Abstract
Mental health disorders and suicidality are rising among adolescents and young adults (A-YA) while rates of treatment engagement remain notoriously low. Emerging research supports the potential of music-based interventions to improve mental health, but their efficacy remains unclear for A-YA. This systematic review evaluates the evidence on music-based psychosocial interventions to improve engagement in treatment and/or mental health outcomes among A-YA. This review was prospectively registered with PROSPERO and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Twenty-six studies were extracted. There was heterogeneity of designs, populations, measures, and outcomes. A typology of music-based interventions emerged, which is characterized by combinations of three broad categories: 1) Somatosensory, 2) Social-Emotional, and 3) Cognitive-Reflective. Most interventions are Socio-Cognitive and Holistically Integrated (combines all three) followed by Socio-Somatic. All interventions involved Social-Emotional processes. Results indicate that most studies report significant effects for mental health outcomes related to social and emotional improvements and reductions of internalizing symptoms for adolescents. Few studies targeted young adults and effects on engagement were rarely measured. There is a need for more studies that use rigorous methods. This review illuminated a need for interventions that are developmentally and culturally tailored to subgroups. Finally, the field is ripe from more studies that apply experimental therapeutics to conceptualize, operationalize, and test mechanisms of change to improve the understanding of how and for whom music-based interventions work. Recommendations for embedding these innovative strategies into research and practice for A-YA are discussed.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10560-022-00893-x.
Keywords: Adolescents, Young adults, Music, Mental health, Treatment engagement, Mechanisms of change
Recent reports from the United States (US) Surgeon General’s Advisory (2021) and the National Research Council (2015) have issued stark warnings on the unprecedented rise of mental health conditions and suicidality among adolescents and young adults (A-YA) along with the need to develop culturally and developmentally responsive interventions. Despite this growing problem, many A-YA do not access mental health services, and those that do access care often disengage prematurely and experience challenges with continuity (Substance Abuse and Mental Health Services Administration [SAMHSA], 2020). Rates of disengagement are higher among minoritized groups (Moore, 2018) many of whom are involved with public systems (Alvarez et al., 2022; NeMoyer et al., 2020) and experience environmental stressors. These concerns are multi-faceted and so must be our strategies to address them. One innovative and youth-centered strategy to address these concerns is the use of music-based interventions. The National Institutes of Health (NIH) in partnership with the Kennedy Center for the Performing Arts recently launched the Sound Health Initiative that awarded $20 million dollars to expand the evidence-base for music-based interventions to address mental health disorders (Collins & Fleming, 2017; NIH, 2018). Building on the promise of such interventions, this systematic review evaluates the evidence-base for psychosocial interventions that use music as an innovative strategy to improve treatment engagement and/or mental health outcomes for A-YA. Results can inform the field on how to use these strategies while also informing practice, research, and policy.
Adolescent and Young Adult Mental Health
The World Health Organization (WHO) (2021) estimates that depression is a leading cause of disability and suicide is the second leading cause of death among A-YA between the ages of 15–29 years worldwide. Recent estimates indicate that mental health conditions and suicidality among this population are rising at alarming rates, particularly in the era of COVID-19, which has enhanced distancing, isolation, and exposure to family stress (Czeisler et al., 2020; Miron et al., 2019; Twenge et al., 2019). Moreover, the developmental transition to adulthood is a vulnerable period during which mental health conditions can emerge and peak in intensity; approximately half of all mental disorders develop by the age of 14 and three-fourths by age 24 (Kessler et al., 2005; McGrath et al., 2016). In the US, the prevalence rate for any mental health disorder (e.g., anxiety, depression, stress) among adolescents aged 13 to 17 in the past year was 40.3% and 8.0% for serious emotional disturbance (e.g., functional impairment, aggression, self-injurious behaviors) (Kessler, Avenevoli, Costello, Green, et al., 2012). These rates and poor mental health continue to rise since the onset of COVID-19, particularly among A-YA (e.g., Czeisler et al., 2020; Jones et al., 2022; Ma et al., 2021). The prevalence rates for any mental health disorder among young adults aged 18 to 25 in the past year, and for a serious mental illness (SMI), are respectively 29.4% and 8.6%, which are high compared to rates of older age cohorts (SAMSHA, 2020). These rates are higher among girls, those who identify as LGBTQ + , and A-YA of color who face elevated risks of stressors including victimization, interpersonal violence, racism, incarceration, complex trauma, and poverty (Alegría et al., 2015; Cole et al., 2020; Comas-Diaz et al., 2019; Salerno et al., 2020; Williams et al., 2003).
Complex trauma, prolonged stress, and other adversities can increase the risk of a variety of undesirable outcomes including poor academic achievement, mental health disorders, suicidality, and substance use across the lifespan and affect disproportionally socially and economically marginalized A-YA (Alvarez et al., 2022; Chartier et al., 2010; Edwards et al., 2003; Polanco-Roman et al., 2016). For example, Copeland and colleagues (2018) found that cumulative childhood trauma was associated with higher rates of later onset psychiatric disorders during the transition to adulthood and poorer functional outcomes (e.g., unemployment, social isolation). Similarly, scientific advances in neurobiology have demonstrated how complex trauma, particularly during developmentally vulnerable stages (Ganzel & Morris, 2011), can have lasting effects on the brain, mind, and body along with one’s capacity for resilience (Boyce & Ellis, 2005; Ford & Courtois, 2020). These advances provide more context and nuance for understanding how complex trauma and prolonged stress can have lasting effects on the developing brain, mind, and body.
Treatment Engagement and Service Use Trends
Despite high rates of mental health disorders and suicidality, the developmental transition from adolescence to young adulthood is marked by an increase in vulnerability for treatment disengagement, fragmented patterns of service use, and premature termination (Copeland et al., 2015; Munson et al., 2012). Among youth transitioning from pediatric to adult service systems, rates of service use decline (McMillen & Raghavan, 2009; Paul et al., 2013). One reason for disengagement is that the developmental transition is characterized by increased autonomy (Erikson, 1968), including more autonomy on how one identifies with their mental health diagnosis and how one makes decisions about how to manage one’s mental health (Munson et al., 2018; Narendorf et al., 2015). Recent estimates indicate that only 39% of young adults with any mental disorder received mental health services in the past year; a rate lower than all older age cohorts (SAMHSA, 2020). Among adolescents aged 12 to 17 with major depression, only 43% received mental health services in the past year (SAMHSA, 2020), consistent with rates for any mental health condition (Olfson et al., 2015). Rates of disengagement are higher and more fragmented among minoritized A-YA (Moore, 2018) involved with public systems (Costello et al., 2014; Fontanella et al., 2020). Furthermore, untreated mental health conditions are costly and forgoing treatment can lead to negative psychosocial outcomes as symptoms often persist into adulthood (Kim-Cohen et al., 2003; Patel et al., 2007).
Treatment engagement is a multidimensional construct that consists of behavioral (e.g., attendance, premature termination) and attitudinal (e.g., involvement, buy-in, alliance) components (Kim et al., 2012; Lakind et al., 2021). No matter how effective evidence-based interventions (EBI) may be for improving mental health, they are of minimal value if A-YA choose not to use these services. Research attributes disengagement to a combination of perceptual (e.g., stigma, mistrust of providers, negative beliefs about treatment) and structural (e.g., cost, access, quality) factors (Gulliver et al., 2010; Munson et al., 2012; Narendorf et al., 2018; Scott et al., 2011). Similarly, the lack of EBIs that use culturally and developmentally responsive strategies contributes to the persistence of this problem (Kirmayer, 2012). This highlights the question of cultural compatibility of EBIs that are typically developed using study populations that lack diversity and amplifies the need for adaptations for distinct subgroups (see Cabassa & Baumann, 2013; McCoy & McKay, 2006).
Music, Mental Health, and Engagement
The WHO recently synthesized a growing body of evidence on how interventions that include music and expressive arts strategies can support engagement, prevention, and treatment of health and mental health conditions (Fancourt & Finn, 2019). This report highlights the capacity of music and expressive arts to stimulate aesthetic engagement, imagination, sensory activation, evocation of emotion, and cognitive attention (Fancourt & Finn, 2019). Research suggests that interventions that incorporate the use of music and rhythm can promote integration, emotion regulation, attunement, and reduce levels of stress, anxiety, and depression (Chanda & Levitin, 2013; Lin et al., 2011; Yinger & Gooding, 2014). Dynamic and multisensory approaches are important, particularly for those affected by traumatic stress, as words cannot always integrate the disorganized emotions and sensations that affect the brain, mind, and body (van der Kolk, 2015). Similarly, leading trauma experts propose that patterned and repetitive rhythmic activities (Perry, 2009) can bypass higher order cognitive processes and engage more primitive regions of the brain (Porges, 2011). While there is a growing body of research that supports the promise of music-based interventions, few studies have systematically and empirically evaluated interventions that operate on these assumptions (McFerran et al., 2020), particularly for A-YA.
There are a variety of approaches and disciplines (e.g., music therapy, expressive arts therapy, hip hop therapy) that use music as a tool to promote mental health and well-being (e.g., Bruscia, 1998; Malchiodi, 2020; McFerran, 2019). Hip Hop Therapy (HHT) and Hip Hop-based strategies are an example of an approach to mental health treatment that integrates Hip-Hop culture into the clinical process (Tyson, 2004; Tyson et al., 2016), and that is rooted in social justice and health equity (Travis, 2016, pp. 115–122). Research suggests that the integration of music listening, discussing song lyrics, and expressive activities can offer a more accessible, appealing, and intuitive way for A-YA to address their mental health (Cole et al., 2018; Munson & Lox, 2012; Thomas et al., 2020) ranging from daily self-care to formal treatment contexts (Saarikallio et al., 2015). For example, the use of Hip Hop-based strategies has gained traction over the past two decades, particularly for marginalized youth, to promote empowerment, resilience, and well-being (e.g., Hadley & Yancy, 2012; Robinson et al., 2018; Travis, 2016, 2019; Levy et al., 2017). Likewise, a study by Kresovich and colleagues (2021) found that mental health references in popular rap music have significantly increased between 1998 to 2018, which may have implications for help-seeking. Furthermore, embedding music-based strategies into social work services may offer one way to reimagine practice and enhance the therapeutic alliance between A-YA and their providers, ultimately leading to better engagement and treatment outcomes.
Although music can support well-being, some research also suggests that music can be associated with negative outcomes if used in unhealthy or risky ways (Saarikallio et al., 2015; Travis, 2013). For example, unhealthy uses of music can intensify or increase the risk of depression, rumination, social isolation, and affect dysregulation (Garrido et al., 2017; Silverman, 2020; Thomson et al., 2014). An emerging body of work and interventions has focused specifically on promoting healthy and empowering uses of music in ways that reduce elements of risk and unhealthy uses (see Travis et al., 2019a; Hense et al., 2018 for examples). This line of research suggests that beyond “risky content” and subjectively risky ways of interpreting and interacting with content, the intentionality of how practitioners use music to engage with youth is most critical (Saarikallio et al., 2015; Travis, 2016). It is important for practitioners to have the clinical skills and training to work with risky and potentially unhealthy content in a manner that facilitates positive therapeutic outcomes. Furthermore, these considerations surrounding the uses of music are important to help inform, educate, and train clinicians to be reflexively critical about how to use these strategies in direct practice.
Previous Systematic Reviews and Meta-Analyses
Previous systematic reviews and meta-analyses on music-based interventions for mental health have focused mostly on capturing outcomes among children and younger adolescents or adults. For example, several reviews focused on adults with depression (Chan et al., 2011; Maratos et al., 2008; Tang et al., 2020; Zhao et al., 2016) while others have examined specific subgroups including those with serious mental illness (Carr et al., 2013; Gold et al., 2009), general mental health conditions (Lee & Thyer, 2013), health-related quality of life (McCrary et al., 2022), and justice-involved youth (Daykin et al., 2013). Systematic reviews and meta-analyses focused on children and adolescents experiencing mental health conditions have reported medium effect sizes (Belski et al., 2021; Geipel et al., 2018; Gold et al., 2004). For example, Geipel and colleagues’ (2018) meta-analysis focused on internalizing disorders and included five studies; the results indicated significant effects in favor of music-based interventions with a medium effect size. Belski and colleagues (2021) focused on RCTs of interventions targeting depression and anxiety symptoms; their review of seven studies suggests symptom improvements however concerns of bias and methodological issues (e.g., lack of randomization, blinding) are noted. Taken together, these reviews contribute to our understanding of the efficacy of music-based interventions for children and adolescents, predominantly those with internalizing symptoms. Young adults have not been included in these reviews and the narrow inclusion criteria have constricted most reviews to less than ten studies, limiting the capacity to have a comprehensive yet systematic assessment of evidence. Similarly, while these reviews have begun to hypothesize how music-based interventions can impact outcomes, the field has not organized the literature systematically to understand the various types of approaches these interventions use for A-YA. Furthermore, less is known about the effects of music-based interventions on mediators and outcomes among A-YA with mental health needs.
Opening the “Black Box:” Potential Mechanisms of Change
Previous systematic reviews have primarily examined if music-based interventions affect outcomes while none have focused on capturing psychosocial mechanisms to explain how change occurs. Reviews that have emphasized mechanisms of change have focused largely on neurological processes (e.g., brainstem activity, neurochemical rewards, parasympathetic activity) (McCrary et al., 2022; Mrázová & Celec, 2010; Yinger & Gooding, 2014) while less is known about psychosocial mechanisms. Indeed, recent reviews have called for more systematic research to uncover mechanisms of change (Gustavson et al., 2021; Hohmann et al., 2017; McCrary et al., 2022; McFerran et al., 2020). For example, McFerran and colleagues (2020) argue that greater precision is needed in providing a theoretical rationale for why certain music-based techniques are used and how they may relate to outcomes. Gustavson and colleagues (2021) identified two studies on adults that hypothesized several psychosocial (e.g., self-expression, emotion regulation, coping skills, self-awareness, community building, visual imagery) and contextual (e.g., shared experiences, cohesion) mechanisms (Ansdell & Meehan, 2010; Maratos et al., 2008). Perkins and colleagues (2020) identified four pathways (i.e., expressing emotions, self-development, respite, social connections) between music engagement and adult well-being. There are no reviews that have focused systematically on capturing psychosocial mechanisms of change that have been empirically tested within intervention studies that are developmentally specific to A-YA.
The Present Study
This systematic review seeks to narrow these gaps by examining the evidence for music-based interventions to improve treatment engagement and mental health outcomes for A-YA. It has three objectives: (1) To summarize and discuss the characteristics and findings of studies that tested the effects of psychosocial music-based interventions to improve treatment engagement and/or mental health outcomes, including an analysis of methodological quality; (2) To identify and synthesize the theoretical frameworks, components, structure, and delivery approaches that guide these interventions; (3) To identify any potential explicit or implicit psychosocial mechanisms (i.e., mediators) targeted by these interventions to effect change in outcomes. To our knowledge, this is one of the first studies that seeks to systematically review evidence on psychosocial interventions using music for A-YA.
Methods
Eligibility Criteria
This review followed the methodological guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Page et al., 2021). The review and its protocol were prospectively registered with PROSPERO (CRD42021202644) (Rodwin et al., 2021). The inclusion criteria were developed by the first and last author. We adopted the Institute of Medicine’s (IOM) (2015) criteria for psychosocial interventions, which are defined as “interpersonal or informational activities, techniques, or strategies that target biological, behavioral, cognitive, emotional, interpersonal, social, or environmental factors with the aim of reducing symptoms of these disorders and improving functioning or well-being” (p. 5). Included studies consist of those that tested the effects of a psychosocial intervention that incorporated music as a tool to improve engagement (e.g., attendance, investment, adherence) and/or mental health (e.g., symptoms, behaviors, cognitions) outcomes. Interventions used active (e.g., music-making, songwriting) and/or receptive (e.g., music listening, lyric analysis) strategies. Rather than focusing on specific disorders (e.g., internalizing or externalizing), we adopted a broader criterion that encompasses social and emotional outcomes (e.g., emotion regulation, self-awareness, relationship skills) as the development of these competencies are linked to positive mental health (Mahoney et al., 2018). Similarly, this definition provides a more inclusive understanding of the features of mental health beyond the narrow constraints of internalizing or externalizing symptoms. Consistent with definitions of adolescents and young adults, participants were aged 13 to 26 (NRC, 2015); the mean age had to fall within this range. This review was a global investigation and was not limited to the US, as music is a worldwide artistic form of expression that transcends geographical and cultural boundaries.
Included studies are those that used single-group (no comparison group), quasi-experimental (nonequivalent comparison group), or experimental (randomization with comparison group) designs. Qualitative or descriptive investigations are not included, as the scope of this review is to examine studies testing the effects of an intervention based on quantitative outcomes data. We acknowledge that limiting “evidence” to quantitative research can be problematic and we elaborate on this in our limitations. Since an aim of this review is to explore psychosocial mechanisms, studies that focused on neuropsychological (e.g., fMRI) manipulations are excluded. Also, studies that focus specifically on autism or neurodevelopmental disorders are excluded given the distinct nature of these conditions. Consistent with the IOM’s (2015) definition of psychosocial interventions, studies that exclusively involved receptive listening in the absence of any interpersonal context were excluded. Finally, given our focus on mental health, studies that targeted substance use or co-morbid medical conditions are excluded. Studies must be published in English and dissertations are not included. There are no other restrictions on the type of articles or year of publication.
For aim three (identifying explicit and implicit mechanisms of change) we rely on the IOM’s (2015) definitions for mechanisms and mediators. Mechanisms capture “how psychosocial interventions effect change, with causal links between treatment and outcomes” (IOM, 2015, p. 27) and mediators capture “the ways in which the action of psychosocial interventions leads to a specific outcome through changes in biological, behavioral, cognitive, emotional, interpersonal, social, or environmental factors; these changes explain or mediate the outcome” (IOM, 2015, p. 32). Studies that conceptualized, operationalized, and tested mediators or mechanisms were considered “explicit.” In contrast, studies that speculated about potential mediators or mechanisms but did not operationalize, measure, or test them were considered “implicit.” We classified studies as “implicit” if they clearly articulated how their intervention may have led to change using keywords such as “mechanism,” “mediator,” “theory of change,” or “target.” We decided not to apply post-hoc abductive logic to speculate about the potential mediators or mechanisms in studies that did not clearly articulate this information as it risks misinterpretation of the aim, processes, and scope of the interventions.
Search Strategy
A wide-net search strategy was used, and database searches were conducted in PsychInfo, Social Service Abstracts, and SocINDEX. A syntax of keywords synonymous for psychosocial intervention and music were combined with keywords synonymous to mental health (see Online Resource 1 for the full search syntax). Filters were applied for age categories of adolescents and young adults when applicable. The search strategy was designed through consultation with a research librarian with expertise in psychology and social work and these databases were identified as the most conceptually relevant to our topic. After database searches were conducted, study eligibility was assessed using a systematic and standardized approach that relied upon Covidence (organizing software for systematic reviews and meta-analyses). Database searches were conducted by the first author and then yielded studies were independently evaluated at each level (i.e., title/abstract, full text, extraction) according to inclusion/exclusion criteria by the first and second authors. Regular team meetings were scheduled to reconcile any differences (i.e., inclusion or exclusion of studies) with the support of the last author. Among studies that met inclusion criteria, study characteristics and outcomes data were extracted and summarized. The first database search was conducted in May 2020 and then in November 2021 to capture any new studies that might have been missed in the first search.
Analysis of Methodological Quality
The methodological quality and characteristics of each study were assessed using an adapted version of the Methodological Quality Rating Scale (MQRS) (Miller et al., 1995; Vaughn & Howard, 2004). We selected the MQRS as the scope of included studies extend beyond RCTs and includes various designs (e.g., single-group, quasi-experimental). Other quality assessments and risk of bias instruments tend to be more suited for pure experimental studies, particularly RCTs. The MQRS assesses 13 dimensions of methodological quality such as study design, replicability, and specification of intervention components (see Online Resource 3 for the full scale). We made surface level adaptations to several of the questions to fit the context of the included studies. One dimension was added to assess the absence or presence of measures with adequate psychometric properties. We piloted the MQRS with 4 studies and discussed discrepancies and refined items. The MQRS was administered independently by the first and second authors to establish interrater agreement and discrepancies were reconciled through discussion with support of the last author.
Results
Study Characteristics and Methodological Quality
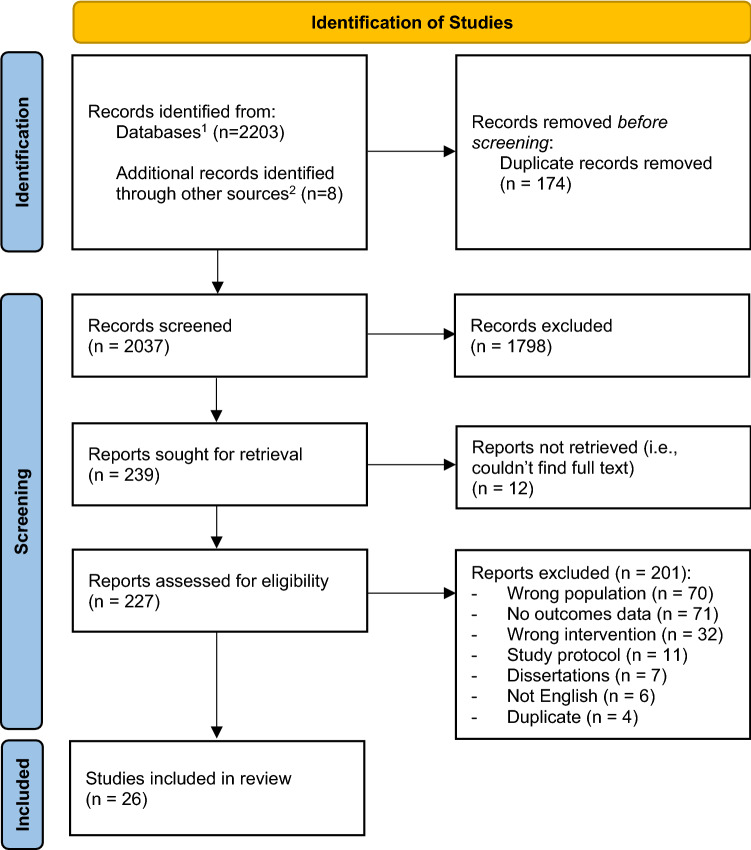
A total of 2,037 records were identified after removing duplicates, which includes 8 articles identified via forward/backward searches based on citations and leads from studies yielded in our initial searches. After title/abstract screening and full text reviews (n = 227), a total of 26 studies were included. One article (Currie & Startup, 2012) reports on two studies testing the same intervention with different methods; thus, this review includes 25 articles that report on 26 studies. Figure 1 illustrates the process of study selection and Table 1 summarizes the characteristics of included studies. Given the broader scope of this review, it was not appropriate to conduct a meta-analysis given the heterogeneity of designs, populations (e.g., age), measures, analyses, and outcomes. International studies in the review come from 14 countries with the majority clustered in the United States (n = 11) and Australia (n = 5). Studies were conducted in a variety of contexts; the majority are in schools (n = 10), college campuses (n = 6), and outpatient mental health (n = 4) settings.
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) flow diagram of the selection process of studies (n = 26) testing the effects of psychosocial interventions integrating music to improve engagement and/or mental health among A-YA. 1Database searches conducted in April 2020 and November 2021. 2Other sources refer to articles that were identified via forward/backward searching to account for articles not yielded in our initial database searches within specified keywords
Table 1.
Summary of Study Characteristics (n = 26) including Design, Population, Setting, Objective, Intervention, Outcome Measures, and Key Findings
| SOCIO-SOMATIC INTERVENTIONS | |||||||
|---|---|---|---|---|---|---|---|
| Study | Design | Study Population | Setting | Objective | Intervention | Outcome Measure(s) | Key Findings |
|
Aalbers et al., 2020 (Netherlands) Music Therapy |
Single-Group Design: Pre/posttest with 1-month F/U | YA females (N = 15) aged 19–30 (M = 23, SD = 3) with depression symptoms; 50% Dutch and 50% German | College Campus | Reduce depression and improve emotion regulation and positive affect |
Emotion-Regulating Improvisational Music Therapy (10 sessions) Active (e.g., group music making and improvision) No comparison |
Primary: Inventory of Depressive Symptomatology Secondary: Difficulties in Emotion Regulation Scale (DERS); Bodily and Emotional Perception of Pain questionnaire (affect) |
Significant reductions for depression and improvement in emotion regulation at posttest, compared to control condition. These results remained at 4-week F/U |
|
Kim et al., 2018 (South Korea) Nursing |
Quasi-Experimental Design: Pre/posttest | Adolescents males (N = 72) with maladjustment and behavioral issues (M age = 15, SD = 2, range NR); Korean identified | School | Increase self-esteem and reduce aggression |
Group music therapy (24 sessions) Active (e.g., group music-making) Active comparison |
CSEI, Mental Health Questionnaire for Korean Adolescents | Participants reported significant improvements in social, academic, and self-esteem and self-injurious aggression at posttest compared to control group. Verbal, object-related, person-related, and total aggression were found to be NS |
|
Martin et al., 2012 (Australia) Art Therapy |
Single-Group Design: Pre/post with 10-week F/U* | YA females (N = 19) aged 16–25 (M = 20; SD NR) with at least 1 episode of NSSI; race/ethnicity NR | College Campus | Reduce the frequency of NSSI and improve emotion regulation, alexithymia, and self-esteem |
Voice Movement Therapy (10 sessions) Active (e.g., group singing, rhythmic sound exercises, music-making with percussive instruments, group movement) No comparison |
Primary: Self-Injury Questionnaire Secondary: DERS, Rosenberg Self-Esteem Scale (RSE), General Health Questionnaire, Toronto Alexithymia Scale |
Significant improvements in emotion regulation, alexithymia, self-esteem, anxiety, somatic symptoms and social dysfunction at posttest and 10-weeks. Changes in depression and self-injury were NS but changes in mean scores suggest small improvements |
|
Porter et al., 2017 (Ireland) Sociology |
Experimental Design: Pre/posttest with 3-month F/U | Adolescents (N = 251) aged 8–16 (M/SD NR) with social, emotional, and behavioral issues; 56% female; 97% white | Outpatient MH | Improve social and communication skills and promote positive changes in social functioning, self-esteem, depression and family functioning |
Alvin model of ‘Free Improvisation' Music Therapy (12 sessions) Active (e.g., music-making, music listening, group improvisation, body movement, singing) Passive comparison |
Primary: Social Skills Improvement System Rating Scales (SSIS) Secondary: RSE, CES-D, Child Behavior Checklist, Family Assessment Device |
Participants 13 and over in the intervention group reported improvements in social skills, self-esteem, and depression at week 13, compared to control group. Changes on guardian reported SSIS, family, and social functioning were NS |
|
Rickson & Watkins, 2003 (New Zealand) Music Therapy |
Experimental Design: Pre/posttest | Adolescent boys (N = 15) aged 11–15 (M = 13, SD NR) with social, emotional, and behavioral issues; race/ethnicity NR | Residential Setting | Promote prosocial behaviors |
Group music therapy: (16 sessions) Hybrid (e.g., music listening, structured rhythmic activities, group songwriting and synchronized singing) Waitlist comparison |
Developmental Behavior Checklist; video analysis of sessions | No significant changes across any outcome measures. However, small changes in mean scores suggest that a MT program that aims to promote autonomy and creativity may help adolescents to interact more appropriately with others, but may also lead to a short-term mild increase in disruptive behavior |
|
Rickson, 2006 (New Zealand) Music Therapy |
Experimental Design: Pre/during/posttest | Adolescent boys (N = 13) aged 11–16 (M = 13, SD NR) with emotional, behavioral, and mood related disorders; race/ethnicity NR | Residential Setting | Reduce impulsivity behaviors |
Instructional music therapy and Improvisational music therapy (16 sessions total) Active (e.g., structured repetitive rhythmic activities with percussion instruments and emotionally themed group improvisation, performance) Waitlist comparison |
Conners Global Index Restless-Impulsive Scale; Conners' DSM-IV Hyperactive-Impulsive Scale; Synchronized Tapping Task Session observation forms, daily notes, and video data were used as measurement tools alongside self-reports |
Instructional and improvisational MT groups both reported significant increases in self-control of motor tasks along with a reduction in restlessness and impulsivity at posttest (teacher reports). However, the music therapist's measures of restlessness and impulsivity during sessions were NS. While NS, both groups reported lower STT scores during the instructional phase |
|
Shuman et al., 2016 (United States) Psychiatry |
Single-Group Design: Pre/posttest | Adolescents (N = 352) aged 12–21 (M = 15, SD = 2) with mood and eating disorders; 88% white; 71% female | Inpatient MH | Promote positive changes in moods |
Group music therapy (# of sessions NR) Hybrid (e.g., group music listening and lyric discussions, drum circles, group improvisation with instruments) No comparison |
Fast Assessment of Child Emotions | Results indicate the probability of a change in total mood score was high. Of the individual mood items, fatigue and energy changed the most. No significant associations between age, gender, or other specific demographics that were tested, nor changes in individual or total mood scores |
|
Wu, 2002 (Taiwan) Music Therapy |
Experimental Design: Pre/posttest with 2-month F/U | YAs (N = 28) aged 19–21 (M and SD NR) with depression, anxiety, and self-esteem challenges; 50% male; Taiwanese identified | College Campus | Reduce anxiety and depression and improve self-esteem |
Group music therapy (10 sessions) Passive comparison |
Zung's Self-Rating Depression and Anxiety; RSE | Experimental group participants demonstrated reductions in anxiety at posttest and at 2-month F/U. Only depression was found to be reduced at 2-month F/U. Qualitative results suggest positive changes such as more pleasure, relaxation, and confidence, and few negative emotions. Self-esteem was NS |
| SOCIO-COGNITIVE INTERVENTIONS | |||||||
|---|---|---|---|---|---|---|---|
| Study | Design | Study Population | Setting | Objective | Intervention | Outcome Measure(s) | Key Findings |
|
Bibb et al., 2019 (Australia) Music Therapy |
Single-Group Design: Pre/posttest | YA females (N = 13) aged 18–41 (M = 26, SD = 7) with eating disorders; race/ethnicity NR | Outpatient MH | Reduce subjective perception of anxiety |
Resource-Oriented Music Therapy (13 sessions) Receptive (e.g., music listening, lyric analysis) No comparison |
Subjective Units of Distress Scale (SUDS) | Significant reductions were observed in post-meal anxiety at posttest |
|
Dingle & Fay, 2017 (United States) Music Psychology |
Experimental Design: Pre/posttest | YAs (N = 51) aged 16–26 (M = 19, SD = 2); 67% female; race/ethnicity NR | College Campus | Improve emotional awareness and regulation skills, and engagement |
Tuned-In: A brief group music psychology intervention (4 sessions) Receptive (e.g., music listening, lyric analysis, guided imagery activities) Waitlist comparison |
DERS, Weekly rating of emotions, attendance and satisfaction, Depression Anxiety Stress Scale | Tuned-In participants reported significant improvements in emotional awareness, ability to clearly identify emotional states, ability to access effective emotion regulation strategies, and overall difficulties in emotion regulation at posttest, compared to comparison group. Results suggest attendance was high (98% attendance rate) |
|
Gee et al., 2019 (United Kingdom) Music Psychology |
Experimental Design: Pre/posttest | YA females (N = 13) aged 18–31 (M = 21, SD = 4) with anxiety and depression; race/ethnicity NR | College Campus | Reduce anxiety and depression and improve social connection |
Blue Notes: A structured and guided songwriting intervention (5 sessions) Active (e.g., structured songwriting activities) Waitlist control |
Primary: Hospital Anxiety and Depression Scale (HADS); Four-Item Measure of Social Identification Secondary: Social Phobia Inventory and UCLA Loneliness Scale |
Blue Notes participants reported significantly lower levels of depression and higher social connection from baseline to posttest compared to control group. Other outcome measures were NS |
|
Gold et al., 2017 (Vienna) Music Therapy |
Experimental Design: Pre/posttest | Adolescents (N = 89) aged 13–15 (M = 14; SD = 1) identified as at-risk and low-income; 67% female; race/ethnicity NR | School | Reduce unhealthy uses of music and increase potentials for healthy uses; improve depressive symptoms, psychosocial well-being, rumination, and reflection |
Group music therapy (8 sessions) Hybrid (e.g., group improvisation, music listening, lyric analysis, playlist creation) Active comparison |
Primary: Healthy and Unhealthy Use of Music scale Secondary: Kessler 10 Depression Scale, Mental Health Continuum-Short Form, Rumination- Reflection Questionnaire |
No significant differences between GMT and SDML groups across any outcome measures. While NS, participants in both groups demonstrated small improvements in MH at posttest |
|
Henderson, 1983 (United States) Music Therapy |
Experimental Design: Pre/posttest | Adolescents (N = 13) with adjustment disorder, mostly low income (M age = 16, SD/range NR); 53% male; race/ethnicity NR | Inpatient MH | Increase self-esteem, awareness of mood, and emotional expression along with social cohesion |
Group music therapy (18 sessions) Receptive (e.g., group music listening, expression and identification of body language) Passive comparison |
CSEI, sociograms, adjective checklist of emotions | Significant differences in favor of experimental group on the adjective checklist of emotions, self-esteem, and expression of group feelings. Changes in group cohesion were NS |
|
Levy, 2019 (United States) School Counseling |
Single-Group Design: Pre/posttest | Adolescents (N = 12) aged 14–18 (M = 15, SD NR); 75% male; 50% Black, 33% Latinx | School | Improve social and emotional well-being with a focus on coping skills, emotional self-awareness, and self-image |
Hip-Hop and Spoken Word Therapy (# of sessions NR) Hybrid (e.g., lyric writing, emotionally themed mixtapes, journaling, hip hop cypher, song recording and performance) No comparison |
Stages of Change for Emotional Coping Scale, Emotional Self-Awareness Scale, PSS | Significant positive movement from the preparation stage to an action stage for emotional coping. Changes in perceived stress and emotional self-awareness were NS but changes in mean scores suggest small improvements. Qualitative findings suggest improvements emotional expression, coping, and self-image |
|
Mogro-Wilson & Tredinnick, 2020 (United States) Social Work |
Quasi-Experimental Design: Pre/posttest | Adolescents (N = 304) (M age = 14, SD = 1, range NR); 51% female; 74% white | School | Promote the development of social and emotional competencies |
Connect with Kids: A classroom based SEL intervention (7 sessions) Receptive (e.g., music listening, lyric analysis, visual arts activities) Passive comparison |
Interpersonal Reactivity Index (subscales on perspective taking, fantasy, empathic concern, and personal distress) | Connect with Kids participants demonstrated significant increases in positive social and emotional behaviors of social awareness and empathy, empathetic concern, and perspective taking, compared with participants in the control group |
|
Munson et al., 2021 (United States) Social Work |
Experimental Design: Pre/posttest with 3-month F/U | YAs (N = 121) aged 18–34 (M = 26, SD = 4) with SMI and low-income; 66% male; 72% Black and Latinx | Outpatient MH | Improve treatment engagement by targeting cognitive, social, and affective barriers to MH service use |
Just Do You: A brief multicomponent meta-intervention (2 sessions) Receptive (e.g., music listening, lyric analysis, group discussions) Passive comparison |
Outcome: Yatchmenoff Engagement Scale Mediators: Adult Hope Scale. Study-specific measures for emotional reactions, behavioral beliefs, social norms, image, emotions, & self-efficacy |
JDY participants reported higher levels of treatment engagement at 3-months, compared to control group. All hypothesized mechanisms of change were significantly associated with engagement, and (2) JDY itself led to significant positive changes in 4 mechanisms of change including stigma, credibility of providers, trust in providers, perceived benefits of treatment. JDY’s effect on other mechanisms of change were NS |
|
Tyson, 2002 (United States) Social Work |
Experimental Design: Pre/post test | Adolescents (N = 11) with behavioral and mental health challenges (M age = 16, SD = 1, range NR); 63% male; 77% Black and Latinx | Residential Setting | Promote therapeutic engagement and improve self-concept and peer relations |
Hip-Hop Therapy (HHT) (12 sessions) Receptive (e.g., music listening, lyric analysis, group discussions) Passive comparison |
Self-Concept Scale for Children; Index of Peer Relations Scale | HHT participants reported significant improvements in peer relations at posttest, compared to control group. Changes in self-concept were NS but change in mean scores suggest small improvements. Qualitative findings suggest that youth enjoyed the sessions, expressed excitement to return to groups, and increases in self-expression via writing lyrics |
| HOLISTICALLY-INTEGRATED INTERVENTIONS | |||||||
|---|---|---|---|---|---|---|---|
| Study | Design | Study Population | Setting | Objective | Intervention | Outcome Measure(s) | Key Findings |
|
Currie & Startup, 2012 (study 1) (Australia) Psychology |
Quasi-Experimental Design: Pre/posttest with 6-month F/U | Adolescent males (N = 54) aged 12–15 (M = 14, SD = 5) with aggression and behavioral issues; rural and low-income; race/ethnicity NR | School | Reduce trait anger and reactive aggression behaviors and improve self-esteem and reduce depression |
Doing Anger Differently (DAD): A structured group percussion therapy program (20 sessions) Active (e.g., structured group percussion and discussions) Waitlist comparison |
Trait Anger Scale; Anger-Out scale; school behavior reports, Beck Depression Inventory (BDI), Coopersmith Self Esteem Inventory (CSEI) | DAD participants reported significant reductions in trait anger, aggression-reports, and depression, and increased self-esteem at posttest, compared to control group. Results maintained at 6-months |
|
Currie & Startup, 2012 (study 2) (Australia) Psychology |
Experimental Design: Pre/posttest with 6-month F/U | Adolescent males (N = 65) aged 12–15 (M = 14, SD = 1) with records of aggressive behavior; race/ethnicity NR | Outpatient MH | Replication of study 1 with a larger randomized sample in a community treatment setting |
DAD: A structured group percussion therapy program (20 sessions) Active (e.g., structured group percussion and discussions) Waitlist comparison |
Trait Anger Scale; Anger-Out scale; school behavior reports, BDI, CSEI | DAD participants reported significant reductions in aggression at 6-months, with lower trait anger and anger expression at posttest, compared to control group. Depression and self-esteem were NS |
|
Hendricks, 1999 (United States) Counseling |
Experimental Design: Pre/posttest | Adolescents (N = 19) aged 14–15 (M and SD NR) with depression symptoms; 89% female; 79% white | School | Reduce symptoms of depression |
Group music therapy (10 sessions) Hybrid (e.g., progressive muscle relaxation, group music listening, drawing activities) Active comparison |
BDI | Significant reductions in depression for those in MT group, compared to control group |
|
Hylton et al., 2019 (United States) Creative Arts Therapy |
Single-Group Design: Pre/posttest | Adolescents (N = 44) (M age = 15, SD = 1, range NR) with depression, anxiety, and PTSD symptoms; 65% female; 44% white and 41% Latinx | School | Improve mental health of adolescents exposed to school shooting |
Creative arts therapy (8 sessions) Hybrid (e.g., group music listening, lyric analysis, songwriting, drumming) No comparison |
Patient Health Questionnaire-8; Generalized Anxiety Disorder 7-Item Scale; Child’s Reaction to Traumatic Events Scale; Positive and Negative Affect Schedule | Subgroup analysis by therapeutic activity group indicate no significant changes across any outcome measures for MT group (N = 7). However, when considering entire sample, significant reductions in posttraumatic stress, depression, anxiety and negative affect were observed at posttest |
|
Kõiv et al., 2015 (Estonia) Art Therapy |
Quasi-Experimental Design: Pre/posttest | Adolescent females (N = 29) aged 14–17 (M = 16, SD = 1) with emotional and behavioral issues; race/ethnicity NR | Correctional Setting | Increase positive self-concept and self-esteem; support emotional expression and regulation skills, promote prosocial skill development |
Integrated Arts Therapy (10 sessions) Hybrid (e.g., group music listening, music-making, song recording, drama, storytelling) Passive comparison |
Strengths & Difficulties Questionnaire and Modified Behavior Checklist |
Participants in experimental group reported significant increases in prosocial behaviors, decreases in aggression, and decreases in emotional symptoms, compared to control group. Hyperactivity and peer problems were found to be NS |
|
Kwok et al., 2018 (China) Social Work |
Experimental Design: Pre/posttest | Adolescents (N = 106) with anxiety symptoms (M age = 14, SD = 1, range NR); 70% male; Chinese identified | School | Increase hope and emotional competence in effort to reduce anxiety and increase happiness |
Resource-Oriented Music Therapy with positive psychology (8 sessions) Hybrid (e.g., music-making, music listening, lyric writing, guided imagery, performance) Passive comparison group |
Outcome: HADS, Subjective Happiness Scale Mediators: Wong & Law Emotional Competence Scale, Children's Hope Scale |
Participants in experimental group reported significant increases in hope, emotional competence, subjective happiness, and decreases in anxiety at posttest compared to control group. Hope was a significant mediator between the intervention and decreases in anxiety and increase in happiness. Paths from emotional competence to anxiety and happiness were NS |
|
Levy & Travis, 2020 (United States) School Counseling |
Quasi-Experimental Design: Pre/posttest | Adolescents (N = 18) with elevated levels of stress between the ages 14–17 (M and SD NR); 56% Latinx and 17% Black; 56% male | College Campus | Promote social and emotional well-being and reduce stress, anxiety, and depression |
Blended intervention: 1) Critical Cycle of Mixtape Creation and 2) Hip Hop and Empowerment (3 group structures—5 sessions) Hybrid (e.g., music listening, lyric analysis, songwriting, hip hop cypher, song recording) Active comparison |
Perceived Stress Scale (PSS), Abbreviated Brief Symptom Inventory (BSI) | Significant decreases for both perceived stress and depression, but not for anxiety across the entire sample. Participants in the semi-structured group reported greatest reductions in perceived stress, compared to the other 2 leadership styles at posttest |
|
Martin et al., 2017 (Australia) Psychology |
Single-Group Design: Pre/posttest | Adolescents (N = 41) (M age = 14, SD = 1, range NR) at risk for MH issues; 58% female; 17% Aboriginal or Torres Strait Islander | School | Improve mental wellbeing and reduce distress, PTS symptoms, and antisocial behavior |
DRUMBEAT: A group-based multicomponent intervention (10 sessions) Active (e.g., group drumming, role play, group discussions, problem solving, relationship building) No comparison |
Warwick–Edinburgh Mental Wellbeing, Kessler-5, PTSD checklist, Self-Reported Delinquency | Significant positive changes in mental wellbeing, PTS symptoms, and antisocial behavior observed for boys at posttest. These changes were NS for girls. Psychological distress outcomes were NS across gender |
|
Travis et al., 2019b (United States) Social Work |
Quasi-Experimental Design: Pre/posttest | Adolescents (N = 35) aged 11–15 (M = 13, SD = 1) with elevated anxiety and depression; 79% Black; 57% female | School | Promote positive youth development and reduce depression and anxiety |
Blended intervention using Hip Hop and Empowerment and Therapeutic Beat Making (# of sessions NR) Hybrid (e.g., music listening, lyric analysis, therapeutic beat making, songwriting) Passive comparison |
BSI, Empowerment-based Positive Youth Development Scale (EMPYD) | Intervention participants reported significant improvements for character (EMPYD), depression, and anxiety at posttest, compared to control group |
Note: Amount of detailed information provided for intervention components differed by study (e.g., race/ethnicity, age range, SD). F/U = follow up. *Intended to have a control group but analyzed as single-group design due to logistical constraints. NR = not reported; YA = young adult; NSSI = non-suicidal self-injury. Not all studies distinguished between primary vs. secondary outcomes
Table 2 presents the specific components of methodological rigor and quality of included studies based on the results of the MQRS. Thirteen studies use experimental designs with randomization, 7 use single-group designs, and 6 use quasi-experimental designs. Among studies using experimental or quasi-experimental designs, most compare interventions to passive (n = 9) or waitlist (n = 5) comparisons while active (n = 4) controls are less common. Sample sizes are small and range from 11 to 352 participants (M = 69, SD = 92); 50% of studies use samples with less than 30 participants. Mean age of participants range between 13 and 26 years old; 73% (n = 19) of studies target adolescents (M age = 13–17 range) and 27% (n = 7) focus on young adults (M age = 18–26 range). Socially and economically marginalized A-YA are underrepresented across samples. Only 50% of studies reported the race or ethnicity of participants while all studies report gender. Fourteen studies have majority female samples, 11 studies have majority male samples, and 1 study is evenly split. Most studies (n = 19) focus on A-YA with common mental disorders (e.g., depression, anxiety, behavioral issues) or those at-risk of developing emotional and behavioral issues while seven studies (Bibb et al., 2019; Martin et al., 2012; Munson et al., 2021; Porter et al., 2017; Rickson & Watkins, 2003; Rickson, 2006; Shuman et al., 2016) included participants with a formally diagnosed SMI (e.g., schizophrenia-spectrum, bipolar, major depressive, eating disorders) or SED (e.g., self-injury, conduct disorders, significant mood symptoms). Finally, most studies rely on convenience samples, and few discuss whether participants had prior experience in mental health services.
Table 2.
Components of Methodological Quality and Rigor of Included Studies (n = 26)
| Methodological Criteria | N | % |
|---|---|---|
| 1. Single-group design (no comparison group) | 7 | 26.9 |
| 2. Quasi-experimental design (non-equivalent comparison group) | 6 | 23.1 |
| 3. Experimental design (randomization with comparison group) | 13 | 50.0 |
| 4. Parallel replications at two or more sites | 6 | 23.1 |
| 5. Procedures contain sufficient detail for replication | 24 | 92.3 |
| 6. Baseline scores, characteristics, or measures reported | 26 | 100.0 |
| 7. Intervention activities standardized or specified by curriculum, protocol, or manual | 25 | 96.2 |
| 8. Dosage or percent of intervention received by participants discussed or enumerated | 15 | 57.7 |
| 9. Measures have adequate psychometric properties & sufficient information provided | 25 | 96.2 |
| 10. Objective source or collateral verification used in addition to self-report measures | 6 | 23.1 |
| 11. Follow up conducted by person blind to treatment condition | 3 | 11.5 |
| 12. Less than 70% follow-up rate or insufficient information provided | 8 | 30.8 |
| 13. 70–84.9% follow-up rate | 5 | 19.2 |
| 14. 85–100% follow-up rate | 13 | 50.0 |
| 15. Dropouts and attrition enumerated or discussed | 19 | 73.1 |
| 16. Rationale for type of analysis provided or appropriate analysis | 24 | 92.3 |
| 17. Sample size considerations articulated or adequate statistical power | 23 | 88.5 |
Note: One article included two sub-studies which were each rated using the MQRS (25 articles = 26 studies)
Twenty-four studies target primarily mental health (i.e., internalizing, externalizing, social and emotional outcomes), one study focuses on treatment engagement outcomes (Munson et al., 2021), and one study examines both mental health and treatment engagement outcomes (Dingle & Fay, 2017). Seven studies focus specifically on internalizing symptoms (e.g., anxiety, depression) (Bibb et al., 2019; Gold et al., 2017; Hendricks et al., 1999; Hylton et al., 2019; Levy & Travis, 2020; Shuman et al., 2016; Wu, 2002), two specifically target externalizing behaviors (e.g., aggression, impulsivity, conduct issues) (Rickson, 2006; Rickson & Watkins, 2003), and two specifically examine social and emotional (e.g., self-esteem, prosocial behaviors, emotion regulation) outcomes (Mogro-Wilson & Tredinnick, 2020; Tyson, 2002). The remaining 15 studies target a combination of at least two categories of mental health outcomes (see Table 1 for detailed clinical features of the study samples and how these outcomes were measured). All studies rely primarily on participant self-report instruments (e.g., Beck Depression Inventory) while four studies use observational checklists (e.g., Behavior Checklist) or objective records to triangulate data. Across the two studies that examine engagement outcomes, one assesses attendance rates (Dingle & Fay, 2017) and one assesses behavioral (i.e., attendance) and attitudinal (i.e., buy-in/involvement) dimensions (Munson et al., 2021). Most studies conduct one follow up assessment within one-week of the conclusion of the intervention. Among the studies that collect a second, longer-term post-intervention assessment, one collects data at one-month (Aalbers et al., 2020), two collect data at two-months (Wu, 2002; Martin, 2012), two collect data at three-months (Munson et al., 2021; Porter et al., 2017), and one collects data at six-months (Currie & Startup, 2012).
Intervention Characteristics: Theoretical Frameworks, Components, and Delivery Approaches
Table 1 summarizes the theoretical frameworks, intervention components, and delivery approaches of the intervention studies. All interventions except for one (Porter et al., 2017) were delivered in a group format by a licensed clinician; the number of sessions range from 2 and 24. Overall, a range of disciplines are represented with the majority in music therapy (n = 7), social work (n = 5), and psychology (n = 4). Four studies use Hip Hop-based approaches and were rooted primarily in social work and counseling disciplines (Levy, 2019; Levy & Travis, 2020; Travis et al., 2019b; Tyson, 2002). These interventions tended to articulate rationales rooted in cultural relevance, health equity, and social justice. Interventions focusing on music-based approaches more broadly, tended to provide rationales related to music’s capacity to support emotional wellness. Interventions are informed by a range of theoretical frameworks (e.g., cognitive, humanistic, strengths-based, psychodynamic, empowerment) with cognitive (n = 5) and humanistic (n = 5) being the most frequently reported (see Online Resource 2). Studies that were guided by humanistic approaches tended to be more client-led with less structure and more improvisation. The humanistic approach is influenced by Carl Rogers’ person-centered therapy, which lends itself to “here and now” activities that are more process-oriented to help individuals cultivate social and emotional awareness (Rogers, 1966). For example, Aalbers and colleagues (2020) used an Emotion-Regulating Improvisational Music Therapy (EIMT) intervention that embeds music-making to enhance attunement and emotion regulation to reduce depression symptoms among female young adults. In EIMT, the client chooses the instrument for improvisation, and the therapist’s role is to mirror and support the client in the process using synchronization techniques (Aalbers et al., 2020).
In contrast, interventions informed by cognitive and behavioral theories tend to include more structured activities that are therapist-directed with less improvisation. These interventions tend to involve activities related to planning, problem solving, and goal setting. For example, Currie and Startup (2012) examined Doing Anger Differently (DAD); a structured percussion program informed by cognitive theory. DAD uses percussion exercises as a tool to foster problem-solving skills. One strategy involved a series of rhythmic exercises to experientially illustrate contrasts between “hot” and “cool” thinking, which lead to group discussions, psychoeducation, and in-vivo activities on identifying and responding to anger (Currie & Startup, 2012). Furthermore, while there are distinctions between these theoretical approaches, the types of music-based strategies (e.g., drumming) often overlap. For example, the EIMT and DAD interventions both involve active strategies such as drumming to improve mental health (Aalbers et al., 2020; Currie & Startup, 2012). However, the difference is reflected in the approach, structure, and process of how the strategy is used.
Overall, studies described and used music-based strategies in diverse ways to improve mental health outcomes. Most were conceptualized as primary interventions in which music-based strategies were described as a standalone tool to address a mental health outcome. For example, many of these studies emphasize the therapeutic capacity of sound, pitch, rhythm, and tempo as a tool to improve emotional wellness. In contrast, some studies were conceptualized as complementary interventions designed to serve as an “add-on” component to support the primary intervention services (e.g., traditional treatment) being provided in the setting. For example, these studies tended to describe music as a tool to provide an additional outlet for self-expression, social support, and engagement. Most interventions used hybrid strategies which consist of active (e.g., music-making, songwriting) and receptive (e.g., listening, lyric analysis) exercises. For example, listening to songs and discussing the meanings behind the lyrics was used across two studies specifically to enhance hope (Kwok, 2018; Munson et al., 2021) and more generally across 10 studies to facilitate therapeutic processes such as emotional expression and self-reflection (Bibb et al., 2019; Dingle & Fay, 2017; Gold et al., 2017; Hylton et al., 2019; Levy & Travis, 2020; Mogro-Wilson & Tredinnick, 2020; Shuman et al., 2016; Travis et al., 2019b; Tyson, 2002). In contrast, Levy and Travis (2020) examine a Hip Hop-based approach that was tested across three groups that were guided by distinct leadership styles and structures (deliberative, semi-structured, and non-deliberative). The results indicated that the semi-structured group was most conducive to reductions in stress compared to the other leadership styles (Levy & Travis, 2020).
Substantive Findings and Synthesis of Results
Twenty-three (88%) of the 26 studies reported that music-based interventions led to positive effects from baseline to initial follow up that were statistically significant for at least one main outcome; three studies reported non-significant effects on all outcome measures (Gold et al., 2017; Hylton et al., 2019; Rickson & Watkins, 2003). One study tested the effects of an intervention on treatment engagement (i.e., involvement, buy-in, and attendance) and found significant main effects (Munson et al., 2021) whereas another study descriptively examined engagement as a secondary outcome, and found a 98% attendance rate, but did not test its significance (Dingle & Fay, 2017). Approximately 12 studies describe how music-based strategies serve as a tool to bolster therapeutic engagement but only two measured it as a mediator or outcome. We found that few studies conducted a second, longer term follow up measurement to assess whether and how long treatment effects were sustained. For example, Wu (2002) found that treatment effects were not sustained for anxiety at two-months while Currie and Startup’s (2012) results were inconclusive at six-months as they were unable to collect follow up data from the comparison group. In contrast, Martin and colleagues (2012) found that effects were maintained at 10-week follow up.
The most frequently assessed mental health outcomes (i.e., internalizing, externalizing, social and emotional) across all categories with significant effects are improvements in social and emotional (e.g., emotion regulation, self-esteem) (n = 15) and internalizing (e.g., anxiety, depression) outcomes (n = 14) among adolescents. Among the six studies that target young adult mental health, five report significant effects for an internalizing and/or social and emotional outcome (Aalbers et al., 2020; Bibb et al., 2019; Gee et al., 2019; Martin et al., 2012; Wu, 2002). The findings are less conclusive for externalizing outcomes (i.e., impulsivity, aggression, conduct issues) as significant effects are only observed across five studies (Currie & Startup, 2012; Kõiv & Kaudne, 2015; Martin & Wood, 2017; Rickson, 2006). In contrast, two studies observed trends suggesting small improvements for aggression and impulsivity, but they were not statistically significant (Kim et al., 2018; Rickson & Watkins, 2003). While there are no studies that reported sustained adverse effects, Rickson and Watkins (2003) found that less structured music therapy activities led to small, temporary increases of disruptive classroom behavior among youth. The authors suggest that smaller and more structured activities may be more appropriate to avoid overstimulation and arousal however more research is needed to support these claims (Rickson & Watkins, 2003).
A Typology of Music-Based Interventions
The results summarized in this review gave rise to a typology of music-based interventions (Fig. 2) that can move the field to precisely classify and make decisions about which strategies to use. A typological analysis is an approach that is relevant to systematic reviews, because it aims to develop an organizing framework for the synthesis of results to better understand and classify a phenomenon of interest (Given, 2008; Page et al., 2021). In this review, the typology emerged based on an analysis of the similarities and differences in how each study embedded music-based components to improve outcomes. Broadly speaking, this framework is grounded in three types of intervention experiences: 1) Somatosensory, 2) Social-Emotional, and 3) Cognitive-Reflective. Somatosensory refers to active experiences that primarily involve bodily, kinesthetic, and sensory elements. Social-emotional refers to experiences that are primarily interpersonal and interactive; these experiences often involve self and social awareness and emotional expression in a relational context. Cognitive-reflective refers to experiences that primarily involve higher order thinking, reflecting, and analyzing surrounding meaning-making. While these are conceptually distinct, results suggest that music-based interventions included activities that combined these experiences. These overlapping experiences gave rise to three hybrid categories: 1) socio-cognitive (n = 9), 2) holistically integrated (n = 9) (combines all three), and 3) socio-somatic (n = 8). No studies demonstrated characteristics of experiences in the cognitive-somatic category. See Online Resource 2 for details on specific intervention components by typology theme.
Fig. 2.
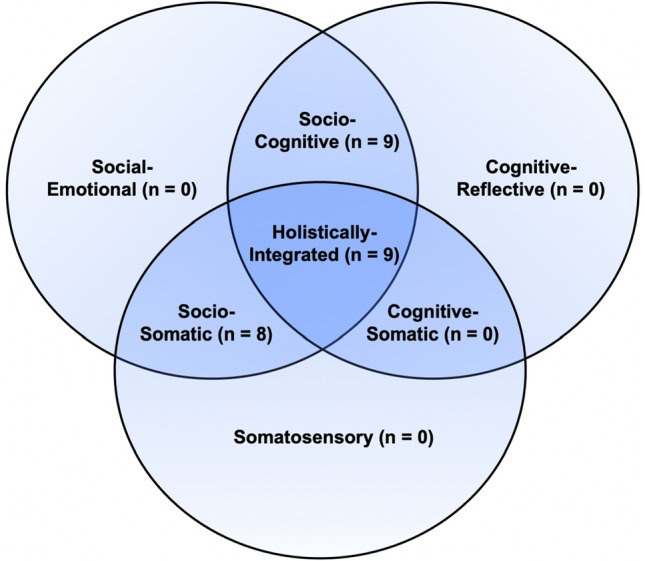
Typology of music-based interventions that emerged from analysis of the similarities and differences in how studies embedded music components
Socio-Cognitive Interventions
Socio-cognitive interventions (n = 9) include activities that are primarily interactive and relational to help participants recognize, process, and express emotions. These interventions also provide activities that primarily involve higher order thinking, analyzing, and reflecting to help participants derive meaning, insight, and knowledge. Socio-cognitive interventions provide activities that were process oriented (e.g., group improvisation) and discussion-based (e.g., lyric analysis). Overall, socio-cognitive interventions are most common across studies that found significant effects for social and emotional and internalizing outcomes. For example, Dingle and Fay (2017) used receptive listening, guided imagery, bodily awareness exercises, and lyric analysis to help young adults improve emotion regulation. Overall, many socio-cognitive interventions use lyric analysis with content that resonates with participants’ lived experience to establish an alliance, bolster engagement, express emotions, validate adverse experiences, form peer relationships, and discuss social issues in a culturally relevant and youth-centered way (e.g., Gold et al., 2017; Henderson, 1983; Hylton et al., 2019; Levy, 2019; Levy & Travis, 2020; Munson et al., 2021; Tyson, 2002).
Socio-Somatic Interventions
Socio-somatic (n = 8) interventions include activities that are primarily relational and engage bodily, kinesthetic, and sensory experiences. Socio-somatic interventions are mostly active and commonly involved activities such as drumming, music-making, synchronized movement, guided imagery, bodily awareness, and structured rhythmic sound exercises. Overall, socio-somatic interventions include the only studies with significant findings for externalizing symptoms alongside combinations of internalizing and socio-emotional outcomes. For example, Martin and colleagues (2012) include activities such as group singing, rhythmic sound exercises, music-making with percussive instruments, and expressive writing to facilitate cognitive and emotional processing of traumatic experiences, emotion regulation, reduction of self-injurious behaviors, and improve internalizing symptoms for young adults.
Holistically Integrated Interventions
Holistically integrated interventions (n = 9) emphasize activities that involve a combination of active and receptive processes which embody sensory, physical, reflective, relational, and emotionally focused experiences. Interventions that use music in holistically integrated ways tend to include activities such as drumming or beat-making, music-guided imagery or group improvisation, lyric analysis, and insight-oriented processes. Overall, holistically integrated interventions have the broadest scope of significant findings with combinations of internalizing, externalizing, and socio-emotional outcomes. For example, Travis and colleagues (2019) provided activities such as therapeutic beat making, lyric analysis, and group expressive activities (e.g., songwriting) to reduce depression and anxiety and promote positive youth development. Furthermore, this was the only typology category with studies that found significant effects for externalizing, internalizing, and social and emotional outcomes (Currie & Startup, 2012; Kõiv & Kaudne, 2015).
Implicit and Explicit Psychosocial Mechanisms of Change
Results indicate that most studies used an outcomes-only design to test if their intervention had significant main effects on the dependent variable(s) while few empirically examined mechanisms hypothesized to explain how change occurs. For example, two studies explicitly tested hypothesized mechanisms of change through measurement of the presumed mediators (Kwok, 2018; Munson et al., 2021), another nine studies implicitly conceptualized how change might occur (potential mechanisms) but did not operationalize, measure, or test their viability (see Online Resource 2 for detailed summary by study).
Explicit Mechanisms of Change
Kwok (2018) tested a resource-oriented music therapy intervention that included elements of positive psychology to reduce anxiety and improve subjective happiness among Chinese adolescents. It relies on a variety of active (i.e., playing instruments, songwriting, performance) and receptive (i.e., listening, guided imagery) music strategies in the context of activities focused on problem-solving, awareness and expression of emotions, and hope enhancement (Kwok, 2018). The intervention targets mediators of hope and emotional competence (e.g., regulation skills) to effect change in anxiety symptoms and subjective happiness. Results indicated (1) that the intervention significantly increased hope, and (2) higher levels of hope were significantly associated with lower levels of anxiety (Kwok, 2018). Also, the intervention significantly affected emotional competence but the path from emotional competence to subjective happiness was not statistically significant (Kwok, 2018). Also, it is important to note that the mediating role of hope was supported for boys and girls while emotional competence was only significant for boys (Kwok, 2018).
Munson and colleagues (2021) tested Just Do You (JDY), a brief intervention designed to help orient marginalized young adults with SMI to their treatment programs with the aim of improving their engagement and personal recovery. JDY embeds Motivational Interviewing principles, psychoeducation, and creative and technology-based strategies to address common mechanisms of treatment engagement (e.g., stigma, mistrust of providers, hope) (Munson et al., 2020). Music integration was primarily receptive, listening to songs with mental health content and having discussions of the lyrics as a tool to reduce stigma, increase hope, process emotions, and enhance self-efficacy. The study indicates that at 3-months, compared to controls, participants in JDY reported higher levels of treatment engagement (Munson et al., 2021). Mediational analyses indicated that: (1) all hypothesized mechanisms of change were significantly associated with treatment engagement, and (2) JDY led to significant positive changes in four hypothesized mechanisms of change, namely, stigma, credibility of providers, trust in providers, perceived benefits of treatment (Munson et al., 2021).
Implicit Mechanisms of Change
Nine studies discussed potential implicit mechanisms of change without formally operationalizing or testing their significance (Aalbers et al., 2020; Currie & Startup, 2012; Dingle & Fay, 2017; Gee et al., 2019; Kõiv & Kaudne, 2015; Levy & Travis, 2020; Martin & Wood, 2017; Travis et al., 2019b; Tyson, 2002). Most of these studies speculated on potential mechanisms as part of their explanation on how changes may have occurred. Across these nine studies, the most common implicit mechanisms were emotional resonance and regulation skills, social cohesion, and self-expression. For example, Aalbers and colleagues (2020) tested an improvisational music therapy intervention to reduce depression symptoms among young adults. The authors conceptualized, measured, and tested emotion regulation as a secondary outcome but then discuss it as a potential mechanism that may explain how depression symptoms are alleviated in their findings (Aalbers et al., 2020). These findings relate to Dingle and colleagues’ (2017) study that tested the Tuned-In program (i.e., receptive music techniques and psychoeducation) to improve emotional regulation among young adults. The authors discuss how the process of listening, analyzing, and discussing the meaning of song lyrics may serve as a mechanism through which music evokes emotions and regulation capacity. Similarly, Travis and colleagues (2019) tested a program that blended Hip Hop and Empowerment (HHE) and Therapeutic Beat Making (TBM) strategies; the authors discuss pathways to change that include evocation, modulation, and termination of emotions (Koelsch, 2015) and self-concept, relational, and expressive processes, respectively.
Martin and colleagues (2017) tested DRUMBEAT, a multi-component program that incorporates drumming and percussion exercises to improve mental well-being and reduce psychological distress, traumatic stress symptoms, and antisocial behavior among adolescents with emotional and behavioral challenges. They discuss potential mechanisms including: 1) cognitive and affective skills; 2) competence enhancement; 3) empowerment; 4) affiliation, rapport, and social cohesion (Martin & Wood, 2017). Tyson (2002) pilot tested Hip Hop Therapy (HHT) to improve therapeutic engagement, self-concept, and peer relations among at-risk adolescents with mental health and behavioral challenges. Tyson (2002) also describes how Hip-Hop culture serves as the “central mechanism of HHT” (p. 134), which reflects a culture of empowerment, expression, and storytelling. Several other studies (see Online Supplement 2) speculate about potential mechanisms, which could help inform future intervention studies aimed at explicitly measuring and testing how music-based interventions lead to change. These results move the field towards uncovering the common targets of these interventions which can be used to reimagine practice strategies with A-YA.
Discussion
This systematic review is the first to assess the evidence of music-based interventions that aim to improve treatment engagement and/or mental health outcomes among A-YA. Our findings provide a foundation to help researchers and practitioners reimagine new ways of conceptualizing how to integrate and use music more effectively to improve the lives of A-YA with mental health conditions. Below we discuss several key findings with respect to future directions for practice and research.
Assessing the Evidence Base for Adolescents and Young Adults
Our findings suggest that “nontraditional” approaches that involve creative, dynamic, and multisensory music-based strategies can lead to improvements in engagement and mental health for A-YA across diverse clinical contexts. Overall, most studies reporting significant main effects for mental health outcomes relate to social and emotional improvements and reductions of internalizing symptoms among adolescents in school settings. In contrast, the effects of music-based interventions on externalizing outcomes were less conclusive and limited by methodological constraints. Previous systematic reviews and meta-analyses have found similar results for children, younger adolescents, and adults with internalizing disorders (Belski et al., 2021; Geipel et al., 2018; Gold et al., 2004; Maratos et al., 2008; Tang et al., 2020). Our attention to social and emotional outcomes (e.g., emotion regulation, self-awareness, relationship skills) beyond the internalizing and externalizing symptoms dichotomy, is meaningful because the importance of these competencies has rarely been captured in previous reviews focused predominantly on specific disorders. We found that many studies described music as a strategy to provide “engaging” activities to address mental health using modalities that can bolster attendance, involvement, and participation. While this is in line with assertions that expressive therapies can encourage participants to become more active in the therapeutic process (Malchiodi, 2013), we found that these assumptions were seldom empirically tested.
Another important finding is the emergence of two distinct ways of using music-based strategies. For example, primary interventions conceptualized music-based strategies as the standalone tool to address a mental health outcome. In contrast, complementary interventions were designed to serve as an adjunct or add-on component to the primary treatment services being provided in the setting (e.g., traditional therapy or medication) to further support A-YA. This result contributes to the literature as few studies have articulated these versatile ways that music-based strategies can be embedded to provide complementary support or bolster motivation to attend primary treatment modalities provided in a service setting for A-YA (Dingle et al., 2008; Plener et al., 2010). Furthermore, this distinction reveals how practitioners can implement music-based strategies as a primary intervention or complementary or add-on component to enhance another intervention, or even as part of a treatment adaptation to enhance cultural and developmental responsiveness.
Our evaluation suggests that most studies demonstrate moderate methodological quality, with the highest proportion of studies including important characteristics such as reporting of baseline characteristics, specified intervention activities, and use of measures with adequate psychometric properties. The need for higher quality methods poses challenges to understanding several substantive areas. First, longer term follow ups are crucial to understanding if and how long effects are sustained beyond short-term relief. Second, more robust research designs would help promote a nuanced understanding of which effects and mechanisms are “specific” to music-based strategies compared to “nonspecific” elements (e.g., therapeutic alliance) that are common to all psychosocial interventions. Third, small sample sizes and overreliance on bivariate analyses are concerns as they limit statistical power to detect significant effects and the ability to account for confounding variables. Finally, it is crucial to prioritize data collection methods in which participants and researchers are blinded, as knowledge of desired outcomes and conditions can increase the risk of bias.
A Typology of Music-Based Interventions: A Practical Framework for Research and Practice
A novel contribution of this systematic review is a typology of music-based interventions that emerged from analyzing the components and processes involved in the included studies. This typology offers practitioners and researchers an organizing framework when considering how to use these strategies in social work practice. We found that all interventions are characterized by a combination of at least two levels (e.g., socio-cognitive) or all three (i.e., holistically integrated) rather than fitting into discrete categories (e.g., McFerran et al., 2020). For example, most interventions placed an emphasis on experiences that were socio-cognitive and holistically integrated followed by socio-somatic. These results illustrate the dynamic and multi-dimensional ways that active and receptive uses of music map onto somatosensory, social-emotional, and cognitive-reflective levels of functioning. These results contribute to the evolving literature that has explored the multidimensional nature of music and expressive therapies (see Lusebrink, 2010; Malchiodi, 2020; McFerran et al., 2020).
Our emergent typology framework maps onto Perry’s Neurosequential Model of Therapeutics that proposes a sequence of engagement (i.e., regulate, relate, and reason) to guide intervention planning when working with youth who have experienced complex trauma (Perry, 2006, 2009; Perry & Dobson 2015). The sequence of engagement posits that “without some degree of regulation, it is difficult to relate with another person, and without relational connection, there is minimal [cognitive] reasoning” (Perry & Winfrey, 2021, p. 142). Perry’s model, coupled with our innovative typology, offers clinicians (and researchers) a person-centered tool for selecting music-based strategies that match the personalized needs of each young person. This is relevant for social work practice given the profession’s attention to vulnerable A-YA who face high rates of environmental stressors.
Consistent with Perry’s (2009) research, our typology suggests that a young person who is dysregulated will benefit more from a socio-somatic music-based strategy that involves “patterned and repetitive rhythmic activity” that is active, synchronized, and interpersonal to focus on regulation and relational connection rather than one that relies on cognitive-reflective processes. Similarly, we would hypothesize that socio-somatic interventions (e.g., beat making, group drumming) may engage the mid and lower regions of the brain to help regulate an over-reactive nervous system using predictable, repetitive, and synchronized rhythmic activities (Greenberg et al., 2021; Perry, 2009; Perry & Dobson, 2015; Porges, 2011; van der Kolk, 2015). Furthermore, practitioners may find socio-cognitive interventions more beneficial when working with A-YA who are more regulated, or beneficial in conjunction with socio-somatic strategies that may foster regulation among those that are more dysregulated and reinforce regulation among the more regulated. In this way, our resultant typology provides a concrete resource for practitioners to help inform the planning and sequencing of music-based interventions.
Toward an Experimental Therapeutics Approach to Uncover How Change Occurs
A key finding of this review is that most studies tested if their intervention had significant main effects while fewer examined the psychosocial mechanisms hypothesized to explain how change in outcomes occur. The experimental therapeutics (ET) approach has gained traction as a guiding framework for psychosocial intervention development that offers a way to improve understanding of mechanisms of change (Gordon, 2017; Insel, 2015; Pintello, 2020). This approach requires investigators to: (a) identify the specific mediators targeted by an intervention (e.g., cognitive, social, affective) and (b) examine the downstream processes and cascading effects that occur after the intervention hits the target (Raghavan et al., 2019). We included this level of analysis to help illuminate how music-based interventions may lead to change. We found that hope was a common explicit mechanism while emotional resonance and regulation skills, social cohesion, and self-expression were common implicit mechanisms targeted by these interventions. Our results contribute to the evolving literature (e.g., Caló et al., 2020; Chin & Rickard, 2014; Greitemeyer, 2009; Papinczak et al., 2015) by identifying mechanisms that have been empirically tested within intervention studies targeting A-YA and potential consensus about implicit mechanisms that can be explicitly tested in future research. Furthermore, these findings inform research and practice by specifying explicit and implicit targets that may bear importance when working with A-YA.
While studies have called for more research examining mechanisms of change, little guidance has been provided to support this process. The ET approach offers a practical framework with potential to enhance the field’s understanding of which strategies are most promising for effecting change in the hypothesized mediators and outcomes. Recent studies have recommended systematic processes for applying ET (see Jaccard, 2021; Munson et al., 2022) and delineating mechanisms of music-based interventions (McFerran et al., 2020). For an example focused on prevention programs using randomized explanatory trials, see Jaccard and Bo (2018). Importantly, the ET approach can inform all phases of the research process (e.g., qualitative studies, designing intervention components) and is not limited to randomized trials (see Munson et al., 2022). Furthermore, this level of analysis and specificity can help illuminate how and for whom music-based interventions work along with areas that may need refinement based on non-significant results.
Cultural Relevance, Co-Creation, and Health Equity
Music is a worldwide form of expression that has been embraced by diverse cultural groups over millennia to support wellness, joy, and build community (Thaut, 2015). Music-based interventions can provide opportunities to enhance the cultural relevance of interventions if approached with humility and curiosity (Hadley & Norris, 2016). For example, we found that Hip Hop-based approaches tend to articulate rationales that centered cultural relevance, social justice, and health equity. Health equity can be understood as, “achieved when every person has the opportunity to attain his or her full health potential” and “no one is disadvantaged from achieving this potential because of social position or other socially determined circumstances” (CDC, 2022). This is consistent with Hip Hop culture’s history that evolved from providing an outlet of creativity, expression, and empowerment for Black and Puerto Rican youth in response to oppressive environments, inequity, and injustice in the Bronx during the 1970s (Chang, 2005; Travis, 2016). Similarly, Hip Hop integrated approaches are often facilitated by clinicians and teaching artists who identify or are intimately involved with elements of the culture (Crooke et al., 2021). Hip Hop-based approaches have the potential to improve health equity considering its focus on building awareness about inequities and conditions that are trauma-inducing while also encouraging advocacy at the individual and community levels (Travis, 2016; Travis & Deepak, 2011). It is important that researchers and clinicians approach the work of embedding music with humility and curiosity in ways that maintain cultural values, authenticity, and reflexivity, beyond providing an appealing way to work with “difficult-to-reach” A-YA (Hadley & Norris, 2016; Viega, 2016). This aligns with the NASW’s Code of Ethics (National Association of Social Workers, 2021), CSWE’s Educational Policy and Accreditation Standards (Council on Social Work Education, 2022), and the Grand Challenges for social work (Teasley, 2021) focused on combatting injustice, inequity, and systemic racism.
Limitations
This review has several limitations. First, while our broader scope yielded a larger number of studies, it also limited our capacity to assess some of the evidence due to heterogeneity of participant age, designs, measures, and outcomes. For example, different age groups (i.e., As vs. YAs) may experience various intervention components in distinct ways which may have implications for how such activities are delivered and developmentally tailored along with their potentially differential effects. Second, our assessment of the evidence was limited to studies presenting quantitative outcomes data published in refereed journals. Therefore, the influence of publication bias needs to be considered along with the reality that the expertise of many clinicians who use these strategies is not represented in the literature. Third, our classification of mechanisms of change was limited to studies that articulated these pathways implicitly or explicitly using keywords. It is possible that some of the studies we classified as “not providing enough information” may have reported these details in publications not included in this review.
Implications for Practice, Research, and Policy
Results from this review have several practice implications that can contribute to reimagining new ways of thinking about how social workers can leverage the potential of music and expressive strategies to support A-YA, particularly among those who are marginalized and experience excessive levels of stress. First, while there have been promising advances in trauma-informed interventions that embed creative, dynamic, and multisensory tools (e.g., strengths-based, mindfulness) (e.g., Bendall et al., 2021; McFerran et al., 2020; Scrine, 2021), our mental health system remains oriented predominantly around treatment paradigms that center on “top-down” (e.g., talk-based strategies focused on changing how we think) approaches which rely on cognitively mediated strategies (Malchiodi, 2020; Perry, 2009; Perry & Winfrey, 2021; van der Kolk, 2015). We describe how music-based interventions can be implemented as a primary or complementary approach, embracing the successes of but reaching beyond the limits of “traditional” strategies, alongside a review of the evidence that suggests these interventions can lead to improvements in engagement and mental health. Second, our intervention typology goes beyond assessing efficacy and effectiveness; it provides a practical and trauma-informed tool to help clinicians personalize and scaffold interventions (e.g., emphasis on socio-somatic or socio-cognitive) in more creative and culturally responsive ways to meet client needs, consistent with recovery and person-centered models of care (Damsgaard & Jensen, 2021; Davidson et al., 2005; Silverman, 2022). Finally, these strategies could potentially help clinicians provide more accessible, culturally affirming, strengths-based, and developmentally oriented ways to intervene with youth with a focus on healthy and empowering uses of music. These more innovative strategies can help A-YA address their mental health and develop trusting relationships with providers in a more authentic and less stigmatizing way.
The field is ripe for more studies that conceptualize, measure, and test hypothesized mechanisms of change to promote a more nuanced understanding of how (i.e., mediators) and for whom (i.e., moderators) music-based interventions work. Our typology enables researchers to examine the differential mechanisms and effects of various music-based interventions (e.g., socio-cognitive vs. socio-somatic). Second, our typology allows for examination of whether delivering these interventions in a scaffolded way (socio-somatic before socio-cognitive), consistent with Perry’s (2009) sequence of engagement, leads to outcomes with larger effects for A-YA experiencing traumatic stress. Third, studies that conceptualize music as a tool to bolster engagement should define, measure, and test these assumptions. Fourth, while there is a need for randomized trials, we acknowledge the tension around this as the only “gold standard” (Deaton & Cartwright, 2018). More rigorous methods such as active comparisons, blind conditions, larger samples, and long-term follow up can help reduce sampling error and advance the evidence base. Fourth, the field would benefit from more studies that examine implementation (e.g., sustainability, fidelity) as bringing “nontraditional” strategies into routine settings may present challenges (e.g., supervision, provider perceptions) that can influence clinical outcomes. Finally, considering COVID-19 and the rise of virtual therapeutic spaces, research should examine how these strategies can be delivered online and if they are as efficacious.
While there have been promising advances in funding opportunities such as NIH-Kennedy Center’s partnership on the Sound Health initiative (Collins & Fleming, 2017; NIH, 2018), there remains a need for more accessible funding mechanisms to develop a more robust evidence base. This funding would provide resources needed to support more rigorous research designs. Further, funding agencies and review panels that are less familiar with music-based interventions can help this process by remaining open to these proposals, especially those demonstrating strong methodological rigor. Second, “non-traditional” approaches continue to face barriers in training and sharing of expertise within social work education and professional development opportunities (Travis, 2019). There is a need for more education, dissemination, and training focused on music and expressive therapies to help clinicians develop the skills needed to use these strategies in practice. This aligns with CSWE’s Educational Policy and Accreditation Standards (2022) that highlight the importance of preparing social workers with the competencies to deliver evidence-informed and culturally responsive interventions. These policy considerations are crucial to support the development, implementation, and sustained use of novel psychosocial interventions. The implications highlighted in this review help us to reimagine new directions for investing in services and supports for adolescents and young adults.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank Stephen Maher for his support and expertise in systematic reviews and assisting with developing and executing database searches. The authors are grateful for J.C. Hall for commenting on the manuscript and providing his clinical expertise to enhance the implications of this work.
Author Contributions
AHR and MRM conceptualized and designed the study. AHR performed the database searches. AHR and RS screened all records, extracted relevant data, and evaluated methodological criteria of included studies. AHR wrote the first draft of the manuscript. RT assisted with synthesis of data, extraction of themes, and manuscript development. All co-authors (RS, RT, KJ, MB, and MRM) contributed to and approved the final manuscript.
Declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aalbers S, Spreen M, Pattiselanno K, Verboon P, Vink A, van Hooren S. Efficacy of emotion-regulating improvisational music therapy to reduce depressive symptoms in young adult students: A multiple-case study design. The Arts in Psychotherapy. 2020 doi: 10.1016/j.aip.2020.101720. [DOI] [Google Scholar]
- Alegría, M., Green, J. G., McLaughlin, K. A., & Loder, S. (2015). Disparities in child and adolescent mental health and mental health services in the US. New York, NY: William T. Grant Foundation. http://cfs.cbcs.usf.edu/projects-research/_docs/Disparities_in_child_and_adolescent_health.pdf
- Alvarez K, Polanco-Roman L, Samuel Breslow A, Molock S. Structural racism and suicide prevention for ethnoracially minoritized youth: A conceptual framework and illustration across systems. American Journal of Psychiatry. 2022;179(6):422–433. doi: 10.1176/appi.ajp.21101001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansdell, G., & Meehan, J. (2010). ‘‘Some Light at the End of the Tunnel’’: Exploring users’ evidence for the effectiveness of music therapy in adult mental health settings. Music and Medicine, 2(1), 29–40. 10.47513/mmd.v2i1.237
- Bendall S, Eastwood O, Cox G, Farrelly-Rosch A, Nicoll H, Peters W, Scanlan F. A systematic review and synthesis of trauma-informed care within outpatient and counseling health settings for young people. Child Maltreatment. 2021;26(3):313–324. doi: 10.1177/1077559520927468. [DOI] [PubMed] [Google Scholar]
- Belski N, Abdul-Rahman Z, Youn E, Balasundaram V, Diep D. The effectiveness of musical therapy in improving depression and anxiety symptoms among children and adolescents–a systematic review. Child and Adolescent Mental Health. 2021 doi: 10.1111/camh.12526. [DOI] [PubMed] [Google Scholar]
- Bibb J, Castle D, Skewes McFerran K. Reducing anxiety through music therapy at an outpatient eating disorder recovery service. Journal of Creativity in Mental Health. 2019;14(3):306–314. doi: 10.1080/15401383.2019.1595804. [DOI] [Google Scholar]
- Boyce WT, Ellis BJ. Biological sensitivity to context: I. An evolutionary–developmental theory of the origins and functions of stress reactivity. Development and Psychopathology. 2005;17(2):271–301. doi: 10.1017/s0954579405050145. [DOI] [PubMed] [Google Scholar]
- Bruscia KE. An introduction to music psychotherapy. 2. Barcelona Publishers; 1998. [Google Scholar]
- Cabassa LJ, Baumann AA. A two-way street: Bridging implementation science and cultural adaptations of mental health treatments. Implementation Science. 2013;8(1):90. doi: 10.1186/1748-5908-8-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caló F, Steiner A, Millar S, Teasdale S. The impact of a community-based music intervention on the health and well-being of young people: A realist evaluation. Health & Social Care in the Community. 2020;28(3):988–997. doi: 10.1111/hsc.12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr C, Odell-Miller H, Priebe S. A systematic review of music therapy practice and outcomes with acute adult psychiatric in-patients. PLoS ONE. 2013;8(8):e70252. doi: 10.1371/journal.pone.0070252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2022). Health Equity. Centers for Disease Control and Prevention. https://www.cdc.gov/chronicdisease/healthequity/index.htm
- Chan MF, Wong ZY, Thayala N. The effectiveness of music listening in reducing depressive symptoms in adults: A systematic review. Complementary Therapies in Medicine. 2011;19(6):332–348. doi: 10.1016/j.ctim.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Chanda ML, Levitin DJ. The neurochemistry of music. Trends in Cognitive Sciences. 2013;17(4):179–193. doi: 10.1016/j.tics.2013.02.007. [DOI] [PubMed] [Google Scholar]
- Chang J. Can't stop won't stop: A history of the hip-hop generation. Martin's Press; 2005. [Google Scholar]
- Chartier MJ, Walker JR, Naimark B. Separate and cumulative effects of adverse childhood experiences in predicting adult health and health care utilization. Child Abuse & Neglect. 2010;34(6):454–464. doi: 10.1016/j.chiabu.2009.09.020. [DOI] [PubMed] [Google Scholar]
- Chin, T., & Rickard, N. S. (2014). Emotion regulation strategy mediates both positive and negative relationships between music uses and well-being. Psychology of Music, 42(5), 692–713. 10.1177/0305735613489916
- Cole A, Jenefsky N, Ben-David S, Munson MR. Feeling connected and understood: The role of creative arts in engaging young adults in their mental health services. Social Work with Groups. 2018;41(1–2):6–20. doi: 10.1080/01609513.2016.1258619. [DOI] [Google Scholar]
- Cole AR, Jaccard J, Munson MR. Young adult trauma symptoms in the context of community violence exposure. Journal of Community Psychology. 2020;48(8):2517–2531. doi: 10.1002/jcop.22437. [DOI] [PubMed] [Google Scholar]
- Collins FS, Fleming R. Sound health: An NIH-Kennedy Center Initiative to Explore Music and the Mind. JAMA. 2017;317(24):2470–2471. doi: 10.1001/jama.2017.7423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas-Diaz L, Hall GN, Neville HA. Racial trauma: Theory, research, and healing: Introduction to the special issue. American Psychologist. 2019;74(1):1–5. doi: 10.1037/amp0000442. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Davis M, Burns BJ, Angold A, Costello EJ. Increase in untreated cases of psychiatric disorders during the transition to adulthood. Psychiatric Services. 2015;66(4):397–403. doi: 10.1176/appi.ps.201300541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Hinesley J, Chan RF, Aberg KA, Fairbank JA, van den Oord EJ, Costello EJ. Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Network Open. 2018;1(7):e184493–e184493. doi: 10.1001/jamanetworkopen.2018.4493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, He JP, Sampson NA, Kessler RC, Merikangas KR. Services for adolescents with psychiatric disorders: 12-month data from the National Comorbidity Survey-Adolescent. Psychiatric Services. 2014;65(3):359–366. doi: 10.1176/appi.ps.201100518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council on Social Work Education. (2022). Educational Policy and Accreditation Standards in Diversity and Social Justice. C. o. S. W. Education. https://www.cswe.org/Accreditation/Information/2022-EPAS
- Crooke, A., Almeida, C., & Comte, R. (2021). A Critical Interpretive Synthesis of Research Linking Hip Hop and Wellbeing in Schools. Journal of Hip Hop Studies, 8(1), 127–160. 10.34718/ts65-ky23
- Currie M, Startup M. Doing Anger Differently: Two controlled trials of percussion group psychotherapy for adolescent reactive aggression. Journal of Adolescence. 2012;35(4):843–853. doi: 10.1016/j.adolescence.2011.12.003. [DOI] [PubMed] [Google Scholar]
- Czeisler, M. É., Lane, R. I., Petrosky, E., Wiley, J. F., Christensen, A., Njai, R., Weaver, M. D., Robbins, R., Facer-Childs, E. R., & Barger, L. K. (2020). Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049. 10.15585/mmwr.mm6932a1 [DOI] [PMC free article] [PubMed]
- Damsgaard JB, Jensen A. Music Activities and Mental Health Recovery: Service Users’ Perspectives Presented in the CHIME Framework. International Journal of Environmental Research and Public Health. 2021;18(12):6638. doi: 10.3390/ijerph18126638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L, O'Connell MJ, Tondora J, Lawless M, Evans AC. Recovery in serious mental illness: A new wine or just a new bottle? Professional Psychology: Research and Practice. 2005;36(5):480. doi: 10.1037/0735-7028.36.5.480. [DOI] [Google Scholar]
- Daykin N, De Viggiani N, Pilkington P, Moriarty Y. Music making for health, well-being and behaviour change in youth justice settings: A systematic review. Health Promotion International. 2013;28(2):197–210. doi: 10.1093/heapro/das005. [DOI] [PubMed] [Google Scholar]
- Deaton A, Cartwright N. Understanding and misunderstanding randomized controlled trials. Social Science & Medicine. 2018;210:2–21. doi: 10.1016/j.socscimed.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dingle, G. A., & Fay, C. (2017). Tuned In: The effectiveness for young adults of a group emotion regulation program using music listening. Psychology of Music, 45(4), 513–529. 10.3389/fpsyg.2016.00859 [DOI] [PMC free article] [PubMed]
- Dingle GA, Gleadhill L, Baker FA. Can music therapy engage patients in group cognitive behaviour therapy for substance abuse treatment? Drug and Alcohol Review. 2008;27(2):190–196. doi: 10.1080/09595230701829371. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Erikson, E. H. (1968). Identity: Youth and crisis. WW Norton & company.
- Fancourt , D., & Finn, S. (2019). What is the evidence on the role of the arts in improving health and well-being? A scoping review (9289054557). W. H. O. R. O. f. Europe. https://apps.who.int/iris/bitstream/handle/10665/329834/9789289054553-eng.pdf [PubMed]
- Fontanella CA, Warner LA, Steelesmith DL, Brock G, Bridge JA, Campo JV. Association of timely outpatient mental health services for youths after psychiatric hospitalization with risk of death by suicide. JAMA Network Open. 2020;3(8):e2012887–e2012887. doi: 10.1001/jamanetworkopen.2020.12887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford J, Courtois C. Treating complex traumatic stress disorders in adults: Scientific foundations and therapeutic models. Guilford; 2020. [Google Scholar]
- Ganzel BL, Morris PA. Allostasis and the developing human brain: Explicit consideration of implicit models. Development and Psychopathology. 2011;23(4):955–974. doi: 10.1017/S0954579411000447. [DOI] [PubMed] [Google Scholar]
- Gee KA, Hawes V, Cox NA. Blue notes: Using songwriting to improve student mental health and wellbeing. A pilot randomised controlled trial. Frontiers in Psychology. 2019;10:423. doi: 10.3389/fpsyg.2019.00423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garrido S, Eerola T, McFerran K. Group rumination: Social interactions around music in people with depression. Frontiers in Psychology. 2017;8:490. doi: 10.3389/fpsyg.2017.00490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geipel J, Koenig J, Hillecke TK, Resch F, Kaess M. Music-based interventions to reduce internalizing symptoms in children and adolescents: A meta-analysis. Journal of Affective Disorders. 2018;225:647–656. doi: 10.1016/j.jad.2017.08.035. [DOI] [PubMed] [Google Scholar]
- Given LM, editor. The Sage encyclopedia of qualitative research methods. Sage; 2008. [Google Scholar]
- Gold C, Saarikallio S, Crooke AHD, McFerran KS. Group music therapy as a preventive intervention for young people at risk: Cluster-randomized trial. The Journal of Music Therapy. 2017;54(2):133–160. doi: 10.1093/jmt/thx002. [DOI] [PubMed] [Google Scholar]
- Gold C, Solli HP, Krüger V, Lie SA. Dose–response relationship in music therapy for people with serious mental disorders: Systematic review and meta-analysis. Clinical Psychology Review. 2009;29(3):193–207. doi: 10.1016/j.cpr.2009.01.001. [DOI] [PubMed] [Google Scholar]
- Gold C, Voracek M, Wigram T. Effects of music therapy for children and adolescents with psychopathology: A meta-analysis. Journal of Child Psychology and Psychiatry. 2004;45(6):1054–1063. doi: 10.1111/j.1469-7610.2004.t01-1-00298.x. [DOI] [PubMed] [Google Scholar]
- Gordon, J. (2017). An Experimental Therapeutic Approach to Psychosocial Interventions. National Institute of Mental Health (NIMH). Retrieved January 15, 2021 from https://www.nimh.nih.gov/about/director/messages/2017/an-experimental-therapeutic-approach-to-psychosocial-interventions
- Greenberg DM, Decety J, Gordon I. The social neuroscience of music: Understanding the social brain through human song. American Psychologist. 2021 doi: 10.1037/amp0000819. [DOI] [PubMed] [Google Scholar]
- Greitemeyer T. Effects of songs with prosocial lyrics on prosocial behavior: Further evidence and a mediating mechanism. Personality and Social Psychology Bulletin. 2009;35(11):1500–1511. doi: 10.1177/0146167209341648. [DOI] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry. 2010;10(1):1–9. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustavson DE, Coleman PL, Iversen JR, Maes HH, Gordon RL, Lense MD. Mental health and music engagement: Review, framework, and guidelines for future studies. Translation Psychiatry. 2021;11(1):370. doi: 10.1038/s41398-021-01483-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley S, Norris MS. Musical multicultural competency in music therapy: The first step. Music Therapy Perspectives. 2016;34(2):129–137. doi: 10.1093/mtp/miv045. [DOI] [Google Scholar]
- Hadley S, Yancy G. Therapeutic uses of rap and hip-hop. Routledge; 2012. [Google Scholar]
- Henderson SM. Effects of a music therapy program upon awareness of mood in music, group cohesion, and self-esteem among hospitalized adolescent patients. Journal Music Therapy. 1983;20(1):14–20. doi: 10.1093/jmt/20.1.14. [DOI] [PubMed] [Google Scholar]
- Hendricks CB, Robinson B, Bradley LJ, Davis K. Using music techniques to treat adolescent depression. The Journal of Humanistic Counseling. 1999;38(1):39. doi: 10.1002/j.2164-490X.1999.tb00160.x. [DOI] [Google Scholar]
- Hense C, Silverman MJ, McFerran KS. Using the healthy-unhealthy uses of music scale as a single-session music therapy intervention on an acute youth mental health inpatient unit. Music Therapy Perspectives. 2018;36(2):267–276. [Google Scholar]
- Hohmann L, Bradt J, Stegemann T, Koelsch S. Effects of music therapy and music-based interventions in the treatment of substance use disorders: A systematic review. PLoS ONE. 2017;12(11):e0187363. doi: 10.1371/journal.pone.0187363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hylton E, Malley A, Ironson G. Improvements in adolescent mental health and positive affect using creative arts therapy after a school shooting: A pilot study. The Arts in Psychotherapy. 2019 doi: 10.1016/j.aip.2019.101586. [DOI] [Google Scholar]
- Insel TR. The NIMH experimental medicine initiative. World Psychiatry. 2015;14(2):151. doi: 10.1002/wps.20227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2015). Psychosocial interventions for mental and substance use disorders: a framework for establishing evidence-based standards. National Academy Press. 10.17226/19013 [PubMed]
- Jaccard, J. (2021). Program Evaluation and Randomized Explanatory Trials: A Structural Equation Modeling Approach. Applied Scientific Analysis. www.explanatorytrials.com
- Jaccard J, Bo A. Prevention science and child/youth development: Randomized explanatory trials for integrating theory, method, and analysis in program evaluation. Journal of the Society for Social Work Research. 2018;9(4):651–687. doi: 10.1086/701388. [DOI] [Google Scholar]
- Jones SE, Ethier KA, Hertz M, DeGue S, Le VD, Thornton J, Geda S. Mental Health, Suicidality, and Connectedness Among High School Students During the COVID-19 Pandemic –Adolescent Behaviors and Experiences Survey, United States, January–June 2021. MMWR Supplements. 2022;71(3):16. doi: 10.15585/mmwr.su7103a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, He J-P, Koretz D, McLaughlin KA, Petukhova M. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2012;69(4):372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello J, Green JG, Gruber MJ, McLaughlin KA, Petukhova M, Sampson NA, Zaslavsky AM, Merikangas KR. Severity of 12-month DSM-IV disorders in the national comorbidity survey replication adolescent supplement. Archives of General Psychiatry. 2012;69(4):381–389. doi: 10.1001/archgenpsychiatry.2011.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kim H, Munson MR, McKay MM. Engagement in mental health treatment among adolescents and young adults: A systematic review. Child and Adolescent Social Work Journal. 2012;29(3):241–266. doi: 10.1007/s10560-012-0256-2. [DOI] [Google Scholar]
- Kim, H.-S., Kim, H.-S., & van Campen, C. (2018). The Effect of a Music Intervention Program on Self-Esteem and Aggression in Korean Male Middle School Students with Maladjustment Problems. In S. Pashang, N. Khanlou, & J. Clarke (Eds.), Today’s Youth and Mental Health (pp. 231–246). Springer. 10.1007/978-3-319-64838-5_13
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: Developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry. 2003;60(7):709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Kirmayer LJ. Cultural competence and evidence-based practice in mental health: epistemic communities and the politics of pluralism. Social Science and Medicine. 2012;75(2):249–256. doi: 10.1016/j.socscimed.2012.03.018. [DOI] [PubMed] [Google Scholar]
- Koelsch S. Music-evoked emotions: principles, brain correlates, and implications for therapy. Annals of New York Academic Science. 2015;1337(1):193–201. doi: 10.1111/nyas.12684. [DOI] [PubMed] [Google Scholar]
- Kõiv K, Kaudne L. Impact of integrated arts therapy: An intervention program for young female offenders in correctional institution. Psychology. 2015;06(01):1–9. doi: 10.4236/psych.2015.61001. [DOI] [Google Scholar]
- Kresovich A, Collins MKR, Riffe D, Carpentier FRD. A content analysis of mental health discourse in popular rap music. JAMA Pediatrics. 2021;175(3):286–292. doi: 10.1001/jamapediatrics.2020.5155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok SYCL. Integrating positive psychology and elements of music therapy to alleviate adolescent anxiety. Research on Social Work Practice. 2018;29(6):663–676. doi: 10.1177/1049731518773423. [DOI] [Google Scholar]
- Lakind D, Bradley WJ, Patel A, Chorpita BF, Becker KD. A multidimensional examination of the measurement of treatment engagement: Implications for children's mental health services and research. Journal of Clinical Child Adolescent Psychology. 2021 doi: 10.1080/15374416.2021.1941057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J, Thyer BA. Does music therapy improve mental health in adults? A review. Journal of Human Behavior in the Social Environment. 2013;23(5):591–603. doi: 10.1080/10911359.2013.766147. [DOI] [Google Scholar]
- Levy I, Emdin C, Adjapong ES. Hip-hop cypher in group work. Social Work with Groups. 2017;41(1–2):103–110. doi: 10.1080/01609513.2016.1275265. [DOI] [Google Scholar]
- Levy I, Travis R. The critical cycle of mixtape creation: reducing stress via three different group counseling styles. The Journal for Specialists in Group Work. 2020;45(4):307–330. doi: 10.1080/01933922.2020.1826614. [DOI] [Google Scholar]
- Levy IP. Hip-hop and spoken word therapy in urban school counseling. Professional School Counseling. 2019 doi: 10.1177/2156759x19834436. [DOI] [Google Scholar]
- Lin S-T, Yang P, Lai C-Y, Su Y-Y, Yeh Y-C, Huang M-F, Chen C-C. Mental health implications of music: Insight from neuroscientific and clinical studies. Harvard Review of Psychiatry. 2011;19(1):34–46. doi: 10.3109/10673229.2011.549769. [DOI] [PubMed] [Google Scholar]
- Lusebrink VB. Assessment and therapeutic application of the expressive therapies continuum: Implications for brain structures and functions. Art Therapy. 2010;27(4):168–177. doi: 10.1080/07421656.2010.10129380. [DOI] [Google Scholar]
- Ma L, Mazidi M, Li K, Li Y, Chen S, Kirwan R, Wang Y. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Affective Disorders. 2021;293:78–89. doi: 10.1016/j.jad.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney JL, Durlak JA, Weissberg RP. An update on social and emotional learning outcome research. Phi Delta Kappan. 2018;100(4):18–23. doi: 10.1177/0031721718815668. [DOI] [Google Scholar]
- Malchiodi CA. Expressive therapies. Guilford; 2013. [Google Scholar]
- Malchiodi CA. Trauma and expressive arts therapy: Brain, body, and imagination in the healing process. Guilford; 2020. [Google Scholar]
- Maratos A, Gold C, Wang X, Crawford M. Music therapy for depression. Cochrane Database of Systematic Reviews. 2008 doi: 10.1002/14651858.CD004517.pub2. [DOI] [PubMed] [Google Scholar]
- Martin KE, Wood LJ. Drumming to a new beat: a group therapeutic drumming and talking intervention to improve mental health and behaviour of disadvantaged adolescent boys. Children Australia. 2017;42(4):268–276. doi: 10.1017/cha.2017.40. [DOI] [Google Scholar]
- Martin S, Martin G, Lequertier B, Swannell S, Follent A, Choe F. Voice movement therapy: evaluation of a group-based expressive arts therapy for nonsuicidal self-injury in young adults. Music and Medicine. 2012;5(1):31–38. doi: 10.1177/1943862112467649. [DOI] [Google Scholar]
- McCoy H, McKay C. Preparing social workers to identify and integrate culturally affirming bibliotherapy into treatment. Social Work Education. 2006;25(7):680–693. doi: 10.1080/02615470600905895. [DOI] [Google Scholar]
- McCrary JM, Altenmüller E, Kretschmer C, Scholz DS. Association of Music Interventions With Health-Related Quality of Life: A Systematic Review and Meta-analysis. JAMA Network Open. 2022;5:3. doi: 10.1001/jamanetworkopen.2022.3236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFerran KS, Garrido S, Saarikallio S. A critical interpretive synthesis of the literature linking music and adolescent mental health. Youth & Society. 2016;48(4):521–538. doi: 10.1177/0044118X13501343. [DOI] [Google Scholar]
- McFerran KS, Lai HIC, Chang WH, Acquaro D, Chin TC, Stokes H, Crooke AHD. Music, rhythm and trauma: A critical interpretive synthesis of research literature. Frontiers in Psychology. 2020;11:324. doi: 10.3389/fpsyg.2020.00324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFerran K. Handbook of music, adolescents, and wellbeing. Oxford University Press; 2019. [Google Scholar]
- McGrath JJ, Saha S, Al-Hamzawi AO, Alonso J, Andrade L, Borges G, Bromet EJ, Oakley Browne M, Bruffaerts R, Caldas de Almeida JM. Age of onset and lifetime projected risk of psychotic experiences: Cross-national data from the World Mental Health Survey. Schizophrenia Bulletin. 2016;42(4):933–941. doi: 10.1093/schbul/sbw011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillen JC, Raghavan R. Pediatric to adult mental health service use of young people leaving the foster care system. Journal of Adolescent Health. 2009;44(1):7–13. doi: 10.1016/j.jadohealth.2008.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Brown JM, Simpson TL, Handmaker NS, Bien TH, Luckie LF, Montgomery HA, Hester RK, Tonigan JS. What works? Allyn & Bacon; 1995. [Google Scholar]
- Miron O, Yu K-H, Wilf-Miron R, Kohane IS. Suicide rates among adolescents and young adults in the United States, 2000–2017. JAMA. 2019;321(23):2362–2364. doi: 10.1001/jama.2019.5054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogro-Wilson C, Tredinnick L. Influencing social and emotional awareness and empathy with a visual arts and music intervention for adolescents. Children & Schools. 2020;42(2):111–119. doi: 10.1093/cs/cdaa008. [DOI] [Google Scholar]
- Moore KL. Mental health service engagement among underserved minority adolescents and young adults: A systematic review. Journal of Racial and Ethnic Health Disparities. 2018;5(5):1063–1076. doi: 10.1007/s40615-017-0455-9. [DOI] [PubMed] [Google Scholar]
- Mrázová M, Celec P. A systematic review of randomized controlled trials using music therapy for children. The Journal of Alternative and Complementary Medicine. 2010;16(10):1089–1095. doi: 10.1089/acm.2009.0430. [DOI] [PubMed] [Google Scholar]
- Munson MR, Jaccard JJ, Scott LD, Narendorf SC, Moore KL, Jenefsky N, Cole A, Davis M, Gilmer T, Shimizu R, Pleins K, Cooper K, Rodwin AH, Hylek L, Amaro A. Engagement intervention versus treatment as usual for young adults with serious mental illness: a randomized pilot trial. Pilot and Feasibility Studies. 2020;6(1):1–14. doi: 10.1186/s40814-020-00650-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munson MR, Jaccard J, Scott LD, Jr, Moore KL, Narendorf SC, Cole AR, Shimizu R, Rodwin AH, Jenefsky N, Davis M. Outcomes of a metaintervention to improve treatment engagement among young adults with serious mental illnesses: Application of a pilot randomized explanatory design. Journal of Adolescent Health. 2021 doi: 10.1016/j.jadohealth.2021.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munson MR, Jaccard J, Smalling SE, Kim H, Werner JJ, Scott LD., Jr Static, dynamic, integrated, and contextualized: A framework for understanding mental health service utilization among young adults. Social Science & Medicine. 2012;75(8):1441–1449. doi: 10.1016/j.socscimed.2012.05.039. [DOI] [PubMed] [Google Scholar]
- Munson MR, Lox JA. Clinical social work practice with former system youth with mental health needs: Perspective of those in need. Clinical Social Work Journal. 2012;40(2):255–260. doi: 10.1007/s10615-012-0381-6. [DOI] [Google Scholar]
- Munson MR, Narendorf SC, Ben-David S, Cole A, Floersch J. Integrated, overwhelmed, and distanced: Narratives of mental health among young adults with prior public system involvement. Journal of the Society for Social Work and Research. 2018;9(3):413–430. doi: 10.1086/699223. [DOI] [Google Scholar]
- Munson MR, Raghavan R, Shimizu R, Rodwin AH, Jaccard J. Methodologies to advance a “Science of How”: Identifying and engaging intervention targets and outcomes. Psychiatric Services, Appi-Ps. 2022 doi: 10.1176/appi.ps.202100202. [DOI] [PubMed] [Google Scholar]
- Narendorf SC, Munson MR, Ben-David S, Cole AR, Scott LD., Jr Race and gender differences in attitudes toward help seeking among marginalized young adults with mood disorders: A mixed-methods investigation. Psychiatric Rehabilitation Journal. 2018;41(4):277. doi: 10.1037/prj0000312. [DOI] [PubMed] [Google Scholar]
- Narendorf SC, Munson MR, Floersch J. Perspectives on psychotropic medication treatment among young adults formerly served in public systems of care: A thematic and narrative analysis. Journal of the Society for Social Work and Research. 2015;6(1):121–143. doi: 10.1086/680318. [DOI] [Google Scholar]
- National Association of Social Workers. (2021). NASW Code of Ethics (Guide to the Everyday Professional Conduct of Social Workers). National Association of Social Workers. https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Code-of-Ethics-English
- National Institutes of Health. (2018). Sound Health: An NIH-Kennedy Center Partnership [Research Plan]. National Institutes of Health. https://www.nih.gov/sound-health/research-plan.
- National Research Council. (2015). Investing in the health and well-being of young adults. The National Academies Press. 10.17226/18869 [PubMed]
- NeMoyer A, Cruz-Gonzalez M, Alvarez K, Kessler RC, Sampson NA, Green JG, Alegría M. Reducing racial/ethnic disparities in mental health service use among emerging adults: Community-level supply factors. Ethnicity & Health. 2020 doi: 10.1080/13557858.2020.1814999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of the Surgeon General. (2021). Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory. https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf
- Olfson M, Druss BG, Marcus SC. Trends in mental health care among children and adolescents. New England Journal of Medicine. 2015;372(21):2029–2038. doi: 10.1056/NEJMc1507642. [DOI] [PubMed] [Google Scholar]
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papinczak ZE, Dingle GA, Stoyanov SR, Hides L, Zelenko O. Young people's uses of music for well-being. Journal of Youth Studies. 2015;18(9):1119–1134. doi: 10.1080/13676261.2015.1020935. [DOI] [Google Scholar]
- Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: A global public-health challenge. The Lancet. 2007;369(9569):1302–1313. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- Paul M, Ford T, Kramer T, Islam Z, Harley K, Singh SP. Transfers and transitions between child and adult mental health services. The British Journal of Psychiatry. 2013;202(s54):s36–s40. doi: 10.1192/bjp.bp.112.119198. [DOI] [PubMed] [Google Scholar]
- Perkins R, Mason-Bertrand A, Fancourt D, Baxter L, Williamon A. How participatory music engagement supports mental well-being: A meta-ethnography. Qualitative Health Research. 2020;30(12):1924–1940. doi: 10.1177/1049732320944142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry BD. Applying principles of neurodevelopment to clinical work with maltreated and traumatized children: The neurosequential model of therapeutics. In: Webb NB, editor. Working with traumatized youth in child welfare. The Guilford Press; 2006. pp. 27–52. [Google Scholar]
- Perry BD. Examining child maltreatment through a neurodevelopmental lens: Clinical applications of the neurosequential model of therapeutics. Journal of Loss and Trauma. 2009;14(4):240–255. doi: 10.1080/15325020903004350. [DOI] [Google Scholar]
- Perry BD, Winfrey O. What Happened to You?: Conversations on Trauma. Flatiron Books; 2021. [Google Scholar]
- Perry, B., & Dobson, C. (2015). The Neurosequential Model of Therapeutics. In J. Ford & C. Courtois (Eds.), Treating Complex Traumatic Stress Disorders in Children and Adolescents: Scientific Foundations and Therapeutic Models. Guilford Press.
- Pintello D. Commentary: Establishing scientific rigor and excellence in implementation science training to improve the deployment of evidence-based mental health services. Administration of Policy and Mental Health. 2020;47(2):265–271. doi: 10.1007/s10488-020-01014-5. [DOI] [PubMed] [Google Scholar]
- Plener, P. L., Sukale, T., Ludolph, A. G., & Stegemann, T. (2010). ‘‘Stop Cutting—Rock!’’: A Pilot Study of a Music Therapeutic Program for Self-Injuring Adolescents. Music and Medicine, 2(1), 59–65. 10.47513/mmd.v2i1.234
- Polanco-Roman L, Danies A, Anglin DM. Racial discrimination as race-based trauma, coping strategies, and dissociative symptoms among emerging adults. Psychological Trauma: Theory, Research, Practice, and Policy. 2016;8(5):609. doi: 10.1037/tra0000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porges, S. W. (2011). The polyvagal theory: neurophysiological foundations of emotions, attachment, communication, and self-regulation (Norton Series on Interpersonal Neurobiology). WW Norton & Company.
- Porter S, McConnell T, McLaughlin K, Lynn F, Cardwell C, Braiden HJ, Boylan J, Holmes V, Music in Mind Study Group Music therapy for children and adolescents with behavioural and emotional problems: A randomised controlled trial. Journal of Child Psychology and Psychiatry. 2017;58(5):586–594. doi: 10.1111/jcpp.12656. [DOI] [PubMed] [Google Scholar]
- Raghavan R, Munson MR, Le C. Toward an Experimental Therapeutics Approach in Human Services Research. Psychiatric Services. 2019;70(12):1130–1137. doi: 10.1176/appi.ps.201800577. [DOI] [PubMed] [Google Scholar]
- Rickson DJ. Instructional and improvisational models of music therapy with adolescents who have attention deficit hyperactivity disorder (ADHD): A comparison of the effects on motor impulsivity. Journal of Music Therapy. 2006;43(1):39–62. doi: 10.1093/jmt/43.1.39. [DOI] [PubMed] [Google Scholar]
- Rickson DJ, Watkins WG. Music therapy to promote prosocial behaviors in aggressive adolescent boys–a pilot study. Journal of Music Therapy. 2003;40(4):283–301. doi: 10.1093/jmt/40.4.283. [DOI] [PubMed] [Google Scholar]
- Robinson C, Seaman EL, Montgomery L, Winfrey A. A review of hip hop-based interventions for health literacy, health behaviors, and mental health. Journal of Racial and Ethnic Health Disparities. 2018;5(3):468–484. doi: 10.1007/s40615-017-0389-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodwin, A.H., Shimizu, R., Travis, R., James, K., Banya, M., Munson, M.R. (2021). A systematic review of psychosocial interventions using music to improve engagement and mental health outcomes for older adolescents and young adults. PROSPERO, CRD42021202644. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021202644 [DOI] [PMC free article] [PubMed]
- Rogers CR. Client-centered therapy. American Psychological Association; 1966. [Google Scholar]
- Saarikallio S, Gold C, McFerran K. Development and validation of the H ealthy-U nhealthy M usic S cale. Child and Adolescent Mental Health. 2015;20(4):210–217. doi: 10.1111/camh.12109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salerno JP, Williams ND, Gattamorta KA. LGBTQ populations: Psychologically vulnerable communities in the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S239. doi: 10.1037/tra0000837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott LD, McCoy H, Munson MR, Snowden LR, McMillen JC. Cultural mistrust of mental health professionals among black males transitioning from foster care. Journal of Child and Family Studies. 2011;20(5):605–613. doi: 10.1007/s10826-010-9434-z. [DOI] [Google Scholar]
- Scrine E. The limits of resilience and the need for resistance: Articulating the role of music therapy with young people within a shifting trauma paradigm. Frontiers in Psychology. 2021;26:1. doi: 10.3389/fpsyg.2021.600245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuman J, Kennedy H, DeWitt P, Edelblute A, Wamboldt MZ. Group music therapy impacts mood states of adolescents in a psychiatric hospital setting. The Arts in Psychotherapy. 2016;49:50–56. doi: 10.1016/j.aip.2016.05.014. [DOI] [Google Scholar]
- Silverman MJ. Music therapy in mental health for illness management and recovery. Oxford University Press; 2022. [Google Scholar]
- Silverman MJ. Music-based affect regulation and unhealthy music use explain coping strategies in adults with mental health conditions. Community Mental Health Journal. 2020;56(5):939–946. doi: 10.1007/s10597-020-00560-4. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. https://www.samhsa.gov/data
- Tang Q, Huang Z, Zhou H, Ye P. Effects of music therapy on depression: A meta-analysis of randomized controlled trials. PLoS ONE. 2020;15:e0240862. doi: 10.1371/journal.pone.0240862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasley, M. L., McCarter, S., Woo, B., Conner, L. R., Spencer, M. S., & Green, T.. (2021). Eliminate racism (Grand Challenges for Social Work initiative Working Paper No. 26). American Academy of Social Work & Social Welfare. https://grandchallengesforsocialwork.org/wp-content/uploads/2021/05/Eliminate-Racism-Concept-Paper.pdf
- Thaut MH. Music as therapy in early history. Progress in Brain Research. 2015;217:143–158. doi: 10.1016/bs.pbr.2014.11.025. [DOI] [PubMed] [Google Scholar]
- Thomson CJ, Reece JE, Di Benedetto M. The relationship between music-related mood regulation and psychopathology in young people. Musicae Scientiae. 2014;18(2):150–165. doi: 10.1177/1029864914521422. [DOI] [Google Scholar]
- Thomas EC, Snethen G, O’Shea A, Suarez J, Hurford I, Salzer MS. An examination of the community participation interests of young adults with serious mental illnesses. The Journal of Behavioral Health Services & Research. 2020;47(4):526–543. doi: 10.1007/s11414-019-09678-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis, R. (2016). The Healing Power of Hip Hop: Intersections of Race, Ethnicity, and Culture. ABC-CLIO.
- Travis R. All awareness and no action: Can social work leverage creative arts’ potential? Research on Social Work Practice. 2019;29(6):708–720. doi: 10.1177/1049731517735178. [DOI] [Google Scholar]
- Travis R, Jr, Deepak A. Empowerment in context: Lessons from hip-hop culture for social work practice. Journal of Ethnic and Cultural Diversity in Social Work. 2011;20(3):203–222. doi: 10.1080/15313204.2011.594993. [DOI] [Google Scholar]
- Travis R, Rodwin AH, Allcorn A. Hip Hop, empowerment, and clinical practice for homeless adults with severe mental illness. Social Work with Groups. 2019;42(2):83–100. doi: 10.1080/01609513.2018.1486776. [DOI] [Google Scholar]
- Travis R, Gann E, Crooke AH, Jenkins SM. Using Therapeutic Beat Making and lyrics for empowerment. Journal of Social Work. 2021;21(3):551–574. doi: 10.1177/1468017320911346. [DOI] [Google Scholar]
- Travis R, Gann E, Crooke AHD, Jenkins SM. Hip Hop, empowerment, and therapeutic beat-making: Potential solutions for summer learning loss, depression, and anxiety in youth [Article] Journal of Human Behavior in the Social Environment. 2019;29(6):744–765. doi: 10.1080/10911359.2019.1607646. [DOI] [Google Scholar]
- Travis, R., Levy, I. P., & Morphew, A. C. (2022). “Now We’re All Family”: Exploring social and emotional development in a summer hip hop mixtape camp. Child and Adolescent Social Work Journal, 1–18. [DOI] [PMC free article] [PubMed]
- Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. Journal of Abnormal Psychology. 2019;128(3):185. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- Tyson EH. Hip hop therapy: An exploratory study of a rap music intervention with at-risk and delinquent youth. Journal of Poetry Therapy. 2002;15(3):131–144. doi: 10.1023/A:1019795911358. [DOI] [Google Scholar]
- Tyson EH. Rap music in social work practice with African-American and Latino youth: A conceptual model with practical applications. Journal of Human Behavior in the Social Environment. 2004;8(4):1–21. doi: 10.1300/J137v08n04_01. [DOI] [Google Scholar]
- Tyson, E. H., Hall, J. C., & Montero, J. (2016, December 5, 2016). Hip Hop Critical Consciousness Circles and Hip Hop Expressive Arts Therapy: Innovations in Youth Mental Health Coalition for Juvenile Justice National Disproportionate Minority Contact Conference Program, Baltimore, MD. https://www.youtube.com/watch?v=zoqsYscwmt4
- van der Kolk BA. The body keeps the score: Brain, mind, and body in the healing of trauma. Penguin Books; 2015. [Google Scholar]
- Vaughn MG, Howard MO. Adolescent substance abuse treatment: A synthesis of controlled evaluations. Research on Social Work Practice. 2004;14(5):325–335. doi: 10.1177/1049731504265834. [DOI] [Google Scholar]
- Viega M. Exploring the discourse in hip hop and implications for music therapy practice. Music Therapy Perspectives. 2016;34(2):138–146. doi: 10.1093/mtp/miv035. [DOI] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health. 2003;93(2):200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2021). Depression: Key Facts. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/depression
- Wu SM. Effects of Music Therapy on Anxiety, Depression and Self-Esteem of Undergraduates. Psychologia. 2002;45(2):104–114. doi: 10.2117/psysoc.2002.104. [DOI] [Google Scholar]
- Yinger OS, Gooding L. Music therapy and music medicine for children and adolescents. Psychiatric Clinics of North America. 2014;23(3):535–553. doi: 10.1016/j.chc.2013.03.003. [DOI] [PubMed] [Google Scholar]
- Zhao K, Bai ZG, Bo A, Chi I. A systematic review and meta-analysis of music therapy for the older adults with depression. International Journal of Geriatric Psychiatry. 2016;31(11):1188–1198. doi: 10.1002/gps.4494. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.