Abstract
Background
Herd immunity is necessary to contain the coronavirus disease 2019 (COVID-19) pandemic. Vaccination is the fastest and safest pandemic control strategy. Healthcare workers (HCWs) are essential in providing vaccination information. The aim of this study was to assess intent to be vaccinated against COVID-19 among HCWs in Egypt and to determine the factors that may influence their decision.
Methods
A questionnaire-based cross-sectional study was conducted among HCWs who care for patients in several hospitals in Delta region, Egypt. The questionnaire included sociodemographic, clinical, and occupational data, intention to receive the COVID-19 vaccine, and beliefs and attitudes towards COVID-19 and its vaccination.
Results
The study included 455 HCWs with a mean age of 36.55 years (SD = 10.31) and 80% were females. The acceptance rate for the COVID-19 vaccine was 70.5%, while hesitancy and resistancy were both 17.6 and 11.9% respectively. About one-third (33.4%) of the subjects had previously contracted COVID-19. Most participants believed that they had a higher risk of contracting COVID-19 (71.6%). More than 64% believed they were at risk for vaccination side effects. Fear of infection and being at high risk of infection were the main drivers for COVID-19 vaccination, while the major barriers were waiting for additional experience with these new vaccines and having doubts about the vaccines’ efficacy.
Conclusions
The acceptance of the COVID-19 vaccination among HCWs is very high. This crucial group needs to be the focus of educational initiatives and campaigns designed to increase public awareness of the safety and effectiveness of COVID-19 vaccination.
Keywords: COVID-19, Vaccine acceptance, Vaccine hesitancy, Health care workers, Egypt
Introduction
Globally, the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) caused coronavirus disease 2019 (COVID-19) pandemic poses a serious threat [1], instigating a pandemic affecting more than 185 countries [2]. The pandemic has crippled global economic activity, overloaded hospital systems, and induced panic among the general population [3].
Vaccination is one of the most important public health measures to stop the spread of certain infectious diseases and to lower their mortality rate [4]. According to the World Health Organization (WHO), vaccines prevented at least 10 million deaths between 2010 and 2015 [5]. To stop the COVID-19 pandemic, high vaccination rates are needed worldwide [6]. Since the emergence of this new corona virus, numerous organizations around the globe have conducted substantial research in an effort to create a vaccine that will protect people from this deadly new virus in a safe and efficient manner [7].
Globally, worries about vaccine hesitancy are rising, particularly in populous nations with poor literacy rates. The definition of vaccine hesitancy is “delay in accepting or refusing vaccinations notwithstanding the availability of vaccination services” [8].
Healthcare workers (HCWs) play a critical role in offering advice and recommendations to patients and the larger community about vaccination, including accurate information about the risks and advantages of the vaccine [9]. A Values Framework for the Allocation and Prioritization of COVID-19 Vaccination was released in September 2020 and recommends that governments give priority to HCWs, older people, and those with chronic diseases to receive the first doses of an approved COVID-19 vaccine [10].
Among the most trusted sources of information about vaccines and vaccination for the general public are the HCWs [11]. But not all HCWs enthusiastically accept or advocate COVID-19 vaccination. To enhance vaccination uptake, HCWs must be targeted with supportive communication [11]. However, there is little information about the beliefs and attitudes of Egyptian HCWs towards COVID-19 vaccination.
Thus, the aim of this study was to assess intent to be vaccinated against COVID-19 among HCWs in Egypt and to determine the factors that may influence their decision to delay or refuse to receive the vaccine.
Materials and methods
Study population
This questionnaire based cross-sectional study was conducted in the duration from August to September 2021. The main population of interest was HCWs who care for patients in several hospitals in Delta region, Egypt. Anyone involved in the delivery of healthcare services, including those who interact directly with patients and those who do not, was generically referred to as a HCW. Thus, a variety of healthcare positions were included by this term such as physicians, pharmacists, radiology, and laboratory technicians ...etc. The study was approved by the institutional review board of Mansoura University (Approval No: R.21.08.1398.R1) and was consistent with declaration of Helsinki 1995. All participants received comprehensive information regarding the study, and their written informed consent was obtained.
Sample size and sampling procedure
Healthcare staff employed by the hospitals were asked to participate in the study. Data were gathered using convenience sampling. The appropriate sample size was determined using the RaoSoft® online sample size calculator. We assumed the population size (current HCWs in Egypt) to be 375 thousand as provided by the most recent report of The Central Agency for Public Mobilization and Statistics (CAPMAS) [12]. Based on 50% predicted response, 5% margin of error and 80% degree of precision 95% confidence level, the minimum sample size was 385 participants.
Survey
The questionnaire was written in English and a bilingual study author translated it into Arabic. Following editing and review, five medical staff members examined the questionnaire design, content, wording, and simplicity of completion as part of a pilot study that validated the questionnaire. Based on this, two new items were added, four were removed, and five were reworded. Then, a preliminary questionnaire was developed and pilot-tested with a small sample of HCWs (n = 22). The internal consistency of the questionnaire was determined using Cronbach’s alpha coefficient. The reliability coefficient was 0.85, indicating that the internal consistency was good. The data of those who participated in the pilot study were subsequently omitted from the statistical analysis of the study. The questions were designed to be as simple and closed-ended as feasible except for the assessment of opinions towards conventional vaccines.
Survey administration
Interviews served as the basis for the study. It was intended to be completed in between 10 and 15 min. Early in the day, the interviewer visited the hospitals and spoke with as much HCWs as possible. All healthcare staff who volunteered to participate were interviewed during the interviewer’s visits to the hospitals. Face-to-face structured interviews were conducted by a single interviewer with each participant. All researchers contributed to the interviews with the HCWs. This mode of questioning makes it feasible to study complex issues than is possible in self-administered modes of questioning as the interviewer can provide more detailed explanations of the questions. Participants’ anonymity and secrecy were guaranteed by not requesting any personal information.
Questionnaire and variables gathered
To adapt the questionnaire to the setting of our study, we included the significant items that were found based on previous literature findings [13–16]. The variables evaluated include:
Sociodemographic and clinical data
The data collected included 8 questions about gender, age, marital status, residence, smoking habit, socioeconomic status, and associated comorbidities.
Occupational data
The participants were asked 4 questions that covered their occupation and occupation settings whether offices, laboratories, inpatient wards, intensive care units or others. Information about dealing with patients or interacting with them was also recorded along with the frequency of contact with COVID-19 patients in the workplace.
Clinical data of SARS-CoV-2 infection
Information was collected related to history and severity of SARS-CoV-2 infection among participants and their household or close friends. This section included 6 questions.
Perception, beliefs and attitudes towards COVID-19 and vaccination
Multiple questions about the perception of COVID-19 were also included. To determine the beliefs and attitudes towards conventional vaccination, the participants were asked to score their perception of efficacy, security, usefulness, and estimated knowledge of conventional vaccination in general where 0 was the lowest score and 10 was the highest score [17].
Additionally, 11 questions about attitudes and convictions regarding the COVID-19 vaccination were included. Eight knowledge-based questions (marked as K for Knowledge, K1-K8: “Yes = 1” vs. “No = 0,” score range: 0 to 8), designed to measure participants’ knowledge score about the COVID-19 vaccine, were included. The participants’ scores indicated how well-versed they were [18]. Also, participants were questioned about their sources of information about COVID-19 vaccine.
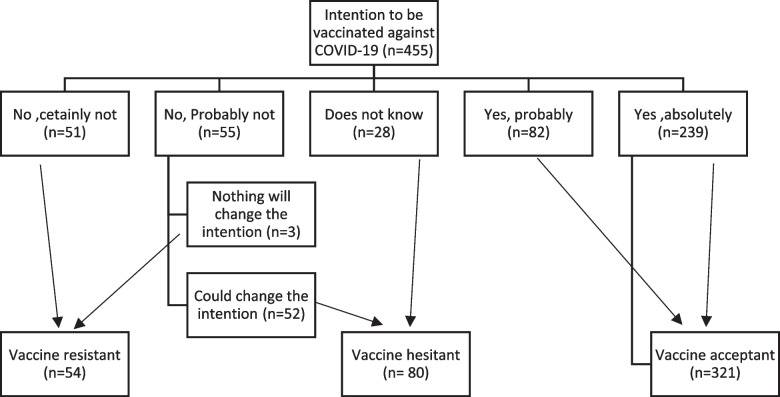
Then, the participants were divided into three groups according to the answer to COVID-19 vaccine intention question. The group who answered “Yes, absolutely” or “Yes, probably” was considered as vaccine acceptant group (VA). Those who answered “No, probably not” or “I do not know” were considered as vaccine hesitant group (VH). Participants were considered as vaccine resistant (VR) when their answers were “No, certainly not” or “No, probably not”. Questions about COVID-19 barriers and motivators were also included.
Status of COVID-19 vaccination
Finally, COVID-19 vaccination status was questioned, and vaccinated participants were asked about the received vaccine type and side effects including allergy, fever, rash, rigors, bone aches, fatigue, headache, GIT upset and chest symptoms.
Statistical analysis
The responses of participants were documented and conveyed to excel spread sheets. Statistical Package for Social Science (SPSS) version 22 was used to analyze the gathered data. Quantitative data were presented as means with standard deviation (SD) for parametric variables or medians (min-max) for nonparametric variables, and qualitative data were given as numbers and percentages. Shapiro-Wilk test was employed to evaluate the normality of the distribution of variables. One-way ANOVA test was used for parametric variables to compare between the study groups, whereas Kruskal-Wallis test was utilized for non-parametric variables. Comparing qualitative variables was done using the Chi-square test. Significant was defined as a P value of less than 0.05.
Results
This study was conducted on 455 HCWs (response rate,75.8%), their mean age was 36.55 years (SD = 10.31). More than 80% of the participants were females. About half of them (50.1%) were from rural origin. Fifty-two were hypertensive (11.4%) and 44 were diabetic (9.7%). Other sociodemographic and clinical data of the participants are illustrated in Table 1.
Table 1.
Sociodemographic and clinical data of the study health care workers according to their intention to get COVID-19 vaccine (n = 455)
| Variable n (%), mean ± SD |
Total (n = 455) |
Vaccine Acceptant group (n = 321) |
Vaccine Hesitant group (n = 80) |
Vaccine Resistsnt group (n = 54) |
P |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 367 (80.7) | 254 (79.1) | 68 (85) | 45 (83.3) | 0.428 |
| Male | 88 (19.3) | 67 (20.9) | 12 (15) | 9 (16.7) | |
| Age, years | 36.55 ± 10.31 | 35.92 ± 10.21 | 37.09 ± 10.19 | 39.46 ± 10.66 | 0.057 |
| 18–24 | 51 (11.2) | 40 (12.5) | 7 (8.8) | 4 (7.4) | 0.539 |
| 25–35 | 182 (40) | 134 (41.7) | 32 (40) | 16 (29.6) | |
| 36–45 | 132 (29) | 88 (27.4) | 25 (31.3) | 19 (35.2) | |
| 46–60 | 86 (18.9) | 57 (17.8) | 15 (18.8) | 14 (25.9) | |
| more than 60 | 4 (0.9) | 2 (0.6) | 1 (1.3) | 1 (1.9) | |
| Marital status | |||||
| Single/divorced/widowed | 128 (28.1) | 103 (32.1) | 19 (23.8) | 6 (11.1) | 0.004* |
| Married | 327 (71.9) | 218 (67.9) | 61 (76.3) | 48 (88.9) | |
| Residence | |||||
| Rural | 228 (50.1) | 148 (46.1) | 53 (66.3) | 27 (50) | 0.006* |
| Urban | 227 (49.9) | 173 (53.9) | 27 (33.8) | 27 (50) | |
| Smoking | |||||
| Never | 421 (92.5) | 296 (92.2) | 76 (95) | 49 (90.7) | 0.687 |
| Former smoker | 8 (1.8) | 5 (1.6) | 2 (2.5) | 1 (1.9) | |
| Current smoker | 26 (5.7) | 20 (6.2) | 2 (2.5) | 4 (7.4) | |
| Active lifestyle | 360 (79.1) | 257 (80.1) | 57 (71.3) | 46 (85.2) | 0.112 |
| Socioeconomic status | |||||
| Low | 44 (9.7) | 26 (8.1) | 10 (12.5) | 8 (14.8) | 0.490 |
| Average | 381 (83.7) | 274 (85.4) | 65 (81.3) | 42 (77.8) | |
| High | 30 (6.6) | 21 (6.5) | 5 (6.3) | 4 (7.4) | |
| Comorbidities | |||||
| Diabetes | 44 (9.7) | 31 (9.7) | 8 (10) | 5 (9.3) | 0.990 |
| Hypertension | 52 (11.4) | 38 (11.8) | 7 (8.8) | 7 (13) | 0.689 |
| Chronic respiratory disease | 9 (2) | 6 (1.9) | 2 (2.5) | 1 (1.9) | 0.934 |
| Psychiatric disorder | 7 (1.5) | 3 (0.9) | 3 (3.8) | 1 (1.9) | 0.184 |
| Ischemic heart disease | 5 (1.1) | 3 (0.9) | 0 | 2 (3.7) | 0.114 |
| Autoimmune Disease | 4 (0.9) | 3 (0.9) | 1 (1.3) | 0 | 0.735 |
| Chronic renal disease | 3 (0.7) | 1 (0.3) | 2 (2.5) | 0 | 0.078 |
| Chronic liver disease | 5 (1.1) | 2 (0.6) | 2 (2.5) | 1 (1.9) | 0.302 |
| Hypersensitivity | 67 (14.7) | 47 (14.6) | 11 (13.8) | 9 (16.7) | 0.894 |
| Obesity | 29 (6.4) | 21 (6.5) | 5 (6.3) | 3 (5.6) | 0.962 |
| Others | 20 (4.4) | 12 (3.7) | 3 (3.8) | 5 (9.3) | 0.178 |
*P < 0.05
Participants were classified according to intention to receive COVID-19 vaccine into 3 groups: the largest group was VA group (321,70.5%), followed by VH (80,17.6%) then VR group (54,11.9%) (Fig. 1).
Fig. 1.
Classification of the study health care workers according to intention to receive COVID-19 vaccine (n = 455)
Occupational data are shown in Table 2. The participants included nurses (37.8%), physicians (25.9%), administrators (10.1%), workers or security officers (5.3%), radiology or laboratory technicians (4.4%), pharmacists (2.2%) and dentist (1.3%). About one third (31.6%) were working in outpatient, radiology, and hemodialysis units while 27.5% were working in inpatient wards, ambulance, emergency, operation and delivery rooms. Most of the participants (80%) were working in patient-facing areas. The frequency of contact with COVID-19 patients in the workplace was reported to be daily by 211 participants (46.4%), weekly by 83 (18.2) and monthly by 65 (14.3%).
Table 2.
Occupational data of the study health care workers (n = 455)
| Variable | Total (n = 455) n (%) |
Vaccine Acceptant group (n = 321) n (%) |
Vaccine Hesitant group (n = 80) n (%) |
Vaccine Resistsnt group (n = 54) n (%) |
P |
|---|---|---|---|---|---|
| Occupation | |||||
| Physician | 118 (25.9) | 102 (31.8) | 13 (16.3) | 3 (5.6) | < 0.001* |
| Nurse | 172 (37.8) | 105 (32.7) | 39 (48.8) | 28 (51.9) | |
| Dentist | 6 (1.3) | 6 (1.9) | 0 | 0 | |
| Pharmacist | 10 (2.2) | 6 (1.9) | 3 (3.8) | 1 (1.9) | |
| Administrator | 46 (10.1) | 38 (11.8) | 4 (5) | 4 (7.4) | |
| Radiology or laboratory technician | 20 (4.4) | 16 (5.) | 3 (3.8) | 1 (1.9) | |
| A worker or security officer | 24 (5.3) | 10 (3.1) | 9 (11.3) | 5 (9.3) | |
| others | 59 (13) | 38 (11.8) | 9 (11.3) | 12 (22.2) | |
| Occupation settings | |||||
| Offices | 45 (9.9) | 32 (10) | 11 (13.8) | 2 (3.7) | 0.012* |
| Labs | 29 (6.4) | 28 (8.7) | 0 | 1 (1.9) | |
| Patient facing non-clinical (community or hospital pharmacy) | 12 (2.6) | 7 (2.2) | 4 (5) | 1 (1.9) | |
| Outpatient, radiology, GP, hemodialysis unit | 144 (31.6) | 99 (30.8) | 29 (36.3) | 16 (29.6) | |
| Inpatient wards, ambulance, ER, Operation room, delivery room | 125 (27.5) | 91 (28.3) | 21 (26.3) | 13 (24.1) | |
| Intensive care | 22 (4.8) | 16 (5) | 3 (3.8) | 3 (5.6) | |
| Others | 78 (17.1) | 48 (15) | 12 (15) | 18 (33.3) | |
| Contact with patients or working in patient-facing areas | 364 (80) | 258 (80.4) | 63 (78.8) | 43 (79.6) | 0.945 |
| Frequency of contact with COVID-19 patients in the workplace | |||||
| Never | 96 (21.1) | 66 (20.6) | 17 (21.3) | 13 (24.1) | 0.272 |
| Daily | 211 (46.4) | 150 (46.7) | 33 (41.3) | 28 (51.9) | |
| Weekly | 83 (18.2) | 62 (19.3) | 12 (15) | 9 (16.7) | |
| Monthly | 65 (14.3) | 43 (13.4) | 18 (22.5) | 4 (7.4) | |
*P < 0.05
As shown in Table 3, about two thirds (63.3%) of the participants reported SARS-CoV-2 infection among their household or close friends. Additionally, 30.8% and 21.5% of our cohort, respectively, reported relative hospitalization or mortality due to SARS-CoV-2 infection. About one third (33.4%) of the subjects had previously contracted COVID-19, with symptoms lasting an average of 6 days. In terms of the COVID-19 course in previously infected individuals, 32.2% had a mild infection that did not require hospitalization or interfere with daily activities, 63.2% had a more complicated disease in the form of a prolonged disease course that did interfere with daily activities, and 4.6% had severe symptoms necessitating hospitalization. There was no ICU admission reported by any of the participants.
Table 3.
Clinical data of SARS-CoV-2 infection reported by the study health care workers (n = 455)
| Variable n (%), median (min-max) |
Total (n = 455) |
Vaccine Acceptant group (n = 321) |
Vaccine Hesitant group (n = 80) |
Vaccine Hesitant group (n = 54) |
P |
|---|---|---|---|---|---|
| COVID-19 diagnosis among the household or close friends | 288 (63.3) | 208 (64.8) | 45 (56.3) | 35 (64.8) | 0.978 |
| A relative has been hospitalized because of SARS-CoV-2 infection | 140 (30.8) | 105 (32.7) | 23 (28.8) | 12 (22.2) | 0.276 |
| A relative died from SARS-CoV-2 infection | 98 (21.5) | 74 (23.1) | 13 (16.3) | 11 (20.4) | 0.406 |
| Infected with COVID-19 | 152 (33.4) | 108 (33.6) | 25 (31.3) | 19 (35.2) | 0.751 |
| Duration of symptoms, from the first day you became ill until symptoms resolved, days | 6 (1–45) | 6 (1–45) | 1 (1–21) | 12 (1–45) | 0.002* |
| Course of SARS-CoV-2 infection | |||||
| Not hospitalized and no difficulties in performing daily activities | 49/152 (32.2) | 39/108 (36.1) | 5/25 (20) | 5/19 (26.3) | 0.029* |
| Not hospitalized but had some difficulties in performing my daily activities | 96/152 (63.2) | 67/108 (62) | 16/25 (64) | 13/19 (68.4) | |
| Hospitalized and did not require ICU | 7/152 (4.6) | 2/108 (1.9) | 4/25 (16) | 1/19 (5.3) | |
| Hospitalized and required ICU care | 0 | 0 | 0 | 0 | |
*P < 0.05
Most participants believed that they had a higher risk of contracting COVID-19 (71.6%). More than 64% thought that they were at risk for vaccination side effects, and the percentage of this perception was significantly higher in VR group (88.9%). Regarding perceptions of efficacy, security, utility, and estimated knowledge of conventional vaccines, there was a statistically significant difference between the VA, VH, and VR groups. Additionally, the knowledge score in the VA group was significantly higher than other groups (p = 0.001). Other beliefs and attitudes towards COVID-19 vaccination are illustrated in Table 4.
Table 4.
Perception, beliefs and attitudes of the study health care workers towards SARS-CoV-2 infection, conventional and COVID-19 vaccination (n = 455)
| Statement n (%), median (min-max) |
Total (n = 455) |
Vaccine Acceptant group (n = 321) |
Vaccine Hesitant group (n = 80) |
Vaccine Hesitant group (n = 54) |
P |
|---|---|---|---|---|---|
| SARS-CoV-2 infection | |||||
| Do you think that you at higher risk of contracting COVID-19? | 326 (71.6) | 230 (71.7) | 54 (67.5) | 42 (77.8) | 0.485 |
| Do you think that you may have more severe COVID-19 due to chronic illness? | 261 (57.4) | 182 (56.7) | 44 (55) | 35 (64.8) | 0.469 |
| Do you think that you are at higher risk of COVID-19 vaccine adverse events | 295 (64.8) | 193 (60.1) | 54 (67.5) | 48 (88.9) | 0.000* |
| Self-rated knowledge level about COVID-19 | |||||
| Very bad | 18 (4) | 11 (3.4) | 5 (6.3) | 2 (3.7) | 0.011* |
| Bad | 35 (7.7) | 15 (4.7) | 13 (16.3) | 7 (13) | |
| Average | 220 (48.4) | 156 (48.6) | 40 (50) | 24 (44.4) | |
| Good | 132 (29) | 100 (31.2) | 15 (18.8) | 17 (31.5) | |
| Very good | 50 (11) | 39 (12.1) | 7 (8.8) | 4 (7.4) | |
| Conventional vaccination (excluding COVID-19 vaccines) | |||||
| Efficacy | 6 (0–10) | 6 (0–10) | 5 (0–10) | 5 (0–10) | 0.001* |
| Security | 6 (0–10) | 7 (0–10) | 5 (0–10) | 3 (0–10) | 0.000* |
| Usefulness | 8 (0–10) | 8 (0–10) | 5 (0–10) | 5 (0–10) | 0.000* |
| Estimated knowledge | 7 (0–10) | 7 (0–10) | 5 (0–10) | 5 (0–10) | 0.001* |
| Knowledge score | 4 (0–8) | 4 (0–8) | 3 (0–6) | 3 (0–8) | < 0.001* |
| COVID-19 vaccination | |||||
| How important do you perceive the COVID-19 vaccine to be? | 354 (77.8) | 284 (88.5) | 43 (53.8) | 27 (50) | < 0.001* |
| How important you think that everyone in the community should get the COVID-19 vaccine once available? | 329 (72.3) | 274 (85.4) | 33 (41.3) | 22 (40.7) | < 0.001* |
| Vaccination of COVID-19 should always be compulsory once it is available | 247 (54.3) | 211 (65.7) | 26 (32.5) | 10 (18.5) | < 0.001* |
| Do you have concerns regarding the COVID-19 vaccination? | 312 (68.6) | 205 (63.9) | 59 (73.8) | 48 (88.9) | < 0.001* |
| Vaccination of COVID-19 should always be compulsory for health care workers once it is available | 311 (68.4) | 256 (79.8) | 37 (46.3) | 18 (33.3) | < 0.001* |
| I think that approval of the vaccine guarantees its safety | 204 (44.8) | 173 (53.9) | 20 (25) | 11 (20.4) | < 0.001* |
| Do you have concerns regarding the adverse effects of the vaccine | 316 (69.5) | 211 (65.7) | 60 (75) | 45 (83.3) | .017* |
| Do you have concerns about the ineffectiveness of the vaccine | 106 (23.3) | 77 (24) | 18 (22.5) | 11 (20.4) | .830 |
| Having a prior bad experience with any vaccines and their adverse reactions | 72 (15.8) | 34 (10.6) | 20 (25) | 18 (33.3) | < 0.001* |
| Do you have concerns for the acquisition of COVID-19 from the vaccine | 248 (54.5) | 148 (46.1) | 54 (67.5) | 46 (85.2) | < 0.001* |
| Do you think that COVID-19 vaccination is the best protective method against COVID-19 | 261 (57.4) | 223 (69.5) | 23 (28.8) | 15 (27.8) | < 0.001* |
*P < 0.05
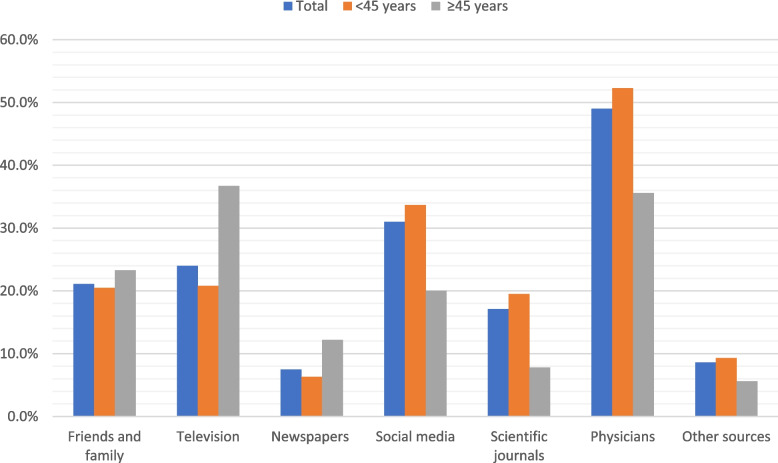
The sources of information about the COVID-19 vaccination are displayed in Fig. 2. Physicians were reported to be primary source of COVID-19 vaccine information in about half of the participants (49%) followed by social media for young participants (< 45 years) and television for others (≥45 years).
Fig. 2.
Sources of information about COVID-19 vaccine among the study health care workers according to the age (n = 455)
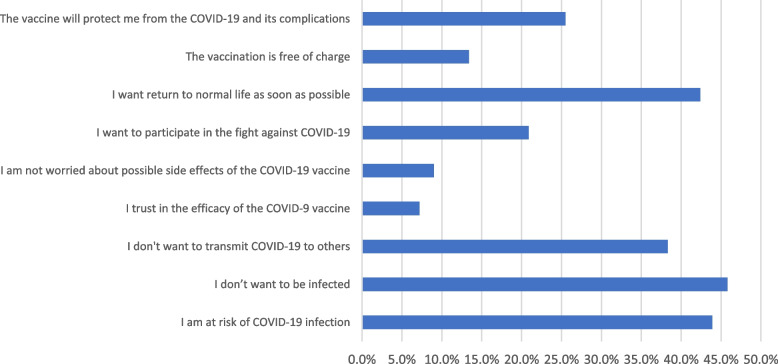
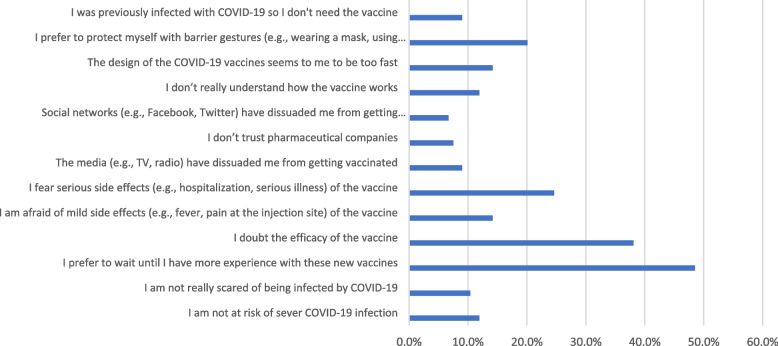
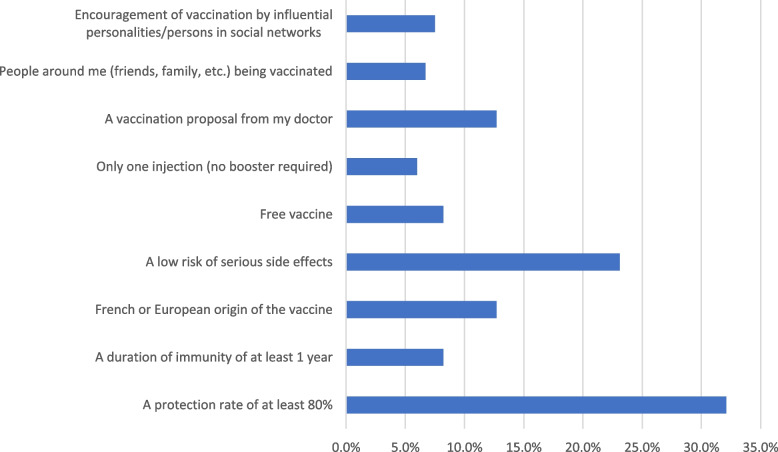
Fear of infection, being at high risk of infection, and the desire to resume normal life were the main drivers for COVID-19 vaccination in the VA group as shown in Fig. 3. On the other hand, the major barriers to the COVID-19 vaccination in the VR group were waiting for additional experience with these new vaccines and having doubts about the vaccines’ efficacy as illustrated in Fig. 4. The most significant factors that could influence the decision of the VH group are illustrated in Fig. 5.
Fig. 3.
The motivators of COVID-19 vaccination among COVID-19 vaccine acceptant group (n = 321)
Fig. 4.
Barriers of COVID-19 vaccination among COVID-19 vaccine hesitant and resistant groups (n = 134)
Fig. 5.
Opportunities to change decision regarding COVID-19 vaccination among COVID-19 vaccine hesitant and resistant groups (n = 134)
Among participants, 179 (39.3%) had received COVID-19 vaccine. Astrzeneca (53.1%) and Sinopharm (20.7%) were the two most frequently received vaccines. The two most frequently reported vaccination adverse effects were fever (45.3%) and body aches (55.3%). However, as demonstrated in Table 5, the least common side effects were rash (3.4%) and anaphylaxis (1.1%).
Table 5.
List of types and adverse effects of COVID-19 vaccines in the study health care workers who have received COVID-19 vaccine (n = 179,39.3%)
| Variables | Vaccinated HCW (n = 179) n (%) |
|---|---|
| Type of COVID-19 vaccine received | |
| Astrazeneca | 95 (53.1) |
| Sinopharm | 37 (20.7) |
| Sinovac | 28 (15.6) |
| Pfizer | 14 (7.8) |
| Sputnik | 4 (2.2) |
| Johnson & Johnson’s Janssen Covid-19 Vaccine | 1 (0.6) |
| Adverse effects of COVID-19 vaccines | |
| Widespread muscle/joint pain | 99 (55.3) |
| Fever or chills | 81 (45.3) |
| Headache | 77 (43) |
| Local skin reaction | 66 (36.9) |
| Fatigue or sleepiness | 49 (27.4) |
| Chest pain – palpitations | 21 (11.7) |
| Nausea | 14 (7.8) |
| Poor appetite | 13 (7.3) |
| Vomiting | 8 (4.5) |
| Rash | 6 (3.4) |
| Anaphylaxis | 2 (1.1) |
Discussion
The COVID-19 vaccination is one of the most crucial strategies for containing the COVID-19 pandemic. HCWs are more likely to contract COVID-19 than the general population. So, their attitude toward the vaccination is crucial since it can determine how well the general population responds to it [19].
The aim of this study was to assess Egyptian HCWs’ attitudes toward the COVID-19 vaccine. The 455 HCWs who participated in this study were divided into three groups—VA, VH, and VR—based on their attitude toward COVID-19 vaccine. Most of participants were vaccine accepting (70.5%). Of the participants, one-third had previously contracted COVID-19, and the majority of them had prolonged disease course. The majority of participants believed that they were at high risk for both SARS-CoV-2 infection and vaccination side effects. There was a statistically significant difference between the VA, VH, and VR groups regarding perception and knowledge of conventional and COVID-19 vaccines. Fear of infection and the desire to resume normal life were the main drivers behind the COVID-19 vaccination. The two major barriers, however, were waiting for additional expertise and having doubts about the effectiveness of the vaccines.
About one third (33.4%) of participants reported having previously contracted COVID-19, a rate that was comparable to that in a prior study also involving Egyptian HCWs [20]. Other studies done in nations with higher incomes found a much lower percentage of SARS-CoV-2 infection [21, 22]. In a different study on the general population, the percentage of people with a history of prior SARS-CoV-2 infection was around 20%, and there was no difference in this percentage between those in the medical and non-medical fields [23].
Most participants in this study were vaccine accepting (70.5%). This high rate of vaccine acceptance was comparable to the findings of earlier studies conducted on family physicians [24], primary care physicians [25], pediatricians [26], pharmacists [27], dentists [28], medical students [29] and HCWs [30, 31]. Additionally, a recent meta-analysis of ten studies on dental practitioners and students indicated that vaccine acceptability was higher in middle eastern nations [32].
The majority of individuals in other studies, however, were shown to be hesitant to receive COVID-19 vaccine [33, 34]. In a global study that was conducted in 12 countries, the majority of participants were in favor of vaccinations; nevertheless, Egypt and African nations had the lowest vaccination acceptance rates. Higher income countries showed greater vaccine adoption in the same study [35]. In another survey of nurses and midwives, the VR group was found to have the highest percentage (more than 90%), with participants worried about the vaccine’s side effects and how rapidly development occurred [36]. Notably, vaccine acceptance in recent surveys was higher than earlier one. This may be ascribed to more recent and available studies, public vaccination campaigns, and political motivations.
Participants from urban areas were more vaccine accepting and these results were consistent with the finding reported by Biswas et al., in which, HCWs working at urban areas, were more vaccine accepting [37]. Rural communities may have limited access to health care services, which may contribute to the gap in vaccine acceptance. As a result, specific initiatives are required to boost vaccine confidence and bridge the gap between urban and rural communities. Public health practitioners could focus on engaging with community-based organisations to increase vaccine confidence, guarantee equitable vaccine access, and urge rural residents to stay up to date on necessary COVID-19 vaccines.
There was no difference as regard age, gender or working with COVID-19 patients in our cohort. In previous studies, it was observed that males and physicians were more accepting of vaccinations than females and nurses [22, 38, 39]. Because of this, physicians play a significant part in increasing public acceptability of the COVID-19 vaccine.
Previous exposure to SARS-CoV-2 infection is associated with higher vaccine acceptance [40]. However, there was no difference between VA, VH, VR groups in this study with relation to prior or family history of SARS-CoV-2 infection.
More acceptance of the vaccine was linked to stronger awareness of the COVID-19 vaccine and higher knowledge scores [34]. In the present study, there was a significant difference between the 3 groups as regard perception towards conventional and COVID-19 vaccination and knowledge score. These results were in line with previous studies, which showed a substantial difference between the VR, VH, and VA groups in terms of attitudes toward vaccination and perceptions of the safety of the COVID-19 vaccine [33, 41].
Physicians were reported to be the primary source of information in about half of our participants (49%) followed by social media for young participants (< 45 years) and television for others (≥45 years). It was found that higher education HCWs rely mainly on institutional sources and scientific literature. However, lower education HCWs rely on internet, mass media and opinions of family and friends [39]. Social and mass media are important sources of information [42]. However, using social media as a source of information is associated with more vaccine hesitancy [43], while using national websites is associated with less hesitancy [33].
In this study, fear of infection, being at high risk of infection, and the desire to resume normal life were the main drivers for COVID-19 vaccination in the VA group. Similar causes were reported by previous studies conducted on family physicians and other HCWs [24, 30].
Concerns about safety and efficacy are also important barriers against vaccination [19, 29]. In this study, the major barriers to the COVID-19 vaccination in the VR group were waiting for additional experience with these new vaccines and having doubts about the vaccines’ efficacy. It was previously reported that the biggest obstacles to vaccination acceptability were the quick creation of the vaccine and a lack of adequate information [42, 44]. Additionally, a lack of clinical trials and concern about side effects are the main reasons why people are hesitant to obtain the vaccination. Providing this group with adequate factual information will boost their acceptance of the vaccine [20].
Among participants, 179 (39.3%) had received COVID-19 vaccine. In certain studies, a lower vaccination rate was noted [19]. However, some research indicated a far greater rate [45, 46]. Astrzeneca (53.1%) and Sinopharm (20.7%) were the two most frequently received vaccines in our cohort. This was according to which was available for each participant. In general, m RNA vaccines are the most preferred vaccines [46]. Additionally, Pfizer and Astrazeneka vaccines are the most popular vaccination types in Arabic-speaking and African countries [47, 48].
Furthermore, there was a disparity between vaccination acceptants (70%) and vaccine recipients (40%) among our cohort. This is due to a limited supply of COVID-19 vaccine at the time of the trial, and the government devised a policy for the sequential inclusion of high priority groups, including HCWs. As a result, all HCWs who accepted to vaccination received it in sequence.
In conclusion, our results emphasize the value of including HCWs in pandemic vaccination campaigns. HCWs were very accepting of COVID-19 vaccines and played a crucial role in assisting patients in their vaccine decisions despite having expressed vaccine concerns. The community adopts these perceptions because of exposure to false information, which is magnified by the media. Recognizing and addressing issues at all levels is essential for increasing the reach of COVID-19 vaccination campaigns. We recommend that this study be replicated using a qualitative research approach to bridge the gap identified between practice and attitude. This study has many strengths. First, we performed a multicenter study including HCWs with various levels of education and employment experiences. Second, this study sheds essential light on the potential obstacles to and drivers behind vaccination among HCWs who are an important source of human resources in vaccination. Third, this study offers important information regarding the actual conversion of vaccine acceptance into vaccine uptake as well as adverse reactions following vaccination.
However, the study has several limitations. First, because the study was cross-sectional, it was challenging to evaluate the causes and effect relationships. Second, we employed convenience sampling, which could have biased the results; those who were accepting the COVID-19 vaccine may be more likely to participate in the survey and this could explain the difference in the results with other studies that reported less acceptance, and a different preference concerning sex. Third, some sites collected data before vaccination began, while others did so after it had begun, which may have an impact on HCWs’ attitudes. Hence, as more information about the safety and efficacy of COVID-19 vaccines becomes available, individuals may have different attitudes towards vaccination.
Acknowledgements
The following collaborators are acknowledged by the authors for their contributions to data collection: Shimaa Mohamed Mohamed Saad (Kafr El Sheikh Faculty of Physical Therapy), Noor Abd Elghani Elsaeed Zayed (Mansoura Faculty of Medicine) and Nada Mohammed Mohammed Abo Musallam (Mansoura Faculty of Medicine).
Abbreviations
- CAPMAS
Central Agency for Public Mobilization and Statistics
- COVID-19
Coronavirus disease 2019
- HCWs
Healthcare workers
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- SPSS
Statistical Package for Social Science
- WHO
World Health Organization
Authors’ contributions
Conceptualization: ST, DKN, MKN, AMS, FH, Investigation: all authors, Data curation, formal analysis: ST, DKN, writing–original draft: MKN, AMS, FH, writing–review & editing: All authors. The authors read and approved the final manuscript.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). This study did not receive any funding.
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The work complies with the ethical standards of the 1995 Helsinki declaration and was approved by Institutional review board of Mansoura university (Approval No: R.21.08.1398.R1). All participants received comprehensive information regarding the study, and their written informed consent was obtained.
Consent for publication
Not applicable.
Competing interests
All authors have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Samar Tharwat, Email: samartharwat2000@mans.edu.eg.
Dalia Kamal Nassar, Email: dalianasser@mans.edu.eg.
Mohammed Kamal Nassar, Email: m_kamal@mans.edu.eg.
Ahmed Mohammed Saad, Email: ahmedsaaaad39@gmail.com.
Fatma Hamdy, Email: fatmahamdyfh88@mans.edu.eg.
References
- 1.Acter T, Uddin N, Das J, Akhter A, Choudhury TR, Kim S. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: A global health emergency. Sci Total Environ. 2020;730:138996. doi: 10.1016/j.scitotenv.2020.138996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coronavirus disease 2019 (COVID-19): situation report, 106. [cited 2022 Jun 24]. Available from: https://apps.who.int/iris/handle/10665/332060
- 3.Nicola M, Alsafi Z, Sohrabi C, … AKI journal of, 2020 undefined. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Elsevier. [cited 2022 Jun 24]; Available from: https://www.sciencedirect.com/science/article/pii/S1743919120303162 [DOI] [PMC free article] [PubMed]
- 4.Orensteina WA, Ahmedb R. Simply put: Vaccination saves lives. Proc Natl Acad Sci U S A. 2017;114(16):4031–4033. doi: 10.1073/pnas.1704507114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Id AJ, Mohan K, Id S, Kaur M, Bhatt A, Nash D, et al. A cross sectional study to examine factors influencing COVID-19 vaccine acceptance, hesitancy and refusal in urban and rural settings in Tamil Nadu, India. PLoS One. 2022;17(6):e0269299. doi: 10.1371/journal.pone.0269299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tatar M, Faraji MR, Montazeri Shoorekchali J, Pagán JA, Wilson FA. The role of good governance in the race for global vaccination during the COVID-19 pandemic. Sci Rep. 2021;11(1):1–7. doi: 10.1038/s41598-021-01831-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haque A, Pant AB. Efforts at COVID-19 Vaccine Development: Challenges and Successes. Vaccines. 2020;8:739. doi: 10.3390/vaccines8040739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacDonald NE, Eskola J, Liang X, Chaudhuri M, Dube E, Gellin B, et al. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 9.Puertas EB, Velandia-Gonzalez M, Vulanovic L, Bayley L, Broome K, Ortiz C, et al. Concerns, attitudes, and intended practices of Caribbean healthcare workers concerning COVID-19 vaccination: A cross-sectional study. Lancet Regional Health Americas. 2022;9:100193. doi: 10.1016/j.lana.2022.100193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Organization WH . WHO SAGE values framework for the allocation and prioritization of COVID-19 vaccination, 14 September 2020. 2020. [Google Scholar]
- 11.Karafillakis E, Dinca I, Apfel F, Cecconi S, Vaccine AW. Vaccine hesitancy among healthcare workers in Europe: A qualitative study. Elsevier; 2016. [DOI] [PubMed] [Google Scholar]
- 12.Egypt Statistical Yearbook 2020 - Health | Arab Development Portal [Internet]. [cited 2022 Jun 25]. Available from: https://www.arabdevelopmentportal.com/publication/egypt-statistical-yearbook-2020-health
- 13.Id AJ, Mohan K, Id S, Kaur M, Bhatt A, Nash D, et al. A cross sectional study to examine factors influencing COVID-19 vaccine acceptance, hesitancy and refusal in urban and rural settings in Tamil Nadu, India. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes Toward a Potential SARS-CoV-2 Vaccine : A Survey of U.S. Adults. Ann Intern Med. 2020;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front Public Health. 2020;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tavolacci MP, Dechelotte P, Ladner J. Covid-19 vaccine acceptance, hesitancy, and resistancy among university students in france. Vaccines (Basel). 2021;9(6) [cited 2022 Jun 24]. Available from: /pmc/articles/PMC8232624/. [DOI] [PMC free article] [PubMed]
- 18.Bari MS, Hossain MJ, Ahmmed F, Sarker MMR, Khandokar L, Chaithy AP, et al. Knowledge, Perception, and Willingness towards Immunization among Bangladeshi Population during COVID-19 Vaccine Rolling Period. Vaccines (Basel). 2021;9(12) [cited 2022 Jun 24]. Available from: https://pubmed.ncbi.nlm.nih.gov/34960195/. [DOI] [PMC free article] [PubMed]
- 19.Shehata WM, Elshora AA, Abu-Elenin MM. Physicians’ attitudes and acceptance regarding COVID-19 vaccines: a cross-sectional study in mid Delta region of Egypt. Environ Sci Pollut Res. 2022;29(11):15838–15848. doi: 10.1007/s11356-021-16574-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fares S, Elmnyer MM, Mohamed SS, Elsayed R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. J Prim Care Community Health. 2021;12:1–9. doi: 10.1177/21501327211013303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Parente DJ, Ojo A, Gurley T, Le Master JW, Meyer M, Wild DM, et al. Acceptance of COVID-19 Vaccination among Health System Personnel. J Am Board Fam Med. 2021;34(3):498–522. doi: 10.3122/jabfm.2021.03.200541. [DOI] [PubMed] [Google Scholar]
- 22.Hatice İ, Sezerol MA, Ta Y, Maral I. 19 vaccine hesitancy and related factors among primary healthcare workers in a district of Istanbul: a cross- sectional study from Turkey. 2022. pp. 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aloweidi A, Bsisu I, Suleiman A, Abu-Halaweh S, Almustafa M, Aqel M, et al. Hesitancy towards covid-19 vaccines: An analytical cross–sectional study. Int J Environ Res Public Health. 2021;18(10):1–12. doi: 10.3390/ijerph18105111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ofei-Dodoo S, Kellerman R, Russell T. Family physicians’ perception of the new mrna covid-19 vaccines. J Am Board Fam Med. 2021;34(5):898–906. doi: 10.3122/jabfm.2021.05.210052. [DOI] [PubMed] [Google Scholar]
- 25.Day P, Strenth C, Kale N, Schneider FD, Arnold EM. Perspectives of primary care physicians on acceptance and barriers to COVID-19 vaccination. Fam Med Comm Health. 2021;9(4):1–7. doi: 10.1136/fmch-2021-001228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gönüllü E, Soysal A, Atıcı S, Engin M, Yeşilbaş O, Kasap T, et al. Pediatricians’ COVID-19 experiences and views on the willingness to receive COVID-19 vaccines: a cross-sectional survey in Turkey. Hum Vaccin Immunother. 2021;17(8):2389–2396. doi: 10.1080/21645515.2021.1896319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Okuyan B, Bektay MY, Demirci MY, Ay P, Sancar M. Factors associated with Turkish pharmacists’ intention to receive COVID-19 vaccine: an observational study. Int J Clin Pharm. 2022;44(1):247–255. doi: 10.1007/s11096-021-01344-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nasr L, Saleh N, Hleyhel M, El-Outa A, Noujeim Z. Acceptance of COVID-19 vaccination and its determinants among Lebanese dentists: a cross-sectional study. BMC Oral Health. 2021;21(1):1–10. doi: 10.1186/s12903-021-01831-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Le CN, Nguyen UTT, Do DTH. Predictors of COVID-19 vaccine acceptability among health professions students in Vietnam. BMC Public Health. 2022;22(1):854. doi: 10.1186/s12889-022-13236-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koh SWC, Liow Y, Loh VWK, Liew SJ, Chan YH, Young D. COVID-19 vaccine acceptance and hesitancy among primary healthcare workers in Singapore. BMC Primary Care. 2022;23(1):1–9. doi: 10.1186/s12875-022-01693-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Youssef D, Abou-Abbas L, Berry A, Youssef J, Hassan H. Determinants of acceptance of Coronavirus disease-2019 (COVID-19) vaccine among Lebanese health care workers using health belief model. PLoS One. 2022;17(2 Febuary):1–17. doi: 10.1371/journal.pone.0264128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin GSS, Lee HY, Leong JZ, Sulaiman MM, Loo WF, Tan WW. COVID-19 vaccination acceptance among dental students and dental practitioners: A systematic review and meta-analysis. PLoS One. 2022;17(4):e0267354. doi: 10.1371/journal.pone.0267354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zammit N, Gueder AE, Brahem A, Ayouni I, Ghammam R, Fredj SB, et al. Studying SARS-CoV-2 vaccine hesitancy among health professionals in Tunisia. BMC Health Serv Res. 2022;22(1):1–14. doi: 10.1186/s12913-022-07803-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Velikonja NK, Velikonja VG, Verdenik I, Jurišić I, Stanisavljević S, Dobrowolska B, et al. Vaccination intention among healthcare workers during the first wave of the coronavirus disease 2019 pandemic in relation to knowledge: a cross-sectional study in Croatia, Slovenia, Serbia, and Poland. Croatian Med J. 2022;63(1):79–88. doi: 10.3325/cmj.2022.63.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Noushad M, Rastam S, Nassani MZ, Al-Saqqaf IS, Hussain M, Yaroko AA, et al. A Global Survey of COVID-19 Vaccine Acceptance Among Healthcare Workers. Front Public Health. 2022;9(February):1–12. doi: 10.3389/fpubh.2021.794673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fakonti G, Kyprianidou M, Toumbis G, Giannakou K. Attitudes and Acceptance of COVID-19 Vaccination Among Nurses and Midwives in Cyprus: A Cross-Sectional Survey. Front Public Health. 2021;9(June):1–10. doi: 10.3389/fpubh.2021.656138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Biswas N, Mustapha T, Khubchandani J, Price JH. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J Community Health. 2021;46(6):1244–1251. doi: 10.1007/s10900-021-00984-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khamis F, Badahdah A, Al Mahyijari N, Al Lawati F, Al Noamani J, Al Salmi I, et al. Attitudes Towards COVID-19 Vaccine: A Survey of Health Care Workers in Oman. J Epidemiol Global Health. 2022;12(1):1–6. doi: 10.1007/s44197-021-00018-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Papini F, Mazzilli S, Paganini D, Rago L, Arzilli G, Pan A, et al. Healthcare Workers Attitudes, Practices and Sources of Information for COVID-19 Vaccination: An Italian National Survey. Int J Environ Res Public Health. 2022;19(2):1–13. doi: 10.3390/ijerph19020733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Malik A, Malik J, Ishaq U. Acceptance of COVID-19 vaccine in Pakistan among health care workers. PLoS One. 2021;16(9 September):1–11. doi: 10.1371/journal.pone.0257237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.El-Sokkary RH, El Seifi OS, Hassan HM, Mortada EM, Hashem MK, Gadelrab MRMA, et al. Predictors of COVID-19 vaccine hesitancy among Egyptian healthcare workers: a cross-sectional study. BMC Infect Dis. 2021;21(1):1–9. doi: 10.1186/s12879-021-06392-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Berry SD, Johnson KS, Myles L, Herndon L, Montoya A, Fashaw S, et al. Lessons learned from frontline skilled nursing facility staff regarding COVID-19 vaccine hesitancy. J Am Geriatr Soc. 2021;69(5):1140–1146. doi: 10.1111/jgs.17136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Di Gennaro F, Murri R, Segala FV, Cerruti L, Abdulle A, Saracino A, et al. Attitudes towards anti-sars-cov2 vaccination among healthcare workers: Results from a national survey in Italy. Viruses. 2021;13(3):1–11. doi: 10.3390/v13030371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bauernfeind S, Hitzenbichler F, Huppertz G, Zeman F, Koller M, Schmidt B, et al. Brief report: attitudes towards Covid-19 vaccination among hospital employees in a tertiary care university hospital in Germany in December 2020. Infection. 2021;49(6):1307–1311. doi: 10.1007/s15010-021-01622-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peirolo A, Posfay-Barbe KM, Rohner D, Wagner N, Blanchard-Rohner G. Acceptability of COVID-19 Vaccine Among Hospital Employees in the Department of Paediatrics, Gynaecology and Obstetrics in the University Hospitals of Geneva, Switzerland. Front Public Health. 2022;9(January):1–10. doi: 10.3389/fpubh.2021.781562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kozak A, Nienhaus A. COVID-19 vaccination: Status and willingness to be vaccinated among employees in health and welfare care in germany. Int J Environ Res Public Health. 2021;18(13):6688. doi: 10.3390/ijerph18136688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yassin EOM, Faroug HAA, Ishaq ZBY, Mustafa MMA, Idris MMA, Widatallah SEK, et al. COVID-19 Vaccination Acceptance among Healthcare Staff in Sudan, 2021. J Immunol Res. 2022;2022:3392667. doi: 10.1155/2022/3392667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saddik B, Al-Bluwi N, Shukla A, Barqawi H, Alsayed HAH, Sharif-Askari NS, et al. Determinants of healthcare workers perceptions, acceptance and choice of COVID-19 vaccines: a cross-sectional study from the United Arab Emirates. Hum Vaccin Immunother. 2022;18(1):1–9. doi: 10.1080/21645515.2021.1994300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.