Abstract
Objective: This study aimed to assess the dietary diversity and its associated factors among pregnant women in Addis Ababa, Ethiopia, 2021.
Methods: An institution-based Cross-sectional was conducted among 320 participants from four health facilities in Addis Ababa selected based on a simple random sampling method from 01 September to 30 December 2021. An Interviewer-administered structured questionnaire was used, following informed consent. Binary (Bivariate and multivariate) logistics regression was applied for the identification factors associated with dietary diversity with their respective 95% confidence interval and less than 5% p-value.
Results: The prevalence of inadequate dietary diversity during pregnancy was 51.6% (95% CI: 46.1%–57.0%). Being illiterate (AOR: 0.591; 95% CI: 1.88–1.901; p < 0.05) and primary education (AOR: 0.347; 95% CI: 0.166–0.728; p < 0.05), having poor knowledge (AOR: 0.437; 95% CI: 0.252–0.757; p < 0.05) and lower monthly income (AOR: 0.395; 95% CI: 0.184–0.845; p < 0.05) were factors associated with inadequate dietary diversity.
Conclusion: A higher level of inadequate dietary diversity was reported. Being illiterate, having primary education, having poor knowledge, and having lower monthly income were associated with inadequate dietary diversity during pregnancy. Concerned bodies were suggested to work on the identified factors.
Keywords: Ethiopia, women, associated factors, dietary practice, Addis Ababa
Introduction
A healthy diet is essential throughout one’s life, but especially during pregnancy. Pregnant women are nutritionally vulnerable due to their increased nutrient demand. Consumption of a variety of dietary sources is important for ensuring optimal maternal and child nutrition, as it prevents nutritional deficiencies and negative consequences [1, 2].
Dietary diversity is about taking varieties of food item and reflected as a proxy measure of micronutrient adequacy [1, 3]. Evidence suggests that dietary diversity promotes nutrient adequacy in women and lowers the risk of a negative birth outcome [4–7]. Dietary diversification is an appealing approach to addressing nutrient deficiency [1].
Micronutrient deficiency remains a major public health concern in low to middle-income countries commonly in reproductive-age women. [1–5], Thus pregnancy augments an additional burden of nutritional requirements for the women and fetus [6–8].
Malnutrition during pregnancy has a long-lasting effect on the physiological development of the fetus through increasing the risk of low birth weight, maternal morbidity and mortality, preterm delivery, and intrauterine growth retardation [9–12].
Optimal nutrient intake during pregnancy reduces the risk of preterm baby, low birth weight, infant mortality, and small for gestational age [13–15]. Moreover, in women who are underweight during their pregnancy supplementation of multiple micronutrients before 20 weeks of gestation reduces the risk of a preterm baby [16–18].
Understanding the enormous benefits of a healthy diet and adequate micronutrient supplementation during pregnancy [19, 20], dietary diversity is one of the best-recommended strategies for the improvement of dietary adequacy and increased food groups in their daily consumption [21]. Thus, dietary diversity refers to the number of different groups of food consumed over some time [22, 23].
Though evidence suggests that the prevalence of nutritional deficiency during pregnancy was higher in Africa [24–26], including Ethiopia, dietary diversification is an essential tool to reduce nutritional deficiencies [27].
To the best of the researcher’s knowledge, the level of dietary diversity and its associated factors during pregnancy was not well investigated in the study settings. Therefore; this study would hopefully fill the existing gap in the literature.
Methods
Participants and Study Design
The institutional-based cross-sectional study design was conducted among 320 participants from the selected health facilities at Addis Ketema Sub-City of Addis Ababa from 01 September to 30 December 2021. The study received Ethical approval from Santé Medical College; a research review ethics committee and applied to the respective Health Facilities. All the participants were provided written informed consent.
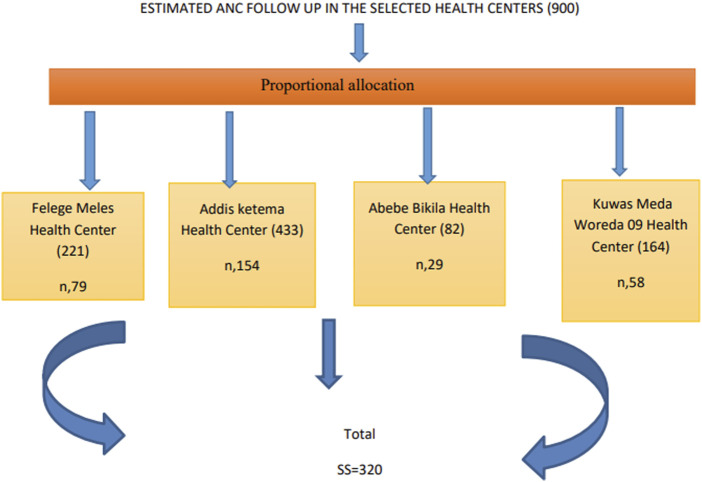
The source population was all pregnant women in Addis Ketema Sub-City, whereas the study population was pregnant women having had ANC follow-up at the selected health facilities; namely; Addis Ketema, Abebe Bikila, Kuwas Meda, and Felege Meles health centers, during the study period. Pregnant women who were available, willing, and free from any severe medical conditions were included in the study. The researcher selected the health facilities by simple random sampling method, after list of all health facilities was determined from the sub city likewise simple random sampling techniques was employed for the selection of the study participants ones their lists were identified from their medical records at respective facilities. Proportional allocation was made based on the health centers monthly follow-up (Figure 1).
FIGURE 1.
Sampling Procedure of the study participants (Addis Ababa, Ethiopia, 2021).
The sample size was determined based on a single population proportion, with the premise that the magnitude of dietary diversity from Shashemene was 25.4% [28], 95% confidence interval of 1.96, and a 5% margin of error. The final sample was 320 inclusive of a 10% non-response rate.
Data were gathered with a pre-tested interviewer-administered questionnaire. The questionnaire was developed by reviewing related pieces of literature [29–32] and then given for two senior researchers working in academic institutions and their inputs were incorporated into the final tool.
Definitions of Concepts
The outcome variable (Dietary diversity) was measured as adquate and inadequate. A minimum dietary diversity score (MDD-W) was used to calculate the sum of the number of different food groups consumed by the pregnant women in the 24 Hours before the assessment. The MDD-W indicator was based on the 10-food group’s women’s dietary diversity score (MDDW-10). These food groups are starch staples (grains, white roots and tubers, and plantains); vitamin A-rich vegetables and fruits; dark green leafy vegetables; other vegetables; other fruits; flesh foods (meat, fish, poultry, and liver/organ meats); eggs; pulses/legumes; nuts and seeds; and dairy products. MDD-W is based on a 24-h dietary recall period [33]. The women were asked to recall all foods consumed from the above food groups on the previous day. Responses were recorded as “yes” or “no.”A “yes” response was scored as “1,” and a “no” response was scored as ‘0’. The scores summed up to yield the women’s MDD-W score. The dietary diversity scores were then classified as inadequate and adequate dietary diversity based on the MDD-W. Women having a diversity score of less than 5 were classified as having low dietary diversity and scores of 5–10 are classified as the high/good dietary diversity scores [34]. Knowledge was measured as true and false questions and categorized as poor versus good knowledge based on median score after constructs forming knowledge were once computed.
Statistical Analysis
Descriptive statistics were used for the summarization of data. For the identification factors associated with dietary diversity, binary (Bi-variable and multivariable) logistics regression was used, with their respective 95% Confidence Interval (CI) and p-value of less than 0.05 as a statistically significant level.
Results
Socio Demographic Characteristics
A total of 320 pregnant women participated in this study making a response rate of 100%. The mean age of study participants was 26.98 with a standard deviation of 4.468. The majority (95%) of the participants were married and more than one-third (37.8%) of their husbands attended primary school. Regarding occupation, most (63.1%) of the study participants were housewives. Almost all (94.4%) of the participants got support from their husband (Table 1).
TABLE 1.
Socio-demographic characteristics of study participants (Addis Ababa, Ethiopia, 2021).
| Variables | Categories | Frequency | % |
|---|---|---|---|
| Age in years | <24 | 88 | 27.5 |
| 24–34 | 208 | 65.0 | |
| ≥35 | 24 | 7.5 | |
| Marital status | Married | 306 | 95.6 |
| Single/divorced/widowed | 14 | 4.3 | |
| Educational status | Illiterate | 22 | 6.9 |
| Reading and writing | 11 | 3.4 | |
| Primary | 121 | 37.8 | |
| Secondary | 104 | 32.5 | |
| Collage and above | 62 | 19.4 | |
| Occupation | Housewife | 202 | 63.1 |
| Private employment | 46 | 14.4 | |
| Government employment | 34 | 10.6 | |
| Merchant | 24 | 7.5 | |
| Student | 5 | 1.6 | |
| Daily laborer | 7 | 2.2 | |
| Other | 2 | 0.6 | |
| Partner level of education | Illiterate | 7 | 2.2 |
| Reading and writing | 9 | 2.8 | |
| Primary | 86 | 26.9 | |
| Secondary | 143 | 44.7 | |
| Collage and above | 75 | 23.4 | |
| Partner occupation | Private employment | 99 | 30.9 |
| Government employment | 47 | 14.7 | |
| Merchant | 92 | 28.8 | |
| Student | 3 | 0.9 | |
| Daly laborer | 60 | 18.8 | |
| Other | 19 | 5.9 | |
| Monthly income | <2,000 | 49 | 15.3 |
| 2,000–3,500 | 70 | 21.9 | |
| >3,500 | 201 | 62.8 | |
| Family size | <4 | 287 | 89.7 |
| ≥4 | 33 | 10.3 | |
| Husband support | No | 18 | 5.6 |
| Yes | 302 | 94.4 |
Maternal Characteristics
Most (59.1%) and (58.4%) were multigravidas and started ANC in their first trimester of pregnancy respectively. About three-fourths (77.8%) of the study participants had information about the importance of dietary diversity during pregnancy whereas less than half (42.8%) of respondents had avoided some kind of food during pregnancy. Most (80.3%) of respondents had a meal frequency of three and above per day (Table 2).
TABLE 2.
Maternal characteristics of the study participants (Addis Ababa, Ethiopia, 2021).
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Pregnancy | Prim Gravida | 131 | 40.9 |
| Multigravida | 189 | 59.1 | |
| Time of ANC started | First trimester | 187 | 58.4 |
| Second trimester | 115 | 35.9 | |
| Third trimester | 18 | 5.6 | |
| No of ANC visit | 1st visit | 108 | 33.8 |
| 2nd visit | 98 | 30.6 | |
| 3rd visit | 77 | 24.1 | |
| 4th and above visit | 37 | 11.6 | |
| Had an information about food diversity | 247 | 77.8 | |
| Avoid any food during current pregnancy | 137 | 42.8 | |
| Meal frequency per day | ≥3 times | 257 | 80.3 |
| 2 times | 50 | 15.6 | |
| <2 times | 13 | 4.1 |
Pregnant Women Knowledge of Dietary Diversity
The proportion of women having had a good dietary diversity knowledge during pregnancy was 69.1% (95% CI: 63.7%–74.1%). A large majority of pregnant women (94.1%) knew the importance of food for the growth and development of the fetus during pregnancy, and (93.4%) perceived food is important for fighting infection. More than three fourth (78.8%) of the study participants reported that inadequate diet can cause miscarriage and stillbirth (Table 3).
TABLE 3.
Dietary diversity knowledge of the study participants (Addis Ababa, Ethiopia, 2021).
| Variables | Option | Number | % |
|---|---|---|---|
| Food is important for growth and development of fetus | Yes | 301 | 94.1 |
| Food provides heat, and energy during pregnancy | Yes | 294 | 91.9 |
| Food is important for fighting infection or disease | Yes | 299 | 93.4 |
| Balanced diet is important during pregnancy | Yes | 295 | 92.2 |
| Inadequate diet can cause miscarriage and still Birth | Yes | 252 | 78.8 |
| Carbohydrate source of foods are recommended during pregnancy | Yes | 258 | 80.6 |
| Protein source of foods are recommended during pregnancy | Yes | 274 | 85 |
| Iron source of foods are recommended during pregnancy | Yes | 227 | 70.9 |
| Vitamin A source of foods are recommended during pregnancy | Yes | 277 | 86.6 |
| Iodine source of foods are recommended during pregnancy | Yes | 210 | 65.6 |
Prevalence of Inadequate Dietary Diversity
The prevalence of inadequate dietary diversity during pregnancy was 51.6% (95% CI: 46.1%–57.0%). Most (90%) of the study participants reported that they consumed cereal-based crops (maize, sorghum, millet, wheat, barley, and teff) before the survey. Dark green leafy vegetables (kale, swiss chard, and green pepper) and legumes were consumed by 59.7% and 55.3% of the subjects respectively 1 day before the survey. More than half (52.8%) of the study participants reported that they consumed other vitamins A-rich vegetables (pumpkin, carrot, and orange-fleshed sweet potato). Among animal products, milk and milk products were consumed by (50.9%) of the study group whereas meat, poultry, fish, and egg were consumed by 31.9% and 29.4%, respectively (Table 4).
TABLE 4.
A 24 h food diversity of the study participants (Addis Ababa, Ethiopia, 2021).
| Food groups | Frequency | Percentage |
|---|---|---|
| Cereals | 288 | 90 |
| Legumes | 177 | 55.3 |
| Nuts and seeds | 78 | 22.4 |
| Milk and Dairy products | 163 | 50.9 |
| Meat, poultry and fish | 102 | 31.9 |
| Egg | 94 | 29.4 |
| Dark Green leafy vegetables | 191 | 59.7 |
| Other vitamin A rich fruits and vegetables | 169 | 52.8 |
| Other vegetables | 294 | 91.9 |
| Other fruits | 206 | 64.4 |
Factors Associated With Dietary Diversity Practice
The bivariate logistics regression identified the age of the mother, educational status, knowledge, attitude, and monthly incomes to be the candidate variables for the multivariate logistics regression at a p-value of <0.25. The multivariable logistics regression identified maternal educational status, knowledge and monthly income were factors statistically associated with dietary diversity of the mother.
The odds of having had inadequate dietary diversity was higher by 40.9% among illiterates compared to those of college and above (AOR: 0.591; 95% CI: 1.88–1.901; p < 0.05). The odds of having inadequate dietary diversity was higher by 65.3% among mothers who had completed primary schooling compared to those of college and above (AOR: 0.347; 95% CI: 0.166–0.728; p < 0.05).
The odds of having inadequate dietary diversity was higher by 56.3% among mothers who had poor knowledge compared to good knowledge (AOR: 0.437; 95% CI: 0.252–0.757; p < 0.05). The odds of having inadequate dietary diversity was higher by 65.5% among mothers who had monthly income <2000 compared to >3500monthly income (AOR: 0.395; 95% CI: 0.184–0.845; p < 0.05) (Table 5).
TABLE 5.
Factors affecting dietary diversity of the study participants (Addis Ababa, Ethiopia, 2021).
| Characteristics | Category | Dietary inadequate | Diversity adequate | COR (95%CI) | AOR (95%CI) |
|---|---|---|---|---|---|
| Age in years | <24 | 55 | 33 | 0.840 (0.335–2.1.6) | 1.151 (0.369–3.597) |
| 24–34 | 96 | 112 | 1.633 (0.694–3.845) | 1.494 (0.548–4.074) | |
| ≥35 | 14 | 10 | 1 | 1 | |
| Mother education | Illiterate | 13 | 9 | 0.306 (0.112–0.837)* | 0.599 (1.88–1.901)* |
| Reading and writing | 8 | 3 | 0.166 (0.40–0.6941)* | 0.337 (0.72–1.581) | |
| Primary | 78 | 43 | 0.244 (0.126–0.469)* | 0.347 (0.166–0.728)* | |
| Secondary | 47 | 57 | 0.536 (0.276–1.041) | 0.535 (0.263–1.088) | |
| College and above | 19 | 43 | 1 | 1 | |
| Husband support | No | 12 | 6 | 0.513 (0.188–1.403) | 1.57 (0.373–3.588) |
| Yes | 153 | 149 | 1 | 1 | |
| Knowledge | Poor Knowledge | 67 | 32 | 0.381 (0.231–0.626)* | 0.437 (0.252–0.757)* |
| Good Knowledge | 98 | 123 | 1 | 1 | |
| Attitude | Unfavorable Attitude | 99 | 66 | 0.494 (0.317–0.772)* | 0.782 (0.469–1.305) |
| Favorable Attitude | 66 | 89 | 1 | 1 | |
| Food insecurity | Food secured | 131 | 133 | 1.569 (0.871–2.825) | 1.077 (0.541–2.146) |
| Food Insecure | 34 | 22 | 1 | 1 | |
| Family size | <4 | 148 | 139 | 0.998 (0.485–2.052) | 1.131 (0.481–2.656) |
| >4 | 17 | 16 | 1 | 1 | |
| Income in birr | <2000 | 35 | 14 | 0.299 (0.152–0.590)* | 0.395 (0.184–0.845)a |
| 2000–3,500 | 44 | 26 | 0.442 (0.253–0.773)* | 0.541 (0.286–1.023) | |
| >3,500 | 86 | 115 | 1 | 1 |
*p < 0.05, **p < 0.001 statistically significance level.
Discussion
In this study, the prevalence of inadequate dietary diversity practice during pregnancy was 51.6%, which was in agreement with 57.4% in Southern Ethiopia [35] and 57% in Dire Dewa, Eastern Ethiopia [36]. A study from the United States reported that 46% of pregnant women had inadequate dietary practice [37], this was also consistent with current findings.
Studies from Gondar; Northwest of Ethiopia reported that about 60% of pregnant women had inadequate dietary diversity [38]. Another study from Shashemene, South Western Ethiopia also reported a dietary diversity practice of 74.6% [28]. In these cases, a lower proportion was reported. The observed difference might be due to differences in sample size and time of the investigation across the studies.
Much lower dietary diversity scores were reported by studies 19.6% in Kenya [6]and 19.9% in Gojjam, Northwest Ethiopia [39]. The dietary diversity practice in this study was much higher than in those studies. Such variations might be associated with differences in time of investigation and population.
A study from Malaysia [40] reported a much higher 74% dietary practice than the current study reported. Such variations might be due to differences in population demographics and access to various dietary sources across the population.
In this study, maternal education was statistically associated with dietary diversity, which was supported by the studies from Ghana [41], Kenya [7], Tanzania [42], and Ethiopia [28]. People that are more educated had good dietary diversity compared to those of uneducated in that the more they had an exposure to different nutritional knowledge and information, the higher they tend to use it.
The other factor statistically associated with dietary diversity was maternal knowledge about dietary diversity during pregnancy. Knowledge can affect positively or negatively the practice, through shaping the attitude of people. This was evidently observed in this study that mothers who had poor dietary diversity knowledge had inadequate dietary diversity, which thus was supported by the studies from Malawi [43], and Ethiopia [29].
Additionally, the other factor statistically associated with dietary diversity was monthly income. Those pregnant women who had higher monthly income were more likely to have had adequate dietary diversity compared to their counterparts. This was supported by the studies from Iran [44] and Kenya [7]. This study has the following limitations; The 24 h dietary might not indicate the usual dietary diversity of the pregnant women as the cross sectional nature of the study. The study might have recall and social desirability bias. Moreover, the study used a lower proportion to compute the sample size.
Conclusion
A higher prevalence of inadequate dietary diversity practice during pregnancy was observed in the study settings. Educational status, knowledge, and monthly income were factors identified to affect the dietary diversity during pregnancy. Being illiterate, primary education, poor dietary knowledge, and lower monthly incomes were associated with inadequate dietary diversity during pregnancy in the study settings.
Acknowledgments
The authors thank study participants for their willingness in taking part in the study.
Data Availability Statement
A finding of this study was generated from the data collected and analyzed on the basis of stated methods and materials hence all data were already available in the article.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics and review board of Sante Medical College. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
AOR, Adjusted Odds Ratio; COR, Crude Odds Ratio; DDS, Dietary Diversity Score; WHO, World Health Organization
References
- 1. Darnton-Hill I, Mkparu UC. Micronutrients in Pregnancy in Low-And Middle-Income Countries. Nutrients (2015) 7(3):1744–68. 10.3390/nu7031744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pasricha S-R, Drakesmith H, Black J, Hipgrave D, Biggs B-A. Control of Iron Deficiency Anemia in Low-And Middle-Income Countries. Blood (2013) 121(14):2607–17. 10.1182/blood-2012-09-453522 [DOI] [PubMed] [Google Scholar]
- 3. Victora CG, Christian P, Vidaletti LP, Gatica-Domínguez G, Menon P, Black RE. Revisiting Maternal and Child Undernutrition in Low-Income and Middle-Income Countries: Variable Progress towards an Unfinished Agenda. Lancet (2021) 397(10282):1388–99. 10.1016/S0140-6736(21)00394-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gernand AD, Schulze KJ, Stewart CP, West KP, Christian P. Micronutrient Deficiencies in Pregnancy Worldwide: Health Effects and Prevention. Nat Rev Endocrinol (2016) 12(5):274–89. 10.1038/nrendo.2016.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chaparro CM, Suchdev PS. Anemia Epidemiology, Pathophysiology, and Etiology in Low‐and Middle‐income Countries. Ann N Y Acad Sci (2019) 1450(1):15–31. 10.1111/nyas.14092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kiboi W, Kimiywe J, Chege P. Dietary Diversity, Nutrient Intake and Nutritional Status Among Pregnant Women in Laikipia County, Kenya. Int J Health Sci Res (2016) 6:378–9. [Google Scholar]
- 7. Kiboi W, Kimiywe J, Chege P. Determinants of Dietary Diversity Among Pregnant Women in Laikipia County, Kenya: a Cross-Sectional Study. BMC Nutr (2017) 3(1):12–8. 10.1186/s40795-017-0126-6 [DOI] [Google Scholar]
- 8. Kemunto ML. Dietary Diversity and Nutritional Status of Pregnant Women Aged 15-49 Years Attending Kapenguria District Hospital West Pokot County. Nairobi, Kenya: Kenya kenayatta University Institutional Repository; (2013). [Google Scholar]
- 9. Muthayya S. Maternal Nutrition & Low Birth Weight-What Is Really Important. Indian J Med Res (2009) 130(5):600–8. [PubMed] [Google Scholar]
- 10. Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ. A Meta-Analysis of Depression during Pregnancy and the Risk of Preterm Birth, Low Birth Weight, and Intrauterine Growth Restriction. Arch Gen Psychiatry (2010) 67(10):1012–24. 10.1001/archgenpsychiatry.2010.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. King JC. The Risk of Maternal Nutritional Depletion and Poor Outcomes Increases in Early or Closely Spaced Pregnancies. J Nutr (2003) 133(5):1732S–1736S. 10.1093/jn/133.5.1732S [DOI] [PubMed] [Google Scholar]
- 12. Suhag A, Berghella V. Intrauterine Growth Restriction (IUGR): Etiology and Diagnosis. Curr Obstet Gynecol Rep (2013) 2(2):102–11. 10.1007/s13669-013-0041-z [DOI] [Google Scholar]
- 13. Tudehope D, Vento M, Bhutta Z, Pachi P. Nutritional Requirements and Feeding Recommendations for Small for Gestational Age Infants. J Pediatr (2013) 162(3):S81–S9. 10.1016/j.jpeds.2012.11.057 [DOI] [PubMed] [Google Scholar]
- 14. De Jesus LC, Pappas A, Shankaran S, Li L, Das A, Bell EF, et al. Outcomes of Small for Gestational Age Infants Born at <27 Weeks' Gestation. J Pediatr (2013) 163(1):55–60. e3. 10.1016/j.jpeds.2012.12.097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ehrenkranz RA. Nutrition, Growth and Clinical Outcomes. World Rev Nutr Diet (2014) 110:11–26. 10.1159/000358455 [DOI] [PubMed] [Google Scholar]
- 16. Abu-Saad K, Fraser D. Maternal Nutrition and Birth Outcomes. Epidemiol Rev (2010) 32(1):5–25. 10.1093/epirev/mxq001 [DOI] [PubMed] [Google Scholar]
- 17. Ramakrishnan U, Grant F, Goldenberg T, Zongrone A, Martorell R. Effect of Women's Nutrition before and during Early Pregnancy on Maternal and Infant Outcomes: a Systematic Review. Paediatr Perinat Epidemiol (2012) 26:285–301. 10.1111/j.1365-3016.2012.01281.x [DOI] [PubMed] [Google Scholar]
- 18. Wu G, Imhoff‐Kunsch B, Girard AW. Biological Mechanisms for Nutritional Regulation of Maternal Health and Fetal Development. Paediatr Perinat Epidemiol (2012) 26:4–26. 10.1111/j.1365-3016.2012.01291.x [DOI] [PubMed] [Google Scholar]
- 19. Jolivet RR, Moran AC, O’Connor M, Chou D, Bhardwaj N, Newby H, et al. Ending Preventable Maternal Mortality: Phase II of a Multi-step Process to Develop a Monitoring Framework. BMC Pregnancy Childbirth (2016–20302018) 18(1):258–13. 10.1186/s12884-018-1763-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. WHO. Strategies towards Ending Preventable Maternal Mortality (EPMM). Geneva, Switzerland: World Health Organization; (2015). [Google Scholar]
- 21. Kennedy GL, Pedro MR, Seghieri C, Nantel G, Brouwer I. Dietary Diversity Score Is a Useful Indicator of Micronutrient Intake in Non-breast-feeding Filipino Children. J Nutr (2007) 137(2):472–7. 10.1093/jn/137.2.472 [DOI] [PubMed] [Google Scholar]
- 22. Chakona G, Shackleton C. Minimum Dietary Diversity Scores for Women Indicate Micronutrient Adequacy and Food Insecurity Status in South African Towns. Nutrients (2017) 9(8):812. 10.3390/nu9080812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kennedy G, Fanou-Fogny N, Seghieri C, Brouwer ID. Dietary Diversity as a Measure of the Micronutrient Adequacy of Women's Diets: Results from Bamako, Mali Site (2009). [Google Scholar]
- 24. Lartey A. Maternal and Child Nutrition in Sub-saharan Africa: Challenges and Interventions. Proc Nutr Soc (2008) 67(1):105–8. 10.1017/S0029665108006083 [DOI] [PubMed] [Google Scholar]
- 25. Baumgartner J. Antenatal Multiple Micronutrient Supplementation: Benefits beyond Iron-Folic Acid Alone. Lancet Glob Health (2017) 5(11):e1050–1. 10.1016/S2214-109X(17)30389-3 [DOI] [PubMed] [Google Scholar]
- 26. Persson LÅ. Prenatal Nutrition, Socioenvironmental Conditions, and Child Development. Lancet Glob Health (2017) 5(2):e127–8. 10.1016/S2214-109X(16)30356-4 [DOI] [PubMed] [Google Scholar]
- 27. Weerasekara PC, Withanachchi CR, Ginigaddara G, Ploeger A. Understanding Dietary Diversity, Dietary Practices and Changes in Food Patterns in Marginalised Societies in Sri Lanka. Foods (2020) 9(11):1659. 10.3390/foods9111659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Desta M, Akibu M, Tadese M, Tesfaye M. Dietary Diversity and Associated Factors Among Pregnant Women Attending Antenatal Clinic in Shashemane, Oromia, Central Ethiopia: a Cross-Sectional Study. J Nutr Metab (2019) 2019:3916864. 10.1155/2019/3916864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zerfu TA, Biadgilign S. Pregnant Mothers Have Limited Knowledge and Poor Dietary Diversity Practices, but Favorable Attitude towards Nutritional Recommendations in Rural Ethiopia: Evidence from Community-Based Study. BMC Nutr (2018) 4(1):43–9. 10.1186/s40795-018-0251-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Yeneabat T, Adugna H, Asmamaw T, Wubetu M, Admas M, Hailu G, et al. Maternal Dietary Diversity and Micronutrient Adequacy during Pregnancy and Related Factors in East Gojjam Zone, Northwest Ethiopia, 2016. BMC Pregnancy Childbirth (2019) 19(1):173–9. 10.1186/s12884-019-2299-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Weldehaweria NB, Misgina KH, Weldu MG, Gebregiorgis YS, Gebrezgi BH, Zewdie SW, et al. Dietary Diversity and Related Factors Among Lactating Women Visiting Public Health Facilities in Aksum Town, Tigray, Northern Ethiopia. BMC Nutr (2016) 2(1):38–9. 10.1186/s40795-016-0077-3 [DOI] [Google Scholar]
- 32. Fite MB, Tura AK, Yadeta TA, Oljira L, Roba KT. Prevalence and Determinants of Dietary Practices Among Pregnant Women in Eastern Ethiopia. BMC Nutr (2022) 8(1):3–10. 10.1186/s40795-021-00494-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Idf DAG. Update of Mortality Attributable to Diabetes for the IDF Diabetes Atlas: Estimates for the Year 2013. Diabetes Res Clin Pract (2015) 109(3):461–5. 10.1016/j.diabres.2015.05.037 [DOI] [PubMed] [Google Scholar]
- 34. Saaka M, Mutaru S, Osman SM. Determinants of Dietary Diversity and its Relationship with the Nutritional Status of Pregnant Women. J Nutr Sci (2021) 10:e14. 10.1017/jns.2021.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Delil R, Zinab B, Mosa H, Ahmed R, Hassen H. Determinants of Dietary Diversity Practice Among Pregnant Women Attending Antenatal Clinic at Wachemo University Nigist Eleni Mohammed Memorial Referral Hospital, Southern Ethiopia. PloS one (2021) 16(4):e0250037. 10.1371/journal.pone.0250037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shenka A, Damena M, Abdo M, Roba KT. Dietary Diversity and Nutritional Status of Pregnant Women Attending Public Hospitals in Dire Dawa City Administration, Eastern Ethiopia. East Afr J Health Biomed Sci (2018) 2(1):10–7. [Google Scholar]
- 37. Shehab L. Nutritional Awareness of Women during Pregnancy. J Am Sci (2012) 8(7). [Google Scholar]
- 38. Alemayehu MS, Tesema EM. Dietary Practice and Associated Factors Among Pregnant Women in Gondar Town north West, Ethiopia, 2014. Int J Nutr Food Sci (2015) 4(6):707–12. 10.11648/j.ijnfs.20150406.27 [DOI] [Google Scholar]
- 39. Demilew YM, Alene GD, Belachew T. Dietary Practices and Associated Factors Among Pregnant Women in West Gojjam Zone, Northwest Ethiopia. BMC Pregnancy Childbirth (2020) 20(1):18–1. 10.1186/s12884-019-2702-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mirsanjari M, Muda W, Ahmad A, Othman MS, Mosavat M. Does Nutritional Knowledge Have Relationship with Healthy Dietary Attitude and Practices during Pregnancy. ICNFS (2012) 39:159–63. [Google Scholar]
- 41. Amugsi DA, Lartey A, Kimani-Murage E, Mberu BU. Women’s Participation in Household Decision-Making and Higher Dietary Diversity: Findings from Nationally Representative Data from Ghana. J Health Popul Nutr (2016) 35(1):16–8. 10.1186/s41043-016-0053-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ochieng J, Afari-Sefa V, Lukumay PJ, Dubois T. Determinants of Dietary Diversity and the Potential Role of Men in Improving Household Nutrition in Tanzania. PloS one (2017) 12(12):e0189022. 10.1371/journal.pone.0189022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Katenga-Kaunda LZ, Kamudoni PR, Holmboe-Ottesen G, Fjeld HE, Mdala I, Shi Z, et al. Enhancing Nutrition Knowledge and Dietary Diversity Among Rural Pregnant Women in Malawi: a Randomized Controlled Trial. BMC Pregnancy Childbirth (2021) 21(1):644–11. 10.1186/s12884-021-04117-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Vakili M, Abedi P, Sharifi M, Hosseini M. Dietary Diversity and its Related Factors Among Adolescents: a Survey in Ahvaz-Iran. Glob J Health Sci (2013) 5(2):181–6. 10.5539/gjhs.v5n2p181 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
A finding of this study was generated from the data collected and analyzed on the basis of stated methods and materials hence all data were already available in the article.