Abstract
Objective:
In March 2020, regulatory and payment changes allowed “brick and mortar” pediatric practices to offer practice-based telemedicine for the first time, joining direct-to-consumer (DTC) telemedicine vendors in the ability to offer visits for common acute pediatric concerns via telemedicine. We sought to characterize the relative contribution of practice-based telemedicine vs. DTC telemedicine models in provision of children’s telemedicine from 2018 through 2021.
Methods:
Using January 2018-September 2021 data from Opium’s de-identified Clinformatics® Data Mart Database (CDM), we identified telemedicine visits by children ≤17, excluding preventive visits and visits to specialists, emergency departments, and urgent care. Among included visits, we defined “telemedicine-only” providers as those with ≥80% of visits via telemedicine and practice-based telemedicine providers as those with ≤50% of visits via telemedicine. We then described the telemedicine visit volume and diagnoses for these categories overall and per 1000 children per month.
Results:
From January 2018-February 2020, telemedicine-only providers accounted for 57,815 telemedicine visits (90.8%), while practice-based telemedicine accounted for 4,192 telemedicine visits (6.6%). From March 2020-September 2021, telemedicine-only providers accounted for 38,282 telemedicine visits (6.1%), while practice-based telemedicine accounted for 555,125 telemedicine visits (88.2%). Per month, telemedicine visits to practice-based telemedicine providers increased from pre-pandemic to pandemic periods (0.1 vs. 12.9 visits per 1000 children/month), while telemedicine visits to telemedicine-only providers occurred at a similar rate from pre-pandemic to pandemic periods (0.92 vs 0.96 visits per 1000 children/month).
Conclusion:
We observed a large increase in telemedicine visits during the pandemic, with the growth in visits exclusively occurring among visits to practice-based telemedicine providers as opposed to telemedicine-only providers.
Introduction
Before 2020, children largely received telemedicine visits via direct-to-consumer (DTC) telemedicine vendors.1 Regulatory and payment changes during the COVID-19 public health emergency facilitated a dramatic rise in telemedicine use among children.2-4 Many “brick and mortar” practices began offering practice-based telemedicine for the first time,4-6 while some DTC telemedicine vendors reported increases in visit volume early in the pandemic.7 As a result, in the first months of the pandemic, up to 44% of problem-based primary care visits occurred via telemedicine, with this declining to 15% by fall of 2020.4
Prior studies have examined the percentage of primary care practice encounters that transitioned to practice-based telemedicine during the early pandemic,4-6 but the contribution of these new practice-based telemedicine visits relative to visits occurring with already existing DTC telemedicine vendors during the pandemic is not known. Understanding the degree to which these two different models cared for children during the pandemic may help inform ongoing policy discussions regarding reimbursement and quality metrics for telemedicine within and outside of primary care medical homes. Thus, we sought to characterize the relative contribution of practice-based vs. DTC telemedicine models in the provision of telemedicine to children from 2018 to 2021.
Methods
Among children ≤17 years old, we applied prior methods to identify telemedicine visits using Current Procedural Terminology (CPT) codes, CPT modifiers, specialty codes, place of service codes, and revenue codes4 from January 2018-September 2021 in Opium’s de-identified Clinformatics® Data Mart Database (CDM), which are derived from a database of administrative health claims for members of a large commercial health plan spanning all 50 states. These data are estimated to cover 13% of commercially insured individuals nationally.4 We used the most recent data available at the time of our analysis. To focus on telemedicine use for non-specialty problem-based outpatient visits, we excluded visits to specialists and preventive health visits. We also excluded telemedicine visits occurring in emergency departments or urgent care settings (<1% of remaining telemedicine visits). Because only a small number of visits used audio-only CPT codes (4.3%), we did not differentiate audio-only from audio-video telemedicine visits in our analysis.
Among the remaining visits, we differentiated telemedicine-only providers vs. practice-based telemedicine providers (i.e., those offering telemedicine along with in-person visits) based on the proportion of visits via telemedicine in 2018-2021. We use the term “provider” because the provider identifier code in the data had the potential to represent a clinic, health system, DTC telemedicine company or an individual clinician, depending on how claims were entered and processed. We defined “telemedicine-only” providers as those with ≥80% of visits via telemedicine and practice-based telemedicine providers as those with ≤50% of visits via telemedicine (Figure 1). We chose the 80% threshold for “telemedicine-only” providers in recognition of imperfect coding in administrative data. Providers with between 50-80% of visits via telemedicine (1.96% of providers; 4.1% of telemedicine visits) or with low volume (<25 total visits; 6.8% of providers; 1.4% of telemedicine visits) were categorized as “unclassified.” We described the telemedicine visit volume over time by these three provider categories. Focusing on visits to telemedicine-only and practice-based telemedicine, we also present visit diagnosis over time, categorized based on primary diagnosis International Statistical Classification of Diseases and Related Health Problem codes (ICD-10) as in prior analyses.6 In sensitivity analysis, we categorized providers based only on pre-pandemic visits, with minimal impact on overall findings.
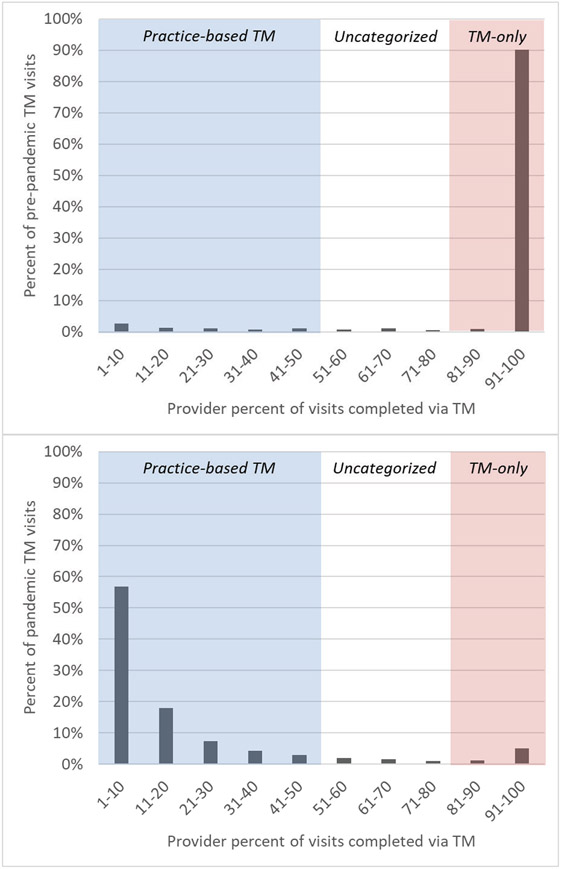
Figure 1. Telemedicine visit volume by provider percentage of telemedicine visits before and during the pandemic.
Volume of visits by provider before the pandemic (Jan 2018-Feb 2020, top) and during the pandemic (March-September 2021, bottom), binned by the percent of visits completed by telemedicine for each provider, ranging from 1% to 100%. The term “provider” is used because the identifier could encompass a single physician or a clinic, system, or DTC TM vendor. Abbreviation: TM, telemedicine.
Results
Across 5.4 million unique children, there were 693,349 telemedicine visits across 73,679 providers. Pre-pandemic (January 2018-February 2020), 1,649 providers billed for 63,683 telemedicine visits, with 142 providers categorized as telemedicine-only (8.6% of providers), 1184 (71.8%) as practice-based telemedicine providers, and 323 (37.2%) uncategorized. Telemedicine-only providers accounted for 57,815 (90.8%) pre-pandemic telemedicine visits (Figure 1). More specifically, four telemedicine-only providers accounted for 80% of telemedicine visits by children pre-pandemic. During this time period, practice-based telemedicine accounted for 4,192 (6.6%) telemedicine visits, and visits to “unclassified” providers were 2,409 (3.8%).
During the pandemic period (March 2020-September 2021), 73,132 providers billed for 629,666 telemedicine visits, with 854 providers categorized as telemedicine-only (1.2% of providers), 65,990 (90.2%) as practice-based telemedicine providers, and 6,288 providers (8.6%) uncategorized. During this period, telemedicine-only providers accounted for 38,282 (6.1%) telemedicine visits. During the same time, practice-based telemedicine providers accounted for 555,125 visits (88.2%). Visits to “unclassified” providers were 5.8% of visits (36,259) during the pandemic.
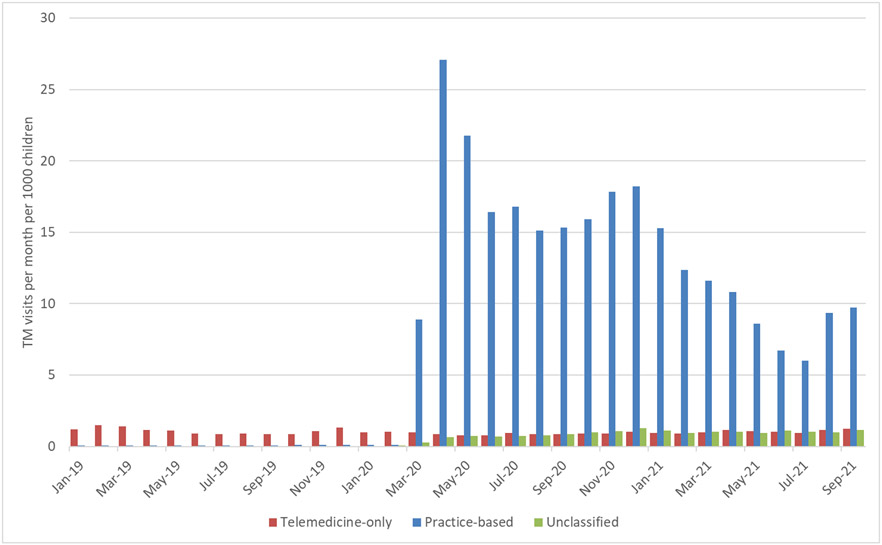
Rates of telemedicine visits by children to any telemedicine provider increased from 1.0 visits per 1000 children/month from January 2018-February 2020 (pre-pandemic) to 15.8 visits per 1000 children/month from March 2020 to September 2021. Per month, telemedicine visits to practice-based telemedicine providers increased from pre-pandemic to pandemic periods (0.1 vs. 12.9 visits per 1000 children/month, Figure 2). Meanwhile, the rate of telemedicine visits to telemedicine-only providers remained similar from pre-pandemic to pandemic periods (0.92 vs 0.96 visits per 1000 children/month).
Figure 2: Telemedicine visit volume by provider percent telemedicine, 2019-2021.
Volume of visits by telemedicine-only providers (≥80% telemedicine, red), practice-based telemedicine providers (≤50% telemedicine, blue), and unclassified (between 50-80% telemedicine or <25 visits total, green) during pre-pandemic (February 2020 and earlier) and pandemic (March 2020 and after) periods. Due to relatively stable findings from January 2018 through February 2020, we omitted the first year of data from the figure, which starts in January 2019.
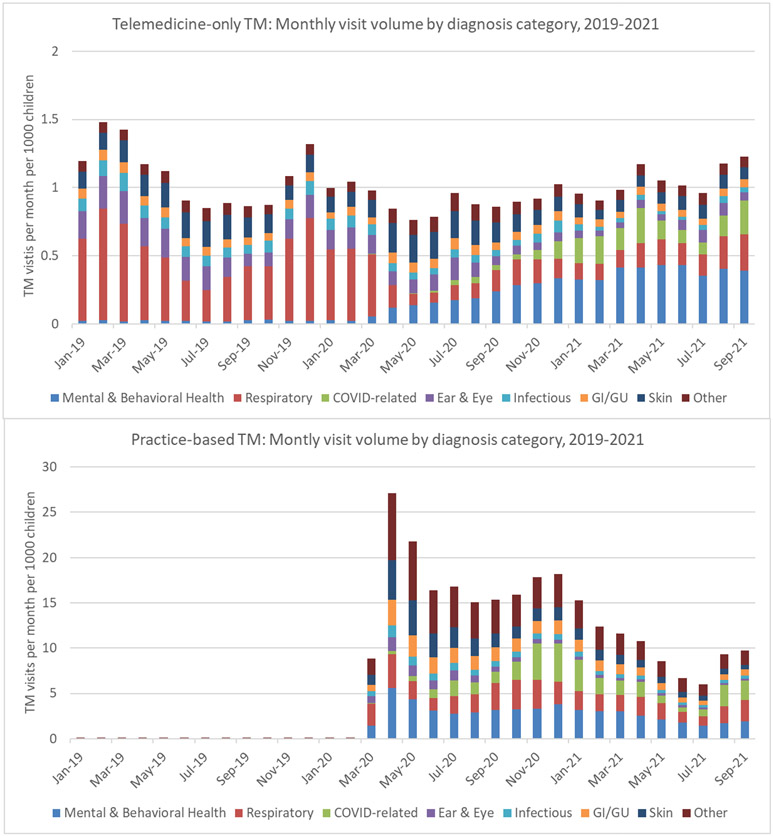
During the pre-pandemic period, the most common diagnosis categories among visits to telemedicine-only providers were respiratory (average of 0.45 visits per 1000 children per month from January 2018-February 2020, 47% of telemedicine-only visits), followed by eye/ear (0.16 visits per 1000 children per month, 17%) and dermatologic (0.13 visits per 1000 children per month, 13%) concerns (Figure 3). In the first six months of the pandemic, skin-related diagnoses (average of 0.19 visits per 1000 children per month from March 2020-August 2020, 22%) were most common among visits to telemedicine-only providers, followed by respiratory (0.17 visits per 1000 children per month, 18%) and mental health diagnoses (0.14 visits per 1000 children per month, 16%). Later in the pandemic (September 2020-September 2021), mental health diagnoses were most common (averaging 0.35 visits per 1000 children per month, 35%), followed by respiratory (0.17 visits per 1000 children per month visits per month, 17%) and COVID-19 related diagnoses (0.14 visits per 1000 children per month, 14%) among visits to telemedicine-only providers.
Figure 3: Telemedicine visit volume by diagnosis category for telemedicine-only and practiced-based telemedicine providers, 2019-2021.
Volume of visits by diagnosis categories for telemedicine-only providers (top) and practice-based telemedicine providers (bottom), January 2019-September 2021. Note that the panels have different y-axis scales. Due to relatively stable findings from January 2018 through February 2020, we omitted the first year of data from the figure, which starts in January 2019. Abbreviation: TM, telemedicine.
During the pre-pandemic period, the most common diagnosis category among telemedicine visits with practice-based providers was mental health (average of 0.03 visits per 1000 children per month from January 2018-February 2020, 49% of practice-based telemedicine visits), followed by respiratory diagnoses (0.01 visits per 1000 children per month, 10%; Figure 3). In the first six months of the pandemic, mental health (average of 3.4 visits per 1000 children per month from March 2020-August 2020, 19%), skin-related (2.7 visits per 1000 children per month, 15%) and respiratory (2.2 visits per 1000 children per month, 13%) were most common diagnoses among telemedicine visits to practice-based providers. Later in the pandemic (September 2020-September 2021), diagnoses among practice-based telemedicine visits were most commonly mental health diagnoses (averaging 2.6 visits per 1000 children per month, 22%), followed by respiratory (2.1 visits per 1000 children per month, 18%) and COVID-19 related diagnoses (2.0 visits per 1000 children per month, 17%).
Discussion
Our findings show a large increase in telemedicine visits per 1000 children at the onset of the pandemic, with the growth in visits exclusively occurring among practice-based telemedicine visits (i.e., visits to brick-and-mortar practices offering telemedicine visits while also providing in-person visits to children). In contrast, telemedicine-only providers, who previously accounted for 90% of telemedicine visits by children, did not increase their provision of telemedicine visits to children from 2018 to 2021.
The American Academy of Pediatrics discourages telemedicine use outside the medical home because of concerns about increased fragmentation and lower quality of care,8 but whether families differentiate between practice-based vs. telemedicine-only providers when selecting pediatric care options is not clear. From the family perspective, practice-based telemedicine may offer continuity of relationships and information and may allow them to connect with a known clinician.3 In contrast, telemedicine-only providers may have appointments available on-demand and when practice-based offices are closed. Given their pre-pandemic years of experience in telemedicine, telemedicine-only providers may also have applications better optimized for user experience and clinicians more experienced in telemedicine care (compared to practice-based settings with evolving training and workflows during the early pandemic9,10). One DTC telemedicine company caring for all age patients reported a 59% increase in visit volume during the early pandemic period,7 suggesting movement towards commercial DTC platforms during the pandemic. Our results suggest distinctly different patterns of care for children during this time, with telemedicine visit growth by children occurring exclusively within practice-based settings. Practice-based telemedicine visit rates were lower in the second year of the pandemic and demonstrated seasonal variation, but remained sixfold to tenfold higher than telemedicine-only visits by children.
Mental health was the most common diagnosis category for practice-based telemedicine both pre-pandemic and during the pandemic, although the volume of these visits grew nearly 100-fold, from 0.03 to 2.6 visits per 1000 children per month. Mental health was an uncommon diagnosis among telemedicine-only providers pre-pandemic, but represented a third of visits in the later pandemic period with a rate of 0.35 visits per 1000 children per month. While the potential for telemedicine to improve access to mental health care has been discussed,11-13 these data provide evidence that telemedicine particularly within practice-based models may be maturing into a model that is indeed contributing to primary care-based mental health care for children.
By the end of the study period, respiratory and COVID-19 related diagnoses were the next most common diagnoses in both telemedicine settings, comprising approximately one-third of visits. COVID-19-related diagnoses were not common in the first 6 months of the pandemic in either setting, but increased over time, likely due to evolving COVID-19 epidemiology and testing capabilities. The volume of visits for COVID-19 related diagnoses to practice-based telemedicine peaked in November and December 2020, consisting with national peaks in COVID-19 cases and testing.14
These data show sustained use of practice-based telemedicine by children through September 2021, but it is worth noting these data all occurred during the ongoing public health emergency, which has simplified technical and financial barriers to practice-based telemedicine for children. Prior to the pandemic, most pediatric primary care practices could not offer telemedicine due to restrictions by health plans and state Medicaid rules regarding patient location and provider type.15 At present, all state Medicaid programs offer payment for at least some types of live interactive telemedicine, but variable restrictions remain within state Medicaid programs regarding reimbursable types of services, types of provider, and patient location. Specifically, the ability to provide telemedicine to children at home is an essential component of primary care telemedicine. However, Medicaid programs for only 33 states and D.C. specifically allow for the patient to be located at home during a telemedicine encounter.15 Private payer laws also vary substantially by state, with components related to both telemedicine-only and practice-based telemedicine including regulations related to payment parity for in-person and telemedicine services, payment for audio-only telemedicine, payment to out-of-network providers or to specific vendors, and provision of culturally and linguistically appropriate telemedicine services.15 Thus, while practice-based telemedicine is proposed as a key to the future of primary care16 and is demonstrably used by families in these data, the regulatory and payment changes that have supported practice-based telemedicine during the pandemic have yet to be made permanent in many state regulations and state Medicaid programs.
Limitations of our analyses include that data were deidentified, so that telemedicine-only versus practice-based telemedicine was defined solely by provider-level visit patterns. Our categorization of telemedicine-only versus practice-based telemedicine left approximately 5% of visits uncategorized. We report these visits separately throughout, but we acknowledge that they follow a temporal trend more similar to the practice-based telemedicine visits over time. This analysis of claims data also does not include measures of clinical outcomes or patient and family experience, and this analysis was not designed to investigate equity in utilization. These results report on a time period during which visits by children and especially visits for common acute respiratory tract infections were markedly lower than prior years due to pandemic-related public health mitigation strategies.4 Additionally, this analysis is limited to a subset of commercially insured patients, and may not generalize to uninsured or Medicaid insured children, many of whom have experience increased barriers to telemedicine both before and during the pandemic.17,18
In conclusion, our results demonstrate that during the pandemic when regulatory changes allowed primary care practices to provide and receive payment for telemedicine to patients at home, the marked growth in telemedicine visits by children occurred exclusively among practice-based telemedicine providers, with visits most commonly occurring for mental health, respiratory, and COVID-19 related diagnoses.
What’s New.
Telemedicine visits by children to practice-based telemedicine providers increased substantially with the onset of the COVID-19 pandemic, while telemedicine visits by children to telemedicine-only providers occurred at a similar rate before and during the pandemic.
Funding Source:
This work was supported by the National Institute of Allergy and Infectious Diseases (R01AI148159; KNR). The content is solely the responsibility of the authors and does not necessarily represent the official views of, nor an endorsement by, the NIH or the US Government.
Role of Funder/Sponsor:
The funder/sponsor did not participate in the work.
Abbreviations:
- CPT
Current Procedural Terminology
- CDM
Clinformatics Data Mart
- DTC
direct to consumer
- TM
telemedicine
Footnotes
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Ray KN, Shi Z, Poon SJ, Uscher-Pines L, Mehrotra A. Use of Commercial Direct-to-Consumer Telemedicine by Children. Acad Pediatr. 2019;19(6):665–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation In Telemedicine Use And Outpatient Care During The COVID-19 Pandemic In The United States. Health Aff (Millwood). 2021;40(2):349–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curfman AL, Hackell JM, Herendeen NE, et al. Telehealth: Improving Access to and Quality of Pediatric Health Care. Pediatrics. 2021;148(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schweiberger K, Patel SY, Mehrotra A, Ray KN. Trends in Pediatric Primary Care Visits During the Coronavirus Disease of 2019 Pandemic. Acad Pediatr. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macy ML, Huetteman P, Kan K. Changes in Primary Care Visits in the 24 Weeks After COVID-19 Stay-at-Home Orders Relative to the Comparable Time Period in 2019 in Metropolitan Chicago and Northern Illinois. J Prim Care Community Health. 2020;11:2150132720969557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schweiberger K, Hoberman A, Iagnemma J, et al. Practice-Level Variation in Telemedicine Use in a Pediatric Primary Care Network During the COVID-19 Pandemic: Retrospective Analysis and Survey Study. J Med Internet Res. 2020;22(12):e24345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uscher-Pines L, Thompson J, Taylor P, et al. Where Virtual Care Was Already a Reality: Experiences of a Nationwide Telehealth Service Provider During the COVID-19 Pandemic. J Med Internet Res. 2020;22(12):e22727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Conners GP, Kressly SJ, Perrin JM, et al. Nonemergency Acute Care: When It's Not the Medical Home. Pediatrics. 2017;139(5). [DOI] [PubMed] [Google Scholar]
- 9.Schinasi DA, Foster CC, Bohling MK, Barrera L, Macy ML. Attitudes and Perceptions of Telemedicine in Response to the COVID-19 Pandemic: A Survey of Naive Healthcare Providers. Front Pediatr. 2021;9:647937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fitzgerald M, Bhatt A, Thompson LA, et al. Telemedicine in Pediatric Training: A National Needs Assessment of the Current State of Telemedicine Education in Pediatric Training. Acad Pediatr. 2021. [DOI] [PubMed] [Google Scholar]
- 11.Buka SL, Beers LS, Biel MG, et al. The Family is the Patient: Promoting Early Childhood Mental Health in Pediatric Care. Pediatrics. 2022;149(Suppl 5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cunningham NR, Ely SL, Barber Garcia BN, Bowden J. Addressing Pediatric Mental Health Using Telehealth During Coronavirus Disease-2019 and Beyond: A Narrative Review. Acad Pediatr. 2021;21(7):1108–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gotkiewicz D, Goldstein TR. Extending Our Virtual Reach: Pediatricians and Mental Health Providers Bridging the Chasm to Mental Health Care for Adolescents and Transition-Age Youth During COVID-19. Clin Pediatr (Phila). 2021;60(9-10):389–391. [DOI] [PubMed] [Google Scholar]
- 14.Center for Disease Control and Prevention. COVID Data Tracker. 2022; https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed May 11, 2022.
- 15.Center for Connected Health Policy. State telehealth laws and Medicaid program policies: a comprehensive scan of the 50 states and District of Columbia. . 2022; https://www.cchpca.org/telehealth-policy/state-telehealth-laws-and-reimbursement-policies-report. Accessed May 11, 2022.
- 16.National Academies of Sciences Engineering and Medicine. Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care. Washington, DC: The National Academies Press;2021. [PubMed] [Google Scholar]
- 17.Webber EC, McMillen BD, Willis DR. Health Care Disparities and Access to Video Visits Before and After the COVID-19 Pandemic: Findings from a Patient Survey in Primary Care. Telemed J E Health. 2021. [DOI] [PubMed] [Google Scholar]
- 18.Rosenthal JL, O'Neal C, Sanders A, Fernandez YGE. Differential Use of Pediatric Video Visits by a Diverse Population During the COVID-19 Pandemic: A Mixed-Methods Study. Front Pedlatr. 2021,’9:645236. [DOI] [PMC free article] [PubMed] [Google Scholar]