Abstract
Introduction
3D printing has recently emerged as an alternative to cadaveric models in medical education. A growing body of research supports the use of 3D printing in this context and details the beneficial educational outcomes. Prevailing studies rely on participants’ stated preferences, but little is known about actual student preferences.
Methods
A mixed methods approach, consisting of structured observation and computer vision, was used to investigate medical students’ preferences and handling patterns when using 3D printed versus cadaveric models in a cardiac pathology practical skills workshop. Participants were presented with cadaveric samples and 3D printed replicas of congenital heart deformities.
Results
Analysis with computer vision found that students held cadaveric hearts for longer than 3D printed models (7.71 vs. 6.73 h), but this was not significant when comparing across the four workshops. Structured observation found that student preferences changed over the workshop, shifting from 3D printed to cadaveric over time. Interactions with the heart models (e.g., pipecleaners) were comparable.
Conclusion
We found that students had a slight preference for cadaveric hearts over 3D printed hearts. Notably, our study contrasts with other studies that report student preferences for 3D printed learning materials. Given the relative equivalence of the models, there is opportunity to leverage 3D printed learning materials (which are not scarce, unlike cadaveric materials) to provide equitable educational opportunities (e.g., in rural settings, where access to cadaveric hearts is less likely).
Keywords: 3D printing, Anatomy, Medical education, Congenital heart deformity
Introduction
Current educational practices that involve cadaveric samples enable students to make spatial connections between relevant structures and gain understanding of pathological processes [1]. However, cadaveric samples are limited resources that pose financial costs for storage and maintenance [2–4], health concerns risks from contact with embalming fluids [5], and potential ethical and psychological challenges for students [3, 5]. As medical programs move from large cities to multiple locations across regional and rural settings, cadaveric samples may not be available, raising equity issues. The recent COVID-19 global pandemic introduced another concern for cadaveric samples, which need to be cleaned between student groups to limit the spread of infectious diseases. The process of cleaning cadaveric objects can be physically and chemically degrading, damaging their structure and fixation. Thus, while cadaveric samples may present the optimal method for learning anatomy and pathology, alternatives that address issues of equity, access, and infection control must be considered.
3D printed models are becoming increasingly prominent in medical education, with applications at every stage of training, including anatomy, pathology, simulation, and pre-surgical planning [4, 6, 7]. Many have reported on methods of producing such models [2, 8, 9], and demonstrated the short-term educational benefits of 3D printed anatomical models in teaching [7, 10]. There is much evidence to suggest that 3D printed models — when compared to two dimensional anatomical drawings, images or atlas, 3D computer models, and even cadaveric models — can improve test scores in structure identification and anatomy [10–13].
Beyond this direct correlation with learning outcomes, recent studies have suggested that inclusion of 3D printed resources in medical education results in an enriched learning experience for students [14]. Studies exploring this line of enquiry often rely on students’ perspectives and recollections (e.g., student opinions collected through focus groups, questionnaires, and surveys) [7, 15]. Students report improved satisfaction with 3D printed models compared with conventional anatomy teaching methods [14]. Notably, there have been no studies to assess if these subjective findings are also seen in the real-time actions of students.
We hypothesize that the use of 3D hearts in learning activities could encourage students to be more inquisitive and open to experimentation as these samples are significantly more robust than cadaveric models. This study aimed to investigate the behaviors and interactions of students with paired cadaveric and replicated 3D printed hearts during a structured learning workshop on congenital heart deformities. Specifically, our investigation establishes whether students have a preference between 3D printed or cadaveric hearts, and whether there are differences in how students interact with each of these educational resources.
Methods
The study employed a mixed methods approach of structured observation [16] and computer vision analysis [17]. Ethics approval was received from the Sydney Children’s Hospitals Network Human Research Ethics Committee (protocol LNR/18/SCHN/337).
Context
This research took place during an existing cardiac pathology practical skills workshop that focused on congenital heart deformities. The workshop was taught during an 8-week pediatric term, which is held four times per year for a rotating cohort as part of a 4-year graduate-entry medical program. At the time of the study, students undertook the term at the end of their third year or beginning of their fourth year. Each term, approximately a 70-student rotation attended the hospital for their structured teaching week, in which the workshop was held. The students had experience of learning with cadaveric specimens during their first and second year, but we are not aware of any formal teaching using 3D printed models.
Recruitment
The study took place during four workshops, held over two terms, from April to June 2019, with each workshop containing different students. Students were invited to participate in the study or attend the usual workshop. A total of 90 students consented to be a part of the study, which included an initial pilot study of 23 students to establish the protocol for the subsequent sessions (such as room layout and how the heart models were circulated) and were not included in the final analyses. No participants withdrew after consenting.
Study Design
Conventionally, the 30-min cardiac pathology practical skills workshops involved Pathology Department tutors (senior paediatric pathologists) using cadaveric heart samples to demonstrate the three-dimensional pathology. The 18 cadaveric congenital heart deformity specimens are regularly used by the Department of Pathology at the Children’s Hospital at Westmead for a practical workshop for medical students from the University of Sydney. These hearts are fixed and waxed, enabling interaction with the models, and were prepared with windows cut to highlight key features. The teaching collection includes examples of pathologies such as tetralogy of Fallot, ventricular septal defect, patent ductus arteriosus, and atrial septal defects (and combinations of pathologies).
For our study, 3D printed replicas of these cadaveric heart models were used alongside the current teaching practice. CT scans of the hearts were performed at 0.4-mm slice thickness using a Siemens SOMATOM Force. The CT scans were exported as DICOM files and segmented using Mimics v19.0 and converted into STL format. Hearts were printed at scale using fused deposition modelling (FDM) on the Stratasys Fortus 450mc in ASA using T12 tips at a layer height of 0.1778 mm with caustic acid–soluble support material SR-30. A total of 18 cadaveric hearts were scanned and replicated using 3D printing.
Students were informed about the study and consented to participate and be video recorded but were not told that the researchers were analyzing their handling of the heart models. This ensured that students acted authentically with the educational models and that their behavior was not influenced by the study’s objective.
Following a didactic lecture on the formation of congenital heart deformities from the lead tutor (a pathologist), cadaveric heart models and their 3D printed replicas (18 paired samples in total) were passed around the students (Fig. 1a). For each type of congenital heart deformity, the paired hearts were passed in plastic trays so that students could access whichever type of heart model they preferred. The paired hearts each had an identical tag, taken from the original cadaveric hearts, which described the patient and heart deformity. The students undertook unstructured exploratory learning as they inspected each heart type and passed along the trays as they finished their observations. Students were encouraged to use a pipe cleaner and their mobile phone lights to inspect the anatomic features of the heart models and identify defects in internal heart chamber walls.
Fig. 1.
The experimental setup, including a the paired 3D printed (left) and cadaveric (right) hearts in a tray, b the room and recording configuration, and c a sample frame from a video recording
Data Collection
The primary mode of data collection was through video recordings of the participants as they interacted with the 3D printed and cadaveric models during the workshop. The room was set up so that tables were in a square shape with a camera rig in the center (Fig. 1b). A custom 3D printed jig housed five GoPro video cameras and was configured to capture all the students sitting around the tables (Fig. 1c). A total of 700 min of video footage was captured across the 4 workshops, each having a duration of approximately 40 min, with the students handling the hearts for approximately 20 min. All videos were filmed with 1920 × 1080 definition at a frame rate between 24 and 48 frames per second (depending on the GoPro used).
Data Coding
Structured Observation
Structured observation was used by the researchers to systematically observe the behavior of students during their cardiac pathology practical skills workshop as they interacted with the 3D printed and cadaveric hearts. Most qualitative methods of observation require retrospective reports by participants (e.g., a post-workshop focus group or survey), or represent scenarios in which behavior can only be inferred [18]. Structured observation was selected for this study as it offers a way to validate findings from previous research through direct observation, rather than subjective measures such as inference, reflection, or participants’ opinions. The observation followed a set protocol to observe and record behavior, allowing the researchers to observe behavior directly. The researchers used a coding scheme to capture the actions and behaviors of students. The coding scheme captured interactions with the 3D printed and cadaveric hearts, including the sequence in which hearts were used by students (i.e., cadaveric or 3D printed heart first, where both were available), particular types of interaction (i.e., used a mobile phone light to highlight features of a heart, poked with a pipe cleaner or fingers to explore the deformities of a heart, and rough handling, e.g., dropping a heart on the table), and instances of collaboration (e.g., where a student discussed model features with another student, or consulted with a tutor for clarification). Each of these interactions was captured in a separate column of the coding scheme, based on the type of interaction and whether it occurred with a 3D printed or cadaveric heart. Instances where students did not have free choice for which heart to use were excluded from the data set for structured observation, i.e., where a pair of students could only reach one tray (as seen in Fig. 1) and each student’s decision to use a cadaveric or 3D printed model was forced as the other student had already picked up one of the available models.
Interactions were observed through recordings of the workshops, with four of the researchers (two PhDs, one Bachelor of Design/PhD student, one Bachelor of Engineering) collectively coding the data. During the initial coding, each researcher individually coded data for one participant. Codes were then compared between researchers, and discrepancies and outlying events were discussed. Triangulation between the researchers in this way assisted in validating the coding and helped the researchers establish a consistent coding style and align results. Once the researchers had aligned their coding practices, further coding was completed so that each participant’s data was coded by only one researcher. The researchers were co-located to maintain rigorous and consistent coding. This allowed the researchers to collectively discuss and interpret any ambiguous interactions that were observed.
In reporting the structured observation, each participant’s heart choice from each tray was represented by the letters P (printed model only), C (cadaveric only), PC (printed then cadaveric), and CP (cadaveric then printed). The choice of heart type was coded each time a tray was available for the student. For example, “CP, CP, PC, C” illustrates the choices made by a participant across four trays.
Computer Vision Analysis
Computer vision analysis was used to quantitatively investigate how students used the hearts. Object detection is a category of computer vision algorithm used to positively identify pre-defined objects within an image or data source. Object detection as a field of study has been accelerated by developments in deep learning and data analytics [19]. In the context of this study, object detection was used to identify two objects, cadaveric hearts, and 3D printed models, as seen in Fig. 1a.
The object detection algorithm employed in this study was YOLOV5 pre-configured object detection model, which was trained on 418 manually coded bounding boxed images of the hearts [17]. Once trained, the system was able to identify the location of either category of object, 3D printed or cadaveric, in the videos of the participants. Several iterations of the dataset’s design were required to achieve a final mean average precision of 0.93 measured at an intersection of union value of 0.5 over 300 epochs, including two augmentations to the dataset (brightness and blur) [20]. The outcome of this process is a model that is 94% accurate at positively identifying 3D printed or cadaveric hearts in the videos of the participants. This model was then applied to all 700 min of the footage and used to generate the analyses presented in the results. Notably, this allowed the researchers to measure the quantity of time that each model type was used. Unlike the structured observation, the computer vision analysis was unable to discriminate between when students had free choice over their heart type.
Data Analysis
Wilcoxon matched pairs signed rank test was used to compare student preferences (time held) in the four sessions and was run on GraphPad Prism version 9.1.2 for Windows (San Diego, CA, USA). To assess student interactions and collaboration, we assumed a null hypothesis that students would choose 3D printed and cadaveric hearts at equal rates (i.e., 50%:50%). We used IBM SPSS version 25 for Windows (Armonk, NY, USA) and tested goodness of fit using the chi-squared statistic to compare observed vs. expected counts based on whether students first picked up a 3D printed or cadaveric heart.
Results
Our findings are split across two primary themes: (i) students’ overall preferences for cadaveric or 3D printed hearts and how these changed over the course of the workshop; and (ii) how students interacted with the different hearts.
Student Preferences for 3D Printed vs. Cadaveric Models
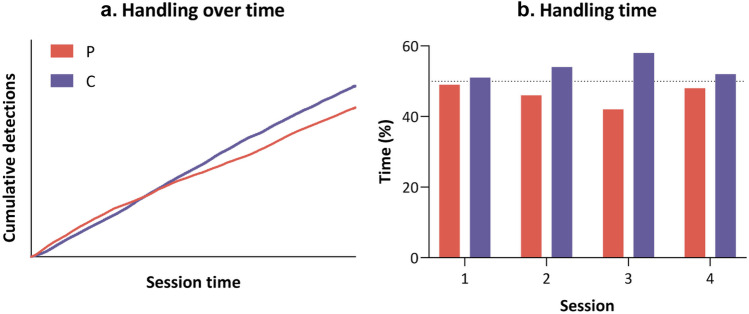
Through our mixed methods approach of structured observation and computer vision, we were able to determine student preferences for 3D printed and cadaveric hearts, along with how these preferences shifted during the four workshops. Computer vision analysis revealed that use of the two types of hearts was relatively similar throughout the workshops (Fig. 2a), with each of the 4 different groups of students (sessions 1 to 4) spending slightly more time holding cadaveric hearts than 3D printed hearts across all four sessions (7.71 vs. 6.73 h for all students). When comparing the four sessions (Fig. 2b), there was no significant difference between the time each heart type was handled (p = 0.1250).
Fig. 2.
Preferences for model type, as shown from a the cumulative time each heart type was handled, and b the time handled for each heart type from computer vision analysis for each session as a percentage of overall time held. P, 3D printed heart; C, cadaveric heart; dotted line represents 50%
Participant preferences for using different types of hearts shifted across the duration of the workshop. From the structured observation, the data sequences for each participant were collated and normalized to provide an overview of student choices across the workshop, highlighted in Fig. 3. This figure shows that most students’ initial preference was to use both types of hearts available (PC and CP), with students seeming to select one “preferred” type of model (P or C) as the workshop progressed. Notably, students’ free choice of heart from the first tray that they received skewed heavily towards picking up a 3D printed heart first, then a cadaveric heart from the same tray (PC). Fewer students interacted with cadaveric hearts first, then picked up a printed heart from the same tray (CP). The majority of students interacted with both hearts available to them in the first tray (PC and CP), while few students stuck to only a printed (P) or cadaveric heart (C). Conversely, students’ choice of hearts for the final tray they received was skewed towards cadaveric hearts (C), with a majority of students interacting with only one type of model from that tray.
Fig. 3.
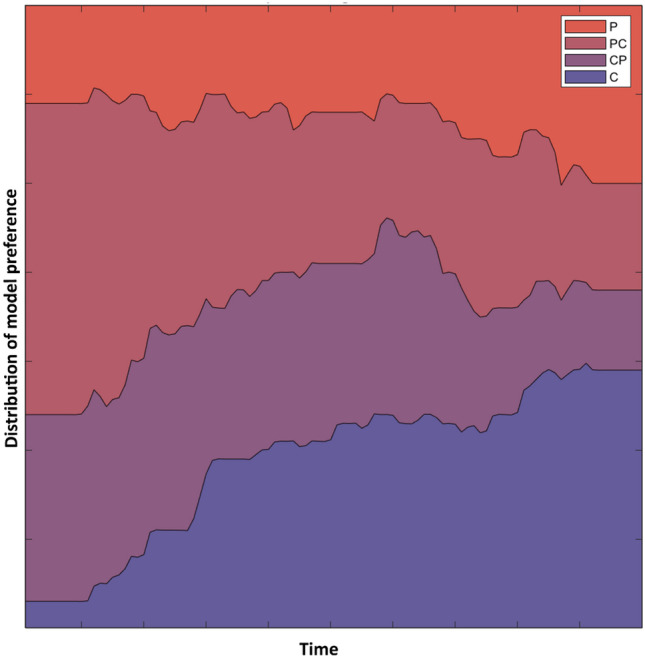
The change in model preference over the time course of the workshop. The time (in minutes) for each tutorial was normalized. P, 3D printed heart; C, cadaveric heart; PC, 3D printed then cadaveric heart; CP, cadaveric then 3D printed heart
Student Interaction with 3D Printed vs. Cadaveric Models
Students had a slight preference to use cadaveric hearts for “softer” activities, such as use of their mobile phone light to highlight features of a heart (P: 33%, C: 46%, CP/PC: 21%; Fig. 4a), but this was not significant (10 vs. 14, chi-square 0.667, 1df, p = 0.414). Preferences for poking with a pipecleaner (P: 39%, C: 42%, CP/PC: 42%; 68 vs. 75, chi-square 0.343, 1df, p = 0.558; Fig. 4b) or fingers (P: 54%, C: 40%, CP/PC: 6%; 68 vs. 75, chi-square 0.343, 1df, p = 0.558; Fig. 4c) were similar across both types of hearts. Students were less reserved when interacting with printed hearts, with a greater proportion of rough handling (P: 78%, C: 22%; 14 vs. 4, chi-square 5.556, 1df, p = 0.018; Fig. 4d), although the overall numbers were small. Rough handling included accidental drops and less careful transfers of the hearts; however, none of the handling coded was considered unprofessional or disrespectful to the cadaveric samples.
Fig. 4.
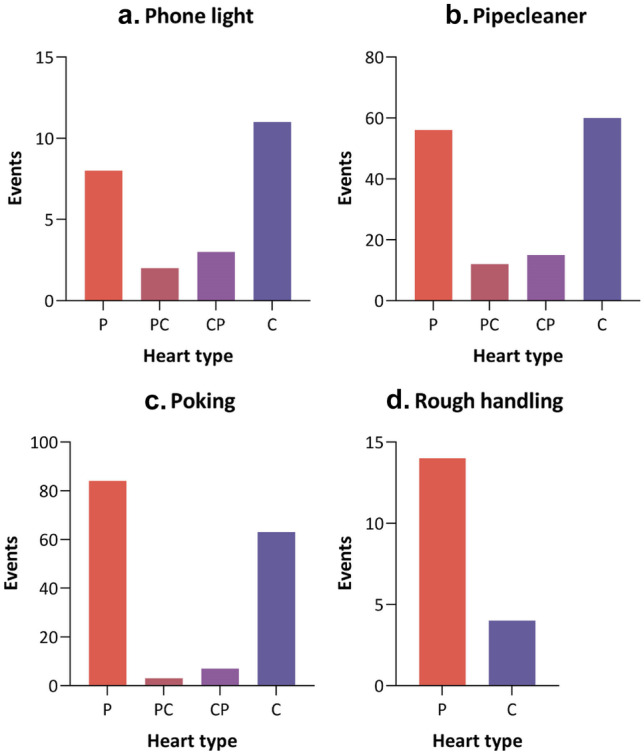
Student interactions and explorations with the different heart model types, including a shining their mobile phone light and b passing pipecleaners through the models to identify defects, c using their fingers to poke, as well as d instances of rough handling, whether seemingly deliberate or accidental. P, 3D printed heart; C, cadaveric heart; PC, 3D printed then cadaveric heart; CP, cadaveric then 3D printed heart
Figure 5 shows coded instances of collaboration among students and with tutors. We found that when there was collaboration between students, they were most likely to be handling the cadaveric hearts (P: 37%, C: 54%, CP/PC: 9%; Fig. 5a). Student to student collaboration was less common with the 3D printed hearts than cadaveric hearts (108 vs. 159, chi-square 9.742, 1df, p = 0.002). When students were talking to the tutors, there was no significant preference for either heart type (P: 35%, C: 52%, CP/PC: 13%; 9 vs. 14, chi-square 1.087, 1df, p = 0.297; Fig. 5b). The researchers also captured which hearts students chose to use to initiate collaboration and which type of heart they responded to collaboration with (e.g., when collaboration was initiated by a student the other student would often “respond” by picking up the paired heart to assist in communication and to better see what was being discussed). However, there was limited difference between use of cadaveric and printed hearts when initiating collaboration and responding to it.
Fig. 5.
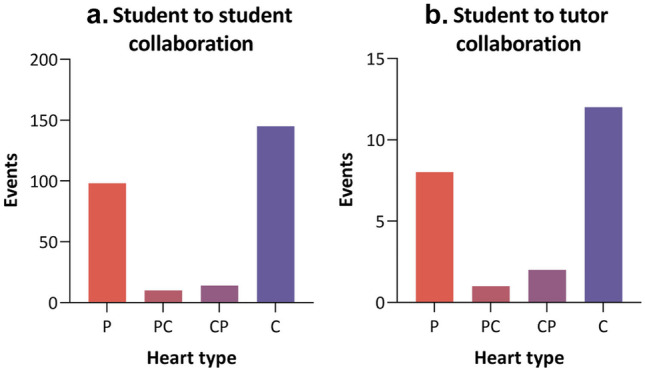
The heart model types used in a collaborative setting, including a between students and b between students and tutors. P, 3D printed heart; C, cadaveric heart; PC, 3D printed then cadaveric heart; CP, cadaveric then 3D printed heart
Discussion
We used a mixed methods approach to understand the preferences of medical students when presented with a choice between 3D printed and cadaveric hearts. Through the novel application of computer vision analysis, we found that the overall amount of time each type of heart was held was comparable but overall students favored cadaveric samples. The preference for cadaveric models is particularly prevalent in the results from structured observation towards the end of the workshop. Structured observation showed that early in the session most students chose to pick up 3D printed hearts but shifted towards favoring cadaveric hearts by the end of the tutorial. Most students chose to interact and collaborate with either the printed or cadaveric hearts, suggesting that these are equivalent in this context. Our results contrast to many studies that found the stated preferences of medical students were for 3D printed anatomy models over other forms [14].
Studies investigating the utility of 3D printed anatomy and pathology teaching materials in medical education indicate that students tend to prefer 3D printed models over conventional materials, but these studies are typically limited to quizzes and questionnaires [14, 21]. One systematic review finding is that 5 out of 6 studies showed improved satisfaction with 3D printed models over conventional methods [14]. Contrary to studies that found a stated preference for 3D printed models, we found that preferences tended towards cadaveric hearts, which could be due to several reasons. Satisfaction and preferences are often captured using Likert scales, which can be confounded by social desirability bias as students respond with what they think the investigators want to hear [21]. In addition, our study is unique as it captured real time student preferences over the course of the workshop rather than being a reflection or subjective measure after the fact.
The 3D printing method chosen led to models being uniformly cream colored, with some print artefacts visible, as opposed to the brown coloring of the aged cadaveric hearts, meaning that the preference towards cadaveric hearts could be due to the appearance of the models. Some small details of the hearts, such as the smaller papillary muscles, were lost in the translation to 3D model and were limited by the 3D printed method chosen (material extrusion tip size, smallest detail possible was 0.1778 mm wide); however, such details are usually not pedagogically relevant for the learning objectives of this workshop.
The participants’ observed behavior could be attributed to curiosity and novelty. Curiosity could offer a rationale for why students chose to interact with both types of hearts in earlier trays, prior to deciding about which one they preferred in later trays. It is possible, given the students’ prior experience with cadaveric models, that initial preferences for printed models were a result of novelty — 3D printed models may have been a new phenomenon to them in a formal educational context. Nevertheless, the total time spent by participants interacting with each heart and their selection of hearts in the final tray indicate that the preference for different hearts is comparable, despite a skew towards cadaveric. Alternatively, initial preferences for printed models could be attributed to students being uncomfortable handling cadaveric models, or concerns about damaging precious, finite samples. The students may have felt the need to acclimatize themselves to handling a cadaveric specimen and the 3D printed model assisted with this. This latter point about concern for samples is also supported by rougher handing of printed hearts compared to the cadaveric hearts. Students were seemingly more willing to manipulate the printed hearts without fear of causing damage.
Although there was a slight preference to the cadaveric heart models over time, the 3D printed hearts were comparable when considering interactions (e.g., using pipecleaners) and collaboration with tutors. This has significant implications when it comes to future workshops and supports our further use of these models. Once the cadaveric heart samples have been digitized, their three-dimensional form has become immortalized and the use of 3D printing enables infinite reproduction of these precious samples. 3D printed models can be used to produce multiple replicates of a single model that can be used in a shared learning experience. The 3D printed models can be distributed to sites that may not be able to maintain a cadaveric teaching collection, improving the equity of access for regional and remote teaching sites. Further, 3D printed models can be easily cleaned (increasingly important following the COVID-19 pandemic), stored, shipped, and can be replaced when broken. We believe that 3D printed anatomy and pathology models play an important role in augmenting traditional cadaver-based medical teaching practices.
Our study is not without limitations. While our structured observation was able to distinguish between free and forced choice (for instance, if students shared the heart models in a tray), our computer vision approach was not able to do this. As such, our computer vision analysis reflects the hearts that were held, as opposed to the hearts that were chosen to be held. We also did not directly ask students as to their preferences of heart type following the study, and thus had to infer student preference based on their actions. However, as students were not aware of what we were researching they were not creating bias in their responses (i.e., social desirability bias; telling us what they thought we wanted to hear). Our study did not include any pre- or post-testing of the students’ knowledge of congenital heart defects, so we are unable to assess any impacts on educational outcomes. Our GoPro device recordings were fish-eye distorted, which limited the spatial information we could assess, such as velocity and acceleration of the heart models.
Future research could focus on the impact of different 3D printing methods with the heart models (such as multi-material and color prints) on student engagement and preferencing. One future line of inquiry would be to increase the overall fidelity of the observational data, allowing for assessment of granular spatial information as it relates to the handling of the hearts. For example, the exact rotation and motion of the heart could be observed to derive more exact measures of participant handling. Another would be to include cultural and emotional evaluations in the study protocol, allowing for analysis of participants’ emotional state and culture-based responses to the models.
Conclusion
In this paper, we investigate students’ preferences between 3D printed and cadaveric hearts in a cardiac pathology practical skills workshop. We used structured observation and object detection to assess how students interacted with the two types of models, and whether students had a preference for either type of model. We found that while students used cadaveric hearts slightly more, in most aspects we explored, such as duration of use and types of interaction, the models were largely comparable. These results support the use of 3D printed models for medical education, especially in areas with limited capacity to support cadaveric samples.
Acknowledgements
Most importantly, the authors wish to sincerely thank the donors of the cadaveric samples and families, whose legacy allows us to stand on the shoulders of giants. Their contribution has been immortalized and will enable us to teach many future generations of medical professionals. The authors would like to thank Rachel Fitzpatrick from Radiography at the Children’s Hospital at Westmead for her support in CT scanning the heart models, Michael Krivanek and Nicole Graf from the Pathology Department at the Children’s Hospital at Westmead for their expertise and support with the cadaveric samples, Caleb Lapointe and Philip Williams from the Kids Simulation Australia at Sydney Children’s Hospitals Network for their advice and support in running the seminars, Jennifer Anderson at the Children’s Hospital at Westmead for her enthusiasm and encouragement for this study, and David Lahoud for his help with structured observations.
Author Contribution
Erez Nusem: study concept and design, acquisition of data, data analysis, drafting and editing of manuscript, approval of article. Liam Bray: data analysis, drafting and editing of manuscript, approval of article. Jonathon Lillia: data analysis, drafting and editing of manuscript, approval of article. Luke Schofield: data analysis, editing of manuscript, approval of article. Karen M. Scott: study concept and design, acquisition of data, data analysis, editing of manuscript, approval of article. Hasantha Gunasekera: study concept and design, acquisition of data, data analysis, editing of manuscript, approval of article. Tegan L. Cheng: study concept and design, acquisition of data, data analysis, drafting and editing of manuscript, approval of article.
Availability of Data
The datasets generated during and/or analyzed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author on reasonable request.
Declarations
Ethics Approval and Consent to Participate
Ethics approval was received from the Sydney Children’s Hospitals Network Human Research Ethics Committee (protocol LNR/18/SCHN/337).
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Winkelmann A. Anatomical dissection as a teaching method in medical school: a review of the evidence. Med Educ. 2007;41(1):15–22. doi: 10.1111/j.1365-2929.2006.02625.x. [DOI] [PubMed] [Google Scholar]
- 2.McMenamin PG, et al. The production of anatomical teaching resources using three-dimensional (3D) printing technology. Anat Sci Educ. 2014;7(6):479–486. doi: 10.1002/ase.1475. [DOI] [PubMed] [Google Scholar]
- 3.Vaccarezza M, Papa V. 3D printing: a valuable resource in human anatomy education. Anat Sci Int. 2015;90(1):64–65. doi: 10.1007/s12565-014-0257-7. [DOI] [PubMed] [Google Scholar]
- 4.McMenamin PG, et al. The reproduction of human pathology specimens using three-dimensional (3D) printing technology for teaching purposes. Med Teach. 2021;43(2):189–197. doi: 10.1080/0142159X.2020.1837357. [DOI] [PubMed] [Google Scholar]
- 5.Raja DS, Sultana B. Potential health hazards for students exposed to formaldehyde in the gross anatomy laboratory. J Environ Health. 2012;74(6):36–41. [PubMed] [Google Scholar]
- 6.Garcia J, et al. 3D printing materials and their use in medical education: a review of current technology and trends for the future. BMJ Simul Technol Enhanc Learn. 2018;4(1):27–40. doi: 10.1136/bmjstel-2017-000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garas M, et al. 3D-printed specimens as a valuable tool in anatomy education: a pilot study. Ann Anat. 2018;219:57–64. doi: 10.1016/j.aanat.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 8.AbouHashem Y, et al. The application of 3D printing in anatomy education. Med Educ Online. 2015;20(1):29847. doi: 10.3402/meo.v20.29847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O'Reilly MK, et al. Fabrication and assessment of 3D printed anatomical models of the lower limb for anatomical teaching and femoral vessel access training in medicine. Anat Sci Educ. 2016;9(1):71–79. doi: 10.1002/ase.1538. [DOI] [PubMed] [Google Scholar]
- 10.Lim KH, et al. Use of 3D printed models in medical education: a randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. Anat Sci Educ. 2016;9(3):213–221. doi: 10.1002/ase.1573. [DOI] [PubMed] [Google Scholar]
- 11.Smith CF, et al. Take away body parts! An investigation into the use of 3D-printed anatomical models in undergraduate anatomy education. Anat Sci Educ. 2018;11(1):44–53. doi: 10.1002/ase.1718. [DOI] [PubMed] [Google Scholar]
- 12.Preece D, et al. “Let's Get Physical”: advantages of a physical model over 3D computer models and textbooks in learning imaging anatomy. Anat Sci Educ. 2013;6(4):216–224. doi: 10.1002/ase.1345. [DOI] [PubMed] [Google Scholar]
- 13.Chen S, et al. The role of three-dimensional printed models of skull in anatomy education: a randomized controlled trail. Sci Rep. 2017;7(1):575. doi: 10.1038/s41598-017-00647-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye Z, et al. The role of 3D printed models in the teaching of human anatomy: a systematic review and meta-analysis. BMC Med Educ. 2020;20(1):335. doi: 10.1186/s12909-020-02242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aung HH, Tin MH. A comparative study of teaching anatomy using cadavers, prosected wet specimens and simulated plastic models among Malaysian undergraduates. In: IRIIE 2012, 21-22 February 2012, Cultural Activities Centre, International Islamic University Malaysia. (Unpublished); 2012. http://irep.iium.edu.my/27151/.
- 16.Ponitz CC, et al. A structured observation of behavioral self-regulation and its contribution to kindergarten outcomes. Dev Psychol. 2009;45(3):605–619. doi: 10.1037/a0015365. [DOI] [PubMed] [Google Scholar]
- 17.Kuznetsova A, Maleva T, Soloviev V. Detecting apples in orchards using YOLOv3 and YOLOv5 in general and close-up images. Cham: Springer International Publishing; 2020. [Google Scholar]
- 18.Bryman A. Social research methods. Oxford University Press; 2012. p. 269–287.
- 19.Viola P, Jones M. Robust real-time object detection. 2001. https://www.cs.cmu.edu/~efros/courses/LBMV07/Papers/viola-IJCV-01.pdf.
- 20.Everingham M, et al. The Pascal visual object classes (VOC) challenge. Int J Comput Vision. 2010;88(2):303–338. doi: 10.1007/s11263-009-0275-4. [DOI] [Google Scholar]
- 21.Fleming C, et al. Effectiveness of three-dimensionally printed models in anatomy education for medical students and resident physicians: systematic review and meta-analysis. J Am Coll Radiol. 2020;17(10):1220–1229. doi: 10.1016/j.jacr.2020.05.030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author on reasonable request.