Abstract
Across the globe, disordered eating disorders alarmingly have increased by over 30% in the general public, as characterised by a wide range of eating, shape and weight concerns. Subsequent physical, functional, social, and mental health issues significantly burden society, conveying various personal sufferings to affected individuals. Disordered eating behaviours and cognitions can increase to clinical severity, such as anorexia nervosa and bulimia nervosa. The present study critically reviewed over 100 major papers on disordered eating to integrate theoretical underpinnings and explore practical insights. The review resulted in identifying seven major theories concerning the development and persistence of disturbed eating behaviour. These include self-esteem theory, interpersonal theory, emotion regulation theory, executive function theory, social neuroscience theory, theory of mind, and trans-diagnostic theory. Furthermore, depression, anxiety, social norms and family functioning also emerged as major psychological and social correlates of disordered eating. The results further suggested significant research gaps and inconsistencies, including directional ambiguity between self-esteem and body dissatisfaction, self-esteem and depression, and executive functioning and eating, as well as mixed findings pertaining to theory of mind deficits, such as perspective taking and emotion recognition, and family functioning. Prospective empirical studies should incorporate these complexities and investigate underlying multiple psychological mediation mechanisms, preferably with experimental designs and longitudinal studies for further causal explanations.
Keywords: Eating disorders, Anorexia, Bulimia, Self-esteem, Trans-diagnostic theory, Emotion regulation, Executive function, Theory of mind
Eating disorders; Anorexia; Bulimia; Self-esteem; Trans-diagnostic theory; Emotion regulation; Executive function; Theory of mind.
Disordered eating includes a spectrum of eating, shape and weight concerns that can manifest in problems of clinical severity such as anorexia nervosa (AN), bulimia nervosa (BN), binge eating and obesity (American Psychiatric Association [APA], 2013; Hirst et al., 2017). To define, AN is a psychological disorder characterised by perceptual distortions of body image, weight gain fixations, excessive exercise and starvation with restrictive food intake. BN is characterised by recurrent binge eating episodes accompanied by purging behaviours, such as self-induced vomiting (Bora and Kose, 2016). Such maladaptive eating habits are often associated with a lifelong difficulty to manage symptomatology (Hirst et al., 2017) presenting further concerns during the COVID-19 pandemic (Christensen et al., 2021; Stewart et al., 2021; Touyz et al., 2020; Weissman et al., 2020). Across the globe, alarming increases in disordered eating and subsequent physical, functional, social and mental health issues significantly burden affected individuals and the wider society (Udo and Grilo, 2018). To illustrate, relative to earlier decades, in the past two decades, statistics indicated approximately 7 times more individuals with obesity (33%) and 11 times more people with restrictive dieting or pathological fasting (5%) in South Australian community samples (Da Luz et al., 2017). The prevalence of eating disorders (4–16%) is predominantly seen in females (Bora and Kose, 2016; Da Luz et al., 2017; Udo and Grilo, 2018; van Eeden et al., 2021; Ward et al., 2019), with gender ratios ranging from 1:4 to 1:10, depending on the source and method (Murray, 2017). In tackling these societal health concerns, a plethora of psychological theories have been proposed to explain disordered eating with their unique approaches.
The present study reviewed surging literature and accumulating evidence through clinical, cognitive and neural studies to better address a wide range of factors influencing the development and maintenance of problematic eating behaviour. Previous literature from more than 100 academic papers and book chapters revealed the most salient seven theories. These were self-esteem theory, interpersonal theory, emotion regulation theory, executive function theory, social neuroscience theories, theory of mind, and trans-diagnostic theory across various eating disorders (Bora and Kose, 2016; Ciarma and Mathew, 2017; Claudat et al., 2016; Fairburn et al., 2003; Xu et al., 2017). Therefore, with a focus on females, the current literature review further evaluated and incorporated existing conceptual evidence and related the main theories to more comprehensively explore how disordered eating behaviour would develop and continue. Moreover, other risk and preventive variables of psychological and social correlates appeared to contribute to the perpetuation of dysfunctional eating. They included depression, anxiety, social norms and family functioning. Finally, this review addressed research gaps and provided implications for prospective study and practical interventions.
1. Theories of eating behaviour
The present review has found that the huge research field on disordered eating presents a complex and convoluted theoretical terrain ranging from cognitive motivations to neuroscientific evidence.
To explain the issue as to why individuals would experience challenges to their basic existential behaviour of eating, seven theories appeared to direct research and practical strategies as reviewed in the following.
1.1. Self-esteem theory and body dissatisfaction
First and foremost, concerning the most fundamental human need and motivation variable, self-esteem theory posits a central explanation that individuals with low self-esteem maintain exacerbated body shape concerns, resulting in disturbed eating behaviour (Claudat et al., 2016; Fairburn et al., 2003; Shea and Pritchard, 2007). Self-esteem is defined as an individual's overall evaluation of self (Rosenberg, 1965). It is a person's subjective appraisal of their self-worth and self-confidence, and the extent to which an individual upholds positive or negative views about themselves (Sedikides and Gress, 2003). The lowest levels of self-esteem have been found in individuals with pathological eating disorders, hence depicting a vicious cycle between self-esteem and the development of this psychological concern (Silverstone and Salsali, 2003) with some bidirectional evidence in longitudinal adolescent samples (Espinoza et al., 2019). Notably, evidence reports negative correlations between self-esteem and problematic eating in both clinical and non-clinical community samples (Lampard et al., 2013; Zamani Sani et al., 2020).
More specifically, a strong associate of diminished self-esteem is body dissatisfaction (Franko and Striegel-Moore, 2007) rather than actual overweight condition (Ozmen et al., 2007), suggesting a responsible cognitive factor for disordered eating. Body dissatisfaction has been one of the strongest predictors of dysfunctional eating symptomatology across differing societies (O'Hara et al., 2016; Teixeira et al., 2016). As a prevalent parallel, body dissatisfaction is often observed as a mediator of the impact of self-esteem upon maladaptive eating (Lim and You, 2017). Specifically, the association between self-esteem with abnormal eating behaviour was not significant whereas lower self-esteem explained why some college students were less likely to be satisfied with their body image. This body dissatisfaction subsequently explained their difficulties in regulating eating which suggested mediated indirect effects of self-esteem. However, these findings embed limitations that do not distinguish between the distinct dieting and bulimia subscale variables. Additionally, suggesting a reversed mediation direction, Brechan and Kvalem (2015) found that both body dissatisfaction and self-esteem had direct effects on restrained eating, whereas body dissatisfaction had an indirect/mediating effect on binge eating through self-esteem as the proximal variable. Specifically, body dissatisfaction explained poor self-esteem which in turn predicted binge eating. While body dissatisfaction paired with reduced self-esteem is evidently a potent risk for both clinical and subclinical dysfunctional eating behaviours (Franko and Striegel-Moore, 2007), further research should examine if the causal direction is reciprocal or bidirectional between these two variables. Although these intrapersonal individual self-perceptions influence our eating, those with disordered eating further display disparities in social perceptions, interpersonal evaluations and related emotion regulation (McAdams et al., 2016), as follows.
1.2. Interpersonal theory and emotion regulation theory
Interpersonal theory and emotional regulation theory explain social factors, as individuals often engage in dysfunctional eating as maladaptive stress responses to interpersonal problems and emotional stress reactivity (Ansell et al., 2012; Ciarma and Mathew, 2017; Rieger et al., 2010; Scholtz et al., 2011). Ciarma and Mathew (2017) suggest interpersonal conflicts and negative social appraisals, such as others’ evaluations, act as a mediator of the impact of social anxieties upon problematic eating. Likewise, Tuschen-Caffier and Vögele (1999) demonstrated in an experimental study that inducing interpersonal stresses through imagery characterising negative social evaluations, resulted in an increase in disordered eating desire and adverse social cognitions such as insecurity, low self-worth and sadness for BN patients. Accompanying no change in restrained eaters and controls, the results indicate stressful interpersonal conflicts may contribute to the elicitation of subclinical bulimic symptomatology. Relations between negative social cognitions/evaluations and eating is largely exacerbated by individual differences to stress reactivity in conjunction with the regulation of emotionality (Hinrichsen et al., 2003).
According to emotion regulation theory, stress reactivity is explained as interpreting external situations as unmanageable and precarious (Scholtz et al., 2011). Multiple theories provide some comprehensive explanation as to why those who experience diminished self-esteem during self or social evaluations as well as feelings of anxiety during interpersonal conflicts (Scholtz et al., 2011), often have difficulty regulating emotional stress reactivity and overall affect (Delinsky and Wilson, 2008). Nonetheless, supporting the experimental evidence (Tuschen-Caffier & Vögele, 1999), research argues that emotion regulation differs across the eating disorder groups. It is suggested that individuals with BN and related tendencies typically numb negative emotions through binge eating and compensatory behaviours (Dallman, 2010). Conversely, those with AN and associated habits attempt to enhance their sense of emotional and self-regulation through extremely restrictive dieting (Hatch et al., 2010). Recently prevention and intervention frameworks aim to improve interpersonal emotion regulations with specifying the regulation processes in terms of situation, attention, cognitive change and response modulation for individuals with disordered eating (Christensen and Haynos, 2020). Through their theoretical review, the researchers discussed therapeutic interpersonal interactions with positive support and non-judgemental attitudes as well as dialectical behavioural therapy to deal with distress tolerance and emotion regulation. Despite the fact that variations between AN and BN warrant further research on interpersonal emotion regulation, these eating disorder groups share similar psychological and cognitive disturbances, as addressed in the following.
1.3. Transdiagnostic theory
A more profound theoretical insight into disordered eating is addressed by transdiagnostic theory. It is proposed that the various eating disorders and behaviours share common psychological disturbances (Fairburn et al., 2003) with the core cognitive concern being unduly influenced by body shape and weight. To illustrate, substantial evidence depicts shared mechanisms, like body dissatisfaction, in explaining both restricted eating and binge eating behaviours (Karazsia et al., 2016). It is theoretically interesting and practically important that the same psychological factors can explain opposite ends of the eating behaviour continuum. Thus, factors like body dissatisfaction should be a treatment focus for both eating disorder types (Karazsia et al., 2016). More recent evidence supported the Fairburn transdiagnostic model by revealing the central role of perfectionism, over-vigilance and inhibition, and ineffectiveness symptoms suggesting interventions to improve cognitive flexibility and self-compassion techniques (Vervaet et al., 2020).
Further, commonalities in neural processing of social concepts like self-perception and social evaluations, have been observed between AN and BN subjects, when compared with healthy controls (McAdams et al., 2016). In terms of cognitive functioning, Fagundo et al. (2012) posited that patients with AN and those with compulsive unhealthy eating share similar executive dysfunctions in areas such as cognitive flexibility, planning and shifting capacities, impulse control, decision-making, and attention. As a resultant, these impairments influence the persistence of such eating behaviours. This finding has been further validated by Hirst et al. (2017) in a meta-analysis, revealing a homogeneity of outcomes when investigating impairments of executive functioning profiles within AN and BN samples. Impediments explored were similar to that of Fagundo et al. (2012), as depicted further in the following paragraphs. In summary, collective evidence demonstrates support for psychological, neurological and cognitive transdiagnostic mechanisms involved in the spectrum of eating behaviours. Ultimately, transdiagnostic deficits associated with problematic eating are frequently observed in executive functioning, as follows.
1.4. Executive function theory
Executive functioning (EF) refers to interrelated higher-order top-down cognitive processes that allow control over behaviours. Basic facets include updating, inhibitory control and mental shifting/cognitive flexibility. More specific functions include problem solving, working memory, attention control and emotion regulation (Dohle et al., 2018; Eichen et al., 2017). EF is typically a transdiagnostic process that provides explanations for the inability to control food intake (Perpina and Sanchez-Reales, 2017). For example, a high level of meta-cognition is needed to control behaviour and emotion regulation, but people with various eating disorders fail to appropriately regulate their eating (Hirst et al., 2017). Although other components exist, it is well-documented that impaired inhibitory control, or impulsivity, plays a critical role in the development and maintenance of dysfunctional eating behaviour (Guerrieri et al., 2009; Limbers and Young, 2015; Nederkoorn et al., 2010). However, as demonstrated by Fagundo et al. (2012) and Hirst et al. (2017), executive deficits are not limited solely to inhibition.
Hirst et al. (2017) proved that small to moderate impairments of EF occurred in those with AN, and moderate to large impairments of EF occurred in individuals with BN. Those impairments included cognitive flexibility, planning and shifting capacities, impulsivity, decision-making, attention as well as processing speed and global processing, as briefly mentioned earlier. Although significant differences in EF are evident between women with eating disorders and healthy controls, Billingsley-Marshall et al. (2013) found that executive dysfunctions were restricted to only a small number of women with disordered eating in their sample of 106 inpatients. These mixed findings indicate that the role of cognitive impairments in clinical and subclinical disordered eating symptomatology is somewhat uncertain at present Rania et al. (2021). Hence, further empirical research is required to investigate the association between symptoms and the disruption of EF, while encompassing all specific components (Hirst et al., 2017). Additionally, the directionality of the relation between eating disorders and EF is also undetermined (Favieri et al., 2019). Dohle et al.’s (2018) comprehensive literature review proposed that eating behaviour may act as a predictor of EF, and inversely, EF may predict eating behaviour. Furthermore, it was suggested EF may play moderating/mediating roles in the impact of desires or automatic attitudes upon eating behaviour. Such conclusions depict a bidirectional relationship between EF and disordered eating. Additional experimental research and longitudinal designs to test mediation and moderation effects is needed to potentially resolve such directional ambiguity, subsequently assisting with provision of more efficient and tailored treatment.
In summary, research suggests EF is a transdiagnostic process (Fairburn et al., 2003; Perpina and Sanchez-Reales, 2017) that contributes to the excessive or inefficient regulation of eating behaviour to different extents (Dohle et al., 2018). However, the direction of this association is still unclear (Favieri et al., 2019). When the associations between executive functions and obesity and overeating behaviours were reviewed the mixed evidence was inconclusive if impaired EF caused overeating or overeating impacted on sound EF such as emotional regulation and judgement etc. In addition to the psychological, interpersonal, transdiagnostic, and cognitive perspectives explaining eating behaviour explored above, the following paragraphs consider a social neuroscience perspective and a developmental perspective coined theory of mind (ToM).
1.5. Social neuroscience theory
Social neuroscience theories have shown brain activations and variations in responding to social cues, such as physical self-perception and social evaluations, were distinct in people with eating disorders, and on recovery, when compared to controls (McAdams et al., 2016; Xu et al., 2017). In particular, Xu et al. (2017) found adolescent girls with AN showed differences in the activation and fMRI measurements of frontal lobe brain regions during social appraisals, which is suggested to contribute to body shape concerns. The Social Identity-V2 Task (McAdams et al., 2016) was used to measure social appraisals. It involved self-evaluations (E.g., “I believe I am deceitful”), friend-evaluations (E.g., “I believe my friend is moody”) and perspective-taking self-evaluations (E.g., “My friend believes I am proud”). As such, neural variations associated with these interpersonal evaluations provide clinical predictive value as women develop and progress into adulthood. Likewise, a study of 17 women with BN, 18 with recent history of AN and 18 healthy controls discovered that when undertaking fMRI interpersonal and self-knowledge tasks requiring social processing, the neural activations of BN patients were comparable to, and not significantly different from, those with AN. Similarities were apparent in domains such as self-liking, social problem solving, levels of avoidance as well as comparable activations during social attribution, social identity and physical identity tasks. Both groups differed from the neural modulations in the right temporo-parietal junction, the precuneus, and dorsal and ventral anterior cingulate observed in healthy individuals (McAdams and Krawczyk, 2013). Notably though, cognitions pertaining to physical appearance were slightly more stable in women with BN than AN. Despite a marginal difference in body appearance concerns, these findings demonstrate several important similarities in neural processing and thus are transdiagnostic in nature, thereby suggesting biological mechanisms are largely involved in processing social concepts for both disordered eating groups (McAdams and Krawczyk, 2013). Prospectively, interventions acknowledging biological components of social processing/evaluations may elicit more effective treatment outcomes, subsequently assisting with achieving sustained recovery in women with eating disorders (Luo et al., 2021). The list of above alluded theories of disordered eating continues to include some developmental theory as follows, particularly the notion of perspective-taking.
1.6. Theory of mind (ToM)
Last but not least, a developmental psychology perspective, ToM, is described as an individual's capacity to make decisive inferences about other people's mental states, thoughts, beliefs and emotions. It involves processing complex affective stimuli and social cognitions (Bora and Kose, 2016; Stone et al., 1998). ToM addresses the rigidity and impairment in taking others' perspectives with proper emotion recognition and realistic understanding displayed in sufferers of disordered eating (Bora and Kose, 2016; Zegarra-Valdivia and Chino-Vilca, 2018). Specifically, in a meta-analysis of 15 studies involving 677 individuals with AN and BN and 514 healthy controls, Bora and Kose (2016) found women with AN suffer significant ToM deficits like perspective-taking, poor insight, decoding mental states and social impairment. In contrast, individuals with BN showed negligible deficits, or none at all. This finding is experimentally supported by Pereira de Sampaio et al. (2013), who assessed ToM in 65 women using the Reading the Mind in the Eyes Test (RMET). AN patients displayed poorer performance in emotion recognition and social cognition, whereas those with BN showed no difference to controls. Contradictorily, also with the RMET measurement, Medina-Pradas et al. (2012) claimed BN patients displayed difficulties interpreting complex emotions in others, while AN patients had no difficulties of this nature. The more viable results may be from Bora and Kose's (2016) meta-analysis being consistent with Pereira de Sampaio et al. (2013), by presenting the more recent analyses with considerable evidence from 22 samples with eating disorders (N = 1,191). Accordingly, mixed results pertaining to ToM deficits warrants further empirical study (Laghi et al., 2021) into emotion recognition profiles of patients with disordered eating.
2. Correlated variables of disordered eating
2.1. Depression and anxiety
Eating disorders, with their increasing prevalence (Da Luz et al., 2017; van Eeden et al., 2021), represent a major public health burden given they are often concurrently associated with other psychopathology (Hudson et al., 2007). Several studies yielded consistent findings demonstrating depression and anxiety is significantly greater in those with AN or BN, compared to healthy controls (Billingsley-Marshall et al., 2013; Perpina and Sanchez-Reales, 2017; Villarejo et al., 2014). Specifically, more than 90% of patients have a co-morbid mood disorder like depression, and approximately 67% have past experiences of anxiety in a 5-year sample of 2436 eating-disordered inpatients (Billingsley-Marshall et al., 2013; Blinder et al., 2006). Such high rates of psychiatric comorbidities may provide various explanations for maladpative eating behaviours. Interestingly, Lim and You (2017) proposed depression did not have a direct effect on abnormal eating such as restrictive dieting, rather, had an indirect/mediating effect through body dissatisfaction. Specifically, low self-esteem concurrent with high depression eventuates to higher levels of body dissatsifaction, and in turn, is associated with increased dysfunctional eating. Notably, evidence also supports the conclusions that low-esteem impacts depression, and inversely, depression can erode self-esteem (Orth and Robins, 2013) as the central mechanism perpetuating disturbed eating (Shea and Pritchard, 2007). In a cognitive sense, few studies have investigated the clinically predictive nature of depression and anxiety relative to EF (Billingsley-Marshall et al., 2013) However, Roberts et al. (2010) asserted that depressive and anxiety symptomatology can hinder set-shifting abilities in eating-disordered individuals. This study used four measures of EF set-shifting, including the Trail Making Test (Reitan, 1955), Wisconsin Card Sorting Test (Heaton et al., 1993), Brixton Task (Burgess and Shallice, 1997) and the Haptic Illusion (Tchanturia et al., 2004). They concluded that diminished mental flexibility/set-shifting capacity was a core consequence of the impact of depression and anxiety upon EF. These results indicate the inability to cognitively regulate appropriate eating behaviour and maintain healthy habits is further impeded by such psychological comorbidities.
The presence of depression and anxiety in eating disorders is transdiagnostic in nature, as demostrated by Godart et al. (2006) who found both AN and BN diagnostic subtypes did not differ on current or lifetime comorbidities of anxiety or depressive illnesses. Bulik (2002), proposed various models to explain the relation between both these known correlates and disorded eating after reviewing clinical, epidemiological and family studies. First, both depression and anxiety become apparent after the experience of disordered eating, with alleviation during recovery. The second model predicts that depression and anxiety precedes, or manifests prior to, the onset of eating disorders. The third posits that eating disorders are merely expressions of latent depressive or anxiety symptoms. The fourth suggested that all disorders share the same underlying causations, such as neurotic tendencies. Lastly, model five posits that all eating, affective and anxiety disorders share the same aetiological factors, although remain separate disorders. Tenative conclusions derived from this review of data claimed that model two and model five were most compelling and viable, thereby suggesting that depression and anxiety are potent risk factors for the development of problematic eating. However, all disorders share similar aetiology (Bulik, 2002).
In summary, substantial research suggests that a vicious cycle of psychological illness perpetuates the maintenance and longevity of problematic eating behaviour (Goel et al., 2021a, Goel et al., 2021b). Through self-esteem and body dissatisfaction, depression can foster disturbed eating pertaining to shape and weight concerns (Lim and You, 2017; Orth and Robins, 2013). The impact of depression and anxiety upon cognitive functioning in turn diminishes an individual's ability to regulate such restrictive or binge eating behaviours (Roberts et al., 2010). Psychiatric comorbidities may also predict the inception of disordered eating (Bulik, 2002), and should be emphasised in interventions before symptomatology eventuates to a clinically severe case.
Not only do existing mental illnesses influence eating behaviour, but social norms and relationships are also known to predict behaviours and perceptions (Bergstrom and Neighbors, 2006). These covariables remain briefly addressed in recent literature, while the following will attempt to explore the linkages with disordered eating behaviour.
2.2. Social norms
Norms are described as a set of standardised traditions, customs, rules and values resulting from affiliation with other individuals. Normative influences and sociocultural perspectives on the ‘ideal’ woman can cultivate body image disturbances (Bergstrom and Neighbors, 2006). Resultantly, aspirations to reach a partcicular standard or subscribe to ideal stereotypes are associated with disordered eating behaviour (Dondzilo et al., 2019). Specifically, in a study of 95 women, a drive for thinness was more prominent than avoidance of non-thin bodies. This indicates that internalising thin-ideal norms can pose a risk for eating disorder symptomatology (Dondzilo et al., 2019). The extent of this is often reliant on whether an individual is aware of norms or if they internalise them, and as such, internalisation of perceived norms is most directly associated with body image disturbances (Stice and Shaw, 2002). Notably, it is important that various socieities may have differing perceptions of body norms/standards. For instance, studies investigating eating attitudes and body norms found significant diffferences in body shape perceptions between individualistic and collectivist cultures (Goel et al., 2021; Lake et al., 2000).
More specifically, perceived social norms are typically categorised into two types: descriptive and injunctive. Descriptive norms regard the prevalence of behaviours (e.g., 55% of women are thin). Injunctive norms refers to the acceptability of behaviours (e.g., women should be thin). Injunctive norms have more of an approval component (Bergstrom and Neighbors, 2006; Cialdini et al., 1990; Forney and Ward, 2013). In order to obtain interpersonal approval and avoid negative social appraisals pertaining to one's body shape, individuals may engage in maladaptive eating (Bergstrom and Neighbors, 2006; Cox and Donelson, 2004; Goel et al., 2021). A study including 223 women found that injunctive norms strengthened the relationship between body dissatisfaction and problematic eating, whereas descriptive norms did not (Forney and Ward, 2013). Thus, norm-based clinical interventions, targeting individual internalised needs and intense desires to meet accepted societal and cultural customs, may alleviate the pressure women face in regards to achieving ‘ideal’ body size and subsequently eating, thereby assisting with healthy recovery.
Research investigating social norms relative to disordered eating has predominantly focused on non-clinical samples of female university/college students (Dondzilo et al., 2019; Forney and Ward, 2013; Giles et al., 2007). However, this should be broadened to encompass the wider female population. This would allow for examination of the association between norms and subclinical symptoms of disturbed eating before the illness progresses to clinical severity. While social norms have shown significant correlations with eating behaviours, especially by internalisation and injunctive standards to be met, another social factor, viz. family relationships and conflict, has also been documented in understanding eating disorders, as follows.
2.3. Family functioning
Family-based intervention presents one of the treatment strategies for disordered eating, acknowledging the family as an efficacious fundamental resource for rehabilitating the eating and nourishment of affected young people (Couturier et al., 2021; Lock and Le Grange, 2019). Previous research typically characterises the families of those with AN and BN as less communicative and less cohesive, with experiences of increased conflict (Laliberte et al., 1999; Latzer et al., 2002). Specifically, Arroyo and Sergin (2013) proposed that corrosive family interaction patterns were associated with reduced social competence and heightened psychological distress, in turn exacerbating disturbed eating behaviours. Negative correlations are also evident between family cohesion and controlled eating, indicating as family systems become less unified the more problematic eating behaviours arise (Hasenboehler et al., 2009).
Although family systems/dynamics are pivotal in the development of problematic eating (Laliberte et al., 1999), past research posited that the eating-disordered groups differ in their family interaction patterns. To illustrate, a study with 30 families of eating-disordered patients found that AN families had a lack of interpersonal boundaries, were stable, cohesive and nonconflictual during interactions. Inversely, BN families displayed more rigid interpersonal boundaries, less stability and little avoidance of conflict (Kog and Vandereycken, 1989). Consistent with this, Vidovic et al. (2005) confirmed significant differences between patients with restrictive anorexia and bulimia, suggesting individuals with restrictive eating behaviours had more conflict avoidance and better perceptions of family cohesiveness and communication. Conversely, Erol et al. (2007) posited that AN and BN groups do not statistically differ in terms of family functioning. Likewise, Laliberte et al. (1999) found that both disordered eating groups scored significantly higher on family climate variables, as described below, when compared to healthy controls. This indicated AN and BN groups differ from healthy controls, but not significantly from one another.
In terms of family climate variables (Laliberte et al., 1999), the family's body dissatisfaction, orientations towards social appearance, and emphasis on achievements was a more powerful predictor of disturbed eating than family process variables such as cohesion, conflict, and expressiveness, thereby suggesting that family climate, rather than family dysfunction may exacerbate eating concerns. However, one of very few earlier experimental studies on the topic investigated family systems in 113 adolescent females who were categorised into non-disturbed, mildly disturbed and highly disturbed eating behaviours and attitudes. They found eating disturbances were associated with perceptions of poor communication with parents, negligible trust in parents' accessibility and responsiveness as well as a conflictual, unsupportive and unstructured family environment (Maharaj et al., 1998).
Whilst more recent studies on family functioning address a range of variables such as overprotection, emotional responsiveness, and trans-generational interactions (Kroplewski et al., 2019), further contemporary empirical research is needed to corroborate whether AN and BN groups vary in their family interaction patterns, or if the characteristics of family systems between groups are more similar. Prospective research should also explicate what particular family variables are more impactful upon eating behaviours and attitudes, because more conclusive evidence regarding the role of family climate variables in the aetiology of eating disorders is needed (Laliberte et al., 1999). Nevertheless, the aforementioned evidence draws attention to the notion that family functioning may be a key contributor to the onset and persistence of disruptive eating behaviours. Importantly, a close, non-chaotic family climate has been found to be associated with recovery for young girls from eating disorders (Nilsson et al., 2012).
3. Research gaps and future directions
Upon exploring the wide array of literature on disordered eating, several research gaps and shortcomings were identified (refer to Table 1). The following will take a more overarching approach to focus on areas for prospective research and intervention insights by encapsulating the whole literature.
Table 1.
Highlights and controversies in the seven theories and major covariates upon explaining disordered eating.
| Theory | Highlights & Controversies |
|---|---|
| 1. Self-esteem | Intrapersonal motivation factor; A vicious cycle of low self-esteem, body dissatisfaction, and disordered eating; Bidirectional mediation impact on disordered eating |
| 2. Interpersonal | Social factor; Stress from relationships; Conflict and negative interpersonal evaluations; Mediates the impact of social anxieties upon disordered eating symptomatology |
| 3. Emotion regulation | Stress reactivity factor; Overall affect; Numb negative emotions through binge eating/compensatory behaviours; Enhance self-regulation through restrictive dieting |
| 4. Executive function (EF) | Cognitive and neurological factor; Impulsivity, decision-making, mental flexibility/shifting capacities, global processing, attention; Directional ambiguity between executive function deficits and problematic eating behaviour |
| 5. Social neuroscience | Biological component; Neural mechanisms and activation of certain brain regions during social processing; Impact upon body shape concerns and unstable eating behaviours |
| 6. Theory of mind (ToM) | Developmental factor on perspective taking; Capacity to decode the mental states, thoughts, beliefs and emotions of others; Mixed results pertaining to ToM deficits in those with disordered eating |
| 7. Transdiagnostic | Shared factors impacting both restrictive and binge eating; Psychological, neurological and cognitive transdiagnostic mechanisms involved in explaining the spectrum of various eating behaviours |
| Covariate | |
| 1. Depression | Comorbid mood issues; indirect effect with concurrent low self-esteem through body dissatisfaction; impaired EF such as set shifting; transdiagnostic between binge and restrictive eating disorders. |
| 2. Anxiety | Comorbid mental disturbance; diminished mental flexibility as in depression; inability to regulate eating; underlying neurotic tendency |
| 3. Social norms | Socio-cultural standards and normative pressure on body image; perceived descriptive and injunctive social norms impacting on eating behaviour; interpersonal and social appraisals; norm-based clinical interventions addressing internalised needs. |
| 4. Family functioning | Main clinical streams of family-based intervention and rehabilitation; family communication, cohesion, and conflict factors; family interaction patterns and psychological distress; mixed evidence on the difference between binge and restrictive eating disorders. |
First, causal directions have not been rigorously tested yet, as no firm evidence as to which core variable precedes between low self-esteem and body dissatisfaction is available (Brechan and Kvalem, 2015). Hence, more longitudinal designs or experimental priming/manipulations are warranted in explaining their causative roles in disordered eating. Similarly, in terms of depression, anxiety and disordered eating, the directionality of the association between depression and the core disturbance of self-esteem is unclear (Orth and Robins, 2013). Future research could resolve directional ambiguity in both clinical and non-clinical samples by testing whether diminished self-esteem is an outcome of depression and anxiety resulting in disturbed eating, or if depression and anxiety are resultant of poor self-esteem, over time or through laboratory-based priming.
In investigating causal direction, experimental designs (McAdams et al., 2016; McAdams and Krawczyk, 2013) with priming state self-esteem and triggering body dissatisfaction in laboratory settings (Svaldi et al., 2012) are needed to provide theoretical and practical insight to better understand how disordered eating develops and continues. Subsequently, efficiency of prevention and provision of treatment initiatives in communities and clinics can be enhanced. Further longitudinal designs will also be powerful in demonstrating the causation among variables. Tracking and examining changes in theory variables such as self-esteem, executive function, and ToM with eating behaviour over time will shed light on the precedence of causal variables to outcome variables (Herle et al., 2020; Yilmaz et al., 2019). These lines of research will inform researchers and practitioners on how to understand and efficiently treat disordered eating. Future research using clinical experiments can also be facilitated to cross-validate causal paths of mediator mechanisms, for instance, by addressing emotional reactivity in self-esteem interventions on maladaptive eating. Another example by Rieger et al. (2010), suggests prospective research should attempt to elucidate interpersonal mechanisms such as social evaluation, and the path by which it is correlated with disordered eating symptoms.
Second, it is unclear if interpersonal difficulties and emotion regulation challenges that appear to fuel binge eating and excessive fasting are also general sources of disordered eating in non-clinical populations, due to majority of studies focusing on clinical patients (Dallman, 2010; Hatch et al., 2010; Tuschen-Caffier & Vö;gele, 1999). Research could sample from the general community to look at interpersonal and emotional factors which have previously been investigated in clinical samples, thus providing a level of predictive value, particularly for adolescents and adult onset groups (Stice et al., 2017).
Third, mixed findings and controversial arguments that require further evidence are observed in cognitive functioning. Hirst et al. (2017) found EF impairments in both AN and BN patients, whereas Billingsley-Marshall et al. (2013) found EF deficits were only apparent in a small number of affected women. The specific EF variables need to be further addressed, for instance, inhibition, cognitive flexibility, and decision making. Additionally, the direction of the association between EF and eating behaviour is undetermined (Dohle et al., 2018). As mentioned, longitudinal research is needed to test mediating/moderating effects of all relevant EF facets upon eating behaviour, thus resolving directional ambiguity and assisting with provision of tailored treatment. Moreover, Roberts et al. (2010) found depression and anxiety hindered mental set-shifting abilities ensuing the dysregulation of eating behaviour. Therefore, more research is warranted to corroborate such findings, because only minimal research has examined the effects of depression and anxiety relative to cognitive functioning (Billingsley-Marshall et al., 2013).
Fourth, mixed results are also observed in ToM research. To illustrate, results from both Bora and Kose (2016) and Pereira de Sampaio et al. (2013) demonstrated that women with AN suffer significant ToM deficits while those with BN display only a minimal deficit that is comparable with healthy controls. Conversely, Medina-Pradas et al. (2012) posited that BN patients showed difficulty interpreting complex emotions of others, while AN patients displayed no perspective-taking impediments. Considering this inconsistent evidence, exploration into social cognitive performances in persons with subclinical eating symptomatology would provide insight into how ToM impairments in the specific facets, develop and sustain in various atypical eating groups.
The fifth gap addresses social dimensions, particularly social norms. While the majority of studies focus on female university students (Dondzilo et al., 2019; Forney and Ward, 2013; Giles et al., 2007), propsective literature could sample from the wider female population to gain more accurate representations of the impact of social norms upon the spectrum of eating behaviours. Concurrently, adolescents and younger people (Stice et al., 2017) should also be studied with more preventative focus. Additionally, the efficacy of norm-based interventions in assisting recovery should be evaluated, to determine if alleviating societal pressure concerning body shape standards subsequently reduces disordered eating (Stok et al., 2016).
Sixth, family functioning and dynamics are less comprehensively researched in recent literature. It remains undetermined whether individuals with AN and BN, respectively, significantly differ in their family patterns (Kog and Vandereycken, 1989; Vidovic et al., 2005), or if they share similar characteristics (Erol et al., 2007). It is also unknown whether family climate (e.g., orientation towards social appearance) or family process variables (e.g., cohesion) are more powerful predictors of disturbed eating behaviour in females (Laliberte et al., 1999; Maharaj et al., 1998). New innovative research may elect to address such inconsistencies to better inform the prevailing family-based interventions.
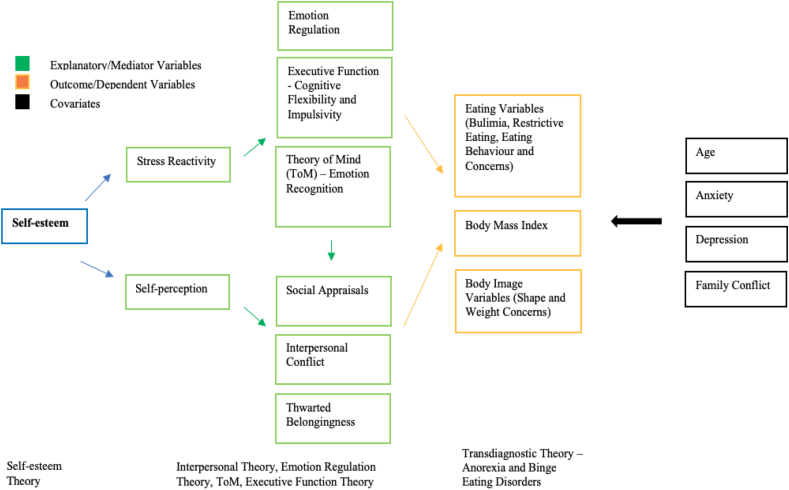
To progress with more integrative discussion, the shortcomings of the entirety of this research present a profound gap in the wider theoretical literature with novel research opportunities. The plethora of theories discussed have never been integrated into a single study design, or within a cohesive review such as this. More power and further explanation of variance in disordered eating can be explained by incorporating the influential theories into a single research design. Addressing this research gap with powerful integration of the theoretical approaches, a cohesive empirical model, incorporating all available conceptual evidence (Menatti et al., 2015), is warranted. Structural Equation Modelling (SEM) could be utilised, engaging a large international sample, to competitively test all major theory variables (Brown et al., 2019; Tylka and Subich, 2004). As illustrated in Figure 1, SEM will allow exploration into potential underlying psychological mechanisms with multiple mediation modelling, for instance, executive function as a mediator in the impact of self-esteem and body shape concerns on disordered eating. Such integrative multi-theory research would inform researchers/practitioners with novel, advanced and comprehensive evidence on potential mechanisms of the explanatory variables derived from the theoretical perspectives, and their impact on eating attitudes and behaviours.
Figure 1.
Example of Hypothetical Mediation Models using Structural Equation Modelling (SEM) to Test all Major Theory Variables. Note.Zanella and Lee (2022)
More specifically, while numerous psychological and neurological theories have sought to explain factors correlated with disordered eating, only few studies have addressed any underlying mediation mechanisms. A mediation mechanism is commonly described as an intermediate variable within the causal sequence that can realize the impact of an explanatory/independent variable upon an outcome/dependent variable. The independent variable typically causes the mediating variable, which then in turn influences the outcome (MacKinnon, 2012). To illustrate, mediator roles of self-esteem or rumination were evident in explaining social anxiety upon eating disorder symptomatology (Dondzilo et al., 2017), and, as aforementioned, body dissatisfaction often mediates the impact of self-esteem upon maladaptive eating (Lim and You, 2017). However, little is known regarding what potential pathways and mediation roles exist among the multiple explanatory variables from the various theories, beyond their simplistic correlations with problematic eating. Accordingly, critical questions may arise if these theories are only parallel, or if there are more complex relationships such as diverse mediation paths that explain disordered eating more comprehensively.
Further strategies are required to fill other methodological research gaps. A methodological challenge for disordered eating research is obtaining access to clinical populations. Investigating functional impacts of subclinical eating symptomatology in non-clinical female community populations is a widely used sampling method in the field (Dondzilo et al., 2017). This research strategy accommodates limited access to clinical populations and addresses the transdiagnostic nature of important variables applied to multiple disordered eating groups along the spectrum (Fairburn et al., 2003). Even the wider general public and individuals widely locating on the disordered eating continuum might serve as research target populations, based on their unregulated eating behaviours, such as excessive dieting desires, overeating, or unhealthy habits in terms of ToM and other theory factors. This research agenda also applies to addressing transdiagnostic issues across various eating disorders. Investigating disordered eating with community samples has been warranted, especially based on the well-documented transdiagnostic theory, as a large portion of the general public presents eating problems, including obesity and dieting behaviour (Da Luz et al., 2017). Furthermore, preventative research/health policies and intervention strategies can benefit from sampling populations from the general public. However, Dondzilo et al. (2017) highlights the importance of expanding methodologies to clinically-diagnosed women with eating disorders, as it should not be assumed that community level findings extend to clinical samples. Likewise, clinical samples may identify significant associations between particular variables and eating that may not exist in general community samples (Bulik, 2002). Knowledge of specific variables may in turn assist with the provision of treatment interventions and inform focal points for recovery.
4. Conclusions
The powerful impacts of psychological, interpersonal, emotional, cognitive and neurological factors upon disordered eating behaviour in women are evident. As such, this review has categorised the diverse literature into major theoretical viewpoints, in which several important conclusions emerge. While depression, anxiety, ‘thinness-ideal’ societal norms and family functioning are prevalent correlates of disordered eating, self-esteem is the core disturbance involved in problematic eating, and is unduly influenced by body dissatisfaction. Further, individuals may respond to negative interpersonal appraisals and cope with subsequent emotion dysregulation through maladaptive eating. The continuum of eating-disordered types, ranging from AN to BN, also share similar trans-diagnostic deficits, particularly in cognitive functioning, perspective-taking (ToM) and the neural processing of social evaluations. Although cogent evidence is elucidated in support for these theories, some inconsistent findings remind the need for further research. Empirical research incorporating the key theories on disordered eating can help contribute to existing knowledge, and bridge theoretical perspectives which have previously been considered in isolation. Experimental designs and longitudinal research are warranted to investigate causative relationships among the major theory variables and eating behaviour. More importantly, this area of research can only continue to benefit the holistic well-being of women and facilitate healthy eating behaviour in today's society.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
No data was used for the research described in the article.
Declaration of interest's statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- American Psychiatric Association . fifth ed. American Psychiatric Publishing; Arlington, VA: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Ansell E.B., Grilo C.M., White M. Examining the interpersonal model of binge eating and loss of control over eating in women. Int. J. Eat. Disord. 2012;45(1):43–50. doi: 10.1002/eat.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arroyo A., Sergin C. Family interaction and disordered eating attitudes: the mediating role of social competence and psychological distress. Commun. Monogr. 2013;80(4):399–424. [Google Scholar]
- Bergstrom R.L., Neighbors C. Body image disturbance and the social norms approach: an integrative review of the literature. J. Soc. Clin. Psychol. 2006;25(6):975–1000. [Google Scholar]
- Billingsley-Marshall R., Basso M.R., Lund B.C., Hernandez E.R., Johnson C.L., Drevets W.C., McKee P.A., Yates W.R. Executive function in eating disorders: the role of state anxiety. Int. J. Eat. Disord. 2013;46(4):316–321. doi: 10.1002/eat.22086. [DOI] [PubMed] [Google Scholar]
- Blinder B.J., Cumella E.J., Sanathara V.A. Psychiatric commorbidities of female inpatients with eating disorders. Psychosom. Med. 2006;68:454–462. doi: 10.1097/01.psy.0000221254.77675.f5. [DOI] [PubMed] [Google Scholar]
- Bora E., Kose S. Meta-analysis of theory of mind in Anorexia Nervosa and Bulimia Nervosa: a specific impairment of cognitive perspective taking in Anorexia Nervosa? Int. J. Eat. Disord. 2016;49(8):739–740. doi: 10.1002/eat.22572. [DOI] [PubMed] [Google Scholar]
- Brechan I., Kvalem I.L. Relationship between body dissatisfaction and disordered eating: mediating role of self-esteem and depression. Eat. Behav. 2015;17:49–58. doi: 10.1016/j.eatbeh.2014.12.008. [DOI] [PubMed] [Google Scholar]
- Brown M., Hochman A., Micali N. Emotional instability as a trait risk factor for eating disorder behaviors in Adolescents: sex differences in a large-scale prospective study. Psychol. Med. 2019;1–12 doi: 10.1017/S0033291719001818. [DOI] [PubMed] [Google Scholar]
- Bulik C.M. In: Eating Disorders and Obesity: A Comprehensive Handbook. Fairburn C.G., Brownwell K.D., editors. Guilford Press; 2002. Anxiety, depression and eating disorders; pp. 193–198. [Google Scholar]
- Burgess P.W., Shallice T. Thames Valley Test Company Ltd; United Kingdom: 1997. The Hayling and Brixton Tests. [Google Scholar]
- Christensen K.A., Forbush K.T., Richson B.N., Thomeczek M.L., Perko V.L., Bjorlie K., Christian K., Ayres J., Wildes J.E., Mildrum Chana S. Food insecurity associated with elevated eating disorder symptoms, impairment, and eating disorder diagnoses in an American University student sample before and during the beginning of the COVID -19 pandemic. Int. J. Eat. Disord. 2021;54(7):1213–1223. doi: 10.1002/eat.23517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen K.A., Haynos A.F. A theoretical review of interpersonal emotion regulation in eating disorders: enhancing knowledge by bridging interpersonal and affective dysfunction. Journal of Eating Disorders. 2020;8:1–10. doi: 10.1186/s40337-020-00298-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cialdini R.B., Reno R.R., Kallgren C.A. A focus theory on normative conduct: recycling the concept of norms to reduce littering in public places. J. Pers. Soc. Psychol. 1990;58(1000):1015–1026. [Google Scholar]
- Ciarma J.L., Mathew J.M. Social anxiety and disordered eating: the influence of stress reactivity and self-esteem. Eat. Behav. 2017;26:177–181. doi: 10.1016/j.eatbeh.2017.03.011. [DOI] [PubMed] [Google Scholar]
- Claudat K., White E.K., Warren C.S. Acculturative stress, self-esteem, and eating pathology in Latina and Asian American female college ctudents. J. Clin. Psychol. 2016;72(1):88–100. doi: 10.1002/jclp.22234. [DOI] [PubMed] [Google Scholar]
- Couturier J., Kimber M., Barwick M., Woodford T., Mcvey G., Findlay S., Webb C., Niccols A., Lock J. Family-based treatment for children and adolescents with eating disorders: a mixed-methods evaluation of a blended evidence-based implementation approach. Translational Behavioral Medicine. 2021;11(1):64–73. doi: 10.1093/tbm/ibz160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox K.S., Donelson R. Proquest Dissertations Publishing; 2004. Social Norm Emergence and the Thin Body Norm. [Google Scholar]
- Dallman M. Stress-induced obesity and the emotional nervous system. Trends Endocrinol. Metabol. 2010;21(3):159–165. doi: 10.1016/j.tem.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Luz F.Q., Sainsbury A., Mannan H., Touyz S., Mitchison D., Hay P. Prevalence of obesity and comorbid eating disorder behaviors in South Australia from 1995 to 2015. International Journal of Obesity; London. 2017;41(7):1148–1153. doi: 10.1038/ijo.2017.79. [DOI] [PubMed] [Google Scholar]
- Delinsky S.S., Wilson G.T. Weight gain, dietary restraint, and disordered eating in the freshman year of college. Eat. Behav. 2008;9(1):82–90. doi: 10.1016/j.eatbeh.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Dohle S., Diel K., Hofmann W. Executive functions and the self-regulation of eating behaviour: a review. Appetite. 2018;124:4–9. doi: 10.1016/j.appet.2017.05.041. [DOI] [PubMed] [Google Scholar]
- Dondzilo L., Rieger E., Jayawardena N., Bell J. Drive for thinness versus fear of fat: approach and avoidance motivation regarding thin and non-thin images in women. Cognitve Therapy and Research. 2019;43(3):585–593. [Google Scholar]
- Dondzilo L., Rieger E., Palermo R., Byrne S., Bell J. The mediating role of rumination in the relation between attentional bias towards thin female bodies and eating disorder symptomatology. PLoS One. 2017;12(5) doi: 10.1371/journal.pone.0177870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichen D.M., Matheson B.E., Appleton-Knapp S.L., Boutelle K.N. Neurocognitive treatments for eating disorders and obesity. Curr. Psychiatr. Rep. 2017;19(9):62. doi: 10.1007/s11920-017-0813-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erol A., Fadime Y., Gulser T. Family functioning of patient with an eating disorder compared with that of patients woth obsessive complusive disorder. Compr. Psychiatr. 2007;48(1):47–50. doi: 10.1016/j.comppsych.2006.05.004. [DOI] [PubMed] [Google Scholar]
- Espinoza P., Penelo E., Mora M., Francisco R., González M.L., Raich R.M. Bidirectional relations between disordered eating, internalization of beauty ideals, and self-esteem: a longitudinal study with adolescents. J. Early Adolesc. 2019;39(9):1244–1260. [Google Scholar]
- Fagundo A.B., da la Torre R., Jimenez-Murcia S., Aguera Z., Granero R., Tarrega S., Botella C., Banos R., Fernandez-Real J.M., Rodriguez R., Forcano L., Fruhbeck G., Gomez-Ambrosi J., Tinahones F.J., Fernandez-Garcia J.C., Casanueva F.F., Fernandez-Aranda F. Executive functions profile in extreme eating/weight conditions: from anorexia nervosa to obesity. PLoS One. 2012;7(8) doi: 10.1371/journal.pone.0043382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn C.G., Cooper Z., Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav. Res. Ther. 2003;41(5):509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Favieri F., Forte G., Casagrande M. The executive functions in overweight and obesity: a systematic review of neuropsychological cross-sectional and longitudinal studies. Front. Psychol. 2019;10 doi: 10.3389/fpsyg.2019.02126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forney K.J., Ward R.M. Examining the moderating role of social norms between body dissatisfaction and disordered eating in college students. Eat. Behav. 2013;14(1):73–78. doi: 10.1016/j.eatbeh.2012.10.017. [DOI] [PubMed] [Google Scholar]
- Franko D.L., Striegel-Moore R.H. Psychosocial risk for eating disorders: whats new? Annual Review of Eating Disorders. 2007;1:51–62. [Google Scholar]
- Giles S.M., Helme D., Krcmar M. Predicted disordered eating intentions among incoming college freshman: an analysis of social norms and body esteem. Commun. Stud. 2007;58(4):395–410. [Google Scholar]
- Godart N., Berthoz S., Rein Z., Perdereau F., Lang F., Venisse J., Halfon O., Bizouard P., Loas G., Corcos M., Jeammet P., Flament M., Curt F. Does the frequency of anxiety and depressive disorders differ between diagnostic subtypes of anorexia nervose and bulimia nervosa? Int. J. Eat. Disord. 2006;39(8) doi: 10.1002/eat.20274. [DOI] [PubMed] [Google Scholar]
- Goel N.J., Sadeh-Sharvit S., Trockel M., Flatt R.E., Fitzsimmons-Craft E.E., Balantekin K.N., Monterubio G.E., Firebaugh M.-L., Wilfley D.E., Taylor C.B. Depression and anxiety mediate the relationship between insomnia and eating disorders in college women. J. Am. Coll. Health. 2021;69(8):976–981. doi: 10.1080/07448481.2019.1710152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel N.J., Thomas B., Boutté R.L., Kaur B., Mazzeo S.E. Body image and eating disorders among South asian American women: what are we missing? Qual. Health Res. 2021;31(13):2512–2527. doi: 10.1177/10497323211036896. [DOI] [PubMed] [Google Scholar]
- Guerrieri R., Nederkoorn C., Shroote M., Martjin C., Jansen A. Inducing impulsivity leads high and low restrained eaters into overeating, whereas current dieters stick to their diet. Appetite. 2009;53(1):93–100. doi: 10.1016/j.appet.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Hasenboehler K., Munsch S., Meyer A.H., Kappler C., Vogele C. Family structure, body mass index, and eating behaviour. Int. J. Eat. Disord. 2009;42(4):332–338. doi: 10.1002/eat.20612. [DOI] [PubMed] [Google Scholar]
- Hatch A., Madden S., Kohn M., Clarke S., Touyz S., Williams L.M. Anorexia nervosa: towards an integrative neuroscience model. Eur. Eat Disord. Rev. 2010;18(3):165–179. doi: 10.1002/erv.974. [DOI] [PubMed] [Google Scholar]
- Heaton R.K., Chelune G.J., Talley J.L., Kay G., Curtiss G. Psychological Assessment Resources; Odessa, Florida: 1993. Wisconsin Card Sorting Test. [Google Scholar]
- Herle M., De Stavola B., Hubel C., Abdulkadir M., Santos Ferreira D., Loos R.J.F., Bryant-Waugh R., Bulik C.M., Micali N. A longitudinal study of eating behaviours in childhood and later eating disorder behaviours and diagnoses. Br. J. Psychiatr. 2020;216(2):113–119. doi: 10.1192/bjp.2019.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinrichsen H., Wright F., Waller G., Meyer C. Social anxiety and coping strategies in the eating disorders. Eat. Behav. 2003;4(2):117–126. doi: 10.1016/S1471-0153(03)00016-3. [DOI] [PubMed] [Google Scholar]
- Hirst R.B., Beard C.L., Colby K.A., Quittner Z., Mills B.M., Lavender J.M. Anorexia nervosa and bulimia nervosa: a meta-analysis of executive functioning. Neurosci. Biobehav. Rev. 2017;83:678–690. doi: 10.1016/j.neubiorev.2017.08.011. [DOI] [PubMed] [Google Scholar]
- Hudson J.I., Hiripi E., Pope H.G., Kessler R.C. The prevalence and correlates of eating disorders in the national comordity survey replication. Biol. Psychiatr. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karazsia B.T., Murnen S.K., Tylka T.L. Is body dissatisfaction changing across time? A cross-temporal meta-analysis. Psychol. Bull. 2016;143(3):293–320. doi: 10.1037/bul0000081. [DOI] [PubMed] [Google Scholar]
- Kog E., Vandereycken W. Family interaction in eating disorder patients and controls. Int. J. Eat. Disord. 1989;8(1):11–23. [Google Scholar]
- Kroplewski Z., Szcześniak M., Furmańska J., Gójska A. Assessment of family functioning and eating disorders – the mediating role of self-esteem. Front. Psychol. 2019;10 doi: 10.3389/fpsyg.2019.00921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laghi F., Pompili S., Bianchi D., Lonigro A., Baiocco R. Drunkorexia: an examination of the role of theory of mind and emotional awareness among adolescents. Dev. Neuropsychol. 2021;46(1):70–81. doi: 10.1080/87565641.2020.1869743. [DOI] [PubMed] [Google Scholar]
- Lake A.J., Staiger P.K., Glowinski H. Effect of western culture on women’s attitude to eating and perceptions of body shape. Int. J. Eat. Disord. 2000;27(1):83–89. doi: 10.1002/(sici)1098-108x(200001)27:1<83::aid-eat9>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Laliberte M., Boland F.J., Leichner P. Family climates: family factors specific to disturbed eating and bulimia nervosa. J. Clin. Psychol. 1999;55(9):1012–1040. doi: 10.1002/(sici)1097-4679(199909)55:9<1021::aid-jclp1>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Lampard M.A., Tasca G., Balfour L., Bissada H. An evaluation of the transdiagnostic cognitive-behavioural model of eating disorders. Eur. Eat Disord. Rev. 2013;21(2):99–107. doi: 10.1002/erv.2214. [DOI] [PubMed] [Google Scholar]
- Latzer Y., Hochdorf Z., Bachar E., Canetti L. Attachment style and family functioning as discriminating factors in eating disorders. Comtemporary Family Therapy. 2002;24:581–599. [Google Scholar]
- Lim S.A., You S. Effects of self-esteem and depression on abnormal eating behavior among Korean female college students: mediating role of body dissatisfaction. J. Child Fam. Stud. 2017;26(1):176–182. [Google Scholar]
- Limbers C., Young D. Executive functions and consumption of fruits/vegetables and high saturated fat foods in young adults. J. Health Psychol. 2015;20(5):602–611. doi: 10.1177/1359105315573470. [DOI] [PubMed] [Google Scholar]
- Lock J., Le Grange D. Family-based treatment: where are we and where should we be going to improve recovery in child and adolescent eating disorders. Int. J. Eat. Disord. 2019;52(4):481–487. doi: 10.1002/eat.22980. [DOI] [PubMed] [Google Scholar]
- Luo Y., Mendoza C., Pelfrey S., Lohrenz T., Gu X., Montague P.R., McAdams C.J. 2021. Elevated Neurobehavioral Responses to Negative Social Interactions in Women with Bulimia Nervosa. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon D. United States of America: Taylor and Francis; NY: 2012. An Introduction to Statistical Mediation Analysis. [Google Scholar]
- Maharaj S.I., Rodin G.M., Olmsted M.P., Daneman D. Eating disturbances, diabetes and the family: an empirical study. J. Psychosom. Res. 1998;44(3-4):479–490. doi: 10.1016/s0022-3999(97)00273-0. [DOI] [PubMed] [Google Scholar]
- McAdams C.J., Jeon-Slaughter H., Evans S., Lohrenz T., Montague P.R., Krawczyk D.C. Neural differences in self-perception during illness and after weight-recovery in anorexia nervosa. Soc. Cognit. Affect Neurosci. 2016;11(11):1823–1831. doi: 10.1093/scan/nsw092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAdams C.J., Krawczyk D.C. Neural responses during social and self-knowledge tals in bulimia nervosa. Front. Psychiatr. 2013;4 doi: 10.3389/fpsyt.2013.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina-Pradas C., Navarro Pastor J.B., Alvarez-Moya E.M., Grau A. Emotional theory of mind in eating disorders. Int. J. Clin. Health Psychol. 2012;12(2):189–202. [Google Scholar]
- Menatti A.R., DeBoer L.B.H., Weeks J.W., Heimberg R.G. Social anxiety and associations with eating psychopathology: mediating effects of fears of evaluation. Body Image. 2015;14:20–28. doi: 10.1016/j.bodyim.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Murray S.B. Gender identity and eating disorders: the need to delineate novel pathways for eating disorder symptomatology. J. Adolesc. Health. 2017;60(1):1–2. doi: 10.1016/j.jadohealth.2016.10.004. [DOI] [PubMed] [Google Scholar]
- Nederkoorn C., Houben K., Hofmann W., Roefs A., Jansen A. Control yourself or just eat what you like? Weight gain over a year is predicted by an interactive effect of response inhibition and implicit preference for snack foods. Health Psychol. 2010;29(4):389–393. doi: 10.1037/a0019921. [DOI] [PubMed] [Google Scholar]
- Nilsson K., Engstrom I., Hagglof B. Family climate and recovery in adolescent onset eating disorders: a propspective study. Eur. Eat Disord. Rev. 2012;20(1):96–102. doi: 10.1002/erv.1127. [DOI] [PubMed] [Google Scholar]
- O’Hara L., Tahboub-Schulte S., Thomas J. Weight-related teasing and internalized weight stigma predict abnormal eating attitudes and behaviours in Emirati female university students. Weight Stigma and Eating Behaviours. 2016;102:44–50. doi: 10.1016/j.appet.2016.01.019. [DOI] [PubMed] [Google Scholar]
- Orth U., Robins R.W. Understanding the link between low self- esteem and depression. Curr. Dir. Psychol. Sci. 2013;22:455–460. [Google Scholar]
- Ozmen D., Ozmen E., Ergin D., Cetinkaya A.C., Sen N., Dundar P.E., Taskin E.O. The association of self-esteem, depression and body satisfaction with obesity among Turkish adolescents. BMC Publ. Health. 2007;7(1):1–7. doi: 10.1186/1471-2458-7-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira de Sampaio F.T., Soneira S., Aulicino A., Allegri R.F. Theory of Mind in eating disorders and their relationships to clinical profiles. Eur. Eat Disord. Rev. 2013;21(6) doi: 10.1002/erv.2247. [DOI] [PubMed] [Google Scholar]
- Perpina C., Sanchez-Reales S. Cognitive flexibility and decision-making in eating disorders and obesity. Eating and Weight Disorders – Studies on Anorexia, Bulimia and Obesity. 2017;22(3):435–444. doi: 10.1007/s40519-016-0331-3. [DOI] [PubMed] [Google Scholar]
- Rania M., Aloi M., de Filippis R., Carbone E.A., Caroleo M., De Fazio P., Segura-Garcia C. Executive functions and depressive symptoms interplay in binge eating disorder: a structural equation model analysis. Eur. Eat Disord. Rev. 2021;29(5):811–819. doi: 10.1002/erv.2854. [DOI] [PubMed] [Google Scholar]
- Reitan R.M. The relation of the trail making test to organic brain damage. J. Consult. Psychol. 1955;19:393–394. doi: 10.1037/h0044509. [DOI] [PubMed] [Google Scholar]
- Rieger E., Van Buren D.J., Bishop M., Tanofsky-Kraff M., Welch R., Wifley D.E. An eating disorder-specific model of interpersonal psychotherapy (IPT-ED): causal pathways and treatment implications. Clin. Psychol. Rev. 2010;30(4):400–410. doi: 10.1016/j.cpr.2010.02.001. [DOI] [PubMed] [Google Scholar]
- Roberts M.E., Tchanturia K., Treasure J.L. Exploring the neurocognitve signature of poor set-shifting in anorexia and bulimia nervosa. J. Psychiatr. Res. 2010;44(14):964–970. doi: 10.1016/j.jpsychires.2010.03.001. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Princeton Univeristy Press; Princeton, NJ: 1965. Society and the Adolescent Self-Image. [Google Scholar]
- Scholtz W., Yim I.S., Zoccola P.M., Jansen L., Schulz P. The perceived stress reactivity scale: measurement invariance, stability, and validity in three countries. Psychol. Assess. 2011;23:80–94. doi: 10.1037/a0021148. [DOI] [PubMed] [Google Scholar]
- Sedikides C., Gress A.P. In: Sage Handbook of Social Psychology. Hogg M.A., Cooper J., editors. Sage; London: 2003. Portraits of the self; pp. 110–138. [Google Scholar]
- Shea M.E., Pritchard M.E. Is self-esteem the primary predictor of disordered eating? Pers. Indiv. Differ. 2007;42(8):1527–1537. [Google Scholar]
- Silverstone P.H., Salsali M. Low self-esteem and psychiatric patients: Part I-The relationship between low self-esteem and psychiatric diagnosis. Ann. Gen. Hosp. Psychiatr. 2003;2(1):2. doi: 10.1186/1475-2832-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart C., Konstantellou A., Kassamali F., McLaughlin N., Cutinha D., Bryant-Waugh R., Simic M., Eisler I., Baudinet J. Is this the ‘new normal’? A mixed method investigation of young person, parent and clinician experience of online eating disorder treatment during the COVID-19 pandemic. Journal of Eating Disorders. 2021;9(1):1–11. doi: 10.1186/s40337-021-00429-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E., Gau J.M., Rohde P., Shaw H.E. Risk factors that predict future onset of each DSM–5 eating disorder: predictive specificity in high-risk adolescent females. J. Abnorm. Psychol. 2017;126(1):38–51. doi: 10.1037/abn0000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E., Shaw H.E. Role of body dissatisfaction in the onset and maintenance of eating pathology: a synthesis of research findings. J. Psychosom. Res. 2002;53:985–993. doi: 10.1016/s0022-3999(02)00488-9. [DOI] [PubMed] [Google Scholar]
- Stok M.F., de Vet E., de Ridder D.T.D., de Wit J.B.F. The potential of peer social norms to shape food intake in adolescents and young adults: a systematic review of effects and moderators. Health Psychol. Rev. 2016;10(3):326–340. doi: 10.1080/17437199.2016.1155161. [DOI] [PubMed] [Google Scholar]
- Stone V.E., Baron-Cohen S., Knight R.T. Frontal lobe contributions to theory of mind. J. Cognit. Neurosci. 1998;10(5):640–656. doi: 10.1162/089892998562942. [DOI] [PubMed] [Google Scholar]
- Svaldi J., Zimmermann S., Naumann E. The impact of an implicity manipulation of self-esteem on body dissatisfaction. J. Behav. Ther. Exp. Psychiatr. 2012;43(1):581–586. doi: 10.1016/j.jbtep.2011.08.003. [DOI] [PubMed] [Google Scholar]
- Tchanturia K., Anderluh M.B., Morris R.G., Rabe-Hesketh S., Collier D.A., Sanchez P., Treasure J.L. Cogntive flexibility in anorexia nervosa and bulimia nervosa. Journal of the International Neuropsychology Society. 2004;10(4):513–520. doi: 10.1017/S1355617704104086. [DOI] [PubMed] [Google Scholar]
- Teixeira M.D., Pereira A.T., Marques M.V., Saraiva J.M., de Macedo A.F. Eating behaviors, body image, perfectionism, and self-esteem in a sample of Portuguese girls. Rev. Bras. Psiquiatr. 2016;38(2):135–140. doi: 10.1590/1516-4446-2015-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touyz S., Lacey H., Hay P. BioMed Central; 2020. Eating Disorders in the Time of COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuschen-Caffier B., Vögele C. Psychological and physiological reactivity to stress: an experimental study on bulimic patients, restrained eaters and controls. Psychother. Psychosom. 1999;68(6):333–340. doi: 10.1159/000012352. [DOI] [PubMed] [Google Scholar]
- Tylka T.L., Subich L.M. Examining a multidimensional model of eating disorder symptomatology among college women. J. Counsel. Psychol. 2004;51(3):314–328. [Google Scholar]
- Udo T., Grilo C.M. Prevalence and correlates of DSM-5–defined Eating Disorders in a nationally representative sample of U.S. adults. Biol. Psychiatr. 2018;84(5):345–354. doi: 10.1016/j.biopsych.2018.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Eeden A.E., van Hoeken D., Hoek H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatr. 2021;34(6):515–524. doi: 10.1097/YCO.0000000000000739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vervaet M., Puttevils L., Hoekstra R.H., Fried E., Vanderhasselt M.-A. European Eating Disorders Review; 2020. Transdiagnostic Vulnerability Factors in Eating Disorders: A Network Analysis. [DOI] [PubMed] [Google Scholar]
- Vidovic V., Vesna V., Begovac I., Mahnik M., Tocilj G. Perceived family cohesion, adaptability and communication in eating disorders. Eur. Eat Disord. Rev. 2005;13(1):19–28. [Google Scholar]
- Villarejo C., Jiménez-Murcia S., Alvarez-Moya E., Granero R., Penelo E., Treasure J., Vilarrasa N., Gil-Montserrat de Bernabé M., Casanueva F.F., Tinahones F.J., Fernández-Real J.M., Fruĥ-beck G., De la Torre R., Botella C., Aguëra Z., Menchoń J.M., Fernańdez-Aranda F. Loss of control over eating: a description of the eating disorder/obesity spectrum in women. Eur. Eat Disord. Rev. 2014;22(1):25–31. doi: 10.1002/erv.2267. [DOI] [PubMed] [Google Scholar]
- Ward Z.J., Rodriguez P., Wright D.R., Austin S.B., Long M.W. Estimation of eating disorders prevalence by age and associations with mortality in a simulated nationally representative US cohort. JAMA Netw. Open. 2019;2(10) doi: 10.1001/jamanetworkopen.2019.12925. e1912925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman R.S., Bauer S., Thomas J.J. Wiley Online Library; 2020. Access to Evidence-Based Care for Eating Disorders during the COVID-19 Crisis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Harper J.A., Van Enkevort E.A., Latimer K., Kelley U., McAdams C.J. Neural activations are related to body-shape, anxiety, and outcomes in adolescent anorexia nervosa. J. Psychiatr. Res. 2017;87:1–7. doi: 10.1016/j.jpsychires.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yilmaz Z., Gottfredson N.C., Zerwas S.C., Bulik C.M., Micali N. Developmental premorbid body mass index trajectories of adolescents with eating disorders in a longitudinal population cohort. J. Am. Acad. Child Adolesc. Psychiatry. 2019;58(2):191–199. doi: 10.1016/j.jaac.2018.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamani Sani S.H., Fathirezaie Z., Gerber M., Pühse U., Bahmani D.S., Bashiri M., Pourali M., Brand S. Psychological Reports; 2020. Self-Esteem and Symptoms of Eating-Disordered Behavior Among Female Adolescents. 0033294120948226. [DOI] [PubMed] [Google Scholar]
- Zanella, Lee . Psychology, RMIT University; 2022. Mediations of Executive Function, Social Cognitions, and Interpersonal Conflict in Explaining the Impact of Self-esteem on Disordered Eating: Structural Equation Modelling.https://www.rmit.edu.au/ Manuscript under review. [Google Scholar]
- Zegarra-Valdivia J.A., Chino-Vilca B.N. Social cognition and executive function impairment in young women with Anorexia Nervosa. Clin. Salud. 2018;29(3):107–113. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.