Abstract
Primary bilateral macronodular adrenal hyperplasia (PBMAH) is often associated with symptoms of cortisol excess, which may include neuropsychological symptoms. We report a patient with PBMAH who presented with manic symptoms that resolved following unilateral adrenalectomy.
1. Introduction
Primary bilateral macronodular adrenal hyperplasia (PBMAH) is an uncommon cause of hypercortisolism. PBMAH is characterized by bilaterally enlarged adrenal glands containing multiple nodules greater than 1cm in size.1 Occurring more commonly in females, PBMAH symptoms often appear insidiously over several years.2 Common features of cortisol excess include weight gain, dorsocervical fat pad, facial rounding, easy bruising, and hypertension. Several neuropsychological symptoms can occur, most commonly emotional lability, depression, irritability, and anxiety. Paranoia and mania are less common.3
Historically, bilateral adrenalectomy was the recommended treatment for patients with symptomatic PBMAH; however, unilateral adrenalectomy has become preferred in patients with less severe hypercortisolism since it normalizes cortisol levels in a significant percentage of patients.4 After correction of hypercortisolism, resolution of the psychiatric symptoms is variable. To our knowledge, we report the first case of hypercortisolism with manic symptoms secondary to PBMAH that resolved completely following unilateral adrenalectomy.
2. Case presentation
A 60-year-old female was evaluated in the emergency room for severe abdominal pain, nausea, and vomiting. Her past medical history was significant for hypertension, right-sided breast cancer status post lumpectomy, and Crohn's disease status post small bowel resection. Over the past year the patient reported fatigue, elevated blood pressure, easy bruising, and delayed wound healing. She denied headaches, palpitations, diaphoresis, or abnormal skin pigmentation.
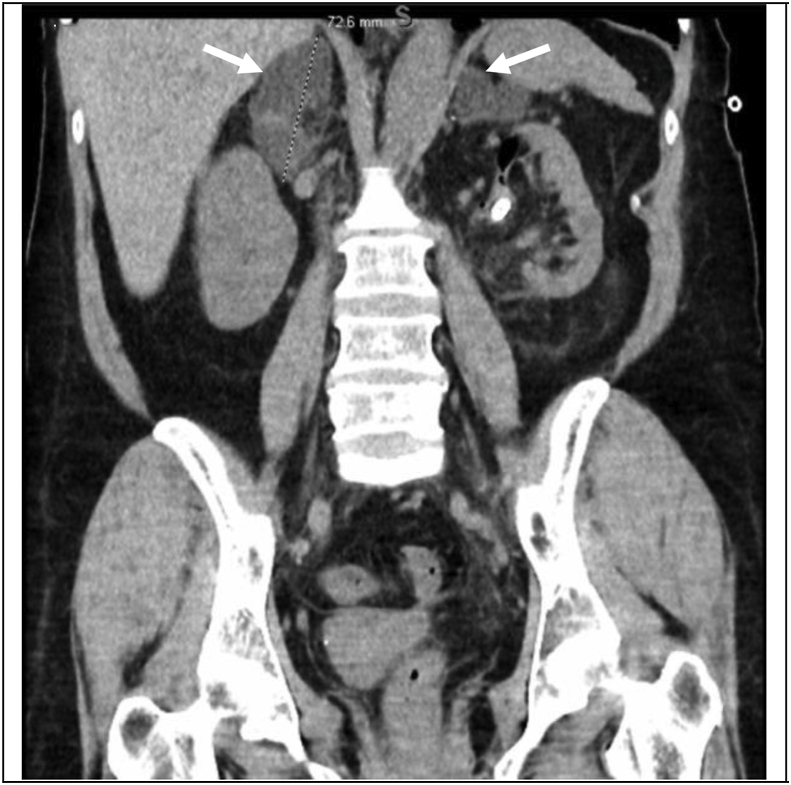
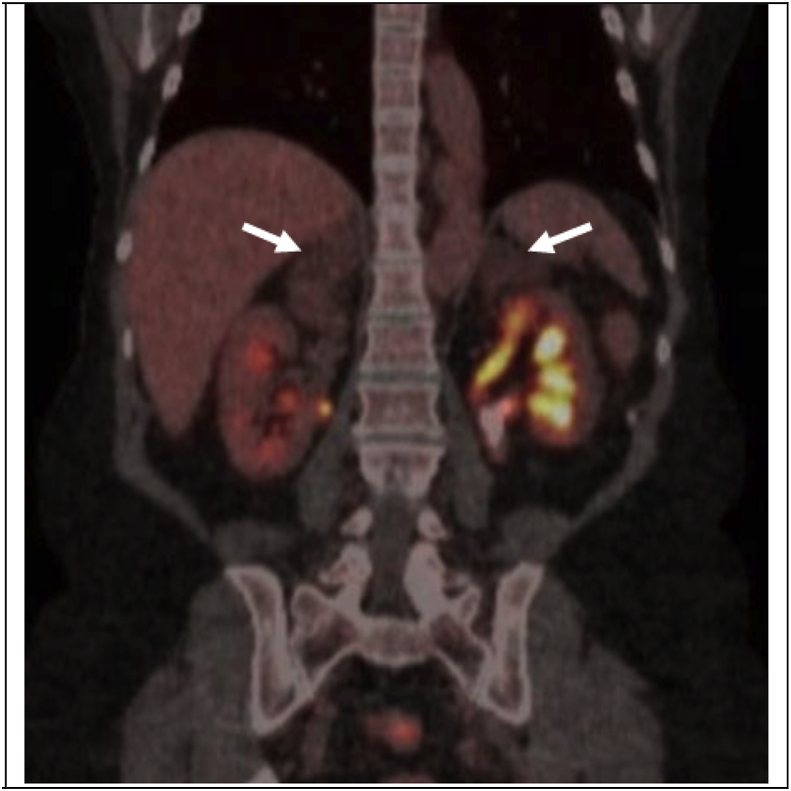
CT imaging revealed bilateral multilobulated adrenal masses – 3.4 × 5.5 × 4.1cm (37 Hounsfield units) on the right and 3.8 × 4.2 × 2.0cm (44 Hounsfield units) on the left (Fig. 1A). These masses were stable in size when compared to a CT scan from 10 years prior. PET/CT did not display abnormal FDG activity (Fig. 1B).
Fig. 1A.
Coronal CT demonstrating bilateral adrenal masses (arrows).
Fig. 1B.
PET/CT indicating adrenal glands with no abnormal FDG activity (arrows).
Biochemical evaluation included random serum cortisol of 12.9 mcg/dL (nl. 3–12), DHEAS of 145 mcg/dL (nl. 13–130), and ACTH of <5pg/mL (nl. 6–58). 8am serum cortisol and dexamethasone levels following a 1mg overnight dexamethasone suppression test were 16.6 mcg/dL (nl. <1.8) and 160ng/dL (nl. < 50), respectively. Aldosterone was mildly elevated at 18.8ng/dL and renin suppressed to 0.9ng/mL/hr. Repeat 1mg overnight dexamethasone suppression test confirmed hypercortisolism with an 8am serum cortisol of 20.3 mcg/dL. Circulating serum levels of estradiol, estrone, androstenedione, LH, FSH, and metanephrines were within normal limits. Bilateral simultaneous adrenal venous sampling was performed to evaluate for lateralization of both aldosterone and cortisol secretion. This was done by measuring serum epinephrine, aldosterone, and levels to determine successful catheter placement and to correct for flow and dilution between the adrenal veins. With regards to hyperaldosteronism, lateralization index criteria to suggest surgically remediable aldosteronism was not met.
However, there was lateralization of cortisol production to the right adrenal gland. Right adrenal vein to peripheral vein cortisol ratio was 9.27 (nl. <6.5) consistent with cortisol hypersecretion. The right to left cortisol ratio was 2.3 (nl. <2.3), and the right to left ratio of the epinephrine corrected cortisol concentration was 2.7, consistent with right-sided predominant hypercortisolism. Lateralization did not persist post-ACTH stimulation (Table 1) as expected for an ACTH-independent process.
Table 1.
Simultaneous adrenal venous sampling demonstrating higher cortisol production from the right adrenal gland based on (a) absolute lab values (b) right to left lateralization index, and (c) epinephrine-corrected lateralization index for cortisol (2.7:1 right to left).
| a. | ||||||
|---|---|---|---|---|---|---|
| Left Adrenal Vein |
Peripheral Vein/IVC |
Right Adrenal Vein |
||||
| Cortisol | Epinephrine | Cortisol | Epinephrine | Cortisol | Epinephrine | |
| Pre ACTH mean values | 45 mcg/dl | 394 pg/ml | 11 mcg/dl | <10 pg/ml | 102 mcg/dl | 303 pg/ml |
| Post ACTH mean values | 520 mcg/dl | 365 pg/ml | 22.3 mcg/dl | 11 pg/ml | 930 mcg/dl | 676 pg/ml |
| b. | |||
|---|---|---|---|
| Left AV/PV cortisol ratios | Right AV/PV cortisol ratios | Right to Left cortisol lateralization ratios | |
| Pre ACTH | 4 | 9.27 | 2.3 |
| Post ACTH | 23 | 41.7 | 1.8 |
| c. | ||||
|---|---|---|---|---|
| Left Adrenal Vein (Epinephrine corrected cortisol ratios) | Peripheral Vein/IVC (Epinephrine corrected cortisol ratios) | Right Adrenal Vein (Epinephrine corrected cortisol ratios) | Right to left epinephrine corrected cortisol lateralization ratio | |
| Pre ACTH | 0.11 | N/A | 0.3 | 2.7 |
| Post ACTH | 1.4 | 2 | 1.3 | 0.9 |
During the course of the workup the patient presented to the ED with acute agitation, pressured speech, grandiose ideation, and emotional lability. It was revealed the patient had been having unprovoked outbursts of irritation for the past 10 years, gradually worsening over the last several months. She had been sleeping 3–4 hours nightly over the past 6 months and involved in several excessive shopping sprees. The patient was admitted to inpatient psychiatry for 10 days for stabilization.
Given the larger right-sided mass, evidence of excess cortisol secretion on the right compared to the left, and her acute worsening of symptoms, the decision was made to proceed with laparoscopic right adrenalectomy. She was counseled that this may not cure her hypercortisolism, but could improve her symptoms and delay the need for bilateral adrenalectomy and subsequent lifelong hormone replacement.
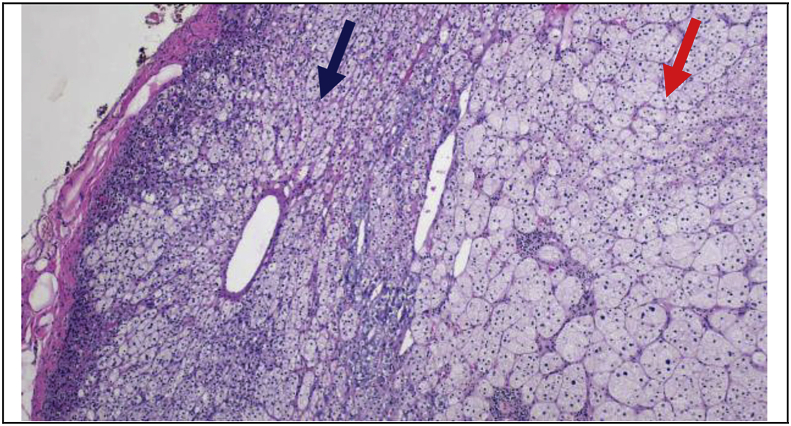
Laparoscopic right adrenalectomy was performed uneventfully. She was discharged to home on postoperative day #1. Grossly, the right adrenal gland weighed 73g and measured 8.3 × 9.8 × 3.5cm. There were multiple nodules ranging in size from 1.5 to 4.6cm, consistent with macronodular adrenal hyperplasia (Fig. 2A, Fig. 2B).
Fig. 2A.
Adrenal cortical hyperplastic nodule (red arrow) compressing background adrenal cortex and medulla on the left (blue arrow) on X40 magnified H&E stained sections. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
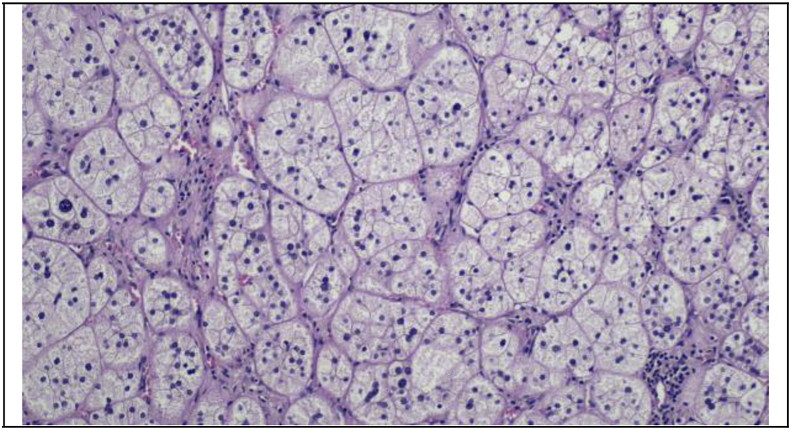
Fig. 2B.
Adrenal cortical hyperplastic nodule consists of larger cells with voluminous foamy cytoplasm on X100 magnified H&E stained sections.
Laboratory evaluation conducted on post-operative day #11 included AM serum cortisol of 11.0 mcg/dL (nl. 7–23) and serum ACTH of 8.2pg/mL (nl. 6–58). Two years later AM serum cortisol was 7.8 mcg/dL, serum ACTH was 8.4pg/mL, and 24-h urine cortisol was 6.27 mcg/day (normal <45 mcg/day), indicating biochemical cure. To date, the patient has not had any return of manic symptoms post-operatively, despite discontinuing all antipsychotic medications.
3. Discussion
While PBMAH commonly presents with hypercortisolism, to our knowledge, we report the first case of PBMAH induced manic symptoms with complete resolution following surgical treatment.
Our patient presented with many of the defining characteristics of hypercortisolism including fatigue, elevated blood pressure, easy bruising, and delayed wound healing. Associated neuropsychological symptoms included emotional lability, depression, anxiety, and mania. The patient had been suffering from distractibility, flight of ideas, grandiosity, and sleep deficiency for at least 6 months. Manic episodes have been observed in about 30% of patients with hypercortisolism, significantly less frequently than emotional lability and depression, the prevalence of which has been reported up to 80%.5
In patients with PBMAH with moderately increased cortisol production (<3 times upper limit) and clinical signs of hypercortisolism, unilateral adrenalectomy is recommended since normocortisolemia can be achieved in >90% of patients.4 Therefore, we made the decision to remove the dominant right adrenal gland, as indicated by both imaging and adrenal venous sampling. Fortunately, the patient's overall cortisol levels returned to baseline once the dominant right adrenal gland was removed. There has been no biochemical recurrence for two years post-operatively.
To our knowledge, manic symptom resolution following biochemical cure of hypercortisolism in the setting of PBMAH has yet to be reported. Studies investigating other neuropsychological symptoms, mainly depression, after successful treatment of hypercortisolism have been mixed, with some suggesting improvement and others suggesting persistent disease.5 Fortunately, our patient has had normal cortisol levels and complete resolution of her manic symptoms, despite discontinuing all antipsychotic medications, for two years following unilateral adrenalectomy. Patient selection and multidisciplinary engagement of endocrine neoplasia, interventional radiology, and urologic surgery teams are critical to providing appropriate care in these often challenging clinical scenarios.
Acknowledgement
We would like to acknowledge Charan K. Singh, MD who is our interventional radiologist with expertise in adrenal venous sampling.
Contributor Information
Benjamin H. Rosenfeld, Email: brosenfeld@uchc.edu.
Benjamin T. Ristau, Email: benristaumd@gmail.com.
References
- 1.Lacroix A. ACTH-independent macronodular adrenal hyperplasia. Best Pract Res Clin Endocrinol Metabol. 2009 Apr;23(2):245–259. doi: 10.1016/j.beem.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 2.Chevalier B., Vantyghem M.C., Espiard S. Bilateral adrenal hyperplasia: pathogenesis and treatment. Biomedicines. 2021 Oct 5;9(10):1397. doi: 10.3390/biomedicines9101397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Starkman M.N. Neuropsychiatric findings in Cushing syndrome and exogenous glucocorticoid administration. Endocrinol Metab Clin N Am. 2013 Sep;42(3):477–488. doi: 10.1016/j.ecl.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 4.Meloche-Dumas L., Mercier F., Lacroix A. Role of unilateral adrenalectomy in bilateral adrenal hyperplasias with Cushing's syndrome. Best Pract Res Clin Endocrinol Metabol. 2021 Mar;35(2) doi: 10.1016/j.beem.2021.101486. [DOI] [PubMed] [Google Scholar]
- 5.Pivonello R., Simeoli C., De Martino M.C., et al. Neuropsychiatric disorders in Cushing's syndrome. Front Neurosci. 2015 Apr 20;9:129. doi: 10.3389/fnins.2015.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]