OBJECTIVES:
Few surveys have focused on physician moral distress, burnout, and professional fulfilment. We assessed physician wellness and coping during the COVID-19 pandemic.
DESIGN:
Cross-sectional survey using four validated instruments.
SETTING:
Sixty-two sites in Canada and the United States.
SUBJECTS:
Attending physicians (adult, pediatric; intensivist, nonintensivist) who worked in North American ICUs.
INTERVENTION:
None.
MEASUREMENTS AND MAIN RESULTS:
We analysed 431 questionnaires (43.3% response rate) from 25 states and eight provinces. Respondents were predominantly male (229 [55.6%]) and in practice for 11.8 ± 9.8 years. Compared with prepandemic, respondents reported significant intrapandemic increases in days worked/mo, ICU bed occupancy, and self-reported moral distress (240 [56.9%]) and burnout (259 [63.8%]). Of the 10 top-ranked items that incited moral distress, most pertained to regulatory/organizational (n = 6) or local/institutional (n = 2) issues or both (n = 2). Average moral distress (95.6 ± 66.9), professional fulfilment (6.5 ± 2.1), and burnout scores (3.6 ± 2.0) were moderate with 227 physicians (54.6%) meeting burnout criteria. A significant dose-response existed between COVID-19 patient volume and moral distress scores. Physicians who worked more days/mo and more scheduled in-house nightshifts, especially combined with more unscheduled in-house nightshifts, experienced significantly more moral distress. One in five physicians used at least one maladaptive coping strategy. We identified four coping profiles (active/social, avoidant, mixed/ambivalent, infrequent) that were associated with significant differences across all wellness measures.
CONCLUSIONS:
Despite moderate intrapandemic moral distress and burnout, physicians experienced moderate professional fulfilment. However, one in five physicians used at least one maladaptive coping strategy. We highlight potentially modifiable factors at individual, institutional, and regulatory levels to enhance physician wellness.
Keywords: burnout, coping, moral distress, pandemic, wellness
KEY POINTS.
Question: We assessed the wellness and coping of physicians who worked in the ICU during the COVID-19 pandemic.
Findings: Physicians experienced, moderate intra-pandemic moral distress, burnout, and professional fulfillment. One in 5 physicians used at least one maladaptive coping strategy. Based on frequency of use of coping strategies, we identified 4 coping profiles (active/social, avoidant, mixed/ambivalent, infrequent) that were associated with significant differences across all wellness measures.
Meaning: Despite moderate intra-pandemic moral distress and burnout, physicians also experienced moderate professional fulfillment during the pandemic. We highlight potentially modifiable factors at individual, institutional, and regulatory levels to enhance physician wellness.
Physician wellness is recognized as an important facet of career satisfaction (1). Moral distress occurs when an individual feels constrained to act or refrain from acting, in contradiction to his/her ethical values (1–4). Common circumstances that incite moral distress for healthcare providers pertain to end-of-life care, failures of workplace, and pressures to reduce costs (5). Burnout is associated with moral distress and is characterized by emotional exhaustion, depersonalization, a reduced sense of personal accomplishment in the workplace (4, 6–9) and develops over time (10). Consequences of burnout range from minor (e.g., detachment from one’s work) (7) to catastrophic (e.g., depression, addiction, and suicide) (6). Professional fulfilment is the satisfaction that individuals feel when they have achieved or are attaining their career goals (11). Coping is broadly defined as efforts that are used to minimize distress associated with negative life experiences (12). Strategies that augment professional fulfilment or enhance coping have been advanced as methods for organizations and individuals to reduce burnout (6, 13).
The COVID-19 pandemic (6, 10, 14, 15) exposed a lack of disaster preparedness in hospitals globally (16). Increased patient volume necessitated development of real-time strategies to increase ICU capacity resulting in changes to personnel, work flow, and workplace culture (6, 11, 14, 16, 17). Wellness surveys typically focus on the diverse and more numerate nonphysician healthcare providers (5, 10) with only limited data on the moral distress (3–5), burnout (4, 18), resilience (4, 18), and compassion fatigue (4) of ICU physicians. To address this gap, we conducted a binational, cross-sectional survey of physicians who worked in North American ICUs to characterize the impact of the pandemic on physician wellness and coping.
MATERIALS AND METHODS
We used rigorous survey methodology to design, test, and administer our questionnaire (19, 20, 21). The study protocol was approved by the Executive Committee of the American Thoracic Society (ATS). The survey was reviewed, and the need for approval was waived (September 25, 2020) by the Ethics review by the Health Sciences Integrated Research Ethics Board (Hamilton, Canada). The survey was implemented in accordance with the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans (22) and with the Declaration of Helsinki (23). The study protocol was approved by the Executive Committee of the ATS (November 23, 2020).
Sampling Frame
We used a multimodal approach (Women in Critical Care [WICC] Interest Group of the ATS membership list, colleague referrals, electronic mail correspondence) to identify site leads. Site leads distributed an electronic questionnaire locally to the larger of one third of attending physicians in their ICUs or at least 10 potential respondent. We excluded nonphysicians, physicians-in-training, and physicians who did not care for ICU patients or were no longer in practice.
Questionnaire Development and Testing
The questionnaire included four validated instruments: the 27-item Measure of Moral Distress for Healthcare Professionals (24), two-item version of the Maslach Burnout Inventory (MBI) (25), 14-item Stanford Professional Fulfilment Index (PFI) (26), and the 14-item Brief Cope scale (12) to assess moral distress, burnout alone, professional fulfilment and burnout, and coping. We collected demographic data about respondents, their practice type and setting, and workload.
We pilot tested the questionnaire with three WICC members to assess flow, salience, and acceptability and assessed its clinical sensibility (comprehensiveness, clarity, and face validity) with three other WICC members. The final questionnaire (59 instrument, 25 demographic items) was formatted in Qualtrics (Provo, UT) in English with nominal, ordinal, and open-ended response formats (Appendix 1, http://links.lww.com/CCM/H202).
Questionnaire Administration
Sixty-two site leads sent a prenotification e-mail (February 6 or 7, 2021), a unique “site lead” link to the initial questionnaire (February 10 or 12, 2021), reminder e-mails (February 24, March 13, March 24, 2021), and up to three optional nudges for questionnaire completion, at 2–3 week intervals, to potential respondents before survey closure (April 16, 2021).
Statistical Analysis
We collapsed responses (a few times a month or more) to report emotional exhaustion, depersonalization and average burnout scores (seven-point scale) using the MBI (25). To summarize Stanford PFI (26) responses, we collapsed response options (moderately, a lot, and extremely) for professional fulfilment (sixitems), work exhaustion (four items), and interpersonal disengagement (six items). We report professional fulfilment and burnout (combined work exhaustion and interpersonal disengagement scores: 10-point scale) using the Stanford PFI with “lower” work exhaustion, “lower” interpersonal disengagement, and “higher” professional fulfilment scores representing desirable outcomes and a Burnout Subscale score greater than 3.3 identifying respondents who experienced burnout (26). We pooled responses (a little, medium amount, or a lot) to reflect use of coping strategies (12). We used the chi-square and Student t test to compare binary and continuous responses, respectively, and Spearman rho (27) to assess correlations between the MBI (25) and Stanford PFI (26). Data are presented using mean and sd unless specified otherwise.
We conducted univariate and multivariable analysis of variance (28) for comparisons between 1) intensivist versus nonintensivist physicians, 2) adult versus pediatric physicians, 3) University versus other hospitals, 4) high versus low days worked/mo (defined by median), 5) scheduled versus unscheduled night shifts (defined by median), and 6) COVID-19 patient volume (ordered categories) and average moral distress (24), professional fulfilment (26), and burnout scores (25, 26) with Bonferroni corrected p values. We used the paired-sample t test to compare days worked/mo and bed occupancy (pre vs intra pandemic) and ordinal logistic regression to assess trends between case load and wellness measures.
We derived profiles of respondents who used (somewhat frequently or more often) similar coping patterns using latent profile analysis and selected the model with an optimal number of profiles (29) using Akaike’s information criterion and Bayesian information criterion (30). Relationships between coping profiles and binary and continuous wellness measures were assessed using the chi-square test and the Brown-Forsythe test of equality of means, respectively. Analyses were performed using SPSS 76.0 (IBM SPSS Statistics for Windows, IBM Corp, Armonk, NY) and R Version 4.0.2 (tidyLPA, Version 1.0.8 [2020-08]; https://data-edu.github.io/tidyLPA/). Bonferroni-corrected p values of less than 0.05 were considered statistically significant.
RESULTS
Response Rate
We analyzed 431 questionnaires from 1,080 potential respondents (crude response rate 43.3%, analyzable response rate 40.0%) from 25 U.S. states and eight Canadian provinces completed in part or in full, and 33 opt out responses. We excluded four questionnaires (three completed by physicians-in-training and one duplicate).
Characteristics of Respondents, Workplaces, and Work Profiles
Respondents were predominantly male (229 [53.1%]), married/partnered (345 [80.0%]), and between the ages of 31–50 years (298 [69.1%]) (Table 1). Most respondents worked at University hospitals (334 [65.0%]) and were in practice 11.8 ± 9.8 years. Pre pandemic, most physicians cared for adult patients (87 [89.8%]) and had mixed (ICU + other) clinical practices (262 [60.8%]). Average ICU bed occupancy increased from 53.4 ± 43.7 pre pandemic to 76.1 ± 66.5 intrapandemic (p < 0.001). Compared with prepandemic, physicians reported an increase in the average number of days they worked/mo in the ICU during the pandemic (10.1 ± 13.9 to 13.1 ± 15.6; p < 0.001).
TABLE 1.
Characteristics of Respondents, Practices, and Workload
| n | % | |
|---|---|---|
| Respondent characteristics | ||
| Gender | ||
| Male | 229 | 53.1 |
| Female | 173 | 40.1 |
| Prefer not to respond | 10 | 2.3 |
| Missing | 19 | 4.4 |
| Age | ||
| < 30 | 2 | 0.5 |
| 31–40 | 153 | 35.5 |
| 41–50 | 145 | 33.6 |
| 51–60 | 69 | 16.0 |
| 61–70 | 30 | 7.0 |
| 71–80 | 6 | 1.4 |
| > 80 | 1 | 0.2 |
| Prefer not respond | 7 | 1.6 |
| Missing | 18 | 4.2 |
| Marital status | ||
| Single | 46 | 10.7 |
| Married/partnered/common law | 345 | 80.0 |
| Widowed | 1 | 0.2 |
| Divorced/separated | 11 | 2.6 |
| Prefer not to respond | 9 | 2.1 |
| Missing | 19 | 4.4 |
| Dependents | ||
| Yes | 264 | 61.3 |
| No | 139 | 32.3 |
| Missing | 21 | 4.9 |
| Prefer not to answer | 7 | 1.6 |
| Years in practice (mean ± sd) | 11.8 | 9.8 |
| Practice types and settings (select all that apply) | ||
| University hospital | 334 | 65.0 |
| Community hospital | 112 | 21.9 |
| Government/VA hospital | 49 | 9.5 |
| Missing | 19 | 3.7 |
| Adult practice | 387 | 89.8 |
| Pediatric/neonatal practice | 17 | 3.9 |
| Both | 8 | 1.9 |
| Missing | 19 | 4.4 |
| Clinical workload (mean ± sd) | ||
| ICU clinical work (days/mo) (year before March 1, 2020) | 10.1 | 13.9 |
| ICU clinical work (days/mo) (March 1, 2020 to questionnaire completion) | 13.1 | 15.6 |
Measure of Moral Distress
The average moral distress score was 95.6 ± 66.9 (maximum 417). Of the 10 top items that incited moral distress, most pertained to regulatory/organizational (n = 6), local/institutional (n = 2) issues, or both (n = 2) (Table 2). Compared with prepandemic, most physicians affirmed that their intrapandemic moral distress increased (240 (56.9%)] or remained similar [174 (41.2%)]. Some respondents (116 [27.2%] and 57 [13.4%]) considered leaving/left or were currently considering leaving their position due to moral distress, respectively.
TABLE 2.
Ranked Scores for Measure of Moral Distress for Healthcare Professionals Items
| Measure of Moral Distress—Healthcare Professionals Item | Mean | sd | Rank |
|---|---|---|---|
| Follow the family insistence to continue aggressive treatment even though it is not in the best interest of the patient. | 8.15 | 4.8 | 1 |
| Continue to provide aggressive treatment for a person who is most likely to die regardless of this treatment when no one will make a decision to withdraw it. | 7.04 | 4.9 | 2 |
| Experience lack of administrative action or support for a problem that is compromising patient care. | 5.11 | 5.1 | 3 |
| Experience compromised patient care due to lack of resources/equipment/bed capacity. | 4.92 | 5.0 | 4 |
| Be required to care for patients who have unclear or inconsistent treatment plans or who lack goals of care. | 4.81 | 4.3 | 5 |
| Have excessive documentation requirements that compromise patient care. | 4.64 | 5.0 | 6 |
| Participate in care that causes unnecessary suffering or does not adequately relieve pain or symptoms. | 4.59 | 4.3 | 7 |
| Feel pressured to order or carry out orders for that I consider to be unnecessary or inappropriate treatments. | 4.42 | 4.2 | 8 |
| Be required to care for more patient than I can safely care for. | 4.20 | 4.7 | 9 |
| Witness healthcare providers giving “false hope” to a patient or family. | 4.14 | 4.0 | 10 |
| Watch patient care suffer because of a lack of provider continuity. | 4.03 | 4.1 | 11 |
| Witness low quality of patient care due to poor team communication. | 3.81 | 4.0 | 12 |
| Be required to work with abusive patients/family members who are compromising quality of care. | 3.64 | 3.9 | 13 |
| Participate on a team that gives inconsistent messages to a patient/family. | 3.38 | 3.9 | 14 |
| Be required to work with other healthcare team members who are not as competent as patient care requires. | 3.32 | 4.1 | 15 |
| Be unable to provide optimal care due to pressures from administration or insurers to reduce cost. | 2.89 | 4.5 | 16 |
| Participate in care that I do not agree with but do so because fears of litigation. | 2.81 | 3.7 | 17 |
| Feel required to overemphasize tasks and productivity or quality measures at the expense of patient care. | 2.70 | 4.1 | 18 |
| Fear retribution if I speak up. | 2.63 | 4.5 | 19 |
| Work within power hierarchies in teams, units, and my institution that compromises patient care. | 2.49 | 4.2 | 20 |
| Work with team members who do not treat vulnerable or stigmatized patients with dignity and respect. | 1.90 | 3.2 | 21 |
| Follow a physician’s or family member’s requests not to discuss the patient’s prognosis with the patient/family. | 1.87 | 2.6 | 22 |
| Feel pressured to ignore situations in which patients have not been given adequate information to ensure informed consent. | 1.61 | 3.0 | 23 |
| Feel unsafe/bullied amongst my own colleagues. | 1.59 | 3.6 | 24 |
| Witness a violation of a standard of practice or a code of ethics and not feel sufficiently supported to report the violation. | 1.46 | 3.3 | 25 |
| Be pressured to avoid taking action when I learn that a physician, nurse, or other team colleague has made a medical error and does not report it. | 1.20 | 2.7 | 26 |
| Be required to care for patients whom I do not feel qualified to care for. | 1.05 | 2.1 | 27 |
Burnout and Professional Fulfillment
With the MBI (25), 144 physicians (34.4%) and 237 physicians (56.6%) reported feeling burnt out at work “once a week” or more and “a few times per month” or more, respectively, Similarly, 69 physicians (16.7%) and 124 physicians (30.1%) acknowledged becoming more callous toward people with the same frequencies. The average MBI burnout score (25) was 3.3 ± 1.5 with average emotional exhaustion and interpersonal disengagement scores of 3.8 ± 1.7 and 2.8 ± 1.6, respectively.
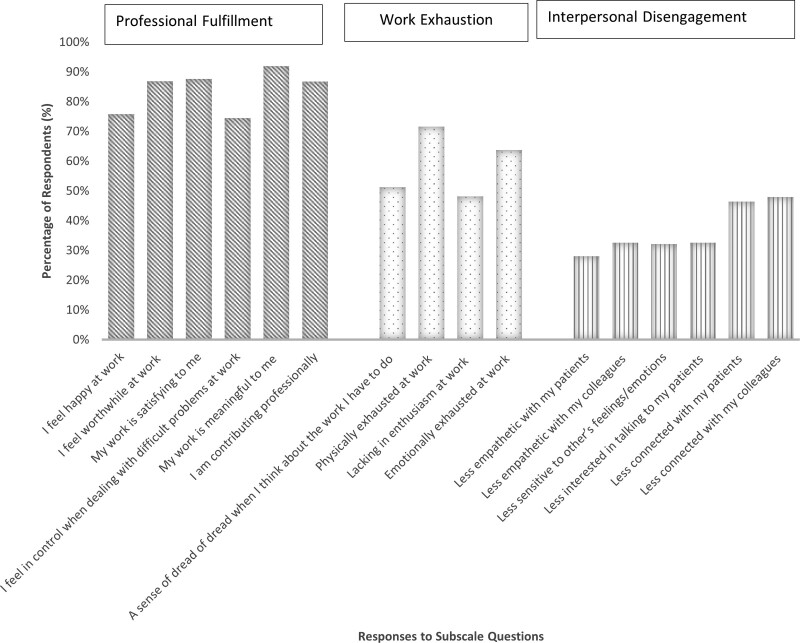
Using the Stanford PFI (26), most respondents found their work meaningful (387 [91.9%]) and satisfying (367 [87.6%]). Physicians felt worthwhile at work (365 [86.9%]) and that they (365 [86.7%]) were contributing professionally in ways that they valued. However, most physicians felt physically (297 [71.6%]) and emotionally (266 [63.8%]) exhausted at work. Some physicians felt at least moderately less interested in talking to patients (137 [32.6%]), whereas others felt less empathetic and connected with both patients (118 [28.1%] and 195 [46.4%], respectively) and colleagues (137 [32.6%] and 201 [47.9%], respectively) (Fig.1).
Figure 1.
Responses to the Stanford professional fulfillment index. Depicts physician responses to each of the questions in the three domains of the Stanford professional fulfillment (23) including professional fulfillment six items), work exhaustion (four items), and interpersonal disengagement (six items).
The average Professional Fulfillment Subscale score (26) was 6.5 ± 2.1 with average work exhaustion and Interpersonal Disengagement Subscale scores of 4.6 ± 2.3 and 3.0 ± 2.2, respectively. The average Stanford PFI Burnout Subscale score (26) was 3.6 ± 2.0 with over half of respondents (227 [54.6%]) meeting burnout criteria. Compared with prepandemic, physicians self-reported that their burnout increased (259 [63.8%]) or remained unchanged (126 [31.0%]) during the pandemic.
Relationships Between Wellness Measures
Professional fulfillment was negatively correlated with all other wellness measures. Moral distress was positively correlated with the Stanford PFI Burnout Subscale score (ρ = 0.52; p = 0.01) (Appendix 2, http://links.lww.com/CCM/H203).
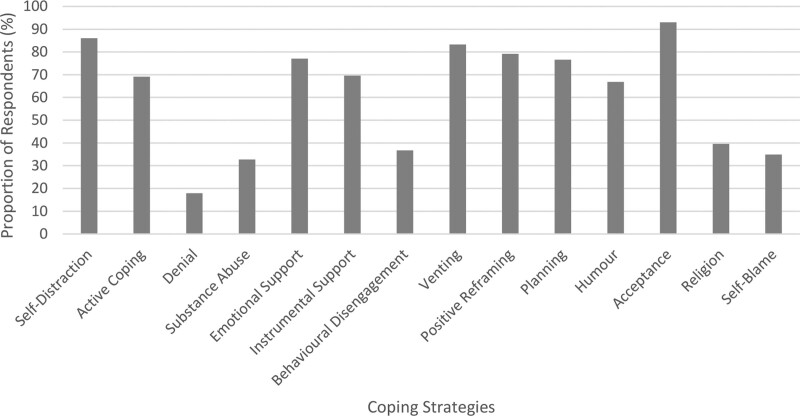
Coping Strategies
Physicians used diverse coping strategies (12) during the pandemic (Fig. 2). Compared with prepandemic, most physicians reported that their coping remained the same (231 [55.9%]) or decreased (102 [24.7%]) during the pandemic.
Figure 2.
Physicians’ use of coping strategies during the pandemic. Depicts physician’s self-reported use of each of the 14 coping strategies included in the Brief Cope (24) instrument.
Coping Profiles and Wellness
We identified four distinct coping profiles based on frequency of use of coping strategies. “Active or social copers” (79/416 [19.0%]) used active (e.g., active coping, planning, positive reframing) and social (e.g., venting, emotional support, instrumental support) coping strategies. “Avoidant copers” (193/416 [46.4%]) used passive, avoidant coping strategies (e.g., self-distraction, denial, substance use, behavioral disengagement, and self-blame). “Mixed/ambivalent copers” (19/416 [4.6%]) used both active (e.g., active coping, planning, positive reframing) and passive or avoidant (e.g., denial, behavioral disengagement, and self-blame) coping strategies. “Infrequent copers” (125/416 [30.0%]) did not use any coping strategies very frequently. Infrequent copers experienced the lowest moral distress, highest professional fulfillment, and lowest burnout scores. Conversely, mixed/ambivalent copers experienced the highest moral distress, lowest professional fulfillment, and highest burnout scores. More active copers and mixed/ambivalent copers met Stanford PFI burnout criteria (Table 3). Many mixed/ambivalent copers (10/18 [55.6%]) affirmed that their ability to cope had decreased from pre pandemic to intrapandemic (Appendix 3, http://links.lww.com/CCM/H204). Senior physicians (> 51 yr) (47/127 [37.0%]) were well-represented among infrequent copers.
TABLE 3.
Associations Between Wellness Measures and Coping Profiles
| Wellness Measures | Coping Profile | p | |||
|---|---|---|---|---|---|
| Active or Social | Avoidant | Mixed or Ambivalent | Infrequent | ||
| Measure of Moral Distress for Healthcare Professionals Scale Score, mean ± sd | 165.6 ± 35.8 | 89.5 ± 25.7 | 270.4 ± 76.8 | 33.9 ± 20.9 | < 0.001 |
| MBI (two items), mean ± sd | 3.4 ± 1.6 | 2.4 ± 1.4 | 3.6 ± 1.6 | 1.4 ± 1.2 | < 0.001 |
| Proportion With Burnout Using MBI, % (95% CI) | 61 (50–72) | 38 (32–45) | 68 (45–91) | 18 (11–25) | < 0.001 |
| Stanford Professional Fulfillment Subscale Score, mean ± sd | 5.3 ± 2.2 | 6.7 ± 1.8 | 4.3 ± 2.9 | 7.3 ± 1.8 | < 0.001 |
| Stanford Burnout Subscale Score, mean ± sd | 4.9 ± 1.8 | 3.8 ± 1.7 | 5.5 ± 2.6 | 2.3 ± 1.5 | < 0.001 |
| Proportion With Burnout Using Stanford professional fulfillment, % (95% CI) | 81 (72–90) | 61 (54–68) | 79 (59–99) | 24 (16–32) | < 0.001 |
MBI = Maslach Burnout Inventory.
Secondary Analyses
We did not find differences in moral distress, professional fulfillment, and burnout scores between intensivists and nonintensivists, adult and pediatric physicians, or practitioners in community versus other settings. Nonintensivists (vs intensivists) reported significantly more moral distress related to “being required to care for patients whom they did not feel qualified to care for” (2.5 ± 2.8 vs 1.0 ± 2.1; p = 0.046) and “working with team members who did not treat vulnerable or stigmatized patients with dignity and respect” (3.9 ± 3.4 vs 1.8 ± 3.2; p = 0.013).
Physicians who worked more (> median) versus less (< median) days/mo experienced significantly more moral distress (228.0 ± 120.2 vs 198.7 ± 87.1; p < 0.001) but similar Stanford PFI Burnout and Professional Fulfillment (26) scores. Similarly, physicians who worked more vs less “scheduled” in-house nightshifts experienced significantly higher moral distress on selected items (Appendix 4, http://links.lww.com/CCM/H205) but no differences in professional fulfillment or burnout. Less “scheduled” (< median) and more “unscheduled” (> median) in-house night shifts were associated with significantly higher moral distress pertaining to feeling required to overemphasize task and productivity or quality measures at the expense of patient care (interaction p = 0.006). More “scheduled” (> median) and more “unscheduled” (> median) in-house night shifts were associated with significantly higher moral distress related to working with team members who do not treat vulnerable or stigmatized patients with dignity and respect (interaction p = 0.018).
Physicians who experienced higher COVID-19 patient volumes had significantly higher moral distress (Wald χ2 (1) = 9.573; p = 0.002) and Stanford PFI burnout scores (Wald χ2 [1] = 8.52; p = 0.004) but similar Professional Fulfillment scores (Wald χ2 [1] = 3.03; p = 0.08) (24, 26). A significant dose-response was noted between higher average COVID-19 patient volume and higher average moral distress scores. Physicians who worked at hospitals that cared for between 501 and 750, and greater than 750 COVID-19 patients had the highest burnout scores (Stanford PFI and MBI) and moral distress scores, respectively (Appendice 5, A and B, http://links.lww.com/CCM/H206).
Post hoc, we found that women (vs men) physicians experienced significantly higher intrapandemic moral distress and burnout and physicians who self-identified as persons of color (vs other) experienced significantly higher moral distress (Appendix 6, http://links.lww.com/CCM/H207).
DISCUSSION
In this binational, intrapandemic survey of attending physicians who worked in the ICU, we identified significant increases in the number of days worked/mo, ICU bed occupancy, and self-reported moral distress and burnout from pre pandemic to intrapandemic. Of the 10 top-ranked items that incited moral distress, most pertained to regulatory/organizational (n = 6) or local/institutional (n = 2) issues or both (n = 2). Over half of physicians who worked in the ICU met burnout criteria. Despite moderate average moral distress and burnout scores, physicians who worked in the ICU also experienced moderate professional fulfilment. Physicians who worked more (vs less) days/mo and more scheduled in-house nightshifts, especially combined with more unscheduled in-house nightshifts, experienced significantly more moral distress on selected items. There was a significant dose-response between higher average patient volume and higher average moral distress scores. One in five physicians used a maladaptive coping strategy. We identified four coping profiles that were associated with significant differences across all wellness measures.
Few surveys have focused on physician wellness. This is related to the challenges inherent in identifying and contacting physicians amidst privacy concerns and the fact that physicians are less numerate than multiprofessional healthcare providers in ICUs. Unlike an earlier multidisciplinary survey conducted in the Netherlands that identified “inadequate emotional support for patients and their families” as the main item inciting moral distress (31), we found that the “need to continue aggressive treatment even though it was not perceived to be beneficial or likely to change outcome” incited the highest moral distress. Compared with a prepandemic survey of 239 Canadian intensivists, we found similar moral distress scores (107 vs 96.6) and alignment among eight of the 10 top-ranked items that incited moral distress (4). Importantly, six of these top 10-ranked items had a locus of control in regulatory or organizational bodies. We also noted significant relationships between increased moral distress and higher patient volume, more days worked/mo, and more scheduled in-house night shifts, especially when combined with unscheduled in-house night shifts. Taken together, our findings highlight several potentially modifiable factors that could be addressed at the individual (coping), institutional (patient volume, workload, scheduling of in-house shifts, administrative support, equipment), and regulatory (documentation requirements, end-of-life care, inappropriate treatment) levels to enhance physician wellness.
Estimates of physician burnout vary based on the scale used and the timing of measurement. Compared with the prepandemic survey of Canadian intensivists by Dodek et al (4), we found similar mean MBI emotional exhaustion (3.5 ± 1.7 vs 3.8 ± 1.7) and depersonalization scores (3.0 ± 1.7 vs 2.8 ± 1.6). Conversely, compared with another survey of Canadian intensivists (1), we found that physicians who worked in ICUs during the pandemic were more likely to report burnout once a week or more (52/272 [19%] vs 144/419 [34.3%]) using the MBI (25). Few studies have used the Stanford PFI (26)—a scale specifically designed to assess professional fulfilment and burnout in “physicians.” Compared with a prepandemic survey of 419 physicians at the University of Toronto, we identified marginally lower professional fulfilment (6.7 ± 2.4 vs 6.5 ± 2.1) but higher work exhaustion (3.5 ± 2.5 vs 4.6 ± 2.3) and interpersonal disengagement (2.2 ± 1.9 vs 3.0 ± 2.2) subscale scores using the Stanford PFI (26). Although our respondents reported higher average intrapandemic burnout (2.7 ± 2.1 vs 3.6 ± 2.0) subscale scores compared with this prepandemic survey, they also experienced moderate professional fulfillment. This finding may reflect the novel challenges posed by the pandemic and the prominence of front-line physicians in the media (14). Finally, we identified a significant relationship between higher COVID-19 patient volume and higher burnout with both the MBI (25) and the Stanford PFI (26).
Compared with moral distress and burnout, considerably less is known about physician coping. In an intrapandemic study of 398 health workers (207 physicians, 133 nurses, and 58 pharmacists) in Pakistan, Salman et al (32) found that religion, acceptance, and planning were commonly used coping strategies, whereas substance use and self-blame were infrequently used. In North America, we found that acceptance (active coping strategy) and self-distraction (avoidant coping strategy) were the most frequently used coping strategies and religion was infrequently used. Although positive coping strategies (active or social) were widely used, coping profiles, based on frequency of use of coping strategies, avoidant copers (46.4%) comprised nearly half of our sample with infrequent copers being the second largest coping profile (19.0%). Coping profiles were associated with significant differences across wellness measures with infrequent copers experiencing the lowest moral distress and burnout scores and the highest professional fulfillment and mixed/ambivalent copers experiencing the highest moral distress and burnout scores and the lowest professional fulfillment. More active copers and mixed/ambivalent copers met Stanford PFI burnout criteria (26).
Our survey has strengths and limitations. First, we used rigorous survey methodology to design, test, and administer our questionnaire (19). Second, our response rate was higher than expected for a large-scale, intrapandemic survey. Third, we worked with 62 local North American site leads to identify and administer our questionnaire to physicians who worked in ICUs during the pandemic. With this approach, we obtained responses from diverse respondents in 25 U.S. states and eight Canadian provinces including respondent groups (junior, women, and community-based physicians) that are typically underrepresented in surveys. We cannot exclude a social desirability effect given that responses were enriched with positive coping strategies. We did not conduct detailed analyses related to potential effect modifiers or corroborate our findings with workload measurements specific to respondent’s ICUs. Third, although we sought a minimum of 10 responses per ICU, some ICUs had few potential respondents and few responses. Finally, our findings represent the physicians surveyed at selected participating centers and consequently may not be generalizable to other ICUs and contexts.
ACKNOWLEDGMENT
We wish to thank the members of the Women in Critical Care Interest Group for their support of this study. We also would like to express our gratitude to Mr. Taimoor Zahir, Ms. Miriam Rodriguez, and the Executive Committee of the American Thoracic Society for their administrative assistance and support of this study.
Supplementary Material
Footnotes
*See also p. 1819.
New affiliation for Dr. Thirugnanam: Oak Valley Health, Markham, ON, Canada. Members of the Diversity-Related Research Committee of the Women in Critical Care (WICC) Interest Group of the American Thoracic Society are as follows: Karen Burns (lead), Karen.Burns@unityhealth.to; Liz Viglianti (lead), eviglian@med.umich.edu; Alison Fox-Robichaud (member), afoxrob@mcmaster.ca; Ellen Burnham (member), ellen.burnham@ucdenver.edu; Geeta Mehta (member), geeta.mehta@sinaihealthsystem.ca; Hayley Gershengorn (member), hbg20@med.miami.edu; Jenny Han (member), jehan2@emory.edu; Kathleen Akgün (member), kathleen.akgun@yale.edu; Kelly Vranas (member), vranas@ohsu.edu; Kusum Mathews (member), kusum.mathews@mssm.edu; Michelle Harkins (member), mharkins@salud.unm.edu; Peter Dodek (member), peter.dodek@ubc.ca; and Snigdha Jain (member), Snigdha.Jain@yale.edu.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Drs. Burns and Dodek contributed to study concept. All authors contributed to questionnaire design. Drs. Burns, Moss, Dodek, Martin, and WICC members contributed to questionnaire testing. All authors contributed to questionnaire administration. Drs. Lorens and Burns contributed to analysis. Drs. Burns, Moss, Dodek, and Jose contributed to article preparation. All authors contributed to approval of final article.
The Canadian Critical Care Society covered the cost of the statistical analysis.
Dr. Karen E. A. Burns is the guarantor for the data used in this study.
Dr. Burns disclosed that the Canadian Critical Care Society (CCSS) paid for the statistical analyses. Dr. Lorens received funding from the CCCS. Drs. Lorens and Kerlin disclosed work for hire. Drs. Viglianti, Kohn, Peltan, and Schnapp received support for article research from the National Institutes of Health (NIH). Dr. Fox-Robichaud’s institution received funding from the Canadian Institutes of Health Research and Hamilton Academic Hospitals. Dr. Mathews’ institution received funding from the National Heart, Lung, and Blood Institute (NHLBI); he received funding from Roivant/Kinevant Sciences. Dr. Jain is supported by the National Institute on Aging (NIA) T32AG019134, the Pepper Scholar Award from Yale Claude D. Pepper Older American Independence Center (P30AG021342), NIA of the NIH GEMSSTAR Award (R03AG078942), Parker B. Francis Fellowship Award, and Yale Physician-Scientist Development Award. Drs. Akgun and Crothers disclosed government work. Dr. Gershengorn received funding from the American Thoracic Society (ATS), Gilead Sciences, and Southeastern Critical Care Summit. Dr. Martin’s institution received funding from BARDA; he received funding from Genetech. Dr. Stapleton disclosed that she is chair of DSMB for Altimmune and a member of the ATS Board of Directors 2019–2021 (elected to Chair the Critical Care Assembly which includes a position on the Board). Dr. Attia’s institution received funding from the NHBLI (NHLBI K23 HL129888 and R03 [pending]), the Centers for Aids Research, and Pediatric HIV/AIDS Cohort Study. Dr. Maddux’s institution received funding from the National Institute of Child Health and Human Development (K23HD096018) and the Francis Family Foundation. Dr. Bagshaw received funding from Baxter and Bioporto. Dr. Crothers’ institution received funding from the NIH and Veteran’s Affairs. Dr. Peltan’s institution received funding from Regeneron and Asahi Kasei Pharma; he received funding from the NIH (K23GM129661) and Janssen. Dr. Schnapp received funding from UptoDate and Elsevier. Dr. Kraft’s institution received funding from the NIH, the American Lung Association, Sanofi, and AstraZeneca Consulting; she received funding from Sanofi, Astra-Zeneca, Chiesi Speaking, and UptoDate; she disclosed she is a cofounder and Chief Medical Officer of RaeSedo LLC. The remaining authors have disclosed that they do not have any potential conflicts of interest.
The survey data will be made available upon written request to Dr. Burns.
REFERENCES
- 1.Burns KEA, Fox-Robichaud A, Lorens E, et al. ; Canadian Critical Care Society: Gender differences in career satisfaction, moral distress, and incivility: A national, cross-sectional survey of Canadian critical care physicians. Can J Anaesth. 2019; 66:503–511 [DOI] [PubMed] [Google Scholar]
- 2.Hossain F: Moral distress among healthcare providers and mistrust among patients during COVID-19 in Bangladesh. Dev World Bioeth. 2021; 21:187–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hines SE, Chin KH, Glick DR, et al. : Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int J Environ Res Public Health. 2021; 18:E488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dodek PM, Cheung EO, Burns KEA, et al. : Moral distress and other wellness measures in Canadian critical care physicians. Ann Am Thorac Soc. 2021; 18:1343–1351 [DOI] [PubMed] [Google Scholar]
- 5.Bruce CR, Miller SM, Zimmerman JL: A qualitative study exploring moral distress in the ICU team: The importance of unit functionality and intrateam dynamics. Crit Care Med. 2015; 43:823–831 [DOI] [PubMed] [Google Scholar]
- 6.Bansal P, Bingemann TA, Greenhawt M, et al. : Clinician wellness during the COVID-19 pandemic: Extraordinary times and unusual challenges for the allergist/immunologist. J Allergy Clin Immunol Pract. 2020; 8:1781–1790.e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romanelli J, Gee D, Mellinger JD, et al. ; SAGES Reimagining the Practice of Surgery Task Force: The COVID-19 reset: Lessons from the pandemic on burnout and the practice of surgery. Surg Endosc. 2020; 34:5201–5207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Restauri N, Sheridan AD: Burnout and posttraumatic stress disorder in the coronavirus disease 2019 (COVID-19) pandemic: Intersection, impact, and interventions. J Am Coll Radiol. 2020; 17:921–926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moss M, Good VS, Gozal D, et al. : An official critical care societies collaborative statement: Burnout syndrome in critical care health care professionals: A call for action. Am J Crit Care. 2016; 25:368–376 [DOI] [PubMed] [Google Scholar]
- 10.Buselli R, Corsi M, Baldanzi S, et al. : Professional quality of life and mental health outcomes among health care workers exposed to SARS-CoV-2 (COVID-19). Int J Environ Res Public Health. 2020; 17:E6180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazarides AL, Belay ES, Anastasio AT, et al. : Physician burnout and professional satisfaction in orthopedic surgeons during the COVID-19 Pandemic. Work. 2021; 69:15–22 [DOI] [PubMed] [Google Scholar]
- 12.Carver CS, Scheier MF, Weintraub JK: Assessing coping strategies: A theoretically based approach. J Pers Soc Psychol. 1989; 56:267–283 [DOI] [PubMed] [Google Scholar]
- 13.Burns KEA, Pattani R, Lorens E, et al. : The impact of organizational culture on professional fulfillment and burnout in an academic department of medicine. PLoS One. 2021; 16:e0252778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu Y, Wang J, Luo C, et al. : A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage. 2020; 60:e60–e65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cour M, Cariou A, Argaud L: Response. Chest. 2021; 160:e678. [DOI] [PubMed] [Google Scholar]
- 16.Vranas KC, Golden SE, Mathews KS, et al. : The Influence of the COVID-19 pandemic on ICU organization, care processes, and frontline clinician experiences: A qualitative study. Chest. 2021; 160:1714–1728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khalafallah AM, Lam S, Gami A, et al. : Burnout and career satisfaction among attending neurosurgeons during the COVID-19 pandemic. Clin Neurol Neurosurg. 2020; 198:106193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart MT, Reed S, Reese J, et al. : Conceptual models for understanding physician burnout, professional fulfillment, and well-being. Curr Probl Pediatr Adolesc Health Care. 2019; 49:100658. [DOI] [PubMed] [Google Scholar]
- 19.Burns KE, Duffett M, Kho ME, et al. ; ACCADEMY Group: A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008; 179:245–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirshner B, Guyatt G: A methodological framework for assessing health indices. J Chronic Dis. 1985; 38:27–36 [DOI] [PubMed] [Google Scholar]
- 21.Burns KEA, Kho ME: How to assess a survey report: A guide for readers and peer reviewers. CMAJ. 2015; 187:E198–E205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, and Social Sciences and Humanities Research Council, Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans. 2018. Available at: http://www.pre.ethics.gc.ca. Accessed September 13, 2022
- 23.World Medical Association: Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects, 2013. Available at: http://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medicalresearch-involving-human-subjects. Accessed May 16, 2022 [DOI] [PubMed]
- 24.Epstein EG, Whitehead PB, Prompahakul C, et al. : Enhancing understanding of moral distress: The measure of moral distress for health care professionals. AJOB Empir Bioeth. 2019; 10:113–124 [DOI] [PubMed] [Google Scholar]
- 25.West CP, Dyrbye LN, Sloan JA, et al. : Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009; 24:1318–1321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trockel M, Bohman B, Lesure E, et al. : A brief instrument to assess both burnout and professional fulfillment in physicians: Reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Acad Psychiatry. 2018; 42:11–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mukaka MM. A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012; 24:69–71 [PMC free article] [PubMed] [Google Scholar]
- 28.Rosenberg JM, Beymer PN, Anderson DJ, et al. ; tidyLPA: An R package to easily carry out latent profile analysis (LPA) using open-source or commercial software. J Open Source Softw. 2018; 3:978 [Google Scholar]
- 29.Kleinbaum DG, Kupper LL, Nizam A, et al. : Applied Regression Analysis and Other Multivariable Methods. Boston, Cengage Learning, 2013 [Google Scholar]
- 30.Rosenberg JM, van Lissa CJ, Beymer PN, et al. ; tidyLPA: Easily Carry Out Latent Profile Analysis (LPA) Using Open-Source or Commercial Software [R Package], 2019. Available at: https://data-edu.github.io/tidyLPA/; https://cran.r-project.org/web/packages/tidyLPA/vignettes/Introduction_to_tidyLPA.html. Accessed September 13, 2022
- 31.Donkers MA, Gilissen VJHS, Candel MJJM, et al. : Moral distress and ethical climate in intensive care medicine during COVID-19: A nationwide study. BMC Med Ethics. 2021; 22:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salman M, Raza MH, Mustafa ZU, et al. : The psychological effects of COVID-19 on frontline healthcare workers and how they are coping: A web-based, cross-sectional study from Pakistan. medRxiv 2020.06.03.20119867 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.