Abstract
Background
Myocardial strain—change in myocardial fibre length over the cardiac cycle—is a measure of cardiac muscle function. It is obtained using conventional techniques such as echocardiography and magnetic resonance imaging, adding additional clinical information to augment the current techniques.
Methods
A narrative review of the current relevant literature with respect to myocardial strain, with a focus on strain measured by echocardiography.
Results
Myocardial strain identifies global and regional abnormalities in myocardial function and differentiates types of cardiomyopathy. It is an earlier marker of myocardial disease than ejection fraction and is predictive of cardiovascular adverse events. Accurate measurement requires high-quality images and experienced practitioners.
Conclusion
This review explains advantages and disadvantages of myocardial strain imaging and explains why, through adding increased precision without additional burden, it should be a standard part of cardiac assessment.
Keywords: Cardiac imaging, Cardio-oncology, Echocardiography, Myocardial strain
Introduction
Modern medical practice requires cardiac imaging that is precise and safe. The ideal technique is minimally invasive, low cost, easily repeatable, and reproducible, without irradiation or interobserver variability [1]. The key parameter for cardiac function is left ventricular ejection fraction (LVEF). The most appropriate technique depends on the clinical situation. The gold standard is cardiac magnetic resonance imaging (CMRI) [2, 3]. It is highly accurate and reproducible and can assess both structure and function. It can be particularly useful to characterise the ventricular myocardium to determine the aetiology of a reduced LVEF [4]. However, it is expensive, time-consuming, and not widely available in clinical practice. Allergies to contrast agents can also be an issue, particularly for patients undergoing repeated studies [4].
Multi-gated acquisition scanning (MUGA) is common and precisely estimates LVEF with little interobserver variability. However, it provides limited information on other important aspects of cardiac function like heart structure and diastolic function [1]. MUGA is expensive and time-consuming with ionising radiation exposure. This makes it inappropriate for repeat tests. It requires specialised staff and equipment. There can be difficulty accessing optimal image acquisition angles and syncing electrocardiograph (ECG) gating in arrhythmias [5]. The usage is in decline [6].
The most widely available and commonly used technique is echocardiography (echo). It is widely available, non-invasive, versatile, and inexpensive with minimal patient discomfort [7]. It gives information on systolic and diastolic heart function and muscle movement. In addition to left and right ventricular function, pericardial and valvular function and ventricular wall mechanics can be recorded [5]. There is no radiation, and contraindications are few. Several consensus documents recommend echo monitoring for patients on cardiotoxic chemotherapy, with CMRI recommended as a second line if echoes are of poor quality [4, 8].
There are inherent limitations nevertheless on how echo assesses heart structure and calculates LVEF. It depends on the assumption that the left ventricle is symmetrical and on reliable visualisation of endocardial borders. LVEF itself also has major drawbacks. It rarely declines to a measurable level until after a critical amount of irreversible myocardial damage [9]. Those with high-grade myocellular injury on biopsy may not have marked LVEF changes [4].
Intra- and interobserver variability, changes in machines and algorithms, and (because LVEF is a dynamic function) dependency on heart rate and load can cause difficulty measuring LVEF serially. Better techniques are needed to mitigate these limitations, improve accuracy, and maintain accessible, low cost, and time-efficient cardiac assessment. The measurement of myocardial strain by 2D and 3D speckle tracking echo can accomplish this with earlier detection of more subtle myocardial function abnormalities than standard echo. While strain can also be measured on CMRI, this review focuses mainly on echo due to its predominance in the clinical setting.
Myocardial strain
Myocardial Strain (strain) is a dimensionless index of total ventricular myocardial deformation in a cardiac cycle (as a percentage). It uses ultrasound wave frequency shifts to calculate fractional change in length of part of the myocardium compared to its original length [10]. Strain rate is the rate of deformation (or stretch). Systolic strain measures the percentage change in myocardial fibre length in multiple directions during left ventricular contraction—usually at ventricular end systole (aortic valve closure) [11].
Myocardial deformation can be circumferential, longitudinal, or radial and the three strains interrelate (Fig. 1). Each is relative, a change in length over time. Myocardial fibres change orientation gradually from a counterclockwise helix (subendocardium) to clockwise in the subepicardium. During the cardiac cycle, the LV deforms in multiple directions: it shortens longitudinally and circumferentially but thickens radially [11]. There is also shear deformation—from the opposing rotation at the LV base and apex—manifested as a ‘twist’.
Longitudinal strain is dominant in systolic strain [11]. It usually has a negative value due to shorter longitudinal fibres.
Circumferential strain measures myocardial wall shortening from inward movement of the overall endocardial circumference. This would still occur even without circumferential fibres. In practice, it measures myocardial diameter reduction as the wall thickens. The thickening relates to wall shortening; heart muscle is not compressible.
Radial strain is in the direction of the ultrasound beam and is really transmural strain (as there are no radial fibres). It is the sum of both subepicardial and subendocardial radial deformations [11].
Fig. 1.

Directions of myocardial strain. Myocardial strain can be longitudinal (1), circumferential (2), and radial (3). Created in BioRender.com
Longitudinal LV mechanics are most sensitive to myocardial disease and predominantly governed by the subendocardium. In early disease, circumferential strain and twist may remain normal as midmyocardial and epicardial function compensate to preserve LV systolic performance [12]. As disease progresses, or after transmural damage, concomitant midmyocardial and subepicardial dysfunction will reduce LV circumferential and twist mechanics and lower LVEF.
Strain can be calculated by standard 2D echo, when images are of appropriate quality, with a high frame rate (50–80 frames/second) to maximise spatial resolution but maintain sensitivity to motion and change [11, 13, 14]. This information is additional to that from conventional echo, during the same intervention, and can mitigate some limitations. CMRI can visualise any desired plane, without limitations on acoustic windows [2]. Longitudinal strain is derived from horizontal and vertical long-axis cines, while circumferential strain is derived from short axis cines. In both cases, results are calculated by software-specific algorithms.
Strain accurately describes contraction/relaxation because it measures myocardial deformation directly [10], global right and left ventricular function, and regional wall deformation. Although it requires specialised equipment, software, expertise, and time, there is no increased patient burden beyond routine echo or CMRI. It is sensitive to subclinical LV systolic function deterioration, with a decrease in strain detectable before overt LVEF change [15]. It can also predict future EF decline [9].
Methods of measurement
The choice of instrument influences myocardial strain utility (see Table 1). Strain was first measured by tissue Doppler imaging (TDI), which uses Doppler to analyse myocardial motion at one point relative to another [16]. To ensure accuracy, TDI-based analysis requires data acquisition for each myocardial segment, with high frame rates and high-quality images. It is angle-dependent, as the walls must be aligned with the Doppler beam. Significant expertise is required for proper interpretation, as there is considerable inter- and intraobserver variability [15]. These factors limit use to specialist cardiology, so it is no longer the method of choice.
Table 1.
Advantages and disadvantages of echocardiographic methods for tissue tracking
| Strain modality | Advantages | Disadvantages |
|---|---|---|
| TDI |
Requires frame rates > 100/s Useful for longitudinal deformation |
Extremely angle dependent Unsuitable for radial/circumferential deformation |
| 2D-STE |
Relatively cheap Portable/bedside test Less angle dependent Allows tracking throughout the cardiac cycle Measures all directions |
Proximal speckle tracking > distal Depends on ultrasound quality Measures one direction at a time Some angle dependence Variability in methods and normal values from hardware and software differences |
| 3D-STE | Simultaneous assessment of deformation in all directions |
Depends on ultrasound quality Limited spatiotemporal resolution Complex offline image processing |
Adapted from Omar and Sengupta 2018 [11]
*TDI tissue Doppler imaging, 2D-STE two-dimensional speckle tracking echocardiography, 3D-STE three-dimensional speckle tracking echocardiography
Speckle tracking echocardiography (STE) tracks natural acoustic reflectors (‘speckles’) within the myocardium from frame to frame to determine both deformation (strain) and deformation speed (strain rate) [5]. This allows measurement of longitudinal, circumferential, and radial strain in multiple segments and rotational parameters. It can be obtained by standard 2D images and 3D echo (Fig. 2) [2]. The reproducibility is superior to TDI-based analysis, and better for longitudinal than radial strain [15]. As speckle tracking is semi-automated, analysis is also faster than TDI.
Fig. 2.
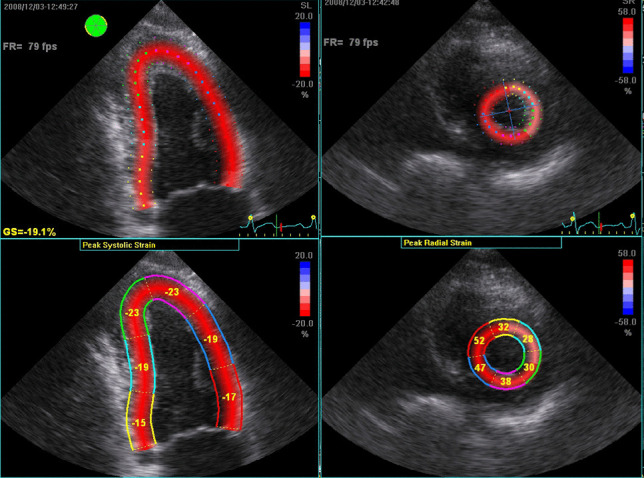
Images shows two-dimensional speckle tracking-derived strain, measured using EchoPac™ (GE Healthcare, Norway) software. Left image shows longitudinal strain on an apical four chamber view. Right image shows radial strain at the level of the papillary muscle. Strain is calculated over each of six standard segments, which are colour-coded (bottom left and right), and then averaged to a global score
The accuracy of STE depends on 2D image quality and frame rates. Low frame rates produce unstable speckle patterns, while high rates reduce image resolution [12]. Artefacts that resemble speckle patterns must be avoided as they impair tracking quality, so interpretative expertise is important [11]. Speckles are recorded more clearly parallel to the sonography angle so apical views are best for longitudinal deformation and the parasternal short axis for circumferential and radial deformation.
There are a number of techniques to calculate strain on CMRI, with the most common being tissue tagging. Different myocardial regions are ‘tagged’ magnetically. The movement of these tags during contraction allows direct measurement of myocardial deformation. An alternative technique is feature tracking using artificial intelligence (AI) algorithm processing. Regions of interest are tracked during post-processing after identification of myocardial boundaries, in a process similar to STE [2].
Clinical utility
Global longitudinal strain (GLS), which measures myocardial shortening of the left ventricular segments from base to apex, is most reliable and clinically relevant for early reductions in myocardial function [17]. It correlates better with CMRI than 2D echo [13]. The prediction of cardiovascular events is more reliable by GLS than LVEF (hazard ratio 1.45 versus 1.23 for LVEF over clinical variables alone) [16]. It is independently associated with all-cause mortality and a composite measure of cardiovascular events (arrhythmia, death, or heart failure hospitalisation) [13, 18]. While it does not replace EF, there is a strong view that all transthoracic echo reports should add GLS to conventional parameters [14, 18].
For myocardial strain to be clinically useful, normal ranges of strain and strain rate in healthy populations are needed, notwithstanding varied methodology and machines. Normal longitudinal systolic strain in most segments varies from − 16 to − 22% [11, 19]. A meta-analysis found a pooled mean normal GLS of − 19.7% (95% confidence interval: − 20.4 to − 18.9%) [15, 20]. Based on this, it has been suggested that − 18.9% be the cut off, with more positive values (i.e. closer to zero) considered abnormal [21]. A global radial strain normal mean of 47.3% (95% CI 43.6–51%), with a range of 35–59%, has been reported [15, 19]. Normal resting longitudinal strain rates vary from 1.0/second (s) to 1.4/s (Standard deviation: 0.5/s to 0.6/s).
Strain is influenced by preload (it increases as LV size increases) and afterload (decreases as blood pressure rises). Strain rate seems less dependent on load than strain. Strain and strain rate vary with age, gender, and race [22]. Strain is consistently higher in females than males and in younger age groups than older (Table 2). The HUNT study (Table 2a) provided age- and gender-specific reference values for longitudinal strain and strain rate from 1266 healthy Norwegian individuals [23]. The JUSTICE study (Table 2b) compared three different strain software packages in 817 healthy Japanese subjects [24].
Table 2.
Above (2a): Systolic strain normal values by age and gender (HUNT study [23]); values considered abnormal if > 2 standard deviations (SD) from the mean. Below (2b): Global Longitudinal Strain (GLS) normal values (%, SD) by vendor, age, and gender (JUSTICE study
[24])
| Age (years) | End systolic strain (%, SD) | Peak systolic strain rate (s−1, SD) | ||||||
|---|---|---|---|---|---|---|---|---|
| Female | Male | Female | Male | |||||
| < 40 | − 17.9 (2.1) | − 16.8 (2.0) | − 1.09 (0.28) | − 1.01 (0.13) | ||||
| 40–60 | − 17.6 (2.1) | − 18.8 (2.2) | − 1.06 (0.13) | − 1.01 (0.12) | ||||
| > 60 | − 15.9 (2.4) | − 15.5 (2.4) | − 0.97 (0.14) | − 0.97 (0.14) | ||||
| Overall | − 17.4 (2.3) | − 15.9 (2.3) | − 1.05 (0.13) | 1.01 (0.13) | ||||
| Age (years) | GLS: Vivid 7 (GE Healthcare) | GLS: iE33 (Philips) | ||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | Overall | Male | Female | Overall | |||
| 0–19 | − 21.7 (3.1) | − 22.4 (1.6) | − 22.1 (2.4) | − 19.4 (2.7) | − 20.5 (2.2) | − 19.9 (2.5) | ||
| 20–29 | − 20.9 (1.9) | − 22.3 (1.6) | − 21.2 (1.9) | − 18.8 (2.0) | − 20.6 (2.3) | − 19.0 (2.1) | ||
| 30–39 | − 20.6 (1.9) | − 22.8 (1.8) | − 21.1 (2.1) | − 19.1 (2.3) | − 20.2 (2.0) | − 19.5 (2.2) | ||
| 40–49 | − 20.9 (1.8) | − 22.6 (2.1) | − 21.4 (2.0) | − 17.9 (2.8) | − 19.3 (0.9) | − 18.2 (2.5) | ||
| 50–59 | − 21.0 (1.9) | − 23.3 (1.9) | − 21.0 (2.2) | − 16.9 (2.3) | − 20.4 (1.5) | − 17.6 (2.5) | ||
| ≥ 60 | − 19.7 (1.4) | − 20.9 (2.1) | − 20.3 (1.9) | − 15.8 (1.4) | − 17.3 (2.3) | − 16.7 (2.1) | ||
Utility in cardiac disease
Deformation imaging is useful in early myocardial disease. Reductions in strain and strain rate precede overall EF reduction, particularly with thickened myocardial walls or small ventricular cavities [16]. In ischaemia, the subendocardial layer is most susceptible to damage, which may be subclinical. Regional longitudinal strain is proportionately significantly reduced after myocardial infarction, within the infarcted area [12]. GLS can identify mild systolic dysfunction not reflected in reduced EF.
Deformation imaging can also identify covert left ventricular dysfunction in cardiomyopathy before conventional methods. Hypertrophic cardiomyopathy is characterised by mutations in sarcomere-related genes that cause myofibril disarray and myocardial hypertrophy [19]. In hypertrophy, including hypertrophic cardiomyopathy, conventional echo may overestimate EF as normal or ‘supernormal’ because wall thickness reduces cavity volumes. Strain and strain rate imaging are superior as they measure dynamic cardiac wall change. They can distinguish myocardial from pericardial pathology, cardiac amyloidosis from other cardiomyopathies, and constrictive pericarditis from restrictive cardiomyopathy (Table 3). Strain can improve prognostication in cardiomyopathies, ischaemic, and valvular heart disease. One standard deviation change in GLS was a stronger predictor of all-cause mortality than the same change in LVEF [13]. In impaired LVEF, GLS and LVEF have a linear relationship—GLS − 11% corresponds to LVEF 35%—whereas with normal LVEF, the relationship is curvilinear. So GLS is of greatest advantage to identify subclinical myocardial dysfunction, before LVEF declines [16].
Table 3.
Myocardial deformation in cardiovascular disease
| GLS | GRS | GCS | |
|---|---|---|---|
| Aortic stenosis | ▼ | ▼ | Normal or ▲ |
| Cardiac risk factor-induced subclinical myocardial dysfunction | ▼ | ▼ | Normal or ▲ |
| Constrictive pericarditis | Normal | Normal | ▼ |
| Dilated cardiomyopathy | ▼ | ▼ | ▼ |
| Heart failure preserved ejection fraction | ▼ | ▼ | Normal or ▲ |
| Heart failure reduced ejection fraction | ▼ | ▼ | ▼ |
| Hypertrophic cardiomyopathy | ▼ | ▼ | Normal or ▲ |
| Ischaemic heart disease | ▼ | ▼ | Normal or ▲ |
| Mitral regurgitation | ▼ | ▼ | Normal or ▲ |
| Restrictive cardiomyopathy | ▼ | ▼ | ▼ |
Adapted from Omar and Sengupta 2018 [11]
*GLS global longitudinal strain, GRS global radial strain, GCS global circumferential strain
Utility in cardio-oncology
Cardiotoxicity of many cancer therapeutic options, including chemotherapy and thoracic radiotherapy, has increased interest in cardiac screening techniques which are acceptable, accurate, reproducible, and safe. Numerous studies on potentially cardiotoxic chemotherapies have shown reductions in myocardial strain before discernible change in EF, which may predict LV dysfunction. A study in breast cancer demonstrated that an 11% relative reduction (95% confidence interval 8.3–14.6%) in GLS during trastuzumab therapy was the strongest predictor of subsequent EF reduction; sensitivity = 65%, specificity = 94% [25]. The American Society of Echocardiography (ASE) and European Association of Cardiovascular Imaging (EACVI) consensus states that a relative percentage reduction in global longitudinal strain > 15% is very likely to be abnormal, whereas < 8% appears to be of no clinical significance [3].
Repeated studies to observe within-patient change provide more robust evidence of clinically significant change in cardiac function and can monitor cardiotoxicity during chemotherapy [19]. A comprehensive review of over 30 studies reported that early change in strain (10–15%) has the best specificity for subclinical dysfunction and subsequent heart failure or reduced EF [16, 19]. Absolute GLS values are also prognostic— GLS > − 17.5% independently predicts cardiotoxicity from low-dose anthracyclines with 67% sensitivity and 97% specificity [26]. GLS ≥ − 16% 3 months into treatment predicts future cardiotoxicity (sensitivity = 80%; specificity = 90%), with negative predictive value of future cancer treatment-related cardiac dysfunction (CTRCD) = 92%. The consensus supported routine clinical use of 2D GLS in serial monitoring of chemotherapy-induced cardiotoxicity [16].
Cancer itself is a significant predictor of reduced strain, even after adjustment for age, sex, and cardiovascular risk factors. This is consistent across different cancer sites, which suggests a common mechanism of dysfunction [27, 28]. There is little information on myocardial strain in untreated cancer patients [17]. A study of 122 patients with solid tumours referred for cardiac assessment pre-chemotherapy demonstrated markedly reduced longitudinal, circumferential, and radial strain compared to controls (non-cancer patients referred for cardiac assessment) [28].
The SUCCOUR trial was the first randomised controlled trial to base treatment on GLS, rather than LVEF [29]. It offers some support for GLS for surveillance of CTRCD [26, 30]. At the 1-year follow-up, more patients got cardioprotective therapy in the GLS arm and fewer met the definition of CTRCD. Although there was no statistical difference in LVEF change in the two trial arms, when the subgroup which received cardioprotective therapy was assessed, those in the GLS-guided arm had significantly lower reductions in LVEF [30, 31]. As yet, there is insufficient evidence to support delaying or withholding cancer treatment based on strain measurements, but any changes should prompt a thorough cardiovascular assessment including imaging and cardiology review.
Utility in healthy populations
It is important that screening techniques avoid burden and toxicity in healthy adults. The information from deformation imaging, additional to conventional echo, could avoid more invasive techniques.
Peak systolic strain of the septal and lateral walls, and radial strain, are significantly higher in elite athletes than comparative healthy controls, while right ventricular (RV) deformation parameters are reduced. However, RV functional reserve is normal in elite endurance athletes, despite lower deformation measures at rest, which highlights the ambiguities between physiologic RV remodelling and pathology [32, 33]. The comparable RV contractile reserve for elite and non-elite athletes suggests that lower resting RV reserve values in elite athletes may represent physiologic changes rather than subclinical myocardial damage.
Cardiac injury is frequently observed in COVID-19 and is associated with higher mortality. A meta-analysis revealed that lower LV-GLS and RV-LS are independently associated with poor COVID-19 outcomes [34]. Hence, routine echocardiography is reasonable and might be useful in people hospitalised with COVID-19.
Limitations of myocardial strain
Strain varies depending on preload, afterload, and heart rate [19]. Interobserver variability is 5.4–8.6% and intraobserver variability 4.9–7.8%. This is comparable with other echocardiographic parameters like EF. It has a substantial learning curve, and accurate reporting relies on multiple technical considerations [16, 21, 24]. To mitigate subjectivity, optimisation of image acquisition parameters is vital to ensure adequate image quality. Extra time (up to 5 min per person) may be required for image analysis, which cumulatively may contribute burden in busy clinical settings [16]. Future software developments will shorten this process. CMRI also requires dedicated acquisition sequences, and time-consuming image post-processing, although report generation can be automated, in settings where this is available [2].
Studies conducted using different echo machine brands are not directly comparable, and there is a high intervendor variability in published norms (Table 2b). Analytic software for raw image analysis is vendor specific [14]. Some discordant results are from differences in image post-processing algorithms, including extent of the myocardial wall included [35]. Tracking can be at the endocardial, mid-muscular, or epicardial border or the full thickness mid-myocardial wall [11, 14]. This disparity has decreased considerably after development of the EACVI consensus [36]. Algorithms can also differ in CMRI analysis, so the specific software used for analysis should be reported in each case [37]. Standardisation, and use of CMRI feature tracking, should also be used.
Serial measurements on individuals, and in research studies, should always be done with the same vendor machine and software, ideally by the same operator [11]. Despite these challenges, GLS has proven to be more reliable and precise than EF in LV function follow-up by multiple observers [26]. Superior temporal and spatial resolution in 3D speckle tracking could circumvent some 2D imaging limitations (Table 1) [12].
Summary
The most appropriate technique to measure cardiac parameters depends on the clinical situation. Modalities which are reproducible, radiation-free, and provide additional clinical information are preferable [38]. GLS is robust for routine clinical application with higher reproducibility than LVEF. It can better define prognosis, particularly when LVEF is normal or almost normal, and thus more appropriately guide management of cardiac disease. It is valuable in assessment of all cardiac patients [16]. Detection of subclinical strain abnormalities can lead to treatment before cardiovascular symptoms develop and prevention of irreversible myocardial damage.
Like all techniques, strain has drawbacks. However, the advantages are evident. Within-patient change may be more valuable than population-based absolute cut-off values. Given the growing recognition of the importance of strain imaging, echo or CMRI should be favoured over MUGA scans [27]. Through increased precision, without additional burden, strain has a clear and vital role in clinical practice and should be routinely incorporated into standard practice [26].
Author contribution
Bernadette Brady conceived of the review, performed the literature review, and drafted the initial manuscript. Gerard King provided data analysis for Fig. 2. All authors critically revised the manuscript and approved the final version. Bernadette Brady is responsible for the overall manuscript.
Declarations
Ethics approval
Ethics approval was not required for this narrative review.
Competing interests
The authors declare no competing interests.
Footnotes
Key messages
• Left ventricular ejection fraction measures systolic cardiac function. However, it does not become abnormal until a substantial amount of myocardial dysfunction is present.
• Myocardial strain can provide increased precision in cardiac assessment without additional burden as it can be measured using standard imaging techniques. It can identify myocardial dysfunction at an earlier stage than ejection fraction.
• Myocardial strain has clinical utility in cardiac disease, cardio-oncology and in screening of healthy populations.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bernadette Brady, Email: bbrady@olh.ie.
Gerard King, Email: gking@stjames.ie.
Ross T. Murphy, Email: rtmurphy@stjames.ie
Declan Walsh, Email: declan.walsh@atriumhealth.org.
References
- 1.Colombo A, Cardinale D. Using cardiac biomarkers and treating cardiotoxicity in cancer. Future Cardiol. 2013;9(1):105–118. doi: 10.2217/fca.12.73. [DOI] [PubMed] [Google Scholar]
- 2.Burrage MK, Ferreira VM. The use of cardiovascular magnetic resonance as an early non-invasive biomarker for cardiotoxicity in cardio-oncology. Cardiovasc Diagn Ther. 2020;10(3):610–624. doi: 10.21037/cdt-20-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Plana JC, Galderisi M, Barac A, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014;27(9):911–939. doi: 10.1016/j.echo.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Jordan JH, Todd RM, Vasu S, et al. Cardiovascular magnetic resonance in the oncology patient. JACC Cardiovasc Imaging. 2018;11(8):1150–1172. doi: 10.1016/j.jcmg.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garg V, Vorobiof G. Echocardiography and alternative cardiac imaging strategies for long-term cardiotoxicity surveillance of cancer survivors treated with chemotherapy and/or radiation exposure. Curr Oncol Rep. 2016;18(8):52. doi: 10.1007/s11912-016-0532-y. [DOI] [PubMed] [Google Scholar]
- 6.Kolla BC, Roy SS, Duval S, et al. Cardiac imaging methods for chemotherapy-related cardiotoxicity screening and related radiation exposure: current practice and trends. Anticancer Res. 2017;37(5):2445–2449. doi: 10.21873/anticanres.11584. [DOI] [PubMed] [Google Scholar]
- 7.Bulten BF, Mavinkurve-Groothuis AM, de Geus-Oei LF, et al. Early myocardial deformation abnormalities in breast cancer survivors. Breast Cancer Res Treat. 2014;146(1):127–135. doi: 10.1007/s10549-014-2997-4. [DOI] [PubMed] [Google Scholar]
- 8.Plana JC, Thavendiranathan P, Bucciarelli-Ducci C, et al. Multi-modality imaging in the assessment of cardiovascular toxicity in the cancer patient. JACC Cardiovasc Imaging. 2018;11(8):1173–1186. doi: 10.1016/j.jcmg.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Rhea IB, Uppuluri S, Sawada S, et al. Incremental prognostic value of echocardiographic strain and its association with mortality in cancer patients. J Am Soc Echocardiogr. 2015;28(6):667–673. doi: 10.1016/j.echo.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Baur LH. Strain and strain rate imaging: a promising tool for evaluation of ventricular function. Int J Cardiovasc Imaging. 2008;24(5):493–494. doi: 10.1007/s10554-008-9301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Omar AMS, Sengupta PP (2018) Myocardial deformation imaging. Echocardiography 129–57
- 12.Geyer H, Caracciolo G, Abe H et al (2010) Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr 23(4):351–69; quiz 453–5. 10.1016/j.echo.2010.02.015 (published Online First: 2010/04/07) [DOI] [PubMed]
- 13.Kalam K, Otahal P, Marwick TH. Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart. 2014;100(21):1673–1680. doi: 10.1136/heartjnl-2014-305538. [DOI] [PubMed] [Google Scholar]
- 14.Kisslo J, Forsha D, Romano MMD et al (2018) Strain basics and global longitudinal strain. Echocardiography 845–66
- 15.Thavendiranathan P, Poulin F, Lim KD et al (2014) Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol 63(25 Pt A):2751–68. 10.1016/j.jacc.2014.01.073 (published Online First: 2014/04/08) [DOI] [PubMed]
- 16.Luis SA, Chan J, Pellikka PA. Echocardiographic assessment of left ventricular systolic function: an overview of contemporary techniques, including speckle-tracking echocardiography. Mayo Clin Proc. 2019;94(1):125–138. doi: 10.1016/j.mayocp.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 17.Venneri L, Khattar RS. Cancer and myocardial dysfunction: is there a link? Expert Rev Cardiovasc Ther. 2016;14(11):1207–1209. doi: 10.1080/14779072.2016.1226129. [DOI] [PubMed] [Google Scholar]
- 18.Szymanski C, Lévy F, Tribouilloy C. Should LVEF be replaced by global longitudinal strain? Heart. 2014;100(21):1655–1656. doi: 10.1136/heartjnl-2014-305538. [DOI] [PubMed] [Google Scholar]
- 19.Fava AM, Meredith D, Desai MY. Clinical applications of echo strain imaging: a current appraisal. Curr Treat Options Cardiovasc Med. 2019;21(10):50. doi: 10.1007/s11936-019-0761-0. [DOI] [PubMed] [Google Scholar]
- 20.Yingchoncharoen T, Agarwal S, Popović ZB, et al. Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr. 2013;26(2):185–191. doi: 10.1016/j.echo.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Abdel-Qadir H, Amir E, Thavendiranathan P. The use of myocardial strain and newer echocardiography imaging techniques in cancer patients. Future Oncol. 2015;11(14):2035–2041. doi: 10.2217/fon.15.122. [DOI] [PubMed] [Google Scholar]
- 22.Collier P, Phelan D, Klein A. A test in context: myocardial strain measured by speckle-tracking echocardiography. J Am Coll Cardiol. 2017;69(8):1043–1056. doi: 10.1016/j.jacc.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 23.Dalen H, Thorstensen A, Aase SA, et al. Segmental and global longitudinal strain and strain rate based on echocardiography of 1266 healthy individuals: the HUNT study in Norway. Eur J Echocardiogr. 2010;11(2):176–183. doi: 10.1093/ejechocard/jep194. [DOI] [PubMed] [Google Scholar]
- 24.Takigiku K, Takeuchi M, Izumi C, et al. Normal range of left ventricular 2-dimensional strain: Japanese ultrasound speckle tracking of the left ventricle (JUSTICE) study. Circ J. 2012;76(11):2623–2632. doi: 10.1253/circj.CJ-12-0264. [DOI] [PubMed] [Google Scholar]
- 25.Negishi K, Negishi T, Hare JL, et al. Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr. 2013;26(5):493–498. doi: 10.1016/j.echo.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 26.McGregor PC, Moura FA, Banchs J, et al. Role of myocardial strain imaging in surveillance and management of cancer therapeutics-related cardiac dysfunction: a systematic review. Echocardiography. 2020 doi: 10.1111/echo.14944. [DOI] [PubMed] [Google Scholar]
- 27.Kirkham AA, Pituskin E, Paterson DI. Does cancer affect cardiac function prior to cancer therapy exposure? Can J Cardiol. 2018;34(3):234–235. doi: 10.1016/j.cjca.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 28.Tadic M, Genger M, Baudisch A, et al. Left ventricular strain in chemotherapy-naive and radiotherapy-naive patients with cancer. Can J Cardiol. 2018;34(3):281–287. doi: 10.1016/j.cjca.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 29.Negishi T, Thavendiranathan P, Negishi K, et al. Rationale and design of the strain surveillance of chemotherapy for improving cardiovascular outcomes: The SUCCOUR trial. JACC Cardiovasc Imaging. 2018;11(8):1098–1105. doi: 10.1016/j.jcmg.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 30.Cocco LD, Chiaparini AF, Saffi MAL, et al. Global longitudinal strain for the early detection of chemotherapy-induced cardiotoxicity: a systematic review and meta-analysis. Clin Oncol (R Coll Radiol) 2022;34(8):514–525. doi: 10.1016/j.clon.2022.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Thavendiranathan P, Negishi T, Somerset E, et al. Strain-guided management of potentially cardiotoxic cancer therapy. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.11.020. [DOI] [PubMed] [Google Scholar]
- 32.King G, Almuntaser I, Murphy RT et al (2013) Reduced right ventricular myocardial strain in the elite athlete may not be a consequence of myocardial damage. “Cream Masquerades as Skimmed Milk”. Echocardiography 30(8):929–35. 10.1111/echo.12153 [DOI] [PubMed]
- 33.La Gerche A, Burns AT, D’Hooge J, et al. Exercise strain rate imaging demonstrates normal right ventricular contractile reserve and clarifies ambiguous resting measures in endurance athletes. J Am Soc Echocardiogr. 2012;25(3):253–62.e1. doi: 10.1016/j.echo.2011.11.023. [DOI] [PubMed] [Google Scholar]
- 34.Wibowo A, Pranata R, Astuti A, et al. Left and right ventricular longitudinal strains are associated with poor outcome in COVID-19: a systematic review and meta-analysis. J Intensive Care. 2021;9(1):9. doi: 10.1186/s40560-020-00519-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Collier P, Koneru S, Tamarappoo B, et al. Strain imaging to detect cancer therapeutics-related cardiac dysfunction: are we there yet? Future Cardiol. 2015;11(4):401–405. doi: 10.2217/FCA.15.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Voigt JU, Pedrizzetti G, Lysyansky P, et al. Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2015;16(1):1–11. doi: 10.1093/ehjci/jeu184. [DOI] [PubMed] [Google Scholar]
- 37.Zange L, Muehlberg F, Blaszczyk E, et al. Quantification in cardiovascular magnetic resonance: agreement of software from three different vendors on assessment of left ventricular function, 2D flow and parametric mapping. J Cardiovasc Magn Reson. 2019;21(1):12. doi: 10.1186/s12968-019-0522-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zamorano JL, Lancellotti P, Rodriguez Munoz D, et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: the task force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC) Eur Heart J. 2016;37(36):2768–2801. doi: 10.1093/eurheartj/ehw211. [DOI] [PubMed] [Google Scholar]


