Abstract
Background
Burnout syndrome is a chronic response to stressors in the workplace. It is characterized by emotional exhaustion and physical and mental burnout and may lead to high employee turnover, work absenteeism, and increased occupational accidents. Most studies use the Maslach Burnout Inventory (MBI) to identify burnout and implement preventive actions and treatments.
Objective
This study presents a scoping review protocol to identify and map studies that used MBI to assess burnout syndrome in health care professionals working in public health services.
Methods
This scoping review protocol follows the Joanna Briggs Institute reviewers’ manual, and this protocol consists of 6 stages: identifying the research question, identifying relevant studies, study selection, data extraction and coding, analysis and interpretation of results, and consultation with stakeholders. We will conduct searches in Embase, LILACS, PubMed/MEDLINE, PsycINFO, Scopus, Web of Science databases, and gray literature. The main research question is as follows: how is MBI used to identify burnout syndrome in health care professionals working in public health services? Inclusion criteria will comprise qualitative and quantitative studies using MBI to identify burnout syndrome in health care professionals working in public health services and no restrictions in language and publication dates. Data will be extracted using a spreadsheet adapted from the Joanna Briggs Institute model. Quantitative and qualitative data will be analyzed using descriptive statistics and thematic analysis, respectively. The consultation with stakeholders will be essential for increasing the knowledge about MBI, identifying new evidence, and developing future strategies to guide public policies preventing burnout syndrome in health care professionals working in public services.
Results
This protocol will guide a scoping review to identify and map studies that used MBI to identify burnout syndrome in health care professionals working in public health services. The results of this review may be useful to public health care professionals, managers, policymakers, and the general population because these findings will help understand the validated, translated, and adapted versions of MBI and domains, number of items, Likert scales, and cutoff points or the latent profile analysis most used in the literature. Furthermore, possible research gaps may be identified to guide future studies. All information regarding the stages of the scoping review favor its transparency and allow it to be methodologically replicated according to the principles of open science, thereby reducing the risk of bias and data duplication.
Conclusions
This study may reveal the multiplicity of scales described in the literature and the different forms of assessing burnout syndrome in health care professionals. This study may help to standardize the assessment of burnout syndrome in health care professionals working in public health services and contribute to the discussion and knowledge dissemination about burnout syndrome and mental health in this population.
International Registered Report Identifier (IRRID)
DERR1-10.2196/42338
Keywords: health care personnel; health care workers; public health services; Maslach burnout inventory; burnout, health care professional; workplace stress; mental health; occupational health; psychological well-being; policymaker
Introduction
Burnout syndrome is a work-related psychological syndrome included in the International Classification of Diseases 11th Revision (code QD85) [1]. Herbert Freudenberger described this syndrome in 1974 [2,3], and it is characterized by a chronic response to interpersonal stressors in the workplace that may be related to work organization and environment [4,5]. The protocol in our study will guide a scoping review to identify and map studies that used the Maslach Burnout Inventory (MBI) to identify burnout syndrome in health care professionals working in public health services. The results of this review may be useful to public health care professionals, managers, policymakers, and the general population since these findings will help understand the validated, translated, and adapted versions of MBI and domains, number of items, Likert scales, and cutoff points or the latent profile analysis most used in the literature. Furthermore, possible research gaps may be identified to guide future studies. All information regarding the stages of the scoping review favor its transparency and allow it to be methodologically replicated according to the principles of open science, thereby reducing the risk of bias and data duplication [3].
Different definitions of the burnout syndrome consider many etiological factors; thus, literature lacks a consensus about its definition and diagnostic criteria [6,7]. Some authors define burnout syndrome as fatigue and emotional exhaustion [8], whereas others consider it as emotional exhaustion and depersonalization [9]. Gil-Monte [10] defines burnout syndrome according to 4 dimensions: enthusiasm toward the job, psychological exhaustion, indolence, and guilt. Bakker et al [11] define the syndrome as mental distance from the job and emotional, physical, and cognitive exhaustion. One of the most used definitions of burnout syndrome was proposed by Maslach and Jackson who considered this syndrome as emotional exhaustion, depersonalization, and personal accomplishment associated with physical and psychological symptoms. Thus, this scoping review protocol used this definition to map the use of MBI [5].
The main characteristics of burnout syndrome are emotional exhaustion, resulting in fatigue; depersonalization, associated with negative behaviors and cynicism in work relationships; and low scores in personal accomplishment, with feelings of incompetence and low productivity [12-14]. Individuals with burnout syndrome see work as a source of misery and unpleasurable [3], leading to high employee turnover, work absenteeism, decreased quantity and quality of work, and increased occupational accidents, thereby representing institutional consequences [15,16]. People working with the general public are more prone to develop the burnout syndrome. Studies have shown burnout in several work fields; however, the most affected were teachers, police officers, and health care professionals (especially physicians and nurses) [6,17-19]. The burnout syndrome affects approximately 10%-70% of nurses and 30%-50% of physicians, nurse practitioners, and physician assistants [20] and is highly prevalent among health care professionals [21-24], especially among those working in public health services [25,26].
Many aspects of burnout syndrome have already been established, and more than 90% of the studies used MBI [27] to identify and implement preventive interventions and treatments [12,28]. MBI is a self-report questionnaire developed by Christina Maslach and Susan Jackson to obtain a multidimensional view of burnout and comprises 22 items divided into 3 sections: emotional exhaustion (9 items), depersonalization (5 items), and personal accomplishment (8 items). The original version uses a 7-point Likert scale (0 corresponds to “never” and 6 to “every day”) [5,29] that assesses burnout according to scores in each dimension: high levels of burnout are characterized by high scores in emotional exhaustion and depersonalization and low scores in personal accomplishment. According to studies, MBI must be used in a 3D approach to enhance the comprehension of the burnout syndrome, since all 3 dimensions are considered important for identifying burnout and the individual dimensions alone do not sufficiently define the construct [21,30-32].
MBI is also intended to investigate the syndrome in other work settings. The MBI-Educators Survey is intended for education professionals, and the MBI-General Survey measures the syndrome in any professional category. For health care professionals, there is a specific version called the MBI Human Services Survey [5,29]. The MBI-Student Survey is designed to identify burnout in students [33]. The literature shows different translated, validated, and adapted versions of MBI. This diversity constitutes a challenge for the development of research using the instrument, since it can impact the interpretation of data and make comparisons between studies impossible, as well as hinder the identification of workers at risk for developing the syndrome because there is no standardization in its use.
The choice of the setting in our study was due to evidence in the literature that professionals working in public health services are more exposed to stress, thereby causing burnout [34]. In these services, there is usually wage-related dissatisfaction on the part of professionals, the need for better planning of actions and work processes [35,36], the difficulty in operationalizing actions, underfunding, and poor infrastructure [35-37]. The evidence of the aforementioned factors in public health services should be considered and will help us in terms of understanding that the development of burnout syndrome in health care professionals may be related to the organization and development of the work process in these services, which reflects the importance of conducting this study in the current context. Considering the global importance of MBI for identifying burnout syndrome [38], we conducted a preliminary search in the Joanna Briggs Institute (JBI) evidence synthesis, the international Prospective Register of Systematic Reviews (PROSPERO), Cochrane Library, and PubMed/MEDLINE databases by using the descriptors “health care professionals,” “public health services,” “Maslach Burnout Inventory,” and “burnout syndrome.” We found only 1 integrative review synthesizing the use of MBI in Brazil; however, this study was not directed to public health care professionals [39]. No studies or protocols were found when expanding the search to other continents.
Therefore, this scoping review protocol will identify and map studies that used MBI to assess burnout syndrome in health care professionals working in public health services. It will allow us to map the evidence describing different translated and validated versions of MBI and assess the consistency in frequencies and cutoff points of the scale and its application in different countries, aiming to guide a possible standardization in its use. We will also evaluate possible research gaps regarding the use of MBI among health care professionals working in public health services.
Methods
Overview
This scoping review protocol follows the JBI reviewers’ manual [40] and is guided by the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) [41]. This protocol is registered in the Open Science Framework [42]. Our review will follow 6 stages [43,44], as shown in Figure 1.
Figure 1.
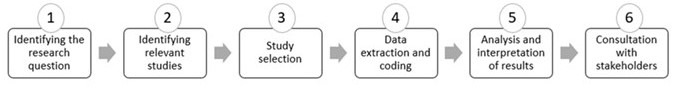
Stages of the scoping review.
First Stage: Identifying the Research Question
The research question was formulated using the Population, Concept, Context mnemonic [40] (Table 1). The Population, Concept, Context mnemonic maps information to identify knowledge gaps, present key concepts, quantify aspects of interest, and identify practices and evidence in the thematic area [45].
Table 1.
Definition of concepts used in the review.
| Research question theme | Definition | |
| Population: health care professionals in public services | ||
|
|
Health care professionals | Workers of health care services, with or without professional qualification, working or not in health programs and institutions, and subjected or not to government regulation |
|
|
Public health services | Responsibilities of the state government regarding health care. It includes responsibilities for executing activities and specific actions in public health, or mobilization, promotion, orientation, and articulation of social agents [46] |
| Concept: use of the Maslach Burnout Inventory | ||
|
|
Maslach Burnout Inventory | Instrument used to investigate burnout syndrome in workers [29] |
| Context: health care professionals with burnout syndrome | ||
|
|
Burnout syndrome | Psychological syndrome characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment and present in individuals working with the public [29] |
In this context, the questions of this scoping review protocol were defined as follows: “How is MBI used to identify burnout syndrome in health care professionals working in public health services?”, “What is the most studied professional category using MBI?”, “What are the main results of MBI in health care professionals working in public health service?”, and “What are the recommendations for clinical practice arising from the use of MBI?”
Second Stage: Identifying Relevant Studies
The search strategy was based on 4 controlled vocabularies in health: health sciences descriptors, medical subject headings, Emtree, and the American Psychological Association thesaurus. Natural language processing was used to increase sensitivity and expand the search results [47,48]. A librarian also refined the search strategy to increase the number of results in all the databases. The strategy was built using a high sensitivity model composed of extraction, conversion, combination, construction, and use [47]. Table 2 shows the conversion of the mnemonics into descriptors.
Table 2.
Conversion of mnemonics.
| Mnemonic | Extraction | Conversion |
| Population | Health care professionals working in public health services | Health care personnel Public health services |
| Concept | Use of the Maslach Burnout Inventory | Maslach Burnout Inventory |
| Context | Health care professionals with burnout syndrome | Burnout |
A description of the complete search strategy for PubMed/MEDLINE is shown in Multimedia Appendix 1. An initial exploratory search was performed in PubMed/MEDLINE to identify the main medical subject headings related to the topic. The search strategy combined the Boolean operators AND and OR and will be further adjusted to each database (Embase, LILACS, PubMed/MEDLINE, PsycINFO, Scopus, and Web of Science). The grey literature will be explored in ProQuest Dissertations & Theses Global, Google Scholar, Brazilian Digital Library of Theses and Dissertations, and Open Access Theses and Dissertations. Additional sources will also be manually retrieved from reference lists. If needed, authors will be contacted for additional information.
Third Stage: Study Selection
The following inclusion criteria will be adopted: quantitative and qualitative full-text studies using MBI among health care professionals working in public health services and no language restriction and no publication date restriction. Duplicated studies, literature reviews, letters, editorials, theoretical essays, opinion articles, and studies analyzing burnout syndrome in non–health care professionals or private services will be excluded. Relevant studies will be retrieved and exported to a spreadsheet. Duplicated studies will be manually excluded. Two independent researchers will read titles and abstracts, and a third reviewer will be consulted in case of disagreement. Texts will be analyzed according to inclusion criteria, and reasons for exclusion will be registered and reported. Following the JBI manual, a pilot test with a random sample of 25 studies (title and abstract) will be conducted to assess eligibility criteria and agreement among the researchers enrolled (it must reach at least 75% of agreement before proceeding with independent assessment) [40]. Details regarding study selection (identification, screening, eligibility, and inclusion) will be presented in a flowchart [41].
Fourth Stage: Data Extraction and Coding
Two independent reviewers will chart data by using an adapted data extraction form based on the JBI model [35] (Table 3).
Table 3.
Instrument for data extraction.a
| Variable | Standardization |
| Study type | Article, dissertation, or thesis |
| Publication date | Year of publication |
| Publication context | Where the study was conducted/published |
| Journal | In which journal the study was published |
| Author qualification | Major degree of the first author |
| Aim/purpose | Aim or purpose of the study |
| Research type | Research type described by authors |
| Data collection | Methods for data collection |
| Study population | Health care professionals and sample size |
| Sample | Number of participants |
| Maslach Burnout Inventory | Version of the Maslach Burnout Inventory used |
| Maslach Burnout Inventory domains used | Emotional exhaustion, depersonalization, and personal accomplishment |
| Items and Likert scale | Number of items and Likert score |
| Cutoff points or Latent profile analysis |
Cutoff points to identify burnout syndrome or Alternative methods for identifying burnout |
| Results | Main results of the study |
| Challenges and limitations | Description of challenges and limitations in using the scale |
| Recommendations for practice Administration method |
How the study contributes to improving the mental health of health care professionals In-person or using digital tools |
aSource: Adapted from Joanna Briggs Institute model [41].
Fifth Stage: Analysis and Interpretation of Results
Quantitative data will be analyzed using descriptive statistics and presented in absolute or relative frequency, whereas qualitative analysis will identify meanings and patterns by using thematic analysis [49].
Sixth Stage: Consultation With Stakeholders
Preliminary results will be presented to 5 researchers in the field of burnout syndrome to contribute to knowledge dissemination, disclosure of findings, and identification of gaps in the use of MBI, frequencies, and cutoff points adopted worldwide. This step will be essential to increase knowledge about MBI, identify new evidence, and develop future strategies to guide public policies preventing burnout syndrome in health care professionals from public services [45]. An email containing the written informed consent and an electronic form with preliminary results will be sent to stakeholders. Interested parties will not be identified, and authors will ask for an analysis of the results.
Ethics Approval
This study followed the ethical principles in human research and was approved by the research ethics committee of the Onofre Lopes University Hospital (4.952.319 and CAAE 46284921.4.0000.5292) on September 3, 2021.
Results
This protocol will guide a scoping review to identify and map studies that used MBI to identify burnout syndrome in health care professionals working in public health services. The results of this review may be useful to public health care professionals, managers, policymakers, and the general population since the findings will help understand the validated, translated, and adapted versions of MBI and domains, number of items, Likert scales, and cutoff points or the latent profile analysis most used in the literature. Furthermore, possible research gaps may be identified to guide future studies. All information regarding the stages of the scoping review favor its transparency and allow it to be methodologically replicated according to the principles of open science, thereby reducing the risk of bias and data duplication.
Discussion
Principal Findings
This protocol will guide a scoping review to identify and map studies that used MBI to identify burnout syndrome in health care professionals working in public health services. This is one of the most important instruments used to identify burnout syndrome and is used worldwide, especially among health care professionals. In addition to the classification by cutoff points, this study advances the consideration of alternative methods for identifying burnout (latent profile analysis) to highlight significant associations and guide the identification of the number of profiles for a given construct. Through this analysis, it will be possible to explore whether the identified profiles differ from the clustering of MBI scores [50,51]. The protocol was developed by a research team with knowledge and experience in scoping reviews and by applying MBI to identify the burnout syndrome. A librarian helped develop a high-sensitivity search strategy based on the combination of 4 vocabularies and no date or language limitations to expand the results and allow a broad access to the literature. All information regarding the stages of the scoping review favor its transparency and allow it to be methodologically replicated according to the principles of open science, thereby reducing the risk of bias and data duplication.
Limitations
As a limitation of the study, we emphasize that the multiplicity of MBI scales that can be found may reveal possible biases regarding the correct use of the instrument. In this sense, we will summarize the results according to the version of MBI most applied in each country and the populations studied. Although this protocol will guide the searches and development of the scoping review, it may not cover the entire literature; thus, studies indexed in different databases may not be found. Although we did not impose a language limitation for inclusion of the studies, the use of descriptors and search terms in English and Portuguese languages may be a limitation for this study.
Conclusions
This study protocol presents the main methodological steps that will guide the scoping review and identify and map studies that used the MBI scale to identify the burnout syndrome in health care professionals working in public health services. This study may reveal the multiplicity of scales described in the literature and the different forms of assessing burnout syndrome in health care professionals. The results of our study may also help to standardize the assessment of burnout syndrome in health care professionals working in public health services and promote knowledge dissemination about burnout syndrome and mental health in this population.
Acknowledgments
The authors acknowledge the support provided by the Wánderson Cássio Oliveira Araújo in constructing the search strategy and Probatus Academic Services for providing scientific language translation, revision, and editing.
Abbreviations
- JBI
Joanna Briggs Institute
- MBI
Maslach Burnout Inventory
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses-Extension for Scoping Reviews
- PROSPERO
International Prospective Register of Systematic Reviews
Complete strategy for the search in MEDLINE/PubMed.
Footnotes
Authors' Contributions: JPS conceptualized this study. JPS, RHL, PBdSM, CRDVS, CCFMR, and JLdC devised the methodology, wrote the original draft of the paper, and reviewed and edited this paper. JPS, RHL, and PBdSM performed data curation and formal analysis. JLdC performed study administration and supervision. All authors have read and agree with the publication of this paper.
Conflicts of Interest: None declared.
References
- 1.International classification of diseases 11th revision. World Health Organization. [2022-07-10]. https://icd.who.int/en .
- 2.Freudenberger HJ. Staff burn-out. Journal of Social Issues. 1974:159–65. doi: 10.1111/j.1540-4560.1974.tb00706.x. doi: 10.1111/j.1540-4560.1974.tb00706.x. [DOI] [Google Scholar]
- 3.Ribeiro KCR. O processo de gestão de pessoas como ferramenta inovadora para o enfrentamento da síndrome de Burnout. Rev Intel Comp. https://iberoamericanic.org/rev/article/view/356 .
- 4.Cardoso HF, Baptista MN, de Sousa DF, Goulart Júnior E. Síndrome de burnout: análise da literatura nacional entre 2006 e 2015. Rev Psicol Organ Trab. http://pepsic.bvsalud.org/pdf/rpot/v17n2/v17n2a07.pdf .
- 5.Maslach C, Jackson S. The measurement of experienced burnout. J Organiz Behav. 1981 Apr;2(2):99–113. doi: 10.1002/job.4030020205. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 6.Perniciotti P, Serrano Júnior CV, Guarita RV, Morales RJ, Romano BW. Síndrome de Burnout nos profissionais de saúde: atualização sobre definições, fatores de risco e estratégias de prevenção. Pepsic. 2020. [2022-10-13]. http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1516-08582020000100005 .
- 7.Soares JP, de Oliveira NHS, Mendes TMC, Ribeiro SS, de Castro JL. Burnout-related factors in health professionals during the Covid-19 pandemic: an integrative review. Saúde debate. 2022. [2022-08-13]. https://scielosp.org/pdf/sdeb/2022.v46nspe1/385-398/en .
- 8.Kristensen T, Borritz M, Villadsen E, Christensen K. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work & Stress. 2005 Jul;19(3):192–207. doi: 10.1080/02678370500297720. doi: 10.1080/02678370500297720. [DOI] [Google Scholar]
- 9.Kalliath T, O'Driscoll M, Gillespie D, Bluedorn A. A test of the Maslach Burnout Inventory in three samples of healthcare professionals. Work & Stress. 2000 Jan;14(1):35–50. doi: 10.1080/026783700417212. doi: 10.1080/026783700417212. [DOI] [Google Scholar]
- 10.Gil-Monte P. Influencia del género sobre el proceso de desarrollo del síndrome de quemarse por el trabajo en profesionales de enfermería. Psicol Estud. 2002;7(1):3–10. doi: 10.1590/s1413-73722002000100003. [DOI] [Google Scholar]
- 11.Bakker A, Demerouti E, Sanz-Vergel A. Burnout and Work Engagement: The JD–R Approach. Annu Rev Organ Psychol Organ Behav. 2014 Mar 21;1(1):389–411. doi: 10.1146/annurev-orgpsych-031413-091235. doi: 10.1146/annurev-orgpsych-031413-091235. [DOI] [Google Scholar]
- 12.Aronsson G, Theorell T, Grape T, Hammarström Anne, Hogstedt C, Marteinsdottir Ina, Skoog Ingmar, Träskman-Bendz Lil, Hall Charlotte. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health. 2017 Mar 16;17(1):264. doi: 10.1186/s12889-017-4153-7. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4153-7 .10.1186/s12889-017-4153-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maslach C, Schaufeli W, Leiter M. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397.52/1/397 [DOI] [PubMed] [Google Scholar]
- 14.Robinson D, Luton O, Mellor K, James O, Hopkins L, Powell A, Hemington-Gorse Sarah, Harries Rhiannon L, Egan Richard J, Lewis Wyn G. Trainee perspective of the causes of stress and burnout in surgical training: a qualitative study from Wales. BMJ Open. 2021 Aug 02;11(8):e045150. doi: 10.1136/bmjopen-2020-045150. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=34341033 .bmjopen-2020-045150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carro AC, Nunes RD. Ideação suicida como fator associado à síndrome de Burnout em estudantes de Medicina. J bras psiquiatr. 2021. [2022-06-13]. https://www.scielo.br/j/jbpsiq/a/NqqrmfgvSp8TcYtGJWQ96CL/?lang=pt .
- 16.Hadžibajramović Emina, Ahlborg G, Grimby-Ekman A. Concurrent and lagged effects of psychosocial job stressors on symptoms of burnout. Int Arch Occup Environ Health. 2019 Oct;92(7):1013–1021. doi: 10.1007/s00420-019-01437-0. https://europepmc.org/abstract/MED/31111207 .10.1007/s00420-019-01437-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silva S, Oliveira A. Burnout among teachers in private institutions of higher education. Psicol. 2019:1–10. doi: 10.1590/2175-35392019017785. doi: 10.1590/2175-35392019017785. [DOI] [Google Scholar]
- 18.Dias CN, de Andrade VLP. A relação entre a síndrome de burnout e o policial militar brasileiro. Cad. Psic. 2020. [2022-10-13]. https://seer.uniacademia.edu.br/index.php/cadernospsicologia/article/view/2837 .
- 19.Pradas-Hernández Laura, Ariza T, Gómez-Urquiza José Luis, Albendín-García Luis, De la Fuente Emilia I, Cañadas-De la Fuente Guillermo A. Prevalence of burnout in paediatric nurses: A systematic review and meta-analysis. PLoS One. 2018;13(4):e0195039. doi: 10.1371/journal.pone.0195039. https://dx.plos.org/10.1371/journal.pone.0195039 .PONE-D-17-35813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bridgeman P, Bridgeman M, Barone J. Burnout syndrome among healthcare professionals. Am J Health Syst Pharm. 2018 Feb 01;75(3):147–152. doi: 10.2146/ajhp170460.ajhp170460 [DOI] [PubMed] [Google Scholar]
- 21.De la Fuente-Solana EI, Pradas-Hernández Laura, González-Fernández Carmen Tamara, Velando-Soriano A, Martos-Cabrera M, Gómez-Urquiza José L, Cañadas-De la Fuente Guillermo Arturo. Burnout Syndrome in Paediatric Nurses: A Multi-Centre Study. Int J Environ Res Public Health. 2021 Feb 01;18(3):1324. doi: 10.3390/ijerph18031324. https://www.mdpi.com/resolver?pii=ijerph18031324 .ijerph18031324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.González-Rodríguez R, López-Castedo A, Pastor-Seller E, Verde-Diego C. Síndrome de burnout en el Sistema de Salud: el caso de las trabajadoras sociales sanitarias. Enf Global. 2020 Mar 13;19(2):141–161. doi: 10.6018/eglobal.382631. doi: 10.6018/eglobal.382631. [DOI] [Google Scholar]
- 23.Owoc J, Mańczak Małgorzata, Tombarkiewicz M, Olszewski R. Burnout, well‑being, and self‑reported medical errors among physicians. Pol Arch Intern Med. 2021 Aug 30;131(7-8):626–632. doi: 10.20452/pamw.16033. https://pamw.pl/en/issue/article/34142768 . [DOI] [PubMed] [Google Scholar]
- 24.Gan Y, Jiang H, Li L, Yang Y, Wang C, Liu J, Yang Tingting, Opoku Sampson, Hu Sai, Xu Hongbin, Herath Chulani, Chang Yuanyuan, Fang Pengqian, Lu Zuxun. Prevalence of burnout and associated factors among general practitioners in Hubei, China: a cross-sectional study. BMC Public Health. 2019 Dec 02;19(1):1607. doi: 10.1186/s12889-019-7755-4. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7755-4 .10.1186/s12889-019-7755-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coetzee J, Kluyts H. Burnout and areas of work-life among anaesthetists in South Africa Part 1 : Burnout. Southern African Journal of Anaesthesia and Analgesia. 2020 Mar 31;26(2):73–82. doi: 10.36303/SAJAA.2020.26.2.2358. doi: 10.36303/SAJAA.2020.26.2.2358. [DOI] [Google Scholar]
- 26.Lim R, Pinto C. Work stress, satisfaction and burnout in New Zealand radiologists: comparison of public hospital and private practice in New Zealand. J Med Imaging Radiat Oncol. 2009 Apr;53(2):194–9. doi: 10.1111/j.1754-9485.2009.02063.x.ARA2063 [DOI] [PubMed] [Google Scholar]
- 27.Olivares Faúndez V. Laudatio: Dra. Christina Maslach, Comprendiendo el Burnout. Cienc Trab. 2017 Apr;19(58):59–63. doi: 10.4067/s0718-24492017000100059. [DOI] [Google Scholar]
- 28.Rodrigues H, Cobucci R, Oliveira A, Cabral J, Medeiros L, Gurgel K, Souza Tházio, Gonçalves Ana Katherine. Burnout syndrome among medical residents: A systematic review and meta-analysis. PLoS One. 2018;13(11):e0206840. doi: 10.1371/journal.pone.0206840. https://dx.plos.org/10.1371/journal.pone.0206840 .PONE-D-18-09735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. Lanham: Scarecrow Education; 1997. [Google Scholar]
- 30.Khan N, Palepu A, Dodek P, Salmon A, Leitch H, Ruzycki S, Townson Andrea, Lacaille Diane. Cross-sectional survey on physician burnout during the COVID-19 pandemic in Vancouver, Canada: the role of gender, ethnicity and sexual orientation. BMJ Open. 2021 May 10;11(5):e050380. doi: 10.1136/bmjopen-2021-050380. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=33972345 .bmjopen-2021-050380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li H, Yuan B, Meng Q, Kawachi I. Contextual Factors Associated with Burnout among Chinese Primary Care Providers: A Multilevel Analysis. Int J Environ Res Public Health. 2019 Sep 23;16(19):3555. doi: 10.3390/ijerph16193555. https://www.mdpi.com/resolver?pii=ijerph16193555 .ijerph16193555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lu S, Zhang L, Klazinga N, Kringos D. More public health service providers are experiencing job burnout than clinical care providers in primary care facilities in China. Hum Resour Health. 2020 Dec 03;18(1):95. doi: 10.1186/s12960-020-00538-z. https://human-resources-health.biomedcentral.com/articles/10.1186/s12960-020-00538-z .10.1186/s12960-020-00538-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carlotto MS, Câmara SG. [ARTIGO RETRATADO]Características psicométricas do Maslach Burnout Inventory - Student Survey (MBI-SS) em estudantes universitários Brasileiros. Psico-USF. 2006 Dec;11(2):167–173. doi: 10.1590/s1413-82712006000200005. [DOI] [Google Scholar]
- 34.Petrelli Fabio, Scuri Stefania, Tanzi Elisabetta, Nguyen Cuc, Grappasonni Iolanda. Public health and burnout: a survey on lifestyle changes among workers in the healthcare sector. Acta Biomed. 2019 Nov 28;90(1):24–30. doi: 10.23750/abm.v90i1.7626. https://europepmc.org/abstract/MED/30889151 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Da Cunha FM, Mendes A. Revisão narrativa sobre a questão da saúde do trabalhador no Sistema Único de Saúde. J Manag Prim Health Care. 2021 Dec 08;13:e018. doi: 10.14295/jmphc.v13.1164. doi: 10.14295/jmphc.v13.1164. [DOI] [Google Scholar]
- 36.Sacardo D, Fortes P, Tanaka OY. Novas perspectivas na gestão do sistema de saúde da Espanha. Saude soc. 2010 Mar;19(1):170–179. doi: 10.1590/S0104-12902010000100014. doi: 10.1590/S0104-12902010000100014. [DOI] [Google Scholar]
- 37.Campos JJBD, Forster AC, Freire Filho JR. Lições aprendidas na comparação dos sistemas de saúde brasileiro e espanhol. RSPP. 2016 Nov 23;17(1):121. doi: 10.22421/1517-7130.2016v17n1p121. [DOI] [Google Scholar]
- 38.Vidotti V, Ribeiro R, Galdino M, Martins J. Burnout Syndrome and shift work among the nursing staff. Rev Lat Am Enfermagem. 2018 Aug 09;26:e3022. doi: 10.1590/1518-8345.2550.3022. https://www.scielo.br/scielo.php?script=sci_arttext&pid=S0104-11692018000100337&lng=en&nrm=iso&tlng=en .S0104-11692018000100337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Campos ICM, Pereira SS, Schiavon ICA, Alves M. Maslach burnout inventory - human services survey (mbi-hss): revisão integrativa de sua utilização em pesquisas brasileiras. Arq Ciênc Saúde Unipar. 2020 Nov 20;24(3):187–195. doi: 10.25110/arqsaude.v24i3.2020.7875. [DOI] [Google Scholar]
- 40.Peters M, Godfrey C, Khalil H, McInerney P, Parker D, Soares C. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015:141–146. doi: 10.1097/XEB.0000000000000050. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 41.Tricco A, Lillie E, Zarin W, O'Brien K, Colquhoun H, Levac D. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern. Med. 2018:467–473. doi: 10.7326/M18-0850. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 42.Soares JP, Lopes RH, de Souza Mendonça PB, de Castro JL. Use of the maslach burnout inventory in public health care professionals: a scoping review protocol. OSF Home. [2022-08-29]. https://osf.io/search/?q=USE%20OF%20THE%20MASLACH%20BURNOUT%20INVENTORY%20IN%20PUBLIC%20HEALTH . [DOI] [PMC free article] [PubMed]
- 43.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005 Feb;8(1):19–32. doi: 10.1080/1364557032000119616. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 44.Levac D, Colquhoun H, O'Brien K. Scoping studies: advancing the methodology. Implement Sci. 2010 Sep 20;5:69. doi: 10.1186/1748-5908-5-69. https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-5-69 .1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Methodology for JBI scoping reviews. Joanna Briggs Institute Reviewers Manual 2015. [2022-10-14]. https://nursing.lsuhsc.edu/jbi/docs/reviewersmanuals/scoping-.pdf .
- 46.Organización PDLS. La salud pública en las americas: nuevos conceptos, análisis del desempeño y bases para la acción. Publicación Científica y Técnica. 2002. Jul 10, [2022-07-10]. https://iris.paho.org/bitstream/handle/10665.2/42858/9275315892_spa.pdf?sequence=1&isAllowed=y .
- 47.Oliveira Araújo WC. Recuperação da informação em saúde: construção, modelos e estratégias. ConCI. 2020 Jul 10;3(2):100–134. doi: 10.33467/conci.v3i2.13447. doi: 10.33467/conci.v3i2.13447. [DOI] [Google Scholar]
- 48.Siddaway A, Wood A, Hedges L. How to Do a Systematic Review: A Best Practice Guide for Conducting and Reporting Narrative Reviews, Meta-Analyses, and Meta-Syntheses. Ann Rev Psychol. 2019 Jan 04;70:747–770. doi: 10.1146/annurev-psych-010418-102803. [DOI] [PubMed] [Google Scholar]
- 49.Moher D, Liberati A, Tetzlaff J, Altman D, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. https://dx.plos.org/10.1371/journal.pmed.1000097 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leiter MP, Maslach C. Latent burnout profiles: A new approach to understanding the burnout experience. Burnout Research. 2016 Dec;3(4):89–100. doi: 10.1016/j.burn.2016.09.001. [DOI] [Google Scholar]
- 51.Berjot S, Altintas E, Grebot E, Lesage F. Burnout risk profiles among French psychologists. Burnout Research. 2017 Dec;7:10–20. doi: 10.1016/j.burn.2017.10.001. doi: 10.1016/j.burn.2017.10.001. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Complete strategy for the search in MEDLINE/PubMed.


