Abstract
Background:
Early magnetic resonance imaging (MRI) for acute low back pain (LBP) has been associated with increased costs, greater health care utilization, and longer disability duration in workers’ compensation claimants.
Objectives:
To assess the impact of a state policy implemented in June 2010 that required prospective utilization review (UR) for early MRI among workers’ compensation claimants with LBP.
Research Design:
Interrupted time series.
Subjects:
In total, 76,119 Washington State workers’ compensation claimants with LBP between 2006 and 2014.
Measures:
Proportion of workers receiving imaging per month (MRI, computed tomography, radiographs) and lumbosacral injections and surgery; mean total health care costs per worker; mean duration of disability per worker. Measures were aggregated monthly and attributed to injury month.
Results:
After accounting for secular trends, decreases in early MRI [level change: −5.27 (95% confidence interval, −4.22 to −6.31); trend change: −0.06 (−0.01 to −0.12)], any MRI [−4.34 (−3.01 to −5.67); −0.10 (−0.04 to −0.17)], and injection [trend change: −0.12 (−0.06 to −0.18)] utilization were associated with the policy. Radiograph utilization increased in parallel [level change: 2.46 (1.24–3.67)]. In addition, the policy resulted in significant decreasing changes in mean costs per claim, mean disability duration, and proportion of workers who received disability benefits. The policy had no effect on computed tomography or surgery utilization.
Conclusions:
The UR policy had discernable effects on health care utilization, costs, and disability. Integrating evidence-based guidelines with UR can improve quality of care and patient outcomes, while reducing use of low-value health services.
Keywords: low back pain, workers’ compensation, diagnostic imaging, early imaging, evidence-based guidelines, MRI, costs, utilization, time series, policy evaluation
Advancements in technology and radiologic research have resulted in a rapid increase in the use of advanced diagnostic imaging in the last decade.1,2 From 1996 to 2002, utilization of complex diagnostic testing, such as magnetic resonance imaging (MRI), among a national sample of workers’ compensation claimants rose 57%.3 The rise in medical technology innovations is cited as a primary driver of high and increasing health care costs in the United States.4,5 Further, overuse of advanced imaging has been linked to increases in downstream health care utilization.6,7 These trends have prompted health care groups and governmental agencies to implement utilization review (UR) programs that encourage use of clinical practice guidelines while controlling inappropriate imaging utilization and associated costs.2,8,9
Advanced imaging procedures, specifically MRI, are common diagnostic procedures in adults with nonspecific acute low back pain (LBP). Acute LBP is neither anatomically nor histologically characterized, so providing a definite diagnosis is challenging. Although MRI are useful in imaging neurological structures of the back and diagnosing early osteomyelitis, discitis, or hematomas,10 it has relatively low specificity and provides equivocal evidence of structural anomalies that could be attributable to acute LBP.11,12 Because most nonspecific LBP episodes spontaneously resolve within 6 weeks without treatment,13,14 the American College of Radiology (ACR) Appropriateness Criteria for LBP assert for uncomplicated, nonspecific LBP without indication of more severe disease/condition (red flags), “early MRI” (in the first 6 wk of symptoms) is not recommended.15,16
Over the last 15 years, a number of studies have identified extensive overuse of MRI of the lumbar spine for LBP.17 Given that LBP is among the most common occupational injuries, lumbar MRI has been identified as a frequently overused diagnostic imaging test by workers’ compensation systems.18,19 Among Washington State (WA) workers’ compensation claimants with LBP, over one third received an MRI after their injury, with ∼20% receiving an early MRI within the first 6 weeks of injury.20 Early MRI may reveal relatively common neurological abnormalities that are unassociated with LBP, such as disk herniation, which is found in 52% of asymptomatic patients.21 The result is a cascade of care that may not address the true source of pain. Early MRI for LBP is associated with increased health care utilization and costs,22–26 without clear indicators of improved health care outcomes (compared with radiography or later MRI).27,28
In 2009, the state of Washington enacted legislation that formed an advanced imaging management work group tasked with identifying and implementing strategies to improve adherence to clinical practice guidelines for advanced imaging.29 State agencies, such as the Department of Labor and Industries (L&I), were directed to implement strategies to control high-cost, high-use imaging studies, as recommended by the work group. On June 1, 2010, L&I implemented prior authorization based on ACR Appropriateness Criteria to control the rising use of advanced diagnostic imaging, including UR requiring prior authorization. For LBP claims, in the absence of red flags, MRI requests during the first 6 weeks after injury were denied. Before this time, providers treating workers with LBP were not required to follow specific guidelines or send referrals before ordering a lumbar MRI. The L&I UR program resulted in considerable cost savings (advanced imaging costs declined from an estimated $30 million in 2009 to $14 million in 2013).9
The purpose of this study was to evaluate the impact of an advanced imaging UR policy on health care utilization, costs, and disability outcomes among Washington workers with occupational LBP. We hypothesized a decrease in overall health care utilization and costs with no negative effect to worker disability.
METHODS
Data Sources and Study Population
We used administrative and medical claims data from the WA workers’ compensation program, which cover two thirds of all nonfederal Washington workers (the remainder are employed by large, self-insured companies, for whom complete data are unavailable). This population includes workers with occupational injuries that occurred and were treated within Washington. The study included adult claimants (18 y old and above) with accepted claims filed between June 1, 2006 and May 31, 2014 for back sprains or strains based on Occupational Injury and Illness Classification System (OIICS) version 1.01 body part codes 231 (back-lumbar), 233 (back-sacral), and 238 (multiple back regions) and nature codes 021 (sprains or strains of joints, ligaments, muscles, or tendons) and 011 (displacement or dislocation of bone or cartilage). Data were collected for all workers for up to 6 months (183 d) after injury.
Worker and Injury Characteristics
Worker demographic characteristics that were extracted from administrative data included sex and age at the time of injury. Claim (injury) characteristics included body part injured, nature of injury, attorney involvement in the claim (yes, no), and total disability duration in the 6 months postinjury.
Outcome Measures
Medical billing data were used to identify procedure types, dates, providers, and allowed charges for all services associated with the work-related injury claim. A variable indicating the duration of time between injury and first MRI (among workers who received an MRI) was created. Outcomes for this study are separated into 3 major categories: medical costs, utilization, and disability outcomes at 6 months.
Total health care costs included total per-worker allowed costs for medical services in the 6 months postinjury. Costs were adjusted for inflation to 2014 US dollars using Consumer Price Index for Medical Care annual averages.30 The aggregate cost measure was calculated as the mean total cost per claim, attributed to the month of injury.
Utilization measures included the following procedures defined using Current Procedural Terminology, 4th edition codes: lumbar imaging [computed tomography (CT), MRI, or radiography], lumbosacral injections, and lumbar surgery (see Table, Supplemental Digital Content 1, http://links.lww.com/MLR/B562, which lists Current Procedural Terminology, 4th edition codes for utilization measures). Because it is not possible to distinguish whether >1 code per day is attributed to a single or multiple procedures, we counted a maximum of 1 distinct procedure per day. The proportion of workers receiving early MRI, any MRI, surgeries, and injections was calculated for each month. Claims data were used to determine the number of days of disability (wage replacement) benefits to estimate cumulative disability duration (d) in the 6 months after injury and the percent of workers receiving disability benefits.
Statistical Analyses
To examine potential changes in the patient population or injury types which could influence temporal trends in health care costs or utilization, we examined differences in patient demographic and injury characteristics, were compared across in prepolicy and postpolicy time periods using independent t tests. Outcome measures were also examined bivariately across time periods using t tests.
We used interrupted time series models31,32 to evaluate changes in monthly aggregated outcome measures in the prepolicy period (June 2006–May 2010) compared with the postpolicy period (June 2010–May 2014). This approach is the preferred methodology for evaluating the impact of policy change on population-level outcomes, as it accounts for characteristics of autocorrelation and nonstationarity that exist in longitudinal data.33 Interrupted time series analysis allows for evaluation of both changes in level (shift in intercept immediately after the policy change) and trend (change in slope or trend over time, before or after the policy change). Regression estimates are based on the model Yt =βo+β1Tt+β2Xt+β3XtTt+εt where βo represents the intercept (starting level of the outcome variable at the beginning of the series), β1 estimates the trend (trajectory) of the outcome until the policy change in June 2010, β2 represents the shift in the level of the outcome after the policy change, β3 represents the difference between prepolicy and postpolicy trends of the outcome, and β1+β3 estimates the trend of the outcome after the policy change (see Fig., Supplemental Digital Content 2, http://links.lww.com/MLR/B563, for a graphical depiction of coefficients).
Three groups of time series models were constructed to describe changes in outcomes over time: 6 health care utilization models (early MRI, any MRI, CT, radiography, surgery, and injections), 1 health care cost model, and 2 models describing disability duration and the percent of workers receiving disability over time. The models were conducted using the itsa command in Stata (with Newey-West SEs).31 The UR policy was fully implemented on June 1, 2010 (no “phase-in” period), with 48 months duration in each prepolicy and postpolicy time period. To adjust for temporal trends in worker characteristics, monthly aggregated measures for age (mean) and sex (proportion of male claimants) were included. In the health care utilization models, we adjusted for disability (proportion of claimants who received wage replacement compensation). Calendar month was fitted in the models as a possible confounder. We tested for autocorrelation in models using the Cumby-Huizinga general test for autocorrelation in models (using the Stata user-written program actest).34 It showed autocorrelation present at lag of 1 month (P < 0.001), which was incorporated in the models.
As a post hoc sensitivity analysis, we examined the possible influence of a separate UR policy for spinal injections implemented by the Washington Healthcare Authority in June 2011,35 as it may influence the findings in level or trend change associated with the early MRI policy. The post hoc model for injection utilization was constructed as above, with an additional intervention point of June 2011.
All analyses were conducted using in Stata MP/14.2. The University of Washington and Washington State University Institutional Review Boards approved the study.
RESULTS
A total of 77,036 accepted claims for back sprains/strains were identified from June 1, 2006 to May 31, 2014. Among these workers, 912 were excluded from the study for the following reasons: claims only occurred 6 months after injury (N=790), rejected claims (N=6), inconsistent injury dates (N=1), missing sex data (N=5), and hospitalization within 1 week of injury (N=115). The final sample size equaled 76,119 workers. Workers injured in prepolicy years were slightly younger and more frequently male than postpolicy years (Table 1). Injuries were frequently lumbar sprains/strains. T tests comparing aggregated data from prepolicy and postpolicy time periods showed significant differences in monthly mean age and proportions of male workers and sprains/strains (P < 0.01), as well as the proportion of lumbar injuries (P=0.013).
TABLE 1.
Selected Descriptive Statistics for Washington State workers’ Compensation Claimants With Acute Low Back Pain, 2006–2014
| Prepolicy Period (June 2006-May 2010) |
Postpolicy Period (June 2010-Mav 2014) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | 2006/2007 | 2007/2008 | 2008/2009 | 2009/2010 | 2010/2011 | 2011/2012 | 2012/2013 | 2013/2014 |
|
| ||||||||
| No. workers (denominator population) | 11,351 | 12,481 | 9956 | 9947 | 8547 | 8374 | 8057 | 7926 |
| Demographics | ||||||||
| Age (mean) (y) | 37.9 | 38.3 | 38.6 | 39.1 | 39.3 | 39.3 | 39.4 | 39.5 |
| Male (%) | 69.5 | 68.5 | 67.9 | 65.9 | 65.7 | 66.1 | 66.9 | 67.1 |
| Injury characteristics | ||||||||
| Back region injured (%) | ||||||||
| Lumbar | 77.9 | 71.8 | 77.1 | 79.4 | 81.1 | 77.8 | 78.8 | 75.8 |
| Sacral or multiple regions | 22.1 | 28.2 | 22.9 | 20.6 | 18.9 | 22.2 | 21.2 | 24.2 |
| Nature of injury (%) | ||||||||
| Dislocation | 7.7 | 5.8 | 5.8 | 6.2 | 5.3 | 5.0 | 4.5 | 3.9 |
| Sprains or strains | 92.3 | 94.2 | 94.2 | 93.8 | 94.7 | 95.0 | 95.5 | 96.1 |
| Attorney involvement in claim (%) | 4.1 | 4.6 | 5.2 | 5.2 | 5.2 | 5.5 | 4.8 | 4.5 |
Time periods extend from June 1 to May 31; each column above represents 1 year (12 mo).
Health Care Utilization
MRI
Before the policy change, 11.5%–12.8% of workers received early MRI on average, compared with 6.9%–5.2% after the policy was implemented (Table 2). T tests comparing monthly proportions of workers who received early MRI before and after the policy change were statistically significant (P < 0.01). Overall, the mean proportion of workers who received any MRI (irrespective of timing) in the 6 months after injury decreased from 21.2% before the policy change to 15.6% afterwards (P < 0.01). The mean duration between injury and first MRI (among workers who received an MRI) increased from 48.5 days (SD, 42.0; median, 35; interquartile range, 17–68) before the policy to 64.1 days (SD, 44.3; median, 53; interquartile range, 30–90) after the policy (Supplemental Digital Content 3, http://links.lww.com/MLR/B564, depicts mean duration from injury to first MRI before and after the policy).
TABLE 2.
Health Care Utilization, Costs, and Worker Wage Replacement Benefits Before and After the Policy Change Limiting Access to Early MRI for Workers’ Compensation Claimants With Acute, Nonspecific Low Back Pain
| Prepolicy Period (June 2006-Mav 2010) |
Postpolicy Period (June 2010-Mav 2014) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Measures | 2006/2007 | 2007/2008 | 2008/2009 | 2009/2010 | 2010/2011 | 2011/2012 | 2012/2013 | 2013/2014 |
|
| ||||||||
| Imaging | ||||||||
| Early MRI (%)* | 11.5 | 12.5 | 12.0 | 12.7 | 6.9 | 6.7 | 5.6 | 5.1 |
| Any MRI (%)* | 20.1 | 21.0 | 21.5 | 22.0 | 17.1 | 16.2 | 14.6 | 14.0 |
| CT (%) | 1.3 | 1.0 | 1.0 | 1.2 | 0.9 | 1.0 | 1.1 | 1.1 |
| Radiograph (%)* | 12.0 | 11.5 | 11.8 | 12.3 | 14.2 | 15.2 | 15.5 | 14.6 |
| Procedures | ||||||||
| Surgery (%) | 1.6 | 1.8 | 1.6 | 1.7 | 1.8 | 1.7 | 1.5 | 1.2 |
| Injections (%)* | 6.1 | 6.1 | 7.1 | 7.1 | 5.9 | 5.6 | 4.5 | 4.5 |
| Health care costs | ||||||||
| Mean costs ($) | 2775 | 2824 | 3032 | 3241 | 3053 | 2946 | 2820 | 2761 |
| Wage replacement benefits (disability) | ||||||||
| Disability duration (mean) (d)* | 16.1 | 16.2 | 17.4 | 18.6 | 17.4 | 16.1 | 15.7 | 15.1 |
| Worker receiving (%)* | 31.5 | 31.9 | 32.1 | 33.2 | 30.5 | 29.6 | 27.1 | 28.0 |
Time periods extend from June 1 to May 31; each column above represents 1 year (12 mo). Values represent aggregated monthly data summarized by year. Significance is based on comparison of outcomes before and after policy change (independent t tests comparing monthly proportions or means).
CT indicates computed tomography; MRI, magnetic resonance imaging.
P < 0.01.
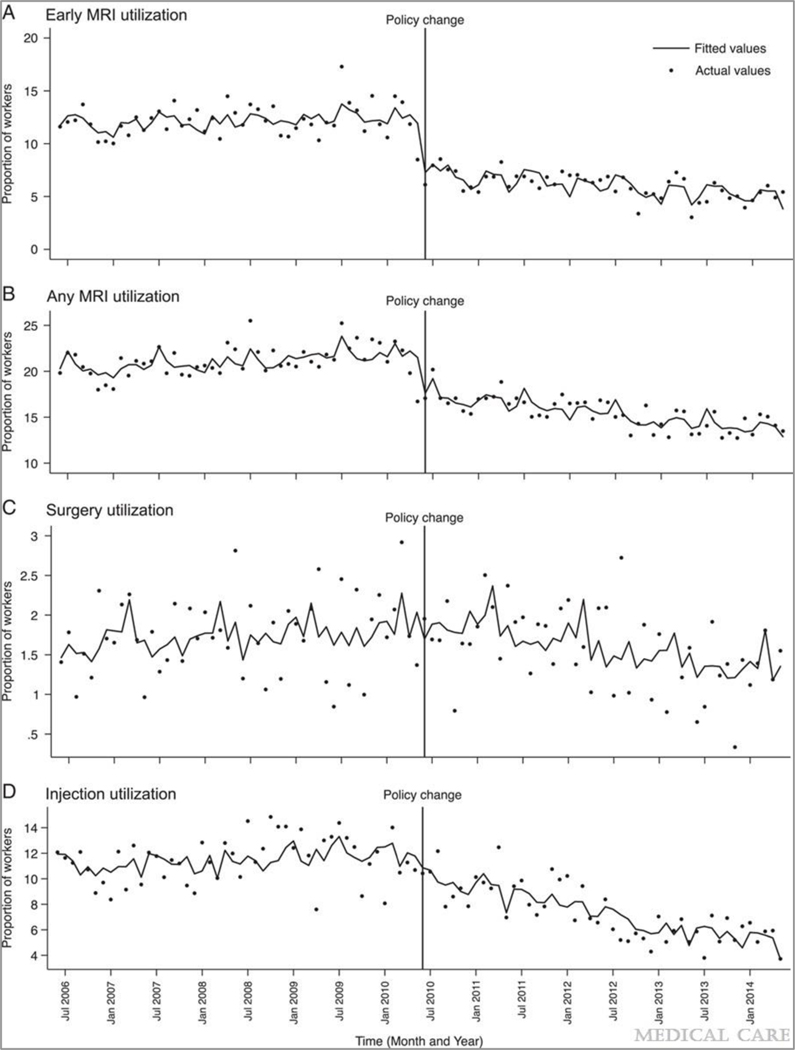
Regression models showed a significant decrease in utilization over time for early MRI and any MRI (Table 3). After policy implementation, the proportion of workers who received early MRI decreased significantly at a rate of 0.04% each month [95% confidence interval (CI), −0.01 to −0.06], compared with the prepolicy trend (Table 3). The change in trend between time periods (β3) was significantly negative, as was the level change after the policy (β2: −5.27; 95% CI, −4.22 to −6.31) (Fig. 1A).
TABLE 3.
Interrupted Time Series Analysis (Segmented Regression Model) Parameters Showing Monthly Trend in Outcomes Before and After Policy Implementation in June 2010
| % (95% CI) |
|||||
|---|---|---|---|---|---|
| Intercept (βo) | Trend Before Policy (β1) |
Level Change After Policy (β2) |
Change in Trend After Policy (β3) |
Trend After Policy (β1+β3) |
|
|
| |||||
| Imaging (% of workers) | |||||
| Early MRI | 28.90 (7.81−50.00)** | 0.03 (−0.02 to 0.08) | −5.27 (−4.22 to −6.31)** | −0.06 (−0.01 to −0.12)* | −0.04 (−0.01 to −0.06)** |
| Any MRI | 32.72 (6.03−59.40)* | 0.03 (−0.03 to 0.10) | −4.34 (−3.01 to −5.67)** | −0.10 (−0.04 to −0.17)** | −0.07 (−0.05 to −0.09)** |
| CT | −5.36 (−13.00 to 2.27) | 0.00 (−0.01 to 0.01) | −0.20 (−0.55 to 0.15) | 0.01 (−0.01 to 0.02) | 0.01 (0.00−0.01) |
| Radiograph | 35.99 (−1.45 to 73.42) | 0.01 (−0.02 to 0.05) | 2.46 (1.24−3.67)** | 0.01 (−0.03 to 0.05) | 0.02 (−0.01 to 0.05) |
| Procedures (% of workers) | |||||
| Surgeries | −2.75 (−13.60 to 8.11) | 0.00 (−0.01 to 0.02) | 0.18 (−0.20 to 0.57) | −0.02 (−0.04 to 0.00)* | −0.02 (−0.01 to −0.02)** |
| Injections | 15.75 (−15.53 to 47.03) | 0.03 (−0.02 to 0.08) | −1.33 (−2.82 to 0.15) | −0.12 (−0.06 to −0.18)** | −0.09 (−0.06 to −0.12)** |
| Health care costs | |||||
| Mean per worker | 5039.49 (2066.70−8012.27)** | 12.06 (7.64−16.48)** | −201.96 (−76.82 to −327.11)** | −18.98 (−13.62 to −24.33)** | −6.91 (−3.76 to −10.01)** |
| Wage replacement benefits (disability) | |||||
| Duration (mean) (d) | 14.14 (−11.94 to 40.22) | 0.07 (0.03−0.10)** | −1.36 (−0.30 to −2.43)* | −0.13 (−0.08 to −0.17)** | −0.06 (−0.03 to −0.09)** |
| % of workers | 6.22 (−18.59 to 31.04) | 0.00 (−0.04 to 0.05) | −2.45 (−0.98 to −3.30)** | −0.08 (−0.02 to −0.13)** | −0.08 (−0.04 to −0.12)** |
Estimates are based on the regression model Yt = βo+β1Tt+β2Xt+β3XtTt+ɛt wherein coefficients are interpreted and reported as the baseline the intercept, or stalling level of the outcome variable at the beginning of the time series (βo), baseline U−end in the outcome measure (β1), the postpolicy trend (β1−β3), the trend change attributable to the policy (comparing prepolicy and postpolicy time periods) (β3), and the change in outcome levels attributable to the policy (β2). Models include covariates representing monthly aggregate measures of claimant sex (proportion male) and age (mean). Utilization and cost models also adjust for the proportion of workers who received wage replacement compensation.
CI indicates confidence interval; CT, computed tomography; MRI, magnetic resonance imaging.
Separate models were estimated for each outcome; significance is designated as follows:
P < 0.05.
P < 0.01.
FIGURE 1.
Utilization of early MRI (A), any MRI (B), lumbosacral surgery (C), and lumbar injections (D) among Washington State workers’ compensation claimants with acute low back sprains and strains from June 1, 2006 to May 31, 2014. MRI indicates magnetic resonance imaging.
The trend in the proportion who received any MRI changed after the policy (Table 3), resulting in a significant deceasing trend of −0.07% (95% CI, −0.05 to −0.09). There was a significant level change in utilization for any MRI immediately following the policy change by −4.34% (β2, 95% CI, −3.01 to −5.67) (Table 3 and Fig. 1B).
Other Imaging Modalities
The proportion of CT imaging did not change across time intervals (Table 2). We observed no significant changes in trend of CT utilization (Table 3). The proportion workers who received radiographs increased over time (Table 2). A significant level change in the utilization of radiographs was observed after the policy, with an increase of 2.46% (95% CI, 1.24–3.67) (Table 3).
Surgery and Injections
Over 96 months, 1184 injured workers underwent at least 1 surgery after injury (1.6%), and the proportion of workers who received surgery was similar before and after the policy change (Table 2). Injections were utilized more frequently (6.0% overall); however, the mean proportion of workers who received injections decreased significantly over time (P < 0.01, Table 2).
Time series models did not show material effects of the early MRI policy on surgery utilization (Table 3) beyond a small decreasing trend in the proportion of workers with surgery after the policy change (β1+β3). The change in trend in the monthly proportion of workers who received injections (β3) was significantly negative after the policy change (compared with the rate beforehand), by −0.12% workers per month (95% CI, −0.06 to −0.18), which influenced the significant decreasing trend in injection utilization after the policy (Table 3). This decrease is discernable graphically (Fig. 1D). Results from the post hoc sensitivity analysis that included an additional intervention timepoint corresponding to the June 2011 injection policy did not materially change our findings of injection utilization (results not shown).
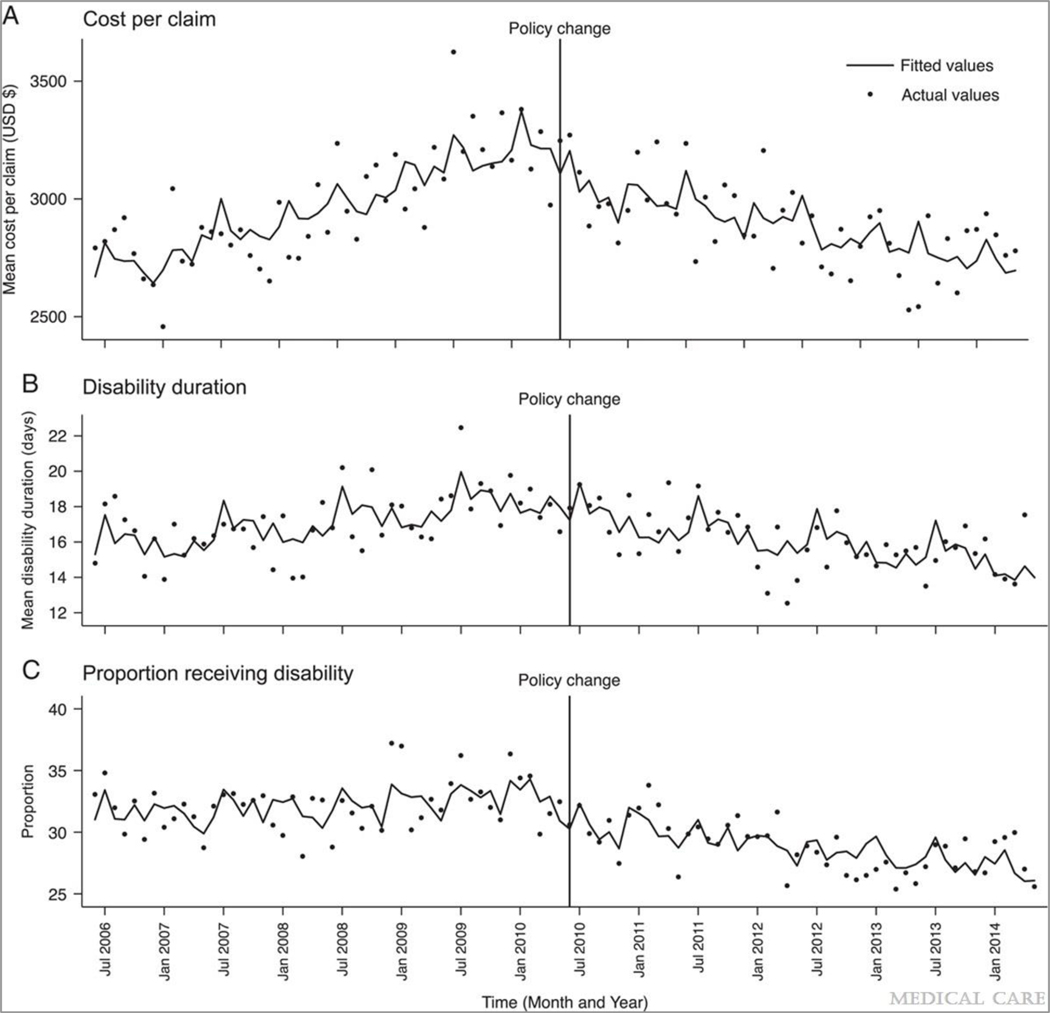
Health Care Costs
Over the 8-year study period, the mean total reimbursed costs per worker was $2928 (SD, 3754). Mean health care costs were slightly higher before the policy change compared with afterwards, although this difference was not statistically significant (Table 2). The changes in mean total claim costs over time reflected in time series analysis indicate a significant, increasing trend in costs over the period before the policy change and a significant negative trend in costs afterwards (Table 3), resulting in a negative change in trend (−6.91, 95% CI,−3.76 to −10.01) (Fig. 2A).
FIGURE 2.
Total costs per workers’ compensation claim (A), mean disability duration (B), and percent of workers receiving disability (C) (wage replacement) benefits among Washington State workers’ compensation claimants with acute low back sprains and strains from June 1, 2006 to May 31, 2014.
Disability Duration
The mean duration of disability (per worker) was 17.1 days before the policy implementation, compared with 16.0 days afterward. The proportion of workers who received disability decreased significantly over time (Table 2). The policy was associated with a significant, negative change in level and trend for mean disability duration and the percent of workers receiving disability (Table 3 and Fig. 2B, C). The mean duration of worker disability decreased by 1.36 days immediately after the policy change, followed by a significant downward trend of −0.06 days per month (Table 3).
DISCUSSION
The rising use of advanced imaging has contributed to mounting health care costs in the United States.4,5 Although guidelines to address overuse of imaging have been developed, such as the ACR Appropriateness Criteria on LBP,15 guidelines and other voluntary efforts alone have not been shown to reduce provider use of inappropriate advanced imaging.36 Approaches to ensuring appropriate care that integrate targeted clinical decision support and utilization “hard stops,” can effectively reduce unnecessary utilization beyond provider education alone.37 Our study examined a statewide policy that required prospective UR and adherence to clinical practice guidelines for use of MRI for workers’ compensation claims for nonspecific, acute LBP,9 which was associated with decreases in imaging and health care costs. The approach described in this study may be of value to state agencies, insurers, provider groups, and health care organizations. Importantly, the utility of this and similar approaches aligns with the mandate from the Centers for Medicare and Medicaid Services (to be implemented in January 2020) requiring use of clinical decision support tools with appropriate use criteria for advanced imaging (including MRI for LBP).38,39
These results are consistent with findings from a prospective cohort study of Washington workers’ compensation claimants, which showed that compared with workers who did not receive early MRI, those who did had significantly higher health care costs and an increased the likelihood of subsequent lumbar injections and surgery.22,23,28 It should be noted that the time period for this study occurred during the Great Recession, during which cost of living adjustments decreased substantially, as did allowed reimbursement amounts for health care services, such as MRI. These changes could contribute to the relatively modest impact on costs.
Advanced imaging utilization has declined nationwide since its peak in the mid-2000s to late-2000s.40 The trends observed in this study may reflect this decline; however, the significant level change in MRI utilization implies a strong association with the UR policy. Also, the trend in MRI utilization did not change prepolicy versus postpolicy, suggesting a limited effect of the policy on the pace of MRI utilization over time. This may be explained by the fact that the policy targeted unnecessary early MRI, not MRI overall. In the workers’ compensation population, early MRI has been commonly cited as an overutilized service.18,19 Restricting utilization of this service could result in an immediate decrease in MRI utilization (and sustained lower rates over time) with no change in the trend over time.
Our findings showed a significant trend change in lumbosacral injection utilization associated with the UR policy change. One year after the early MRI policy implementation, in June 2011, the WA Health Technology Clinical Committee released a guideline limiting coverage for specific types of therapeutic spinal injections.35 The injection policy, while not concurrent with the early MRI policy, could have contributed to the significant negative trend change observed in the postintervention period in this study. However, sensitivity analyses did not indicate this among the worker population. Additional research is needed to examine the effect of the injection policy on a broader population of patients for whom this procedure may be specified.
The findings from this policy evaluation are consistent with these previous studies, illustrating a significant reduction disability duration and percent of workers receiving disability benefits after implementation of the policy (Fig. 2C). Although these changes in disability outcomes appear modest, it is worth noting that this study focused solely on a policy change to limit unnecessary use of imaging. The key to preventing workers’ transition to long-term disability is to avoid over-testing, which may lead to inappropriate interventions, and to implement stepped care management to address the psychosocial barriers to recovery. Proactive interventions involving provider and organizational support and incentives can significantly reduce disability days and costs among workers with back pain.41
Health systems and insurers employ UR programs in an effort to reduce unnecessary care while maintaining health outcomes. The Washington L&I has a history of using evidence-based guidelines to inform UR of high-cost, low-value services.9,42 This study illustrates the integration of evidence-based guidelines and UR into a statewide policy as an informed approach to improving the quality of care of injured workers and preserving limited health care resources.
This study has limitations. First, interrupted time series analyses can control for secular trends in utilization; however, models may not contain unknown or unmeasured confounders temporally related to the policy change.32 Second, this study relied on administrative data that lack detailed information on injury severity and patient outcomes, which may contribute to utilization of services and health care costs. To avoid including severely injured workers in the study, we excluded workers hospitalized at the outset of their injury. We also adjusted for the monthly proportion of workers who received disability benefits (a marker for injury severity) in health care utilization models. Because data in regression models were aggregated at the month-level, including granular individual-level variables was not possible; however, we did control for mean age and proportions of male workers. Nonetheless, it is possible that residual confounding remained. Third, we were unable to examine whether the UR program resulted in changes in quality of care or self-reported health outcomes. However, disability duration is a key workers’ compensation outcome measure to examine whether workers experienced poorer recovery over time. Disability duration is frequently used as a proxy for recovery in workers’ compensation studies and is significantly associated with workers’ expectation of returning to work.43
Despite these limitations, this study has several strengths. First, it is a population-based study with near universal data collection on all paid claims, eliminating the likelihood of dropout due to enrollment changes, as can be the case with claims data. Second, time series analysis is one of the strongest quasiexperimental designs to estimate intervention effects in a nonrandomized setting.44 This analysis structure allows for the controlling of trends in utilization before the policy change and addresses maturation and history biases.32 Pre-post designs, which are often used to evaluate health services programs, do not address these important threats to internal validity.45 Finally, this natural experiment of a statewide policy consisted of the universal implementation of the policy at a single timepoint, without a phase-in period. This allows us to better model and estimate the association between time, intervention point, and outcomes.
Implementation of a mandatory UR program through a state policy can impact the utilization not only of the target care (ie, MRI), but also associated downstream care. Future research could examine the impact of similar UR programs on overutilized services and health care resources, such as pain medication. In addition, given that our data showed a significant level change in lumbar radiographs after the policy change, it may be worthwhile to examine a possible substitution effect for early MRI, with consideration for risks associated with radiation dose.
This study shows a measurable impact of a statewide policy for advanced imaging management within a single-payer workers’ compensation system. Strategies focused beyond the clinical provider, such as patient-centered delivery innovations, may contribute an additional impact and reduction in unnecessary care and improved outcomes.46
Supplementary Material
Acknowledgments
Supported by Centers for Disease Control and Prevention (CDC) National Institute for Occupational Safety and Health (NIOSH) grants 1 R0 OH04069 and 1 T42 OH008433 and Agency for Healthcare Research and Quality (AHRQ) grant R01 HS019222-01. Also supported by the Accident and Medical Aid Funds of the State of Washington, Department of Labor and Industries. Federal funds were received in support of this work. The research funds are targeted toward reducing the incidence and disability related to occupational injuries and illnesses.
J.G.J. reports grants during the conduct of the study from NIH, AHRQ, PCORI, and PhysioSonics (an ultrasound-based technology company), personal fees from HealthHelp (radiology benefits management company), personal fees from UpToDate, and personal fees from Springer Publishing, outside the submitted work. The remaining authors declare no conflicts of interest.
Footnotes
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website, www.lww-medicalcare.com.
REFERENCES
- 1.Iglehart JK. The new era of medical imaging—progress and pitfalls. N Engl J Med. 2006;354:2822–2828. [DOI] [PubMed] [Google Scholar]
- 2.Iglehart JK. Health insurers and medical-imaging policy—a work in progress. N Engl J Med. 2009;360:1030–1037. [DOI] [PubMed] [Google Scholar]
- 3.Shuford H, Restrepo T, Beaven N, et al. Trends in components of medical spending within workers compensation: results from 37 states combined. J Occup Environ Med. 2009;51:232–238. [DOI] [PubMed] [Google Scholar]
- 4.Bodenheimer T. High and rising health care costs. Part 2: technologic innovation. Ann Intern Med. 2005;142:932–937. [DOI] [PubMed] [Google Scholar]
- 5.Mongan JJ, Ferris TG, Lee TH. Options for slowing the growth of healthcare costs. N Engl J Med. 2008;358:1509–1514. [DOI] [PubMed] [Google Scholar]
- 6.Deyo RA. Cascade effects of medical technology. Annu Rev Public Health. 2002;23:23–44. [DOI] [PubMed] [Google Scholar]
- 7.Deyo RA, Mirza SK, Turner JA, et al. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009;22:62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blackmore CC, Budenholzer B. Applying evidence-based imaging to policy: the Washington State experience. J Am Coll Radiol. 2009;6: 366–371. [DOI] [PubMed] [Google Scholar]
- 9.Stockbridge H, d’Urso N. Application and outcomes of treatment guidelines in a utilization review program. Phys Med Rehabil Clin N Am. 2015;26:445–452. [DOI] [PubMed] [Google Scholar]
- 10.Humphreys SC, Eck JC, Hodges SD. Neuroimaging in low back pain. Am Fam Physician. 2002;65:2299–2306. [PubMed] [Google Scholar]
- 11.Johanning E. Evaluation and management of occupational low back disorders. Am J Ind Med. 2000;37:94–111. [DOI] [PubMed] [Google Scholar]
- 12.Sheehan NJ. Magnetic resonance imaging for low back pain: indications and limitations. Ann Rheum Dis. 2010;69:7–11. [DOI] [PubMed] [Google Scholar]
- 13.Pengel LH, Herbert RD, Maher CG, et al. Acute low back pain: systematic review of its prognosis. BMJ. 2003;327:323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waddell G 1987 Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine. 1987;12:632–644. [DOI] [PubMed] [Google Scholar]
- 15.Davis PC, Wippold FJ, Brunberg JA, et al. ACR Appropriateness Criteria on low back pain. J Am Coll Radiol. 2009;6:401–407. [DOI] [PubMed] [Google Scholar]
- 16.Patel ND, Broderick DF, Burns J, et al. ACR appropriateness criteria low back pain. J Am Coll Radiol. 2016;13:1069–1078. [DOI] [PubMed] [Google Scholar]
- 17.Chou R, Quaseem A, Owens DK, et al. Diagnostic imaging for low backpain: advice for high-value health care from the American College of Physicians. Ann Intern Med. 2011;154:181–189. [DOI] [PubMed] [Google Scholar]
- 18.Tacci JA, Webster BS, Hashemi L, et al. Clinical practices in the management of new-onset, uncomplicated, low back workers’ compensation disability claims. J Occup Environ Med. 1999;41:397–404. [DOI] [PubMed] [Google Scholar]
- 19.Clendenin BR, Conlon HA, Burns C. Overuse of diagnostic imaging for work-related injuries. Workplace Health Saf. 2017;65:54–56. [DOI] [PubMed] [Google Scholar]
- 20.Graves JM, Fulton-Kehoe D, Martin DP, et al. Factors associated with early MRI utilization for acute occupational low back pain: a population-based study from Washington State workers compensation. Spine. 2012;37:1708–1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. [DOI] [PubMed] [Google Scholar]
- 22.Webster BS, Choi Y, Bauer AZ, et al. The cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine. 2014;39:1433–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Graves JM, Fulton-Kehoe D, Jarvik JG, et al. Health care utilization and costs associated with adherence to clinical practice guidelines for early magnetic resonance imaging among workers with acute occupational low back pain. Health Serv Res. 2014;49:645–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Webster BS, Bauer AZ, Choi Y, et al. Iatrogenic consequences of early magnetic resonance imaging in acute, work-related, disabling low back pain. Spine. 2013;38:1939–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Webster BS, Cifuentes M. Relationship of early magnetic resonance imaging for work-related acute low back pain with disability and medical utilization outcomes. J Occup Environ Med. 2010;52:900–907. [DOI] [PubMed] [Google Scholar]
- 26.Lurie JD, Birkmeyer NJ, Weinstein JN. Rates of advanced spinal imaging and spine surgery. Spine. 2003;28:616–620. [DOI] [PubMed] [Google Scholar]
- 27.Jarvik JG, Gold LS, Comstock BA, et al. Association of early imaging for back pain with clinical outcomes in older adults. JAMA. 2015;313:1143–1153. [DOI] [PubMed] [Google Scholar]
- 28.Graves JM, Fulton-Kehoe D, Jarvik JG, et al. Early imaging for acute low back pain: one-year health and disability outcomes among Washington State workers. Spine. 2012;37:1617–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Washington State Engrossed Substitute House Bill 2105: diagnostic imaging workgroup. 2009. Available at: https://app.leg.wa.gov/ReportsToTheLegislature/Home/GetBillPdf?displayNumber=2105-S&biennium=2009-10.
- 30.Bureau of Labor Statistics Consumer price index for medical care. 2017. Available at: www.bls.gov/cpi/. Accessed August 28, 2017.
- 31.Linden A Conducting interrupted time-series analysis for single-and multiple-group comparisons. Stata J. 2015;15:480–500. [Google Scholar]
- 32.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27:299–309. [DOI] [PubMed] [Google Scholar]
- 33.Lagarde M How to do (or not to do)… Assessing the impact of a policy change with routine longitudinal data. Health Policy Plan. 2012;27:76–83. [DOI] [PubMed] [Google Scholar]
- 34.Baum C, Schaffer M. ACTEST: Stata module to perform Cumby-Huizinga general test for autocorrelation in time series, Statistical Software Components, S457668: Boston College Department of Economics; revised January 24, 2015. Available at: https://ideas.repec.org/c/boc/bocode/s457668.html. [Google Scholar]
- 35.Brown GT, Goehlert A, Director A, et al. Mind, body and sport: understanding and supporting student-athlete mental wellness. NCAA Publications. 2014. [Google Scholar]
- 36.Rao JK, Kroenke K, Mihaliak KA, et al. Can guidelines impact the ordering of magnetic resonance imaging studies by primary care providers for low back pain? Am J Manag Care. 2002;8:27–35. [PubMed] [Google Scholar]
- 37.Blackmore CC, Mecklenburg RS. Taking charge of imaging: implementing a utilization program. Appl Radiol. 2012;7:18–23. [Google Scholar]
- 38.Centers for Medicare and Medicaid Services. Final policy, payment, and quality provisions in the Medicare physician fee schedule for calendar year 2018. 2017. Available at: www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2017-Fact-Sheet-items/2017-11-02.html. Accessed February 1, 2018.
- 39.Centers for Medicare and Medicaid Services, Department of Health and Human Services. Medicare program; revisions to payment policies under the physician fee schedule and other revisions to part B for CY 2017: appropriate use criteria for advanced diagnostic imaging services. Fed Regist. 2016;81:80403–80428. [Google Scholar]
- 40.Levin DC, Rao VM, Parker L, et al. Bending the curve: the recent marked slowdown in growth of noninvasive diagnostic imaging. Am J Roentgenol. 2011;196:W25–W29. [DOI] [PubMed] [Google Scholar]
- 41.Wickizer TM, Franklin G, Fulton-Kehoe D, et al. Improving quality, preventing disability and reducing costs in workers’ compensation healthcare: a population-based intervention study. Med Care. 2011;49:1105–1111. [DOI] [PubMed] [Google Scholar]
- 42.Javaher SP. Guideline development process in a public workers’ compensation system. Phys Med Rehabil Clin N Am. 2015;26:427–434. [DOI] [PubMed] [Google Scholar]
- 43.Young AE, Besen E, Willetts J. The relationship between work-disability duration and claimant’s expected time to return to work as recorded by workers’ compensation claims managers. J Occup Rehabil. 2017;27:284–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi experimental Designs for Generalized Causal Inference. Boston, MA: Houghton, Mifflin and Company; 2002. [Google Scholar]
- 45.Naci H, Soumerai SB. History bias, study design, and the unfulfilled promise of pay-for-performance policies in health care. Prev Chronic Dis. 2016;13:E82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Colla CH, Mainor AJ, Hargreaves C, et al. Interventions aimed at reducing use of low-value health services: a systematic review. Med Care Res Rev. 2017;74:507–550. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.