Abstract
We present a previously healthy young man with cardiac tamponade. He underwent emergency pericardiocentesis. The pericardial fluid was exudative, and Salmonella sp. was grown on both pericardial and blood cultures. Further investigations revealed that this patient had classical Hodgkin lymphoma, which explains his immunocompromised state predisposing him to this infection. (Level of Difficulty: Advanced.)
Key Words: cardiac tamponade, classical Hodgkin Lymphoma, massive pericardial effusion, salmonellosis
Abbreviations and Acronyms: ECG, electrocardiogram; LDH, lactate acid dehydrogenase; RV, right ventricular
Central Illustration
Case Presentation
A 21-year-old male student presented to the emergency department with intermittent low-grade fever, shortness of breath, and palpitations of 1 week’s duration. He had a history of regular kratom (Mitragyna speciosa) tea intake for the past 4 years. Apart from that, he also had reduced appetite and experienced some weight loss. He had no recent travel history, no contact with a tuberculosis patient, and no history of eating undercooked eggs or taking illicit drugs.
Learning Objectives
-
•
To be aware that an unusual cause of cardiac tamponade is most often found in the immunocompromised patient.
-
•
To highlight the importance of good clinical judgment for early intervention in cardiac tamponade.
-
•
To be aware that cardiac tamponade can have a subacute onset, especially with an infective or malignant cause.
In the emergency department, his initial blood pressure was 96/72 mm Hg, his pulse rate 120 beats/min, his respiratory rate 25 breaths/min, and his oxygen saturation was 100% under high-flow oxygen therapy. His jugular venous pressure was elevated and distended with the presence of pulsus paradoxus, and his heart sounds were muffled. On auscultation of the lungs, breath sounds were reduced at the bilateral lower zones, and multiple matted cervical lymph nodes were palpable bilaterally.
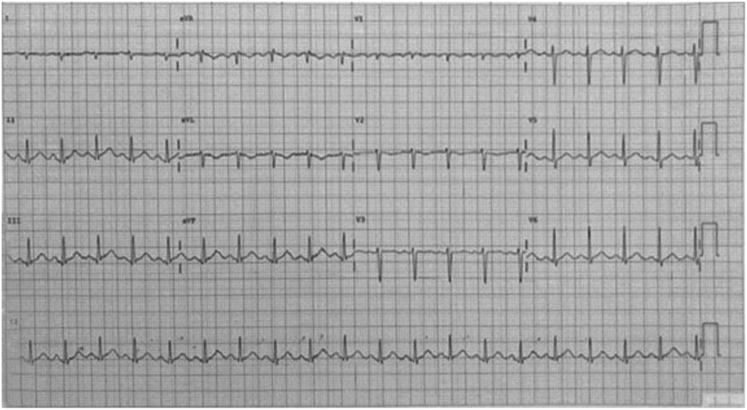
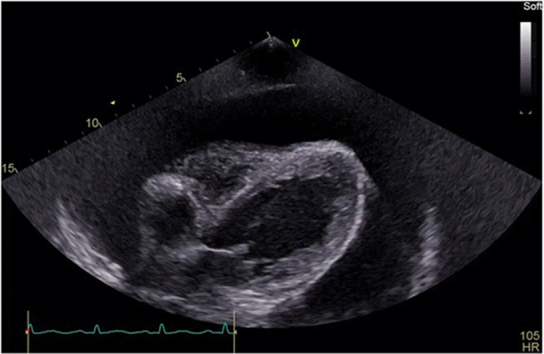
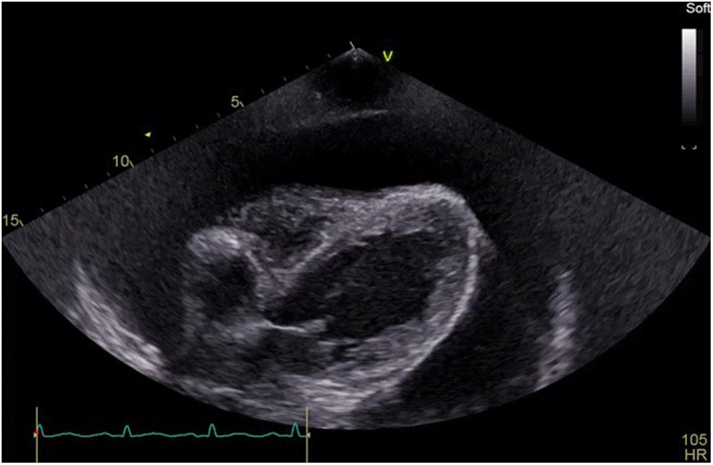
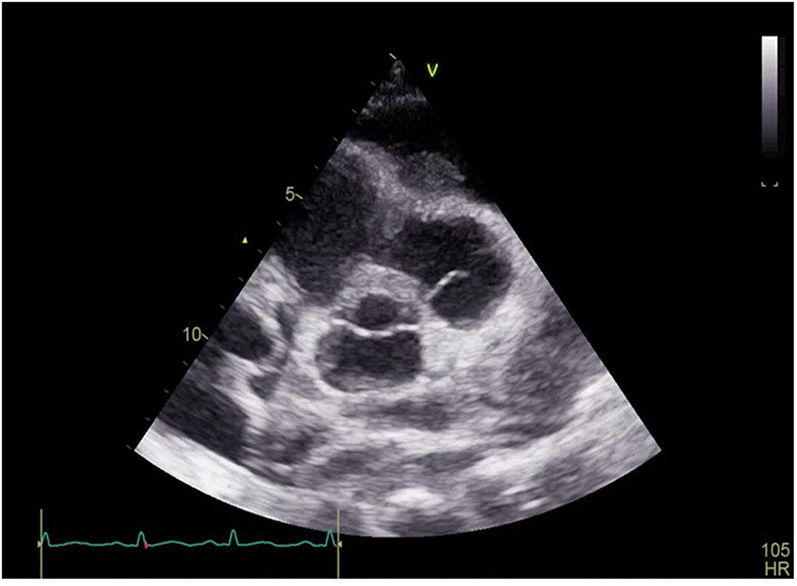
Transthoracic echocardiography (Figures 1 and 2, Videos 1 and 2) showed a massive pericardial effusion with right atrial and right ventricular (RV) collapse during diastole. The chest radiograph (Figure 3) exhibited cardiomegaly with bilateral pleural effusions. His electrocardiogram (ECG) (Figure 4) showed sinus tachycardia, low ECG voltage, and electrical alternans.
Figure 1.
Subcostal View Showing Massive Global Pericardial Effusion With Right Ventricular and Right Atrial Collapse During Diastole
Figure 2.
Short-Axis View on the Aortic Level Showing a Right Atrial Indentation During Diastole
Figure 3.
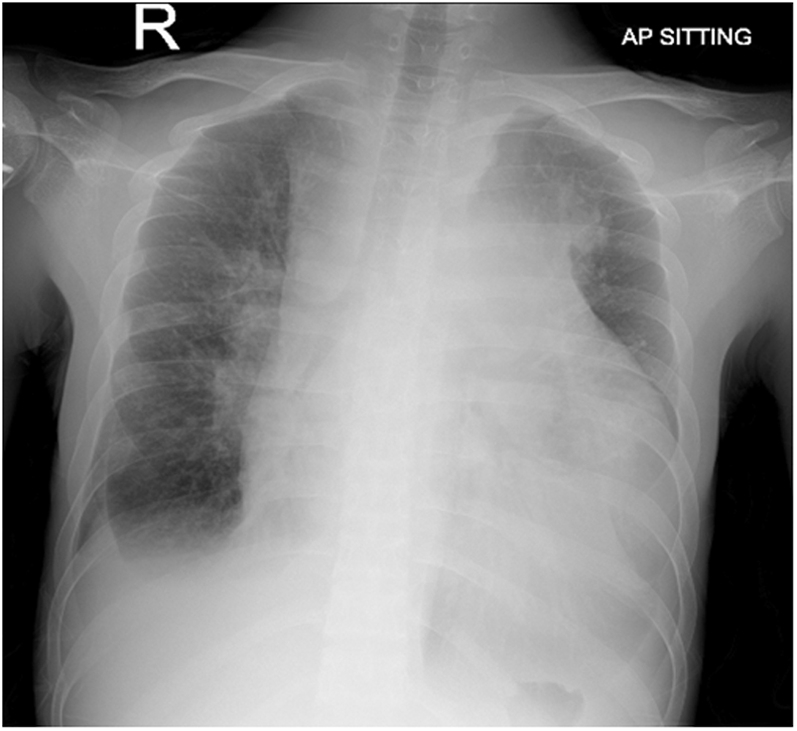
Globular Heart Shadow With Bilateral Pleural Effusion
AP = anteroposterior; R = right.
Figure 4.
Electrocardiogram Showing Sinus Tachycardia With Low Electrocardiographic Voltage and Electrical Alternans
Emergency pericardiocentesis through the subcostal approach was done, and 500 mL of serous pericardial fluid was drained. Blood testing showed a white blood cell count of 23 × 109/L, a hemoglobin level of 10 g/dL, a platelet count of 471 × 109/L, and normal liver and renal function test results. The serum lactate dehydrogenase (LDH) level was 1,024 U/L. Pericardial fluid analysis showed the following: protein, 53 g/dL (range: 0.15-0.45 g/dL); glucose, 4.8 mmol/L (range: 2.2-4.4 mmol/L); and LDH, 1,024 U/L, which confirmed exudative fluid. His retroviral and hepatitis screening results were negative. Direct smear examination of the pericardial fluid was unremarkable. On review of pericardial cytology, there were no suspicious cells; hence no flow cytometry was performed. On McConkey agar, pericardial fluid culture and blood culture yielded non–lactose-fermenting colonies, and the Gram stain revealed gram-negative bacilli (Figure 5). The organism was identified as a Salmonella sp by a standard biochemical test, serotyping, and the VITEK 2 system (bioMérieux).
Figure 5.
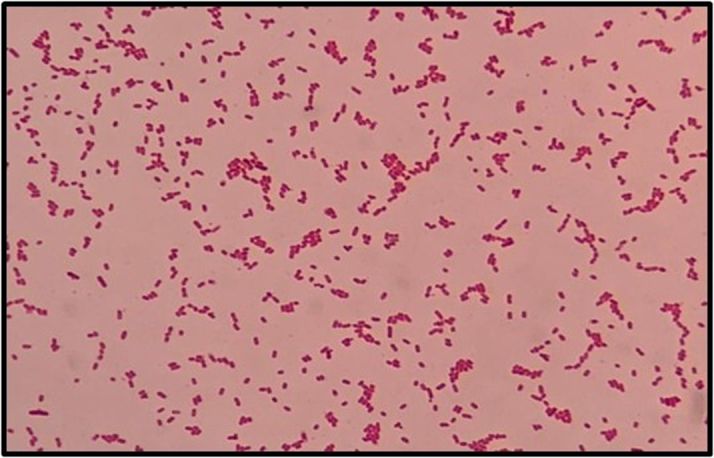
Gram-Negative Bacilli on Gram Stain
The 16S molecular test confirmed Salmonella enterica subspecies enterica serovar enteritidis. It was susceptible to ampicillin, ceftriaxone, and trimethoprim-sulfamethoxazole.
Before culture and sensitivity testing, empirical antibiotic therapy with intravenous piperacillin-tazobactam, 4.5 g 3 times daily, was given for 3 days, and then it was changed to intravenous ceftriaxone, 2 g twice daily for 2 weeks, after pericardial fluid and blood culture isolated Salmonella enterica. The patient was subsequently under the care of a hematologist for his classical Hodgkin lymphoma. He received a diagnosis of disseminated nontyphoidal salmonellosis. Because he had multiple matted cervical lymph nodes, fine-needle aspiration cytologic examination of a cervical lymph node was done and showed a lymphoid neoplasm. Subsequently, excisional biopsy confirmed classical Hodgkin lymphoma. The patient was discharged with a regimen of oral trimethoprim-sulfamethoxazole, 2 tablets twice daily for a total duration of 4 weeks. Repeat echocardiography 4 weeks later showed minimal residual pericardial effusion, and chemotherapy for classical Hodgkin lymphoma was initiated.
Discussion
The pericardium is a sac surrounding the heart that contains 20 to 60 mL of ultrafiltrate, and it is relatively stiff.1 In patients with acute cardiac tamponade, the pericardium is rapidly filled by approximately 200 to 300 mL of fluid, and symptoms are more acute in onset.1 Conversely, in patients with subacute cardiac tamponade, the pericardium sac is slowly filled with up to 1 to 2 L of fluid, and symptoms are more insidious.1 Because of this pathophysiology, our patient’s presentation was subacute, rather than the acute onset of cardiac tamponade, although the amount of pericardial fluid was massive. Cardiac tamponade is an emergency that requires early detection and recognition from clinical findings and is confirmed by echocardiography, as shown in our patient’s clinical presentation. Urgent pericardiocentesis is mandatory in patients with cardiac tamponade to improve RV function and increase venous return.1 The pericardiocentesis approach is varied; however, the safest approach is the subcostal approach.1
Salmonella infection usually involves the gastrointestinal tract and is significant. Nontyphoidal extraintestinal Salmonella infection is less prevalent compared with intestinal nontyphoidal Salmonella infection.3 Extraintestinal nontyphoidal Salmonella infection commonly occurs in the meninges, the musculoskeletal system, and the urinary tract. In contrast, pericardial involvement is low, reported as <2%.2 Salmonella infection as a cause of cardiac tamponade in Malaysia is rare.4 Although the prevalence is low, nontyphoidal Salmonella pericarditis or tamponade has a high mortality.
In Kelantan, Malaysia, kratom has been used as a homemade supplement drink for energy, and kratom ingestion is a possible reason that this patient with an undiagnosed immunocompromised condition contracted salmonellosis. According to an article by the U.S. Food and Drug Administration in 2018, there was an outbreak of salmonellosis from multiple strains linked to kratom and its products.5 The investigation led to mandatory recall of all kratom and its products from the market.
In the patient with nontyphoidal salmonellosis with pericarditis, there is no clear evidence on the duration of antibiotic given to the patient on the basis of guidelines. Trimethoprim-sulfamethoxazole had good bioavailability with good tissue penetration; hence this patient received this medication for 4 weeks after receiving intravenous ceftriaxone for 2 weeks. The patient underwent long-term chemotherapy for his classical Hodgkin lymphoma. Cholecystectomy would be considered if disseminated nonthypoidal salmonellosis recurs.
Conclusions
Cardiac tamponade is a life-threatening condition in which early recognition and intervention are mandatory. This case describes a young patient with undiagnosed classical Hodgkin lymphoma who presented with subacute cardiac tamponade secondary to salmonellosis bacteremia, a rare cause of exudative pericardial effusion.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental videos, please see the online version of this article.
Appendix
Subcostal View Showed Massive Global Pericardial Effusion With RV and RA Collapse During Diastole
Short-Axis View on the Aortic Level Showed RA Indentation During Diastole
References
- 1.Imazio M., de Ferrari G.M. Cardiac tamponade: an educational review. Eur Heart J Acute Cardiovasc Care. 2021;10(1):102–109. doi: 10.1177/2048872620939341. [DOI] [PubMed] [Google Scholar]
- 2.O’Mahony D., Peikarz R.L., Bandettini W.P., Arai A.E., Wilson W.H., Bates S.E. Cardiac involvement with lymphoma: a review of the literature. Clin Lymphoma Myeloma. 2008;8(4):249–252. doi: 10.3816/CLM.2008.n.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sudhaharan S., Kanne P., Vemu L., Bhaskara A. Extraintestinal infections caused by non-typhoidal Salmonella from a tertiary care center in India. J Lab Physicians. 2018;10(4):401–405. doi: 10.4103/JLP.JLP_79_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Low Q.J., Teo K.Z., Thien L.K., Lim T.H., Cheo S.W. Cardiac tamponade: experience from a Malaysian district hospital. J R Coll Physicians Edinb. 2020;50(4):387–391. doi: 10.4997/JRCPE.2020.407. [DOI] [PubMed] [Google Scholar]
- 5.FDA investigated multistate outbreak of Salmonella infections linked to products reported to contain kratom. U.S. Food and Drug Administration. 2018. https://www.fda.gov/food/outbreaks-foodborne-illness/fda-investigated-multistate-outbreak-salmonella-infections-linked-products-reported-contain-kratom
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Subcostal View Showed Massive Global Pericardial Effusion With RV and RA Collapse During Diastole
Short-Axis View on the Aortic Level Showed RA Indentation During Diastole