Abstract
To compare the district level prevalence of childhood stunting between NFHS-4 and NFHS-5 and to explore the correlates of it at the district level. Although malnutrition rates in India have decreased over a period, country is still a home for the highest number of stunted and wasted children in the world. Among the South Asian countries, India has the second highest number of stunted children. An ecological study conducted by using the data from fourth and fifth round of National Family Health Survey. Study concentrated on percentage of children who were stunted across 692 Indian districts during 2 survey periods and its correlates from NFHS-5. District level change in childhood stunting was calculated by differencing the NFHS-5 estimates from NFHS-4. Descriptive statistics were used to understand the nature of the variables and Moran’s I statistic was calculated to check for the spatial autocorrelation in the childhood stunting. Spatial error regression model was used to identify the correlates of childhood stunting. Among the Indian districts considered, 243 districts showed the increase in childhood stunting between the time periods considered. Currently, about 33.56% of children in India are stunted and there is high spatial disparity in the prevalence of childhood stunting among the districts of it. Major hotspots of childhood stunting were found in the parts of UP, Bihar, Jharkhand, and West Bengal. Households access to improved sanitation facility, iodized salt, clean fuel, women 10 plus years of schooling, post-natal care of mother were found to be the significant protective factors. Closed spacing of births, teenage pregnancy, low BMI of women, childhood diarrhea, and anemia were found to be the significant risk factors of childhood stunting. Stunting depends on several other factors apart from poverty, working on these factors will help in reducing childhood stunting in India.
Keywords: childhood stunting, maternal health, women health, national family health survey, spatial regression
What do we already know about this topic
India had witnessed the dramatic decrease in the prevalence of childhood stunting from 48% in 2005-06 to 38.5% in 2015-16 and it is working toward eliminating all forms of malnutrition in the country.
How does your research contribute to the field?
This study helps in understanding the district level change in the prevalence of childhood stunting from NFHS-4 to NFHS-5, current scenario of childhood stunting in the districts and identifying the different factors other than poverty that are influencing the prevalence of childhood stunting in India.
What are your research’s implications toward theory practice, or policy?
Comparative and spatial analysis taken up in this study will help in assessing the performance of policies and programs taken up by the government to combat childhood stunting in the last 5 years and planning future interventions.
Introduction
Though India has recently achieved considerable progress in reducing the childhood stunting, childhood stunting is still one among the major public health concerns in India as country bears the highest number of stunted and wasted children in the world.1 Childhood stunting being one of the indicators of child nutritional status, indicates the chronic malnutrition.2 Stunting refers to a child who is too short for his or her age. Children are defined as stunted if their height-for-age is more than 2 standard deviations below the WHO Child Growth Standards median.3 Impacts of childhood stunting are not just restricted to childhood but far beyond childhood. Children affected by stunting may have impaired brain development, poor cognition, and perform poor in learning.4 Besides, it also affects working ability and earning capacity of child in later ages.4 Considering all these adverse effects of childhood stunting, in the World Summit for Children that was held at New York in 1990, the decision was made to take up the actions to “end the child death and child malnutrition and to provide the basic protection for the normal physical and mental development of all the world’s children.”5 This international commitment was quickened in the Millenium Development Goals era, and further accelerated with the adoption of Global Targets 2025 set by WHO, the UN Sustainable Development Goals 2030, and the WHO/UNICEF 2030 nutrition targets.6 In accordance with these global targets with the international cooperation, Government of India is working hard to reduce malnutrition in the country by taking up numerous interventions and implementing policies and programs at nationwide.7 Along with the existing programs such as Integrated Child Development Scheme (ICDS), Reproductive & Child Health (RCH), National Rural Health Mission (NRHM), Anganwadi Services, schemes for Adolescent Girls, Pradhan Mantri Matru Vandana Yojana (PMMVY) and so on), has launched world’s largest nutrition program, POSHAN Abhiyaan with the aim of improving nutrition among children and mothers in 2018.7,8 From the recent round of National Family Health Survey (NFHS-5) reports, it was evident that India showed a declining trend in childhood stunting from 48% in 2006 to 35.5% in 2021. Despite of this remarkable decline, according to the recent report by the world bank (2019), among the South Asian countries India has the second highest number of stunted children (38%), after Afghanistan (41%).9 Numerous studies have been conducted in India in the past few years to understand the prevalence of childhood stunting at district level and to identify the demographic, environmental, and socio-economic factors that significantly influence the childhood malnutrition which helped in planning and implementation of policies & programs. With the poverty being one of the associated factors, multiple studies identified a significant association of mother’s with low Body Mass Index (BMI),1,10-12 women educational status,1,11-13 maternal health,11,14 breastfeeding practices,15 infections and poor child care,15,16 teenage pregnancy,1,11,12 closely spaced births,12,13 availability of safe drinking water,1,13,15 and improved sanitation facility with childhood malnutrition.1,13 Though plenty of studies are available for India to understand the trend and spatial distribution of childhood stunting across its districts and risk factors associated with it, no studies are there to give insight into the change in the prevalence of stunting across all the districts of India in the last 5 years (2015-2016-2019-21).Recently, NFHS-5 reports at the national level indicated the improvement in many characteristics that were associated with childhood stunting in the last 5 years, but improvements in childhood stunting is not in line with them. Hence it is essential to re examine the association of stunting with factors which are already known to have influence on it, which will help in taking up better interventions. Along with these, it is also necessary to check the change in the spatial distribution of childhood stunting for the better understanding before formulating any policies and programs and allocate the funds.
Considering these needs, the present study has been taken up with the following objectives. First, to study the spatial distribution and change in childhood stunting from NFHS-4 to NFHS-5 among the districts of India. Second, to re-examine the factors influencing the prevalence of childhood stunting using NFHS-5 data. The findings from the study may help policy makers, public health researchers and health workers in better understanding of the dynamic nature of the childhood stunting across Indian districts and gives insight into the factors influencing its prevalence.
Material and Methods
Data Source
The present ecological study was done for India, comprising of 28 states and 8 union territories which are further divided into districts. In India, National Family Health Surveys are the main source to track the status of health and development of the nation. The National Family Health Survey (NFHS) is a large-scale, cross-sectional, and multi-round survey conducted in India with the aim of collecting essential information and emerging issues related to health, nutrition, and family welfare for India and each state/union territory (UTs).17 Five rounds of survey have been conducted since the first survey in 1992-93. First 3 surveys were designed to provide a reliable estimate on different health indicators for national and state level but not to the district level. It was only the fourth round of survey (NFHS-4 conducted in 2015-16) that provided the reliable estimates of key indicators of health and nutrition of the country up to the district level. The recent survey, National Family Health Survey 2019-21 (NFHS-5), being the fifth in the series is also designed to provide the disaggregated estimates up to district level for many important health and nutrition indicators. This study was carried out considering 2 time periods of the NFHS series (NFHS-4 and NFHS-5).17 Since the framework and content in both NFHS-5 and NFHS-4 is very similar, comparing the childhood stunting between these 2 periods is possible.18 Fact sheets for each district which are freely available in the respective websites (http://rchiips.org/nfhs/) can be accessed without any official requests.
For the comparative study, the district level percentage of children under 5 years who are stunted were collected for 692 districts of India for both the periods using corresponding fact sheets. For identifying the correlates of childhood stunting for the period 2019-21, additional 17 predictor variables information at district level were collected using NFHS-5 fact sheets. The predictor variables considered in this study were chosen based on the extensive literature survey.1,10-16 Details about variables used in this study are provided in Table 1.
Table 1.
Variables Considered in the Study and Their Descriptive Statistics.
| Variables (%) | Mean ± SD | Range (Min-Max) | CV (%) |
|---|---|---|---|
| Outcome variable | |||
| Children under 5 year who are stunted (Stunting) (NFHS-5) | 33.57 ± 8.47 | 13.20-60.60 | 25.22 |
| Risk factors | |||
| Population living in households with an improved drinking-water source (DW) | 93.87 ± 8.41 | 41.20-100.00 | 8.96 |
| Population living in households that use an improved sanitation facility (SAN) | 71.90 ± 14.41 | 29.20-99.90 | 20.15 |
| Households using clean fuel for cooking (CF) | 54.31 ± 24.10 | 8.60-99.70 | 44.38 |
| Women with 10 or more years of schooling (WTL) | 40.44 ± 14.2 | 13.60-88.20 | 35.1 |
| Birth in 5 year preceding the survey that are third or higher order (TMB) | 2.07 ± 1.61 | 0.00-8.00 | 77.81 |
| Women aged 15 to 19 year who were already mothers or pregnant at the time of the survey (MTP) | 6.14 ± 5.00 | 0.00-27.30 | 81.46 |
| Women whose Body Mass Index (BMI) is below normal (BMI < 18.5 kg/m2) (BMI) | 17.97 ± 7.42 | 1.20-43.60 | 41.28 |
| Mother who had at least 4 ANC visit (MAC) | 60.50 ± 20.35 | 4.40-98.70 | 33.63 |
| Mother who consumed iron and folic acid (IFA) for 100 days or more when they are pregnant (MIFA) | 46.30 ± 21.34 | 1.60-95.00 | 46.08 |
| Mothers who received the post-natal care (MPC) | 78.82 ± 15.11 | 7.1-99.50 | 19.18 |
| Children who received the post-natal care (CPC) | 79.12 ± 14.81 | 22.40-99.60 | 18.72 |
| Prevalence of diarrhea in the 2 week preceding the survey (CD) | 6.51 ± 4.11 | 0.00-39.3 | 63.05 |
| Prevalence of symptoms of acute respiratory infection (ARI) in the 2 week preceding the survey (CARI) | 2.55 ± 2.06 | 0.00-11.20 | 80.81 |
| Children aged 6 to 59 month who are anemic (<11.0 g/dl) (CA) | 65.86 ± 12.01 | 28.00-95.50 | 18.24 |
| Households using iodized salt (IS) | 95.06 ± 5.50 | 47.90-100.00 | 5.79 |
| Children aged 9 to 35 month who received a Vitamin A dose in last 6 month (CVA) | 72.44 ± 13.30 | 27.50-98.10 | 18.36 |
| Children under age 3 year breastfed within 1 h of birth (EIBF) | 44.64 ± 16.35 | 7.80-88.50 | 36.62 |
Statistical Analysis
During NFHS-4, there were 640 districts within which the survey was carried out, while at the time of NFHS-5 there were 707 districts. To compare the change in prevalence of childhood stunting from NFHS-4 to NFHS-5, adjustment was made for the increase in number of districts. For the new districts that were carved from 1 single district, estimates of childhood stunting were assigned same as their parent districts. In cases where the districts have been carved from multiple districts, average values of the parent districts have been used for new districts.19 Change in the prevalence of childhood stunting in each district between NFHS-4 and NFHS-5 was calculated by differencing the NFHS-5 estimate from NFHS-4. Districts were grouped into 3 groups depending on the value of the % change in childhood stunting (Prevalence increased group if % increase is ≥1, prevalence decreased group if % decrease ≥1, no change group if % change is between −1and +1). Details are given in Supplemental File 1. To understand the spatial distribution of childhood stunting between NFHS-4 and NHFS-5, Prevalence maps univariate Local indicator of spatial autocorrelation (LISA) cluster map and Moran’s I were estimated using QGIS and Geoda 1.18.0 software.20 LISA cluster maps will classify the clusters into high-high, high-low, low-high, and low-low clusters. Usually, high- high (hotspots) and low-low (cold spots) are spatial clusters. Other 2 clusters are termed as outliers.21 Moran’s statistic value ranges from −1 to +1, where value of zero indicates the absence of spatial autocorrelation (ie, areas with similar % childhood stunting are randomly distributed), a positive Moran’s value indicates positive spatial autocorrelation (ie, areas with similar % childhood stunting are closely distributed), and a negative Moran’s value indicates negative spatial autocorrelation (ie, areas with dissimilar % childhood stunting are closely distributed).20
Further, descriptive statistics such as mean, standard deviation (SD), minimum, maximum, and Coefficient of variation for each variable included in the study (that are collected from NFHS-5 fact sheets) were calculated to understand the detailed nature of the variables included in the study. Pearson’s correlation coefficient has been used to check the association between the outcome variable (% childhood stunting of NFHS-5) and the predictor variables considered in the study. Based on the significant nature of the association of predictor variables with outcome variable (positive or negative), predictor variables were grouped into 2 groups for further analysis.
To identify the risk factors of childhood stunting among children under 5 years in India, 3 regression models were considered separately for 2 groups of predictors. The 3 models were: ordinary least square (OLS) regression model, spatial lag model (SLM), and spatial error model (SEM). OLS model is the most widely used regression model, which depends on some of the assumptions like, errors are normally distributed with equal variance, and they are uncorrelated. After fitting the OLS, diagnostics were carried out for checking the normality, homogeneity, and independency of residuals. The Jarque-Bera test for checking the normality of error terms, Breusch-Pagan test for checking the homogeneity of variance of the error terms and Lagrange Multiplier (LM) test and Robust LM test for checking the dependency among the error terms were used.
In the presence of spatial dependency in the data, the OLS model suffers from a misspecification problem and the results will be unreliable.20 Spatial dependency in the data can be taken into account while modeling by using spatial regression models. Spatial lag models (SLM) account for spatial correlation (dependence) in the dependent variable.22 Spatial error models (SEM) account for spatial dependence in the error term.22 Fitted models were compared using the R2 and Akaike information criterion (AIC) where model with highest R2 and lowest AIC value was considered as the most suitable model. All the 3 models OLS, SLM, and SEM were fitted in GeoDa 1.18.0 software. Mathematical structure and description of all the models used in this study along with the source of shape file used in the study are given in Supplementary File 2.
Results
Spatial Distribution and Change in the Prevalence of Childhood Stunting Between 2015-16 and 2019-21 in Districts of India
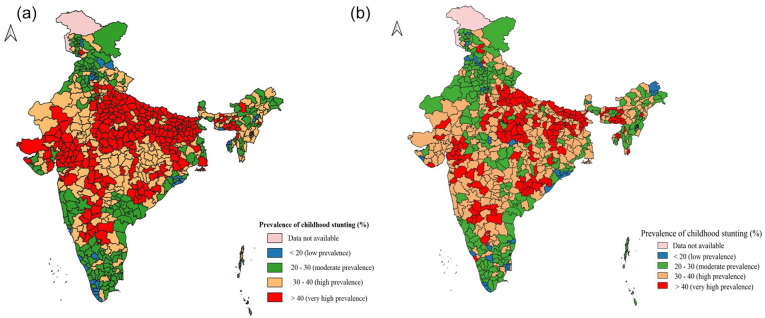
Complete list of districts that are considered in the present study along with their corresponding change in the % childhood stunting between NFHS-4 and NFHS-5 is given in the Supplemental file 3. Prevalence maps of childhood stunting across the districts of India for the 2 time periods are given in Figure 1. During 2015-16, childhood stunting varied from 12.4% in Ernakulum district of Kerala to 65.1% in Bahraich district of Uttar Pradesh. Whereas in 2019-21, childhood stunting varied from 13.2% in Jagatsinghpur district of Odisha to 60.6% in Pashchimi Singhbhum district of Jharkhand. According to the comparative analysis of childhood stunting from 2 rounds of NFHS, there were total of 278 districts that had the % childhood stunting greater than national average (ie, 38.4%) in 2015-16 however; in 2019-21 there are 283 districts that exceed the national average of 35.5%. Results from change detection study shows that, there are 231 districts that showed the increasing trend in the childhood stunting between 2015-16 and 2019-21. Among these districts, Kowhai district of Tripura and Kozhikode district of Kerala showed the highest increase in childhood stunting (27.5% and 25.4% respectively) in the last 5 years. On the other hand, 411 districts out of 692 showed decreasing trend in the childhood stunting. Highest decrease was observed in Bhopal and Tikamgarh districts of Madhya Pradesh (27.2% and 22.2% decrease respectively). There are 50 districts which had no significant change the childhood stunting. List of districts corresponding to each state that showed increasing, decreasing or no trend has been given in the Supplemental File 4.
Figure 1.
District level prevalence of childhood stunting in India during (a) 2015-16 (NFHS-4) and (b) 2019-21 (NFHS-5).
Further, Moran-I statistics was calculated which gives the strength of geospatial clustering of Indian districts relative to childhood stunting. The value of Moran’s-I was 0.652 (P-value < .001) for the period 2015-16 whereas for 2019-21, it was 0.520 (P-value < .001). The high value of Moran’s I depicted the close clustering of the districts with similar prevalence of childhood stunting.
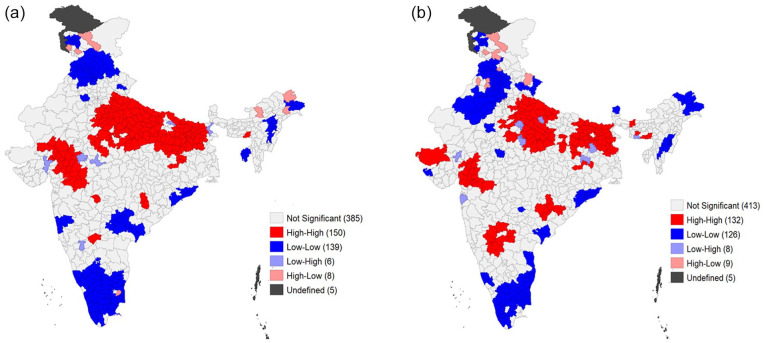
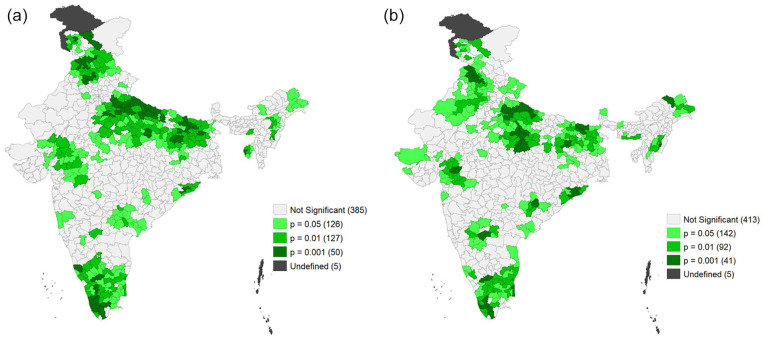
Once the presence of clustering is confirmed, univariate LISA cluster and significance maps (Figures 2 and 3) were used to identify the significant clusters of childhood stunting for both the periods. Comparing the 2 cluster maps it was evident that most of the high-high clusters consists of districts of Uttar Pradesh, Bihar, Jharkhand, Madhya Pradesh, and Gujarat during 2015-16 and 2019-21. However, additional hotspots were found in the districts of Karnataka and Chhattisgarh during 2019-21. Low-low clusters were from the district of Tamil Nadu, Kerala, Punjab, and Haryana during both periods. Addition to these, during 2015-16 few of the cold spots were also from Himachal Pradesh and Telangana whereas in 2019-21 excluding few of these cold spots, new cold spots came from Rajasthan.
Figure 2.
Cluster map for prevalence of childhood stunting across the districts of India during (a) 2015-16 (NFHS-4) and (b) 2019-21 (NFHS-5).
Figure 3.
Cluster map for prevalence of childhood stunting across the districts of India during (a) 2015-16 (NFHS-4) and (b) 2019-21 (NFHS-5).
Descriptive measures (such as mean, SD, minimum, and maximum) for predictor variables considered in the study are provided in Table 1. Results from descriptive analysis revealed that, mean 93.87% of households had access to improved drinking water sources ranging from 41.2% in Hailakandi of Assam to 100% in 33 districts of India. Average percentage of households which use an improved sanitation facility was 71.77 with the lowest percentage at Purulia of West Bengal (29.2%) to Malappuram of Kerala (99.9%). Percentage of households using clean fuel for cooking ranged from 8.6% in West Khasi Hills of Meghalaya to 99.7% in North-East Delhi with a mean of 54.3%. The Women with 10 or more years of schooling accounted for 40.44%, with the minimum in Pakur (13.6%, Jharkhand) and the maximum in Mahe (88.2%, Pondicherry). Average of closely spaced births (3 or more births in the last 5 years) was 2.07% with highest closely spaced births were observed in Patna district of Bihar and West Khasi Hills of Meghalaya (8%) and there were 64 districts out of 692 where there were no closely spaced births. Women who were pregnant at the teenage (15-19 years) ranged from 0% to 27.3% (Koch Bihar, West Bengal), with a mean of 6.14%. On an average 17.97% of women aged 15 to 49 had below normal BMI with the lowest proportion in Tawang district of Arunachal Pradesh (1.2%) and highest percentage of low BMI women in Bijapur district of Chhattisgarh (43.6%). Average of 60.5% of women who were pregnant had at least 4 antenatal care visits with the lowest in Tuensang (4.4%, Nagaland) and highest in Theni (98.7%, Tamil Nadu). Mothers who consumed IFA tablets during their pregnancy ranged from 1.6% (in Kiphire district of Nagaland) to 95% (Tirupur district of Tamil Nadu) with average of 46.3%. Similarly on an average 78.81% of mothers and 79.12% of children had the post-natal care from health professionals with mother’s post-natal care ranging from 7.1% in Raichur district of Karnataka to 99.5% in south Goa and Child postnatal care ranging from 22.4% in Mon district of Nagaland to 99.6% in Navsari district of Gujrat. Average of 6.61% and 2.5% of children were having diarrhea and Acute respiratory infection (ARI) in the 2 weeks preceding the survey respectively. Highest prevalence of diarrhea (39.3%) was found in Supaul district of Bihar and ARI was highest (11.2%) in Gonda district of Uttar Pradesh. Nearly 65.76% of the total children were anemic (having hemoglobin <11.0 g/dl) with lowest proportion (7.55%) of anemic children in Jorhat district of Assam and Highest (95.5%) in Leh district of Ladakh. Nearly 95% of households were using iodized salt for cooking with spatially varying from 47.9% to 100%. On an average 72.44% of children received vitamin A supplement with the lowest proportion in Tuensang (27.5%, Nagaland) and highest percentage (98.1%) in Mysore district of Karnataka. Similarly, children who were breastfed within 1 hour of birth ranged from 7.8% (Bhadohi, UP) to 88.5% (West Jaintia Hills, Meghalaya), with a mean of 44.64%.
Table 2 gives the correlation coefficient value and its significance for each predictor variable with the outcome variable. Bivariate analysis indicated that out of 17 predictor variables considered in the study, 15 variables had the significant association with the outcome variable and 2 variables (DW and CVA) had no significant association with the childhood stunting. Those variables that have positive association with the childhood stunting can be called as potential risk factors and those having negative association with childhood stunting can be referred as protective factors. Highest positive correlation of childhood stunting was found with BMI and TMB and highest negative correlation was found with WTL.
Table 2.
Grouping of the Predictor Variables Based on the Nature of Their Relationship With the Childhood Stunting.
| Group 1: Variables having “−ve”
association with stunting (Protective factors) |
Group 2: Variables having “+ve”
association with stunting (Risk factors) |
||
|---|---|---|---|
| Variable | Correlation coefficient (r) | Variable | Correlation coefficient (r) |
| SAN | −0.482** | TMB | .508** |
| CF | −0.420** | MTP | .233** |
| WTL | −0.536** | BMI | .544** |
| MAC | −0.369** | CD | .228** |
| MIFA | −0.383** | CARI | .140** |
| MPC | −0.361** | CA | .311** |
| CPC | −0.339** | Variables with No significant Association | |
| IS | −0.259** | DW (r = −.03) | |
| EIBF | −0.282** | CVA (r = −.06) | |
Protective Factors of Childhood Stunting
To identify the significant protective factors (Table 2) of childhood stunting, OLS regression model was fitted between stunting and 9 protective factors, and the model diagnostics were carried out. The Jarque-Bera test indicated that errors are following the normal distribution (P-value > .05) whereas Breusche-Pagan test indicated the presence of heteroscedasticity in the error terms (P-value < .05). Further, LM test and Robust LM test were also significant (P-value < .001) indicating the presence of spatial dependency. Hence, spatial regression models (SLM & SEM) were fitted to identify the potential protective factors of childhood stunting. Results from all the 3 models (OLS, SLM, and SEM) are presented in Table 3. R2 and AIC vales were used to identify the better fitting model for the spatial data. Among the 3 models, highest R2 (54%) and lowest AIC (4456.98) was reported for SEM. So, SEM was used for identifying the protective factors. Among the 9 variables included, only 5 (SAN, CF, WTL, MPC, and IS) were significantly associated with the prevalence of childhood stunting. Among the 5 significant variables, larger effect on childhood stunting was from WTL (β = −.14, SE = 0.03) and IS (β = −.11, SE = 0.05) indicating, increasing/improving these factors by 1% going to significantly decrease the childhood stunting by 0.14% and 0.11%, respectively.
Table 3.
Estimates of the Regression Coefficients of Determinants of Childhood Stunting From Ordinary Least Square (OLS), Spatial Lag Model (SLM) and Spatial Error Model (SEM).
| OLS | SLM | SEM | |
|---|---|---|---|
| Protective factors | |||
| SAN | −0.12(0.02)** | −0.08(0.02)** | −0.09(0.020)** |
| CF | −0.02(0.01) | −0.02(0.01) | 0.04(0.02)* |
| WTL | −0.16(0.02)** | −0.10(0.02)** | −0.14(0.03)** |
| MAC | 0.00(0.02) | 0.02(0.02) | 0.04(0.02) |
| MIFA | −0.00(0.02) | 0.00(0.02) | −0.02(0.02) |
| MPC | −0.08(0.04)* | −0.07(0.03)* | −0.08(0.03)* |
| CPC | −0.03(0.04) | −0.02(0.04) | −0.03(0.04) |
| IS | −0.24(0.05) ** | −0.15(0.04)** | −0.11(0.05)* |
| EIBF | −0.07(0.02)** | −0.04(0.02)* | −0.03(0.02) |
| AIC | 4578.08 | 4468.53 | 4456.98 |
| R2 | 0.40 | 0.51 | 0.54 |
| Risk factors | |||
| TMB | 1.89(0.16)** | 1.36(0.16)** | 1.58(0.18)** |
| MTP | 0.22(0.05)** | 0.14(0.05)** | 0.13(0.06)* |
| CD | –0.07(0.07) | –0.08(0.06) | –0.06(0.07) |
| CA | 0.07(0.13)** | 0.03(0.02) | 0.07(0.02)** |
| CARI | 0.30(0.13)* | 0.26(0.12 * | 0.26(0.12)* |
| BMI | 0.40(0.04)** | 0.27(0.04)** | 0.40(0.04)** |
| AIC | 4536.21 | 4433.97 | 4416.62 |
| R2 | 0.44 | 0.53 | 0.55 |
Indicates significance at %% level of confidence. **Indicates significance at 1% level of confidence.
Risk Factors of Childhood Stunting
Like identification of protective factors which have potential to decrease the childhood stunting by increasing their coverage, we tried to identify the risk factors which are responsible for the high prevalence of childhood stunting. First, OLS model was fit for outcome variable and probable risk factors considered in the study. Diagnostic tests revealed the normality and homogeneity of errors (Jarque-Bera test & Breusche-Pagan test P-value > .05). But LM and Robust LM test were significant indicating the spatial dependency among the errors. Hence, spatial regressions (SLM and SEM) were used to identify the risk factors of childhood stunting. The results of regression analysis (OLS, SLM, and SEM) are provided in the Table 3. By looking at the R2 and AIC of each model it was evident that SEM was better fitting the spatial data compared to other 2 models. From the results of SEM, 5 factors out of 6 (TMB, MTP, CA, CARI, and BMI) were significant risk factors indicating that increase in these factors will significantly increase the prevalence of childhood stunting. Among the 5 risk factors highest effect is from TMB (β = 1.58, SE = 0.18) and next it is BMI (β = .40, SE = 0.04) and CARI (β = .26, SE = 0.04). This confirms that for every 1% decrease in these factors going to minimize the stunting prevalence by 1.58%, 0.40%, and 0.26% respectively.
Discussion
Study used comparative and spatial analysis to understand the change and distribution of prevalence of childhood stunting between 2015-16 and 2019-21 and to re-examine the association between the factors associated with childhood stunting. Study shows that, though childhood stunting has reduced in the last 5 years, the rate of reduction is slow compared to that of the period between 2005-2006and 2015-16 & along with that there is huge disparity in the rate of change and prevalence of childhood stunting at the district level. 23,24 In the last 5 years, childhood stunting has increased in more than one-third of the Indian districts and in two-third of the districts its prevalence in high. Hotspot analysis results indicated the formation of new clusters of childhood stunting apart from those present during 2015-16. This unexpected trend in the childhood stunting even after implementation of several programs and policies indicate the inefficiency of the interventions to reach the targeted group. Other reasons could be poor implementation, failing to monitor the implemented programs and interventions, lack of funds and resources for the program implementation, poor acceptance of the interventions by the target group or it may be due to the diversity existing with respect to demography and socio-cultural practices among Indian districts.14,25,26 Though preset study doesn’t involve poverty as one of the predictor variables, considering the previous study results conducted in India and in the similar set ups and the current facts released on poverty among Indian states, we can say, high prevalence of stunting can also be associated to high prevalence of poverty in the Indian states.10,27-30 Factors having the significant association with childhood stunting were identified using spatial regression method. Like the previous studies, in the present study, household variables like, using iodized salt and clean fuel for cooking and improved sanitation facility found to have significant potential to decrease the childhood stunting.6-8 This is likely because clean environment and good food intake will minimize the chance of getting infection and increase the resistance in the body which in turn promote a good growth and development in children.11 Among the women related characteristics, 10 plus schooling and postnatal care of a mother have a significant potential to decrease the childhood stunting.1,10-12,28 This is because, women being the primary care takers, as their education increases awareness about the malnutrition and its impact and importance of good food and healthy practices also increases. Thereby, help in reducing the childhood stunting. As the we know postnatal care of both child and mother is crucial as it is this period in which most of the maternal and child death occur. As the availability of post-natal care increase, chances of disabilities or deaths will decrease and increases the health of both newborn and mother.31,32 Factors like access to improved drinking water, mother’s antenatal care and taking iron supplements during pregnancy did not show any significant association with the childhood stunting unlike in previous studies.6,11,13 Since the reasons are not known, it is better to take up the study to check for the association with individual level data. Similar to previous studies, even in our study, proportion of women with low BMI, closely spaced births, teenage pregnancy were the major risk factors for childhood stunting.1,10-13 This is because, most of the teen mothers will be underweight and devoid of the health services (which is also may happen in case of closely spaced births) which leads to the adverse health consequences and complications (ex: child and/or maternal mortality, preterm birth) there by increasing the risk of child being stunted.30,33 Among the child health related factors, anemia and acute respiratory infections found to have significant association with stunting. This is likely that, as child starts getting infections and early disease, linear growth of the child reduces which results in stunting.
This study has some policy suggestions. First, since POSHAN Abhiyan 2.0 has been recently announced, district with high prevalence and those showed increase or no change in the past 5 years in the prevalence of childhood stunting has to be prioritized in allocating the funds and resources. Huge difference in the % change between the districts indicates the extent of additional efforts needed to reduce the childhood stunting. Considering the public opinion on policies & programs and planning the interventions based on that will help in increasing acceptance and success rate of the policies & programs. Involving the community representatives and village level health workers (ex. ASHA workers) for creating awareness and implementation of programs may enhance the outcome. As it was evident from the study, childhood stunting is influenced by multiple factors (household, socio-economic, women and child related factors). Hence, formulating and implementing the multisectoral approaches considering the geographical diversity of India at granular level seems to be effective to curb the childhood stunting.
Conclusion
Being the first in the line of studies to understand the district level change in the prevalence of childhood stunting in the last 5 years (2015-16 to 2019-21), study helped in identifying the high priority districts and helps in formulating policies & program implementation. Study facilitated the identification of factors having significant association with current prevalence of childhood stunting and this will help in planning the evidence-based interventions. Despite the benefits, study has a limitation. Historical antecedents like poverty, inequality and food insecurity which are known to influence the prevalence of childhood stunting are not included in the study. Even with that, the study will help the researchers and policy makers for carrying out the district specific studies and planning and execution of policies to effectively control childhood stunting in India.
Supplemental Material
Supplemental material, sj-docx-1-inq-10.1177_00469580221127122 for Understanding the Change in the Prevalence and Factors Influencing the Childhood Stunting Using District-Level Data from NFHS-4 and NFHS-5 in India by B.S. Pooja and Vasudeva Guddattu in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-docx-2-inq-10.1177_00469580221127122 for Understanding the Change in the Prevalence and Factors Influencing the Childhood Stunting Using District-Level Data from NFHS-4 and NFHS-5 in India by B.S. Pooja and Vasudeva Guddattu in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-docx-3-inq-10.1177_00469580221127122 for Understanding the Change in the Prevalence and Factors Influencing the Childhood Stunting Using District-Level Data from NFHS-4 and NFHS-5 in India by B.S. Pooja and Vasudeva Guddattu in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-docx-4-inq-10.1177_00469580221127122 for Understanding the Change in the Prevalence and Factors Influencing the Childhood Stunting Using District-Level Data from NFHS-4 and NFHS-5 in India by B.S. Pooja and Vasudeva Guddattu in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
We are grateful to the three anonymous reviewers for their comments, which contributed to the overall improvement in the manuscript.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Data used for this study are obtained from the National Family Health Survey -5 (2019-2021). Data are freely available in public domain for use (http://rchiips.org/nfhs/districtfactsheet_NFHS-5.shtml). No separate ethics statement and consent for publication was required for this study as the NFHS followed ethical clearance guidelines and norms
ORCID iD: Pooja B. S.  https://orcid.org/0000-0002-3516-3112
https://orcid.org/0000-0002-3516-3112
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Biswas M. Identifying geographical heterogeneity in associations between under-five child nutritional status and its correlates across Indian districts. Spat Demogr. 2022;10:143-187. doi: 10.1007/s40980-022-00104-2 [DOI] [Google Scholar]
- 2. World Health Organization. Updates on the Management of Severe Acute Malnutrition in Infants and Children. World Health Organization; 2013:6-54. [PubMed] [Google Scholar]
- 3. World Health Organization, United Nations Children’s Fund.WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: Joint Statement. World Health Organization; 2019. [PubMed] [Google Scholar]
- 4. Oot L, Sethuraman K, Ross J, Sommerfelt AE. The effect of chronic malnutrition (stunting) on learning ability, a measure of human capital: a model in PROFILES for country-level advocacy. Washington, DC, FHI; 2016. 360. [Google Scholar]
- 5. UNICEF. World Declaration on the Survival, Protection and Development of Children and Plan of Action for implementing the World Declaration on the Survival, Protection and Development of Children in the 1990s. 1990. [DOI] [PubMed] [Google Scholar]
- 6. Hemalatha R, Pandey A, Kinyoki D, Ramji S, Lodha R, Kumar GA, et al. Mapping of variations in child stunting, wasting and underweight within the states of India: the global burden of disease study 2000-2017. EClinicalMedicine. 2020;22:100317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kapur K, Suri S. Towards a Malnutrition-Free India: Best Practices and Innovations From POSHAN Abhiyaan. ORF Special Report; 2020. [Google Scholar]
- 8. Paul VK, Singh A, Palit S. POSHAN Abhiyaan: Making nutrition a Jan Andolan. Proc Indian Natn Sci Acad. 2018;84(4):835-841. [Google Scholar]
- 9. World Health Organization. Levels and Trends in Child Malnutrition: UNICEF/WHO/The World Bank Group Joint Child Malnutrition Estimates: Key Findings of the 2021 Edition. World Health Organization; 2021. [Google Scholar]
- 10. Khan J, Mohanty SK. Spatial heterogeneity and correlates of child malnutrition in districts of India. BMC Public Health. 2018;18(1):1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Menon P, Headey D, Avula R, Nguyen PH. Understanding the geographical burden of stunting in India: a regression-decomposition analysis of district-level data from 2015–16. Matern Child Nutr. 2018;14(4):e12620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Striessnig E, Bora JK. Under-five child growth and nutrition status: spatial clustering of Indian districts. Spat Demogr. 2020;8(1):63-84. [Google Scholar]
- 13. Gupta AK, Santhya KG. Proximal and contextual correlates of childhood stunting in India: a geo-spatial analysis. PLoS One. 2020;15(8):e0237661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rode S. Child malnutrition and low access to health care facilities in Mumbai metropolitan region. Double Blind Peer Review Int Res J. 2015;15(2):49-59. [Google Scholar]
- 15. World Health Organisation. Childhood Stunting: Contexts, Causes and Consequences; A technical document; 2016, April 7. [Google Scholar]
- 16. Raj SM, Ekanayake R, Crowley K, Bhat M, Kadandale J, Pingali PL. Risk factors in childhood stunting in Karnataka, India, vary by geography. Curr Sci. 2021;121(4):502-510. [Google Scholar]
- 17. International Institute for Population Sciences. National Family Health Survey (NFHS-5) 2019-21. International Institute for Population Sciences; 2021. [Google Scholar]
- 18. Das P, Roy R, Das T, Roy TB. Prevalence and change detection of child growth failure phenomena among under-5 children: a comparative scrutiny from NFHS-4 and NFHS-5 in West Bengal, India. Clin Epidemiol Glob Health. 2021;12:100857. [Google Scholar]
- 19. Srivastava S, Chandra H, Singh SK, Upadhyay AK. Mapping changes in district level prevalence of childhood stunting in India 1998-2016: an application of small area estimation techniques. SSM Popul Health. 2021;14:100748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pfeiffer DU, Robinson TP, Stevenson M, Stevens KB, Rogers DJ, Clements AC. Spatial Analysis in Epidemiology. Oxford university press; 2008. [Google Scholar]
- 21. Anselin L. Local indicators of spatial association-LISA. Geogr Anal. 1995;27(2):93-115. [Google Scholar]
- 22. Fischer MM, Wang J. Spatial Data Analysis: Models, Methods and Techniques. Springer Science & Business Media; 2011. [Google Scholar]
- 23. National Family Health Survey. India Fact Sheet. 2020. Accessed May 6, 2022. http://rchiips.org/nfhs/NFHS-5_FCTS/India.pdf
- 24. Singh A. Childhood malnutrition in India. In: Bhattacharya Sujit K. (ed.) Perspective of Recent Advances in Acute Diarrhoea. IntechOpen; 2020; 9-34. [Google Scholar]
- 25. Dinachandra Singh K, Alagarajan M, Ladusingh L. What explains child malnutrition of indigenous people of Northeast India? PLoS One. 2015;10(6):e0130567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Karigi LN, Mutuli LA, Bukhala P. Socio-cultural practices and beliefs influencing infant and young child feeding in Lubao sub-location Kakamega County. J Nutr Health Food Eng. 2016;5(1):00160. [Google Scholar]
- 27. Esha ROY. NFHS data says Chandigarh has highest number of rich people in India: Find out where y our state stands. The Indian Express. May 12, 2022. [Google Scholar]
- 28. Avula R, Nguyen PH, Tran LM, et al. Reducing childhood stunting in India: insights from four subnational success cases. Food Secur. 2022;14:1085-1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Siddiqui F, Salam RA, Lassi ZS, Das JK. The intertwined relationship between malnutrition and poverty. Public Health Front. 2020;8:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rahman MA, Rahman MS, Shakur SM, et al. Risk factors of chronic childhood malnutrition: an analysis of the Bangladesh demographic and health survey 2014 data. J Public Health. 2020;30:309-321. [Google Scholar]
- 31. World Health Organization. WHO recommendations on maternal and newborn care for a positive postnatal experience. 2022. [PubMed] [Google Scholar]
- 32. Wudineh KG, Nigusie AA, Gesese SS, Tesfu AA, Beyene FY. Postnatal care service utilization and associated factors among women who gave birth in Debretabour town, North West Ethiopia: a community- based cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Dhingra S, Pingali PL. Effects of short birth spacing on birth-order differences in child stunting: Evidence from India. Proc Natl Acad Sci U S A. 2021;118(8):e2017834118. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-inq-10.1177_00469580221127122 for Understanding the Change in the Prevalence and Factors Influencing the Childhood Stunting Using District-Level Data from NFHS-4 and NFHS-5 in India by B.S. Pooja and Vasudeva Guddattu in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-docx-2-inq-10.1177_00469580221127122 for Understanding the Change in the Prevalence and Factors Influencing the Childhood Stunting Using District-Level Data from NFHS-4 and NFHS-5 in India by B.S. Pooja and Vasudeva Guddattu in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-docx-3-inq-10.1177_00469580221127122 for Understanding the Change in the Prevalence and Factors Influencing the Childhood Stunting Using District-Level Data from NFHS-4 and NFHS-5 in India by B.S. Pooja and Vasudeva Guddattu in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Supplemental material, sj-docx-4-inq-10.1177_00469580221127122 for Understanding the Change in the Prevalence and Factors Influencing the Childhood Stunting Using District-Level Data from NFHS-4 and NFHS-5 in India by B.S. Pooja and Vasudeva Guddattu in INQUIRY: The Journal of Health Care Organization, Provision, and Financing