Background:
Ankle sprains occur very frequently in daily life, but people who do not pay attention to them and do not receive proper diagnosis and treatment are very prone to develop chronic ankle lateral instability (CALI) at a later stage. For CALI where conservative treatment has failed, reconstruction of the lateral collateral ligament of the ankle can achieve satisfactory results, but there are various and controversial ways of ligament reconstruction. While percutaneous reconstruction of ankle lateral ligament (PLCLR) needs to be performed repeatedly under fluoroscopy, total arthroscopic reconstruction of ankle lateral ligament (ALCLR) is increasingly recognized by experts and scholars for its minimally invasive and precise characteristics, and has achieved good clinical results. Therefore, it is imperative that a meta-analysis be performed to provide evidence as to whether there is a difference between ALCLR and PLCLR in the treatment of CALI.
Methods:
We will search articles in 7 electronic databases including Chinese National Knowledge Infrastructure, Wanfang Data, Chinese Scientific Journals Database, Chinese databases SinoMed, PubMed, Embase, and Cochrane Library databases. All the publications, with no time restrictions, will be searched without any restriction of language and status, the time from the establishment of the database to September 2022.We will apply the risk-of-bias tool of the Cochrane Collaboration for Randomized Controlled Trials to assess the methodological quality. Risk-of-Bias Assessment Tool for Non-randomized Studies was used to evaluate the quality of comparative studies. Statistical analysis will be conducted using RevMan 5.4 software.
Results:
This systematic review will evaluate the functional outcomes and radiographic results of ALCLR in the treatment of CALI.
Conclusion:
The conclusion of this study will provide evidence for judging whether ALCLR is superior to PLCLR for treatment of CALI.
Trial registration number:
CRD42022362045.
Keywords: arthroscopic reconstruction of ankle lateral ligament, chronic ankle lateral instability, percutaneous reconstruction of ankle lateral ligament, protocol
1. Introduction
Up to 50% to 70% of patients may develop chronic ankle lateral instability later after ankle sprains.[1] The most frequent injury from sprains is to the lateral collateral ligament of the ankle, including the anterior talofibular ligament (ATFL), which has the highest rate of injury, and the calcaneofibular ligament (CFL), which has a 50% to 75% probability of injury.[2] Acute ankle sprains that are not properly diagnosed and treated late will pose a risk of ankle instability, which can lead to chronic ankle instability, resulting in pain and limited motion and accelerated joint degeneration.[3–5] With increasing attention to ankle sprains, early treatment with more standardized treatment can effectively reduce the probability of late ankle instability.[6,7] However, due to the degree of injury to the lateral collateral ligament of the ankle, many patients still develop chronic ankle instability, and then surgery is required to restore ankle stability.[8,9]
Since most of the ligaments in patients with chronic lateral ankle instability cannot be repaired, surgical treatment usually requires reconstruction of the ATFL and CFL ligaments to restore joint stability.[10–12] Currently, due to the prevalence of minimally invasive concepts, the main methods of ligament reconstruction are percutaneous reconstruction and arthroscopic reconstruction.[13–15] Percutaneous reconstruction often requires repeated x-ray fluoroscopic confirmation, which will undoubtedly increase the operative time and aggravate the damage to the medical staff and patients.[16,17] However, due to the rapid development of arthroscopic techniques, more and more experts and scholars have mastered the all-scopic reconstruction of ATFL and CFL ligaments.[18,19] Arthroscopy allows for the combined management of intra-articular injuries, such as cartilage damage and free body formation due to repeated impingement; in addition, arthroscopy allows for the precise localization of the ligament footprint area, reducing the number of x-ray fluoroscopies and avoiding increased operative time and physical damage.[20,21]
However, due to the increasing number of relevant studies published in recent years, the lack of high-level guidelines and evidence-based medical evidence has seriously affected clinical decision making and application. In this study, we attempted to conduct a meta-analysis of relevant studies to evaluate and compare the functional outcomes and complication rates of arthroscopic reconstruction of ankle lateral ligament with percutaneous reconstruction of ankle lateral ligament for chronic ankle lateral instability, and our findings are expected to provide a reference for guiding future treatment options.
2. Methods
2.1. Study registration
We have prospectively registered this research at the international prospective register of systematic reviews-Registration number: CRD42022362045. We performed this protocol based on the Preferred Reporting Items for Systematic Review and Meta-analysis Protocols (PRISMA-P) statement guidelines.[22]
2.2. Inclusion criteria
2.2.1. Type of participants.
The participants diagnosed as chronic ankle lateral instability will be included regardless their country, ethnicity, sex, occupation and mechanism of injury.
2.2.2. Type of interventions.
In the experimental group, all patients received arthroscopic reconstruction of ankle lateral ligament. In the control group, all patients received percutaneous reconstruction of ankle lateral ligament.
2.2.3. Type of outcome measurements.
2.2.3.1. Primary outcomes.
American Orthopaedic Foot and Ankle Society midfoot score will be defined as the primary outcomes to assess the function and stability.
2.2.3.2. Secondary outcomes.
Visual analog scale, Tegner score, complications will be defined as secondary outcomes.
2.2.4. Type of studies.
We will include comparative studies which published in Chinese or English, such as randomized controlled trials, retrospective studies and cohort studies. Review, case reports, experimental studies, expert experience, animal studies and conference abstracts will be excluded.
2.3. Search strategy
CNKI, Wanfang, VIP, CBM, PubMed, Embase, and Cochrane Library databases were searched for this study. using the keywords “ankle,” “ankle instability,” “ankle ligament injury,” “arthroscopy,” “percutaneous,” “reconstruction,” and “surgery.” The search strategy in PubMed is shown in Table 1. In addition, the reference lists of previously published systematic reviews of Ligament Reconstruction for ankle instability were manually examined for further pertinent studies.
Table 1.
Pubmed database search strategy.
| Search number | Items |
|---|---|
| 1 | “ ankle instability ”[Mesh] |
| 2 | ankle [Title/Abstract] |
| 3 | ankle instability[Title/Abstract] |
| 4 | ankle ligament injury[Title/Abstract] |
| 5 | 1 OR 2 OR 3 OR 4 |
| 6 | arthroscopic[Title/Abstract] |
| 7 | percutaneous[Title/Abstract] |
| 8 | reconstruction[Title/Abstract] |
| 9 | surgery[Title/Abstract] |
| 10 | 6 OR 7 OR 8 OR 9 |
| 11 | 5 AND 10 |
2.4. Study selection
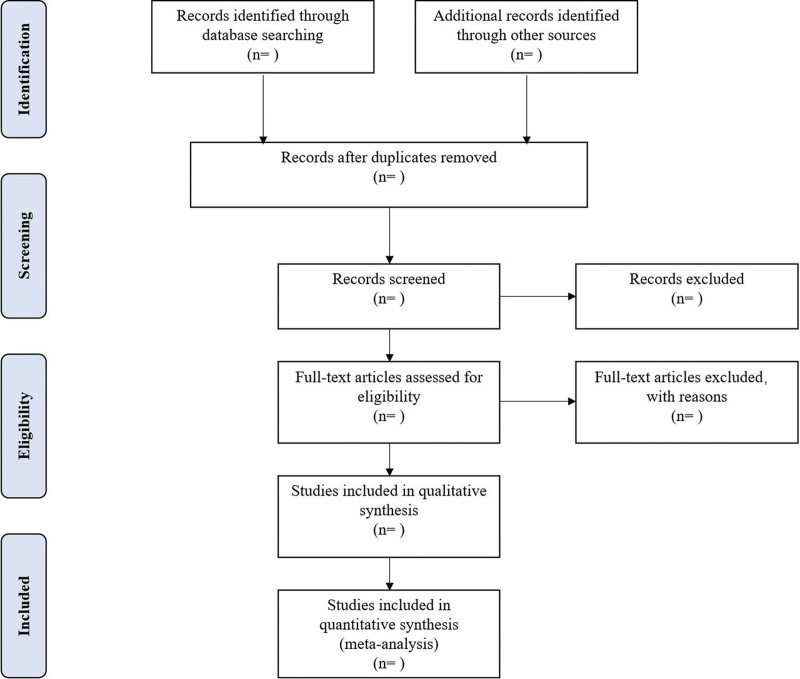
Different researchers (XZ and HH) will separately screen the titles and abstracts of records acquired potential eligibility which comes from the electronic databases. The obtained literature is managed by Notoexpress, irrelevant and duplicate articles are excluded by reading the title and abstract, full texts screening and data extraction will be conducted afterward independently, and finally selected according to the inclusion criteria, any disagreement will be resolved by discussion with the third author (JL) until consensus is reached or by consulting a third author. PRISMA-P flowchart Will be used to show the selection procedure (Fig. 1).
Figure 1.
Flowchart of literature selection.
2.5. Data extraction and management
The following data were extracted: lead author; publication year; country of origin; study design; sample size; age; injury type; reconstruction technique; outcome measures and complications. Any differences of opinion will be resolved through group discussion or consultation with a third reviewer. When relevant data is not reported, we will contact the author via email or other means to obtain missing data. The PRISMA flow diagram will be filled out after the screening study is completed to provide specific information.
2.6. Risk of bias assessment
Two independent (XZ and WG) investigators evaluated the quality of the included studies. The Cochrane Collaboration Risk of Bias Tool was used to evaluate the quality of the randomized controlled trials. The methodological quality of the non-randomized studies was assessed using the Risk-of-Bias Assessment Tool for Non-randomized Studies. The level of evidence was assessed according to the Oxford Centre for Evidence-based Medicine Levels of Evidence.
2.7. Data synthesis
Statistical analysis will be conducted using RevMan 5.4 software (Cochrane Collaboration). The mean difference will be used as the effect analysis statistic for continuous variables, while the risk ratio will be used as the effect analysis statistic for categorical variables. We will also calculate 95% confidence interval for each statistic, and summarize statistical heterogeneity among summary data using the I2 statistic. Cases with I2 ≤ 50% will not be considered to have significant heterogeneity, thus a fixed-effects model will be applied for meta-analysis. In cases where there is statistical heterogeneity among studies, we will further analyze the source of heterogeneity. A random-effects model will be used to pool the data, after excluding the obvious source of clinical heterogeneity, and in cases where obvious clinical heterogeneity exists, the researchers will perform subgroup, sensitivity or only descriptive analyses. Study-specific and pooled estimates will be graphically presented using forest plots, and P < .05 considered statistically significant.
2.8. Subgroup analysis
Subgroup analysis according to the age, injury type and the classifications for chronic ankle lateral instability will be performed to find the source of heterogeneity when significant clinical heterogeneity is observed.
2.9. Sensitivity analysis
Sources of heterogeneity were assessed by sensitivity analysis, by excluding studies of low quality or small sample size, if the heterogeneity did not change significantly, the results were robust. otherwise, the excluded studies may have been source of heterogeneity.
2.10. Publication bias
In this study, fewer than 10 included studies were evaluated for publication bias using funnel plot, otherwise Egger regression test would be used.[23,24]
2.11. Ethics and dissemination
No ethical approval is required because the study will be a review of literature and will not obtain data from a single patient. We will publish our findings through a peer-reviewed journal.
3. Discussion
The purpose of this study was to comparatively evaluate the functional outcomes and complications of arthroscopic reconstruction of ankle lateral ligament and percutaneous reconstruction of ankle lateral ligament in the treatment of CAIL. With the maturation of arthroscopic techniques, more and more experts and scholars are using arthroscopic minimally invasive and precise treatment of ankle instability. To the best of our knowledge, this study integrates the most recent and comprehensive clinical evidence in this field, hoping to provide patients and clinicians with useful and high-grade evidence-based medicine.
Author contributions
Conceptualization: Xing Zhou, Jinlei Li.
Data curation: Huiming Hou.
Formal analysis: Ming Zhou, Hong Yin.
Funding acquisition: Rujie Zhuang, Jinlei Li.
Investigation: Huiming Hou, Xing Zhou, Hong Yin.
Methodology: Huiming Hou, Wenxuan Guo.
Resources: Ming Zhou, Xing Zhou, Wenxuan Guo.
Software: Ming Zhou, Xing Zhou.
Supervision: Ming Zhou, Jinlei Li.
Writing – original draft: Huiming Hou, Xing Zhou.
Writing – review & editing: Rujie Zhuang, Jinlei Li.
Abbreviations:
- ALCLR =
- arthroscopic reconstruction of ankle lateral ligament
- ATFL =
- anterior talofibular ligament
- CALI =
- chronic ankle lateral instability
- CFL =
- calcaneofibular ligament
- PLCLR =
- percutaneous reconstruction of ankle lateral ligament
- PRISMA-P =
- preferred reporting items for systematic review and meta-analysis protocols
HH, MZ, and XZ contributed equally to this work.
The study is supported by Scientific Research Project of Zhejiang Chinese Medicine University (2021FSYYZZ10) and the Science and Technology Planning Project of Yunnan Provincial Science and Technology Department (grant number: 2019FF002(-085)). The funders had and will not have a role in any of the aspects in the study design, data collection and analysis, publication or development of the manuscript.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are publicly available.
How to cite this article: Hou H, Zhou M, Zhou X, Guo W, Zhuang R, Yin H, Li J. Comparison arthroscopic reconstruction and percutaneous reconstruction of ankle lateral ligament for chronic ankle lateral instability: A protocol for a meta-analysis of comparative studies. Medicine 2022;101:45(e31926).
Contributor Information
Huiming Hou, Email: houhuiming860526@163.com.
Ming Zhou, Email: 459378343@qq.com.
Xing Zhou, Email: 459378343@qq.com.
Wenxuan Guo, Email: guowenxuan2019@163.com.
Rujie Zhuang, Email: rujiezhuang@163.com.
Hong Yin, Email: 455833103@qq.com.
References
- [1].Ribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. Br J Sports Med. 2014;48:1014–8. [DOI] [PubMed] [Google Scholar]
- [2].Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11:659–62. [DOI] [PubMed] [Google Scholar]
- [3].Gribble PA. Evaluating and differentiating ankle instability. J Athl Train. 2019;54:617–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Doherty C, Bleakley C, Hertel J, et al. Dynamic balance deficits in individuals with chronic ankle instability compared to ankle sprain copers 1 year after a first-time lateral ankle sprain injury. Knee Surg Sports Traumatol Arthrosc. 2016;24:1086–95. [DOI] [PubMed] [Google Scholar]
- [5].Doherty C, Bleakley C, Hertel J, et al. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am J Sports Med. 2016;44:995–1003. [DOI] [PubMed] [Google Scholar]
- [6].Gribble PA, Bleakley CM, Caulfield BM, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;50:1496–505. [DOI] [PubMed] [Google Scholar]
- [7].Gribble PA, Bleakley CM, Caulfield BM, et al. 2016 consensus statement of the International Ankle Consortium: prevalence, impact and long-term consequences of lateral ankle sprains. Br J Sports Med. 2016;40:1493–5. [DOI] [PubMed] [Google Scholar]
- [8].Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wikstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45:201–9. [DOI] [PubMed] [Google Scholar]
- [9].Broström L. Sprained ankles, VI: surgical treatment of “‘chronic’” ligament ruptures. Acta Chir Scand. 1966;132:551–65. [PubMed] [Google Scholar]
- [10].Vuurberg G, Hoorntje A, Wink LM, et al. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. Br J Sports Med. 2018;52:956956–956.. [DOI] [PubMed] [Google Scholar]
- [11].Bonnel F, Toullec E, Mabit C, Tourné Y; Sofcot. Chronic ankle instability: biomechanics and pathomechanics of ligaments injury and associated lesions. Orthop Traumatol Surg Res. 2010;96:424–32. [DOI] [PubMed] [Google Scholar]
- [12].Russo A, Giacchè P, Marcantoni E, et al. Treatment of chronic lateral ankle instability using the Broström-Gould procedure in athletes: long-term results. Joints. 2016;4:94–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Yasui Y, Shimozono Y, Kennedy JG. Surgical procedures for chronic lateral ankle instability. J Am Acad Orthop Surg. 2018;26:223–30. [DOI] [PubMed] [Google Scholar]
- [14].Feng SM, Sun QQ, Wang AG, Chang B-Q, Cheng J. Arthroscopic anatomical repair of anterior talofibular ligament for chronic lateral instability of the ankle: medium- and long-term functional follow-up. Orthop Surg. 2020;12:505–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Acevedo JI, Mangone PG. Arthroscopic lateral ankle ligament reconstruction. Tech Foot Ankle Surg. 2011;10:111–6. [Google Scholar]
- [16].Glazebrook M, Eid M, Alhadhoud M, Stone J, Matsui K, Takao M. Percutaneous ankle reconstruction of lateral ligaments. Foot Ankle Clin. 2018;23:581–92. [DOI] [PubMed] [Google Scholar]
- [17].Youn H, Kim YS, Lee J, Choi WJ, Lee JW. Percutaneous lateral ligament reconstruction with allograft for chronic lateral ankle instability. Foot Ankle Int. 2012;33:99–104. [DOI] [PubMed] [Google Scholar]
- [18].Guillo S, Cordier G, Sonnery-Cottet B, Bauer T. Anatomical reconstruction of the anterior talofibular and calcaneofibular ligaments with an all-arthroscopic surgical technique. Orthop Traumatol Surg Res. 2014;100:S413–7. [DOI] [PubMed] [Google Scholar]
- [19].Guillo S, Takao M, Calder J, Karlson J, Michels F, Bauer T; Ankle Instability Group. Arthroscopic anatomical reconstruction of the lateral ankle ligaments. Knee Surg Sports Traumatol Arthrosc. 2016;24:998–1002. [DOI] [PubMed] [Google Scholar]
- [20].Michels F, Cordier G, Guillo S, Stockmans F; ESKKA-AFAS Ankle Instability Group. Endoscopic ankle lateral ligament graft anatomic reconstruction. Foot Ankle Clin. 2016;21:665–80. [DOI] [PubMed] [Google Scholar]
- [21].Guillo S, Archbold P, Perera A, et al. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3:593–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Shamseer L, Moher D, Clarke M, et al. PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [23].Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Sutton AJ, Duval SJ, Tweedie RL, Abrams KR, Jones DR. Empirical assessment of effect of publication bias on meta-analyses. BMJ. 2000;320:1574–7. [DOI] [PMC free article] [PubMed] [Google Scholar]