The COVID-19 pandemic led to significant reductions in sexually transmitted infection testing rates and fewer diagnoses of chlamydia, gonorrhea, and HIV, but compared with prepandemic periods, syphilis diagnosis rates increased by 32%.
Abstract
We evaluated changes in rates of testing and diagnoses of sexually transmitted infections during the 2017–2020 period at Kaiser Permanente Southern California. During the COVID-19 pandemic period, we observed profound reductions in testing and fewer diagnoses of chlamydia, gonorrhea, and HIV compared with prepandemic periods, but syphilis diagnoses rates increased by 32%.
In the United States over the past decade, significant increases in sexually transmitted infection (STI) rates and persistent HIV incidence have posed complex challenges to public health.1,2 The synergy between STI and HIV transmission is well described, and control efforts require routine screening, linkage to care, and early treatment.
The ongoing COVID-19 pandemic has disrupted health care access and delivery, impacting sexual health prevention and treatment services.3–9 Utilization of routine screening has been affected by provider-driven shifts in the availability of face-to-face visits and patient-driven concerns about accessing health care safely. Strained public health resources were diverted from STI programs toward COVID-19 mitigation efforts.10 Furthermore, shortages of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) testing materials11 required some clinics to limit STI screening when supplies were unavailable or were prioritized for SARS-CoV-2 testing.
Widespread testing and early diagnosis of STIs and HIV are necessary to curb STI incidence and end the HIV epidemic. To inform strategies to improve STI/HIV outcomes in the context of the ongoing COVID-19 pandemic, we evaluated changes in testing and diagnosis rates for syphilis, chlamydia, gonorrhea, and HIV during the 2017–2020 period in Southern California.
METHODS
Study Setting
Kaiser Permanente Southern California (KPSC) is an integrated health system that provides health care and insurance to more than 4.7 million members with diverse socioeconomic and racial/ethnic backgrounds, similar to the underlying population.12 Members are enrolled through employer-provided, prepaid, or federally sponsored insurance plans. Comprehensive electronic health records capture details of health services received across inpatient and outpatient settings.
The guidelines of KPSC for STI and HIV testing are aligned with national guidelines, recommending that all adults should be tested for HIV at least once during their life, and more frequently based on sexual practices.13,14 Testing for syphilis, chlamydia, and gonorrhea is recommended based on sexual practices. Quarterly STI testing is also recommended for individuals taking preexposure prophylaxis for HIV prevention.
At the onset of the COVID-19 pandemic, a local emergency was declared in Los Angeles County, with closures of dining and entertainment venues beginning March 15, 2020. Kaiser Permanente Southern California responded by increasing SARS-CoV-2 testing, postponing nonessential procedures, and, when possible, shifting care delivery to virtual platforms. Statewide stay-at-home orders were implemented between March 19, 2020, and June 12, 2020, and again after the start of the second COVID-19 surge on November 21, 2020.
Study Design
We conducted a retrospective study among an open cohort of KPSC members age 12 years or older during the January 1, 2017–December 31, 2020 period. We defined the period March 1, 2020, to December 31, 2020, as the COVID-19 pandemic period and examined changes in rates of STI and HIV testing and diagnoses during this period compared with prepandemic periods (January 1, 2017–December 31, 2017; January 1, 2018–December 31, 2018; and January 1, 2019–February 29, 2020), to evaluate longitudinal trends in testing and diagnosis of STIs/HIV. The KPSC Institutional Review Board approved this study, waiving the written informed consent requirement.
Study Variables
We identified STI/HIV laboratory tests and diagnoses from electronic health record. Individuals could have multiple tests performed during the study period. Incident syphilis was defined using the reverse sequence algorithm.15 We excluded multiple syphilis diagnoses occurring within a 3-month period. Incident chlamydia and gonorrhea were defined by newly positive nucleic acid amplification test results from genital or extragenital sites sampled if there were no other positive results within the prior 30 days, or if the most recent result was negative. HIV diagnosis was based on the Abbott Architect fourth-generation HIV antigen/antibody combination test and the KPSC HIV/AIDS registry, which identifies new infections.
Statistical Analysis
We calculated rates as the number of events (tests performed or new diagnoses) per 100,000 person-years, accounting for the number of KPSC members within each period. For each prepandemic period and the pandemic period, we assessed percent change compared with the period immediately prior. We used log-linear Poisson regression with generalized estimating equations to estimate rate ratios and 95% confidence intervals (CIs) for each outcome, comparing the pandemic period with the combined prepandemic periods. Data were analyzed using SAS (Version 9.4 for Unix; SAS Institute, Cary, NC).
RESULTS
During the COVID-19 pandemic period, ≥1 tests were performed for 212,215 individuals for syphilis, 258,720 for chlamydia, 258,656 for gonorrhea, and 225,949 for HIV; ≥1 diagnoses occurred among 3019 individuals for syphilis, 11,448 for chlamydia, 3422 for gonorrhea, and 347 for HIV (Supplemental Table 1, http://links.lww.com/OLQ/A824). A majority of individuals tested were aged 20 to 44 years (>70%) and were women (>60%). Although 61% of individuals with chlamydia diagnoses were women, men comprised 66% of those with gonorrhea, 86% of those with syphilis, and 91% of those with HIV. Individuals with Hispanic ethnicity comprised 46% to 49% of those tested and 43% to 52% of those with STI or HIV diagnoses, reflecting the Southern California population.
Similar distributions of demographic characteristics were observed in the 3 prepandemic periods (Supplemental Table 1, http://links.lww.com/OLQ/A824). Longitudinal trends in the prepandemic periods showed steady, modest increases in testing for all STIs/HIV (Table 1; Supplemental Fig. 1, http://links.lww.com/OLQ/A824). We also observed increases in the diagnosis of chlamydia and syphilis and declines in the diagnosis of gonorrhea and HIV before the pandemic.
TABLE 1.
Incidence Rates of Testing and Diagnoses of Syphilis, Chlamydia, Gonorrhea, and HIV During the January 1, 2017–December 31, 2020 Period
| n (Individuals) | Total Person-Years | Tests | Test Rate Per 100,000 Person-Years | Percent Change in Test Rate* | Diagnoses | Diagnoses Rate Per 100,000 Person-Years | Percent Change in Diagnoses Rate* | |
|---|---|---|---|---|---|---|---|---|
| Syphilis | ||||||||
| January 1, 2017–December 31, 2017 | 4,193,334 | 3,682,191 | 324,391 | 8810 | N/A | 2327 | 63 | N/A |
| January 1, 2018–December 31, 2018 | 4,337,202 | 3,809,580 | 351,512 | 9227 | 5 | 2650 | 70 | 10 |
| January 1, 2019–February 29, 2020 | 4,609,736 | 4,526,681 | 468,765 | 10,356 | 12 | 3507 | 77 | 11 |
| March 1, 2020–December 31, 2020 | 4,327,412 | 3,318,538 | 261,231 | 7872 | −24 | 3056 | 92 | 19 |
| Chlamydia | ||||||||
| January 1, 2017–December 31, 2017 | 4,193,334 | 3,682,191 | 534,177 | 14,507 | N/A | 18,247 | 496 | N/A |
| January 1, 2018–December 31, 2018 | 4,337,202 | 3,809,580 | 575,767 | 15,114 | 4 | 19,843 | 521 | 5 |
| January 1, 2019–February 29, 2020 | 4,609,736 | 4,526,681 | 715,087 | 15,797 | 5 | 23,815 | 526 | 1 |
| March 1, 2020–December 31, 2020 | 4,327,412 | 3,318,538 | 344,776 | 10,389 | −34 | 12,167 | 367 | −30 |
| Gonorrhea | ||||||||
| January 1, 2017–December 31, 2017 | 4,193,334 | 3,682,191 | 534,177 | 14,507 | N/A | 4439 | 121 | N/A |
| January 1, 2018–December 31, 2018 | 4,337,202 | 3,809,580 | 575,768 | 15,114 | 4 | 4563 | 120 | −1 |
| January 1, 2019–February 29, 2020 | 4,609,736 | 4,526,681 | 715,082 | 15,797 | 5 | 5202 | 115 | −4 |
| March 1, 2020–December 31, 2020 | 4,327,412 | 3,318,538 | 344,668 | 10,386 | −34 | 3638 | 110 | −5 |
| HIV | ||||||||
| January 1, 2017–December 31, 2017 | 4,193,334 | 3,682,191 | 366,329 | 9949 | N/A | 538 | 15 | N/A |
| January 1, 2018–December 31, 2018 | 4,337,202 | 3,809,580 | 392,993 | 10,316 | 4 | 532 | 14 | −4 |
| January 1, 2019–February 29, 2020 | 4,609,736 | 4,526,681 | 490,785 | 10,842 | 5 | 622 | 14 | −2 |
| March 1, 2020–December 31, 2020 |
4,327,412 | 3,318,538 | 257,013 | 7745 | −29 | 347 | 10 | −24 |
*Change in rate compared with prior time period.
N/A indicates not available.
However, during the pandemic period, steep declines in testing rates were observed for all STIs/HIV (Table 1), especially in the first 3 months of the pandemic (Supplemental Fig. 1, http://links.lww.com/OLQ/A824). The rate of syphilis testing (7872 per 100,000 person-years) during the pandemic period was 24% lower than the rate during the prior January 1, 2019–February 29, 2020 period. Rates of chlamydia testing (10,389 per 100,000 person-years) and gonorrhea testing (10,386 per 100,000 person-years) during the pandemic period were both 34% lower compared with the prior period, and the rate of HIV testing (7745 per 100,000 person-years) was 29% lower compared with the prior period. Rate ratio (95% CI) comparing rates of testing during the pandemic with rates in the combined prepandemic periods were 0.83 (0.83–0.84) for syphilis, 0.69 (0.68–0.69) for both chlamydia and gonorrhea, and 0.75 (0.74–0.75) for HIV (Fig. 1).
Figure 1.
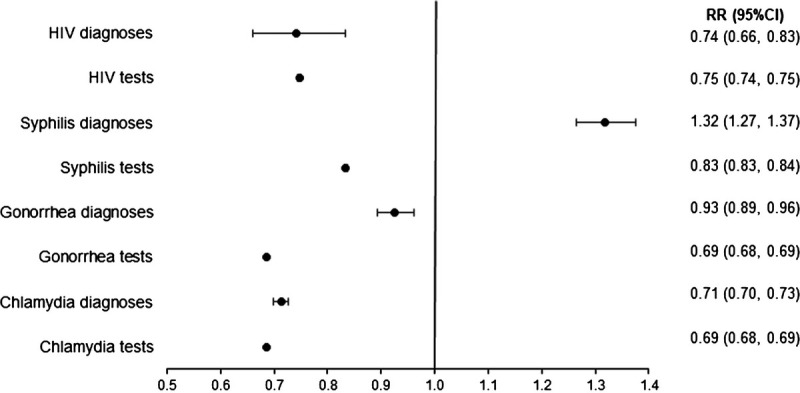
Rate ratios for STI/HIV testing and diagnoses during the COVID-19 pandemic period (March 1, 2020–December 31, 2020) compared with the combined prepandemic periods (January 1, 2017–February 29, 2020).
We also observed changes during the pandemic in rates of new STI and HIV diagnoses (Table 1). During the pandemic period, rates of syphilis diagnoses (92 per 100,000 person-years) were 19% higher than rates during the prior January 1, 2019–February 29, 2020 period. Rates of chlamydia diagnoses (367 per 100,000 person-years) and HIV diagnoses (10 per 100,000 person-years) were 30% and 24% lower, respectively, during the pandemic compared with the prior period, and rates of gonorrhea diagnoses (110 per 100,000 person-years) were 5% lower compared with the prior period. Rate ratio (95% CI) comparing rates of diagnoses during the pandemic with rates in the combined prepandemic periods were 1.32 (1.27–1.37) for syphilis, 0.71 (0.70–0.73) for chlamydia, 0.93 (0.89–0.96) for gonorrhea, and 0.74 (0.66–0.83) for HIV (Fig. 1).
DISCUSSION
Our findings suggest widespread underutilization of testing, likely leading to underdiagnosis of chlamydia and HIV in Southern California during the COVID-19 pandemic. Given decreased diagnoses of chlamydia and HIV, relatively stable diagnoses of gonorrhea despite decreased testing, and increased diagnoses of syphilis despite decreased testing, we infer that sexual behavior and activity during the 10-month pandemic period may not have declined substantially from the prepandemic period. Rather, STI/HIV testing declined steeply, more likely because of changes in health care delivery, systemic supply shortages for STI testing, and care-seeking behavior. These findings have concerning implications for onward transmission of undiagnosed STI/HIV within sexual networks, specifically for chlamydia and HIV, and may result in reproductive tract sequelae in women and repercussions for Ending the HIV Epidemic efforts.
Symptom-driven testing may help explain the observed differences in patterns of testing and diagnoses in our study. Although chlamydia and HIV diagnoses rates markedly declined during the pandemic period, the percent change in gonorrhea diagnoses rates was not substantially different from 2019 (5% lower). For syphilis, a higher-than-expected percent increase (19%) was observed from 2019 to 2020, compared with an 11% increase in diagnoses from 2018 to 2019. Gonorrhea and syphilis may have longer symptomatic periods than chlamydia (often asymptomatic) or HIV (likely symptomatic in early or late stages, interspersed by clinically silent periods). Individuals with symptoms may have been more likely to seek testing, whereas routine screening for asymptomatic individuals may have been less prioritized even as the pandemic continued.
Our study is consistent with other studies that found reductions in STI/HIV testing and diagnoses early in the COVID-19 pandemic, in that we observed substantial declines in testing in the first 3 months of the pandemic.3–5,7,9 A study of US national reference clinical laboratory data found that chlamydia and gonorrhea testing declined to 60% of prepandemic levels in April 2020, recovering to approximately 85% of prepandemic levels in June 2020; the authors estimated that 26.4% of chlamydia and 16.5% of gonorrhea cases were potentially missed.3 In King County, Washington, declines in STI diagnoses from March to June 2020 were largely attributed to declines in asymptomatic screening.9 Similarly, in New York City, reductions were observed in HIV/STI from March to June 2020, with infections rebounding to similar or higher levels than in 201916; in contrast, in our study including a longer pandemic period, chlamydia and HIV diagnoses did not fully rebound through December 2020.
This study has several limitations and strengths. First, we were unable to ascertain the stage at which syphilis was diagnosed, as diagnosis was based on laboratory data rather than clinical information or diagnoses codes. Thus, it was not possible to determine whether increases in syphilis diagnosis rates occurred for both latent and symptomatic stages. Second, KPSC members may have sought STI and HIV testing outside of KPSC, potentially underestimating rates in our study. However, because KPSC is a prepaid system, members are incentivized to seek care within KPSC. Furthermore, the COVID-19 pandemic disrupted sexual health services at both public health and KPSC clinics, such that misclassification likely had a minimal impact on rate ratios comparing outcomes during pandemic versus prepandemic periods. Third, although KPSC members might have had better access to care than uninsured or underinsured individuals, who might have experienced even more profound decreases in STI/HIV testing during the COVID-19 pandemic, the generalizability of our study is enhanced by the large, demographically and socioeconomically diverse cohort receiving comprehensive care at KPSC. Fourth, a strength of our study is that we included both positive and negative STI/HIV test results in our analysis, which is often not possible when using public health surveillance data.
In conclusion, during the first year of the COVID-19 pandemic, we observed profound reductions in testing and diagnoses of chlamydia, gonorrhea, and HIV. Despite reduced testing, rates of syphilis diagnoses increased substantially, suggesting that the syphilis epidemic continues to worsen. Our findings indicate widespread underdiagnosis of STIs and HIV during the ongoing COVID-19 pandemic, highlighting the need for innovative strategies to improve early detection and treatment.
Footnotes
This work was supported by the Regional Research Committee of Kaiser Permanente Southern California (grant number KP-RRC-20201006).
Conflict of Interest and Sources of Funding: J.J.C. and Q.C. have no conflicts of interest to declare. R.C.H. has received funding from Gilead for unrelated research. J.D.-O. has funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development for unrelated research. K.J.B. has received funding from Gilead, Dynavax, GlaxoSmithKline, Moderna, and Pfizer for unrelated research.
Conference Presentations: Oral abstract presentation at CROI 2022.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://www.stdjournal.com).
Contributor Information
Jennifer J. Chang, Email: Jennifer.Jiwen.Chang@kp.org.
Qiaoling Chen, Email: Qiaoling.Chen@kp.org.
Jodie Dionne-Odom, Email: jdionne@uabmc.edu.
Rulin C. Hechter, Email: Rulin.C.Hechter@kp.org.
REFERENCES
- 1.Centers for Disease Control and Prevention . Sexually Transmitted Disease Suveillance 2019. Atlanta, GA: US Department of Health and Human Services, 2021. [Google Scholar]
- 2.Centers for Disease Control and Prevention . HIV Surveillance Report, 2019:32. Available at: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2021. Accessed May 6, 2022.
- 3.Pinto CN Niles JK Kaufman HW, et al. Impact of the COVID-19 pandemic on chlamydia and gonorrhea screening in the U.S. Am J Prev Med 2021; 61:386–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitlock GG McOwan A Nugent D, Dean Street Collaborative Group . Gonorrhoea during COVID-19 in London, UK. Sex Transm Infect 2021; 97:622–623. [DOI] [PubMed] [Google Scholar]
- 5.Chow EPF Ong JJ Denham I, et al. HIV testing and diagnoses during the COVID-19 pandemic in Melbourne, Australia. J Acquir Immune Defic Syndr 2021; 86:e114–e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Baetselier I Apers L Platteau T, et al. The impact of physical restriction measures imposed during the two waves of COVID-19 on chlamydia and gonorrhea diagnoses in Belgium. Results of an sexually transmitted infection clinic. Int J STD AIDS 2021; 32:998–1003. [DOI] [PubMed] [Google Scholar]
- 7.Sentis A Prats-Uribe A Lopez-Corbeto E, et al. The impact of the COVID-19 pandemic on sexually transmitted infections surveillance data: Incidence drop or artefact? BMC Public Health 2021; 21:1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill BJ, Anderson B, Lock L. COVID-19 pandemic, pre-exposure prophylaxis (PrEP) care, and HIV/STI testing among patients receiving care in Three HIV epidemic priority states. AIDS Behav 2021; 25:1361–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berzkalns A Thibault CS Barbee LA, et al. Decreases in reported sexually transmitted infections during the time of COVID-19 in King County, WA: Decreased transmission or screening? Sex Transm Dis 2021; 48:S44–S49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson KA Burghardt NO Tang EC, et al. Measuring the impact of the COVID-19 pandemic on sexually transmitted diseases public health surveillance and program operations in the state of California. Sex Transm Dis 2021; 48:606–613. [DOI] [PubMed] [Google Scholar]
- 11.Bachmann LH, Bolan G. Pages. 2020. Available at: https://www.cdc.gov/std/general/DCL-Diagnostic-Test-Shortage.pdf. Accessed October 28, 2021.
- 12.Koebnick C Langer-Gould AM Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: Comparison with US Census Bureau data. Perm J 2012; 16:37–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Workowski KA Bachmann LH Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 2021; 70:1–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Preventive Services Task Force . Screening for HIV infection: US Preventive Services Task Force recommendation statement. JAMA 2019; 321:2326–2336. [DOI] [PubMed] [Google Scholar]
- 15.Park IU Chow JM Bolan G, et al. Screening for syphilis with the treponemal immunoassay: Analysis of discordant serology results and implications for clinical management. J Infect Dis 2011; 204:1297–1304. [DOI] [PubMed] [Google Scholar]
- 16.Braunstein SL Slutsker JS Lazar R, et al. Epidemiology of reported HIV and other sexually transmitted infections during the COVID-19 pandemic. New York City J Infect Dis 2021; 224:798–803. [DOI] [PMC free article] [PubMed] [Google Scholar]


