Abstract
Objective
This study aimed to evaluate the efficacy of a 4-week mindfulness-based stress reduction (MBSR) program on psychological distress in patients with lung cancer and elucidate its mechanisms.
Methods
This single-center, single-blinded, longitudinal, randomized controlled trial was conducted on 175 patients with lung cancer randomly allocated to a 4-week MBSR or a waiting-list group. The efficacy and mechanisms of the 4-week MBSR program were evaluated by outcome measures at preintervention (T0), the immediate postintervention (T1), 1 month (T2), and 3 months (T3). We analyzed the collected data using the per-protocol set principle, independent sample t-test, repeated measure analysis of variance, and structural equation modeling.
Results
The 4-week MBSR program significantly alleviated psychological distress (F = 15.05, P < 0.001), decreased perceived stigma (F = 8.260, P = 0.005), improved social support (F = 16.465, P < 0.001), and enhanced mindfulness (F = 17.207, P < 0.001) compared with usual care at T1, T2, and T3. All variables significantly changed over time except for copying style (P = 0.250). The changes in social support, mindfulness, and perceived stigma mediated the efficacy of the 4-week MBSR program on psychological distress (β = −0.292, P = 0.005; β = −0.358, P = 0.005).
Conclusions
This study shows the benefits of the MBSR program for psychological distress, social support, mindfulness, and perceived stigma in patients with lung cancer. Also, it elucidates the mechanisms by which the MBSR program alleviates psychological distress by improving social support, enhancing mindfulness, and decreasing perceived stigma. The findings provide insights into applying the MBSR program to reduce psychological distress among patients with lung cancer.
Keywords: Lung cancer, Psychological distress, Mindfulness, MBSR, Structural equation modeling
Introduction
Lung cancer remains the first reason of cancer-related death worldwide, accounting for approximately 18% of all cancer deaths.1 In China, according to the statistics published in 2022, lung cancer ranked first in incidence and cancer-related mortality, with new cases of 828,100 and cancer-related deaths of 657,000.2 Patients with cancer will suffer from various psychological problems except for various physical symptoms (eg, fatigue and shortness of breath) due to cancer diagnosis and anticancer treatment, especially psychological distress.3,4 Psychological distress will exist throughout the cancer trajectory,5 having different prevalence across studies, cancers, and countries,6 with a range from 20% to 58%.7, 8, 9, 10 Compared with other cancers, lung cancer was associated with the highest psychological distress prevalence,11,12 varying from 17.0% to 73.0%.13, 14, 15 In addition, a recent meta-analysis reported a mean prevalence of 48.3% of psychological distress in Chinese patients with lung cancer .16
Distress refers to “a multifactorial and unpleasant emotional experience, involving changes in psychological, social, spiritual, and physical aspects,” according to the definition given out by the National Comprehensive Cancer Network (NCCN) guideline.17 Patients and oncologists prefer the term “distress” because it is less stigmatizing; therefore, the NCCN guideline panel used “distress” rather than “psychological distress.”18 However, both terms are used interchangeably in the literature. Clinically significant psychological distress is associated with a range of adverse consequences,17 such as interruption of anticancer treatment19, 20, 21, prolonged hospital stay,22 higher suicidal risk,23 poor quality of life,14,24 and higher risk of mortality.25,26 Moreover, a previous study also evidenced that psychological distress can accelerate the growth of tumor cells.27 Therefore, regular and timely screening of psychological distress among patients with cancer is critical because it has been recognized as the sixth vital sign.17,28 Indeed,it is critical to alleviate it after early and precise detection of psychological distress.
Currently, psychological interventions have been demonstrated efficacy in improving the psychological well-being of patients with cancer.29, 30, 31 Among the available psychological interventions, mindfulness-based stress reduction (MBSR), initially developed by Kabat-Zinn et al,32 has been widely applied in cancer settings31,33 and might also the best psychological intervention to relieve cancer-related fatigue.34 Based on previously published evidence,35, 36, 37 the practice of mindfulness can guide participants purposefully pay attention to the present moment and nonjudgmentally monitor the unfolding of experiences moment by moment, thus having profound benefit via the mind–body connection. The standard MBSR program comprises an 8-week psychoeducational course and four meditative techniques, including sitting meditation, body scan, gentle Hatha yoga, and walking meditation.32,36,38 Studies have demonstrated the effectiveness and safety of MBSR program on psychosocial well-being and quality of life.31,33,39,40 Currently, several studies have initially investigated the role of MBSR program in patients diagnosed with lung diseases, such as lung cancer41,42 and interstitial lung diseases.43,44 Furthermore, our meta-analysis further demonstrated the positive impact of the MBSR program on psychological states in patients with lung cancer.45 However, a definitive conclusion regarding the efficacy of the MBSR program for psychological distress has not obtained and should be further investigated in future studies with larger sample sizes.
Although a previous study attempted to explore the efficacy of MBSR program on psychological distress from three perspectives, including mindfulness skills, self-compassion, and rumination,42 the exact psychosocial mechanisms by which MBSR program alleviates psychological distress remain unclear. Previous studies have revealed that several psychosocial factors in patients with cancer are associated with psychological distress, such as social support,46 perceived stigma,47 perceived stress,48 intrusive thoughts,49 symptom burden,49 type D personality,49 coping style,50 self-esteem,51 mindfulness,52,53 and illness perception.54,55 In addition, our previous studies explicitly investigated the roles of social support, perceived stigma, perceived stress, coping styles, self-esteem, mindfulness, and illness perception in the development of psychological distress in patients with lung cancer.15,56, 57, 58 However, it remains unclear which pathways may mediate the interventional effects of the MBSR program on psychological distress in patients with lung cancer.
Therefore, based on currently available evidence, we hypothesized that (a) a 4-week MBSR program could alleviate psychological distress in patients with lung cancer and (b) by affecting social support, coping style, self-esteem, mindfulness, perceived stress, perceived stigma, and illness perception.
Methods
Study design
The present study was a single-center, single-blinded, longitudinal, randomized, controlled, parallel trial, including a 4-week MBSR program group and a waiting-list group. We recruited eligible participants from a hospital in southwest China between January 1 and September 30, 2021.
Data collection
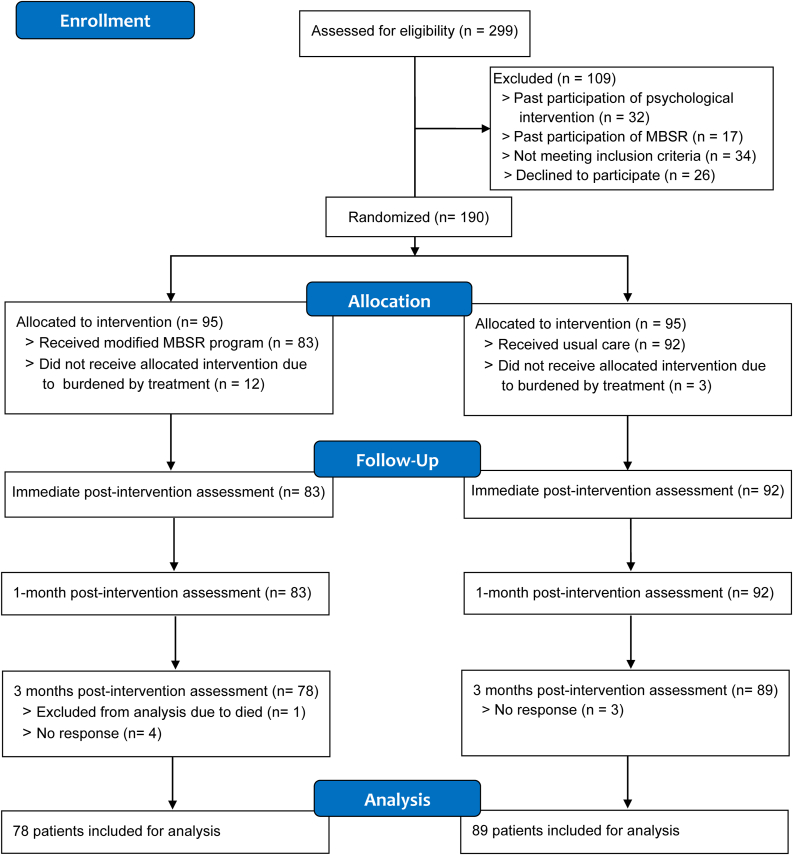
We designed a face-to-face questionnaire survey to collect data, administered by a trained research nurse at three time points (Fig. 1): baseline (T0), the immediate postintervention (T1), 1 month postintervention (T2), and 3 months postintervention (T3).
Fig. 1.
The Consolidated Standards for Reporting Trials (CONSORT) flow diagram of participant recruitment.
Sample size
We estimated the sample size using psychological distress as the main effect indicator for this study. According to our previous meta-analysis,45 the MBSR program was associated with an effect size of 0.418, which was estimated based on the pooled result of psychological distress. Therefore, we estimated a theoretical sample size of 75 cases to ensure a statistical power of 80.0%. After considering a 20% dropout rate, 90 patients were calculated and then randomized to the 4-week MBSR or the waiting-list group. We used the G∗Power software (version 3.1) to estimate the sample size.
Participant criteria
We selected potential participants according to the following inclusion criteria: (a) cytological or histological diagnosis of lung cancer; (b) age ≥18 years; (c) patients with proven clinically significant psychological distress or at high risk of suffering from psychological distress; (d) known their diagnosis and were willing to participate in this study; and (e) able to read, write, and speak Chinese.
Exclusion criteria included: (a) a concurrent diagnosis of other cancers or psychiatric disorders; (b) a history of suicide attempts; (c) participation in any other psychosocial interventions within 3 months before enrollment; (d) prior experience with mindfulness-based interventions (MBIs); and (e) physical or cognitive (< 26 on the Mini-Mental State Examination) impairments hampering participation in the 4-week MBSR program or completion of questionnaires. Dropout criteria included: (a) unable to complete the intervention and (b) loss to follow-up.
Recruitment
The trained research nurses enrolled participants from the respiratory and medical oncology inpatient departments of a general hospital in southwest China at patient visits. Trained research nurses assessed their eligibility, introduced the purpose of the study, and explained research content to potential participants and ensured that participants voluntarily participated in this study.
Randomization, allocation concealment, and blinding
After signing a written informed consent, eligible participants formally participated in this study. We first conducted a baseline survey of all participants in this study. Then, we randomly assigned participants to a 4-week MBSR or waiting-list group using random numbers generated by SPSS software (version 22.0). An independent research nurse used sealed and opaque envelopes for assignments. We invited independent psychologists qualified in the MBSR program to conduct a 4-week MBSR program for participants in the experimental group. Since all participants have been informed of the detailed processes of this study, it is not possible to blind participants. However, outcome assessments were blinded because independent staff analyzed all outcomes.
Interventions
Experimental group
Participants in the experimental group received both usual care and a 4-week MBSR program. In this study, we selected a 4-week MBSR program as an intervention according to our meta-analysis45 because patients with lung cancer usually have a relatively short median survival time and fast deterioration in physical health.59 During this 4-week MBSR program, all participants in the experimental group practiced MBSR under the guidance and supervision of a psychologists qualified as mindfulness trainer. The details of this 4-week program were as follows: 10-min explanation and meditation in the first week, 10-min walking meditation in the second week, 10-min breathing meditation in the third week, and 20-min experience sharing in the fourth week. Details of each session in this 4-week MBSR program are summarized in Table S1. Participants were supervised to daily practice at home by psychologists twice weekly using telephone or WeChat (a popular social media in China).
Waiting-list group
Participants in the waiting list group first received usual care, including dietary instruction, health education, rehabilitation excise, emotional counseling, and medication instruction. Following the conclusion of this study, these participants were invited to voluntarily receive a 4-week MBSR program and were provided with videos and materials for the intervention.
Demographics
At baseline, we used a self-designed data collection sheet to collect the demographic and clinical characteristics, including demographic information (gender, age, education level, occupation, marital status, residence, medical insurance, yearly income, family history of lung cancer, and smoking history) and clinical characteristics (TNM tumor stage, metastases, comorbidities, and pain degree).
Outcome measures
Psychological distress
We used the distress thermometer (DT) to measure psychological distress on an 11-point thermometer scale from 0 to 10 in this study, and 0 and 10 indicate no distress and extreme distress, respectively.17 The reliability and validity of DT across different settings have been extensively tested.60 Previous empirical studies indicated a score of ≥ 4 effectively confirms clinically significant psychological distress.60,61 A score of 4 was also demonstrated as the cut-off value for defining clinically significant psychological distress in Chinese cancer populations.60 Meanwhile, we used the predictive algorithm, which was previously developed by our team,62 to identify those patients at high risk of psychological distress. In this predictive algorithm, a score of ≥ 66 indicates that patients have a high risk of suffering from psychological distress. We selected patients with lung cancer who scored ≥4 in DT or ≥ 66 in the predictive algorithm to participate in this study.
Social support
The 12-item Multidimensional Scale of Perceived Social Support was used to measure social support from three aspects, including family, friends, and significant others, on a 7-point Likert scale (1 indicates very strongly disagree but 7 represents very strongly agree).63 A previous study tested the psychological properties of Multidimensional Scale of Perceived Social Support and reported coefficient alpha values of subscales ranging from 0.81 to 0.98.63 The Chinese version had a reliability of 0.90.64 We used the Chinese version in this study, which had an overall Cronbach's alpha coefficient of 0.818, 0.785, 0.835, and 0.701 at T0, T1, T2, and T3, respectively, to measure social support.
Coping style
The 20-item Medical Coping Modes Questionnaire was used to evaluate the coping styles, including confrontation, avoidance, and giving up coping, on a linear 4-point Likert scale from 1 to 3.65 Shen et al66 validated the Chinese version of the Medical Coping Modes Questionnaire, reporting a Cronbach's alpha coefficient of more than 0.60 for three subscales. We used the Chinese version in this study, which had an overall Cronbach's alpha of 0.561, 0.542, 0.753, and 0.537 at T0, T1, T2, and T3, respectively, to measure coping style.
Self-esteem
The 10-item Rosenberg Self–Esteem Scale was developed to measure global self-esteem, having a Cronbach's alpha of 0.88.67 A higher score indicated a higher level of self-esteem.67 The Chinese version of the Rosenberg Self-esteem Scale has been validated by Wu et al68 and has been extensively used in China.69, 70, 71 We used the Chinese version in this study, which had an overall Cronbach's alpha coefficient of 0.809, 0.774, 0.750, and 0.775 at T0, T1, T2, and T3, respectively, to measure self-esteem.
Mindfulness
The 39-item Five Facet Mindfulness Questionnaire was first developed by Baer et al72 to assess mindfulness from five facets on a 5-point Likert scale: observing, describing, acting with awareness, non-judging, and non-reacting.72 The original Five Facet Mindfulness Questionnaire has been translated into Chinese73 with good psychometric properties. In addition, a recent study continued to confirm the psychometric properties of the Chinese version in patients with cancer using a Bayesian structural equation modeling approach.74 We used the Chinese version in this study, which had an overall Cronbach's alpha coefficient of 0.644, 0.704, 0.731, and 0.749 at T0, T1, T2, and T3, respectively, to measure mindfulness.
Perceived stress
The 10-item Perceived Stress Scale was used to measure perceived stress on a linear 5-point Likert scale from 0 to 4.75 A higher score represents a greater stress level. The 10-item Chinese version has been validated and got a Cronbach's alpha of 0.619.76 We used the Chinese version in this study, which had an overall Cronbach's alpha coefficient of 0.614, 0.608, 0.699, and 0.682 at T0, T1, T2, and T3, respectively, to measure perceived stress.
Perceived stigma
The 31-item Cataldo lung cancer stigma scale was used to measure perceived stigma, categorized into stigma and shame, social isolation, discrimination, and smoking, on a linear 0- to 4-point.77 A higher score indicates a higher level of perceived stigma. Yu et al78 translated the original version to Chinese and reported an overall Cronbach’s alpha of 0.932. In addition, four subscales had a Cronbach’s alpha of 0.799, 0.922, 0.863, and 0.803, respectively. This study used the Chinese version of the Cataldo lung cancer stigma scale, which had an overall Cronbach's alpha coefficient of 0.863, 0.717, 0.709, and 0.730 at T0, T1, T2, and T3, respectively, to measure perceived stigma.
Illness perception
Weinman et al79 first developed the Brief Illness Perception Questionnaire to measure illness's emotional and cognitive representations on a continuous linear 0 to 10 point. A higher score represents a more negative illness perception. Broadbent et al80 have shown a good test–retest reliability and predictive and discriminant validity of the Brief Illness Perception Questionnaire. Xue et al81 translated the original version to Chinese, and it has been widely used in China.82,83 We used the Chinese version in this study, which had an overall Cronbach's alpha coefficient of 0.657, 0.676, 0.643, and 0.630 at T0, T1, T2, and T3, respectively, to measure illness perception.
Statistical analysis
We used descriptive statistics to present participants’ demographics. The Kolmogorov–Smirnov tests showed that, in addition to age and risk scores in the prediction algorithm, the distribution of scores for psychological distress, social support, coping style, self-esteem, mindfulness, perceived stress, perceived stigma, and illness perception was abnormal at most time points. However, we preferred to use mean ± standard deviation (SD) for all continuous variables because (a) parametric tests are more powerful than nonparametric tests, (b) the results of the Kolmogorov–Smirnov test are not necessarily true, especially for relatively large sample size,84 and (c) according to kurtosis and skewness values, our data followed a normal distribution.85 Therefore, we used the Chi-square test and independent-sample t-test to compare the variables between the two groups. However, repeated measure analysis of variance was used to analyze changes or differences of variables between the groups (experimental vs. waiting-list groups), within-group (time), and interaction (group∗time) effects.
Furthermore, we used structural equation modeling to elucidate the mediating role of significant variables that showed significant differences in the efficacy of a 4-week MBSR program on psychological distress between the two groups after intervention We first defined the interventions used in the experimental and waiting-list groups as dummy variables using 1 (experimental group) and 0 (waiting-list group), respectively. In addition, we adjusted all variables obtained from postintervention using the baseline value.86
We employed IBM Statistical Package for Social Sciences (SPSS) version 22.0 and Amos version 21.0 for statistical analysis.
Ethical consideration
This study strictly followed the statement of the Declaration of Helsinki. The ethical institutional board of the hospital approved this trial (Approval No. CZLS2021183-A), and we also registered the study protocol at the Chinese Clinical Trials Registry (Registration No. ChiCTR2100041899). Before participating in this study, all eligible participants signed informed consent and were freely allowed to withdraw from this study.
Results
Recruitment
As depicted in the CONSORT flowchart (Fig. 1), 299 patients with lung cancer were eligible for evaluation, but 190 patients who were eligible agreed to participate in this study. Of the 190 patients, 95 were randomly assigned to the experimental or waiting-list groups. However, 12 and 3 patients received no interventions in the experimental and waiting-list groups, respectively. One hundred seventy-five patients completed the study and underwent T1 and T2 assessments; however, at the T3 assessment, 5 and 3 patients were missed from the experimental and waiting-list groups, respectively. There was no statistically significant difference in the lost participants between the two groups at T3 (P = 0.480).
Participants’ characteristics
The mean age of the participants in the experimental and waiting-list groups was 58.98 (SD = 9.72) and 59.90 (SD = 8.72), respectively, without significant difference (P = 0.507). Of the 175 patients analyzed, most patients were male (61.7%) and lived in the urban areas (58.9%). Most patients were married (97.1%) and had low education (85.7% with a middle–high school education or less). Most of the patients paid medical costs using resident basic health insurance (97.7%) and had no family history of lung cancer (96.0%). Still, most patients were pain free (68.0%), had no comorbidity (76.6%), and were at stage III or IV. There remaining demographic and clinical data of the two groups were no significantly different (P > 0.05), as presented in Table 1.
Table 1.
Demographic and clinical characteristics of the patients (N = 175).
| Variable | Experimental (n = 83) | Control (n = 92) | t/χ2 | P-value |
|---|---|---|---|---|
| Gender | 0.059∗ | 0.809 | ||
| Male | 52 | 56 | ||
| Female | 31 | 36 | ||
| Age, years | 58.98 ± 9.72 | 59.90 ± 8.72 | 0.664# | 0.507 |
| Education | 3.086∗ | 0.214 | ||
| Primary school or below | 15 | 26 | ||
| Middle and high school | 57 | 52 | ||
| College and above | 11 | 14 | ||
| Occupation | 6.726∗ | 0.081 | ||
| No work | 42 | 38 | ||
| Working | 8 | 17 | ||
| Retire | 30 | 37 | ||
| Marital status | 1.128∗ | 0.569 | ||
| Single | 1 | 0 | ||
| Married | 80 | 90 | ||
| Divorced/widowed | 2 | 2 | ||
| Residence | 0.938∗ | 0.333 | ||
| City | 52 | 51 | ||
| Rural areas | 31 | 41 | ||
| Medical insurance | 1.248∗ | 0.264 | ||
| Self-payment | 3 | 1 | ||
| Residents' basic health insurance | 80 | 91 | ||
| Yearly income, yuan | 5.080∗ | 0.166 | ||
| < 20,000 | 3 | 9 | ||
| 20,001-50000 | 25 | 17 | ||
| 50,001-100,0000 | 38 | 46 | ||
| > 100,000 | 17 | 20 | ||
| Family history of LC | 1.040∗ | 0.308 | ||
| Yes | 2 | 5 | ||
| No | 81 | 87 | ||
| Smoking history | 0.217∗ | 0.641 | ||
| Yes | 39 | 40 | ||
| No | 44 | 52 | ||
| TNM tumor stage | 3.055∗ | 0.383 | ||
| I | 10 | 15 | ||
| II | 22 | 15 | ||
| III | 18 | 20 | ||
| IV | 33 | 42 | ||
| Metastases | 1.361∗ | 0.506 | ||
| Yes | 48 | 48 | ||
| No | 35 | 43 | ||
| Comorbidities | 2.525∗ | 0.112 | ||
| Yes | 15 | 26 | ||
| No | 68 | 66 | ||
| Pain degree | 4.102∗ | 0.251 | ||
| No pain | 54 | 65 | ||
| Mild | 15 | 13 | ||
| Moderate | 13 | 9 | ||
| Severe | 1 | 5 |
LC, lung cancer; TNM, tumor-node-metastasis. ∗χ2, #t.
The effect of the intervention on outcomes
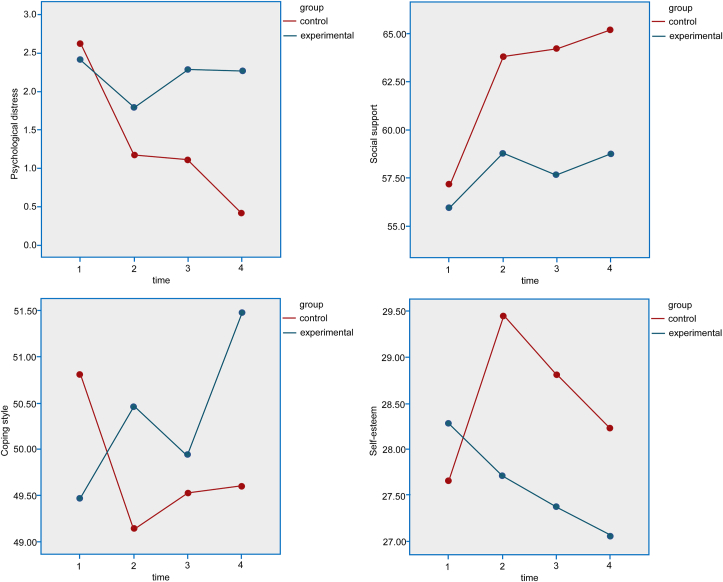
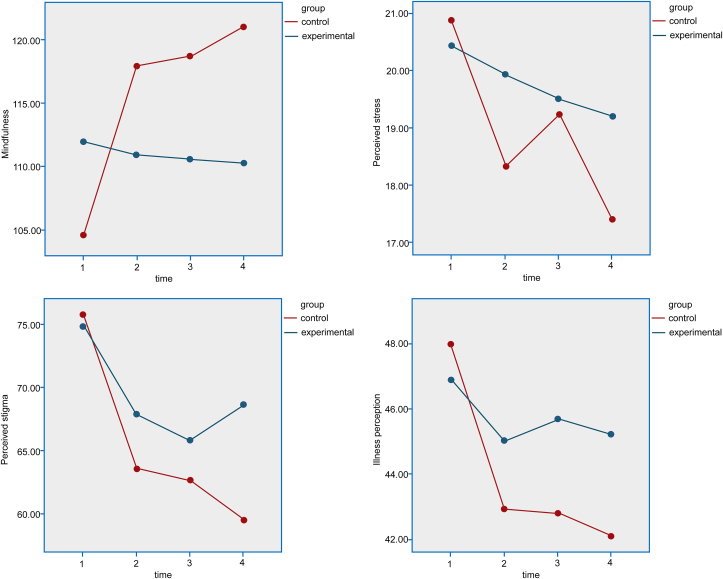
The scores of seven variables between the two groups were not significantly different (P > 0.05) at the baseline except for the score in the mindfulness, which was significantly higher in patients in the waiting-list group than patients in the 4-week MBSR program group (t = 4.746, P < 0.001). After the intervention, as shown in Fig. 2, Fig. 3, apart from the coping style (F = 1.386, P = 0.250), the remaining variables changed significantly over time (P < 0.05). As presented in Table 2, the 4-week MBSR program significantly alleviated psychological distress (F = 15.051, P < 0.001), improved social support (F = 16.465, P < 0.001), enhanced mindfulness (F = 17.207, P < 0.001), and reduced perceived stigma (F = 8.260, P = 0.005) at immediate postintervention, 1-month postintervention, and 3 months postintervention. In addition, the difference in interventional effects between the two groups was statistically significant over time (P < 0.05).
Fig. 2.
The changes of scores in psychological distress, social support, coping style, and self-esteem before and after intervention between the two groups.
Fig. 3.
The change of scores in mindfulness, perceived stress, perceived stigma, and illness perception before and after intervention between the two groups.
Table 2.
A comparison of the outcome variables between the two groups before and after the intervention.
| Variable | T0 (mean ± SD) |
T1 (mean ± SD) |
T2 (mean ± SD) |
T3 (mean ± SD) |
F1 (P) | F2 (P) | F3 (P) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Experimental (n = 83) | Control (n = 92) | Experimental (n = 83) | Control (n = 92) | Experimental (n = 92) | Control (n = 83) | Experimental (n = 78) | Control (n = 89) | ||||
| Risk score | 67.84 ± 24.42 | 66.39 ± 29.90 | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. |
| t = −0.350 | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | ||
| P = 0.727 | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | n.a. | ||
| Psychological distress | 2.70 ± 2.13 | 2.45 ± 2.21 | 1.16 ± 1.57 | 1.78 ± 1.74 | 1.07 ± 1.53 | 2.27 ± 1.27 | 0.43 ± 1.08 | 2.26 ± 1.25 | 56.245 (< 0.001) | 15.051 (< 0.001) | 37.762 (< 0.001) |
| t = −0.617 | t = −2.519 | t = −6.278 | t = −9.580 | ||||||||
| P = 0.537 | P = 0.012 | P=<0.001 | P=<0.001 | ||||||||
| Social support | 57.31 ± 7.17 | 55.66 ± 12.32 | 64.02 ± 7.34 | 58.80 ± 9.38 | 64.48 ± 8.35 | 57.73 ± 9.50 | 65.30 ± 6.42 | 58.81 ± 9.11 | 33.911 (< 0.001) | 16.465 (< 0.001) | 8.598 (< 0.001) |
| t = −0.170 | t = −3.752 | t = −4.865 | t = −4.769 | ||||||||
| P = 0.865 | P < 0.001 | P < 0.001 | P < 0.001 | ||||||||
| Coping style | 50.77 ± 4.89 | 49.54 ± 4.50 | 49.10 ± 3.51 | 50.48 ± 4.93 | 49.47 ± 3.73 | 50.02 ± 5.23 | 49.56 ± 5.25 | 51.60 ± 4.15 | 1.386 (0.250) | 1.515 (0.220) | 4.995 (0.005) |
| t = −1.702 | t = −1.486 | t = −0.203 | t = −2.372 | ||||||||
| P = 0.091 | P = 0.137 | P = 0.839 | P = 0.018 | ||||||||
| Self-esteem | 27.72 ± 4.04 | 28.17 ± 5.00 | 29.59 ± 4.34 | 27.67 ± 4.00 | 29.00 ± 4.53 | 27.44 ± 3.91 | 28.30 ± 4.70 | 27.14 ± 4.19 | 4.894 (0.006) | 2.425 (0.121) | 9.181 (< 0.001) |
| t = −0.754 | t = −3.018 | t = −2.765 | t = −2.419 | ||||||||
| P = 0.451 | P = 0.003 | P = 0.006 | P = 0.016 | ||||||||
| Mindfulness | 104.57 ± 10.87 | 111.97 ± 9.03 | 117.54 ± 9.78 | 110.88 ± 7.71 | 118.30 ± 10.05 | 110.59 ± 6.98 | 120.90 ± 11.20 | 110.31 ± 6.60 | 43.216 (< 0.001) | 17.207 (< 0.001) | 64.963 (< 0.001) |
| t = −4.746 | t = −4.540 | t = −5.138 | t = −6.568 | ||||||||
| P < 0.001 | P < 0.001 | P < 0.001 | P < 0.001 | ||||||||
| Perceived stress | 20.95 ± 4.64 | 20.48 ± 4.65 | 18.35 ± 3.86 | 19.97 ± 2.95 | 19.23 ± 3.62 | 19.55 ± 3.06 | 17.49 ± 3.61 | 19.26 ± 3.03 | 17.365 (< 0.001) | 3.755 (0.054) | 5.405 (0.002) |
| t = −1.099 | t = 3.106 | t = −1.206 | t = 3.498 | ||||||||
| P = 0.272 | P = 0.002 | P = 0.228 | P = 0.001 | ||||||||
| Perceived stigma | 75.83 ± 15.14 | 75.22 ± 16.06 | 63.57 ± 8.27 | 67.79 ± 8.87 | 62.55 ± 7.51 | 59.50 ± 7.70 | 68.58 ± 9.10 | 86.42 ± 9.10 | 87.520 (< 0.001) | 8.260 (0.005) | 12.988 (< 0.001) |
| t = −0.571 | t = −4.309 | t = −2.436 | t = 6.995 | ||||||||
| P = 0.568 | P=<0.001 | P = 0.016 | P=<0.001 | ||||||||
| Illness perception | 48.19 ± 7.81 | 46.98 ± 4.63 | 43.20 ± 7.00 | 45.00 ± 7.69 | 43.00 ± 7.49 | 45.62 ± 12.17 | 42.21 ± 7.20 | 45.13 ± 12.20 | 15.240 (< 0.001) | 2.365 (0.126) | 4.760 (0.009) |
| t = −0.782 | t = 1.571 | t = −1.080 | t = −1.539 | ||||||||
| P = 0.434 | P = 0.118 | P = 0.280 | P = 0.124 | ||||||||
T0, baseline; T1, the immediate postintervention; T2, 1-month postintervention; T3, 3 months postintervention; F1, time effect; F2, group effect; F3, group∗time effect; SD, standard deviation.
Results of the mediating analysis
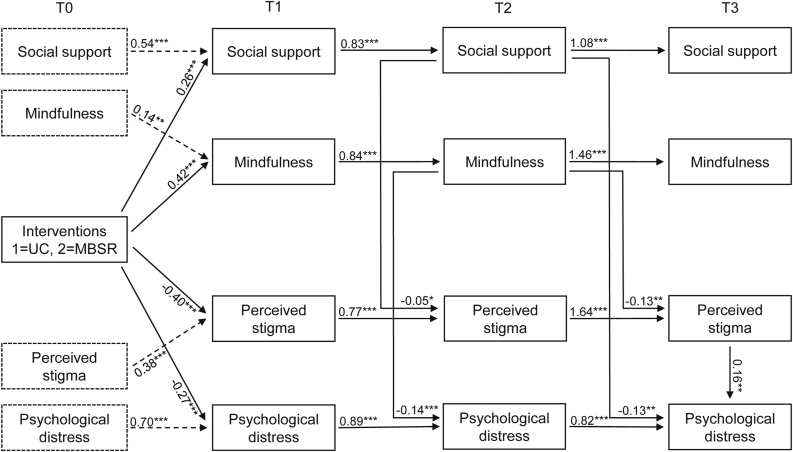
We only included three variables in the mediation analysis, including social support, mindfulness, and perceived stigma, according to predesigned criteria. After structural equation modeling and appropriate adjustment of the pathways between variables according to the modification index and empirical evidence, the model fitted our data better (χ2/df = 3.451, CFI = 0.893, TLI = 0.855, RMSEA = 0.122 [95% CI: 0.108–0.136]).
Overall, the effects of the 4-week MBSR program on psychological distress at T1, T2, and T3 were −0.274, −0.292, and −0.358, respectively. At the immediate postintervention (T1), the 4-week MBSR program alleviated psychological distress directly (β = −0.274, P = 0.005), not mediated by other variables. The effect of the 4-week MBSR program on mindfulness at T1 and T2 continued to help alleviate psychological distress at T2 (β = −0.049). The effects of the 4-week MBSR program on social support and mindfulness at T1 and T2 also continued to alleviate psychological distress at T3 by reducing perceived stigma at T2 and T3 (β = −0.039). The effect of the 4-week MBSR program on perceived stigma at T1, T2, and T3 also influenced psychological distress at T3 (β = −0.081). Moreover, there was a continuous effect between psychological distress from T1 to T3 (β = 0.886 from T1 to T2, β = 0.816 from T2 to T3), indicating that the 4-week MBSR program had a persistent effect on psychological distress (β = −0.198). The results of mediation analysis are summarized in Table 3, and the mechanism pathways are depicted in Fig. 4.
Table 3.
Path coefficient of variables in intervention mechanism analysis.
| Pathway | Β | 95% CI | P |
|---|---|---|---|
| Total effects | −0.924 | ||
| Psychological distress (T1) | −0.274 | −0.461 to −0.144 | 0.005 |
| Psychological distress (T2) | −0.292 | −0.434 to −0.715 | 0.005 |
| Psychological distress (T3) | −0.358 | −0.530 to −0.237 | 0.005 |
| Direct effects | −0.274 | −0.461 to −0.144 | 0.005 |
| Psychological distress (T1) | −0.274 | ||
| Indirect effects | −0.650 | ||
| Psychological distress (T2) | −0.292 | −0.434 to −0.175 | 0.005 |
| Intervention → Psychological distress (T1) → Psychological distress (T2) | −0.274∗0.886 = −0.243 | ||
| Intervention → Mindfulness (T1) → Mindfulness (T2) →Psychological distress (T2) | −0.141∗0.415∗0.844 = −0.049 | ||
| Psychological distress (T3) | −0.358 | −0.401 to −0.236 | 0.005 |
| Intervention → Psychological distress (T1) → Psychological distress (T2) → Psychological distress (T3) | −0.274∗0.886∗0.816 = −0.198 | ||
| Intervention → Mindfulness (T1) → Mindfulness (T2) → Perceived stigma (T3) → Psychological distress (T3) | −0.129∗0.415∗0.844∗∗0.160 = −0.007 | ||
| Intervention → Mindfulness (T1) → Mindfulness (T2) → Psychological distress (T2) → Psychological distress (T3) | −0.141∗0.415∗0.844∗0.816 = −0.040 | ||
| Intervention → Perceived stigma (T1) → Perceived stigma (T2) →Perceived stigma (T3) → Psychological distress (T3) | −0.403∗0.768∗1.639∗0.160 = −0.081 | ||
| Intervention → Social support (T1) → Social support (T2) → Psychological distress (T3) | −0.132∗0.264∗0.827∗ = −0.029 | ||
| Intervention → Social support (T1) → Social support (T2) → Perceived stigma (T2) → Perceived stigma (T3) → Psychological distress (T3) | −0.052∗0.264∗0.827∗1.639∗0.160 = −0.003 |
T1, immediate postintervention; T2, 1-month postintervention; T3, 3 months postintervention; β, standardized regression coefficients; CI, confidence interval.
Fig. 4.
Mechanism model of the 4-week MBSR program to alleviate psychological distress in patients with lung cancer. MBSR, mindfulness-based stress reduction.
Discussion
In this study, we aimed to validate the interventional effects of a 4-week MBSR program on psychological distress in patients with lung cancer and to further elucidate the psychosocial mechanisms by which the program alleviates psychological distress. Our findings suggest that the 4-week MBSR program, as an effective psychological intervention, significantly alleviates the psychological distress. The 4-week MBSR program also improved patients’ social support considerably, enhanced mindfulness, and reduced perceived stigma. Furthermore, the results of the structural equation modeling suggest that the 4-week MBSR program can exert an interventional effect by directly targeting psychological distress. Meanwhile, the 4-week MBSR program supports continuous interventional effects on psychological distress by indirectly affecting social support, mindfulness, and perceived stigma.
MBSR has been extensively used in cancer settings.31,33 Currently, many meta-analyses30,31,40,87,88 have demonstrated the benefits of MBSR program in improving the psychological well-being of patients with cancer. Furthermore, our recent meta-analysis confirmed that the MBSR program significantly diluted negative psychological states and enhanced positive psychological states. In this study, we further validated the beneficial role of the MBSR program in alleviating psychological distress in patients with lung cancer. Although it remains not entirely unclear why and how the MBSR program improves psychological well-being, previous studies35, 36, 37 suggest that the practice of mindfulness instructs participants to deliberately focus on the present moment and monitor the unfolding of experiences all the time without passing judgment. As a result, participants experience profound benefits through the mind-body connection. Thus, it is plausible that patients with lung cancer experience significant alleviation in psychological distress, improvement in social support, enhancement in mindfulness, and reduction in perceived stigma following a 4-week MBSR program.
This study also showed that the MBSR program had a retained effect on psychological distress after ending the intervention through indirect effects of social support, mindfulness, and perceived stigma. Both mindfulness89 and social support90 are positive sources for copying with negative psychological states, and our previous studies have demonstrated the inverse association between mindfulness and social support and psychological distress.15,56,58 In contrast, stigma, a negative emotional experience that includes isolation, rejection, degradation, and criticism due to undesirable conditions,77 has been demonstrated to be a predictor of psychological distress in patients with lung cancer.47 In general, psychosomatic balance plays a vital role in regulating the psychological well-being of patients with cancer.91 Therefore, patients would suffer from significant physical and psychological problems when specific events (eg, cancer diagnosis) destroyed psychosomatic balance.87
According to the Mindful Coping Model,92 we can easily explain why MBSR program can consistently affect psychological distress through social support, mindfulness, and perceived stigma. Specifically, the destructive effects of internal and external stressors (eg, cancer diagnosis, anticancer treatment, and symptom burden) can cause psychological distress in patients; however, the implementation of an MBSR program can initiate psychological adjustment to trigger or enhance the protective effects of positive sources (improvement in social support and enhancement in mindfulness) and weaken the harmful effects of negative sources (reduction in perceived stigma)93 and may then significantly dilute the destructive impacts of stressors (alleviation in psychological distress).94
Strengths and limitations
Overall, our study obtained these valuable findings due to several strengths. First, we enrolled both patients with clinically significant psychological distress and those at high risk of psychological distress by applying both DT and the risk prediction algorithm we developed, which significantly expanded the applicability of our findings in clinical practice. Second, we estimated the theoretical sample size from our meta-analysis, which ensured the statistical power of our results. Third, we explored the intervention mechanisms of the 4-week MBSR program by determining the role of significant variables after the intervention, which benefited more simply revealing the active ingredients of the 4-week MBSR program. Fourth, all potential mediating variables included in the intervention mechanism analysis have been previously investigated for their role in the development of psychological distress, increasing the reliability of theoretical evidence. Finally, our study was also rated as high in methodological quality because it met the six Cochrane collaboration criteria for high-quality trials,95 except that blinding participants due to the nature of the psychological intervention.
We cannot deny the fact that our study has several limitations. First and foremost, we used self-reported instruments to collect data, which may affect the accuracy of the results. Therefore, more objective tools need to be developed to measure these variables. Second, we recruited potentially eligible participants from only one hospital in southwest China due to the limited time. Therefore, we are unable to eliminate the adverse impact of selection bias and time constraints on our findings. As a result, adequately powered studies with more extended intervention and follow-up duration are warranted to demonstrate our findings. Third, we selected only those variables tested in our previous studies to explore possible mechanisms of the MBSR program on psychological distress. However, we did not consider those factors that we did not investigate previously. Therefore, more intervention mechanism analysis is needed to fully reveal the nature of MBSR program in alleviating psychological distress in patients with lung cancer. Fourth, we used a 4-week MBSR program with abbreviated sessions instead of a standard 8-week MBSR program in this study, which may have underestimated the intervention effect of the MBSR program due to inadequate duration of intervention. Therefore, future studies should further balance the interventional effects and applicability of the MBSR program in patients with lung cancer. More importantly, it is necessary to further investigate the interventional effects of the enhanced protocol with adequate sessions in future studies. Fifth, the mechanism model fitted our data relatively when we explored the intervention mechanism of the MBSR program to alleviate psychological distress, which limited the generalization of our results. Therefore, considering that limited participants were enrolled in our study, we suggest future studies with larger sample sizes to further elucidate the intervention mechanism of the MBSR program in alleviating psychological distress. Sixth, we chose brief versions of the scales to ensure the quality of the data collection process in this study; however, the average time for a patient to complete all scales was still up to 45 min. Although no patients were excluded for failing to complete scales, we could not eliminate the psychological burden caused by the need to complete multiple scales. Finally, in this study, we did not consider the impacts of sleep, fatigue, and exercise on the psychological status of patients with lung cancer. Therefore, we suggest future studies to address this limitation.
Conclusions
In summary, the present study validated the intervention effect of the MBSR program in alleviating psychological distress, and provided relatively robust and reliable evidence for clinical practitioners to integrate the MBSR program into usual care to improve psychological well-being of patients with lung cancer. Meanwhile, this study also suggested the positive effects of MBSR program on social support, mindfulness, and perceived stigma, which provided a reference for the application of MBSR program to improve clinical outcomes. Furthermore, this study revealed the direct impact of the MBSR program on short-term psychological distress. Additionally, it indicated the continuous effect of the MBSR program on psychological distress through social support, mindfulness, and perceived stigma.
Acknowledgements
The authors would like to acknowledge the funding support of the Chongqing Natural Science Foundation, the Basic Science and Frontier Technology Research Project of Chongqing, and the Medical Research Project which was jointly approved by the Chongqing Science and Technology Bureau and Health Commission of Chongqing Municipal City, China. The authors also thank the patients with lung cancer who participated in this study.
Author contributions
Conceived and designed the analysis: Xu Tian, Guihua Chen, María F. Jiménez Herrera.
Collected the data: Xu Tian, Zhongli Liao, Ling Tang.
Contributed data or analysis tools: Xu Tian, María F. Jiménez Herrera.
Performed the analysis: Xu Tian, Zhongli Liao, Lijuan Yi.
Wrote the paper: Xu Tian, Zhongli Liao, Guihua Chen, María F. Jiménez Herrera.
Declaration of competing interest
None declared.
Funding
This study was supported by the Chongqing Natural Science Foundation (Grant No. cstc2020jcyj-msxmX0212), the Basic Science and Frontier Technology Research Project of Chongqing (Grant No. cstc2048jcyjAX0775), and the Medical Research Project which was jointly approved by the Chongqing Science and Technology Bureau and Health Commission of Chongqing Municipal City (Grant No. 2022MSXM067).
Ethics statement
This study was approved by the Clinical Research Ethics Board of the Chongqing University Cancer Hospital (Approval No. CZLS2021183-A).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.apjon.2022.100151.
Contributor Information
Guihua Chen, Email: CMUSH_ChenGH@163.com.
María F. Jiménez Herrera, Email: maria.jimenez@urv.cat.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Sung H., Ferlay J., Siegel R.L., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Zheng R., Zhang S., Zeng H., et al. Cancer incidence and mortality in China, 2016. Journal of the National Cancer Center. 2022;2(1):1–9. doi: 10.1016/j.jncc.2022.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoffman B.M., Zevon M.A., D'Arrigo M.C., Cecchini T.B. Screening for distress in cancer patients: the NCCN rapid-screening measure. Psycho Oncol. 2004;13(11):792–799. doi: 10.1002/pon.796. [DOI] [PubMed] [Google Scholar]
- 4.Lee J. Physiologic and psychologic adaptation to exercise interventions in lung cancer patients undergoing chemotherapy: a systematic review and meta-analysis of randomized controlled trials. Supportive Care in Cancer. 2021 doi: 10.1007/s00520-020-05939-3. Official Journal of the Multinational Association of Supportive Care in Cancer. [DOI] [PubMed] [Google Scholar]
- 5.Gao W., Bennett M.I., Stark D., Murray S., Higginson I.J. Psychological distress in cancer from survivorship to end of life care: prevalence, associated factors and clinical implications. Eur J Cancer. 2010;46(11):2036–2044. doi: 10.1016/j.ejca.2010.03.033. [DOI] [PubMed] [Google Scholar]
- 6.Sun H., Thapa S., Wang B., Fu X., Yu S. A systematic review and meta-analysis of the distress thermometer for screening distress in asian patients with cancer. J Clin Psychol Med Settings. 2021;28(2):212–220. doi: 10.1007/s10880-020-09705-9. [DOI] [PubMed] [Google Scholar]
- 7.Grassi L., Johansen C., Annunziata M.A., et al. Screening for distress in cancer patients: a multicenter, nationwide study in Italy. Cancer. 2013;119(9):1714–1721. doi: 10.1002/cncr.27902. [DOI] [PubMed] [Google Scholar]
- 8.Vodermaier A., Linden W., MacKenzie R., Greig D., Marshall C. Disease stage predicts post-diagnosis anxiety and depression only in some types of cancer. Br J Cancer. 2011;105(12):1814–1817. doi: 10.1038/bjc.2011.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehnert A., Hartung T.J., Friedrich M., et al. One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psycho Oncol. 2018;27(1):75–82. doi: 10.1002/pon.4464. [DOI] [PubMed] [Google Scholar]
- 10.Funk R., Cisneros C., Williams R.C., Kendall J., Hamann H.A. What happens after distress screening? Patterns of supportive care service utilization among oncology patients identified through a systematic screening protocol. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2016;24(7):2861–2868. doi: 10.1007/s00520-016-3099-0. [DOI] [PubMed] [Google Scholar]
- 11.Zabora J., BrintzenhofeSzoc K., Curbow B., Hooker C., Piantadosi S. The prevalence of psychological distress by cancer site. Psycho Oncol. 2001;10(1):19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 12.Carlson L.E., Angen M., Cullum J., et al. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90(12):2297–2304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lynch J., Goodhart F., Saunders Y., O'Connor S.J. Screening for psychological distress in patients with lung cancer: results of a clinical audit evaluating the use of the patient Distress Thermometer. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2010;19(2):193–202. doi: 10.1007/s00520-009-0799-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chambers S.K., Baade P., Youl P., et al. Psychological distress and quality of life in lung cancer: the role of health-related stigma, illness appraisals and social constraints. Psycho Oncol. 2015;24(11):1569–1577. doi: 10.1002/pon.3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tian X., Jin Y., Chen H., Tang L., Jiménez-Herrera M.F. Relationships among social support, coping style, perceived stress, and psychological distress in Chinese lung cancer patients. Asia Pac J Oncol Nurs. 2021;8(2):172–179. doi: 10.4103/apjon.apjon_59_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen H., Gao J., Xian Y.Y., et al. Prevalence of psychological distress in patients with lung cancer:a meta-analysis [Chinese] Mod Prev Med. 2021;48(16):3059–3064. [Google Scholar]
- 17.Riba M.B., Donovan K.A., Andersen B., et al. Distress management, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2019;17(10):1229–1249. doi: 10.6004/jnccn.2019.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riba M.B., Donovan K.A., Andersen B., et al. Distress management, version 3.2019, NCCN clinical practice guidelines in oncology. Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw. 2019;17(10):1229–1249. doi: 10.6004/jnccn.2019.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mausbach B.T., Schwab R.B., Irwin S.A. Depression as a predictor of adherence to adjuvant endocrine therapy (AET) in women with breast cancer: a systematic review and meta-analysis. Breast Cancer Res Treat. 2015;152(2):239–246. doi: 10.1007/s10549-015-3471-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin C., Clark R., Tu P., Bosworth H.B., Zullig L.L. Breast cancer oral anti-cancer medication adherence: a systematic review of psychosocial motivators and barriers. Breast Cancer Res Treat. 2017;165(2):247–260. doi: 10.1007/s10549-017-4317-2. [DOI] [PubMed] [Google Scholar]
- 21.Yee M.K., Sereika S.M., Bender C.M., Brufsky A.M., Connolly M.C., Rosenzweig M.Q. Symptom incidence, distress, cancer-related distress, and adherence to chemotherapy among African American women with breast cancer. Cancer. 2017;123(11):2061–2069. doi: 10.1002/cncr.30575. [DOI] [PubMed] [Google Scholar]
- 22.Nipp R.D., El-Jawahri A., Moran S.M., et al. The relationship between physical and psychological symptoms and health care utilization in hospitalized patients with advanced cancer. Cancer. 2017;123(23):4720–4727. doi: 10.1002/cncr.30912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hockey M., Rocks T., Ruusunen A., et al. Psychological distress as a risk factor for all-cause, chronic disease- and suicide-specific mortality: a prospective analysis using data from the National Health Interview Survey. Soc Psychiatr Psychiatr Epidemiol. 2022;57(3):541–552. doi: 10.1007/s00127-021-02116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fox S.W., Lyon D.E. Symptom clusters and quality of life in survivors of lung cancer. Oncol Nurs Forum. 2006;33(5):931–936. doi: 10.1188/06.ONF.931-936. [DOI] [PubMed] [Google Scholar]
- 25.Batty G.D., Russ T.C., Stamatakis E., Kivimäki M. Psychological distress in relation to site specific cancer mortality: pooling of unpublished data from 16 prospective cohort studies. BMJ. 2017;356:j108. doi: 10.1136/bmj.j108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamer M., Chida Y., Molloy G.J. Psychological distress and cancer mortality. J Psychosom Res. 2009;66(3):255–258. doi: 10.1016/j.jpsychores.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y., Zanos P., Jackson I.L., et al. Psychological stress enhances tumor growth and diminishes radiation response in preclinical model of lung cancer. Radiother Oncol. 2020;146:126–135. doi: 10.1016/j.radonc.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 28.Howell D., Olsen K. Distress-the 6th vital sign. Curr Oncol. 2011;18(5):208–210. doi: 10.3747/co.v18i5.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galway K., Black A., Cantwell M., Cardwell C.R., Mills M., Donnelly M. Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients. Cochrane Database Syst Rev. 2012;11(11) doi: 10.1002/14651858.CD007064.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang H.P., He M., Wang H.Y., Zhou M. A meta-analysis of the benefits of mindfulness-based stress reduction (MBSR) on psychological function among breast cancer (BC) survivors. Breast Cancer. 2016;23(4):568–576. doi: 10.1007/s12282-015-0604-0. [DOI] [PubMed] [Google Scholar]
- 31.Cillessen L., Johannsen M., Speckens A.E.M., Zachariae R. Mindfulness-based interventions for psychological and physical health outcomes in cancer patients and survivors: a systematic review and meta-analysis of randomized controlled trials. Psycho Oncol. 2019;28(12):2257–2269. doi: 10.1002/pon.5214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kabat-Zinn J., Wheeler E., Light T., et al. Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemotherapy (PUVA) Psychosom Med. 1998;60(5):625–632. doi: 10.1097/00006842-199809000-00020. [DOI] [PubMed] [Google Scholar]
- 33.Lee C.E., Kim S., Kim S., Joo H.M., Lee S. Effects of a mindfulness-based stress reduction program on the physical and psychological status and quality of life in patients with metastatic breast cancer. Holist Nurs Pract. 2017;31(4):260–269. doi: 10.1097/HNP.0000000000000220. [DOI] [PubMed] [Google Scholar]
- 34.Yuan Y., Lin L., Xie C., et al. Effectiveness comparisons of various psychosocial therapies for cancer-related fatigue: a Bayesian network meta-analysis. J Affect Disord. 2022;309:471–481. doi: 10.1016/j.jad.2022.04.152. [DOI] [PubMed] [Google Scholar]
- 35.Kabat-Zinn J., Santorelli S. Center for Mindfulness in Medicine. Health Care, and Society, UMMS; Boston: 2002. Mindfulness-Based Stress Reduction Professional Training-Scientific Papers from the Stress Reduction Clinic. [Google Scholar]
- 36.Kabat-Zinn J., Lipworth L., Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8(2):163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- 37.Kabat-Zinn J. 2003. Mindfulness-based Interventions in Context: Past, Present, and Future. [Google Scholar]
- 38.Kabat-Zinn J., Massion A.O., Kristeller J., et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatr. 1992;149(7):936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 39.Xie C., Dong B., Wang L., et al. Mindfulness-based stress reduction can alleviate cancer- related fatigue: a meta-analysis. J Psychosom Res. 2020;130 doi: 10.1016/j.jpsychores.2019.109916. [DOI] [PubMed] [Google Scholar]
- 40.Xunlin N.G., Lau Y., Klainin-Yobas P. The effectiveness of mindfulness-based interventions among cancer patients and survivors: a systematic review and meta-analysis. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2020;28(4):1563–1578. doi: 10.1007/s00520-019-05219-9. [DOI] [PubMed] [Google Scholar]
- 41.van den Hurk D.G., Schellekens M.P., Molema J., Speckens A.E., van der Drift M.A. Mindfulness-Based Stress Reduction for lung cancer patients and their partners: results of a mixed methods pilot study. Palliat Med. 2015;29(7):652–660. doi: 10.1177/0269216315572720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schellekens M.P.J., van den Hurk D.G.M., Prins J.B., et al. Mindfulness-based stress reduction added to care as usual for lung cancer patients and/or their partners: a multicentre randomized controlled trial. Psycho Oncol. 2017;26(12):2118–2126. doi: 10.1002/pon.4430. [DOI] [PubMed] [Google Scholar]
- 43.Sgalla G., Cerri S., Ferrari R., et al. Mindfulness-based stress reduction in patients with interstitial lung diseases: a pilot, single-centre observational study on safety and efficacy. BMJ open respiratory research. 2015;2(1) doi: 10.1136/bmjresp-2014-000065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arefnasab Z., Ghanei M., Noorbala A.A., et al. Effect of mindfulness based stress reduction on quality of life (SF-36) and spirometry parameters, in chemically pulmonary injured veterans. Iran J Public Health. 2013;42(9):1026–1033. [PMC free article] [PubMed] [Google Scholar]
- 45.Tian X., Yi L.J., Liang C.S.S., et al. The impact of mindfulness-based stress reduction (MBSR) on psychological outcomes and quality of life in lung cancer patients: a meta-analysis. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.901247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Matzka M., Mayer H., Köck-Hódi S., et al. Relationship between resilience, psychological distress and physical activity in cancer patients: a cross-sectional observation study. PLoS One. 2016;11(4) doi: 10.1371/journal.pone.0154496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rose S., Boyes A., Kelly B., Cox M., Palazzi K., Paul C. Lung cancer stigma is a predictor for psychological distress: a longitudinal study. Psycho Oncol. 2021;30(7):1137–1144. doi: 10.1002/pon.5665. [DOI] [PubMed] [Google Scholar]
- 48.Segrin C., Badger T.A., Sikorskii A., et al. Longitudinal dyadic interdependence in psychological distress among Latinas with breast cancer and their caregivers. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2020;28(6):2735–2743. doi: 10.1007/s00520-019-05121-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lv X.Q., Wang B.Q., Tong H.H., Liu S.S., Tang H.J., Hong J.F. Predictive model of psychological distress in patients with lung cancer: a cross-sectional study. Cancer Nurs. 2022;45(1):E59–e67. doi: 10.1097/NCC.0000000000000837. [DOI] [PubMed] [Google Scholar]
- 50.Liu Y., Cao C. The relationship between family history of cancer, coping style and psychological distress. Pakistan J Med Sci. 2014;30(3):507–510. doi: 10.12669/pjms.303.4634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.den Heijer M., Seynaeve C., Vanheusden K., et al. The contribution of self-esteem and self-concept in psychological distress in women at risk of hereditary breast cancer. Psycho Oncol. 2011;20(11):1170–1175. doi: 10.1002/pon.1824. [DOI] [PubMed] [Google Scholar]
- 52.Schellekens M.P.J., Karremans J.C., van der Drift M.A., et al. Are mindfulness and self-compassion related to psychological distress and communication in couples facing lung cancer? A dyadic approach. Mindfulness (N Y) 2017;8(2):325–336. doi: 10.1007/s12671-016-0602-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cho D., Kim S., Durrani S., Liao Z., Milbury K. Associations between spirituality, mindfulness, and psychological symptoms among advanced lung cancer patients and their spousal caregivers. J Pain Symptom Manag. 2021;61(5):898–908.e1. doi: 10.1016/j.jpainsymman.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang N., Fielding R., Soong I., et al. Illness perceptions as predictors of psychological distress among head and neck cancer survivors: a longitudinal study. Head Neck. 2018;40(11):2362–2371. doi: 10.1002/hed.25343. [DOI] [PubMed] [Google Scholar]
- 55.Zhang Z., Yang L., Xie D., et al. Illness perceptions are a potential predictor of psychological distress in patients with non-muscle-invasive bladder cancer: a 12-month prospective, longitudinal, observational study. Psychol Health Med. 2020;25(8):969–979. doi: 10.1080/13548506.2019.1707242. [DOI] [PubMed] [Google Scholar]
- 56.Tian X., Jin Y., Chen H., Tang L., Jiménez-Herrera M.F. The positive effect of social support on psychological distress among Chinese lung cancer patients: the mediating role of self-esteem. Nurs Open. 2021;8(4):1642–1651. doi: 10.1002/nop2.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lei H., Tian X., Jin Y.F., Tang L., Chen W.Q., Jiménez-Herrera M.F. The chain mediating role of social support and stigma in the relationship between mindfulness and psychological distress among Chinese lung cancer patients. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2021;29(11):6761–6770. doi: 10.1007/s00520-021-06278-7. [DOI] [PubMed] [Google Scholar]
- 58.Tian X., Tang L., Yi L.J., Qin X.P., Chen G.H., Jiménez-Herrera M.F. Mindfulness affects the level of psychological distress in patients with lung cancer via illness perception and perceived stress: a cross-sectional survey study. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.857659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Walker J., Sawhney A., Hansen C.H., et al. Treatment of depression in people with lung cancer: a systematic review. Lung Cancer. 2013;79(1):46–53. doi: 10.1016/j.lungcan.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 60.Hong J., Wei Z., Wang W. Preoperative psychological distress, coping and quality of life in Chinese patients with newly diagnosed gastric cancer. J Clin Nurs. 2015;24(17-18):2439–2447. doi: 10.1111/jocn.12816. [DOI] [PubMed] [Google Scholar]
- 61.Donovan K.A., Grassi L., McGinty H.L., Jacobsen P.B. Validation of the distress thermometer worldwide: state of the science. Psycho Oncol. 2014;23(3):241–250. doi: 10.1002/pon.3430. [DOI] [PubMed] [Google Scholar]
- 62.Tian X., Jin Y., Tang L., Pi Y.-P., Chen W.-Q., Jimenez-Herrera M.F. Predicting the risk of psychological distress among lung cancer patients: development and validation of a predictive algorithm based on sociodemographic and clinical factors. Asia-Pacific Journal of Oncology Nursing. 2021;8(4):403–412. doi: 10.4103/apjon.apjon-2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zimet G.D., Powell S.S., Farley G.K., Werkman S., Berkoff K.A. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3-4):610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 64.Yang J., Li S., Zheng Y. Predictors of depression in Chinese community-dwelling people with type 2 diabetes. J Clin Nurs. 2009;18(9):1295–1304. doi: 10.1111/j.1365-2702.2008.02703.x. [DOI] [PubMed] [Google Scholar]
- 65.Feifel H., Strack S. Coping with conflict situations: middle-aged and elderly men. Psychol Aging. 1989;4(1):26–33. doi: 10.1037//0882-7974.4.1.26. [DOI] [PubMed] [Google Scholar]
- 66.Shen X.H., Jiang J.Q. Report on application of Chinese version of MCMQ in 701 patients. Chinese Journal of Behavioral Medical Science. 2000;9(1):18–20. [Google Scholar]
- 67.Rosenberg M., Schooler C., Schoenbach C. Self-esteem and adolescent problems: modeling reciprocal effects. Am Socio Rev. 1989;54(6):1004–1018. [Google Scholar]
- 68.Wu Y., Zuo B., Wen F., Yan L. Rosenberg self-esteem scale: method effects, factorial structure and scale invariance across migrant child and urban child populations in China. J Pers Assess. 2017;99(1):83–93. doi: 10.1080/00223891.2016.1217420. [DOI] [PubMed] [Google Scholar]
- 69.Cai Z., Gui Y., Wang D., Yang H., Mao P., Wang Z. Body image dissatisfaction and impulse buying: a moderated mediation model. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.653559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Qian Y., Yu X., Liu F. Comparison of two approaches to enhance self-esteem and self-acceptance in Chinese college students: psychoeducational lecture vs. Group intervention. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.877737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Xiao X., Zheng X. The effect of parental phubbing on depression in Chinese junior high school students: the mediating roles of basic psychological needs satisfaction and self-esteem. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.868354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Baer R.A., Smith G.T., Hopkins J., Krietemeyer J., Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 73.Deng Y.-Q., Liu X.-H., Rodriguez M.A., Xia C.-Y. The five facet mindfulness questionnaire: psychometric properties of the Chinese version. Mindfulness. 2011;2(2):123–128. [Google Scholar]
- 74.Fong T.C.T., Wan A.H.Y., Wong V.P.Y., Ho R.T.H. Psychometric properties of the Chinese version of Five Facet Mindfulness Questionnaire-short form in cancer patients: a Bayesian structural equation modeling approach. Health Qual Life Outcome. 2021;19(1):51. doi: 10.1186/s12955-021-01692-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 76.Yuan L.X., Lin N. Research on factor structure of perceived stress scale in Chinese college students (in Chinese) Journal of Guangdong Education Institute. 2009;29(2):45–49. [Google Scholar]
- 77.Cataldo J.K., Slaughter R., Jahan T.M., Pongquan V.L., Hwang W.J. Measuring stigma in people with lung cancer: psychometric testing of the catalog lung cancer stigma scale. Oncol Nurs Forum. 2011;38(1):E46–E54. doi: 10.1188/11.ONF.E46-E54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yu Y., Wang L., Zhang M., Du Y.H., Bai Y., Liu J.E. Psychometric evaluation of the Chinese version of the cataldo lung cancer stigma scale (CLCSS) Chin J Nurs. 2017;52(5):636–640. [Google Scholar]
- 79.Weinman J., Petrie K.J., Moss-Morris R. The Illness Perception Questionnaire: a new method for assessing illness perceptions. Psychol Health. 1996;1:431–446. [Google Scholar]
- 80.Broadbent E., Petrie K.J., Main J., Weinman J. The brief illness perception questionnaire. J Psychosom Res. 2006;60(6):631–637. doi: 10.1016/j.jpsychores.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 81.Xue F, Lin Y. Brief illness perception questionnaire: Chinese version. Available at: www.uib.no/ipq/pdf/B-IPQ-Chinese.pdf.
- 82.Zhang N., Fielding R., Soong I., et al. Psychometric assessment of the Chinese version of the brief illness perception questionnaire in breast cancer survivors. PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0174093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Schaefert R., Höner C., Salm F., et al. Psychological and behavioral variables associated with the somatic symptom severity of general hospital outpatients in China. Gen Hosp Psychiatr. 2013;35(3):297–303. doi: 10.1016/j.genhosppsych.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 84.Steinskog D.J., Tjøstheim D.B., Kvamstø N.G. A cautionary note on the use of the Kolmogorov–smirnov test for normality. Mon Weather Rev. 2007;135(3):1151–1157. [Google Scholar]
- 85.Kim H.-Y. Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor Dent Endod. 2013;38(1):52–54. doi: 10.5395/rde.2013.38.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shenk C.E., Putnam F.W., Rausch J.R., Peugh J.L., Noll J.G. A longitudinal study of several potential mediators of the relationship between child maltreatment and posttraumatic stress disorder symptoms. Dev Psychopathol. 2014;26(1):81–91. doi: 10.1017/S0954579413000916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhang Q., Zhao H., Zheng Y. Effectiveness of mindfulness-based stress reduction (MBSR) on symptom variables and health-related quality of life in breast cancer patients-a systematic review and meta-analysis. Support Care Cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2019;27(3):771–781. doi: 10.1007/s00520-018-4570-x. [DOI] [PubMed] [Google Scholar]
- 88.Haller H., Winkler M.M., Klose P., Dobos G., Kümmel S., Cramer H. Mindfulness-based interventions for women with breast cancer: an updated systematic review and meta-analysis. Acta Oncol. 2017;56(12):1665–1676. doi: 10.1080/0284186X.2017.1342862. [DOI] [PubMed] [Google Scholar]
- 89.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10(2):144–156. [Google Scholar]
- 90.Teixeira R.J., Pereira M.G. Psychological morbidity, burden, and the mediating effect of social support in adult children caregivers of oncological patients undergoing chemotherapy. Psycho Oncol. 2013;22(7):1587–1593. doi: 10.1002/pon.3173. [DOI] [PubMed] [Google Scholar]
- 91.Bãrbuş E., Peştean C., Larg M.I., Piciu D. Quality of life in thyroid cancer patients: a literature review. Clujul Med. 2017;90(2):147–153. doi: 10.15386/cjmed-703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Garland E., Gaylord S., Park J. The role of mindfulness in positive reappraisal. Explore. 2009;5(1):37–44. doi: 10.1016/j.explore.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jeffers L., Reid J., Fitzsimons D., Morrison P.J., Dempster M. Interventions to improve psychosocial well-being in female BRCA-mutation carriers following risk-reducing surgery. Cochrane Database Syst Rev. 2019;10(10) doi: 10.1002/14651858.CD012894.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Galante J., Friedrich C., Dawson A.F., et al. Mindfulness-based programmes for mental health promotion in adults in nonclinical settings: a systematic review and meta-analysis of randomised controlled trials. PLoS Med. 2021;18(1):e1003481–e. doi: 10.1371/journal.pmed.1003481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Higgins J.P.T., Altman D.G., Gøtzsche P.C., et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ (Clinical research ed) 2011;343:d5928–d. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.