Abstract
Background and aims
The mortality rate of stroke has been increasing worldwide. Poststroke somatic dysfunctions are common. Motor function rehabilitation of patients with such somatic dysfunctions enhances the quality of life and has long been the primary practice to achieve functional recovery. In this regard, we aimed to delineate the new trends and frontiers in stroke motor function rehabilitation literature published from 2004 to 2022 using a bibliometric software.
Methods
All documents related to stroke rehabilitation and published from 2004 to 2022 were retrieved from the Web of Science Core Collection. Publication output, research categories, countries/institutions, authors/cocited authors, journals/cocited journals, cocited references, and keywords were assessed using VOSviewer v.1.6.15.0 and CiteSpace version 5.8. The cocitation map was plotted according to the analysis results to intuitively observe the research hotspots.
Results
Overall, 3,302 articles were retrieved from 78 countries or regions and 564 institutions. Over time, the publication outputs increased annually. In terms of national contribution, the United States published the most papers, followed by China, Japan, South Korea, and Canada. Yeungnam University had the most articles among all institutions, followed by Emory University, Fudan University, and National Taiwan University. Jang Sung Ho and Wolf S.L. were the most productive (56 published articles) and influential (cited 1,121 times) authors, respectively. “Effect of constraint-induced movement therapy on upper extremity function 3–9 months after stroke: the Extremity Constraint Induced Therapy Evaluation randomized clinical trial” was the most frequently cited reference. Analysis of keywords showed that upper limbs, Fugl–Meyer assessment, electromyography, virtual reality, telerehabilitation, exoskeleton, and brain–computer interface were the research development trends and focus areas for this topic.
Conclusion
Publications regarding motor function rehabilitation following stroke are likely to continuously increase. Research on virtual reality, telemedicine, electroacupuncture, the brain–computer interface, and rehabilitation robots has attracted increasing attention, with these topics becoming the hotspots of present research and the trends of future research.
Keywords: CiteSpace, VOSviewer, stroke, motor function, rehabilitation
Introduction
Stroke is a cerebrovascular disease typically caused by the rupture or obstruction of blood vessels in the brain. The interruption of blood flow to the brain induces brain tissue damage (Isaacs-Itua and Wong, 2021). The global incidence risk of stroke has been increasing, and stroke has become a major cause of death (Stinear et al., 2020). Motor dysfunction is a common sequela in patients after recovery from stroke, accounting for ~50%–70% of all sequelae (Borges et al., 2018). Motor function is the primary evaluation index and the most critical problem in responding to the complaints of such patients. Improving the motor function of patients is necessary to enhance the quality of life, reduce social effects and socioeconomic expenses, and decrease the incidence of disability. Rehabilitation therapy is frequently used to rehabilitate motor function after stroke (Le Danseur, 2020). Effective rehabilitation strategies can manipulate neuroplasticity to strengthen the motor function of the patients and improve their quality of life (Dimyan and Cohen, 2011). Recently, various treatment methods, including sports, music, and mirror therapies, have gradually been introduced in the rehabilitation of motor function after stroke (Daniel et al., 2021; Saavedra-García et al., 2021; Timmermans et al., 2021). More scientists are focusing on rehabilitating motor function after stroke and have published several articles regarding the same; however, the direction and hotspots of research in this field remain unclear. It is necessary to conduct a bibliographic analysis of research on motor function rehabilitation after stroke to fully utilize the existing research foundation and identify the research hotspots.
The published bibliometric analyses report the temporal trends, geographic distribution, and socioeconomic determinants of scientific production related to cerebrovascular and cardiovascular disease rehabilitation (Ugolini et al., 2013). Furthermore, there exists a bibliometric analysis regarding the effectiveness of rehabilitation treatment and a quantitative analysis regarding exercise interventions for stroke (Feng et al., 2013; Dong et al., 2022) However, to the best of our knowledge, there has been no detailed bibliometric analysis regarding the rehabilitation of motor function after stroke, thereby necessitating qualitative and quantitative analyses on motor function rehabilitation after stroke. Literature metrology is a widely accepted statistical method. It considers the writing framework and estimation qualities the exploration article and uses numerical, factual, and other estimation techniques to depict the collected data and patterns in particular research fields (Osareh, 1996). Recently, bibliometrics have provided clear insights into several biological areas, such as ophthalmic, health information and environmental science fields (Efron, 2021; Kokol et al., 2021; Zhou et al., 2021). However, from a bibliometric perspective, the comprehensive knowledge structure, evolutionary pathways, and research hotspots of motor function rehabilitation after stroke have not been analyzed. Bibliometric research on this topic will complement the existing knowledge regarding motor function rehabilitation after stroke and intuitively provide researchers with visual information and potential research directions, promoting the further development of motor function rehabilitation technologies. Hence, this study performed a statistical analysis of articles related to stroke motor function rehabilitation published in the past 18 years and introduced the basic situation and development trends of motor rehabilitation after stroke, providing direction for further research.
Materials and methods
Data collection
Science Citation Index Expanded of the Web of Science Core Collection (WoSCC) was selected as the source database for data retrieval. WoSCC is an online database contains the standardized and latest reference datasets for scientific study and analysis, with SCIEXPANDED considered the most suitable data bank for bibliometric analysis (Chen et al., 2020; Yao et al., 2020).
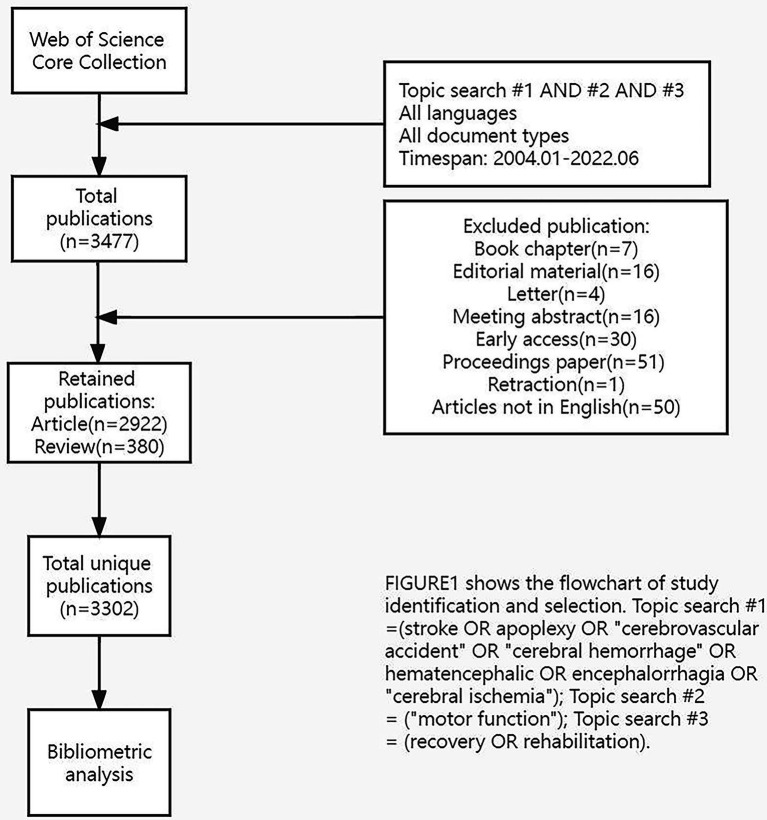
The following were the data retrieval strategies: TS = (stroke OR apoplexy OR “cerebrovascular accident” OR “cerebral hemorrhage” OR hematencephalic OR encephalorrhagia OR “cerebral ischemia”) AND TS = (“motor function”) AND TS = (recovery OR rehabilitation). To eliminate deviations, articles or reviews published from 2004 to 2022 were systematically searched between January 1, 2004 and June 23, 2022, and downloaded in 1 day (June 23, 2022). Some irrelevant literature was excluded, including proceedings papers, early access, and book chapters. In total, 3,302 original English articles (including 2,922 articles and 380 reviews) were screened. The flowchart in Figure 1 illustrates the identification and selection processes of the studies.
Figure 1.
The flowchart of study identification and selection.
The complete records of each article, including publication outputs, research categories, countries/institutions, authors/cocited authors, journals/cocited journals, cocited references, and keywords, were downloaded from the WoSCC database in text format.
Data analysis
We combined the same author names and synonymous keywords and removed any spelling errors. Subsequently, the processed data were imported to CiteSpace version 5.8 and VOSviewer v.1.6.15.0 for bibliometric analysis.
CiteSpace visualizes and analyzes citations and provides an intuitive understanding of the research hotspots and evolution of various areas of a particular field and predicts its future development (Synnestvedt et al., 2005). Instead of focusing on the partial contributions of specific papers, close attention was paid to their academic influence on the overall development of the field. CiteSpace dissected the essential data of the articles, including countries, institutions, cocited references, and reference burst, by producing visual maps. In addition, cocitations and coreferences were visualized to analyze collaborations among the recognized distributions (Dong et al., 2022).
VOSviewer constructs and visualizes bibliometric maps. VOSviewer was primarily used to analyze the bibliometric network, construct a visual organization map, and understand the structural and dynamic development of academic research (Ma et al., 2021). VOSviewer was also used to visually analyze the authors, research categories, countries, journals, keywords, and timelines and identify the frontier hotspots.
Results
Publication trends
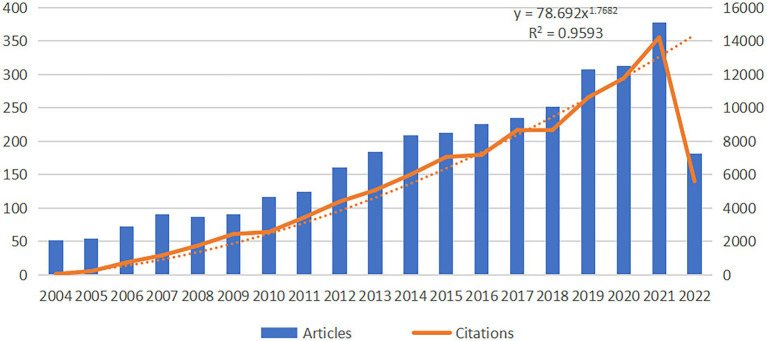
The distribution of articles in every period indicates the general examination patterns in the field. Figure 2 shows that the number of articles on motor function rehabilitation after stroke exhibits an increasing trend yearly. From 2004 to 2009, the number of publication outputs gradually increased. From 2009 to 2021, the number of documents steadily and rapidly increased, indicating that motor rehabilitation after stroke had received particular attention in that timeframe. In 2021, the publication output was 377. Although complete information for 2022 is not yet available, it is estimated that the final data for 2022 will show a rapid growth trend compared to before.
Figure 2.
Annual publication trend of stroke motor function rehabilitation. The data for 2022 is not complete.
Country/region and institution contributions
Overall, 3,302 articles from 78 countries or regions and 564 institutions had been published. As depicted in Table 1, the United States contributed the most papers in this field (953 publications, 28.86%), followed by China (674 publications, 20.41%), implying that the contributions of US and China were significantly more than that of the other countries in this field, followed by Japan (293 publications, 8.87%), South Korea (282 publications, 8.54%), and Canada (222 publications, 6.72%). We used CiteSpace for the visual analysis of the countries or regions (Supplementary Figure S1A). The size of the circle denotes the number of articles distributed by countries or regions, and the line reflects the strength of cooperation between the countries or regions. The purple circle outside the circle represents intermediate centrality. Additionally, cluster analysis was performed for countries or regions (Figure 3A). The size of the circle was directly proportional to the number of articles published in that country/region. The United States had the highest centrality, followed by England, Germany, Canada, Australia, France, Belgium, and Spain. The higher the centrality of a node, the more times it appears in the shortest path of the whole network and greater its influence and significance.
Table 1.
Top 10 countries/regions and institutions related to stroke motor function rehabilitation.
| Rank | Country/Region | Total link strength | Count (%) | Institution | Total link strength | Count (%) |
|---|---|---|---|---|---|---|
| 1 | United States | 527 | 953 (28.86%) | Yeungnam Univ | 32 | 76 (2.30%) |
| 2 | China | 204 | 674 (20.41%) | Emory Univ (United States) | 106 | 66 (1.99%) |
| 3 | Japan | 188 | 293 (8.87%) | Fudan Univ (China) | 36 | 63 (1.91%) |
| 4 | South Korea | 163 | 282 (8.54%) | Natl Taiwan Univ (China) | 139 | 63 (1.91%) |
| 5 | Canada | 160 | 222 (6.72%) | Chang Gung Univ (China) | 119 | 59 (1.79%) |
| 6 | Germany | 157 | 214 (6.48%) | Natl Taiwan Univ Hosp (China) | 132 | 56 (1.69%) |
| 7 | England | 118 | 181 (5.48%) | Univ British Columbia (Canada) | 61 | 49 (1.48%) |
| 8 | Italy | 116 | 169 (5.11%) | Univ Maryland (United States) | 67 | 47 (1.42%) |
| 9 | Taiwan | 93 | 149 (4.51%) | Hong Kong Polytech Univ (China) | 31 | 44 (1.33%) |
| 10 | Australia | 88 | 141 (4.27%) | Sun Yat Sen Univ (China) | 28 | 43 (1.30%) |
Figure 3.
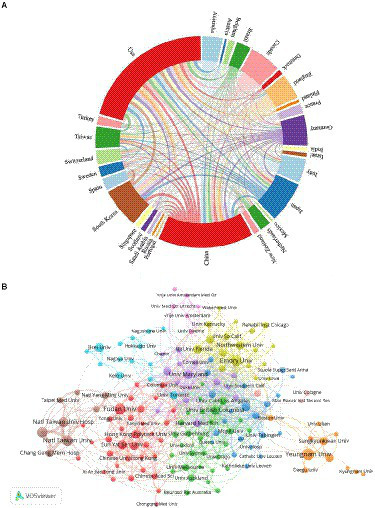
(A) countries/regions clustering analysis; (B) institution’s clustering analysis.
The institutions with the most number of articles are Yeungnam University (76 publications, 2.30%), followed by Emory University (66 publications, 1.99%), Fudan University (63 publications, 1.91%), and National Taiwan University (63 publications, 1.91%). In Supplementary Figure S1B, the size of the circle denotes the number of published articles by an institution. The purple circle represents centrality. Emory University and Harvard University showed high centrality. CiteSpace was also used to visually cluster analyze the institutions and those using keywords were marked. Various tones address various groups. As shown in Supplementary Figure S1C, the largest cluster is #0, labeled “CI therapy,” indicating that this term was used the most by the various institutions, followed by “electroacupuncture” (cluster #1), “telemedicine” (cluster #2), and “rehabilitation robotics” (cluster #3). Other significant groups included “neurorecovery,” “diffusion tensor imaging,” and “psychometrics.” The cluster analysis of the institutions is presented in Figure 3B. The hub size denotes the number of distributions of institutions, and the line represents the cooperation among the institutions. Node colors represent different clusters.
Authors and cocited authors
Altogether, 14,523 authors were associated with publications related to motor function recovery after stroke. Analyzing the authors of the literature enabled us to determine the representative scholars and core research forces in this field. As shown in Table 2, Sung Ho Jang had the largest number of distributed articles (56, 1.69%), followed by Ching-Yi Wu (41, 1.24%) and Keh-Chung Lin (39, 1.18%). Among the top 10 authors, Ching-Yi Wu (81) and Keh-Chung Lin (80) showed high total link strength, which indicated a close cooperative relationship of these authors with other authors. As shown in Figures 4A,B, each circle represents a different author, lines connecting the circles reflect connections between the authors, and variously colored networks of the linkages represent the groups of authors who frequently collaborate. Cocited authors were defined as at least two authors who are referred to in at least one ensuing paper, and they are said to have a cocitation relationship. Seven of the top 10 cocited authors were cited >500 times (Table 2). S. Wolf (1,121) was the most cited author, followed by G. Kwakkel (866) and E. Taub (827). Moreover, as shown in Supplementary Figure S2, the time of publication can be clearly and intuitively observed to understand the research hotspots in real time.
Table 2.
Top 10 authors and co-cited authors related to stroke motor function rehabilitation.
| Rank | Author | Count (%) | Total link strength | Co-cited author | Citation | Total link strength |
|---|---|---|---|---|---|---|
| 1 | Jang Sung Ho | 56 (1.69%) | 63 | Wolf Sl | 1,121 | 23,158 |
| 2 | Wu Ching-Yi | 41 (1.24%) | 81 | Kwakkel G | 866 | 18,728 |
| 3 | Lin Keh-Chung | 39 (1.18%) | 80 | Taub E | 827 | 17,892 |
| 4 | Wolf Steven L. | 37 (1.12%) | 73 | Fuglmeyer Ar | 694 | 11,946 |
| 5 | Kim Yun-Hee | 25 (0.75%) | 53 | Page Sj | 657 | 16,488 |
| 6 | Taub Edward | 25 (0.75%) | 73 | Duncan Pw | 556 | 10,509 |
| 7 | Winstein Carolee J. | 24 (0.72%) | 43 | Ward Ns | 504 | 12,209 |
| 8 | Uswatte Gitendra | 23 (0.69%) | 72 | Stinear Cm | 496 | 11,750 |
| 9 | Boyd Lara A. | 22 (0.66%) | 24 | Liepert J | 469 | 12,636 |
| 10 | Cohen Leonardo G. | 22 (0.66%) | 30 | Nudo Rj | 462 | 10,270 |
Figure 4.
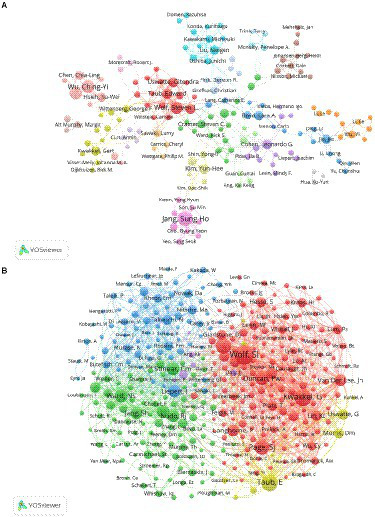
(A) Co-author related to stroke motor function rehabilitation; (B) co-cited author related to stroke motor function rehabilitation.
Research categories
The category graph generated using CiteSpace showed 113 nodes, suggesting that the field of study involves 113 categories. Moreover, the hub size represents the recurrence of the event, the lines between them denote the strength of the association, and the purple circle represents centrality (Figure 5A). The most frequently occurring and extensive classification was neuroscience, with a recurrence of 400, followed by rehabilitation (315 distributions). Other frequent categories include clinical neurology (231 distributions), sports sciences (195 distributions), and science and technology (193 distributions). Moreover, in the overlay of the dual map of research publishing in journals (Figure 5B), the left half of the diagram depicts the referring to diaries, the right half depicts the referred to diaries, and the bends constitute the reference lines that ultimately depict the reference setting. More articles a diary distributes, more extended the upward pivot of the oval, and the more writers, the more extended the event hub of the circle. We found six predominantly cited pathways (color orange, pink), showing that studies published in molecular, biological and genetic journals and in psychology, education and social science journals were predominantly cited by studies published in molecular, biological and immunological journals.
Figure 5.
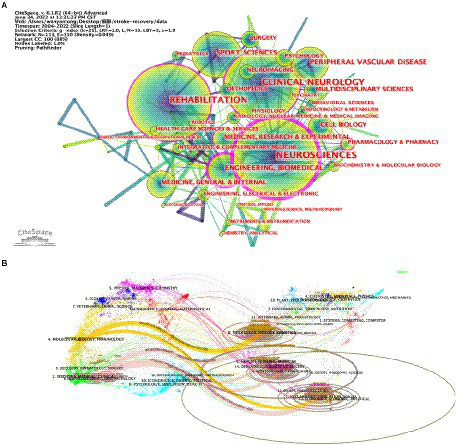
Category network map in the field of stroke motor function rehabilitation: (A) publication distribution among different categories; (B) dual-map overlay of journal publishing research.
Journals and coreferred scholarly periodicals
In total, 3,302 articles were distributed in 595 journals related to motor recovery after stroke. The distributed diaries were visually examined via VOSviewer programming. As presented in Table 3, the journal Neurorehabilitation and Neural Repair had the most number of articles (184, 5.57%), followed by Archives of Physical Medicine and Rehabilitation (100, 3.02%). Of the top 10 journals, Stroke (10.17) had the highest impact factor (IF). Of the top 10 coreferred to journals (Table 3), Stroke had the highest number of citations (11,443), indicating that the journal had important implications for motor function recovery after stroke, followed by Archives of Physical Medicine and Rehabilitation (6,427) and Neurorehabilitation and Neural Repair (6,321). The influence of journals depends on the number of joint citations. Additionally, more than half the journals belonged to Q1. As shown in Figures 6A,B, each circle represents a journal; the size of the circle depends on the strength of connection and number of references. The color of the circle denotes the different groups to which the journals belong, with the various bunches representing various categories. We can observe information, such as cooperation among journals, using this figure. The journals Stroke, Archives of Physical Medicine and Rehabilitation, and Neurorehabilitation and Neural Repair have more co-citations and greater influence. Figure 6C shows the number of journal publications, citation frequency, and overall strength of links over time, with larger circles indicating higher citation frequencies and darker colors indicating higher overall strength of links. Neurorehabilitation and Neural Repair has been cited frequently and has the highest total link strength.
Table 3.
Top 10 journals and co-cited journals related to stroke motor function rehabilitation.
| Rank | Journal | Count (%) | IF (2022) | JCR | Co-cited journal | Citation | IF (2022) | JCR |
|---|---|---|---|---|---|---|---|---|
| 1 | Neurorehabilitation and Neural Repair | 184 (5.57%) | 4.895 | Q2 | Stroke | 11,170 | 10.17 | Q1 |
| 2 | Archives of Physical Medicine and Rehabilitation | 100 (3.02%) | 4.06 | Q1 | Arch Phys Med Rehab | 6,427 | 4.06 | Q1 |
| 3 | Journal of Neuroengineering and Rehabilitation | 97 (2.94%) | 5.208 | Q2 | Neurorehab Neural Re | 6,321 | 4.895 | Q2 |
| 4 | Frontiers in Neurology | 96 (2.91%) | 4.086 | Q2 | Brain | 3,336 | 15.255 | Q1 |
| 5 | Stroke | 81 (2.45%) | 10.17 | Q1 | J Neurosci | 2,986 | 6.709 | Q1 |
| 6 | Topics in Stroke Rehabilitation | 78 (2.36%) | 2.177 | Q3 | Neuroimage | 2,836 | 7.4 | Q1 |
| 7 | Restorative Neurology and Neuroscience | 77 (2.33%) | 2.976 | Q3 | Clin Rehabil | 2,634 | 2.884 | Q2 |
| 8 | Neural Regeneration Research | 65 (1.96%) | 6.058 | Q2 | Phys Ther | 2,388 | 3.14 | Q1 |
| 9 | Journal of Stroke & Cerebrovascular Diseases | 62 (1.88%) | 2.677 | Q4 | Neurology | 2,128 | 11.8 | Q1 |
| 10 | Plos One | 57 (1.73%) | 3.752 | Q2 | Clin Neurophysiol | 2,006 | 4.861 | Q2 |
Figure 6.
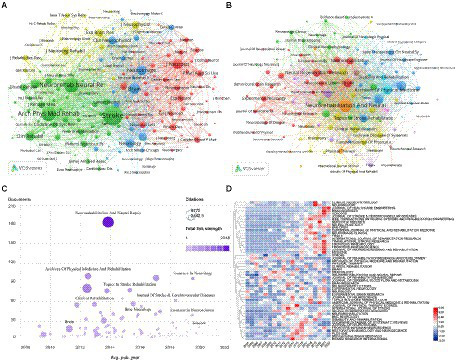
(A) Co-cited journals related to stroke motor function rehabilitation; (B) Journals related to stroke motor function rehabilitation; (C) number of journal publications, frequency of citations, total link strength over time; (D) journals heat map on stroke motor function recovery.
Furthermore, we conducted a comparative analysis of the popularity of the journals (Figure 6D). Each line was compared with the one another. The value in the box denotes the number of articles distributed in the journal divided by the number of articles distributed per year, thereby representing the prevalence of the diary in the ongoing year. The popularity of the journals was illustrated using a heat map, wherein the intensity of the red color was used to indicate the popularity of a journal in a given year. Through this heat map, shifts in the exploration course, accentuation in this field, and developmental trends could be determined. For example, in 2014 and 2015, articles were mainly published in Biome Research International and Journal of Physical Therapy Science. From 2016 to 2020, several articles were published in Clinical Neurophysiology, Neuroreport, and Scientific Reports. From 2019 to 2022, Medicine, Journal of Neuroengineering and Rehabilitation, Translational Stroke Research, Sensors, Brain Sciences, and Journal of Healthcare Engineering had several publications. The direction of research in this field was observed to gradually shift from physical therapy to neurorehabilitation and neuroscience.
Cocited references and reference burst
Of the 3,302 retrieved documents, the top 15 most frequently cited documents are presented in Table 4. “Effect of constraint-induced movement therapy on upper extremity function 3 to 9 months after stroke: the EXCITE randomized clinical trial” is the most frequently cited reference (1,303 citations). The main content of this paper is a prospective, single-blind, randomized, multisite clinical trial—EXCITE trial. The study reported that 2 weeks of CIMT improved upper-limb function in patients more than 1 year after stroke for at least a year. “Influence of interhemispheric interactions on motor function in chronic stroke” is the second most frequently cited reference (1,014 citations). This paper explored the interaction between the hemispheres during the autonomic development of deadened hands in patients with ongoing subcortical stroke and new corpus callosum. The third was Effects of robot-assisted therapy on upper limb recovery after stroke: A systematic review (948 citations), which was a systematic review of studies on the effects of robot-assisted therapy on motor and functional recovery in stroke patients.
Table 4.
Top 15 co-cited references related to stroke motor function rehabilitation.
| Rank | Author | Title | Source | Citation | Year | DOI |
|---|---|---|---|---|---|---|
| 1 | Wolf, SL, et al. | Effect of constraint-induced movement therapy on upper extremity function 3–9 months after stroke – The EXCITE randomized clinical trial | JAMA-J AM MED ASSOC | 1,303 | 2006 | 10.1177/1545968307305457 |
| 2 | Murase, N, et al. | Influence of interhemispheric interactions on motor function in chronic stroke | ANN NEUROL | 1,014 | 2004 | 10.1056/NEJMoa0911341 |
| 3 | Kwakkel, G, et al. | Effects of robot-assisted therapy on upper limb recovery after stroke: A systematic review | NEUROREHAB NEURAL RE | 948 | 2008 | 10.1177/1545968307305457 |
| 4 | Lo, AC, et al. | Robot-Assisted Therapy for Long-Term Upper-Limb Impairment after Stroke | NEW ENGL J MED | 856 | 2010 | 10.1056/NEJMoa0911341 |
| 5 | Hummel, F, et al. | Effects of non-invasive cortical stimulation on skilled motor function in chronic stroke | BRAIN | 827 | 2005 | 10.1093/brain/awh369 |
| 6 | Laver, KE, et al. | Virtual reality for stroke rehabilitation | COCHRANE DB SYST REV | 701 | 2011 | 10.1002/14651858.CD008349.pub2 |
| 7 | Lindvall, O, et al. | Stem cells for the treatment of neurological disorders | NATURE | 631 | 2006 | 10.1038/nature04960 |
| 8 | Maciejasz, P, et al. | A survey on robotic devices for upper limb rehabilitation | J NEUROENG REHABIL | 618 | 2014 | 10.1186/1743-0003-11-3 |
| 9 | Hummel, FC, et al. | Non-invasive brain stimulation: a new strategy to improve neurorehabilitation after stroke? | LANCET NEUROL | 581 | 2006 | 10.1016/S1474-4422(06)70525-7 |
| 10 | Veerbeek, JM, et al. | What Is the Evidence for Physical Therapy Poststroke? A Systematic Review and Meta-Analysis | PLOS ONE | 575 | 2014 | 10.1371/journal.pone.0087987 |
| 11 | Clarkson, AN, et al. | Reducing excessive GABA-mediated tonic inhibition promotes functional recovery after stroke | NATURE | 570 | 2010 | 10.1038/nature09511 |
| 12 | Ramos-Murguialday, A, et al. | Brain-Machine Interface in Chronic Stroke Rehabilitation: A Controlled Study | ANN NEUROL | 543 | 2013 | 10.1002/ana.23879 |
| 13 | Carter, AR, et al. | Resting Interhemispheric Functional Magnetic Resonance Imaging Connectivity Predicts Performance after Stroke | ANN NEUROL | 530 | 2010 | 10.1002/ana.21905 |
| 14 | Zhou, HY, et al. | Human motion tracking for rehabilitation-A survey | BIOMED SIGNAL PROCES | 472 | 2008 | 10.1016/j.bspc.2007.09.001 |
| 15 | Saposnik, G, et al. | Effectiveness of Virtual Reality Using Wii Gaming Technology in Stroke Rehabilitation A Pilot Randomized Clinical Trial and Proof of Principle | STROKE | 464 | 2010 | 10.1161/STROKEAHA.110.584979 |
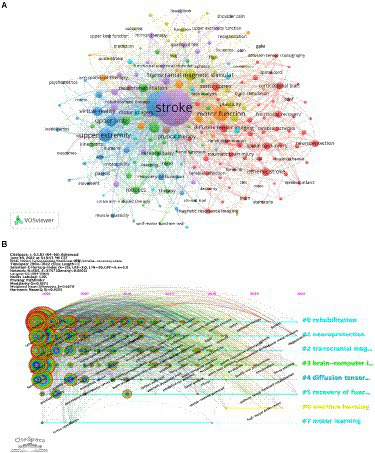
Coreference implies that at least two articles are referred to at the same time in at least one report, and the two articles are co-references. Likewise, the bunching capability of CiteSpace to fabricate a visual guide to group the coreference writings was utilized and the recovered written works were partitioned into 15 bunches via group examination (Figures 7A,B). Each cluster is closely linked and collaborates in specific areas. The seclusion Q is 0.7107, whereas the typical weighted outline is 0.8722, showing that the bunching structure is steady and has high certainty and persuasiveness. From purple to yellow, Figure 7B depicts the time dimension, which also represents the shift of research focus and direction. The biggest cluster was #0, labeled “virtual,” followed by “cerebrovascular” (cluster #1), “constraint-induced movement therapy” (cluster #2), and “prognosis” (cluster #3). Other important clusters include “cortical reorganization,” “repetitive,” “transcranial magnetic stimulation,” and “transcranial direct current stimulation.”
Figure 7.
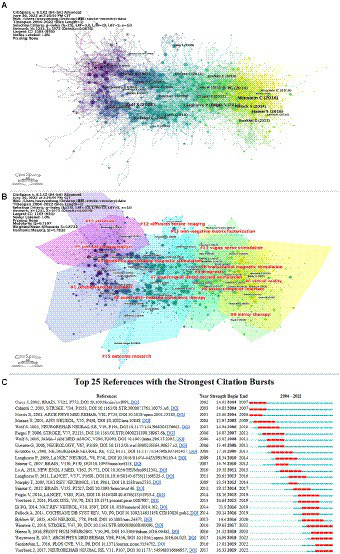
(A) Co-cited references related to stroke motor function rehabilitation; (B) cluster view of co-cited references in stroke motor function rehabilitation research; (C) CiteSpace visualization map of top 25 references with the strongest citation bursts involved in stroke motor function rehabilitation.
This study further analyzed the prominent literature. Figure 7C shows the main 25 articles with the most grounded burst force and ranks them in chronological order. In Figure 7C, the research hotspots and time duration can be effectively observed. A large portion of the cocited literature has been referred to in the past 10 years, demonstrating that future examination on stroke may steadily increase.
Key topics of research hotspots
Cluster analysis
Clustering keywords, summarizing research themes, and performing cluster analysis are helpful for understanding the research hotspots. The keywords were grouped using VOSviewer, with circles and labels forming a single unit in the Figure 8A and different colored units representing different clusters. As displayed in Figure 8A, seven clusters are available, each representing seven different search directions. The following are the fundamental catchphrases of the red cluster: diffusion tensor imaging, motor cortex, corticospinal tract, spinal cord injury, and ischemic stroke. The main keywords of the purple cluster include stroke transcranial magnetic stimulus, robot-assisted therapy, and mirror therapy. The keywords of the blue cluster are upper extremity and virtual reality and those of the green cluster are neurorehabilitation and robotics. Other keywords also include motor function and transcranial magnetic stimulus. This indicates the research hotspots and provides some guidance for future researchers.
Figure 8.
(A) Cluster view of keywords in stroke motor function rehabilitation research; (B) CiteSpace visualization map of timeline viewer related to stroke motor function rehabilitation research.
Timeline analysis
Figure 8B depicts a timeline analysis based on VOSviewer mapping software, which intuitively shows the phased research hotspots and development directions of stroke motion recovery from the time dimension. From 2004 to 2012, coordination, traumatic brain injury, cortical activation, assisted therapy, double-blind, randomized trials, guidelines, mirror movement, and other keywords have been widely researched. From 2012 to 2020, research mainly focused on emerging rehabilitation methods of motor function after stroke, and the main keywords used were rehabilitation robotics, brain–computer interface, aerobic exercise, muscle spasm, virtual reality, ankle–foot orthosis, and paired associative stimulation. The interest in studying Fugl-Meyer assessment and exoskeleton began in 2020 and lasted until 2022.
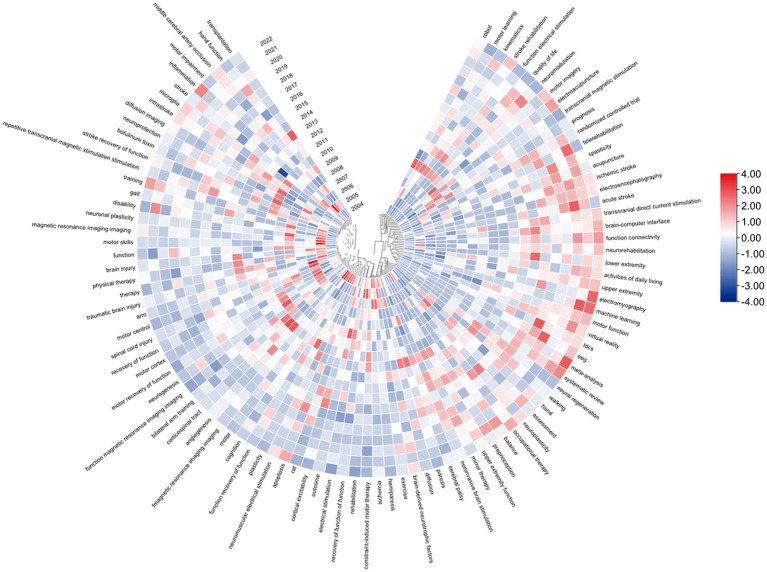
Explosion detection
Catchphrase burst identification alludes to detecting high-frequency keywords for some time, which assists scientists to break down the advancement of examination on the recuperation of motor function after stroke. According to Table 5, excluding “stroke” (1,754), the keywords with high frequency in this study were “rehabilitation” (811), “upper extremity” (390), “motor function” (259), “hemiparesis” (177), and “transcranial magnetic stimulation” (171), suggesting that these fields were the research hotspots. To further visualize the popularity of the keywords, a heat map of the keywords is presented in Figure 9. The value of each grid is divided by the frequency of occurrence by the number of articles distributed annually because as this field shows a rapid growth trend, if only the frequency of occurrence is used, it will produce an error in the number of articles and misjudgment of the popular keywords in that year. As depicted in Figure 8B, changes in future research topics can be intuitively predicted using keywords. Additionally, in Figure 8B, the outer circle denotes the keyword, and the line denotes time. A box replaces the burst intensity of each keyword. The redder the color, more popular the keyword in a particular year. For example, in 2022, the keywords with redder colors were systematic review meta-analysis, machine learning, and electromyography. The popular keywords in recent years are virtual reality, EEG, machine learning, and acute stroke. We can predict that the future research hotspots may be in these areas.
Table 5.
Top 20 keywords related to stroke motor function rehabilitation.
| Rank | Keyword | Occurrences | Total link strength | Rank | Keyword | Occurrences | Total link strength |
|---|---|---|---|---|---|---|---|
| 1 | Stroke | 1,754 | 4,560 | 11 | Neurorehabilitation | 102 | 365 |
| 2 | Rehabilitation | 811 | 2,403 | 12 | Robot | 87 | 360 |
| 3 | Upper extremity | 390 | 1,258 | 13 | Virtual reality | 84 | 348 |
| 4 | Motor function | 259 | 723 | 14 | Constraint-induced movement therapy | 82 | 271 |
| 5 | Hemiparesis | 177 | 547 | 15 | Ischemic stroke | 79 | 167 |
| 6 | Transcranial magnetic stimulation | 171 | 537 | 16 | Neuroplasticity | 73 | 206 |
| 7 | Motor recovery | 148 | 408 | 17 | Plasticity | 70 | 208 |
| 8 | Recovery of function | 141 | 448 | 18 | Diffusion | 69 | 353 |
| 9 | Stroke rehabilitation | 130 | 337 | 19 | Repetitive transcranial magnetic stimulation | 64 | 253 |
| 10 | Magnetic resonance imaging | 124 | 361 | 20 | Corticospinal tract | 62 | 217 |
Figure 9.
Keywords heat map on stroke motor function recovery.
Discussion
Global trends
This study conducted a bibliometric analysis of motor function rehabilitation after stroke from 2004 to 2022. An annual increase in the number of papers and citations published in the journal was observed. The most significant growth period was noted from 2020 to 2021, with the highest number of publications in 2021(Figure 2). Furthermore, research related to motor function rehabilitation after stroke is expected to continue increasing in the future.
In terms of refereed journals, among the top 10 journals, 20%, 50%, 20%, and 10% were Q1, Q2, Q3, and Q4, respectively. Neurorehabilitation and Neural Repair was cited the most (9,770 times). One of the top 10 journals had an IF of more than 10 (Stroke). Three journals had an IF of 1–3 (Thomas In Stroke Rehabilitation, Restorative Neurology and Neuroscience, and Journal of Stroke & Cerebrovascular Diseases), four journals had an IF of 3–5 (Neurorehabilitation and Neural Repair, Archives of Physical Medicine and Rehabilitation, Frontiers in Neurology, and PLOS One), and two journals had an IF of 5–10 (Journal of Neuroengineering and Rehabilitation and Neural Regeneration Research; Table 3). These results suggest that the quality of research on motor function rehabilitation after stroke is relatively high. The United States (953) was the most significant contributor to the number of papers published in the above mentioned journals, with China (674) and Japan (293) closely behind. Furthermore, the United States had the greatest total link strength (527) and the most citations (45,080). In terms of traditional institutions, the largest cluster was labeled “CI therapy,” followed by “electroacupuncture,” “telemedicine,” and “rehabilitation robotics” (Supplementary Figure S1C). CI therapy, also known as CIMT, is a neurorehabilitation therapy aimed at recuperating the function of an affected limb after stroke. The affected limb is forced to be used instead of the healthy one (Wang et al., 2022). Many studies have confirmed the efficacy of CIMT in improving limb motor function (Ju and Yoon, 2018; Wang et al., 2022). Electroacupuncture therapy combines traditional Chinese medicine acupuncture therapy and Western medicine rehabilitation therapy. When electroacupuncture is applied to both antagonistic and active muscles in patients with spasms after stroke, the intermittent wave improves the excitability of the muscle tissue. The short-term application of low-frequency, continuous waves can also excite the muscles. However, its long-term application can inhibit the sensory and motor nerves (Zhang et al., 2022). Telerehabilitation is developed based on telemedicine owing to the development of telecommunication and information technology (Nikolaev and Nikolaev, 2022). Telecommunication technology, rehabilitation diagnostics, and treatment methods are used to provide rehabilitation services to patients in families, communities, or remote areas (Chumbler et al., 2012). Telerehabilitation is a promising rehabilitation treatment and a realistic choice to deal with coronavirus disease 2019 (COVID-19; Maresca et al., 2020; Suso-Martí et al., 2021). The concept of rehabilitation robotics was developed in engineering. It combines the latest technologies with rehabilitation medicine. Multiple rehabilitation robots are being developed, including upper- and lower-limb rehabilitation robots (Bernhardt and Mehrholz, 2019; Rodgers et al., 2019). Owing to its advantages in improving rehabilitation efficiency, ensuring rehabilitation quality, and reducing human costs, it has gradually become a research hotspot locally and internationally (Morone et al., 2017).
Research hotspots and frontiers
Articles on motor function rehabilitation after stroke covered several areas, among which rehabilitation, neuroscience, and clinical neurology were the most popular. Other areas included sports sciences, peripheral vascular disease, engineering biomedical, cell biology, medicine, and multidisciplinary sciences, indicating that motor function recovery after stroke is a complex issue warranting multidisciplinary intervention (Figure 5).
One of the most significant factors during the assessment of the quality of research of motor function rehabilitation after stroke is the number of citations. This can help identify the interest areas in the research. After the top 15 frequently cited literature were read and analyzed, the results showed that CIMT, robot-assisted therapy, noninvasive brain stimulation, virtual reality, stem cells, physical therapy, and brain–machine interface were widely concerned by researchers at a particular period in this field (Table 4). The following are the most cited papers that highlight the various research hotspots related to the rehabilitation of patients with stroke. One of these is a multicenter randomized controlled study that reported that rehabilitation using robotic-assisted technology significantly improved the outcomes of patients with long-term extremity dysfunction (Lo et al., 2010). A systematic review of 19 studies involving 565 individuals showed that interactive video games and virtual reality improved activities of daily living functions (Laver et al., 2011). A study involving patients with chronic stroke revealed that training the brain using computer-assisted technology improved motor function. This could form the basis of a new therapeutic approach for treating neurological disorders (Ramos-Murguialday et al., 2013). In the highly cited literature, the main research directions closely correlate to the rehabilitation methods, among which the intelligent rehabilitation technology is the most popular.
A sudden increase in the number of citations of a paper indicates that the paper focuses on a vital issue in the field, known as burst reference. Veerbeek et al. (2017), Santisteban et al. (2016), Woytowicz et al. (2017), Hatem et al. (2016), and Winstein et al. (2016) were the top five strongest burst references in the last 5 years (Figure 7C). A meta-analysis systematically reviewed the impact of robot-assisted treatment on motor function and activities of daily living of the paralyzed arm (Veerbeek et al., 2017). A review showed that Fugl–Meyer assessment was the most commonly used measurement method (Santisteban et al., 2016). A study quantified the upper extremity motor deficits in patients with chronic stroke using cluster analysis of the Fugl–Meyer findings (Woytowicz et al., 2017). A systematic review summarized emerging interventions, including virtual reality, robot-assisted training, and noninvasive brain stimulation (Hatem et al., 2016). This is consistent with most of the previous research hotspots of institutional clustering. The fifth strongest burst reference is the growth-up stroke restoration and recuperation rule (Winstein et al., 2016). In 5 years, except for one guideline, burst references were connected with upper-limb motor function, two with upper-limb motor function assessment, and two with upper-limb motor function rehabilitation methods. Hence, research on the motor function of the upper limb has been popular in the last 5 years. Moreover, this emphasizes the need to reach a worldwide consensus regarding optimal assessment methods of motor function after stroke. The challenge now is to develop evidence-based treatment protocols for different patients.
Clustering analysis of keywords revealed that among the top 10 keywords, alongside the words related to the retrieval words, the study in this field mainly revolved around the upper limbs (top 3), transcranial magnetic stimulation (top 6), and magnetic resonance imaging (top 10; Table 5). Transcranial magnetic stimulation is used for various functional assessments and treatments of the nervous system. It has been proven effective in promoting motor recovery in patients with stroke (Bai et al., 2022). It acts on the central nervous system, changes the membrane potential of cortical neurons, and causes corresponding physiological and biochemical reactions. Magnetic resonance imaging is a standard imaging examination in patients with stroke. Upper limbs and noninvasive brain stimulation are also hot topics in burst literature, indicating that these hotspots will remain popular for some time. Subsequently, combined with timeline analysis and burst detection, an overall understanding of the research progress and future directions of motor function recovery after stroke can be formed, with Fugl–Meyer assessment, electromyography, exoskeleton, home training, telemedicine, and virtual reality becoming the new hot words from 2019 onward (Figures 8B, 9). The main contents are as follows.
Motor function evaluation after stroke
The Fugl–Meyer assessment is widely used to assess sensorimotor function after stroke (Santisteban et al., 2016), and electromyography is a popular tool for measuring muscle activity (Cè et al., 2020). Owing to the COVID-19 pandemic, the motor function of several patients with stroke required to be assessed online. Thus, Pérez-Robledo et al. (2022) designed an online Spanish version of the Fugl–Meyer assessment scale. Because the scoring and action guidance of the Fugl–Meyer assessment scale require the participation of professional rehabilitation therapists and the evaluation is difficult to perform at home, Shen and Liu (2022) proposed a video-based Fugl–Meyer assessment system, allowing users to use a camera for at-home Fugl–Meyer assessment. Yamamoto et al. (2020) conducted a cross-sectional study to explore the connection between the results of the upper extremity Fugl–Meyer scale and motor function scores of Functional Independent Measure. Cecchi et al. (2021) developed an Italian version of the Fugl–Meyer assessment by transcultural interpretation and approval. Suponeva et al. (2021) reported high sensitivity, reliability, and validity of the Russian version of the Fugl–Meyer assessment. Rech et al. (2020) concluded that the Fugl–Meyer assessment could be used to assess the quality of motor performance in patients with chronic stroke and different degrees of functional impairment owing to the consistency of the scores as determined with instrumental kinematic measures. Formstone et al. (2021) used a new combination of wearable inertial and mechanical mapping sensors to quantify motor function after stroke, demonstrating that the results of Fugl–Meyer assessment were consistent with those of the mapping sensors. Pan et al. (2021) quantitatively assessed motor function in patients with stroke by collecting surface electromyography (sEMG) signals and inertial sensor data during the voluntary upward reach of the upper extremity. As evidenced by new publications in the last 3 years, the Fugl–Meyer scale has been widely used worldwide. Ongoing research has linguistically and culturally adapted the Fugl–Meyer assessment and confirmed its validity, reliability, and sensitivity. Simultaneously, owing to the outbreak of the COVID-19 pandemic, some studies have proposed online versions of the Fugl–Meyer scale and a video-based Fugl–Meyer assessment system that does not require the involvement of therapists. However, the Fugl–Meyer scale still has some shortcomings, including the imprecision of the scale itself and the variability between different assessors (Formstone et al., 2021). Quantitative assessment of motor function is extremely significant for patients after stroke because it can be used to develop a more precise rehabilitation treatment plan (Pan et al., 2021). Therefore, many automation systems have been proposed for empirical quantification of motor assessments; however, they are insufficient. Clinical practice based on this aspect is required in the future to provide a premise for the broad clinical reception of automated and quantitative instrument applications in poststroke motor assessments.
Electromyography can quantitatively and qualitatively analyze the neuromuscular function of target muscles by collecting surface signals during muscle activity and speculating on the damage extent and nature of target muscles, thereby offering noninvasive and real-time measurements (Cè et al., 2020; Feldner et al., 2021; Fujita et al., 2021; Papazian et al., 2021). Liu et al. (2022) combined sEMG devices and video games to develop a biofeedback-based therapeutic play system, which could improve patient training initiative and compliance. Lee (2022) found that EMG-guided pedaling training was effective for enhancing activities of daily living and improving motor dysfunction in patients with stroke. Khan et al. (2021) proposed a wireless data acquisition system by combining sensors and sEMG, which reduces the dependence of patients on caregivers and enables them to complete daily activities independently by helping them control different devices in real time. Ito et al. (2021) developed an electromyography-controlled gamified movement system that motivates patients with stroke with various degrees of paralysis to complete repetitive finger and wrist movements in enjoyment. Yu et al. (2020) developed an artificial intelligence system using real-time EMG signals that can obtain accurate stroke predictions. This shows that electromyography can potentially be used to predict disease occurrence, and the combination of electromyography and rehabilitation training based on the biofeedback theory is a promising rehabilitation method. Therefore, further development and research are warranted to test the potential efficacy of this combination treatment in the future.
Emerging rehabilitation treatment techniques for motor function after stroke
Exoskeleton, home training, telemedicine, and virtual reality are the new keywords from 2020 to 2022. The exoskeleton, a wearable rehabilitation robot, assists patients in daily life activities and gait training and has gained considerable popularity in recent years (Molteni et al., 2017; Nolan et al., 2020). Rodríguez-Fernández et al. (2021) systematically evaluated lower extremity exoskeleton robots to reveal the potential of wearable exoskeletons for applications in early rehabilitation, thereby promoting functional recovery and daily life activities in homes and communities. Chen et al. (2022) developed a tendon-driven soft hand exoskeleton, paving the way for a fully driven soft hand exoskeleton. Chen et al. (2021) proposed a therapeutic system comprising sensory and motor gloves. The sensory gloves worn on the fitness hands contain force and flex sensors, which measured the gripping force and bending angle of each finger joint for motion detection. Simultaneously, micromotors provide an auxiliary driving force for the motor gloves worn on the affected hand to perform training tasks. Exoskeleton equipment has considerably improved, from a large upper and lower limb exoskeleton to a delicate hand exoskeleton and from heavy and bulky devices to comfortable, safe, and soft gloves. However, evidence supporting its benefits has been restricted owing to small study samples, inconsistent clinical protocols, and short intervention durations; therefore, in the future, large-sample, long-term, normalized randomized controlled trials are warranted to demonstrate the clinical effectiveness of the exoskeletons.
Home training is frequently associated with telerehabilitation (Truijen et al., 2022). A review presumed that telerehabilitation is an appropriate option for at-home recovery (Perrochon et al., 2019). Chae et al. (2020) proposed a home rehabilitation system that can be used for at-home treatment of patients with stroke using a smartwatch and cell phone application to identify and record the type and frequency of rehabilitation exercises performed by the user. Cramer et al. (2019) demonstrated that telerehabilitation and general rehabilitation significantly improved arm motor function, indicating that telerehabilitation was as effective as in-hospital rehabilitation. Similarly, Knepley et al. (2021) reviewed articles related to telerehabilitation and concluded that telerehabilitation is less expensive and more effective than in-clinic rehabilitation for improving functional impairment in patients with stroke and that telerehabilitation can be combined with different treatments, including virtual reality. For patients with stroke, the utilization of virtual reality in the rehabilitation process has been proved to improve motor function (Norouzi-Gheidari et al., 2019; Domínguez-Téllez et al., 2020; Karamians et al., 2020; Mekbib et al., 2020). Thielbar et al. (2020) found that multiuser virtual reality training was better for at-home rehabilitation by comparing patient engagement and subjective experience with multiuser and single-user virtual reality therapy. Lee et al. (2020) validated the feasibility of fully immersive virtue reality technology with head mounted displays for the upper-limb recovery of patients with stroke. Qiu et al. (2020) developed a virtual rehabilitation system for home use that can be remotely customized for a certain intensity of upper extremity training. Patients with stroke benefit from longer treatment duration when their motor function improves. However, in the current one-to-one treatment model, increasing the duration of treatment is usually impossible (Norouzi-Gheidari et al., 2019). Therefore, virtual reality and telerehabilitation allow patients to complete the same or even more training at home as in a medical facility (Truijen et al., 2022). Additionally, although there have been more randomized clinical trials performed to test the efficacy of virtual reality, it is difficult to conclude its effectiveness owing to the significant differences between interventions and comparative participants in the different studies. The field is emerging, and stronger examination is expected to have more precise inferences (Laver et al., 2020). Meanwhile, according to Thielbar’s research conclusion (Thielbar et al., 2020), more multiuser-connected rehabilitation systems should be developed based on virtual reality and remote rehabilitation to improve the enthusiasm for rehabilitation training for patients with stroke.
Limitation
The study had few limitations. First, only the publications distributed in the WoSCC database was incorporated. Second, the selected articles were written in English, which may disregard a few literary works of different language in this field. Therefore, some limitations in literature retrieval occurred. Conversely, recently, the sum of cocitation frequency in the published literature may be rather low owing to the short publishing time, thereby generating contrasts between the study results and genuine circumstances. Finally, because of different algorithms while using CiteSpace to generate visual maps, there are no unitary setting processes of time division, threshold, and clipping methods, which may produce some deviation.
Conclusion
In this study, we first searched the WoSCC database for the last 18 years of literature regarding poststroke motor function rehabilitation and performed bibliometric and visual analyses using CiteSpace and VOSviewer software, presenting a relatively scientific and intuitive overview of research on this topic. Visual analysis revealed that research in this field is in the stage of rapid development, and the related literature on this topic is constantly emerging, showing a steady growth trend. Briefly, rehabilitation of the upper limb is the most common research hotspot. Regarding rehabilitation evaluation and assessment, the Fugl–Meyer assessment may be the most generally utilized assessment scale. Meanwhile, research on quantitative measurement techniques, including electromyography, has gradually emerged. Regarding rehabilitation treatment technology, in addition to conventional intervention methods, such as CI therapy and noninvasive brain stimulation, research on virtual reality, telemedicine, electroacupuncture, brain–computer interface, and rehabilitation robots, including exoskeleton, has attracted increasing attention. These topics have become research hotspots on poststroke motor function rehabilitation and reveal future research trends. Future research on motor function rehabilitation after stroke should be focused on these points: first, formulate normative and systematic rehabilitation interventions throughout the whole course of stroke, and second, develop targeted interventions for patients with different types and stages of stroke.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
DL, JZ, QZ and GH: conception and design, revising the article. JH, JZ, and YW: study conduct and editing the article. YW and PD: data acquisition and analysis. JH, JZ, QY, GL, XW, and LZ: writing the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (grant nos. 81874032, 82072528, and 82002380), Natural Science Foundation of Guangdong Province, (2214050003841 to DL, 2022A1515012460 to GH) and College Student’s Innovative Entrepreneurial Training Plan Program (grant no. S202212121168).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnagi.2022.1024163/full#supplementary-material
Acknowledgments
The author group would like to thank the English Language Institute (www.enago.cn) for providing the English touch-ups.
References
- Bai Z., Zhang J., Fong K. N. K. (2022). Effects of transcranial magnetic stimulation in modulating cortical excitability in patients with stroke: a systematic review and meta-analysis. J. Neuroeng. Rehabil. 19:24. doi: 10.1186/s12984-022-00999-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernhardt J., Mehrholz J. (2019). Robotic-assisted training after stroke: RATULS advances science. Lancet 394, 6–8. doi: 10.1016/S0140-6736(19)31156-0, PMID: [DOI] [PubMed] [Google Scholar]
- Borges L. R., Fernandes A. B., Melo L. P., Guerra R. O., Campos T. F. (2018). Action observation for upper limb rehabilitation after stroke. Cochrane Database Syst. Rev. 2018:CD011887. doi: 10.1002/14651858.CD011887.pub2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cè E., Longo S., Limonta E., Coratella G., Rampichini S., Esposito F. (2020). Peripheral fatigue: new mechanistic insights from recent technologies. Eur. J. Appl. Physiol. 120, 17–39. doi: 10.1007/s00421-019-04264-w, PMID: [DOI] [PubMed] [Google Scholar]
- Cecchi F., Carrabba C., Bertolucci F., Castagnoli C., Falsini C., Gnetti B., et al. (2021). Transcultural translation and validation of Fugl-Meyer assessment to Italian. Disabil. Rehabil. 43, 3717–3722. doi: 10.1080/09638288.2020.1746844, PMID: [DOI] [PubMed] [Google Scholar]
- Chae S. H., Kim Y., Lee K. S., Park H. S. (2020). Development and clinical evaluation of a web-based upper limb home rehabilitation system using a smartwatch and machine learning model for chronic stroke survivors: prospective comparative study. JMIR Mhealth Uhealth 8:e17216. doi: 10.2196/17216, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X., Gong L., Wei L., Yeh S., Da Xu L., Zheng L., et al. (2021). A wearable hand rehabilitation system with soft gloves. IEEE Trans. Ind. Inf. 17, 943–952. doi: 10.1109/TII.2020.3010369 [DOI] [Google Scholar]
- Chen W., Li G., Li N., Wang W., Yu P., Wang R., et al. (2022). Soft exoskeleton with fully actuated thumb movements for grasping assistance. IEEE Trans. Robotics. 38, 2194–2207. doi: 10.1109/TRO.2022.3148909 [DOI] [Google Scholar]
- Chen S., Lu Q., Bai J., Deng C., Wang Y., Zhao Y. (2020). Global publications on stigma between 1998–2018: a bibliometric analysis. J. Affect. Disord. 274, 363–371. doi: 10.1016/j.jad.2020.05.006 [DOI] [PubMed] [Google Scholar]
- Chumbler N. R., Quigley P., Li X., Morey M., Rose D., Sanford J., et al. (2012). Effects of telerehabilitation on physical function and disability for stroke patients: a randomized, controlled trial. Stroke 43, 2168–2174. doi: 10.1161/STROKEAHA.111.646943, PMID: [DOI] [PubMed] [Google Scholar]
- Cramer S. C., Dodakian L., Le V., See J., Augsburger R., McKenzie A., et al. (2019). Efficacy of home-based telerehabilitation vs in-clinic therapy for adults after stroke: a randomized clinical trial. JAMA Neurol. 76, 1079–1087. doi: 10.1001/jamaneurol.2019.1604, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniel A., Koumans H., Ganti L. (2021). Impact of music therapy on gait after stroke. Cureus 13, –e18441. doi: 10.7759/cureus.18441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimyan M. A., Cohen L. G. (2011). Neuroplasticity in the context of motor rehabilitation after stroke. Nat. Rev. Neurol. 7, 76–85. doi: 10.1038/nrneurol.2010.200, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domínguez-Téllez P., Moral-Muñoz J. A., Salazar A., Casado-Fernández E., Lucena-Antón D. (2020). Game-based virtual reality interventions to improve upper limb motor function and quality of life after stroke: systematic review and meta-analysis. Games Health J. 9, 1–10. doi: 10.1089/g4h.2019.0043, PMID: [DOI] [PubMed] [Google Scholar]
- Dong X. T., Tan Y. C., Zhuang D. L., Hu T. T., Zhao M. Y. (2022). Global characteristics and trends in research on ferroptosis: a data-driven bibliometric study. Oxidative Med. Cell. Longev. 2022, 1–12. doi: 10.1155/2022/8661864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong Y. L., Weng L. M., Hu Y. H., Mao Y. X., Zhang Y. J., Lu Z. F., et al. (2022). Exercise for stroke rehabilitation: a bibliometric analysis of global research from 2001 to 2021. Front. Aging Neurosci. 14:876954. doi: 10.3389/fnagi.2022.876954, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron N. (2021). Exploring the bibliometrics of various ophthalmic fields. Clin. Exp. Optom. 104, 559–560. doi: 10.1080/08164622.2021.1913044, PMID: [DOI] [PubMed] [Google Scholar]
- Feldner H. A., Papazian C., Peters K. M., Creutzfeldt C. J., Steele K. M. (2021). Clinical use of surface electromyography to track acute upper extremity muscle recovery after stroke: a descriptive case study of a single patient. Appl. Syst. Innov. 4:32. doi: 10.3390/asi4020032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng X. D., Liu C. M., Guo Q. C., Bai Y. J., Ren Y. F., Ren B. B., et al. (2013). Research progress in rehabilitation treatment of stroke patients a bibliometric analysis. Neural Regen. Res. 8, 1423–1430. doi: 10.3969/j.issn.1673-5374.2013.15.010, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Formstone L., Huo W., Wilson S., McGregor A., Bentley P., Vaidyanathan R. (2021). Quantification of motor function post-stroke using novel combination of wearable inertial and mechanomyographic sensors. IEEE Trans. Neural Syst. Rehabil. Eng. 29, 1158–1167. doi: 10.1109/TNSRE.2021.3089613, PMID: [DOI] [PubMed] [Google Scholar]
- Fujita K., Kobayashi Y., Hitosugi M. (2021). Temporal changes in electromyographic activity and gait ability during extended walking in individuals post-stroke: a pilot study. Healthcare (Basel). 9:444. doi: 10.3390/healthcare9040444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatem S. M., Saussez G., Della Faille M., Prist V., Zhang X., Dispa D., et al. (2016). Rehabilitation of motor function after stroke: a multiple systematic review focused on techniques to stimulate upper extremity recovery. Front. Hum. Neurosci. 10:442. doi: 10.3389/fnhum.2016.00442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs-Itua A., Wong S. C. (2021). Stroke rehabilitation and recovery. Br. J. Hosp. Med. 82, 1–7. doi: 10.12968/hmed.2020.0701 [DOI] [PubMed] [Google Scholar]
- Ito K., Uehara S., Yuasa A., Kim C. M., Kitamura S., Ushizawa K., et al. (2021). Electromyography-controlled gamified exercise system for the distal upper extremity: a usability assessment in subacute post-stroke patients. Disability and Rehabilitation-Assistive Technology 8, 1– 6. [DOI] [PubMed] [Google Scholar]
- Ju Y., Yoon I. J. (2018). The effects of modified constraint-induced movement therapy and mirror therapy on upper extremity function and its influence on activities of daily living. J. Phys. Ther. Sci. 30, 77–81. doi: 10.1589/jpts.30.77, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karamians R., Proffitt R., Kline D., Gauthier L. V. (2020). Effectiveness of virtual reality- and gaming-based interventions for upper extremity rehabilitation poststroke: a meta-analysis. Arch. Phys. Med. Rehabil. 101, 885–896. doi: 10.1016/j.apmr.2019.10.195, PMID: [DOI] [PubMed] [Google Scholar]
- Khan M. A., Bayram B. M., Das R., Puthusserypady S. (2021). Electromyography and inertial motion sensors based wearable data acquisition system for stroke patients: a pilot study. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2021, 6953–6956. doi: 10.1109/EMBC46164.2021.9630245 [DOI] [PubMed] [Google Scholar]
- Knepley K. D., Mao J. Z., Wieczorek P., Okoye F. O., Jain A. P., Harel N. Y. (2021). Impact of telerehabilitation for stroke-related deficits. Telemed. J. E Health 27, 239–246. doi: 10.1089/tmj.2020.0019, PMID: [DOI] [PubMed] [Google Scholar]
- Kokol P., Blažun Vošner H., Završnik J. (2021). Application of bibliometrics in medicine: a historical bibliometrics analysis. Health Inf. Libr. J. 38, 125–138. doi: 10.1111/hir.12295 [DOI] [PubMed] [Google Scholar]
- Laver K. E., Adey-Wakeling Z., Crotty M., Lannin N. A., George S., Sherrington C. (2020). Telerehabilitation services for stroke. Cochrane Database Syst. Rev. 2020:CD010255. doi: 10.1002/14651858.CD010255.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laver K. E., George S., Thomas S., Deutsch J. E., Crotty M. (2011). Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev.:CD008349. doi: 10.1002/14651858.CD008349.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Danseur M. (2020). Stroke rehabilitation. Crit. Care Nurs. Clin. North Am. 32, 97–108. doi: 10.1016/j.cnc.2019.11.004 [DOI] [PubMed] [Google Scholar]
- Lee K. (2022). EMG-triggered pedaling training on muscle activation, gait, and motor function for stroke patients. Brain Sci. 12:76. doi: 10.3390/brainsci12010076, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S. H., Jung H. Y., Yun S. J., Oh B. M., Seo H. G. (2020). Upper extremity rehabilitation using fully immersive virtual reality games with a head mount display: a feasibility study. PM R 12, 257–262. doi: 10.1002/pmrj.12206, PMID: [DOI] [PubMed] [Google Scholar]
- Liu Y., Silva R. M. L., Friedrich J. B., Kao D. S., Mourad P. D., Bunnell A. E. (2022). Surface electromyography-driven therapeutic gaming for rehabilitation of upper extremity weakness: a pilot study. Plast. Reconstr. Surg. 150, 125–131. doi: 10.1097/PRS.0000000000009208, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo A. C., Guarino P. D., Richards L. G., Haselkorn J. K., Wittenberg G. F., Federman D. G., et al. (2010). Robot-assisted therapy for long-term upper-limb impairment after stroke. N. Engl. J. Med. 362, 1772–1783. doi: 10.1056/NEJMoa0911341, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma D., Yang B., Guan B., Song L., Liu Q., Fan Y., et al. (2021). A bibliometric analysis of pyroptosis from 2001 to 2021. Front. Immunol. 12:731933. doi: 10.3389/fimmu.2021.731933, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maresca G., Maggio M. G., De Luca R., Manuli A., Tonin P., Pignolo L., et al. (2020). Tele-neuro-rehabilitation in Italy: state of the art and future perspectives. Front. Neurol. 11:563375. doi: 10.3389/fneur.2020.563375, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekbib D. B., Han J., Zhang L., Fang S., Jiang H., Zhu J., et al. (2020). Virtual reality therapy for upper limb rehabilitation in patients with stroke: a meta-analysis of randomized clinical trials. Brain Inj. 34, 456–465. doi: 10.1080/02699052.2020.1725126, PMID: [DOI] [PubMed] [Google Scholar]
- Molteni F., Gasperini G., Gaffuri M., Colombo M., Giovanzana C., Lorenzon C., et al. (2017). Wearable robotic exoskeleton for overground gait training in sub-acute and chronic hemiparetic stroke patients: preliminary results. Eur. J. Phys. Rehabil. Med. 53, 676–684. doi: 10.23736/S1973-9087.17.04591-9, PMID: [DOI] [PubMed] [Google Scholar]
- Morone G., Paolucci S., Cherubini A., De Angelis D., Venturiero V., Coiro P., et al. (2017). Robot-assisted gait training for stroke patients: current state of the art and perspectives of robotics. Neuropsychiatr. Dis. Treat. 13, 1303–1311. doi: 10.2147/NDT.S114102, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaev V. A., Nikolaev A. A. (2022). Recent trends in telerehabilitation of stroke patients: a narrative review. NeuroRehabilitation 51, 1–22. doi: 10.3233/NRE-210330, PMID: [DOI] [PubMed] [Google Scholar]
- Nolan K. J., Karunakaran K. K., Chervin K., Monfett M. R., Bapineedu R. K., Jasey N. N., et al. (2020). Robotic exoskeleton gait training during acute stroke inpatient rehabilitation. Front. Neurorobot. 14:581815. doi: 10.3389/fnbot.2020.581815, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norouzi-Gheidari N., Hernandez A., Archambault P. S., Higgins J., Poissant L., Kairy D. (2019). Feasibility, safety and efficacy of a virtual reality exergame system to supplement upper extremity rehabilitation post-stroke: a pilot randomized clinical trial and proof of principle. Int. J. Environ. Res. Public Health 17:133. doi: 10.3390/ijerph17010113, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osareh F. (1996). Bibliometrics, Citation analysis and Co-Citation analysis: a review of literature I. Libri 46, 149–158. doi: 10.1515/libr.1996.46.3.149 [DOI] [Google Scholar]
- Pan B., Huang Z., Jin T., Wu J., Zhang Z., Shen Y. (2021). Motor function assessment of upper limb in stroke patients. J. Healthc. Eng. 2021, 1–11. doi: 10.1155/2021/6621950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papazian C., Baicoianu N. A., Peters K. M., Feldner H. A., Steele K. M. (2021). Electromyography recordings detect muscle activity before observable contractions in acute stroke care. Arch. Rehabil. Res. Clin. Transl. 3:100136. doi: 10.1016/j.arrct.2021.100136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Robledo F., Llamas-Ramos R., Llamas-Ramos I., Bermejo-Gil B. M., Sánchez-González J. L., Martín-Nogueras A. M. (2022). Adaptation and feasibility of the online version of the Fugl Meyer scale for the assessment of patients following cerebrovascular accidents. Rev. Neurol. 74, 156–162. doi: 10.33588/rn.7405.2021385, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrochon A., Borel B., Istrate D., Compagnat M., Daviet J. C. (2019). Exercise-based games interventions at home in individuals with a neurological disease: a systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 62, 366–378. doi: 10.1016/j.rehab.2019.04.004, PMID: [DOI] [PubMed] [Google Scholar]
- Pitt K. M., McCarthy J. W. (2021). Strategies for highlighting items within visual scene displays to support augmentative and alternative communication access for those with physical impairments. Disabil. Rehabil. Assist. Technol., 1–6. [DOI] [PubMed] [Google Scholar]
- Qiu Q., Cronce A., Patel J., Fluet G. G., Mont A. J., Merians A. S., et al. (2020). Development of the home based virtual rehabilitation system (HoVRS) to remotely deliver an intense and customized upper extremity training. J. Neuroeng. Rehabil. 17:155. doi: 10.1186/s12984-020-00789-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Murguialday A., Broetz D., Rea M., Läer L., Yilmaz O., Brasil F. L., et al. (2013). Brain-machine interface in chronic stroke rehabilitation: a controlled study. Ann. Neurol. 74, 100–108. doi: 10.1002/ana.23879, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rech K. D., Salazar A. P., Marchese R. R., Schifino G., Cimolin V., Pagnussat A. S. (2020). Fugl-Meyer assessment scores are related with kinematic measures in people with chronic hemiparesis after stroke. J. Stroke Cerebrovasc. Dis. 29:104463. doi: 10.1016/j.jstrokecerebrovasdis.2019.104463, PMID: [DOI] [PubMed] [Google Scholar]
- Rodgers H., Bosomworth H., Krebs H. I., van Wijck F., Howel D., Wilson N., et al. (2019). Robot assisted training for the upper limb after stroke (RATULS): a multicentre randomised controlled trial. Lancet 394, 51–62. doi: 10.1016/S0140-6736(19)31055-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Fernández A., Lobo-Prat J., Font-Llagunes J. M. (2021). Systematic review on wearable lower-limb exoskeletons for gait training in neuromuscular impairments. J. Neuroeng. Rehabil. 18:22. doi: 10.1186/s12984-021-00815-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saavedra-García A., Moral-Munoz J. A., Lucena-Anton D. (2021). Mirror therapy simultaneously combined with electrical stimulation for upper limb motor function recovery after stroke: a systematic review and meta-analysis of randomized controlled trials. Clin. Rehabil. 35, 39–50. doi: 10.1177/0269215520951935, PMID: [DOI] [PubMed] [Google Scholar]
- Santisteban L., Térémetz M., Bleton J. P., Baron J. C., Maier M. A., Lindberg P. G. (2016). Upper limb outcome measures used in stroke rehabilitation studies: a systematic literature review. PLoS One 11:e0154792. doi: 10.1371/journal.pone.0154792, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen X. W., Liu X. (2022). Automatic Fugl-Meyer assessment based on videos. J. Electron. Meas. Instrum. 36, 1–11. doi: 10.13382/j.jemi.B2104225 [DOI] [Google Scholar]
- Stinear C. M., Lang C. E., Zeiler S., Byblow W. D. (2020). Advances and challenges in stroke rehabilitation. Lancet Neurol. 19, 348–360. doi: 10.1016/S1474-4422(19)30415-6, PMID: [DOI] [PubMed] [Google Scholar]
- Suponeva N. A., Yusupova D. G., Zimin A. A., Rimkevichus A. A., Melchenko D. A., Ilyina K. A., et al. (2021). Validation of the Russian version of the Fugl-Meyer assessment of physical performance for assessment of patients with post-stroke paresis. Zh. Nevrol. Psikhiatr. Im. S S Korsakova 121, 86–90. doi: 10.17116/jnevro202112108286, PMID: [DOI] [PubMed] [Google Scholar]
- Suso-Martí L., La Touche R., Herranz-Gómez A., Angulo-Díaz-Parreño S., Paris-Alemany A., Cuenca-Martínez F. (2021). Effectiveness of telerehabilitation in physical therapist practice: an umbrella and mapping review with meta–meta-analysis. Phys. Ther. 101:pzab075. doi: 10.1093/ptj/pzab075, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Synnestvedt M. B., Chen C., Holmes J. H. (2005). CiteSpace II: visualization and knowledge discovery in bibliographic databases. AMIA Annu. Symp. Proc. 2005, 724–728. PMID: [PMC free article] [PubMed] [Google Scholar]
- Thielbar K. O., Triandafilou K. M., Barry A. J., Yuan N., Nishimoto A., Johnson J., et al. (2020). Home-based upper extremity stroke therapy using a multiuser virtual reality environment: a randomized trial. Arch. Phys. Med. Rehabil. 101, 196–203. doi: 10.1016/j.apmr.2019.10.182, PMID: [DOI] [PubMed] [Google Scholar]
- Timmermans C., Roerdink M., Meskers C. G. M., Beek P. J., Janssen T. W. J. (2021). Walking-adaptability therapy after stroke: results of a randomized controlled trial. Trials 22:923. doi: 10.1186/s13063-021-05742-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truijen S., Abdullahi A., Bijsterbosch D., van Zoest E., Conijn M., Wang Y., et al. (2022). Effect of home-based virtual reality training and telerehabilitation on balance in individuals with Parkinson disease, multiple sclerosis, and stroke: a systematic review and meta-analysis. Neurol. Sci. 43, 2995–3006. doi: 10.1007/s10072-021-05855-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ugolini D., Neri M., Cesario A., Marazzi G., Milazzo D., Volterrani M., et al. (2013). Bibliometric analysis of literature in cerebrovascular and cardiovascular diseases rehabilitation: growing numbers, reducing impact factor. Arch. Phys. Med. Rehabil. 94, 324–331.e1. doi: 10.1016/j.apmr.2012.08.205, PMID: [DOI] [PubMed] [Google Scholar]
- Veerbeek J. M., Langbroek-Amersfoort A. C., van Wegen E. E., Meskers C. G., Kwakkel G. (2017). Effects of robot-assisted therapy for the upper limb after stroke: a systematic review and meta-analysis. Neurorehabil. Neural Repair 31, 107–121. doi: 10.1177/1545968316666957 [DOI] [PubMed] [Google Scholar]
- Wang D., Xiang J., He Y., Yuan M., Dong L., Ye Z., et al. (2022). The mechanism and clinical application of constraint-induced movement therapy in stroke rehabilitation. Front. Behav. Neurosci. 16:828599. doi: 10.3389/fnbeh.2022.828599, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winstein C. J., Stein J., Arena R., Bates B., Cherney L. R., Cramer S. C., et al. (2016). Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 47, e98–e169. doi: 10.1161/STR.0000000000000098, PMID: [DOI] [PubMed] [Google Scholar]
- Woytowicz E. J., Rietschel J. C., Goodman R. N., Conroy S. S., Sorkin J. D., Whitall J., et al. (2017). Determining levels of upper extremity movement impairment by applying a cluster analysis to the Fugl-Meyer assessment of the upper extremity in chronic stroke. Arch. Phys. Med. Rehabil. 98, 456–462. doi: 10.1016/j.apmr.2016.06.023, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto H., Takeda K., Koyama S., Morishima K., Hirakawa Y., Motoya I., et al. (2020). Relationship between upper limb motor function and activities of daily living after removing the influence of lower limb motor function in subacute patients with stroke: a cross-sectional study. Hong Kong J. Occup. Ther. 33, 12–17. doi: 10.1177/156w.9186120926609, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao R. Q., Ren C., Wang J. N., Wu G. S., Zhu X. M., Xia Z. F., et al. (2020). Publication trends of research on sepsis and host immune response during 1999–2019: a 20-year bibliometric analysis. Int. J. Biol. Sci. 16, 27–37. doi: 10.7150/ijbs.37496, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J., Kwon S.-H., Ho C. M. B., Pyo C.-S., Lee H. (2020). Stroke disease prediction system using real-time electromyography signals. Appl. Sci.-Basel. 10:6791. doi: 10.3390/app10196791 [DOI] [Google Scholar]
- Zhang J. B., Wei R. P., Yang H., Han B. (2022). Effect of electroacupuncture at antagonistic muscle and agonistic muscle on motor function in patients with upper-extremity spasticity after stroke. Zhongguo zhen jiu = Chinese acupuncture & moxibustion. 42, 381–384. doi: 10.13703/j.0255-2930.20210406-k0001, PMID: [DOI] [PubMed] [Google Scholar]
- Zhou M., Wang R., Cheng S., Xu Y., Luo S., Zhang Y., et al. (2021). Bibliometrics and visualization analysis regarding research on the development of microplastics. Environ. Sci. Pollut. Res. 28, 8953–8967. doi: 10.1007/s11356-021-12366-2, PMID: [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.