Abstract
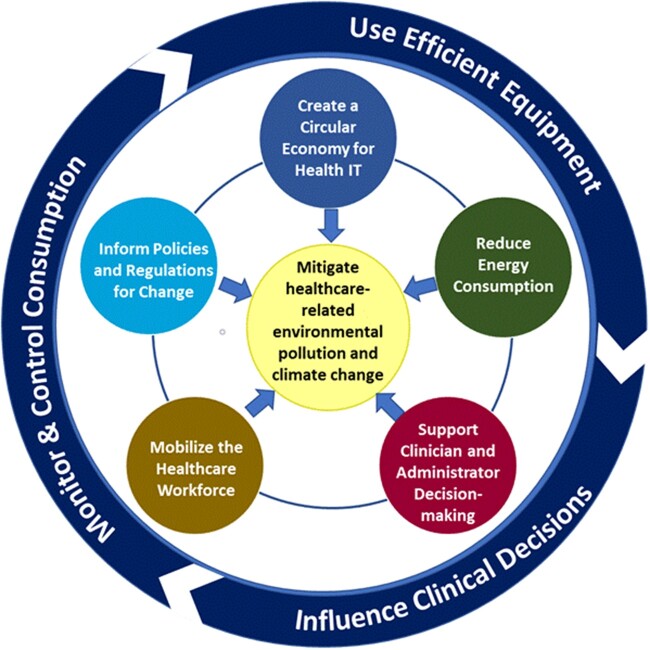
Addressing environmental pollution and climate change is one of the biggest sociotechnical challenges of our time. While information technology has led to improvements in healthcare, it has also contributed to increased energy usage, destructive natural resource extraction, piles of e-waste, and increased greenhouse gases. We introduce a framework “Information technology-enabled Clinical cLimate InforMAtics acTions for the Environment” (i-CLIMATE) to illustrate how clinical informatics can help reduce healthcare’s environmental pollution and climate-related impacts using 5 actionable components: (1) create a circular economy for health IT, (2) reduce energy consumption through smarter use of health IT, (3) support more environmentally friendly decision-making by clinicians and health administrators, (4) mobilize healthcare workforce environmental stewardship through informatics, and (5) Inform policies and regulations for change. We define Clinical Climate Informatics as a field that applies data, information, and knowledge management principles to operationalize components of the i-CLIMATE Framework.
Keywords: climate change, electronic health records, clinical climate informatics, medical informatics, i-CLIMATE
INTRODUCTION
Addressing environmental pollution, climate change, and ultimately the sustainability of our planet as we know it represents one of the biggest sociotechnical challenges of our time.1 Tremendous improvements in technology and specifically information technology over the past 60 years have led to global progress in nearly all sectors and industries of our modern economy. In the healthcare sector, improvements in healthcare delivery have been enabled by electronic health records (EHRs) and the development of large, centralized medical centers. However, many of these same improvements have also contributed to increased energy usage,2 destructive natural resource extraction,3 piles of electronic waste (e-waste),4 unsustainable increases in greenhouse gas emissions (GHGs),5 and global warming. US healthcare contributes 8.5% of national greenhouse gases that, along with similar fractions of harmful air pollutants, cause indirect harm similar in magnitude to medical errors.6 Reducing healthcare pollution is, therefore, a social, moral, professional, and economic imperative.7
Health information technology (IT) tools and applications, specifically the EHR, are now an integral part of healthcare delivery and can be used to support decarbonization efforts (ie, reducing the release of greenhouse gases into the atmosphere), reductions in electronic and plastic waste, and increased environmental sustainability (ie, meeting the needs of the present while maintaining ecological balance and not compromising the needs of the future).8 But, EHR-related hardware and software also introduce challenges such as increased natural resource extraction, energy consumption, e-waste, and manufactured obsolescence.9 Returning to paper-based medical record-keeping systems is not an option, from either a healthcare quality, patient safety, or environmental sustainability perspective. Health IT must be used intelligently and to its fullest capacity to ensure safe, effective, high-quality patient care, while also helping address healthcare-related environmental pollution and climate change.
GUIDING PRINCIPLES FOR A CLINICAL INFORMATICS-CENTRIC APPROACH TO REDUCE ENVIRONMENTAL POLLUTION FROM HEALTHCARE
We propose 3 principles that should guide an informatics-centric approach to how information technology can and should be used to reduce healthcare’s carbon emissions and electronic waste and promote sustainability. These principles are based on expert opinions of the authors gained from previous health IT10 and environmental sustainability work,11 a review of the literature, participation in national [JDS, MJE, AD, HS] and international [JDS, MJE] groups focused on improving the sustainability of healthcare, and conversations among the multidisciplinary group of authors who are experienced in healthcare informatics [DFS, AD, HS], information technology management [AD], clinical medicine [JDS, HS], and environmental sustainability and engineering [JDS, MJE].
First, IT and healthcare-related equipment and software should be optimized to directly reduce their energy and material consumption.12 For example, smart automation that allows powering down or turning off equipment or devices that are not expected to be in service can reduce electricity use, as can procuring more energy-efficient equipment.13 Further, many computing devices are replaced on a schedule that does not necessarily reflect their useful lifespan. Increasing the length of time devices are used before they are replaced can reduce both the materials and energy required to manufacture IT equipment as well as e-waste that must be managed.14 Second, computing technology should help quantify, control, and monitor energy usage, resource consumption, and waste in the building infrastructure and services that support various aspects of the healthcare delivery enterprise, such as heating, ventilation, air-conditioning (HVAC), and lighting.15 Third, health IT and especially EHRs should influence resources used in the delivery of clinical care, for example by identifying and facilitating more efficient clinical and administrative processes, and by informing environmentally preferable procurement and clinical decision-making.11 All 3 principles—use of more efficient IT/equipment, use of IT/equipment to monitor and control energy consumption/waste related to buildings and support services, and use of IT/equipment to influence care delivery and clinical decision-making, should be considered in any informatics-centric approach to promoting decarbonization and environmental sustainability.
In the sections below, we build on these 3 guiding principles, define the field Clinical Climate Informatics, and propose an actionable clinical informatics framework to reduce healthcare’s environmental pollution and climate-related impacts. The proposed framework, which is derived from an established 8-dimension sociotechnical model,16 focuses on “Information technology-enabled Clinical cLimate InforMAtics acTions for the Environment” and henceforth titled the “i-CLIMATE Framework.” It has 5 actionable components, each of which includes specific considerations and sustainability solutions. We define Clinical Climate Informatics as a field that applies data, information, and knowledge management principles to operationalize components of the i-CLIMATE Framework. The framework has a sociotechnical foundation that involves both technical (eg, hardware/software, clinical content, user interface) and nontechnical, social considerations (eg, organizational policies, workflow, work environment, culture, people, external rules, regulations, and policies).16 We first outline the 5 components of the action framework, their goals, and rationale. We then use these 5 components to organize a set of example actions, discuss the corresponding risks, barriers, and potential unintended consequences that will be faced in implementing these actions, and suggest potential strategies to address them. This conceptual approach can help to advance both knowledge and action for how clinical climate informatics can drive healthcare decarbonization activities toward net-zero emissions, reducing e-waste, promoting responsible resource stewardship, and achieving environmental sustainability.
THE USE OF i-CLIMATE FRAMEWORK TO GUIDE INTERVENTIONS AND ACTIONS
The i-CLIMATE Framework has the following 5 components related to promoting decarbonization activities and reducing e-waste in healthcare (Figure 1).
Figure 1.
The i-CLIMATE framework and the relationship between the 3 guiding principles and the 5 action components for how clinical informatics can help reduce healthcare’s environmental pollution and climate-related impacts.
Create a circular economy for health IT
Goals: reuse, refurbish, repurpose, and recycle
The principles of a circular economy which include the elimination of waste and pollution along with decisions to reuse, refurbish, or repurpose equipment and materials are well-known outside of healthcare, but these ideas need to quickly make their way into clinical informatics and healthcare.17 For example, in high-income countries, healthcare organizations commonly implement high-end computer hardware and it is generally recommended that they replace the vast majority of these devices every 2–4 years depending on improvements in technology, clinical, or administrative use cases, and budget availability.14 This rapid turnover in computer equipment ensures that users experience good performance and high reliability necessary for them to run the latest releases of operating systems and application software. By replacing or upgrading key components (eg, power supplies, cooling fans, hard drives, or adding RAM—random access memory) and continuing to use the same hardware longer, an organization can significantly reduce their contribution to product life cycle emissions and the enormous amount of e-waste created every year.18 In addition, organizations can preferably contract with certified “green” vendors that have take-back programs to ensure repurposing of equipment and components,17 and take responsibility for recycling materials only when reuse is no longer feasible, rather than throwing materials away.19–21 When acquiring new, and upgrading existing equipment, Energy Star efficiency ratings should also be prioritized, to maximize energy efficiency.22
Reduce energy consumption
Goals: power down, use low-power devices, and increase use of renewable energy
A large healthcare organization uses significant quantities of electricity to run their computers, and HVAC systems required to maintain the climate-controlled environment. By combining administrative data from the EHR (eg, operating room, clinic schedules, or hospital room assignments) with building-level energy and device monitoring software,15 an organization could identify facility areas, not in use and automatically reduce lighting, ventilation, and power down electronics. Modifying current energy delivery to an “on-demand” model can reduce energy consumption not just related to building and computer use but also other hospital equipment.23 This would require manufacturers to develop, and healthcare organizations to adopt and use, functionality (eg, electrical submetering and other sensor-based infrastructures24) to allow them to monitor their equipment, safely enter a low-power standby mode, and then power up quickly as needed. It may also be possible to improve overall energy efficiency by reducing patient and staff driving, for example, by using telehealth for relatively simple follow-up visits.25 This will require clinicians, healthcare organizations, and payers to develop and implement guidelines for appropriate use and billing of telehealth services based on patients’ conditions and preferences beyond those adopted during recent emergency pandemic conditions.26
Support clinician and administrator decision-making
Goals: measure, display, and monitor data and performance improvement
In addition to making changes in the procurement, use, and configuration of the hardware and software itself to address climate change, health IT can also enable clinicians and healthcare administrators to make climate-informed changes in their procurement and work processes.11
A primary goal of Clinical Climate Informatics is to support more climate-friendly clinical decision-making. Substantial overuse of testing, medications, and supplies is ubiquitous in healthcare.27 In instances where there are clinical outcomes equipoise, clinicians may reconsider alternatives before prescribing a product with a large carbon footprint or while prescribing similar medications or supplies that have very different carbon footprints.11 For example, considerable work has been done to assess the impacts of commonly used anesthetic gases isoflurane, desflurane, sevoflurane, and nitrous oxide on climate change.28,29 Assuming the cooperation and support of EHR vendors, it would be relatively simple to display in real-time the carbon dioxide equivalent impacts of each anesthesia option available to clinicians at the point-of-care, along with more familiar equivalencies such as miles driven,30 to encourage environmentally preferable choices. Real-time alerts for fresh gas flow rates have been available for over a decade and have demonstrated waste reduction success.31 Such information displays might serve to nudge clinicians to select anesthetic gases with fewer climate impacts32 and reduce their overall use.28
Using embodied carbon emissions when evaluating the purchase of supplies or equipment is not well known to middle management who make systems-level procurement decisions. For example, SAP recently released its Product Carbon Footprint Analytics tool which provides a means for organizations in select industries to assess the carbon footprint of their devices or supplies across the value chain.33 Similar tools could be developed to cover the healthcare industry. Health IT could then help by creating organization-wide dashboards that incorporate this type of product lifecycle carbon emissions information to help clinicians and healthcare administrators consider, track, and compare the environmental costs of different supplies, similar to those used to monitor EHR usage,34 safety,35 maintenance,36 or financial costs.37 Often, displaying and monitoring the actual or relative costs of different options is enough to change behavior.11
The EHR can facilitate measuring, displaying, and monitoring information that estimates the effects of various decisions regarding the use of supplies, treatments, or medications on GHGs. Similarly, tracking procurement and supply chain data can provide information on how a healthcare system uses and disposes of supplies. Health IT can be used to track all of the information on use, cleaning, and disposal of different supplies and related work processes. Displaying this information to clinicians and administrators who make decisions about procurement and supply chain management within a healthcare organization can nudge them into better resource stewardship and more carbon-friendly choices.
Mobilize the healthcare workforce
Goals: train, educate, and incentivize
To achieve high impact from the i-CLIMATE Framework, the entire healthcare community should ideally be involved, including informaticians, payers, suppliers, administrators, clinicians, and patients. Most chief information officers (CIO) and chief medical informatics officers (CMIO) are not taught about this in any informatics curriculum even though they control a significant portion of the equipment purchasing and other decisions responsible for generating a significant amount of GHGs, environmental waste, and energy consumption. Most C-suite executives and their boards of directors in healthcare that make key decisions also do not currently have data or information to guide them about climate actions even though they may realize it is an important area to focus on.38 Informaticians can play a key role here. In addition to ensuring these influential executives can understand quantitative data about the problem, they can communicate how informatics and health IT can make a difference.39 These concepts apply to administrators and clinicians too. For instance, the CMIO can help educate and support clinicians in their day-to-day decision-making through judicious use of both active and passive clinical decision support within the EHR. Finally, if healthcare organizations included information about their decarbonization activities, efforts to reduce e-waste, and activities to promote responsible resource stewardship and environmental sustainability in their annual reports and community outreach activities, future staff would be able to use this information to help them choose where to work.40 There is a possibility that climate-conscious patients would also make use of this information when making elective healthcare decisions.41
The current climate emergency needs bolder actions and this is also true for clinical informatics. We propose the development of a specific clinical climate informatics curriculum that focuses on use of data, information, and knowledge and their associated principles of management to operationalize the 5 components of the i-CLIMATE Framework. For example, healthcare organizations need new educational content to address the importance of mitigating GHGs and environmental waste in building a sustainable future, along with education on how best to use utilization and emissions data for strategic management within their healthcare delivery system. This latter activity in turn would generate new information on how healthcare organizations could modify existing applications, decisions, devices, and processes to address the problems of climate change. Finally, informaticians can nudge and motivate health system administrators to change by integrating activities for reducing GHGs, energy consumption, or environmental waste with activities already being undertaken as part of existing incentive programs.
Inform policies and regulations for change
Goals: incentivize, motivate, report, and regulate
Ultimately, various types of economic, social, regulatory, and political strategies are needed to effect change. Healthcare organizations spend a tremendous amount of money on computer and networking equipment in addition to utility bills. Better IT-enabled methods still need to be developed to capture and report carbon footprint data. Health IT can also better capture the health-related impact of climate change, for example, through new pollution-related disease classification codes.42 For example, even though certain conditions (asthma exacerbation from smoke, heat-related illnesses) are precipitated by climate changes and pollution, the current billing codes infrastructure and our EHRs do not accurately account for this. These methods could provide a more powerful data-informed “burning platform” to impact policies and regulations. Furthermore, clinical climate informatics and use of large-scale, integrated electronic data could not only help advance knowledge about the health impacts of climate change but also help understand their mechanisms, enable opportunities to intervene, and provide early warning signals to protect patients and the public.43 Such climate-related data could be of immense value to policymakers who serve vulnerable populations and communities.
Informatics can enable the data and information that organizations need to exert their economic power to put pressure on IT, utility, and service suppliers to encourage them to “go green.” In addition, healthcare organizations and their IT leadership can use this data and information to work with their local, state, and national political representatives to encourage them to enact climate-friendly legislation, including driving rapid shifts to clean power.44
i-CLIMATE framework implementation
Given the financial, technical, and personnel constraints that exist in the modern healthcare delivery system, implementing the i-CLIMATE framework will be challenging. However, rapid implementation is critical if we are to make the necessary changes required to meet aggressive climate targets.45 Currently, work underway in both the National Academy of Medicine Action Collaborative to Decarbonize the U.S. Health Sector46 and the U.S. Health and Human Services Office of Climate Change and Health Equity47 could bolster such efforts. Table 1 (below) gives pragmatic examples of actions that could be taken in each of the i-CLIMATE framework’s components. With each potential action or intervention designed to reduce energy consumption or environmental pollution, we provide its rationale, potential barriers or risks that implementers may encounter, along with a suggested strategy to address them. Success in implementing these actions will require a concerted effort, attention to potential unintended consequences, a consideration of tradeoffs, and compromise. Implementation thus is a shared responsibility that involves many stakeholders including clinicians, patients, informaticians, senior IT, and administrative leadership, EHR vendors, policymakers, and the government. Successful implementation will also require a strong scientific foundation that involves implementation and behavioral scientists, especially human factors experts and organizational psychologists, alongside environmental scientists who have experience with similar efforts in other industries.
Table 1.
Operationalizing the i-CLIMATE framework to decarbonize healthcare and reduce environmental pollution
| i-Climate framework component | Potential action or intervention | Rationale | Potential barriers or risks | Strategy to address barrier or risk |
|---|---|---|---|---|
| Circular Health IT Economy | Lengthen replacement cycles for servers and clinical workstations to 4–6 years. | Reduce consumption of natural resources, computer components, and waste generation; save money; save work | Reduced computer performance and reliability | Consider adding RAM to workstations; Make sure devices are free from disk clutter and malware |
| Right to update, repair, or replace internal computer hardware components | Reduce downtime; increase supply chain resilience; Save money | Reduced safety and reliability; Often requires reapproval by FDA, Lack of policies to support activities | Adopt Federal Trade Commission recommendations on the “right to repair”48 | |
| Contract with take-back programs certified to responsibly repurpose, refurbish, and (lastly) recycle devices49 | Reduce consumption of resources required to manufacture devices (eg, greenhouse gases used to generate electricity; plastics used in computers, rare earth elements used in computer hardware) | Risk of inadvertent disclosure of protected health information on old disks. Challenge to ensure sustainability claims to avoid greenwashing50 | Scrub all hard drives and memory before recycling. Mandated standard environmental disclosures. Use certified vendors. | |
| Encourage health IT-related suppliers to go green | Reduce consumption of resources required to manufacture and dispose of devices, and use safer materials | Suppliers may try to raise prices to accommodate “green” initiatives | Negotiate with multiple suppliers; get competitive bids; Mandated standard environmental disclosures | |
| Greenwashing | ||||
| Reduce Energy Consumption | Use IT to identify unused areas and equipment to power down | Save electricity | Decreased lifespan of devices; increased time to login in the morning; difficult to do nightly updates to software/operating systems | Develop applications to automatically shut down unused devices and restart machines before work starts |
| Use low electrical consumption CPUs | Reduce electricity consumption | Slower computers result in longer response times for clinicians | Newer devices should have minimal differences in performance | |
| Use shared cloud computing resources rather than locally hosted solutions | Savings on electric, heating, cooling resources51 | Loss of local control; potential increased risk of data breach | Require remote-hosting services to sign a business associate agreement as specified in HIPAA | |
| Use clean energy sources for data center; | Reduce greenhouse gases and toxic air emissions from fossil fuel combustion used to generate electricity | Underdeveloped high-reliability, clean energy infrastructure | Invest in newer battery technology and solar panels; Work with local utilities to maximize ability to respond to emergencies; encourage state-level policies to drive investments in clean energy | |
| Optimize algorithms to reduce computational complexity and memory requirements | Reduce computational requirements—save electricity; enable organizations to use smaller computers | Assumes that algorithms are not already optimized. | With a concerted effort, most software can be significantly improved | |
| Reduction in printed reference books | Increased availability of reference material via computer; Reduced printing costs; Save natural resources | Information not available during power outages; | Work to reduce impact of power outages | |
| Increased use of telemedicine52 | Reduce driving for patients | In-person visits are still needed for testing, procedures, and certain treatments. Increased technology and energy requirements. | Develop guidelines for appropriate use of telemedicine services based on patient condition | |
| Support Clinical or Administrative Decisions | Alerts to reduce ordering/use of tests, medications, procedures; Personalized resource consumption and associated emissions reports | Reductions in unnecessary test, medications, procedures; Reduce costs and pollution | Decreased revenue for health system; Increase alert burden for clinicians; Reduction in adherence to other alerts | Use noninterruptive information displays; Work with payors to share cost savings |
| Adopt pollution-related disease classification codes53 | Help improve our understanding of the effects of pollution on health | Insufficient knowledge to utilize existing codes; insufficient codes | Work with clinical content vendors to make codes widely available; advocate for new climate-related diagnosis codes42 | |
| Reporting and displaying estimates of carbon-equivalent emissions in EHR, to influence environmentally preferable choices | Increased awareness of the problem; promote change | Increased time, effort, and cost to generate reports; information overload for clinicians; reduced screen space for other clinical information; vendor greenwashing of product and service emissions | Work with EHR vendors to create reports that can be shared across their customer base; governmental emissions reporting standards | |
| Reporting and displaying estimates of carbon-equivalent measures in procurement databases to influence environmentally preferable choices; | Reduce shipping and handling costs | Potential increase in costs; vendor greenwashing of product and service emissions | Work with suppliers to reduce impact of changes; governmental emissions reporting standards | |
| Use data analysis to streamline work processes, procedures, and procurement processes (eg, shortest driving routes) | Eliminate waste of supplies; optimize driving and delivery routes | Information gaps and lack of integration. | Many of these services are already commonly available; work with vendors for seamless data integration. | |
| Mobilize workforce | Mobilize healthcare workforce around climate change issues | Increase awareness of the problem; promote change | Reduced time for other important clinical matters | Work to make climate issues part of daily life |
| Inform policy development | Use IT to control energy consumption of the building (lighting, HVAC) | Decrease energy consumption; save money | Small, short-term impact during periods of change from nonuse to high-intensity usage; nonevidence-based policy barriers around infection control. | Careful attention to transitions should minimize impacts. Rational policies to permit HVAC setbacks. |
| Policy changes for Payors to set and incentivize “green” targets for data centers and workstations | Increase awareness of the problem; promote change | Potential to reduce time devoted to other issues; legislative inertia. | This should become commonplace over the next few years; international policy drivers. |
CONCLUSIONS
The current climate emergency calls for bold involvement from the clinical informatics community. We define a new subfield of biomedical informatics, “Clinical Climate Informatics” that focuses on use of data, information, and knowledge and their associated principles of management to operationalize actions to drive healthcare decarbonization activities toward net-zero emissions, reduce e-waste, and promote environmental sustainability. This field supports implementation of the i-CLIMATE Framework. While the framework is bound to evolve over time, it is currently pragmatic and actionable enough to start creating the much-needed momentum to leverage data, information, knowledge management technologies, and informatics approaches to accelerate healthcare’s journey to net-zero emissions. Implementation of this framework using sociotechnical principles54 which include consideration of hardware and software as well as people involved, their communication patterns, workflows, culture, environment, and external rules and regulations, can help ensure an important role for health IT-enabled healthcare and its practitioners in addressing environmental sustainability and improving planetary health.
FUNDING
HS is supported by the Veterans Affairs (VA) Health Services Research and Development (HSR&D, IIR17-127), the Agency for Healthcare Research and Quality (R01HS27363), the Gordon and Betty Moore Foundation (GBMF 8838 and GBMF 5498), and the CanTest Research Collaborative funded by a Cancer Research UK Population Research Catalyst award (C8640/A23385). HS is also partially supported by the Houston VA HSR&D Center for Innovations in Quality, Effectiveness and Safety (CIN 13–413). The opinions expressed are those of the authors and not necessarily of the Department of Veterans Affairs or the US government.
Author Contributions
All authors made substantial contributions to the conception of this work. DS wrote the first draft of the manuscript. All authors participated in substantial critical revisions of the manuscript for important intellectual content and approved the final version to be published. All authors agree to be accountable for all aspects of the work.
Conflict of interest statement
None declared.
Contributor Information
Dean F Sittig, School of Biomedical Informatics, University of Texas Health Science Center, Houston, Texas, USA.
Jodi D Sherman, Department of Anesthesiology, Yale School of Medicine, New Haven, Connecticut, USA; Department of Environmental Sciences, Center on Climate Change and Health, Yale School of Public Health, New Haven, Connecticut, USA.
Matthew J Eckelman, Department of Civil & Environmental Engineering, Northeastern University, Boston, Massachusetts, USA.
Andrew Draper, Health Data Informatics and Analytics, University of Denver, HCA Continental Division, GreenCIO.org, Denver, Colorado, USA.
Hardeep Singh, Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey Veterans Affairs Medical Center and Baylor College of Medicine, Houston, Texas, USA.
Data Availability
All data are incorporated into the article.
REFERENCES
- 1. Atwoli L, Baqui AH, Benfield T, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. BMJ 2021; 374: n1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bawaneh K, Ghazi Nezami F, Rasheduzzaman M, Deken B.. Energy consumption analysis and characterization of healthcare facilities in the United States. Energies 2019; 12 (19): 3775. [Google Scholar]
- 3. Hilty L, Lohmann W, Huang EM.. Sustainability and ICT-an overview of the field. Notizie di Politeia 2011; 27 (104): 13–28. [Google Scholar]
- 4.U.S. Environmental Protection Agency, U.S. General Services Administration, U.S. Department of Energy. National Strategy for Electronics Stewardship: Accomplishments. January 2017. https://www.epa.gov/sites/default/files/2017-08/documents/national_strategy_for_electronics_stewardship_accomplishments_report_final_8_7_17.pdf Accessed April 15, 2022.
- 5. Eckelman MJ, Huang K, Lagasse R, Senay E, Dubrow R, Sherman JD.. Health care pollution and public health damage in the United States: an update. Health Aff (Millwood) 2020; 39 (12): 2071–9. PMID: 33284703. [DOI] [PubMed] [Google Scholar]
- 6. Eckelman MJ, Sherman J.. Environmental impacts of the U.S. health care system and effects on public health. PLoS One 2016; 11 (6): e0157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sherman JD, MacNeill A, Thiel C.. Reducing pollution from the health care industry. JAMA 2019; 322 (11): 1043–4. [DOI] [PubMed] [Google Scholar]
- 8. Remondino M. Information technology in healthcare: HHC-MOTES, a novel set of metrics to analyse IT sustainability in different areas. Sustainability 2018; 10 (8): 2721. [Google Scholar]
- 9. Barteková E, Börkey P. (2022), Digitalisation for the Transition to a Resource Efficient and Circular Economy, OECD Environment Working Papers, No. 192, Paris: OECD Publishing. 10.1787/6f6d18e7-en. https://www.oecd-ilibrary.org/deliver/6f6d18e7-en.pdf?itemId=%2Fcontent%2Fpaper%2F6f6d18e7-en&mimeType=pdf Accessed April 11, 2022 [DOI] [Google Scholar]
- 10. Sittig DF, Singh H.. Electronic health records and national patient-safety goals. N Engl J Med 2012; 367 (19): 1854–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sherman JD, Thiel C, MacNeill A, et al. The green print: advancement of environmental sustainability in healthcare. Resour Conserv Recycling 2020; 161: 104882. [Google Scholar]
- 12. Podder S, Burden A, Singh SK, Maruca R. How green is your software? Harvard Business Review; 2020. https://hbr.org/2020/09/how-green-is-your-software Accessed 6.8.2022
- 13. Energy Star. 16 more ways to cut energy waste in the data center. https://www.energystar.gov/products/16_more_ways_cut_energy_waste_data_center Accessed 6.3.2022
- 14. Gold AJ. Replacing enterprise PCs: the fallacy of the 3-4 year upgrade cycle. 2014. https://i.crn.com/custom/INTELBCCSITENEW/WhitePaper_EnterpriseRefresh.pdf Accessed April 15 2022
- 15. Ali AS, Coté C, Heidarinejad M, Stephens B.. Elemental: an open-source wireless hardware and software platform for building energy and indoor environmental monitoring and control. Sensors (Basel) 2019; 19 (18): 4017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sittig DF, Singh H.. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care 2010; 19Suppl 3: i68–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. MacNeill AJ, Hopf H, Khanuja A, et al. Transforming the medical device industry: Road map to a circular economy: study examines a medical device industry transformation. Health Aff (Millwood) 2020; 39 (12): 2088–97. [DOI] [PubMed] [Google Scholar]
- 18.WEEEForum. International e-waste day: 57.4M tonnes expected in 2021. https://weee-forum.org/ws_news/international-e-waste-day-2021/ Accessed March 22, 2022
- 19.Apple Trade In. https://www.apple.com/shop/trade-in Accessed April 12, 2022
- 20.Dell Trade In. https://tradein.dell.com/ Accessed April 12, 2022
- 21. O’Connor MP, Zimmerman JB, Anastas PT, Plata DL.. A strategy for material supply chain sustainability: enabling a circular economy in the electronics industry through green engineering. ACS Sustainable Chem Eng 2016; 4 (11): 5879–88. [Google Scholar]
- 22.ENERGY STAR® Program Requirements for Computers Version 5.0. Available: https://www.energystar.gov/ia/partners/prod_development/revisions/downloads/computer/Version5.0_Computer_Spec.pdf?0f42-51d9 Accessed April 12, 2022.
- 23. Rohde T, Martinez R.. Equipment and energy usage in a large teaching hospital in Norway. J Healthc Eng 2015; 6 (3): 419–33. [DOI] [PubMed] [Google Scholar]
- 24. Koulamas C, Moronis A, Kalogeras A, Liberanome D. Choosing measures for energy efficient hospital buildings. In: 2017 22nd IEEE International Conference on Emerging Technologies and Factory Automation (ETFA). IEEE, 2017: 1-7.
- 25. Turley M, Porter C, Garrido T, et al. Use of electronic health records can improve the health care industry's environmental footprint. Health Aff (Millwood) 2011; 30 (5): 938–46. [DOI] [PubMed] [Google Scholar]
- 26. Anvari S, Neumark S, Jangra R, Sandre A, Pasumarthi K, Xenodemetropoulos T.. Best practices for the provision of virtual care: a systematic review of current guidelines [published online ahead of print May 9, 2022]. Telemed J E Health 2022; doi: 10.1089/tmj.2022.0004. [DOI] [PubMed] [Google Scholar]
- 27. Brownlee S, Chalkidou K, Doust J, et al. Evidence for overuse of medical services around the world. Lancet 2017; 390 (10090): 156–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Nair BG, Peterson GN, Neradilek MB, Newman SF, Huang EY, Schwid HA.. Reducing wastage of inhalation anesthetics using real-time decision support to notify of excessive fresh gas flow. Anesthesiology 2013; 118 (4): 874–84. [DOI] [PubMed] [Google Scholar]
- 29. Sherman J, Le C, Lamers V, Eckelman M.. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg 2012; 114 (5): 1086–90. [DOI] [PubMed] [Google Scholar]
- 30.Environmental Protection Agency. Greenhouse gas equivalencies calculator. https://www.epa.gov/energy/greenhouse-gas-equivalencies-calculator Accessed April 18, 2022
- 31. Feldman JM. Managing fresh gas flow to reduce environmental contamination. Anesth Analg 2012; 114 (5): 1093–101. [DOI] [PubMed] [Google Scholar]
- 32. Zuegge KL, Bunsen SK, Volz LM, et al. Provider education and vaporizer labeling lead to reduced anesthetic agent purchasing with cost savings and reduced greenhouse gas emissions. Anesth Analg 2019; 128 (6): e97–e99. [DOI] [PubMed] [Google Scholar]
- 33.SAP Product Carbon Footprint Analytics. https://help.sap.com/docs/SAP_ANALYTICS_CLOUD/21868089d6ae4c5ab55f599c691726be/da1a548fe1ba4728a45178a339924c6d.html Accessed April 15, 2022.
- 34. Simpao AF, Ahumada LM, Desai BR, et al. Optimization of drug-drug interaction alert rules in a pediatric hospital's electronic health record system using a visual analytics dashboard. J Am Med Inform Assoc 2015; 22 (2): 361–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Murphy DR, Savoy A, Satterly T, Sittig DF, Singh H.. Dashboards for visual display of patient safety data: a systematic review. BMJ Health Care Inform 2021; 28 (1): e100437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Iadanza E, Gonnelli V, Satta F, Gherardelli M.. Evidence-based medical equipment management: a convenient implementation. Med Biol Eng Comput 2019; 57 (10): 2215–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sherman JD, Raibley LA 4th, Eckelman MJ.. Life cycle assessment and costing methods for device procurement: comparing reusable and single-use disposable laryngoscopes. Anesth Analg 2018; 127 (2): 434–43. [DOI] [PubMed] [Google Scholar]
- 38. Daugherty P, Lacy P, Podder S, Singh SK. Uniting technology and sustainability. Accenture Research Report, 2022. https://www.accenture.com/_acnmedia/PDF-177/Accenture-Tech-Sustainability-uniting-Sustainability-and-Technology.pdf#zoom=40 Accessed 6.8.2022
- 39.The Green CIO: the unexpected environmentalist and sustainability champion. https://greencio.org/ Accessed 3.38.2022
- 40. Boyd P, Bialowitz J, Scannell T, Sherman JD. The case for net-zero health care. NEJM Catalyst, 2021. https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0372 Accessed 6.6.2022.
- 41. Tomson C. Reducing the carbon footprint of hospital-based care. Future Hosp J 2015; 2 (1): 57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wheat S, Lernery J, Limaye VS. We’re awash in climate change data, but health damages remain undercounted. Health Affairs Forefront. 2022; doi:10.1377/forefront.20220323.649504. https://www.healthaffairs.org/do/10.1377/forefront.20220323.649504/ Accessed March 25, 2022
- 43. Gray K. Climate change, human health, and health informatics: a new view of connected and sustainable digital health. Front Digit Health 2022; 4: 869721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.The Medical Society Consortium on Climate Change and Health. Mission statement. https://medsocietiesforclimatehealth.org/about/mission-and-consensus-statement/ Accessed April 10, 2022
- 45.United Nations Paris Agreement. https://unfccc.int/sites/default/files/english_paris_agreement.pdf; 2016; Accessed 6.6.2020
- 46. Dzau VJ, Levine R, Barrett G, Witty A.. Decarbonizing the U.S. health sector - a call to action. N Engl J Med 2021; 385 (23): 2117–9. [DOI] [PubMed] [Google Scholar]
- 47.US Department of Health and Human Services. About the Office of Climate Change and Health Equity (OCCHE). https://www.hhs.gov/ash/ocche/about/index.html Accessed 6.6.2022
- 48.Federal Trade Commission. Policy Statement of the Federal Trade Commission on Repair Restrictions Imposed by Manufacturers and Sellers. Matter Number: P194400. 2021. http://www.ftc.gov/system/files/documents/public_statements/1592330/p194400repairrestrictionspolicystatement.pdf Accessed April 10, 2022.
- 49. Villanueva C. Rethinking recycling. 2022. https://www.dell.com/en-us/blog/rethinking-recycling/ Accessed 4.15.2022
- 50. Gordon D, Zuegge KL.. Greenwashing in health care marketing. ASA Monitor 2020; 84: 18–21. [Google Scholar]
- 51.Verdantix. Carbon Disclosure Project Study 2011 Cloud computing – the IT solution for the 21st century. https://www.att.com/Common/about_us/files/pdf/cdp_us_cloud_computing.pdf Accessed April 18, 2022
- 52. Purohit A, Smith J, Hibble A.. Does telemedicine reduce the carbon footprint of healthcare? A systematic review. Future Healthc J 2021; 8 (1): e85–e91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ryan JL. Diagnoses and charges of patients with ICD-10-CM environmental pollution exposure codes in Florida. J Clim Change Health 2022; 5: 100083. [Google Scholar]
- 54. Singh H, Sittig DF.. A sociotechnical framework for safety-related electronic health record research reporting: the SAFER reporting framework. Ann Intern Med 2020; 172 (11 Suppl): S92–S100. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are incorporated into the article.