Abstract
Background:
Longstanding biases have fostered the erroneous notion that only those of higher socioeconomic status (SES) experience eating disorders (EDs); however, EDs present across all SES strata. Considering the dearth of ED research among those of lower SES, this study examined 1) the overall association between SES and ED prevalence, and 2) ED prevalence in the context of four relevant social identities (i.e., SES, gender identity, sexual orientation, and race/ethnicity) from an intersectional perspective, as unique combinations of multiple social identities may differentially influence risk.
Methods:
A sample of 120,891 undergraduate/graduate students from the Healthy Minds Study self-reported family SES with a single-item question, gender identity, sexual orientation, and race/ethnicity, and were screened for ED risk.
Results:
Participants of lower SES had 1.27 (95% CI: 1.25–1.30) times greater prevalence of a positive ED screen than those of higher SES. Substantial heterogeneity was observed across the four social identities beyond the association with SES. For example, positive ED screens were particularly common among lower SES, Latinx, sexual minority cisgender men and women, with 52% of bisexual men and 52% of lesbian women of Latinx ethnicity and lower SES screening positive.
Conclusions:
Although positive ED screens were more common among undergraduate/graduate students of lower SES, the particularly high ED risk reported by certain groups of lower SES with multiple minority identities reinforces the importance of investigating multi-layered constructs of identity when identifying groups at disproportionate risk.
Keywords: eating disorders, prevalence, intersectionality, socioeconomic status, gender identity, sexual orientation, race/ethnicity, multiply marginalized, disparities, screening
Eating disorders (EDs) affect over five million individuals in the United States (U.S.) each year, with approximately 21 million in the U.S. estimated to experience an ED in their lifetime (Deloitte Access Economics, 2020). EDs are associated with increased risk for other mental and physical health conditions (Field et al., 2012; Micali et al., 2015) and high economic burden (Deloitte Access Economics, 2020), underscoring the importance of efficient ED identification and intervention. Although some demographic groups may bear this burden more than others (e.g., Marques et al., 2011; Rodgers et al., 2018), identification of specific demographic groups who may be at greatest risk for EDs is needed to allocate resources most effectively.
Individuals of low socioeconomic status (SES) may represent one such group at elevated risk for EDs, given documented associations between food insecurity and homelessness with ED risk (e.g., Becker et al., 2019; Lydecker & Grilo, 2019; Rasmusson et al., 2019; West et al., 2019). Once-monthly allocation of governmental food benefits (e.g., Supplemental Nutrition Assistance Program in the U.S.) is often insufficient to meet monthly nutritional needs (Carlson, 2009), leading to a hypothesized feast-or-famine cycle of eating corresponding to binge-eating at the beginning of the month when SNAP resources are received in response to the significant dietary restraint needed towards the end of the month when the SNAP resources are depleted (e.g., Hazzard, Loth, et al., 2020; Stadterman et al., 2022). Structural barriers for those of low SES include limited financial resources for healthcare expenses (Sareen et al., 2007), which reduces access to mental health services for EDs (Steel et al., 2007). Additionally, perhaps due to historical stereotypes that framed EDs as diseases of affluence (Becker et al., 2003; Gard & Freeman, 1996; Sonneville & Lipson, 2018), individuals of lower SES with ED symptoms are less likely to perceive a need for treatment (Sonneville & Lipson, 2018). Similarly, societal and provider bias may contribute to disparities in diagnosis and care among individuals with EDs of lower SES, given historical ED stereotypes (Becker et al., 2003; Gard & Freeman, 1996). Together, these factors may constitute barriers to the identification of EDs among those of low SES.
Although these barriers, along with longstanding biases in data collection and interpretation, have fostered the erroneous notion that only individuals of higher SES experience EDs, EDs present across all SES strata, with some EDs reported at greater prevalence among those with more restricted financial means (Mulders-Jones et al., 2017). However, recent efforts to collate the existing data regarding the associations between SES and ED risk have reported a lack of consistent patterns (Huryk et al., 2021). Such discrepancies may be partly due to methodological inconsistencies. However, lack of attention to specific high-risk groups when considering the intersections of SES and other identifies may obscure the ways in which SES is associated with ED risk. Therefore, further attention to individuals of lower SES, a historically underrepresented group, is of great importance. Moreover, further research is needed to illuminate the possibility that SES disparities may be best understood by accounting for groups that hold additional socially-marginalized identities.
Intersectionality Theory
Intersectionality theory provides a foundation for understanding ED risk and prevalence in multiply-marginalized groups (Burke et al., 2020). Founded on the work of Black feminist scholars and critical race theorists (e.g., Beale, 1970; Crenshaw, 1993), intersectionality theory recognizes that structural and systemic factors (e.g., policies and practices fostering racism, classism, sexism, and heterosexism) influence individuals’ multiple social identities and their level of risk and resilience in unique and potentially compounded ways (Cole, 2009). Intersectionality theory posits that social identities are intertwined with societal aspects of power, privilege, and oppression, with minoritized identities often associated with greater risk for harmful experiences and negative outcomes. Consistent with this view, socially-constructed hierarchies of power and privilege shaped and embedded in historical and political practices have been shown to influence mental health disparities for persons from socioeconomically disadvantaged backgrounds (e.g., Williams et al., 2016), and for gender (Mayer et al., 2008), sexual (Mayer et al., 2008), and racial/ethnic (e.g., Williams et al., 2016) minorities. In contrast with the more traditional additive model of risk, which assumes that risk associated with each individual identity is cumulative (Rouhani, 2014), an intersectional approach allows for a more nuanced analysis of risk, acknowledging that multiple marginalized identities may confer greater or lower levels of risk than the sum of risks associated with each of identity. In other words, individuals with multiple intersecting marginalized identities (e.g., women of low SES) may experience disproportionate rates of risk for poor health outcomes due to systemic factors that may be obscured when comparing groups according to a single identity in isolation (e.g., women only; low SES only). By examining multiple aspects of identity simultaneously, considering group-specific resilience and strength factors that may counter societal stressors and discrimination related to minority status, and considering risk to be more than simply additive (Bauer, 2014), an intersectional approach allows for the possibility that one held identity may influence the experience of (and risk associated with) another held identity. In this respect, an intersectional approach facilitates deeper understanding of how, within the context of systems that influence one’s lived experience, an individual’s multiple identities may uniquely influence risk or resilience.
Emerging ED research has supported the theory’s predictions, indicating that ED prevalence among groups with multiple marginalized identities may be disproportionate to the prevalence associated with each individual identity in isolation (Burke, Hazzard, et al., 2021; Rodgers et al., 2017). For example, intersectional approaches have indicated that the interactions of gender and Latinx identity produce specific vulnerabilities, with Latina adolescent girls presenting some of the highest risks of ED behaviors compared to their peers (Beccia et al., 2019; Rodgers et al., 2017). Similarly, research examining the intersection of sexual orientation and race/ethnicity indicates a particularly high prevalence of EDs among Latinx and Black sexual minority individuals (Feldman & Meyer, 2007). However, existing intersectional ED research has focused primarily on the interaction between two domains of identity, with few studies (e.g., Austin et al., 2013; Beccia et al., 2021) examining the interacting influences of more than two identities on ED risk. This limitation may obscure important group differences and impede the field’s ability to identify specific subgroups at greatest risk for ED pathology (Austin et al., 2013). Therefore, research examining the intersecting influence of numerous salient identities on ED risk represents an important step for the field.
Current Study
Low SES increases risk for many mental health concerns (Kivimäki et al., 2020), and intersectional approaches emphasize the importance of considering SES along with other salient social identities that are implicated in ED prevalence (Burke et al., 2020). Applications of these approaches will advance our understanding of ED prevalence among multiply-marginalized populations, particularly as they are often overlooked in the context of ED research (Burke et al., 2020). Such work would serve to identify specific populations at greatest risk for ED pathology and could be used to focus assessment and intervention resources appropriately. Therefore, the aim of the current study was twofold: to examine 1) the overall association between SES and ED prevalence, and 2) ED prevalence in the context of four relevant social identities (SES, gender identity, sexual orientation, and race/ethnicity) that independently relate to ED risk (e.g., Kamody et al., 2020; Marques et al., 2011; Mulders-Jones et al., 2017; Murray, 2017) from an intersectional perspective. Given evolving quantitative approaches to examining intersectional risk, we compared additive and intersectional models when exploring aim 2. We hypothesized that individuals of lower SES would report equal or greater ED prevalence compared to their higher SES counterparts. Consistent with intersectionality theory, we hypothesized that those with multiply-marginalized identities may be at particularly heightened risk, but did not put forward a priori hypotheses regarding individual groups.
Method
Study Design
Data came from the Healthy Minds Study (HMS), an annual, web-based survey about mental health in undergraduate/graduate students (Eisenberg & Lipson, 2019). Five years of data from 199 U.S. colleges/universities voluntarily enrolled between 2014–2019 were used. Data from the most recent wave were used for institutions with >1 wave of information (n=25). At larger institutions, a random 4,000-student sample was invited to participate. At smaller institutions, all students were invited. Students aged 18+ were recruited via email and were eligible to win a gift card regardless of participation. All procedures were approved by Institutional Review Boards at participating institutions, and all respondents provided informed consent.
Response rates ranged from 16%−27% across waves. To account for non-response bias, sample probability weights were constructed based on gender, race/ethnicity, academic level, and grade point average. Weights were larger for respondents with underrepresented characteristics, ensuring estimates represented the full undergraduate/graduate student population in terms of these characteristics.
Measures
Gender identity.
In the 2014–2015 survey, participants self-identified as male, female, or transgender in response to the question, “What is your gender?”. In the 2015–2016 and subsequent surveys, participants were asked their (1) assigned sex at birth (male or female) and (2) gender identity (male, female, trans male/trans man, trans female/trans woman, genderqueer/gender non-conforming, or other identity)1. To have at least 10 respondents in each gender identity x sexual orientation x race/ethnicity x SES stratum, the current sample was restricted to cisgender men and women.
Sexual orientation.
Participants self-identified as heterosexual, questioning, bisexual, gay, lesbian, or another sexual orientation to “How would you describe your sexual orientation?”. To have at least 10 respondents in each gender identity x sexual orientation x race/ethnicity x SES stratum, the current sample was restricted to heterosexual, bisexual, gay, or lesbian respondents.
Race/ethnicity.
Respondents self-identified as White, Black/African American, Hispanic/Latino/a, Asian/Asian American, Native Hawaiian/Pacific Islander, American Indian/Alaskan Native, Middle Eastern/Arab/Arab American, and/or as “other” racial/ethnic identity. Respondents could select as many response options as were applicable. In the 2015–2016 survey, race and ethnicity were assessed via separate questions, with Hispanic/Latinx2 assessed via the ethnicity question. Other survey years, race and ethnicity were assessed simultaneously via one race/ethnicity question. If participants selected “other” as a response (n=2,977), they could write in their racial/ethnic identity. Certain “other” responses were recoded back into the original racial/ethnic identity mappings (n=288). More specifically, participants who selected “other” and wrote in a racial/ethnic identity that matched the identity language used within the original question were recoded into the original identity that their response mapped onto (i.e., if an individual wrote in “Latina”, they were recoded into the “Hispanic/Latinx” race/ethnicity identity). To have at least 10 respondents in each gender identity x sexual orientation x race/ethnicity x SES stratum, the current sample was restricted to monoracial respondents (i.e., those identifying with a single race/ethnicity) who identified as White, Black/African American, Hispanic/Latinx, or Asian/Asian American.
Socioeconomic status.
In the 2014–2016 surveys, participants were asked, “Which of the following best describes your socioeconomic background?”. For the current study, responses of “very poor, not enough to get by” or “had enough to get by but not many ‘extras’” were categorized as lower SES, and responses of “comfortable” or “well to do” were categorized as higher SES. In the 2016–2019 surveys, participants were asked, “How would you describe your financial situation while growing up?”. For the current study, responses of “always stressful,” “often stressful,” or “sometimes stressful” were categorized as lower SES, and responses of “rarely stressful” or “never stressful” were categorized as higher SES. These delineations and SES conceptualizations are consistent with recommendations for measuring SES in psychological research (Diemer et al., 2013) and similar to previous work (e.g., Neumark-Sztainer et al., 2020; Price et al., 2002). For sensitivity analyses, another variable using a stricter cut-off for lower SES was also defined, such that only responses of “very poor, not enough to get by” (2014–2016 surveys) or “always stressful” (2016–2019 surveys) were categorized as lower SES. Participants’ SES background versus their current SES was used in analyses given scarcity’s longstanding influence on current behaviors (Mullainathan & Shafir, 2013).
Eating disorder pathology.
ED pathology was assessed with the five-item SCOFF (Morgan et al., 1999), a widely used ED screening tool. Item response options are dichotomous (yes=1, no=0), with total scores ranging from 0 to 5. The cut-off for a positive screen (i.e., likely ED diagnosis) was ≥2 affirmative responses, which yields the optimal trade-off between sensitivity and specificity (Mond et al., 2008). A positive screening was used as a proxy for prevalence (e.g., Burke, Hazzard, et al., 2021). The SCOFF has been validated and utilized across gender (e.g., Mitchell et al., 2021), sexual orientation (e.g., Hazzard, Simone, et al., 2020), race/ethnicity (e.g., Mitchell et al., 2021), and SES (e.g., Thielemann et al., 2019).
Statistical Analysis
The analytic sample included 120,891 undergraduate and graduate students with information on all variables of interest. Analyses were conducted in Stata 16.1 and incorporated sample probability weights to account for non-response. Age-adjusted prevalence estimates of positive SCOFF screens with corresponding 95% confidence intervals (CIs) were predicted via log-binomial regression models in which gender identity, sexual orientation, race/ethnicity, and SES were included as model predictors.
The primary model, which we will refer to as the intersectional model, included a four-way interaction term between each of these social identities, and all lower-order interaction terms. We tested for interaction (corresponding to differences in absolute risk) using the identity link function for the binomial model. Age-adjusted prevalence estimates from the intersectional model were compared across social strata, with non-overlapping 95% CIs indicating statistical significance.
For contrast, we also ran a model without any interaction terms (i.e., only including main effect terms for each social identity), which we will refer to as the additive model. The additive model assumes additive “risk” based on each social identity, whereas the intersectional model allows for “risk” that is less than or greater than the sum of the independent “risks” for each social identity. Non-overlapping 95% CIs between the age-adjusted prevalence estimates from the additive and intersectional models for a specific social stratum indicated a statistically significant departure from additivity, meaning the identified point estimate was significantly greater or lesser than the summed risk associated with the individual identities. The overall association between SES and positive SCOFF screen is also reported from this additive model, as well as from a separate model adjusted only for age.
For sensitivity analyses, all analyses were conducted using the alternative operationalization of SES with a stricter cut-off for lower SES. The results of these sensitivity analyses are reported as supplemental material.
Results
Nearly a quarter of the sample met criteria for elevated ED pathology (see Table 1), consistent with other college student populations screened with the SCOFF (e.g., Hill et al., 2010; Tavolacci et al., 2015). Sample sizes of the intersectional social strata are presented in Figure 1.
Table 1.
Sample characteristics (N = 120,891)
| % (n) | |
|---|---|
| Age | |
| 18–22 years | 67.5 (79,448) |
| 23–25 years | 12.1 (16,306) |
| 26–30 years | 9.1 (13,069) |
| 31+ years | 11.3 (12,068) |
| Gender identity | |
| Cisgender male | 42.6 (38,444) |
| Cisgender female | 57.4 (82,447) |
| Sexual orientation | |
| Heterosexual | 87.4 (106,329) |
| Bisexual | 8.4 (9,954) |
| Gay/lesbian | 4.2 (4,608) |
| Race/ethnicity | |
| White | 73.4 (90,396) |
| Black/African American | 7.9 (6,722) |
| Hispanic/Latinx | 7.3 (7,691) |
| Asian/Asian American | 11.3 (16,082) |
| Socioeconomic status | |
| Lower | 50.0 (55,130) |
| Higher | 50.0 (65,761) |
| Positive SCOFF screen | 22.4 (27,650) |
Note. Frequencies represent observed counts; percentages are weighted to account for non-response.
Figure 1.
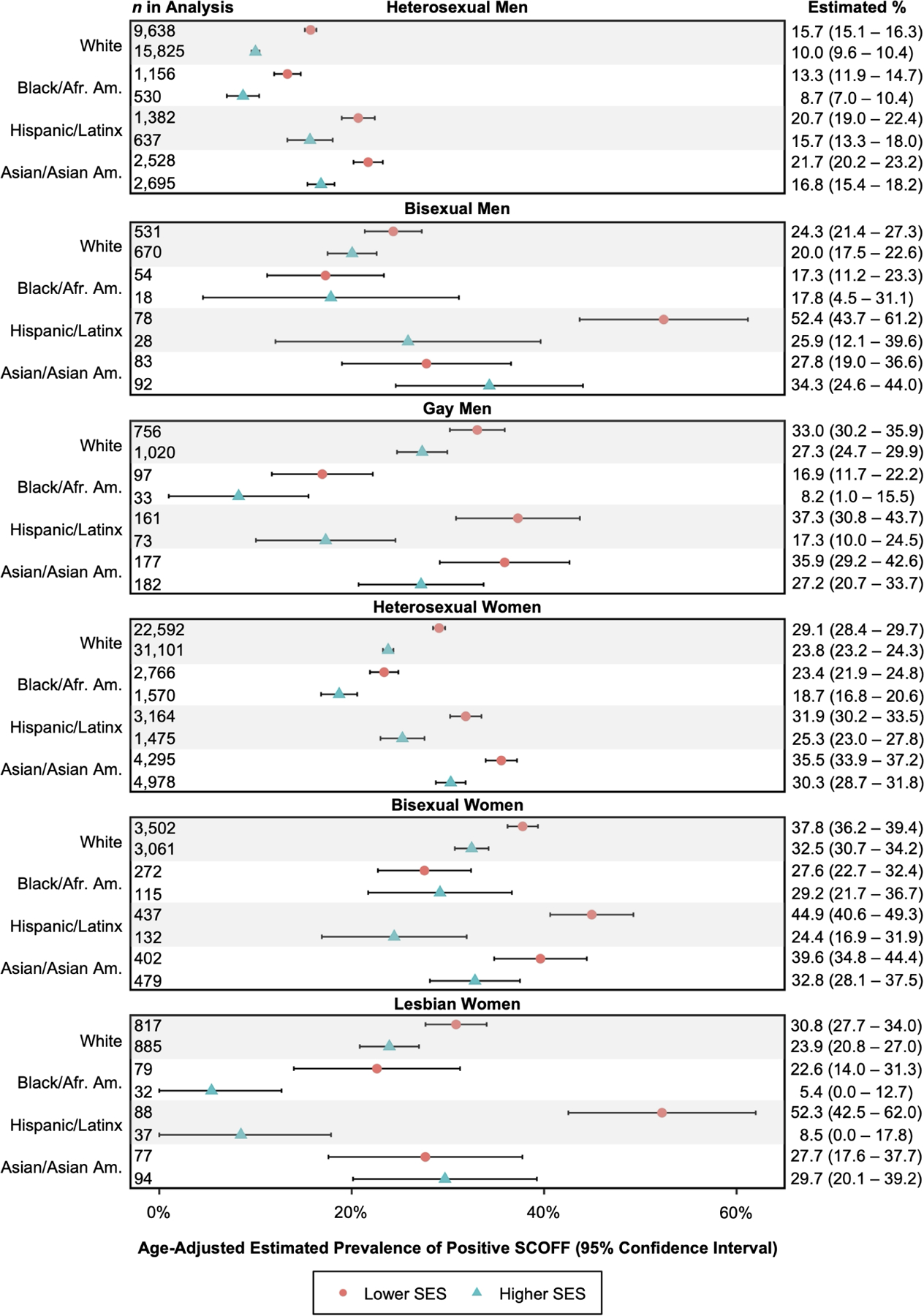
Age-adjusted prevalence estimates of positive SCOFF based on intersectional model
Socioeconomic Status
When adjusting only for age, participants of lower SES had 1.33 (95% CI: 1.31–1.36) times greater ED prevalence than those of higher SES. After additionally adjusting for gender identity, sexual orientation, and race/ethnicity, participants of lower SES had 1.27 (95% CI: 1.25–1.30) times greater ED prevalence than those of higher SES.
Intersectional Model Results
Generally, results (see Figure 1) revealed more heterogeneity in ED prevalence estimates across racial/ethnic and SES strata among bisexual (ranges: 17.8%–52.4% and 24.4%–44.9%, respectively) and gay/lesbian (ranges: 8.2%–37.3% and 5.4%–52.3%) men and women, relative to heterosexual men and women (ranges: 8.7%–21.7% and 18.7%–35.5%, respectively). Similarly, more heterogeneity was present among Hispanic/Latinx individuals (8.5%–52.4%) compared to all other racial/ethnic groups, and among lower SES (13.3%–52.4%) versus higher SES (5.4%–34.3%) individuals.
When examining more specific patterns, ED prevalence estimates across both men and women tended to be particularly high among Hispanic/Latinx sexual minorities of lower SES. For example, the estimated prevalence among bisexual Hispanic/Latino men of lower SES was 52.4%, significantly higher than other subgroups of men except bisexual Asian/Asian American men of higher SES and gay Hispanic/Latino men of lower SES, who had prevalence estimates of 34.3% and 37.3%, respectively. Relatedly, the estimated prevalence among lesbian Hispanic/Latina women of lower SES was 52.3%, significantly higher than all other subgroups of women except bisexual Hispanic/Latina and Asian/Asian American women of lower SES, who had prevalence estimates of 44.9% and 39.6%, respectively. Conversely, prevalence estimates across both men and women were lowest among Black/African American participants of higher SES who identified as gay or lesbian. For example, the estimated prevalence among gay Black/African American men of higher SES was 8.2%, though several other subgroups of men exhibited prevalence estimates that were not significantly different. The estimated prevalence among lesbian Black/African American women of higher SES was 5.4%, significantly lower than all other subgroups of women except lesbian Hispanic/Latina women of higher SES, who had a prevalence estimate of 8.5%.
A significant four-way interaction between gender identity, sexual orientation, race/ethnicity, and SES in the intersectional model was observed (joint test p=.04). The results of all joint tests from the intersectional model are reported in Table 2.
Table 2.
Joint tests from the intersectional model
| Model Term | df | Wald χ2 | p |
|---|---|---|---|
| SES | 1 | 265.14 | < .001 |
| Gender | 1 | 1,505.96 | < .001 |
| Sexual orientation | 2 | 219.37 | < .001 |
| Race/ethnicity | 3 | 108.57 | < .001 |
| Age | 3 | 260.85 | < .001 |
| SES x gender | 1 | 3.17 | .08 |
| SES x sexual orientation | 2 | 1.23 | .54 |
| SES x race/ethnicity | 3 | 1.79 | .62 |
| Gender x sexual orientation | 2 | 65.71 | < .001 |
| Gender x race/ethnicity | 3 | 14.59 | .002 |
| Sexual orientation x race/ethnicity | 6 | 29.51 | < .001 |
| SES x gender x sexual orientation | 2 | 1.37 | .50 |
| SES x gender x race/ethnicity | 3 | 2.02 | .57 |
| SES x sexual orientation x race/ethnicity | 6 | 17.97 | .006 |
| Gender x sexual orientation x race/ethnicity | 6 | 7.05 | .32 |
| SES x gender x sexual orientation x race/ethnicity | 6 | 13.22 | .04 |
Note. df = degrees of freedom; SES = socioeconomic status. The model terms presented here represent a total of 96 unique combinations (e.g., lower SES x female x lesbian x Black/African American) included in the model, tested in a generalized linear model with a binomial distribution and identity link function.
Additive and Intersectional Model Comparisons
The additive model results are presented alongside the intersectional model results in Figure 2, allowing evaluation of departures from additive risk for each specific social stratum. Departure from additive risk is observed when prevalence estimates between the additive and intersectional models differ and confidence intervals do not overlap. Several statistically significant departures from additivity were observed in these data (summarized in Table 3). Among men, all but one statistically significant departure from additivity reflected higher than expected prevalence of ED pathology (bisexual and gay Hispanic/Latino men of lower SES, bisexual Asian/Asian American men of higher SES, and gay White men of both lower and higher SES), while one group (heterosexual White men of higher SES) exhibited slightly lower than expected prevalence. In contrast, all but one statistically significant departure from additivity among women reflected lower than expected prevalence of ED pathology (bisexual Hispanic/Latina women of higher SES, bisexual Asian/Asian American women of lower SES, lesbian White women of both lower and higher SES, lesbian Black/African American women of higher SES, lesbian Hispanic/Latina women of higher SES, and lesbian Asian/Asian American women of lower SES), while one group (heterosexual White women of higher SES) exhibited slightly higher than expected prevalence. We have highlighted some of the findings and encourage readers to review Figures 1 and 2 for additional groups of interest.
Figure 2.
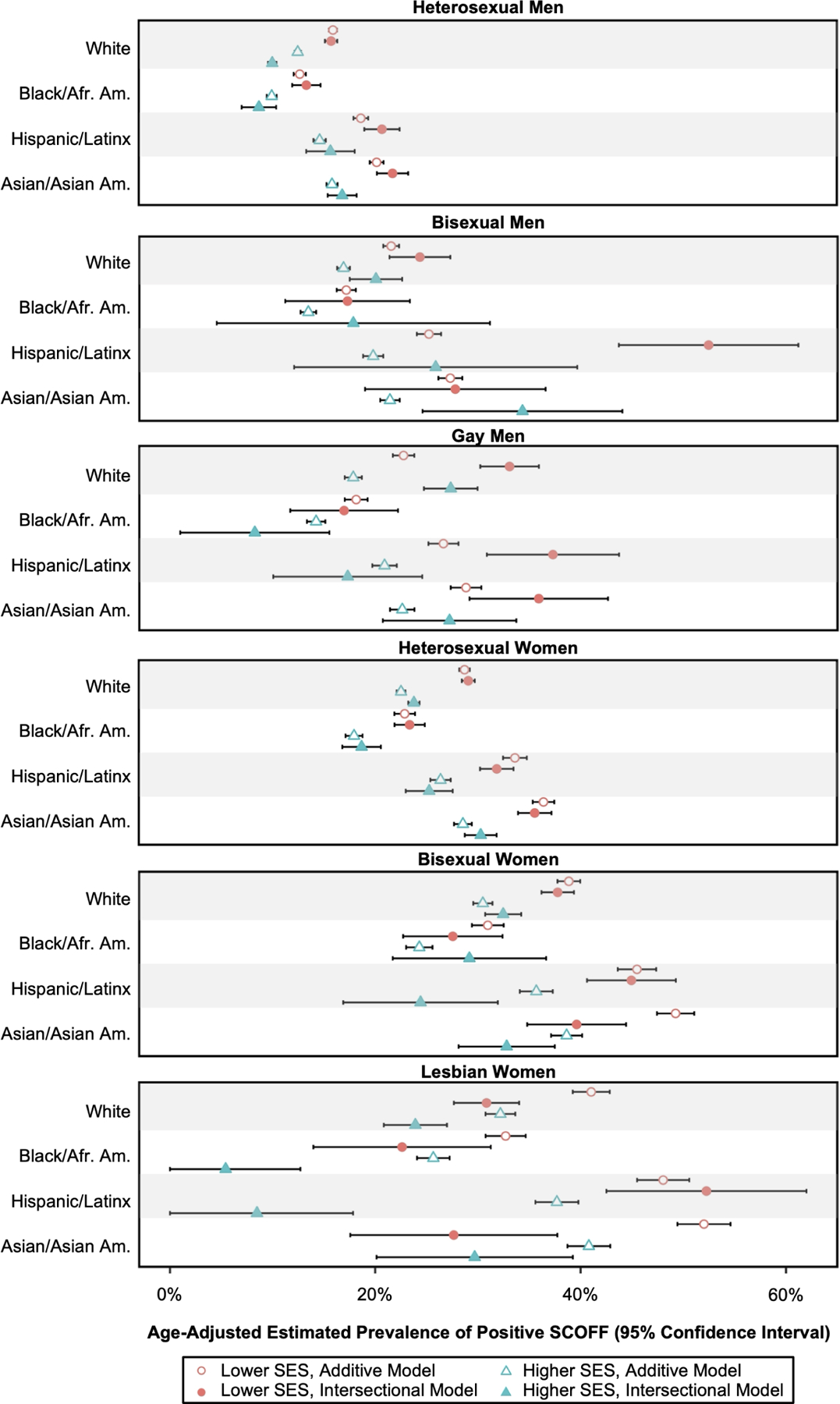
Age-adjusted prevalence estimates of positive SCOFF based on additive and intersectional models
Note. Evidence for a departure from additive risk is observed when prevalence estimates across additive and intersectional models differ and confident intervals do not overlap.
Table 3.
Statistically significant differences in age-adjusted prevalence estimates of positive SCOFF based on intersectional (“observed”) versus additive (“expected”) models
| Difference in Observed Versus Expected Age-Adjusted Prevalence Estimate | |
|---|---|
|
Observed prevalence statistically significantly greater than expected based on each individual social identity
| |
| Hispanic/Latino bisexual men of lower SES | 27.2% greater than expected |
| Asian/Asian American bisexual men of higher SES | 12.9% greater than expected |
| Hispanic/Latino gay men of lower SES | 10.7% greater than expected |
| White gay men of lower SES | 10.3% greater than expected |
| White gay men of higher SES | 9.5% greater than expected |
| White heterosexual women of higher SES | 1.3% greater than expected |
|
Observed prevalence statistically significantly lower than expected based on each individual social identity | |
| Hispanic/Latina lesbian women of higher SES | 29.2% lower than expected |
| Asian/Asian American lesbian women of lower SES | 24.4% lower than expected |
| Black/African American lesbian women of higher SES | 20.2% lower than expected |
| Hispanic/Latina bisexual women of higher SES | 11.3% lower than expected |
| White lesbian women of lower SES | 10.2% lower than expected |
| Asian/Asian American bisexual women of lower SES | 9.6% lower than expected |
| White lesbian women of higher SES | 8.3% lower than expected |
| White heterosexual men of higher SES | 2.5% lower than expected |
Note. SES = socioeconomic status. Within each section of the table, differences in observed versus expected age-adjusted prevalence estimates are listed in descending order by the magnitude of difference.
Discussion
Given how little is known about SES and EDs, particularly in the context of other identities, the present study had two main aims: to examine the 1) overall association between SES and ED prevalence, and 2) intersections of SES, gender identity, sexual orientation, and race/ethnicity on ED prevalence. Overall, findings indicated that ED prevalence was greater among undergraduate/graduate students of lower SES compared to those of higher SES. However, the strength of the relationship between SES and ED varied across gender, sexual orientation, and race/ethnicity groupings. Consistent with intersectionality theory, particularly high ED prevalence was reported by certain groups with multiple minority identities, reinforcing the importance of recognizing identity as a complex and multi-layered construct when aiming to identify groups at disproportionate ED risk. In addition, our findings highlight important discrepancies between the additive and intersectional risk models, providing further support for intersectional theory and newer quantitative approaches for examining group variation in ED prevalence. Taken together, the present findings advance the ED research base and further dispel the myth that EDs are solely experienced by affluent individuals within a homogenous, narrow, and privileged set of demographic characteristics.
Consistent with our hypothesis, and similar to other areas of mental health (Meyer et al., 2014; Reiss, 2013), the current study provides evidence of increased ED risk among individuals of lower SES. Though more research is needed to understand the mechanisms underlying the association between SES and ED risk, several factors may be at play. Structural oppression and income inequality contribute to health disparities (Homan et al., 2021), which is consistent with intersectionality theory’s focus on systems – versus identities – conferring risk. Financial difficulties frequently contribute to interpersonal stress, trauma, and negative affect (Sturgeon et al., 2016), which are in turn all linked to the development and maintenance of ED pathology (e.g., Arcelus et al., 2013; Brewerton, 2007; Fairburn et al., 2003; Sturgeon et al., 2016). Food insecurity, which is more common among those of lower SES (Coleman-Jensen et al., 2019), may increase risk for ED pathology (Hazzard, Loth, et al., 2020). Attempting to control one’s outward appearance may also be perceived as a way to increase one’s social standing, in particular for women (Wang et al., 2020). Given the robust disparity in ED risk for individuals of lower SES, further investigation into the mechanisms of this association will be a critical step on the path toward improved health equity.
Importantly, the relationship between SES and ED prevalence was moderated by other dimensions of identity. Although reviewing results for each individual group is beyond the scope of this discussion, select findings are commented upon in more depth below. Based on the intersectional model, ED prevalence across both men and women tended to be particularly high among Hispanic/Latinx sexual minorities of lower SES, adding to research observing higher prevalence of ED pathology among sexual minorities compared to heterosexuals (Calzo et al., 2017; Feldman & Meyer, 2007; Miller & Luk, 2019), and among Latinx sexual minorities compared to Black and White sexual minorities (Feldman & Meyer, 2007). While U.S. Latinx adults have indicated similar rates of acceptance of non-heterosexuality as the general public, views on sexual orientation vary by immigrant generational status, with those of first-generation status typically less accepting compared to later generations (Taylor et al., 2012). It is possible that systemic factors influencing aspects of identities not assessed here (e.g., generational status, acculturation) may partially explain the current study’s findings; however, additional research is needed to determine this.
Notably, for several groups, ED risk was more—or less—than would be expected based on additive models, highlighting the importance of using intersectional models. For instance, as overall ED prevalence for women is higher than for men (Murray, 2017); the additive model broadly assumes greater risk for women and lesser risk for men, potentially overestimating and underestimating risk, respectively, in certain populations. Further, several important findings—particularly for sexual minority groups—were obscured in the additive model. For example, among Hispanic/Latina lesbian women of high SES, the additive model overestimated ED risk by roughly 30%, which concealed a nearly 44% difference in risk between high and low SES groups. In addition, comparison of intersectional and additive analyses indicated that ED prevalence was higher than expected were risk to be additive among Hispanic/Latino gay and bisexual men of lower SES, and similarly lower than expected were risk to be additive among Hispanic/Latina lesbian and bisexual women of higher SES. These results underscore the capacity of intersectional models to identify heightened levels of risk and resiliency in specific groups. However, again here, additional research is needed to uncover the specific mechanisms underlying these findings. Variables of interest may include religiosity and religious affiliation (Horowitz, 2013; Taylor et al., 2012), outness (i.e., the degree to which sexual orientation is disclosed to others; Feldman & Wright, 2013; Kosciw et al., 2015), and variations of acceptance of sexual minority identity by one’s community or culture of origin (Giano et al., 2020; Kosciw et al., 2015; Poushter & Kent, 2020).
Intersectionality theory acknowledges that risk operates within social, political, and economic systems that benefit some, as much as they disadvantage others (Cole, 2009). While many groups identifying with the four historically marginalized identities examined within this study evidenced heightened risk, several multiply-marginalized groups exhibited relatively low levels of ED risk. For instance, Black lesbian women of higher SES (who experience “triple jeopardy” due to the combination of their race/ethnicity, sexual orientation, and gender identity; Bowleg, 2008), evidenced the lowest ED prevalence of all groups, which warrants questioning what might be particularly protective for this group. Overall, Black women tend to report less ED pathology compared to their White, Hispanic/Latina, and Asian/Asian American peers (e.g., Burke, Schaefer, et al., 2021; Rakhkovskaya & Warren, 2016), which may be attributable to deriving supportive appearance-based messages from culturally-specific sources (e.g., ethnic media outlets, church, family, and friends) that are protective (Rogers Wood & Petrie, 2010). In addition, it is possible that this group’s higher financial resources allow for participation in community and social groups that may especially facilitate resilience (Meyer, 2003). However, the lower prevalence rate may also be due to measurement issues as the SCOFF may not fully capture eating- and body-related experiences for this group. Although the current research represents an important step in understanding how complex social identities relate to ED prevalence, additional quantitative and qualitative work is needed to better understand these relationships.
From a clinical perspective, the present findings underscore the need for clinicians to approach individuals holistically, considering the interplay between unique risk/resilience factors associated with each aspect of patient identity and social positionality. For example, person-centered assessment techniques embrace multiple aspects of identity and should be considered for evaluation and treatment planning (e.g., the Cultural Formulation Interview; Lewis-Fernandez et al., 2014; Lewis-Fernandez et al., 2020). In addition, community healthcare institutions, which typically serve diverse populations and patients of lower SES often include regular screenings for early detection of anxiety and depression (Mulvaney-Day et al., 2018). Such institutions should also consider adding brief ED screens to better serve these at-risk populations.
From the research perspective, results from the intersectional model support the basic tenets of the intersectionality theory that an individual’s level of ED risk/resilience is dynamically influenced by the unique interactions of their multiple social identities (Burke et al., 2020) that are fostered within systems of power, priviledge, and oppression. The present study also provided evidence that additive models of risk may overestimate/underestimate ED risk, by failing to account for multiple identities with varying degrees of power and privilege that can influence risk. Comparatively, intersectional models may more accurately capture the real-world phenomenon of lived human experience. Finally, the present work highlights particular groups at disproportionate risk for ED pathology for whom researchers and granting agencies should orient resources, conduct further quantitative and qualitative work, adapt treatments, and screen more regularly for EDs. Identification of factors related to resilience and strength in the face of multiple stressors is especially encouraged, as identified factors/experiences could be utilized to fortify existing interventions and improve their efficacy.
The current study had several strengths including clarification of ED risk among multiply-marginalized groups who are often ignored in ED research using a large sample size that facilitated simultaneous examination of four important social identities, consistent with the identities originally conceptualized in intersectionality discourse (e.g., Combahee River Collective, 1977/1995). In addition, the comparison of two different statistical approaches provided important information regarding the relative “fit” of these techniques with intersectionality tenets. Limitations included the exclusion of transgender and multiracial individuals, both of whom may be at heightened risk for ED pathology (e.g., Burke, Hazzard, et al., 2021; Nagata et al., 2020), due to small sample sizes. In addition, although the SCOFF is widely used to assess ED pathology and has accumulated evidence to support the validity of scale scores in numerous samples (see Method section), the scale may not adequately capture culturally-relevant forms of ED symptoms for all groups, which is a broader issue in ED measurement (e.g., Kelly et al., 2012; Murray et al., 2017; Wilfred & Lundgren, 2021). Therefore, continued development of and research using alternative measures is encouraged. Additionally, though weighting accounts for the lower response rates of those with lower SES, nonresponse bias by SES could potentially have influenced our results. Data were obtained from both public and private schools distributed broadly across the US; nevertheless, college student samples limit generalizability, particularly as lower SES individuals may be underrepresented in a college sample (ACSFA, 2001). Consequently, those with the greatest financial hardships may not be adequately captured in this sample. SES was conceptualized in the current study as financial resources, in direct comparison to antiquated notions of EDs as “diseases of affluence” (Bruch, 1975) and in consideration of the income-related stereotypes that influence ED identification and treatment in low SES populations (Huryk et al., 2021). Nevertheless, SES is a complex, multidimensional construct (Diemer et al., 2013), and it is possible that other SES-related factors (e.g., education, occupation) may be differentially related to ED risk. Related to the use of sample probability weights to account for non-response, the present study used a traditional interaction term-based approach to examine intersectionality rather than multilevel analysis of individual heterogeneity and discriminatory accuracy (MAIHDA; Evans et al., 2018), a novel statistical method for examining intersectionality, because conventional statistical software do not yet have the capability to incorporate sample probability weights into Bayesian multilevel models such as those used in MAIHDA. Finally, further research is needed to replicate the current results as some of the subgroups were quite small, assess other relevant aspects of identity and associated factors (e.g., weight status, acculturative stress, outness, etc.), and clarify the mechanisms – including systemic factors – through which these associations persist.
In sum, the current findings support previous research dispelling the notion that EDs effect only affluent individuals and highlight previously overlooked groups in need of assessment and intervention. Improving our capacity to identify high risk groups is an important endeavor for better resource allocation, as well as targeted prevention, and these findings contribute to our understanding of the nuances of ED risk among individuals based on their intersecting identities. In addition to replication of these findings, further research is needed to better understand the mechanisms underlying variations in ED prevalence, and to continue to illuminate and eventually dismantle the factors that place individuals with multiply-marginalized identities at greater risk for ED and other mental health concerns.
Supplementary Material
Acknowledgements
The authors would like to thank Yvette G. Karvay, M.A., for her work coding the race/ethnicity variables utilized in the current study.
Funding Statement:
This research was supported in part by the Fordham University Faculty Fellowship (NLB), the National Institute of Mental Health grant number T32MH082761 (VMH), the National Institute of General Medical Science grant number 1P20GM134969–01A1 (LMS), and the National Institute of Minority Health and Health Disparities K99MD015770 (MS).
Footnotes
Conflicts of Interest: None
Throughout, we utilize the nouns “men” and “women” when referring to gender identity.
We acknowledge the lack of consensus around the current nomenclature; however, throughout, we utilize “Latinx” as the plural, inclusive term for those of Latino/a identity.
References
- Advisory Committee on Student Financial Assistance. (ACSFA, 2001). Access denied: Restoring the nation’s commitment to equal educational opportunity Washington, D. C. https://files.eric.ed.gov/fulltext/ED453770.pdf [Google Scholar]
- Arcelus J, Haslam M, Farrow C, & Meyer C (2013). The role of interpersonal functioning in the maintenance of eating psychopathology: A systematic review and testable model. Clin Psychol Rev, 33(1), 156–167. 10.1016/j.cpr.2012.10.009 [DOI] [PubMed] [Google Scholar]
- Austin SB, Nelson LA, Birkett MA, Calzo JP, & Everett B (2013). Eating disorder symptoms and obesity at the intersections of gender, ethnicity, and sexual orientation in US high school students. American Journal of Public Health, 103(2), e16–22. 10.2105/ajph.2012.301150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer GR (2014). Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Social Science & Medicine, 110, 10–17. 10.1016/j.socscimed.2014.03.022 [DOI] [PubMed] [Google Scholar]
- Beale F (1970). Double Jeopardy: To be Black and Female. In Cade T (Ed.), The Black woman: An anthology (pp. 90–100). Signet. [Google Scholar]
- Beccia AL, Baek J, Austin SB, Jesdale WM, & Lapane KL (2021). Eating-related pathology at the intersection of gender identity and expression, sexual orientation, and weight status: An intersectional Multilevel Analysis of Individual Heterogeneity and Discriminatory Accuracy (MAIHDA) of the Growing Up Today Study cohorts. Social Science & Medicine, 281, 114092. 10.1016/j.socscimed.2021.114092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beccia AL, Baek J, Jesdale WM, Austin SB, Forrester S, Curtin C, & Lapane KL (2019). Risk of disordered eating at the intersection of gender and racial/ethnic identity among U.S. high school students. Eating Behaviors, 34, 101299. 10.1016/j.eatbeh.2019.05.002 [DOI] [PubMed] [Google Scholar]
- Becker AE, Franko DL, Speck A, & Herzog DB (2003). Ethnicity and differential access to care for eating disorder symptoms. International Journal of Eating Disorders, 33(2), 205–212. 10.1002/eat.10129 [DOI] [PubMed] [Google Scholar]
- Becker CB, Middlemass KM, Gomez F, & Martinez-Abrego A (2019). Eating disorder pathology among individuals living with food insecurity: A replication study. Clinical Psychological Science, 7(5), 1144–1158. 10.1177/2167702619851811 [DOI] [Google Scholar]
- Bowleg L (2008). When Black + Lesbian + Woman ≠ Black Lesbian Woman: The methodological challenges of qualitative and quantitative intersectionality research. Sex Roles, 59(5–6), 312–325. 10.1007/s11199-008-9400-z [DOI] [Google Scholar]
- Brewerton TD (2007). Eating disorders, trauma, and comorbidity: Focus on PTSD. Eating Disorders, 15(4), 285–304. 10.1080/10640260701454311 [DOI] [PubMed] [Google Scholar]
- Bruch H (1975). Obesity and anorexia nervosa: Psychosocial aspects. Australian and New Zealand Journal of Psychiatry, 9(3), 159–161. 10.3109/00048677509159842 [DOI] [PubMed] [Google Scholar]
- Burke NL, Hazzard VM, Karvay YG, Schaefer LM, Lipson SK, & Rodgers RF (2021). Eating disorder prevalence among multiracial US undergraduate and graduate students: Is multiracial risk different than the sum of each identity? Eating Behaviors, 41, 101501. Advance online publication. 10.1016/j.eatbeh.2021.101501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke NL, Schaefer LM, Hazzard VM, & Rodgers RF (2020). Where identities converge: The importance of intersectionality in eating disorders research. International Journal of Eating Disorders, 53(10), 1605–1609. 10.1002/eat.23371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke NL, Schaefer LM, Karvay YG, Bardone-Cone AM, Frederick DA, Schaumberg K, Klump KL, Anderson DA, & Thompson JK (2021). Does the tripartite influence model of body image and eating pathology function similarly across racial/ethnic groups of White, Black, Latina, and Asian Women? Eating Behaviors, 42, 101519. Advance online publication. 10.1016/j.eatbeh.2021.101519 [DOI] [PubMed] [Google Scholar]
- Calzo JP, Blashill AJ, Brown TA, & Argenal RL (2017). Eating disorders and disordered weight and shape control behaviors in sexual minority populations. Current Psychiatry Reports, 19(8), 49. 10.1007/s11920-017-0801-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson S (2019). More Adequate SNAP Benefits Would Help Millions of Participants Better Afford Food. Center on Budget and Policiy Priorities https://www.cbpp.org/research/food-assistance/more-adequate-snap-benefits-would-help-millions-of-participants-better#:~:text=The%20research%20summarized%20here%20indicates,a%20nutritious%20diet%3B%20and%20the
- Cole ER (2009). Intersectionality and research in psychology. American Psychologist, 64(3), 170–180. 10.1037/a0014564 [DOI] [PubMed] [Google Scholar]
- Coleman-Jensen A, Rabbitt MP, Gregory CA, & Singh A (2019). Household Food Security in the United States in 2018, ERR-270. U.S. Department of Agriculture, Economic Research Service
- Combahee River Collective. (1995). Combahee River Collective statement. In Guy-Sheftall B (Ed.), Words of fire: An anthology of African American feminist thought (pp. 232–240). New York: New Press. (Original work published 1977) [Google Scholar]
- Crenshaw K (1993). Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. In Weisbert DK (Ed.), Feminist Legal Theory: Foundations (pp. 383–395). Temple University Press. (Original work published 1989) [Google Scholar]
- Deloitte Access Economics. (2020). The Social and Economic Cost of Eating Disorders in the United States of America: A Report for the Strategic Training Initiative for the Prevention of Eating Disorders and the Academy for Eating Disorders https://www.hsph.harvard.edu/striped/report-economic-costs-of-eating-disorders/
- Diemer MA, Mistry RS, Wadsworth ME, López I, & Reimers F (2013). Best practices in conceptualizing and measuring social class in psychological research. Analyses of Social Issues and Public Policy, 13(1), 77–113. 10.1111/asap.12001 [DOI] [Google Scholar]
- Eisenberg D, & Lipson SK (2019). The Healthy Minds Study [DOI] [PubMed]
- Evans CR, Williams DR, Onnela JP, & Subramanian SV (2018). A multilevel approach to modeling health inequalities at the intersection of multiple social identities. Social Science and Medicine, 203, 64–73. 10.1016/j.socscimed.2017.11.011 [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R (2003). Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41(5), 509–528. 10.1016/s0005-7967(02)00088-8 [DOI] [PubMed] [Google Scholar]
- Feldman MB, & Meyer IH (2007). Eating disorders in diverse lesbian, gay, and bisexual populations. International Journal of Eating Disorders, 40(3), 218–226. 10.1002/eat.20360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman SE, & Wright AJ (2013). Dual impact: Outness and LGB identity formation on mental health. Journal of Gay & Lesbian Social Services, 25(4), 443–464. 10.1080/10538720.2013.833066 [DOI] [Google Scholar]
- Field AE, Sonneville KR, Micali N, Crosby RD, Swanson SA, Laird NM, Treasure J, Solmi F, & Horton NJ (2012). Prospective association of common eating disorders and adverse outcomes. Pediatrics, 130(2), e289–e295. 10.1542/peds.2011-3663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gard MC, & Freeman CP (1996). The dismantling of a myth: a review of eating disorders and socioeconomic status. International Journal of Eating Disorders, 20(1), 1–12. [DOI] [PubMed] [Google Scholar]
- Giano Z, Currin JM, Wheeler DL, & Hubach RD (2020). Outness amplifies the negative effect of gay related rejection in rural, but not urban sexual minority men. Psychology & Sexuality, 1–15. 10.1080/19419899.2020.1765411 [DOI]
- Hazzard VM, Loth KA, Hooper L, & Becker CB (2020). Food insecurity and eating disorders: A review of emerging evidence. Current Psychiatry Reports, 22(12), 74. 10.1007/s11920-020-01200-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazzard VM, Simone M, Borg SL, Borton KA, Sonneville KR, Calzo JP, & Lipson SK (2020). Disparities in eating disorder risk and diagnosis among sexual minority college students: Findings from the national Healthy Minds Study. International Journal of Eating Disorders, 53(9), 1563–1568. 10.1002/eat.23304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill LS, Reid F, Morgan JF, & Lacey JH (2010). SCOFF, the development of an eating disorder screening questionnaire. International Journal of Eating Disorders, 43(4), 344–351. 10.1002/eat.20679 [DOI] [PubMed] [Google Scholar]
- Homan P, Brown TH, & King B (2021). Structural intersectionality as a new direction for health disparities research. Journal of Health and Social Behavior, 62(3), 350–370. 10.1177/00221465211032947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JM (2013). Americans less accepting of homosexuality than other westerners – religion may be one reason. Pew Research Center https://www.pewresearch.org/fact-tank/2013/06/12/americans-are-less-accepting-of-homosexuality-than-canadians-western-europeans-and-religion-may-be-one-explanation/
- Huryk KM, Drury CR, & Loeb KL (2021). Diseases of affluence? A systematic review of the literature on socioeconomic diversity in eating disorders. Eating Behaviors, 43, 101548. 10.1016/j.eatbeh.2021.101548 [DOI] [PubMed] [Google Scholar]
- Kamody RC, Grilo CM, & Udo T (2020). Disparities in DSM-5 defined eating disorders by sexual orientation among U.S. adults. International Journal of Eating Disorders, 53(2), 278–287. 10.1002/eat.23193 [DOI] [PubMed] [Google Scholar]
- Kelly NR, Mitchell KS, Gow RW, Trace SE, Lydecker JA, Bair CE, & Mazzeo S (2012). An evaluation of the reliability and construct validity of eating disorder measures in white and black women. Psychological Assessment, 24(3), 608–617. 10.1037/a0026457 [DOI] [PubMed] [Google Scholar]
- Kivimäki M, Batty GD, Pentti J, Shipley MJ, Sipilä PN, Nyberg ST, Suominen SB, Oksanen T, Stenholm S, Virtanen M, Marmot MG, Singh-Manoux A, Brunner EJ, Lindbohm JV, Ferrie JE, & Vahtera J (2020). Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. The Lancet Public Health, 5(3), e140–e149. 10.1016/s2468-2667(19)30248-8 [DOI] [PubMed] [Google Scholar]
- Kosciw JG, Palmer NA, & Kull RM (2015). Reflecting resiliency: openness about sexual orientation and/or gender identity and its relationship to well-being and educational outcomes for LGBT students. American Journal of Community Psychology, 55(1–2), 167–178. 10.1007/s10464-014-9642-6 [DOI] [PubMed] [Google Scholar]
- Lewis-Fernandez R, Aggarwal NK, Baarnhielm S, Rohlof H, Kirmayer LJ, Weiss MG, Jadhav S, Hinton L, Alarcon RD, Bhugra D, Groen S, van Dijk R, Qureshi A, Collazos F, Rousseau C, Caballero L, Ramos M, & Lu F (2014). Culture and psychiatric evaluation: operationalizing cultural formulation for DSM-5. Psychiatry, 77(2), 130–154. 10.1521/psyc.2014.77.2.130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis-Fernandez R, Aggarwal NK, & Kirmayer LJ (2020). The Cultural Formulation Interview: Progress to date and future directions. Transcultural Psychiatry, 57(4), 487–496. 10.1177/1363461520938273 [DOI] [PubMed] [Google Scholar]
- Lydecker JA, & Grilo CM (2019). Food insecurity and bulimia nervosa in the United States. International Journal of Eating Disorders, 52(6), 735–739. 10.1002/eat.23074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, & Diniz JB (2011). Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. International Journal of Eating Disorders, 44(5), 412–420. 10.1002/eat.20787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer KH, Bradford JB, Makadon HJ, Stall R, Goldhammer H, & Landers S (2008). Sexual and gender minority health: What we know and what needs to be done. American Journal of Public Health, 98(6), 989–995. 10.2105/ajph.2007.127811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer OL, Castro-Schilo L, & Aguilar-Gaxiola S (2014). Determinants of mental health and self-rated health: A model of socioeconomic status, neighborhood safety, and physical activity. American Journal of Public Health, 104(9), 1734–1741. 10.2105/AJPH.2014.302003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micali N, Solmi F, Horton NJ, Crosby RD, Eddy KT, Calzo JP, Sonneville KR, Swanson SA, & Field AE (2015). Adolescent eating disorders predict psychiatric, high-risk behaviors and weight outcomes in young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 54(8), 652–659.e651. 10.1016/j.jaac.2015.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JM, & Luk JW (2019). A systematic review of sexual orientation disparities in disordered eating and weight-related behaviors among adolescents and young adults: Toward a developmental model. Adolescent Research Review, 4(2), 187–208. 10.1007/s40894-018-0079-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell KS, Masheb R, Smith BN, Kehle-Forbes S, Hardin S, & Vogt D (2021). Eating disorder measures in a sample of military veterans: A focus on gender, age, and race/ethnicity. Psychological Assessessment 10.1037/pas0001050 [DOI] [PMC free article] [PubMed]
- Mond JM, Myers TC, Crosby RD, Hay PJ, Rodgers B, Morgan JF, Hubert Lacey J, & Mitchell JE (2008). Screening for eating disorders in primary care: EDE-Q versus SCOFF. Behaviour Research and Therapy, 46(5), 612–622. 10.1016/j.brat.2008.02.003 [DOI] [PubMed] [Google Scholar]
- Morgan JF, Reid F, & Lacey JH (1999). The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ (Clinical research ed.), 319(7223), 1467–1468. 10.1136/bmj.319.7223.1467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulders-Jones B, Mitchison D, Girosi F, & Hay P (2017). Socioeconomic correlates of eating disorder symptoms in an Australian population-based sample. PLoS ONE, 12(1), e0170603. 10.1371/journal.pone.0170603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullainathan S, & Shafir E (2013). Scarcity: The new science of having less and how it defines our lives Times Books, Henry Holt. [Google Scholar]
- Mulvaney-Day N, Marshall T, Downey Piscopo K, Korsen N, Lynch S, Karnell LH, Moran GE, Daniels AS, & Ghose SS (2018). Screening for behavioral health conditions in primary care settings: A systematic review of the literature. Journal of General Internal Medicine, 33(3), 335–346. 10.1007/s11606-017-4181-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray SB (2017). Gender identity and eating disorders: The need to delineate novel pathways for eating disorder symptomatology. Journal of Adolescent Health, 60(1), 1–2. 10.1016/j.jadohealth.2016.10.004 [DOI] [PubMed] [Google Scholar]
- Murray SB, Nagata JM, Griffiths S, Calzo JP, Brown TA, Mitchison D, Blashill AJ, & Mond JM (2017). The enigma of male eating disorders: A critical review and synthesis. Clinical Psychology Review, 57, 1–11. 10.1016/j.cpr.2017.08.001 [DOI] [PubMed] [Google Scholar]
- Nagata JM, Ganson KT, & Austin SB (2020). Emerging trends in eating disorders among sexual and gender minorities. Current Opinion in Psychiatry, 33(6), 562–567. 10.1097/yco.0000000000000645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall MM, Choi J, Barr-Anderson DJ, Telke S, & Mason SM (2020). Exposure to adverse events and associations with stress levels and the practice of yoga: Survey findings from a population-based study of diverse emerging young adults. The Journal of Alternative and Complementary Medicine, 26(6), 482–490. 10.1089/acm.2020.0077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poushter J, & Kent N (2020). The global divide on homosexuality persists. Pew Research Center https://www.pewresearch.org/global/wp-content/uploads/sites/2/2020/06/PG_2020.06.25_Global-Views-Homosexuality_FINAL.pdf
- Price RH, Choi JN, & Vinokur AD (2002). Links in the chain of adversity following job loss: how financial strain and loss of personal control lead to depression, impaired functioning, and poor health. Journal of Occupational Health Psychology, 7(4), 302–312. 10.1037/1076-8998.7.4.302 [DOI] [PubMed] [Google Scholar]
- Rakhkovskaya LM, & Warren CS (2016). Sociocultural and identity predictors of body dissatisfaction in ethnically diverse college women. Body Image, 16, 32–40. 10.1016/j.bodyim.2015.10.004 [DOI] [PubMed] [Google Scholar]
- Rasmusson G, Lydecker JA, Coffino JA, White MA, & Grilo CM (2019). Household food insecurity is associated with binge‐eating disorder and obesity. International Journal of Eating Disorders, 52(1), 28–35. 10.1002/eat.22990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss F (2013). Socioeconomic inequalities and mental health problems in children and adolescents: A systematic review. Social Science & Medicine, 90, 24–31. 10.1016/j.socscimed.2013.04.026 [DOI] [PubMed] [Google Scholar]
- Rodgers RF, Berry R, & Franko DL (2018). Eating disorders in ethnic minorities: An update. Current Psychiatry Reports, 20(10), 90. 10.1007/s11920-018-0938-3 [DOI] [PubMed] [Google Scholar]
- Rodgers RF, Watts AW, Austin SB, Haines J, & Neumark‐Sztainer D (2017). Disordered eating in ethnic minority adolescents with overweight. International Journal of Eating Disorders, 50(6), 665–671. 10.1002/eat.22652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers Wood NA, & Petrie TA (2010). Body dissatisfaction, ethnic identity, and disordered eating among African American women. Journal of Counseling Psychology, 57(2), 141–153. 10.1037/a0018922 [DOI] [PubMed] [Google Scholar]
- Rouhani S (2014). Intersectionality-informed quantitative research: A primer Institute for Intersectionality Research and Policy, Simon Fraser University.
- Sareen J, Jagdeo A, Cox BJ, Clara I, ten Have M, Belik S-L, de Graaf R, & Stein MB (2007). Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatric Services, 58, 357–364. 10.1176/ps.2007.58.3.357 [DOI] [PubMed] [Google Scholar]
- Sonneville K, & Lipson S (2018). Disparities in eating disorder diagnosis and treatment according to weight status, race/ethnicity, socioeconomic background, and sex among college students. International Journal of Eating Disorders, 51(6), 518–526. 10.1002/eat.22846 [DOI] [PubMed] [Google Scholar]
- Stadterman J, Karvay YG, Feuerstahler L, & Burke NL (2022). Comparison of ad libitum snack consumption and acquisition between adolescents living with food security and food insecurity: A stage 1 registered report. International Journal of Eating Disorders. Advance online publication 10.1002/eat.23693 [DOI] [PubMed]
- Steel L, Dewa C, & Lee K (2007). Socioeconomic status and self-reported barriers to mental health service use. The Canadian Journal of Psychiatry, 52(3), 201–206. 10.1177/070674370705200312 [DOI] [PubMed] [Google Scholar]
- Sturgeon JA, Arewasikporn A, Okun MA, Davis MC, Ong AD, & Zautra AJ (2016). The psychosocial context of financial stress: Implications for inflammation and psychological health. Psychosomatic Medicine, 78(2), 134–143. 10.1097/PSY.0000000000000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavolacci MP, Grigioni S, Richard L, Meyrignac G, Déchelotte P, & Ladner J (2015). Eating Disorders and Associated Health Risks Among University Students. Journal of Nutrition Education and Behavior, 47(5), 412–420.e411. 10.1016/j.jneb.2015.06.009 [DOI] [PubMed] [Google Scholar]
- Taylor P, Lopez MH, Martinez J, & Velasco G (2012). When Labels Don’t Fit: Hispanics and Their Views of Identity - Politics, Values and Religion. Pew Research Center https://www.pewresearch.org/hispanic/2012/04/04/v-politics-values-and-religion/
- Thielemann D, Richter F, Strauss B, Braehler E, Altmann U, & Berger U (2019). Differential item functioning in brief instruments of disordered eating. European Journal of Psychological Assessment, 35(6), 823–833. 10.1027/1015-5759/a000472 [DOI] [Google Scholar]
- Wang X, Teng F, Chen Z, & Poon K-T (2020). Control my appearance, control my social standing: Appearance control beliefs influence American women’s (not men’s) social mobility perception. Personality and Individual Differences, 155. 10.1016/j.paid.2019.109629 [DOI] [Google Scholar]
- West CE, Goldschmidt AB, Mason SM, & Neumark‐Sztainer D (2019). Differences in risk factors for binge eating by socioeconomic status in a community‐based sample of adolescents: Findings from Project EAT. International Journal of Eating Disorders 10.1002/eat.23079 [DOI] [PMC free article] [PubMed]
- Wilfred SA, & Lundgren JD (2021). The Double Consciousness Body Image Scale: A body image assessment centering the experiences of Black women. International Journal of Eating Disorders 10.1002/eat.23581 [DOI] [PubMed]
- Williams DR, Priest N, & Anderson N (2016). Understanding associations between race, socioeconomic status and health: Patterns and prospects. Health Psychology, 35(4), 407–411. 10.1037/hea0000242 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


