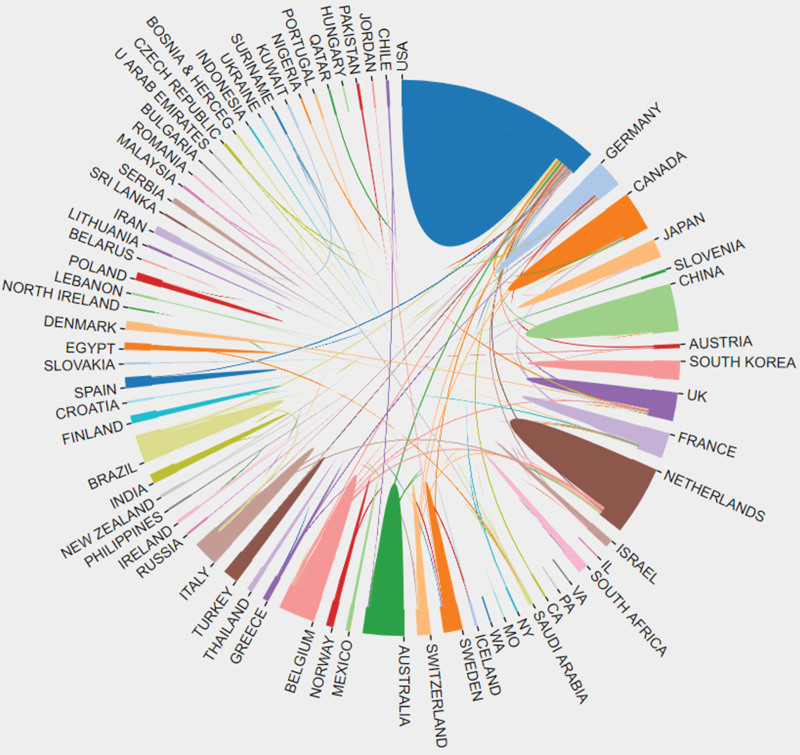
The analysis in terms of volume and centrality of publications shows that there is no doubt that the United States is the leader in this field (Fig. 2). We found that although developing countries such as China, Turkey, and Brazil published a considerable amount of literature, the intensity of cooperation with other countries was not high (Fig. 3), suggesting that developing countries should enhance international cooperation. Developed countries occupies a high number of seats. The reason for this distribution seems obvious: These developed countries have well-developed disciplines and infrastructure that can support the clinical studies more conveniently and successfully conducted by investigators, and in the meantime offer more new treatments than developing countries to improve current medical stresses when dealing with the health and survival pressures faced by SCP patients and their families.
Figure 2.
Growth trends of the top 10 contributing countries. Horizontal coordinate: year; vertical coordinate: number of publications; color: Country; area of color: number of publications.
Figure 3.
The network of cooperation between countries. Color block: Country; area of color block: number of publications; line between different color blocks: the presence of cooperation.
3.3. Institutional analysis
In total 652 institutions published constructive papers. Table 2 lists the top ten productive institutions with specific information. The Vrije Universiteit Amsterdam is the most published institution with 59 articles and a centrality of 0.05, indicating his great effort in this field. Five of the top ten institutions belong to the USA, indicating that American research institutions are crucial in the field of SCP treatment and that they may carry out more in-depth and pioneering work. Notably, 3 of the top ten ranked institutions are comprehensive health care providers. Nemours Alfred I. DuPont Hospital for Children is a major pediatric hospital in the United States and is known for its orthopedic and neurosurgical services. The Royal Children’s Hospital Melbourne is a specialized children’s hospital in Australia that combines health care and prevention of childhood and adolescent diseases. The Leuven University Hospital is the largest general university hospital in Belgium. These institutions are the mainstay of SCP treatment and have made tremendous contributions to patient nursing and the promotion of innovative therapies.
3.4. Author analysis
Table 3 lists the top ten most productive authors of SCP treatment studies. The productive authors are all concentrated in developed countries such as the USA, the Netherlands, and Germany, which means that most of the researchers are from developed countries, which is consistent with the results of the country distribution and institutional analysis. The author with the highest total number of articles was Becher JG from the Netherlands who published 30 articles with an Hirsch index of 15 and 695 citations. The highest total number of citations is Graham HK from the Royal Melbourne Children’s Hospital, Australia, with an average of 53.13 citations per year. Each article was cited 79.7 times. This indicates that these 2 scholars are authorities in the field and play an important role in leading the research frontier and advancing the knowledge base.
Table 3.
The top 10 productive authors.
| Rank | Author | Publications | H index | Total citations | Average citations | Affiliation |
|---|---|---|---|---|---|---|
| 1 | Becher JG | 30 | 15 | 695 | 23.17 | Netherlands |
| 2 | Desloovere K | 27 | 14 | 537 | 17.90 | Belgium |
| 3 | Miller F | 27 | 17 | 974 | 32.47 | USA |
| 4 | Molenaers G | 26 | 15 | 600 | 20.00 | Belgium |
| 5 | Gordon AM | 22 | 13 | 430 | 14.33 | USA |
| 6 | Dreher T | 21 | 12 | 378 | 12.60 | Switzerland |
| 7 | Graham HK | 20 | 17 | 1594 | 53.13 | Australia |
| 8 | Park TS | 17 | 11 | 325 | 10.83 | USA |
| 9 | Doderlein L | 16 | 12 | 367 | 12.23 | Germany |
| 10 | Wolf SI | 16 | 10 | 339 | 11.30 | Germany |
3.5. Journal analysis
833 journals were extracted from 1668 records using CiteSpace. «Developmental Medicine and Child Neurology» is leading the other journals for both citation frequency and centrality. This journal has contributed significantly to the treatment of SCP. The top 5 journals were listed in Table 4. It was interesting that 4 journals ranked in the top 5 for both the number of publications and co-citations, Developmental Medicine and Child Neurology, Journal of Pediatric Orthopaedics, gait Posture, and archives of Physical Medicine and Rehabilitation, respectively. The research results on SCP treatment are mainly published in these journals, which are considered core journals. They covered 54 categories including pediatrics, neuroscience, exercise, and sports science. Pediatrics ranked first, which is related to the fact that children are the main patients of SCP.[15]
Table 4.
The top 5 productive journals.
| Rank | Journal | Publications | Quartile in Category | Impact Factor | Research Domain | Hirsch index |
|---|---|---|---|---|---|---|
| 1 | Developmental Medicine and Child Neurology | 150 | Q1 | 5.449 | Clinical neurology; Pediatrics | 143 |
| 2 | Journal of Pediatric Orthopaedics | 69 | Q3/Q2 | 2.343 | Orthopedics; Pediatrics | 96 |
| 3 | Gait Posture | 52 | Q3/Q2 | 2.746 | Neurosciences; Orthopedics; Sport sciences | 148 |
| 4 | Archives of Physical Medicine and Rehabilitation | 37 | Q1/Q2 | 3.966 | Rehabilitation; Sport Sciences | 188 |
| 5 | Journal of Child Neurology | 34 | Q4/Q3 | 1.987 | Clinical Neurology; Pediatrics | 105 |
3.6. Highly co-cited references analysis
Table 5 shows the top ten co-cited publications in the field of SCP treatment, which were cited more than 160 times. Six of these were from the journal of Developmental Medicine and Child Neurology. The most cited article was “A systematic review of interventions for children with developmental medicine and child neurology,” published by Novak I from the University of Sydney in Developmental Medicine and Child Neurology in 2013, which has been cited 45 times, with an average of 6.45 times per year. This study systematically described 15 optimal interventions for childhood with CP.[16] Rank’s second paper suggested a revised definition of CP and content of the classification. Rank’s third paper revealed that selective dorsal rhizotomy combined with physical and occupational therapy resulted in significant improvements in motor function. Strong evidence was shown for botulinum toxin type A for the treatment of lower limb spasticity in CP in a fourth-ranked paper. Critically, randomized controlled trials (RCT) are deemed the most prevalent method for evaluating clinical validity and efficacy.[17] They are the most classical publications with great reference value and formed the theoretical and experiential basis of scientific studies citing them,[18] contributing to a comprehensive understanding of the treatment of CP.
Table 5.
The top 10 co-cited publications.
| Rank | Author | Year | Title | Journal | Citations | Average citations per year |
|---|---|---|---|---|---|---|
| 1 | Novak I, et al | 2013 | A systematic review of interventions for children with cerebral palsy: state of the evidence | Developmental Medicine and Child Neurology | 45 | 6.43 |
| 2 | Rosenbaum P, et al | 2007 | A report: the definition and classification of cerebral palsy – April 2006 | Developmental Medicine and Child Neurology | 33 | 2.54 |
| 3 | Wright FV, et al | 1998 | Evaluation of selective dorsal rhizotomy for the reduction of spasticity in cerebral palsy: a randomized controlled trial | Developmental Medicine and Child Neurology | 22 | 1.00 |
| 4 | Koman LA, et al | 2000 | Botulinum toxin type A neuromuscular blockade in the treatment of lower extremity spasticity in cerebral palsy: A randomized, double-blind, placebo-controlled trial | Journal of Pediatric Orthopedics | 22 | 1.10 |
| 5 | McLaughlin JF, et al | 1998 | Selective dorsal rhizotomy: efficacy and safety in an investigator-masked randomized clinical trial | Developmental Medicine and Child Neurology | 21 | 0.95 |
| 6 | Heinen F, et al | 2010 | The updated European Consensus 2009 on the use of Botulinum toxin for children with cerebral palsy | European Journal of Paediatric Neurology | 21 | 2.10 |
| 7 | Steinbok P, et al | 1997 | A randomized clinical trial to compare selective posterior rhizotomy plus physiotherapy with physiotherapy alone in children with spastic diplegic cerebral palsy | Developmental Medicine and Child Neurology | 20 | 0.87 |
| 8 | Bax M, et al | 2005 | Proposed definition and classification of cerebral palsy, April 2005 – Introduction | Developmental Medicine and Child Neurology | 20 | 1.33 |
| 9 | Graham HK, et al | 2000 | Recommendations for the use of botulinum toxin type A in the management of cerebral palsy | Gait Posture | 17 | 0.85 |
| 10 | Koman LA, et al | 2004 | Cerebral palsy | Lancet | 16 | 1.00 |
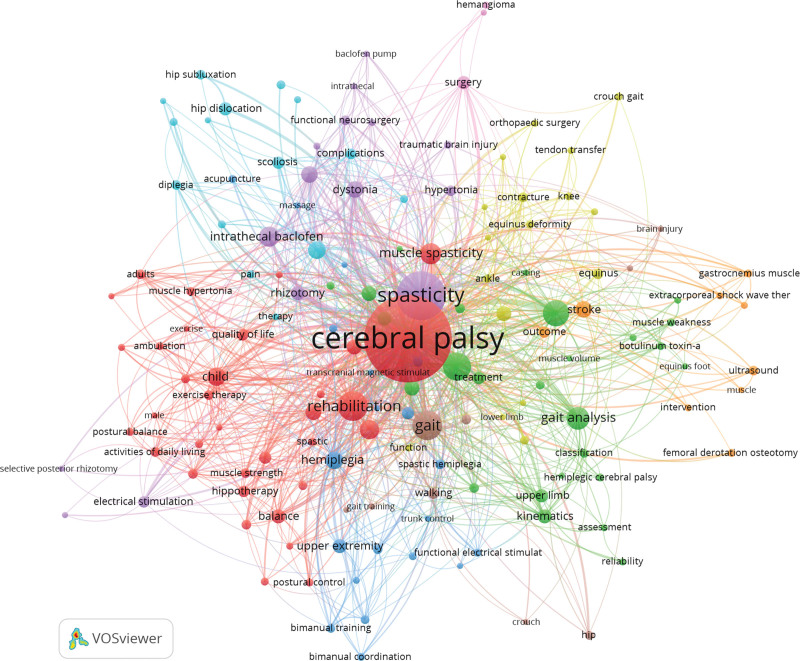
3.7. Keyword co-occurrence and co-citation clustering
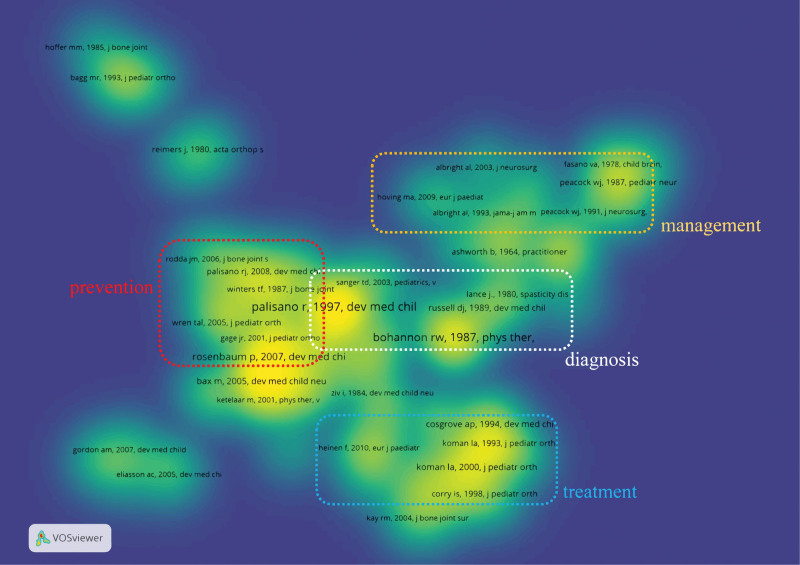
Keywords reflect a publication’s condensed topic and content. The presence of keywords in a series of publications suggests a close thematic relationship.[19] Co-citation clustering can also reveal the knowledge structure and relationship network of a particular domain, because references comprise the knowledge base.[20] Consequently, we combined studies with high significance to determine the core themes and structure of research on SCP treatment. Keyword co-occurrence and co-citation clustering graphs were created using VOSviewer (Figs. 4 and 5). The size of the circle represents the total frequency of the keywords and the line indicates the strength of the relationship between the 2 keywords in the SCP therapeutic area. In Figure 4, it can be seen that these keywords from the 1668 publications can be colored to determine their co-occurrence relationship. Similarly, as shown in Figure 5 the cited literature can be divided into 4 theme clusters with high relevance: Prevention, Diagnosis, Treatment, and Management. To better understand the 4 theme clusters, the representative keywords and cited literature included in each module are listed in Table 6.
Figure 4.
The network of keywords co-occurrence. Each circle represents a keyword; the larger the area of the circle; the more often this keyword appears, and the same color between different circles means that these keywords usually appear together, probably on the same research topic, and thus can be defined as a cluster.
Figure 5.
The network of co-citation clusters. Each title is a reference, and the relevance of each title is similar or different in color. The same color indicates high relevance, probably for the same research topic, and thus can be defined as a cluster.
Table 6.
Four clusters and their representative keywords and cited literature.
| Clusters | Keywords | Cited reference |
|---|---|---|
| Prevention | Prevention, Stroke, brain injury, complications, hip joint | 1. Predictors of outcome of distal rectus femoris transfer surgery in ambulatory children with cerebral palsy. 2. Hip surveillance in children with cerebral palsy. Impact on the surgical management of spastic hip disease. 3. Predicting gross motor function in cerebral palsy. |
| Diagnosis | Gait analysis, gross motor function, classification, motor function, infant, ultrasound, electromyography | 1. Development and reliability of a system to classify gross motor function in children with cerebral palsy 2. A report: the definition and classification of cerebral palsy April 2006 3. Proposed definition and classification of cerebral palsy, April 2005 |
| Treatment | Treatment, surgery, botulinum toxin, intrathecal baclofen, selective dorsal rhizotomy, effectiveness, reliability | 1. Management of Cerebral Palsy with Botulinum-A Toxin. 2. A systematic review of interventions for children with cerebral palsy: state of the evidence. 3. Evaluation of selective dorsal rhizotomy for the reduction of spasticity in cerebral palsy: a randomized controlled trial. |
| Management | Muscle strength, quality of life, balance, walking, young adult, adult | 1. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. 2. Impact of hippotherapy on gross motor function and quality of life in children with bilateral cerebral palsy: a randomized open-label crossover study. 3. Optimizing Nutrition and Bone Health in Children with Cerebral Palsy |
3.7.1. Cluster #1(Prevention).
CP is believed to originate from complex interactions between multiple risk factors. Inflammation before and after preterm birth, infection, hypoxicae, ischemia, and stroke during the antepartum and peripartum periods are major contributors to the risk of CP.[21] The probability of prevalence increases with the accumulation of these risk factors.[22,23] Most of the etiologies and high-risk factors for CP are well known and can be prevented. Adequate prenatal and postnatal care and interventions to prevent intrauterine infections are effective measures for reducing the incidence of preterm birth, low birth weight, and subsequent neurological abnormalities. Magnesium sulfate,[24,25] prenatal corticosteroids,[26] therapeutic hypothermia,[27,28] caffeine,[29] melatonin,[30] erythropoietin,[31] and stem cell[32] have been used in the last 3 decades for the prevention of CP. This has reduced the risk of developing CP. Monitoring procedures of the hip joint in infants also prevent the development of complications due to hip dislocation.[33] The incidence of CP has decreased over time in developed countries (Europe, Australia, the USA, etc.) owing to specific preventive and interventional measures.[34–36] However, up to 40% of CP cases do not have an identifiable cause.[37] Genetic etiologies regarding CP are constantly being discovered, and this revolutionary field may lead to the development of new prevention and treatment targets.[38] A revolutionary breakthrough would be made in this field, which would enhance our understanding of the causes of CP.
3.7.2. Cluster #2(Diagnosis)
Diagnosis should be made as early as possible which helps infants access early intervention and effective treatment resources.[39,40] The current literature in this cluster focused mainly on topics related to gait analysis, gross motor function, motor function, quality of life, and graded classification systems. The diagnosis of CP includes clinical diagnosis and assessment of motor function, which involves the use of neuroimaging, standardized neurology, and standardized motor assessment. High-quality evidence demonstrated the accuracy of these diagnostic tools. Before 5 months of corrected age, the most effective tools for predicting risk are The General Movements Assessment, MRI, and The Hammersmith Infant Neurological Examination (HINE) are the most effective methods for predicting CP. MRI and HINE are the most effective methods for predicting the risk of CP after 5 months of corrected age.[41,42] Even if an assessment of General Movements Assessment or MRI is not available in some low- and middle-income countries, it can be used for fairly accurate early diagnoses such as gait analysis, HINE, or cranial ultrasound, which provides objective information about the severity.[41–43] Clinicians need to identify motor disorders and screen for comorbidities that often accompany CP and provide timely prevention and intervention. The combination of at least 2 tools for accurate diagnosis is recommended because it allows patients to receive specific interventions and treatments as early as possible.[44] There is growing evidence that specific early interventions can maximize neural cell plasticity, and minimize deleterious modifications to muscle development and bone growth,[45] and the subsequent need for surgery.[46] To better assess prognosis, many functional classification systems have been developed,[47] the most widely used is the Gross Motor Function Classification System.
3.7.3. Cluster #3(Treatment)
The treatment of SCP is centered on specific symptoms of movement disorder. Spasticity is the most common movement disorder and has been the focus of recent academic literature. The major research in this cluster concentrated efforts on botulinum toxin, intrathecal baclofen, surgery, physiotherapy, effectiveness, and reliability. Treatment should consider the functional level and expectations of the families of patients with CP and select appropriate interventions to be performed within the International Classification of Functioning, Disability and Health. Initial treatment approaches included physiotherapy to improve spasticity,[48] which has been shown to improve large muscle motor skills and gait.[49] A recent study showed that repeated injections of Abobo botulinum toxin reduced muscle tone and significantly reduced upper limb spasticity in children with CP.[50,51] This is an attractive approach for improving spasticity in children with CP because it enables less invasive treatments. In addition, alternative treatment explored in the literature include intrathecal baclofen),[52] selective dorsal rhizotomy (intrathecal baclofen therapy is not available),[53] and extracorporeal shockwave therapy has been applied to the treatment of spasticity.[54] There are some limitations, however, it is still evaluating the effectiveness and reliability of these therapies by RCT.[8] Since the aim of treatment has tended to improve the quality of life of patients and their families rather than focusing simply on the improvement of individual functional indicators. The treatment should therefore focus on the management of a variety of comorbidities to seek a better quality of life.
3.7.4. Cluster #4(Management).
The ultimate goal of management is to improve the quality of life and social participation status of the patient and their caregivers beyond that achieved with standard therapy alone.[55] Relevant issues in this cluster included following keywords: Management, strength, gait, adults, comorbidities, balance, and quality of life. CP may be regarded as a static brain lesion that cause permanent motor impairment with ongoing comorbidities and secondary conditions.[56,57] The management of CP is strongly associated with evidence-based targeted interventions. Traditional evidence-based medical treatment for pain, epilepsy, sleep, vision, and hearing problems in CP has been suggested to improve child’s outcome.[58] This implies that multidisciplinary involvement in management and rehabilitation planning, as well as long-term monitoring, is required. It seems especially important for individuals with CP to evaluate motor function by observing muscle strength and balance ability, and thus determine whether they can participate more in social activities. Hence, strength training and fitness programs should be a part of their daily lives, such as robot-assisted gait and treadmill training.[59,60] Equally significant, support from parents is indispensable in management because they assist patients with strength training and avoid psychological problems. Spasticity, muscle strength, and gross motor function were measured using the modified ashworth scale, manual muscle testing, and Gross Motor Function Classification System to supplement other interventional approaches.[61]
3.8. Burst keywords analysis
CiteSpace has a burst detection module that can be used to determine the decrease or growth in a topic by detecting large changes in keywords over time. High-breaking keywords indicate that the interest of researchers is growing rapidly. The emergence, evolution, and decline of research topics and themes, as well as the shift in the focus of research hotspots, could be described by the introduction of burst analysis.[62,63] Figure 6 shows the top 29 keywords with high intensity and their dynamic evolution in the area of SCP treatment from 1990 to 2020. The blue line represents the time interval, and the red line represents the time of the keyword burst. Muscle strength, muscle spasticity, interrater reliability, balance, intervention, individual, intrathecal baclofen therapy, classification system, and multilevel surgery may be research hotspots in the future.
Figure 6.
Top 29 keywords with the strongest citation bursts. Year: the first occurrence of the keyword; strength: the larger the value, the stronger the emergence of the keyword; begin: the start time of the keyword burst; end: the end time of the keyword burst. The blue line represents the time interval and the red line represents the time of the keyword burst.
Overall, burst keyword analysis revealed a clear evolutionary progression of SCP treatment. First, the features of the overall study changed from macroscopic observations of clinical efficacy to more specific indicators. In the early stages, research on SCP treatment mainly focused on the rehabilitation of selective dorsal rhizotomy, botulinum toxin A, and baclofen, and gait analysis has been applied to clinical diagnosis and curative effect evaluation to improve patient management.[43] Scholars have redirected their emphasis to deeper comprehension and more specific content as a result of the rapid advancement of different disciplines such as motor function, muscle strength, feet, ankles, and upper limbs. This has led to the extension of research topics that are in line with modern scientific consensus. This includes the exploration and utilization of new therapies (induction of movement therapy, femoral de-rotation osteotomy, intrathecal baclofen), evaluation of the validity and reliability of clinical therapy based on RCT, and the establishment of a classification system and criteria for CP.
Second, SCP treatment research has evolved to represent various age-related characteristics, such as the burst words infant, young adult, and age. SCP is inevitably a lifelong disease owing to its incurable nature. Early studies focused on infants and children and considered SCP a pediatric disease. Healthcare faces difficulties in successfully transferring services from children to adults, with some neglect by adult patients.[64] To address these challenges, experts from different domains are actively helping researchers better define the etiology of CP and improve nursing standard for adult patients with SCP. Comprehensive care for adult patients with SCP is mirrored in general hospitals and adjuvant therapies have been expanded outside medical facilities.[65]
Third, the quality of life of the patients and their caregivers have been valued. In 2001, the World Health Organization published the International Classification of Functioning, Disability and Health, which emphasized that the purpose of treatment is not only to repair the disability and promote functional activity, but also to recognize that personal and environmental factors are indispensable for the well-being of individuals.[66] This initiative has had a huge influence on the direction of research, and social care has begun to emphasize quality of life.[67] The study of controlling muscle tone, increasing muscle strength, and improving gait posture has been transformed into a core point of SCP treatment, thus promoting functional activities and facilitating patient participation. Treatment goals and management of CP have shifted from treating impairment and disabilities to integrating elements of health, activity, and social participation.
Fourth, the planning, implementation, and verification of multidisciplinary services is a trend of SCP treatment. Emergent words included multiple surgeries, randomized controlled trials, and interrater reliability. On the 1 hand, the patient is an individual, and he/she should pay attention to a personalized treatment plan when he/she is treated. On the other hand, a patient is also a social group, and he needs help from society and more participation in social activities. Patients faced unpredictable clinical problems due to physical and psychological deficits. Involving a multidisciplinary team to refine various aspects of care, started in well-equipped and staffed institutions, can improve the appropriate diagnosis and treatment of patients with CP and ensure improved long-term results.[68] Efforts should be made to provide and sustain such medical services in developing countries. In addition, using an RCT to verify the validity and reliability of therapies is an integral part of the SCP treatment.
4. Discussion
This quantitative analysis identified trends in the treatment of SCP that can be considered when designing a treatment program. Evidence-based interventions can significantly improve the health of patients with SCP. Monitoring and ensuring these benefits, from suggestion to reality, is the joint effort of patients, caregivers, clinicians, and social workers. There is indeed a long way to go before the ultimate goal of SCP can be cured.[8] In addition, we found a research gap between developed and developing countries, in terms of the volume of publications, countries, and research institutions. This gap was reflected in the clinic, for example, the prevalence rate in high-income countries is 1.7 to 3.1 per 1000 live births, while it is higher in low-income countries.[69] Constraints on the availability of public resources for health care in developing countries limit access to necessary services.[70] The greater health and survival pressures on individuals with SCP and their families have forced countries to look for new ways to improve the current health care pressure. The following recommendations, which are based on the findings of the bibliometric analysis, may be useful for researchers and public health policymaking.
4.1. The significance of CP prevention
CP should be regarded as a public health priority for prevention to avoid a significant economic burden.[71] As pointed out by Nana Amankwah, Canadian dollars were about $11,700 for children with CP aged 1 to 4 years versus about $600 for those without the condition, and their quality of life was poor.[72] Moreover, children with CP in developing countries face greater economic, geographic, and social barriers in accessing medical and rehabilitative interventions. prevention would significantly reduce its prevalence.[21] However, the prevention of CP is infinitely challenging because it results from the interaction of multiple factors along a causal pathway. Many epidemiological studies are currently underway,[73] most of them are population- or registry-based and focus on identifying risk factors that will ultimately lead to the implementation of prevention strategies.
4.2. Seeking new treatments
At present, traditional therapies such as physical therapy, drug intervention, orthopedics, and neurosurgery are still mainstream, but the beneficial evidence is weak. There is an urgent need to discover new, safe and alternative approaches to deal with the current weak evidence of therapeutic benefits. Traditional Chinese medicine (TCM), including acupuncture, massage, Chinese herbal medicine, and other TCM methods, has attracted considerable attention for the treatment of CP. Specifically, TCM established individualized therapy to achieve the desired therapeutic effect by thoroughly considering the characteristics of each patient’s symptoms. In line with some studies’ reports on the benefits of enhancing nerve recovery and relieving spasms with TCM methods,[74,75] it was quite common in East Asian nations to use Chinese medicine to treat patients with CP.[76] More importantly, Acupuncture has emerged as a cost-effective and available treatment modality and could dramatically decrease health care expenditures.[77,78]
4.3. Information collection and sharing platform construction
Although CP is the most common childhood disability, its etiology remains complex and unknown. A large population base is needed to assemble a sufficient number of cases to answer the research questions, as the prevalence of CP is not very high even in moderately severe ischemic-hypoxic neonates and preterm infants, posing many difficulties for research.[79] Over the past decade, countries and institutions worldwide have made clearified the importance of information collection platform.[80] By collecting information on children with CP, aggregating data, analyzing changes in regional clinical practice, accessing healthcare, and further refining the way children with CP are described.[4] Simultaneously, a standard definition and classification system for CP have been established to provide targeted intervention activities for patients. To this end Europe, the United States, and Canada have established CP registry management organizations. This facilitated linking changes in prevalence to changes in prenatal, perinatal, and postnatal care to identify CP and its risk factors, and could also provide a sound basis for future treatment, management, and prevention of CP.
4.4. Update of social care model
Increasing evidence has shown that good parental care results are not applicable in low-and middle-income countries, and that the quality of life of patients and their caregivers is even worse.[81,82] Community-based health worker program is popular all over the world.[83] Community-based medical care and prevention provided by highly-skilled community members who have received different levels of formal or technical education is a highly effective and feasible nursing model for infants with CP. This model is highly scalable, transferable, and can be popularized in developing countries.[84] Therefore, equal emphasis should be placed on involving the local communities in the treatment and management of patients with CP. Skilled social workers and community workers can integrate better into the nursing teams. Such a public network can not only train parents with the latest medical and health knowledge to prevent CP[85] but can also help patients with CP learn and alleviate psychological disorders (e.g., depression, post-treatment stress disorder) to improve their health status and quality of life.[86] Community-based complementary therapies are being developed.[65]
5. Limitation
To our knowledge, this is the first study to perform a bibliometric analysis and visual display of SCP treatment. Our study had some limitations. First, owing to the limitation of the software, we only searched and analyzed English learning in WoSCC. Second, there are few documents from developing countries. However, these differences may not have changed the overall trends of this study.
6. Conclusion
Through a bibliometric analysis of 1668 related publications published from 1990 to 2020, this study attempts to outline the research hotspots and valuable viewpoints in the field of SCP treatment, as well as the global development trend of SCP treatment. The field of SCP treatment has entered a rapid development stage, which has attracted considerable attention worldwide. A total of 76 countries or regions contributed to this field. Most of the research was conducted in developed countries such as North America and Europe, and some developing countries also participated in it. More targeted research on people with SCP in developing countries is required. The research basement showed 4 theme clusters (prevention, diagnosis, treatment, and management) because the clustering pattern, is offered to better grasp the current global achievements and perspectives on future development. Finally, hot spots and trends could be confirmed by observing burst words, which may help shape the scientific research of researchers and clinical treatment planning of patients.
Acknowledgments
We appreciate the work of editors and anonymous reviewers. We also thank Prof Fuyuan He and M.S. Kaivin Deng for their guidance on the significance of this study.
Author contributions
Conceptualization: Dingfang Chen, Jin Zhou.
Data curation: Dingfang Chen, Yuefeng Wu.
Formal analysis: Dingfang Chen, Xue Pan.
Methodology: Dingfang Chen.
Project administration: HaiYing Li.
Supervision: Jin Zhou.
Visualization: Dingfang Chen.
Writing – original draft: Dingfang Chen.
Writing – review & editing: Jin Zhou.
Supplementary Material
Abbreviations:
- CP =
- cerebral palsy
- HINE =
- Hammersmith Infant Neurological Examination
- MRI =
- magnetic resonance imaging
- RCT =
- randomized controlled trial
- SCP =
- spastic CP
- TCM =
- traditional Chinese medicine
- WoSCC =
- Web of Science Core Collection
This work was supported by the National Natural Science Foundation of China (grant no. 81903759), Scientific Research Project of Hunan Provincial Department of Education (21A0256), ChangSha Science and Technology Bureau Project (kq2004059), Hunan Provincial Department of Education Science Research Project (21A0256), and Natural Science Foundation of Hunan Province (2022JJ80090).
The authors have no conflicts of interest to disclose.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Supplemental Digital Content is available for this article.
How to cite this article: Chen D, Wu Y, Li H, Pan X, Zhou J. Treatment on patients with spastic cerebral palsy in the past 30 years: A systematic review and bibliometric analysis. Medicine 2022;101:45(e30535).
Contributor Information
Dingfang Chen, Email: 20202666@stu.hnucm.edu.cn.
Yuefeng Wu, Email: 20203681@stu.hnucm.edu.cn.
HaiYing Li, Email: 1576970046@qq.com.
Xue Pan, Email: 405465029@qq.com.
References
- [1].Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol. 2007;109:8–14. [PubMed] [Google Scholar]
- [2].Robinson MN, Peake LJ, Ditchfield MR, Reid SM, Lanigan A, Reddihough DS. Magnetic resonance imaging findings in a population-based cohort of children with cerebral palsy. Dev Med Child Neurol. 2009;51:39–45. [DOI] [PubMed] [Google Scholar]
- [3].Van Naarden Braun K, Doernberg N, Schieve L, Christensen D, Goodman A, Yeargin-Allsopp M. Birth prevalence of cerebral palsy: a population-based study. Pediatrics. 2016;137:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Europe SoCPi. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Surveillance of Cerebral Palsy in Europe (SCPE). Dev Med Child Neurol. 2000;42:816–24. [DOI] [PubMed] [Google Scholar]
- [5].Vitrikas K, Dalton H, Breish D. Cerebral palsy: an overview. Am Fam Physician. 2020;101:213–20. [PubMed] [Google Scholar]
- [6].Surana BK, Ferre CL, Dew AP, Brandao M, Gordon AM, Moreau NG. Effectiveness of Lower-Extremity Functional Training (LIFT) in young children with unilateral spastic cerebral palsy: a randomized controlled trial. Neurorehabil Neural Repair. 2019;33:862–72. [DOI] [PubMed] [Google Scholar]
- [7].Borish CN, Bertucco M, Berger DJ, d’Avella A, Sanger TD. Can spatial filtering separate voluntary and involuntary components in children with dyskinetic cerebral palsy? PLoS One. 2021;16:e0250001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Colver A, Fairhurst C, Pharoah PO. Cerebral palsy. Lancet. 2014;383:1240–9. [DOI] [PubMed] [Google Scholar]
- [9].Noble JJ. Estimating muscle volume from two-dimensional measurements: a promising method for assessment. Dev Med Child Neurol. 2018;60:9–10. [DOI] [PubMed] [Google Scholar]
- [10].Agarwal A, Durairajanayagam D, Tatagari S, et al. Bibliometrics: tracking research impact by selecting the appropriate metrics. Asian J Androl. 2016;18:296–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gao Y, Wang Y, Zhai X, et al. Publication trends of research on diabetes mellitus and T cells (1997-2016): a 20-year bibliometric study. PLoS One. 2017;12:e0184869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Yuan M, Lin H, Wu H, Yu M, Tu J, Lü Y. Community engagement in public health: a bibliometric mapping of global research. Arch Pub Health. 2021;79:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Huang L, Shi X, Zhang N, et al. Bibliometric analysis of trends and issues in traditional medicine for stroke research: 2004-2018. BMC Compl Med Ther. 2020;20:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Yu Y, Li Y, Zhang Z, et al. A bibliometric analysis using VOSviewer of publications on COVID-19. Ann Transl Med. 2020;8:816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ruiz Brunner MLM, Cuestas E, Heinen F, Schroeder AS. Growth in infants, children and adolescents with unilateral and bilateral cerebral palsy. Sci Rep. 2022;12:1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Novak I, McIntyre S, Morgan C, et al. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol. 2013;55:885–910. [DOI] [PubMed] [Google Scholar]
- [17].Wiart L, Rosychuk RJ, Wright FV. Evaluation of the effectiveness of robotic gait training and gait-focused physical therapy programs for children and youth with cerebral palsy: a mixed methods RCT. BMC Neurol. 2016;16:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Camarasa C, Nageli C, Ostermeyer Y, Klippel M, Botzler S. Diffusion of energy efficiency technologies in European residential buildings: a bibliometric analysis. Energy Build. 2019;202:109339. [Google Scholar]
- [19].RachBeisel J, Scott J, Dixon L. Co-occurring severe mental illness and substance use disorders: a review of recent research. Psychiatr Serv. 1999;50:1427–34. [DOI] [PubMed] [Google Scholar]
- [20].Li XW, Du JG, Long HY. A comparative study of Chinese and Foreign Green development from the perspective of mapping knowledge domains. Sustainability. 2018;10:4357. [Google Scholar]
- [21].Korzeniewski SJ, Slaughter J, Lenski M, Haak P, Paneth N. The complex aetiology of cerebral palsy. Nat Rev Neurol. 2018;14:528–43. [DOI] [PubMed] [Google Scholar]
- [22].Zheng J, Wei C, Zhao M, Zhao D. Phototherapy is associated with the decrease in serum globulin levels in neonatal hyperbilirubinemia. Biomed Rep. 2019;10:63–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Schneider RE, Ng P, Zhang X, et al. The association between maternal age and cerebral palsy risk factors. Pediatr Neurol. 2018;82:25–8. [DOI] [PubMed] [Google Scholar]
- [24].Rouse DJ, Hirtz D; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. What we learned about the role of antenatal magnesium sulfate for the prevention of cerebral palsy. Semin Perinatol. 2016;40:303–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Rouse DJ, Hirtz DG, Thom E, et al. ; Eunice Kennedy Shriver NICHD Maternal-Fetal Medicine Units Network. A randomized, controlled trial of magnesium sulfate for the prevention of cerebral palsy. N Engl J Med. 2008;359:895–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Shepherd E, Salam RA, Middleton P, et al. Antenatal and intrapartum interventions for preventing cerebral palsy: an overview of Cochrane systematic reviews. Cochr Database Syst Rev. 2017;8:Cd012077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Chandrasekaran M, Swamy R, Ramji S, Shankaran S, Thayyil S. Therapeutic hypothermia for neonatal encephalopathy in Indian Neonatal units: a survey of national practices. Indian Pediatr. 2017;54:969–70. [DOI] [PubMed] [Google Scholar]
- [28].Thayyil S, Oliveira V, Lally PJ, et al. ; HELIX Trial group. Hypothermia for encephalopathy in low and middle-income countries (HELIX): study protocol for a randomised controlled trial. Trials. 2017;18:432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Al Hazzani F. Survival without disability to age 5 years after neonatal caffeine therapy for apnea of prematurity. J Clin Neonatol. 2012;1:64–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Wilkinson D, Shepherd E, Wallace EM. Melatonin for women in pregnancy for neuroprotection of the fetus. Cochrane Database Syst Rev. 2016;3:Cd010527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Fischer HS, Reibel NJ, Bührer C, Dame C. Prophylactic early erythropoietin for neuroprotection in preterm infants: a meta-analysis. Pediatrics. 2017;139:e20164317. [DOI] [PubMed] [Google Scholar]
- [32].Kiasatdolatabadi A, Lotfibakhshaiesh N, Yazdankhah M, et al. The role of stem cells in the treatment of cerebral palsy: a review. Mol Neurobiol. 2017;54:4963–72. [DOI] [PubMed] [Google Scholar]
- [33].Huser A, Mo M, Hosseinzadeh P. Hip surveillance in children with cerebral palsy. Orthop Clin North Am. 2018;49:181–90. [DOI] [PubMed] [Google Scholar]
- [34].Reid SM, Meehan E, McIntyre S, Goldsmith S, Badawi N, Reddihough DS; Australian Cerebral Palsy Register Group. Temporal trends in cerebral palsy by impairment severity and birth gestation. Dev Med Child Neurol. 2016;58(Suppl 2):25–35. [DOI] [PubMed] [Google Scholar]
- [35].Sellier E, Platt MJ, Andersen GL, Krägeloh-Mann I, De La Cruz J, Cans C; Surveillance of Cerebral Palsy Network. Decreasing prevalence in cerebral palsy: a multi-site European population-based study, 1980 to 2003. Dev Med Child Neurol. 2016;58:85–92. [DOI] [PubMed] [Google Scholar]
- [36].Andersen GL, Romundstad P, De La Cruz J, et al. Cerebral palsy among children born moderately preterm or at moderately low birthweight between 1980 and 1998: a European register-based study. Dev Med Child Neurol. 2011;53:913–9. [DOI] [PubMed] [Google Scholar]
- [37].Numata Y, Onuma A, Kobayashi Y, et al. Brain magnetic resonance imaging and motor and intellectual functioning in 86 patients born at term with spastic diplegia. Dev Med Child Neurol. 2013;55:167–72. [DOI] [PubMed] [Google Scholar]
- [38].Jin SC, Lewis SA, Bakhtiari S, et al. Mutations disrupting neuritogenesis genes confer risk for cerebral palsy. Nat Genet. 2020;52:1046–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Baird G, McConachie H, Scrutton D. Parents’ perceptions of disclosure of the diagnosis of cerebral palsy. Arch Dis Child. 2000;83:475–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Rentinck IC, Ketelaar M, Schuengel C, et al. Short-term changes in parents’ resolution regarding their young child’s diagnosis of cerebral palsy. Child Care Health Dev. 2010;36:703–8. [DOI] [PubMed] [Google Scholar]
- [41].Bosanquet M, Copeland L, Ware R, Boyd R. A systematic review of tests to predict cerebral palsy in young children. Dev Med Child Neurol. 2013;55:418–26. [DOI] [PubMed] [Google Scholar]
- [42].Romeo DM, Ricci D, Brogna C, Mercuri E. Use of the Hammersmith infant neurological examination in infants with cerebral palsy: a critical review of the literature. Dev Med Child Neurol. 2016;58:240–5. [DOI] [PubMed] [Google Scholar]
- [43].Baker R, Esquenazi A, Benedetti MG, Desloovere K. Gait analysis: clinical facts. Eur J Phys Rehabil Med. 2016;52:560–74. [PubMed] [Google Scholar]
- [44].Skiöld B, Eriksson C, Eliasson AC, Adén U, Vollmer B. General movements and magnetic resonance imaging in the prediction of neuromotor outcome in children born extremely preterm. Early Hum Dev. 2013;89:467–72. [DOI] [PubMed] [Google Scholar]
- [45].Damiano DL, Longo E. Early intervention evidence for infants with or at risk for cerebral palsy: an overview of systematic reviews. Dev Med Child Neurol. 2021;63:771–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Dobson F, Boyd RN, Parrott J, Nattrass GR, Graham HK. Hip surveillance in children with cerebral palsy. Impact on the surgical management of spastic hip disease. J Bone Joint Surg Br. 2002;84:720–6. [DOI] [PubMed] [Google Scholar]
- [47].Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23. [DOI] [PubMed] [Google Scholar]
- [48].Sakzewski L, Ziviani J, Boyd RN. Efficacy of upper limb therapies for unilateral cerebral palsy: a meta-analysis. Pediatrics. 2014;133:e175–204. [DOI] [PubMed] [Google Scholar]
- [49].Franki I, Bar-On L, Molenaers G, et al. Tone reduction and physical therapy: strengthening partners in treatment of children with spastic cerebral palsy. Neuropediatrics. 2020;51:89–104. [DOI] [PubMed] [Google Scholar]
- [50].Gracies JM, Brashear A, Jech R, et al. ; International AbobotulinumtoxinA Adult Upper Limb Spasticity Study Group. Safety and efficacy of abobotulinumtoxinA for hemiparesis in adults with upper limb spasticity after stroke or traumatic brain injury: a double-blind randomised controlled trial. Lancet Neurol. 2015;14:992–1001. [DOI] [PubMed] [Google Scholar]
- [51].Delgado MR, Tilton A, Carranza-Del Río J, et al. ; Dysport in PUL study group. Efficacy and safety of abobotulinumtoxinA for upper limb spasticity in children with cerebral palsy: a randomized repeat-treatment study. Dev Med Child Neurol. 2021;63:592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Reis PV, Vieira CR, Midões AC, Rebelo V, Barbosa P, Gomes A. Intrathecal Baclofen infusion pumps in the treatment of spasticity: a retrospective cohort study in a Portuguese Centre. Acta Med Port. 2019;32:754–9. [DOI] [PubMed] [Google Scholar]
- [53].Velnar T, Spazzapan P, Rodi Z, Kos N, Bosnjak R. Selective dorsal rhizotomy in cerebral palsy spasticity – a newly established operative technique in Slovenia: a case report and review of literature. World J Clin Cases. 2019;7:1133–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Oh JH, Park HD, Han SH, Shim GY, Choi KY. Duration of treatment effect of extracorporeal shock wave on spasticity and subgroup-analysis according to number of shocks and application site: a meta-analysis. Ann Rehabil Med. 2019;43:163–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Roebroeck ME, Jahnsen R, Carona C, Kent RM, Chamberlain MA. Adult outcomes and lifespan issues for people with childhood-onset physical disability. Dev Med Child Neurol. 2009;51:670–8. [DOI] [PubMed] [Google Scholar]
- [56].Ostojic K, Paget SP, Morrow AM. Management of pain in children and adolescents with cerebral palsy: a systematic review. Dev Med Child Neurol. 2019;61:315–21. [DOI] [PubMed] [Google Scholar]
- [57].Speyer R, Cordier R, Kim JH, Cocks N, Michou E, Wilkes-Gillan S. Prevalence of drooling, swallowing, and feeding problems in cerebral palsy across the lifespan: a systematic review and meta-analyses. Dev Med Child Neurol. 2019;61:1249–58. [DOI] [PubMed] [Google Scholar]
- [58].Novak I, Hines M, Goldsmith S, Barclay R. Clinical prognostic messages from a systematic review on cerebral palsy. Pediatrics. 2012;130:e1285–312. [DOI] [PubMed] [Google Scholar]
- [59].Ammann-Reiffer C, Bastiaenen CH, Meyer-Heim AD, van Hedel HJ. Effectiveness of robot-assisted gait training in children with cerebral palsy: a bicenter, pragmatic, randomized, cross-over trial (PeLoGAIT). BMC Pediatr. 2017;17:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Valentín-Gudiol M, Mattern-Baxter K, Girabent-Farrés M, Bagur-Calafat C, Hadders-Algra M, Angulo-Barroso RM. Treadmill interventions in children under six years of age at risk of neuromotor delay. Cochrane Database Syst Rev. 2017;7:Cd009242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Park EY, Kim WH. Effect of neurodevelopmental treatment-based physical therapy on the change of muscle strength, spasticity, and gross motor function in children with spastic cerebral palsy. J Phys Ther Sci. 2017;29:966–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Liu S, Sun YP, Gao XL, Sui Y. Knowledge domain and emerging trends in Alzheimer’s disease: a scientometric review based on CiteSpace analysis. Neural Regener Res. 2019;14:1643–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Li R, Sun J, Hu H, et al. Research trends of acupuncture therapy on knee osteoarthritis from 2010 to 2019: a bibliometric analysis. J Pain Res. 2020;13:1901–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Ko B, McEnery G. The needs of physically disabled young people during transition to adult services. Child Care Health Dev. 2004;30:317–23. [DOI] [PubMed] [Google Scholar]
- [65].Taylor NF, Dodd KJ, Baker RJ, Willoughby K, Thomason P, Graham HK. Progressive resistance training and mobility-related function in young people with cerebral palsy: a randomized controlled trial. Dev Med Child Neurol. 2013;55:806–12. [DOI] [PubMed] [Google Scholar]
- [66].WHO. International Classification of Functioning, Disability and Health. Geneva, Switzerland: World Health Organisation, 2001. [Google Scholar]
- [67].Makris T, Dorstyn D, Crettenden A. Quality of life in children and adolescents with cerebral palsy: a systematic review with meta-analysis. Disabil Rehabil. 2021;43:299–308. [DOI] [PubMed] [Google Scholar]
- [68].Bulekbayeva S, Daribayev Z, Ospanova S, Vento S. Cerebral palsy: a multidisciplinary, integrated approach is essential. Lancet Global Health. 2017;5:e401. [DOI] [PubMed] [Google Scholar]
- [69].Khandaker G, Smithers-Sheedy H, Islam J, et al. Bangladesh Cerebral Palsy Register (BCPR): a pilot study to develop a national cerebral palsy (CP) register with surveillance of children for CP. BMC Neurol. 2015;15:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Schachinger F, Farr S. The effects of preterm birth on musculoskeletal health-related disorders. J Clin Med. 2021;10:50825082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Shih STF, Tonmukayakul U, Imms C, et al. Economic evaluation and cost of interventions for cerebral palsy: a systematic review. Dev Med Child Neurol. 2018;60:543–58. [DOI] [PubMed] [Google Scholar]
- [72].Amankwah N, Oskoui M, Garner R, et al. Cerebral palsy in Canada, 2011-2031: results of a microsimulation modelling study of epidemiological and cost impacts. Health Promotion Chronic Dis Prev Canada. 2020;40:25–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Jöud A, Sehlstedt A, Källén K, Westbom L, Rylander L. Associations between antenatal and perinatal risk factors and cerebral palsy: a Swedish cohort study. BMJ Open. 2020;10:e038453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Gao J, He L, Yu X, et al. Rehabilitation with a combination of scalp acupuncture and exercise therapy in spastic cerebral palsy. Complement Ther Clin Pract. 2019;35:296–300. [DOI] [PubMed] [Google Scholar]
- [75].Ghafoor U, Lee JH, Hong KS, Park SS, Kim J, Yoo HR. Effects of acupuncture therapy on MCI patients using functional near-infrared spectroscopy. Front Aging Neurosci. 2019;11:237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Liao HH, Yen HR, Muo CH, et al. Complementary traditional Chinese medicine use in Children with cerebral palsy: a nationwide retrospective cohort study in Taiwan. BMC Complement Altern Med. 2017;17:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Nicolian S, Butel T, Gambotti L, et al. Cost-effectiveness of acupuncture versus standard care for pelvic and low back pain in pregnancy: a randomized controlled trial. PLoS One. 2019;14:e0214195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Taylor P, Pezzullo L, Grant SJ, Bensoussan A. Cost-effectiveness of acupuncture for chronic nonspecific low back pain. Pain Pract. 2014;14:599–606. [DOI] [PubMed] [Google Scholar]
- [79].Perra O, Rankin J, Platt MJ, et al. Decreasing cerebral palsy prevalence in multiple births in the modern era: a population cohort study of European data. Arch Dis Child Fetal Neonatal Ed. 2021;106:125–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Koy A, Timmermann L. Deep brain stimulation in cerebral palsy: challenges and opportunities. Eur J Paediatr Neurol. 2017;21:118–21. [DOI] [PubMed] [Google Scholar]
- [81].Thrush A, Hyder AA, Hyder A. The neglected burden of caregiving in low- and middle-income countries. Disability Health J. 2014;7:262–72. [DOI] [PubMed] [Google Scholar]
- [82].Vadivelan K, Sekar P, Sruthi SS, Gopichandran V. Burden of caregivers of children with cerebral palsy: an intersectional analysis of gender, poverty, stigma, and public policy. BMC Public Health. 2020;20:645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Benfer KA, Novak I, Morgan C, et al. Community-based parent-delivered early detection and intervention programme for infants at high risk of cerebral palsy in a low-resource country (Learning through Everyday Activities with Parents (LEAP-CP): protocol for a randomised controlled trial. BMJ Open. 2018;8:e021186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Scott K, Beckham SW, Gross M, et al. What do we know about community-based health worker programs? A systematic review of existing reviews on community health workers. Human Res Health. 2018;16:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Dada S, Tunçalp O, Portela A, Barreix M, Gilmore B. Community mobilization to strengthen support for appropriate and timely use of antenatal and postnatal care: a review of reviews. J Glob Health. 2021;11:04076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Dambi JM, Jelsma J. The impact of hospital-based and community based models of cerebral palsy rehabilitation: a quasi-experimental study. BMC Pediatr. 2014;14:301. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.