Abstract
Repeated infections with Neisseria gonorrhoeae are common among patients attending sexually transmitted disease clinics. We examined whether previous infections or site of infection altered the local and systemic antigonococcal antibody levels in males and females. Antibodies against N. gonorrhoeae MS11 and the patients’ homologous infecting isolates were measured by enzyme-linked immunosorbent assay. In general, the local and systemic immune responses to gonococci were extremely modest. There was a slight increase in serum immunoglobulin G (IgG) against the MS11 strain and the homologous isolates in infected males. Levels of serum IgA1 antibodies against MS11 were slightly higher in infected than in uninfected females. A history of previous infections with N. gonorrhoeae did not alter the antibody levels in patients with a current infection, suggesting that immunological memory is not induced by uncomplicated gonococcal infections. Antibody responses to infected subjects’ homologous isolates were observed in cervical mucus; IgA1 levels increased while IgG levels decreased. The decline in mucosal IgG against the homologous isolates was less common in subjects having both rectal and cervical infections; otherwise, no effect of rectal involvement was observed. The absence of substantially higher antibody levels to gonococci where there is infection at a site known to contain organized lymphoid tissue suggests that the low levels of responses to uncomplicated infections may not be due simply to an absence of inductive sites in the genital tract. We propose that in addition to its potential ability to avoid the effects of an immune response, N. gonorrhoeae does not elicit strong humoral immune responses during uncomplicated genital infections.
Neisseria gonorrhoeae is an exclusively human pathogen transmitted most often by sexual contact. For the majority of patients, antibiotic treatment is effective and there are few long-term sequelae. In some women, however, N. gonorrhoeae may infect the upper genital tract and cause pelvic inflammatory disease with serious consequences including sterility. The risk of complicated infection may increase in the future as the number of antibiotic-resistant strains of N. gonorrhoeae also increases (15). Another consequence of gonococcal infection is its potential to enhance the risk of acquiring other sexually transmitted diseases (STD), including human immunodeficiency virus infection (1, 22, 35). These important health concerns have sparked continuing interest into the development of vaccines against gonorrhea as well as other STD.
Several prototype gonococcal vaccines have shown limited or no protection against reinfection with N. gonorrhoeae despite the generation of serum antibody responses against the vaccine antigens (3, 24, 47). The results from vaccine trials parallel observations regarding natural gonococcal infections, where local and systemic antibodies have been detected by immunofluorescence in secretions and serum from infected patients, yet there is a high rate of recidivism of gonococcal infections among patients attending STD clinics (19, 25, 26, 34, 44, 46). Some evidence of partial serovar-specific immunity has been reported among sex workers (37). The high rate of reinfection despite the presence of antigonococcal antibodies leads to the assumption that N. gonorrhoeae evades the host’s immune response. Indeed, N. gonorrhoeae possess several mechanisms which could potentially thwart the effects of immune responses directed toward this organism in vivo, including hypervariation of surface antigens (29), resistance to complement-mediated bacteriolysis (39, 42), and the production of immunoglobulin A1 (IgA1) protease (36).
Recent quantitative enzyme-linked immunosorbent assay (ELISA) measurements of the levels of antigonococcal antibodies indicated that while such antibodies could be detected in serum and secretions from infected patients, their levels were unexpectedly low (14). These results suggested that the levels of antigonococcal antibodies generated during natural infections may not be adequate to provide protection against reinfection and that this might explain the lack of immunity to N. gonorrhoeae. It is known that repeated exposure to an antigen or organism enhances immune responses by evoking memory within the immune system. This study was therefore designed to examine whether a history of gonococcal infection elicits greater antibody responses in patients with uncomplicated gonorrhea and whether infection of the rectum, which contains organized lymphoid follicles (32, 33) and may serve as an inductive site for local and genital tract antibody responses (5, 18, 21), results in significantly greater mucosal immune responses, particularly as manifested in the genital tract.
MATERIALS AND METHODS
Patients.
Male and female patients attending the Jefferson County Department of Health STD clinic (Birmingham, Ala.) were recruited into the study, and informed consent was obtained from each patient prior to enrollment. Patients attending the clinic, but not infected with N. gonorrhoeae, were enrolled as controls. Presumption of infection and treatment were based on clinical criteria, including Gram-stained smears, and infection was confirmed by routine culture methods (see below). Clinical data and history, including age, onset of menses, known previous STD, and concurrent infections with Chlamydia trachomatis and Trichomonas vaginalis (Table 1), were recorded for each patient. Where possible, samples of cervical mucus, vaginal wash, and blood were obtained from the patients during each of three visits to the STD clinic at approximately 2-week intervals following the initial visit; however, not all specimens were obtained from every patient. All diagnosed patients were given appropriate antibiotic treatment during the first visit and were retested for infection at subsequent visits; no patient remained infected after treatment.
TABLE 1.
Distribution of current and previous STD and other variables in participating patients
| Sex | Current infection | n | No. of patients
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Menses | Site of current N. gonorrhoeae infection
|
Previous STD exposurea
|
||||||||
| Cervix | Rectum and cervix | Urethra | None | Ngo | Ctr | Tva | ||||
| Female | ||||||||||
| None | 18 | 2 | 3 | 9 | 2 | 4 | ||||
| N. gonorrhoeae | 12 | 5 | 7 | 5 | 2 | 5 | 2 | 3 | ||
| T. vaginalis and C. trachomatis | 13 | 3 | 0 | 5 | 5 | 3 | ||||
| N. gonorrhoeae, T. vaginalis, and C. trachomatis | 8 | 1 | 4 | 4 | 0 | 4 | 3 | 1 | ||
| Male | ||||||||||
| None | 11 | 7 | 4 | |||||||
| N. gonorrhoeae | 58 | 58 | 27 | 31 | ||||||
Patients were asked to provide a history of STD infections at the time of treatment; clinical confirmation of their responses was not possible. Ngo, N. gonorrhoeae; Ctr, C. trachomatis; Tva, T. vaginalis.
Sample collection and handling.
Cervical mucus (∼0.05 to 0.5 ml) was mechanically collected by using a sterile swab and dispersed in an approximately equal volume of sterile phosphate-buffered saline (PBS) containing a 2× protease inhibitor cocktail (10 mM EGTA, 150 mM NaN3, 0.01% [wt/vol] leupeptin [Sigma Chemical Co., St. Louis, Mo.], 0.02 M Pefabloc [Boehringer Mannheim, Indianapolis, Ind.]). The suspended mucus was treated with Nonidet P-40 (NP-40; 10 μl/ml; Sigma) and then diluted 1:5 or up to 2 ml with PBS, vortexed, stored overnight at 4°C, and finally centrifuged at 2,000 rpm for 10 min at 4°C. The preparations were then aliquoted and stored at −70°C.
Vaginal wash specimens were collected by instilling 10 ml of PBS and recovering approximately 8 ml by aspiration; 0.1 volume of the above-described protease inhibitor cocktail at 10× concentration was then added. The wash was centrifuged at 2,000 rpm for 10 min at 4°C, and the supernatant was treated with NP-40, aliquoted, and stored at −70°C.
Peripheral venous blood was collected in a Vacutainer tube and allowed to clot, and the serum was recovered by centrifugation. NP-40 was added as described above, and aliquots were stored at −70°C.
Urethral swab specimens were collected from males by using Dacron-tipped nasopharyngeal swabs with stainless-steel shafts. Swabs were inserted 1.5 cm into the urethra and then placed directly into PBS–2× protease inhibitor and processed as described above. Urethral swabs for antibody determination were collected before other urethral specimens.
Bacteria.
N. gonorrhoeae was isolated from infected patients by swab culture on modified Thayer-Martin medium and identified by conventional microbiological criteria. Following initial culture, gonococcal isolates from participants were subcultured on chocolate agar and maintained frozen at −70°C until required. N. gonorrhoeae MS11 was obtained from Mogens Kilian (University of Århus, Århus, Denmark) and maintained frozen in liquid nitrogen.
Antigen preparation.
For antigen preparation, MS11 and homologous gonococcal isolates were taken from frozen stocks and cultured on chocolate agar plates (Becton Dickinson, Cockeysville, Md.) at 37°C in a 5% CO2–air atmosphere. Gonococci were scraped from confluent plate cultures, resuspended in 1 ml of PBS/plate, and fixed with 0.5% formaldehyde at 4°C overnight. The optical density of each culture was measured at a wavelength of 590 nm, and the bacterial concentration was estimated by comparison to a previously determined standard ratio of bacterial cell concentration and optical density at 590 nm; 100-μl aliquots of gonococci at 1010 CFU/ml were subsequently frozen at −70°C until use. One confluent plate culture of each homologous isolate and 20 confluent plate cultures of MS11 provided sufficient bacteria for all antibody analyses presented here.
Ig and antibody assays.
Cervical mucus, vaginal wash, and serum samples were assayed for concentrations of total IgA1, IgA2, IgG, and IgM by ELISA. Primary antibody or antigen coating for all assays was carried out in PBS. Prevention of nonspecific Ig binding was accomplished by blocking all assays with PBS-Tween (PBS containing 0.15% Tween 20 [Sigma]) for 4 h. All washes and subsequent sample or antibody additions were carried out in the presence of PBS-Tween. To measure total IgG and IgM, plates were coated with anti-human IgG or IgM (Dako Corp., Carpinteria, Calif.) and then duplicate serial dilutions of sample were incubated overnight. Bound Igs were detected with peroxidase-conjugated anti-human IgG or IgM (Dako) for 4 h. For IgA1 and IgA2 measurement, plates were initially coated with human-absorbed goat anti-mouse IgG (Southern Biotechnology Associates, Birmingham, Ala.) followed by overnight incubation with either anti-human IgA1 (Sigma) or anti-human IgA2 (Recognition Sciences Ltd., Birmingham, England) at appropriate concentrations. Duplicate serial dilutions of sample were incubated overnight. Bound Igs were detected with peroxidase-conjugated goat anti-human IgA (Jackson ImmunoResearch Laboratories Inc., West Grove, Pa.) incubated for 4 h.
The levels of IgA1, IgA2, IgM, and IgG antibodies to N. gonorrhoeae MS11, as well as each patient’s own infecting isolate (where possible), were estimated in the same samples. Whole, formaldehyde-treated, N. gonorrhoeae cells were used to coat plates at a concentration of 5 × 106 CFU/well, followed by duplicate serial dilutions of sample incubated overnight. Bound IgG or IgM antibodies were detected with peroxidase-conjugated anti-human IgG or IgM (Dako) for 4 h. Bound IgA1 or IgA2 was detected by incubation with either anti-human IgA1 or IgA2 followed by incubation with peroxidase-conjugated anti-mouse IgG (Southern Biotechnology Associates) for 4 h. For all assays, color development used a substrate consisting of o-phenylenediamine and H2O2 in citrate-phosphate buffer (pH 4.0); development was stopped with sulfuric acid after 15 min, and absorbance was read at 490 nm in a Vmax microplate reader (Molecular Devices Corp., Menlo Park, Calif.) interfaced to a Macintosh computer for data retrieval. Standard curves were determined for each plate and type of assay from serial dilutions of human Ig calibrator at appropriate concentrations (The Binding Site Ltd., Birmingham, England). Unknowns were interpolated on standard curves generated by a computer program with four-parameter logistic algorithms (40), and parallelism between unknown and standard dilution curves was demonstrated over the range of unknown dilutions used for calculation.
Antibody levels in secretions of each isotype were normalized to compensate for sample-to-sample variations in antibody secretion and dilution by comparison to the concentration of total corresponding Ig isotype in that sample. For each isotype and sample, the antibody level as a percentage of total Ig was calculated as [antibody] (ng/ml)/[Ig] (ng/ml) × 100.
Statistics.
Statistical tests were performed with the Instat statistics program for Macintosh computers. The Kruskal-Wallis test was used for comparisons of more than two statistical groups. Wilcoxon signed-rank test, Mann-Whitney U test, Spearman’s correlation, and Fisher’s exact test were used as appropriate. Differences between groups or visits where P was <0.05 were considered significant.
RESULTS
Total Ig concentrations in female genital tract secretions in relation to gonococcal and other genital tract infections.
It is not clear whether total Ig levels in female genital secretions are affected by the presence of concomitant STD. Some previous reports have shown higher Ig levels in the genital tract during infections with organisms causing STD (4), while others have not (9, 48). Therefore, we measured the concentrations of total IgA1, IgA2, IgG, and IgM in cervical mucus, vaginal wash, and serum samples from volunteers without demonstrable infection, from volunteers in whom only N. gonorrhoeae was detected, and from volunteers infected with other pathogens (C. trachomatis or T. vaginalis) with or without N. gonorrhoeae.
The concentrations of total Ig isotypes in local secretions from noninfected female patients (Table 2) were similar to those found in recently published studies (2, 16). There were no differences between the concentrations of total IgA1, IgA2, IgG, and IgM in genital tract secretions in patients with different STD compared with noninfected women. High levels of IgG were detected in a few but not all cervical mucus and vaginal wash samples obtained during menses, but this applied equally to noninfected and infected groups and did not significantly bias the comparison between groups. There was no significant correlation between the concentrations of each Ig isotype in serum and secretions or between the concentrations of different isotypes within each type of sample.
TABLE 2.
Total Ig levels in female genital tract secretions from noninfected subjects and patients with STD
| Sample | Ig isotype | Median Ig level (μg/ml) (range) [n])
|
|||
|---|---|---|---|---|---|
| No current infection | Current infection witha:
|
||||
| Tva and/or Ctr | Ngo | Ngo, Tva, and/or Ctr | |||
| Cervical mucus | IgA1 | 46 (1–227 [18]) | 67 (5–1,150 [13]) | 68 (10–630 [10]) | 33 (1–129 [7]) |
| IgA2 | 30 (2–140 [17]) | 37 (2–356 [12]) | 13 (0–196) [8]) | 14 (1–67 [7]) | |
| IgG | 128 (2–2,732 [18]) | 162 (20–950 [13]) | 116 (5–1,353 [11]) | 177 (38–1,891 [7]) | |
| IgM | 17 (1–111 [17]) | 26 (0–1,080 [13]) | 60 (8–116 [9]) | 13 (3–51 [8]) | |
| Vaginal wash | IgA1 | 4.9 (0.2–70.0 [17]) | 1.8 (0.1–20.7 [13]) | 4.6 (0.6–39.4 [10]) | 8.6 (1.1–35.8 [8]) |
| IgA2 | 4.2 (0.2–44.6 [17]) | 2.7 (0.0–28.5 [13]) | 3.1 (0.0–11.4 [10]) | 2.0 (0.0–19.9 [8]) | |
| IgG | 18.3 (1.0–218.9 [17]) | 25.3 (0.7–57.6 [13]) | 12.3 (3.1–72.2 [12]) | 11.3 (4.2–171.7 [8]) | |
| IgM | 0.6 (0.0–13.7 [10]) | 0.5 (0.0–3.7 [9]) | 1.9 (0.1–2.6 [3]) | 0.6 (0.1–0.8 [3]) | |
Ctr, C. trachomatis; Tva, T. vaginalis; Ngo, N. gonorrhoeae.
Antibody responses to N. gonorrhoeae MS11.
We chose to examine the antibody levels to fixed whole bacteria instead of attempting to follow responses to a single (variable) antigen. We first assayed the levels of IgA1, IgA2, IgG, and IgM antibodies specific for N. gonorrhoeae MS11 (a widely studied gonococcal strain) in female mucosal secretions and serum, in order to compare the levels of antigonococcal antibodies in gonococcus-infected and noninfected patients.
Antibodies that recognize N. gonorrhoeae MS11 were found at low levels in local secretions and sera from female patients, both infected and noninfected (Table 3). To compensate for sample-to-sample variations in antibody secretion and dilution, all statistical analyses of antibody levels in cervical mucus and vaginal wash samples were performed relative to the concentration of total corresponding Ig isotype. IgA1 antibody levels in serum, but not in secretions, were higher in female patients infected with N. gonorrhoeae than in noninfected patients at both visit 1 (P = 0.0015) and visit 2 (P = 0.0054). IgA2 antibodies to N. gonorrhoeae MS11 were detected in one cervical mucus sample and in no vaginal wash samples. IgA2 antibodies were detected in sera from some noninfected (3 positive/30 visit 1 samples) and infected (5 positive/19 visit 1 samples) female patients. The levels of IgG and IgM antibodies in serum and secretions were not different between gonococcus-infected and noninfected patients. There were no significant correlations between the levels of systemic and local antibody for any antibody isotype in females or between the concentrations of different antibody isotypes within each type of sample.
TABLE 3.
Antibody levels to N. gonorrhoeae MS11 in serum and genital secretions from noninfected and infected female patients
| Sample | Median antibody level (ng/ml) (range)
|
|||
|---|---|---|---|---|
| Visit 1
|
Visit 2
|
|||
| Noninfected (n = 30) | N. gonorrhoeae infected (n = 17) | Noninfected (n = 15) | N. gonorrhoeae infected (n = 13) | |
| Cervical mucus | ||||
| IgA1 | 0 (0–196) | 0 (0–326) | 0 (0–174) | 0 (0–119) |
| IgA2 | 0 (0–27)a | 0 (0–0) | 0 (0–0) | 0 (0–0) |
| IgG | 850 (0–12,034) | 1,188 (0–15,600) | 556 (0–7,895) | 1,000 (0–9,810) |
| IgM | 0 (0–2,936) | 0 (0–2,632) | 0 (0–4,655) | 242 (0–2,775) |
| Vaginal wash | ||||
| IgA1 | 0 (0–212) | 0 (0–40) | 0 (0–30) | 6 (0–55) |
| IgA2 | 0 (0–0) | 0 (0–94)a | 0 (0–0) | 0 (0–0) |
| IgG | 66 (0–671) | 81 (0–12,143) | 91 (0–619) | 96 (0–1,319) |
| IgM | 0 (0–66) | 0 (0–85) | 0 (0–174) | 0 (0–782) |
| Serum | ||||
| IgA1 | 122 (16–923) | 413d (137–1,817) | 249 (83–380) | 397d (65–2,725) |
| IgA2 | 0 (0–751)b | 0 (0–136)c | 0 (0–145)a | 0 (0–3,417)a |
| IgG | 27,800 (11,000–82,700) | 21,655 (10,316–71,234) | 22,140 (11,200–52,716) | 26,780 (8,551–65,433) |
| IgM | 19,650 (0–90,000) | 19,990 (10,230–40,700) | 13,100 (3,450–29,190) | 21,387 (4,710–61,935) |
One patient was positive for IgA2 antibodies.
Three patients were positive for IgA2 antibodies.
Five patients were positive for IgA2 antibodies.
P < 0.05 compared with noninfected subjects at same time (Mann-Whitney U test).
Slightly different patterns of antibody levels were observed in male compared with female patients. Antigonococcal antibodies were present in sera and in some urethral swabs from both infected and noninfected males (Table 4). There was no difference between the levels of serum IgA1, IgA2, and IgG antibodies to N. gonorrhoeae MS11 in sera from infected and noninfected males at visit 1. Statistical analysis of potential differences between these groups at visit 2 was not valid due to the low numbers of returning noninfected males. The levels of serum IgG antibodies, but not of other isotypes, increased from visit 1 to visit 2 (P = 0.0476, Wilcoxon signed-rank test). In general, antibody levels in urethral swabs were measurable only when the total Ig concentration for that isotype was greater than 10 μg/ml. Total Ig levels from 30 to 40% of the swabs did not reach this level, and the levels of antibodies in those samples could therefore not be quantitated. Consequently, to avoid bias of the data due to the selection of only positive samples, statistical comparisons of the antibody responses in urethral swabs from infected and noninfected patients were not performed.
TABLE 4.
Antibody levels to N. gonorrhoeae MS11 in serum and urethral swabs from noninfected and infected males
| Sample | Antibody isotype | Median antibody level (ng/ml) (range) [n]
|
|||
|---|---|---|---|---|---|
| Visit 1
|
Visit 2
|
||||
| Noninfected | N. gonorrhoeae infected | Noninfected | N. gonorrhoeae infected | ||
| Serum | IgA1 | 621 (86–11,728) [13] | 719 (118–7,161) [58] | 636 (300–3,957) [4] | 845 (242–4,319) [20] |
| IgA2 | 0 (0–1,319) [13] | 179 (0–3,392) [58] | 97 (0–328) [4] | 178 (0–1,477) [20] | |
| IgG | 23,736 (9,177–156,400) [13] | 19,429 (4,400–100,828) [58] | 28,720 (9,538–56,338) [4] | 20,981a (13,349–117,894) [20] | |
| Urethral swab | IgA1 | 0 (0–99) [14] | 0 (0–170) [36] | 0 [5] | 0 (0–128) [13] |
| IgA2 | 77 (0–354) [14] | 213 (0–432) [36] | 0 [5] | 0 (0–300) [13] | |
| IgG | 0 (0–442) [14] | 119 (0–685) [36] | 0 [5] | 105 (0–450) [13] | |
P = 0.0476 (Wilcoxon signed-rank test) compared with IgG antibody levels at visit 1.
Antibody responses to homologous infecting isolates of N. gonorrhoeae.
In addition to the antibody levels to MS11, we also examined the local and systemic antibody responses against each infected patient’s homologous isolate of N. gonorrhoeae.
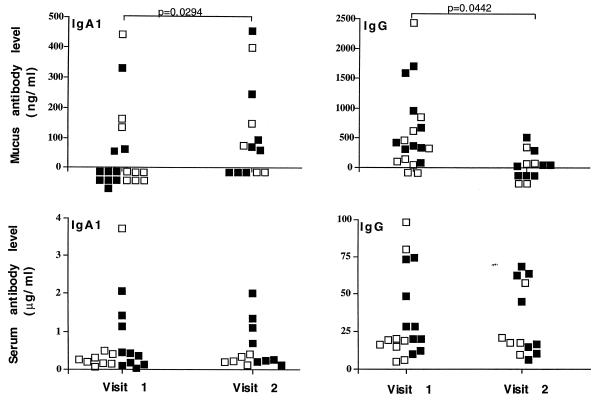
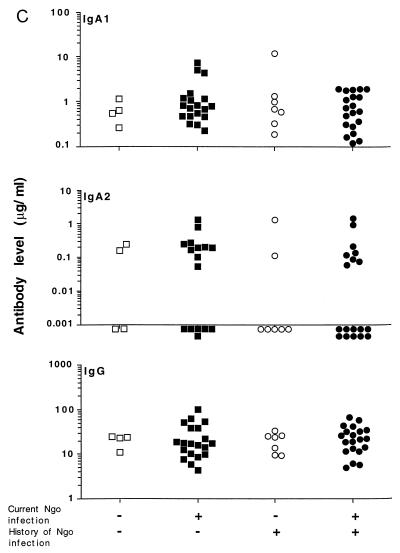
IgA2 antibodies to the homologous isolates were not detected in cervical mucus, vaginal wash, or serum samples from any female patient. Median levels of IgA1 antibodies in cervical mucus and serum samples at visit 1 were 0 and 267 ng/ml, respectively, and those at visit 2 were 71 and 268 ng/ml, respectively (Fig. 1). Notably, isolate-specific IgA1 antibodies in cervical mucus samples were higher at visit 2 than at visit 1 (P = 0.0294). Median levels of IgG antibodies in cervical mucus and serum samples to the homologous isolates at visit 1 were 383 and 19,961 ng/ml respectively, and those at visit 2 were 13 and 17,481 ng/ml, respectively (Fig. 1). In contrast to IgA1, isolate-specific IgG antibodies in cervical mucus samples were lower at visit 2 than at visit 1 (P = 0.0442). The levels of isolate-specific IgA1 and IgG antibodies in serum samples were unchanged from visit 1 to visit 2.
FIG. 1.
Cervical mucus and serum IgA1 and IgG antibody levels to the homologous infecting isolates from female patients at visit 1 (enrollment and treatment) and visit 2 (2 weeks after treatment). Differences between visits were compared with the Wilcoxon signed-rank test on data expressed relative to the corresponding total Ig levels. Filled symbols indicate patients reporting at least one previous episode of gonorrhea.
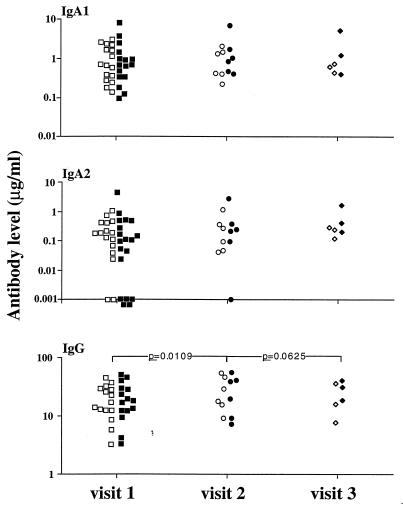
The median levels of isolate-specific IgA1 antibodies in sera from male patients at visits 1, 2, and 3 were 709, 929, and 677 ng/ml, respectively (Fig. 2). Median IgA2 antibody levels in sera at visits 1, 2, and 3 were 124, 231, and 271 ng/ml, respectively. There were no differences in the levels of isolate-specific IgA1 or IgA2 antibodies from visits 1 to 3. Unlike the other isotypes, IgG antibodies to the homologous infecting isolates increased from visit 1 (median = 17.9 μg/ml) to visit 2 (median = 25.0 μg/ml; P = 0.0059 by Wilcoxon signed-rank test). The median level of IgG antibody to the infecting isolate at visit 3 was 25 μg/ml (P = 0.0625 compared with visit 2 levels by Wilcoxon signed-rank test).
FIG. 2.
Serum IgA1, IgA2, and IgG antibody levels to the homologous infecting isolates from male patients at visit 1 (enrollment and treatment), visit 2 (2 weeks after treatment), and visit 3 (4 weeks after treatment). Differences between visits were compared with the Wilcoxon signed-rank test. Filled symbols indicate patients reporting at least one previous episode of gonorrhea. Note logarithmic scales.
Comparison of antibody levels against MS11 and the patients’ homologous isolates.
We anticipated that greater responses might be evident against patients’ homologous isolates than against the MS11 strain. In general this was not the case, however, and with some exceptions the responses to the patients’ homologous isolates were similar to those against the MS11 strain. In cervical mucus from infected women, the levels of isolate-specific IgG antibodies were significantly lower than those against MS11 at both visit 1 and visit 2 (P = 0.02 and P = 0.0193, respectively). Serum and mucus IgA1 and serum IgG antibodies to the infecting strains were not significantly different from those detected against MS11. In male serum samples, the levels of isolate-specific IgA2 antibodies were higher than those against the MS11 strain at both visit 1 (P = 0.0024) and visit 2 (P = 0.0294), while the levels of isolate-specific and MS11-specific IgG and IgA1 antibodies were not significantly different.
Significant correlations between isolate-specific and MS11-specific antibody levels were observed for IgG, but not IgA1, antibodies in cervical mucus (rs = 0.5279, p = 0.0243, by Spearman’s correlation) and serum (rs = 0.5018, p = 0.0286, by Spearman’s correlation) samples from female patients. In male serum, there was a significant correlation between isolate-specific and MS11-specific antibody levels for IgG (rs = 0.7357, P < 0.0001, by Spearman’s correlation) and IgA1 (rs = 0.8963, P < 0.0001, by Spearman’s correlation) but not for IgA2.
Effect of previous gonococcal infections on antibody responses to N. gonorrhoeae.
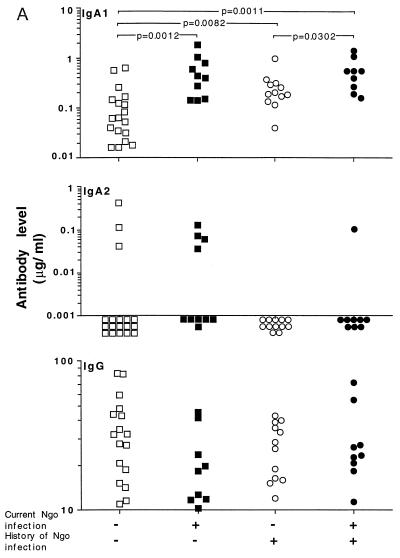
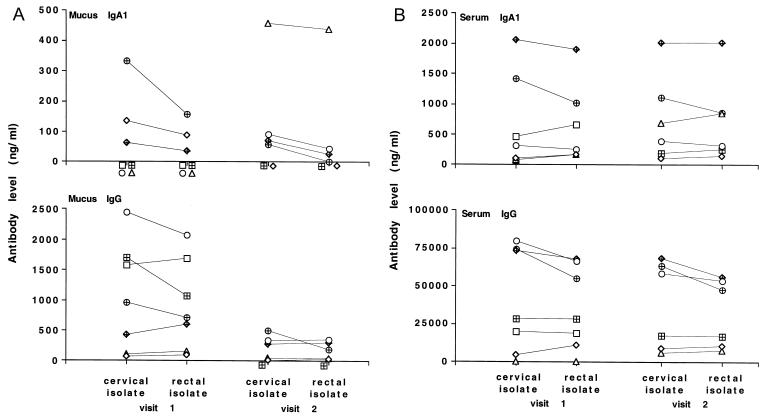
Approximately 40% of the female patients and 50% of the male patients in this study reported at least one previous episode of gonorrhea. We therefore examined whether the antibody responses to N. gonorrhoeae were different in patients reporting previous infections compared to those with no history of gonorrhea. In female patients, the levels of serum antigonococcal IgA1 antibodies were higher in currently infected than in noninfected patients without regard to previous history of gonococcal infection (Fig. 3A). Serum IgA1 antibodies to N. gonorrhoeae were higher in patients reporting previous episodes of gonorrhea but who were not currently infected than in similar patients who reported no previous gonorrhea. In currently infected patients, however, there was no effect of previous gonorrhea on the levels of serum IgA1 antibodies to MS11. The levels of serum antigonococcal antibodies of other isotypes and the antibody levels of all tested isotypes in cervical mucus were not affected by previous infection with N. gonorrhoeae (Fig. 3B). Previous episodes of gonorrhea had no effect on the levels of antibodies of any isotype in serum or cervical mucus to the homologous infecting isolates (Fig. 1).
FIG. 3.
IgA1, IgA2, and IgG antibody levels to N. gonorrhoeae MS11 in serum (A) and cervical mucus (B) from female patients and in serum (C) from male patients at visit 1. Differences between groups were compared with the Kruskal-Wallis and Mann-Whitney U tests. Note logarithmic scales.
Previous episodes of gonorrhea did not influence the levels of serum antibodies of any isotype to MS11 in either currently infected or noninfected males (Fig. 3C). In addition, there was no difference in the levels of antibodies to the homologous isolates in currently infected patients with and without a history of gonorrhea (Fig. 2).
Effects of rectal coinfection on antibody responses to N. gonorrhoeae.
Although the rectum was not a unique site of infection among the patients examined in this study, rectal coinfections with N. gonorrhoeae were detected in approximately 50% of the cervically infected patients. Since the rectum, unlike the normal genital tract, contains organized lymphoid tissue (32, 33, 43) and is therefore considered to be an inductive site for the common mucosal immune system (28), we examined whether rectal coinfections resulted in enhanced antibody responses to N. gonorrhoeae. Serum IgA1, IgA2, and IgG antigonococcal antibodies to MS11 and to participants’ cervical isolates (expressed as a percentage of total Ig) were not different in patients with rectal coinfection compared to patients with cervical infections alone (Table 5). In contrast, the median levels of mucus IgG antibodies at visit 1 to the cervical isolates were 0.09 and 0.32% in cervically infected and coinfected patients, respectively, but this difference did not reach statistical significance (P = 0.0782). At visit 2, the levels of mucus IgG antibodies were higher in rectally coinfected tpatients (0.37%) than in patients with cervical infections alone (0%; P = 0.0303). The levels of other mucus antibodies at either visit were not affected by rectal coinfection. Salivary antibodies to the infecting isolates were not altered by rectal infection (Table 5).
TABLE 5.
Comparison of serum, saliva, and cervical mucus IgA1 and IgG antibody levels to N. gonorrhoeae MS11 and infecting isolates in patients with cervical infections and patients with cervical and rectal infections
| Sample | Ig isotype | Visit | Median antibody level (% of total Ig) (range [n])
|
|||
|---|---|---|---|---|---|---|
| Anti-MS11 antibodies
|
Anti-cervical isolate antibodies
|
|||||
| Cervical infection | Cervical and rectal infection | Cervical infection | Cervical and rectal infection | |||
| Cervical mucus | IgA1 | 1 | 0.00 (0.00–0.21 [11]) | 0.16 (0.00–0.45 [6]) | 0.00 (0.00–0.08 [12]) | 0.00 (0.00–0.15 [6]) |
| IgA1 | 2 | 0.03 (0.00–1.12 [7]) | 0.00 (0.00–0.07 [6]) | 0.07 (0.00–1.97 [7]) | 0.08 (0.00–0.73 [6]) | |
| IgG | 1 | 0.57 (0.00–12.40 [11]) | 0.85 (0.41–1.55 [6]) | 0.09 (0.00–0.94 [11]) | 0.32a (0.08–2.43 [6]) | |
| IgG | 2 | 0.74 (0.03–2.90 [7]) | 0.71 (0.00–0.86 [5]) | 0.00 (0.00–0.07 [7]) | 0.37b (0.01–1.39 [5]) | |
| Saliva | IgA1 | 1 | 0.06 (0.00–0.42 [7]) | 0.04 (0.00–0.09 [5]) | 0.01 (0.00–0.07 [8]) | 0.00 (0.00–0.03 [6]) |
| IgA1 | 2 | 0.03 (0.00–0.24 [5]) | 0.03 (0.01–0.05 [4]) | 0.01 (0.01–0.20 [5]) | 0.01 (0.00–0.02 [5]) | |
| IgG | 1 | 0.12 (0.00–1.58 [8]) | 0.30 (0.00–0.40 [5]) | 0.26 (0.00–1.91 [8]) | 0.06 (0.00–0.46 [6]) | |
| IgG | 2 | 0.47 (0.00–1.77 [5]) | 0.00 (0.00–0.59 [3]) | 0.15 (0.00–4.30 [5]) | 0.00 (0.00–0.43 [5]) | |
| Serum | IgA1 | 1 | 0.01 (0.00–0.02 [12]) | 0.02 (0.01–0.05 [7]) | 0.01 (0.00–0.06 [12]) | 0.01 (0.00–0.09 [7]) |
| IgA1 | 2 | 0.01 (0.00–0.02 [7]) | 0.02 (0.01–0.05 [6]) | 0.01 (0.01–0.02 [7]) | 0.01 (0.00–0.08 [6]) | |
| IgG | 1 | 0.25 (0.14–1.41 [12]) | 0.28 (0.20–1.13 [7]) | 0.21 (0.06–3.42 [12]) | 0.77 (0.00–0.94 [7]) | |
| IgG | 2 | 0.28 (0.13–0.58 [7]) | 0.33 (0.25–1.29 [6]) | 0.25 (0.19–0.85 [7]) | 0.46 (0.08–0.79 [6]) | |
P = 0.0782 compared with patients with cervical infection.
P = 0.0303 compared with patients with cervical infection.
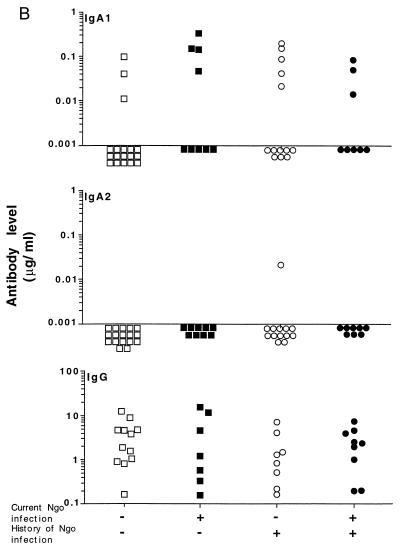
Comparison of the antibody responses to the rectal and cervical isolates.
There was no significant difference at either visit 1 or visit 2 between the levels of IgA1, IgA2, and IgG antibodies in serum or cervical mucus against the cervical and rectal isolates (Fig. 4). There was, however, an overall trend for the IgA1 and IgG antibody levels to the rectal isolate to be lower than the levels to the cervical isolate, especially among patients with the highest antibody responses, though this difference did not reach statistical significance.
FIG. 4.
IgA1 and IgG antibody levels to homologous rectal and cervical isolates from female patients in cervical mucus (A) and in serum (B). Differences between groups were compared with the Wilcoxon signed-rank test.
DISCUSSION
The evident lack of protective immunity to gonorrhea, despite the presence of detectable antigonococcal antibodies, has been ascribed to the various potentially defensive mechanisms possessed by this organism, including variation of outer membrane proteins and lipooligosaccharides (29), resistance to complement-mediated bacteriolysis (39, 42), as well as the production of IgA1 protease (36). Recent preliminary evidence indicated, however, that while antigonococcal antibodies were detected in infected patients, the levels of both systemic and local antibodies were surprisingly low (14). We postulated, therefore, that in addition to evading the effects of an immune response, N. gonorrhoeae may avoid initiating an immune response as a means of survival. This hypothesis was tested in three ways. We first examined and compared the antibody responses to a patient-independent strain of N. gonorrhoeae (MS11) as well as to the patients’ own homologous infecting isolates (where appropriate). Second, we examined whether previous exposure to N. gonorrhoeae affected antigonococcal antibody levels. Third, we examined whether the site of infection (genital tract and rectum) played a role in the antibody responses to N. gonorrhoeae. Overall, our results indicate that while there are some minor antibody responses associated with uncomplicated gonococcal infection in males and females, the antibody levels are lower than with other mucosal infections (8, 10, 17, 38). Furthermore, the antibody levels in infected subjects were not substantially affected by either a history of previous exposure to N. gonorrhoeae or the site of infection. We believe that these results support the hypothesis that N. gonorrhoeae avoids initiating antibody responses as a mechanism employed by the organism to enhance its survival.
It is an accepted concept of gonococcal pathogenesis that antibodies are generated during infection but N. gonorrhoeae evades their effects through a variety of strategies including extensive antigenic variation. In addition to the potential to thwart the effects of an immune response, such variation may also reduce the likelihood that antibody responses to a single antigen will be representative of responses to gonococci in general. To minimize this possibility in this study, we chose to examine the responses to whole fixed gonococci prepared as batch cultures rather than any one antigen. Based on the concept that gonococci evade the immune response, we expected that antibody responses to N. gonorrhoeae would be substantially higher in infected than in noninfected patients. Local genital and systemic antibodies to N. gonorrhoeae MS11 were detected in both infected and noninfected male and female patients. Both the IgA1 and IgG antibodies in cervical mucus and vaginal wash appeared to be of local rather than systemic origin, since neither isotype of response displayed correlations between the circulatory and genital mucosal compartments. Serum IgA1 anti-MS11 antibody responses were detected at very modest levels in female but not male patients in response to gonococcal infection. This result appears to be consistent with the serum antigonococcal IgA antibody response observed in a small number of adolescent women infected with gonococci (34). In contrast to female patients, no significant difference between the antibody levels of any isotype was detectable in sera from infected and noninfected male patients. Using paired statistical analysis of serum from infected males, however, we detected a slight increase in the serum IgG antibody levels between visits 1 and 2. It is possible that with more samples, a small but significant difference between infected and noninfected males will emerge. It is not clear why modest antibody responses were detectable in female but not male patients. The overt inflammatory responses to gonorrhea in males may allow for more rapid treatment and bacterial clearance compared to females. It is therefore possible that there is less opportunity for any immune response to develop in males compared to females.
In addition to the MS11 strain, we examined antibody levels to each infected patient’s homologous isolate, anticipating that the responses to the participants’ own infecting isolates would be higher than responses to the laboratory strain of N. gonorrhoeae. In infected female patients, there was a slight increase in the level of infecting isolate-specific, but not MS11-specific, IgA1 antibodies in cervical mucus between the time of antibiotic treatment and 2 weeks thereafter. Such isolate-specific responses may contribute to the reduced risk of reinfection with the same serovar of N. gonorrhoeae reported by Plummer et al. (37). In contrast, there was a decrease in the level of isolate-specific IgG antibodies between visits 1 and 2 in these same patients. In males, there was a slight increase in serum IgG antibodies against the patients’ homologous isolates from visit 1 to visit 2. In contrast to our expectations, we found, with a few exceptions (IgG in cervical mucus and IgA2 in male serum), that the levels of antibody to the homologous infecting isolates were similar to those to the MS11 strain in both males and females. The absence of a substantial antibody response to N. gonorrhoeae stands in marked contrast to the serum and secretory antibody responses produced by mucosal infections with other bacterial pathogens such as N. meningitidis or Vibrio, Salmonella, and Shigella species (8, 10, 17, 38). The absence of substantial levels of antibodies to both the MS11 strain and the homologous isolates suggests that there is little to no antibody response during and after uncomplicated gonococcal infections in males and females.
The concept that previous exposure to an antigen results in increased levels of protective antibodies upon reexposure is central to the development of vaccines against infectious organisms. Repeated infections with N. gonorrhoeae are common; therefore, given the low antibody levels detected in response to current gonococcal infection, we examined whether a history of previous exposure to N. gonorrhoeae affected the levels of antigonococcal antibodies. Surprisingly, a history of gonorrhea did not significantly alter the levels of any antibodies in male patients. In female patients, only serum IgA1 antibody levels showed any effect arising from previous exposure; antibody levels of other isotypes in serum and all antibodies in cervical mucus were unaffected by previous gonococcal infections. Previous infections with N. gonorrhoeae resulted in marginally higher levels of serum IgA1 antibodies to MS11 in female patients who were not currently infected with gonococci and did not alter the antibody levels of any isotype in female patients with an ongoing infection either to the MS11 strain or to the patient’s infecting isolate. Therefore, while some effects of previous exposure to gonococci were discernible, in general the differences in antibody levels between patients with and without previous infections were unexpectedly small. These results further support the possibility that repeated infections with N. gonorrhoeae are common because there is little development of immune memory and therefore only minimal levels of protective immunity.
One potential explanation for the paucity of antibody responses to N. gonorrhoeae in uncomplicated genital tract infections may be related to the absence of organized mucosa-associated lymphoid tissue, such as the Peyer’s patches of the small intestine or Waldeyer’s ring in the pharynx, which are recognized as major sites for the uptake and processing of antigens leading to generalized disseminated mucosal immune responses (20, 41). Several studies have been performed on intravaginal immunization in women and experimental animals, with a variety of antigenic materials, including those known to have potent immunogenic and adjuvant properties by other mucosal routes of administration (23, 27, 31, 45). Although in some studies, local vaginal antibody responses were recorded, overall it appears that, by comparison with oral or nasal administration (21), intravaginal immunization in humans is inefficient in inducing either circulating or generalized mucosal antibody responses. Given the requirement to minimize responses to allogenic sperm, this should not be surprising.
In contrast to the genital tract, the rectum contains lymphoid follicles (32, 43) resembling Peyer’s patches that likely serve as an inductive site of the common mucosal immune system (5, 6, 16, 18, 30). In addition, it has been suggested that these sites may preferentially supply specific antibody-secreting cell precursors to the adjacent genital tract which shares the same lymphoid drainage (5, 16). Therefore, it seemed likely that persons infected at both the rectum and genital sites might be expected to display enhanced antibody responses to the infecting organism, both in the genital tract and perhaps also in remote secretions. Rectal infections with N. gonorrhoeae were common among the female patients of this study. This allowed us to examine whether more pronounced antigonococcal antibody responses were generated by gonococcal infection at a site known to contain organized inductive lymphoid tissue. There was a small effect of rectal infection on the levels of isolate specific IgG in cervical mucus. IgG antibodies decreased from the time of treatment to 2 weeks thereafter in patients with only cervical infections but not in patients with concomitant rectal infections. In contrast to the genital tract, rectal infection did not alter the levels of antigonococcal antibodies of any isotype or specificity in saliva. Overall, we found little difference in antibody levels in patients with cervical compared with cervical and rectal infections, suggesting that rectal infection was no more efficient than the genital tract infection for inducing humoral responses to N. gonorrhoeae.
The development of an antigonococcal vaccine has been based on the presumption that there is an antibody response to N. gonorrhoeae but the organism evades that response. Although antigonococcal antibodies are present in serum and secretions of most subjects regardless of infections, we find that the antibody levels to a representative gonococcal strain and to the patients’ infecting isolates are low and that while some antibody responses to infection are detectable, these responses are weak at best. Moreover, we have not observed any clear indications of immune memory toward gonococci as evidenced by the failure of previous exposure to this organism to generate more pronounced antibody responses. It is unlikely that the poor antibody responses in both male and female patients to N. gonorrhoeae was simply due to an absence of known inductive sites in the genital tract, since female patients with rectal infections did not show any marked enhancement of the antigonococcal responses. Based on these results, we propose that gonococci avoid inducing humoral immune responses during uncomplicated natural infections. If correct, this hypothesis suggests that gonococci use an as yet undefined mechanism of protection which may subvert the natural immune response. A possible corollary of these observations is that the use of alternative approaches for generating antibodies in the genital tract against appropriate gonococcal antigens may have protective value. These results suggest that vaccination endeavors should therefore be directed toward exploiting novel concepts and strategies of mucosal or systemic immunizations; examples include nasal immunization, which has been shown to generate antibody responses in genital secretions (49–51), use of alternative adjuvants to enhance humoral responses (11–13), and DNA-based vaccines which exploit different mechanisms of antigen presentation than conventional vaccines (7).
ACKNOWLEDGMENTS
This study was supported by PHS grants AI34970 and AI28147 and the Swedish Medical Research Council.
We thank Lisa Kallman and Kathy Brandt for excellent technical assistance in the laboratory, and we thank Carol Blalock, Annalee Hughes, and Sharon Davis, for the recruitment of patients and clinical procedures in the Jefferson County STD clinic.
REFERENCES
- 1.Beck E J, Mandalia S, Leonard K, Griffith R J, Harris J R, Miller D L. Case-control study of sexually transmitted diseases as cofactors for HIV-1 transmission. Int J STD AIDS. 1996;7:34–38. doi: 10.1258/0956462961917023. [DOI] [PubMed] [Google Scholar]
- 2.Bélec L, Dupré T, Prazuck T, Tévi-Bénissan C, Kanga J-M, Pathey O, Lu X-S, Pillot J. Cervicovaginal overproduction of specific IgG to human immunodeficiency virus (HIV) contrasts with normal or impaired IgA local response in HIV infection. J Infect Dis. 1995;172:691–697. doi: 10.1093/infdis/172.3.691. [DOI] [PubMed] [Google Scholar]
- 3.Boslego J W, Tramont E C, Chung R C, McChesney D G, Ciak J, Sadoff J C, Piziak M V, Brown J D, Brinton C C, Jr, Wood S W, Bryan J R. Efficacy trial of a parenteral gonococcal pilus vaccine in men. Vaccine. 1991;9:154–162. doi: 10.1016/0264-410x(91)90147-x. [DOI] [PubMed] [Google Scholar]
- 4.Chipperfield E J, Evans B A. Effect of local infection and oral contraception on immunoglobulin levels in cervical mucus. Infect Immun. 1975;11:215–221. doi: 10.1128/iai.11.2.215-221.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crowley-Nowick P A, Bell M C, Brockwell R, Edwards R P, Chen S, Partridge E E, Mestecky J. Rectal immunization for induction of specific antibody in the genital tract of women. J Clin Immunol. 1997;17:370–379. doi: 10.1023/a:1027312223474. [DOI] [PubMed] [Google Scholar]
- 6.Forrest B D, Shearman D J C, LaBrooy J T. Specific immune responses in humans following rectal delivery of live typhoid vaccine. Vaccine. 1990;8:209–212. doi: 10.1016/0264-410x(90)90047-p. [DOI] [PubMed] [Google Scholar]
- 7.Fynan E F, Webster R G, Fuller D H, Haynes J R, Santoro J C, Robinson H L. DNA vaccines: protective immunizations by parenteral, mucosal, and gene-gun inoculations. Proc Natl Acad Sci USA. 1993;90:11478–11482. doi: 10.1073/pnas.90.24.11478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glass R I, Svennerholm A M, Khan M R, Huda S, Huq M I, Holmgren J. Seroepidemiological studies of El Tor cholera in Bangladesh: association of serum antibody levels with protection. J Infect Dis. 1985;151:236–242. doi: 10.1093/infdis/151.2.236. [DOI] [PubMed] [Google Scholar]
- 9.Govers J, Girard J P. Some immunological properties of human cervical and vaginal secretions. Gynecol Investig. 1972;3:184–194. doi: 10.1159/000301774. [DOI] [PubMed] [Google Scholar]
- 10.Guttormsen H K, Wetzler L M, Naess A. Humoral immune response to the class 3 outer membrane protein during the course of meningococcal disease. Infect Immun. 1994;61:4734–4742. doi: 10.1128/iai.61.11.4734-4742.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haack B M, Emmrich F, Resch K. Cholera toxin inhibits T cell receptor signaling by covalent modification of the CD3-ζ subunit. J Immunol. 1993;150:2599–2606. [PubMed] [Google Scholar]
- 12.Hajishengallis G, Hollingshead S K, Koga T, Russell M W. Mucosal immunization with a bacterial protein antigen genetically coupled to cholera toxin A2/B subunits. J Immunol. 1995;154:4322–4332. [PubMed] [Google Scholar]
- 13.Hajishengallis G, Michalek S M, Russell M W. Persistence of serum and salivary antibody responses after oral immunization with a bacterial protein antigen genetically linked to the A2/B subunits of cholera toxin. Infect Immun. 1996;64:665–667. doi: 10.1128/iai.64.2.665-667.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hedges S R, Sibley D, Mayo M S, Hook III E, Russell M W. Cytokine and antibody responses in women infected with Neisseria gonorrhoeae: effects of concomitant infections. J Infect Dis. 1998;178:742–751. doi: 10.1086/515372. [DOI] [PubMed] [Google Scholar]
- 15.Hook E W, Brady W E, Reichart C A, Upchurch D M, Sherman L A, Wasserheit J N. Determinants of emergence of antibiotic-resistant Neisseria gonorrhoeae. J Infect Dis. 1989;159:900–907. doi: 10.1093/infdis/159.5.900. [DOI] [PubMed] [Google Scholar]
- 16.Hordnes K, Tynning T, Kvam A I, Jonsson R, Haneberg B. Colonization in the rectum and uterine cervix with group B streptococci may induce specific antibody responses in cervical secretions of pregnant women. Infect Immun. 1996;64:1643–1652. doi: 10.1128/iai.64.5.1643-1652.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Islam D, Wretlind B, Ryd M, Lindberg A A, Christensson B. Immunoglobulin subclass distribution and dynamics of Shigella-specific antibody responses in serum and stool samples in shigellosis. Infect Immun. 1995;63:2054–2061. doi: 10.1128/iai.63.5.2054-2061.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kantele A, Häkkinen M, Moldoveanu Z, Lu A, Savilahti E, Alvarez R D, Michalek S, Mestecky J. Differences in immune responses induced by oral and rectal immunizations with Salmonella typhi Ty21a: evidence for compartmentalization within the common mucosal immune system. Infect Immun. 1998;66:5630–5635. doi: 10.1128/iai.66.12.5630-5635.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kearns D H, O’Reilly R J, Lee L, Welch B G. Secretory IgA antibodies in the urethral exudate of men with uncomplicated urethritis due to Neisseria gonorrhoeae. J Infect Dis. 1973;127:99–101. doi: 10.1093/infdis/127.1.99. [DOI] [PubMed] [Google Scholar]
- 20.Kelsall B, Strober W. Gut associated lymphoid tissue: antigen handling and T-lymphocyte responses. In: Ogra P L, Mestecky J, Lamm M E, Strober W, Bienenstock J, McGhee J R, editors. Mucosal immunology. London, England: Academic Press; 1999. pp. 293–317. [Google Scholar]
- 21.Kozlowski P A, Cu-Uvin S, Neutra M R, Flanigan T P. Comparison of the oral rectal and vaginal immunization routes for induction of antibodies in rectal and genital tract secretions. Infect Immun. 1997;65:1387–1394. doi: 10.1128/iai.65.4.1387-1394.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le Bacq F, Mason P R, Gwanzura L, Robertson V J, Latif A S. HIV and other sexually transmitted diseases at a rural hospital in Zimbabwe. Gen Med. 1993;69:352–356. doi: 10.1136/sti.69.5.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lehner T, Bergmeier L A, Panagiotidi C, Tao L, Brookes R, Klavinskis L S, Walker P, Walker J, Ward R G, Hussain L, Gearing A J H, Adams S E. Induction of mucosal and systemic immunity to a recombinant simian immunodeficiency viral protein. Science. 1992;258:1365–1369. doi: 10.1126/science.1360702. [DOI] [PubMed] [Google Scholar]
- 24.McChesney D, Tramont E C, Boslego J W, Ciak J, Sadoff J, Brinton C C. Genital antibody response to a parenteral gonococcal pilus vaccine. Infect Immun. 1982;36:1006–1012. doi: 10.1128/iai.36.3.1006-1012.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McMillan A, McNeillage G, Young H. Antibodies to Neisseria gonorrhoeae: a study of the urethral exudates of 232 men. J Infect Dis. 1979;140:89–95. doi: 10.1093/infdis/140.1.89. [DOI] [PubMed] [Google Scholar]
- 26.McMillan A, McNeillage G, Young H, Bain S S R. Secretory antibody response of the cervix to infection with Neisseria gonorrhoeae. Br J Vener Dis. 1979;55:265–270. doi: 10.1136/sti.55.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Menge A C, Michalek S M, Russell M W, Mestecky J. Immune response of the female rat genital tract after oral and local immunization with keyhole limpet hemocyanin conjugated to cholera toxin B subunit. Infect Immun. 1993;61:2162–2171. doi: 10.1128/iai.61.5.2162-2171.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mestecky J. The common mucosal immune system and current strategies for induction of immune response in external secretions. J Clin Immunol. 1987;7:265–276. doi: 10.1007/BF00915547. [DOI] [PubMed] [Google Scholar]
- 29.Meyer T F, Gibbs C P, Haas R. Variation and control of protein expression in Neisseria. Annu Rev Microbiol. 1990;44:451–477. doi: 10.1146/annurev.mi.44.100190.002315. [DOI] [PubMed] [Google Scholar]
- 30.Nardelli-Haefliger D, Kraehenbuhl J-P, Curtiss R, Schödel F, Potts A, Kelly S, de Grandi P. Oral and rectal immunization of adult female volunteers with a recombinant attenuated Salmonella typhi vaccine strain. Infect Immun. 1996;64:5219–5224. doi: 10.1128/iai.64.12.5219-5224.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ogra P L, Ogra S S. Local antibody response to poliovaccine in the female genital tract. J Immunol. 1973;110:1307–1311. [PubMed] [Google Scholar]
- 32.O’Leary A D, Sweeney E C. Lymphoglandular complexes of the colon: structure and distribution. Histopathology. 1986;10:267–283. doi: 10.1111/j.1365-2559.1986.tb02481.x. [DOI] [PubMed] [Google Scholar]
- 33.O’Leary A D, Sweeney E C. Lymphoglandular complexes of the normal colon: histochemistry and immunohistochemistry. Ir J Med Sci. 1987;156:142–148. doi: 10.1007/BF02953232. [DOI] [PubMed] [Google Scholar]
- 34.O’Reilly R J, Lee L, Welch B G. Secretory IgA antibody responses to Neisseria gonorrhoeae in the genital secretions of infected females. J Infect Dis. 1976;133:113–125. doi: 10.1093/infdis/133.2.113. [DOI] [PubMed] [Google Scholar]
- 35.Parazzini F, D’Oro L C, Naldi L, Bianchi C, Chatenoud L, Ricci E, Cainelli T, Pansera B, Mezzanotte C, Tessari G P, Locatelli A. Sexually transmitted diseases and risk of HIV infection. Acta Dermatol Venereol. 1996;76:147–149. doi: 10.2340/0001555576147149. [DOI] [PubMed] [Google Scholar]
- 36.Plaut A G, Gilbert J V, Artenstein M S, Capra J D. Neisseria gonorrhoeae and Neisseria meningitidis: extracellular enzyme that cleaves human immunoglobulin A. Science. 1975;190:1103–1105. doi: 10.1126/science.810892. [DOI] [PubMed] [Google Scholar]
- 37.Plummer F A, Simonsen J N, Chubb H, Slaney L, Kimata J, Bosire M, Ndinya-Achola J O, Ngugi E N. Epidemiologic evidence for the development of serovar-specific immunity after gonococcal infection. J Clin Investig. 1989;83:1472–1476. doi: 10.1172/JCI114040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qadri F, Wenneras C, Albert M J, Hossain J, Mannoor K, Begum Y A, Mohi G, Salam M A, Sack R B, Svennerholm A M. Comparison of immune responses in patients infected with Vibrio cholerae O139 and O1. Infect Immun. 1997;65:3571–3576. doi: 10.1128/iai.65.9.3571-3576.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rice P A, Vayo H E, Tam M R, Blake M S. Immunoglobulin G antibodies directed against protein III block killing of serum resistant Neisseria gonorrhoeae by immune serum. J Exp Med. 1986;164:1735–1748. doi: 10.1084/jem.164.5.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Russell M W, Brown T A, Radl J, Haaijman J J, Mestecky J. Assay of human IgA subclass antibodies in serum and secretions by means of monoclonal antibodies. J Immunol Methods. 1986;87:87–93. doi: 10.1016/0022-1759(86)90347-9. [DOI] [PubMed] [Google Scholar]
- 41.Sminia T, Kraal G. Nasal-associated lymphoid tissue. In: Ogra P L, Mestecky J, Lamm M E, Strober W, Bienenstock J, McGhee J R, editors. Mucosal immunology. London, England: Academic Press; 1999. pp. 357–364. [Google Scholar]
- 42.Smith H, Cole J A, Parsons N J. The sialylation of gonococcal lipopolysaccharide by host factors: a major impact on pathogenicity. FEMS Microbiol Lett. 1992;100:287–292. doi: 10.1111/j.1574-6968.1992.tb14054.x. [DOI] [PubMed] [Google Scholar]
- 43.Strindel H. Bartels ‘Tonsille des Mastdarmes’ und ihre Stellung in der Pathologie des Lymphatischen Apparates des Mastdarmes. Zentrbl Chir. 1935;62:2594–2607. [Google Scholar]
- 44.Tapchaisri P, Sirisinha S. Serum and secretory antibody responses to Neisseria gonorrhoeae in patients with gonococcal infections. Br J Vener Dis. 1976;52:374–380. doi: 10.1136/sti.52.6.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thapar M A, Parr E L, Parr M B. Secretory immune responses in mouse vaginal fluid after pelvic, parenteral, or vaginal immunization. Immunology. 1990;70:121–125. [PMC free article] [PubMed] [Google Scholar]
- 46.Tramont E C. Inhibition of adherence of Neisseria gonorrhoeae by human genital secretions. J Clin Investig. 1977;59:117–124. doi: 10.1172/JCI108608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tramont E C, Sadoff J C, Boslego J W, Ciak J, McChesney D, Brinton C C, Wood S, Takafuji E. Gonococcal pilus vaccine. Studies of antigenicity and inhibition of attachment. J Clin Investig. 1981;68:881–888. doi: 10.1172/JCI110343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Waldman R H, Cruz J, Rowe S. Immunoglobulin levels and antibodies to Candida albicans in human cervicovaginal secretions. Clin Exp Immunol. 1972;10:427–434. [PMC free article] [PubMed] [Google Scholar]
- 49.Wu H-Y, Nguyen H, Russell M W. Nasal lymphoid tissue (NALT) as a mucosal immune inductive site. Scand J Immunol. 1997;46:506–513. doi: 10.1046/j.1365-3083.1997.d01-159.x. [DOI] [PubMed] [Google Scholar]
- 50.Wu H-Y, Russell M W. Induction of mucosal immunity by intranasal application of a streptococcal surface protein antigen with the cholera toxin B subunit. Infect Immun. 1993;61:314–322. doi: 10.1128/iai.61.1.314-322.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu H-Y, Russell M W. Comparison of systemic and mucosal priming for mucosal immune responses to a bacterial protein antigen given with or coupled to cholera toxin (CT) B subunit, and effects of pre-existing anti-CT immunity. Vaccine. 1994;12:215–222. doi: 10.1016/0264-410x(94)90197-x. [DOI] [PubMed] [Google Scholar]