Abstract
Background
The COVID-19 pandemic and restrictions on travel and quarantine measures made people turn to self-medication (SM) to control the symptoms of their diseases. Different studies were conducted worldwide on different populations, and their results were different. Therefore, this global systematic review and meta-analysis was conducted to estimate the pooled prevalence of self-medication.
Methods
In this systematic review and meta-analysis, databases of Scopus, PubMed, Embase, and Web of Science were searched without a time limit. All eligible observational articles that reported self-medication during the COVID-19 pandemic were analyzed. Heterogeneity among the studies was assessed using Cochran's Q test and I2 statistics. A random-effects model was used to estimate the pooled prevalence of self-medication. The methodological quality of the articles was evaluated with the Newcastle-Ottawa Scale.
Results
Fifty-six eligible studies were reviewed. The pooled prevalence of self-medication was 48.6% (95% CI: 42.8–54.3). The highest and lowest prevalence of self-medication was in Asia (53%; 95% CI: 45–61) and Europe (40.8%; 95% CI: 35–46.8). Also, the highest and lowest prevalence of self-medication was related to students (54.5; 95% CI: 40.8–68.3) and healthcare workers (32.5%; 16–49). The prevalence of self-medication in the general population (48.8%; 40.6–57) and in patients with COVID-19 (41.7%; 25.5–58). The prevalence of self-medication was higher in studies that collected data in 2021 than in 2020 (51.2 vs. 48%). Publication bias was not significant (p = 0.320).
Conclusion
During the COVID-19 pandemic, self-medication was highly prevalent, so nearly half of the people self-medicated. Therefore, it seems necessary to provide public education to control the consequences of self-medication.
Keywords: self-medication, prevalence, systematic review, COVID-19, meta-analysis
Introduction
On January 30, 2020, the World Health Organization (WHO) declared a state of public health emergency due to the emergence of COVID-19 disease. Six months later, ~20 million cases and 700,000 deaths were reported worldwide (1). People resorted to self-medication (SM) due to the fear of contracting COVID-19, misinformation, and low access to health services. With people confined to their homes, the Internet was the only source of information they had access to. Also, when the hospitals were filled with patients, people were afraid to go to the hospitals and started self-medication (2).
Self-medication refers to choosing and using drugs to treat self-diagnosed symptoms and diseases without consulting a doctor (3). Self-medication includes the purchase and use of over-the-counter (OTC) medications, prescription-only medications (POMs), and leftover medication out of recommended (4). Self-medication leads to resource waste, increased pathogens resistance, and antibiotic resistance (3, 5). Also, self-medication is associated with incorrect dosage, incorrect route of administration, long-term use, improper storage, drug interactions, polypharmacy, and the risk of dependence and abuse, so it has become a serious public health problem worldwide (6, 7). In most cases, the feeling of the mildness of the disease and no need to consult a doctor, previous pleasant experiences with self-treatment, the feeling of being able to self-care, and the lack of availability of a doctor increase self-treatment (4). Furthermore, socio-economic factors, lifestyle, sources of medical information, access to medicines, and the potential of managing some diseases through self-care are related to the continuous increase of self-treatment worldwide (7, 8). On the other hand, self-treatment reduces the economic burden on patients, the high cost of hospital treatments, and the pressure on health care systems, limiting the number of hospital visits (6, 9). Because self-treatment starts with self-diagnosis, the probability of its being incorrect is high, and even a correct diagnosis can be associated with the wrong treatment choice. Also, the average consumers do not know if they are in a particular group with significant side effects of medicine or not; they are unaware of drug contraindications. Sometimes, the patients take the same active ingredient with a different name, and there is a risk of double medication or harmful interactions. Sometimes there is a risk of the wrong prescription (e.g., intravenous instead of intramuscular) (10).
Different studies that have investigated the prevalence of self-medication in the COVID-19 pandemic around the world have reported different results. Knowing the prevalence of self-medication in this pandemic can provide health policymakers and researchers with helpful information. Therefore, the present study was conducted to estimate the overall prevalence of self-medication in the COVID-19 pandemic.
Methods
This systematic review and meta-analysis, which sought to estimate the pooled prevalence of self-medication in endemic COVID-19 globally, was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (11). The PRISMA checklist is attached as a Supplementary File 1. The protocol of this systematic review was not registered in Cochrane and PROSPERO.
Search strategy
We searched PubMed, Scopus, Web of Science, and Embase databases from January 2020 to May 2022 using the following terms: (“Self Medication” OR “Self Medicat*” OR “SelfMedicat*”) AND (“COVID-19” OR “SARS-CoV-2” OR “COVID 19” OR “2019-nCoV” OR “Coronavirus Disease-19” OR “SARS CoV 2” OR “2019 Novel Coronavirus” OR “Wuhan Coronavirus” OR “SARS Coronavirus 2” OR “Wuhan Seafood Market Pneumonia Virus”). Databases were searched in June 2022. To access more articles, the reference list of selected articles was reviewed. Further details are provided in Table 1.
Table 1.
The search strategy.
| PubMed | (“Self Medication”[Mesh] OR “Self Medicat*”[tiab] OR “Self-Medicat*”[tiab] OR “SelfMedicat*”[tiab]) AND (“COVID-19”[Mesh] OR “SARS-CoV-2”[Mesh] OR “COVID 19”[tiab] OR “2019-nCoV”[tiab] OR “Coronavirus Disease-19”[tiab] OR “SARS CoV 2”[tiab] OR “2019 Novel Coronavirus”[tiab] OR “Wuhan Coronavirus”[tiab] OR “SARS Coronavirus 2”[tiab] OR “Wuhan Seafood Market Pneumonia Virus”[tiab] ) |
| Scopus | TITLE-ABS-KEY(“Self Medicat*” OR “Self-Medicat*” OR “SelfMedicat*”) AND TITLE-ABS-KEY (“COVID-19” OR “SARS-CoV-2” OR “COVID 19” OR “2019-nCoV” OR “Coronavirus Disease-19” OR “SARS CoV 2” OR “2019 Novel Coronavirus” OR “Wuhan Coronavirus” OR “SARS Coronavirus 2” OR “Wuhan Seafood Market Pneumonia Virus”) |
| Web of science | TS=(“Self Medicat*” OR “Self-Medicat*” OR “SelfMedicat*”) AND TS=(“COVID-19” OR “SARS-CoV-2” OR “COVID 19” OR “2019-nCoV” OR “Coronavirus Disease-19” OR “SARS CoV 2” OR “2019 Novel Coronavirus” OR “Wuhan Coronavirus” OR “SARS Coronavirus 2” OR “Wuhan Seafood Market Pneumonia Virus”) Timespan: All years. Indexes: SCI-EXPANDED, SSCI, A&HCI, ESCI. |
| Embase | ('Self Medicat*':ta,ab,kw OR 'Self-Medicat*':ta,ab,kw OR 'SelfMedicat*':ta,ab,kw) AND ('COVID-19':ta,ab,kw OR 'SARS-CoV-2':ta,ab,kw OR 'COVID 19':ta,ab,kw OR '2019-nCoV':ta,ab,kw OR 'Coronavirus Disease-19':ta,ab,kw OR 'SARS CoV 2':ta,ab,kw OR '2019 Novel Coronavirus':ta,ab,kw OR 'Wuhan Coronavirus':ta,ab,kw OR 'SARS Coronavirus 2':ta,ab,kw OR 'Wuhan Seafood Market Pneumonia Virus':ta,ab,kw) |
Selection of studies and data extraction
The inclusion criteria were: observational studies reporting data on the prevalence or frequency of self-medication during the COVID-19 pandemic and published in English. Exclusion criteria included unrelated studies, interventional studies, review articles, theses, case reports, and repeated articles. According to the inclusion and exclusion criteria, the authors independently read the title and abstract of all articles and separated the relevant ones. In the next step, the authors reviewed the full text of these articles, and essential information such as the first author's name, year of publication, sample size, type of study, country, target group, mean age, and time of data collection were recorded in a pre-prepared form. Any disagreement was resolved by consultation and discussion.
Quality assessment
We used the Newcastle-Ottawa scale to check the methodological quality and assess the bias of the articles, which included seven items and three dimensions of selection, comparison, and result. These dimensions were assigned 5, 2, and 3 stars, respectively. The selection dimension with four items evaluates the target population, sample size estimation, non-response rate, and measurement tool. The first three items can be assigned up to one star and the fourth item up to two stars. The comparable dimension evaluates the use of the control group and can get up to two stars. The result dimension has two items evaluating the result (two stars) and statistical tests (one star). High-quality articles were defined as ≥4 stars (12). The bias assessment was checked by two authors independently, and any disagreements were resolved through consultation.
Meta-analysis
STATA version 16 software was used for data analysis. We used the binomial distribution to combine the selected studies. To show the general prevalence of self-medication from the Forest plot and to examine the heterogeneity among the selected studies, we used the I2 index and Cochran's Q test. We considered the I2 level >75% as high heterogeneity. Because the I2 index in this study was more than 75% and Cochran's Q test was significant, the random effects model was used to combine the selected studies. Subgroup analysis was performed based on the continent, target population, and year of data collection. Also, a meta-regression test was used to investigate the relationship between the prevalence of self-medication and the mean age of the participants. The publication bias of the studies was evaluated using a funnel plot based on Egger's regression.
Results
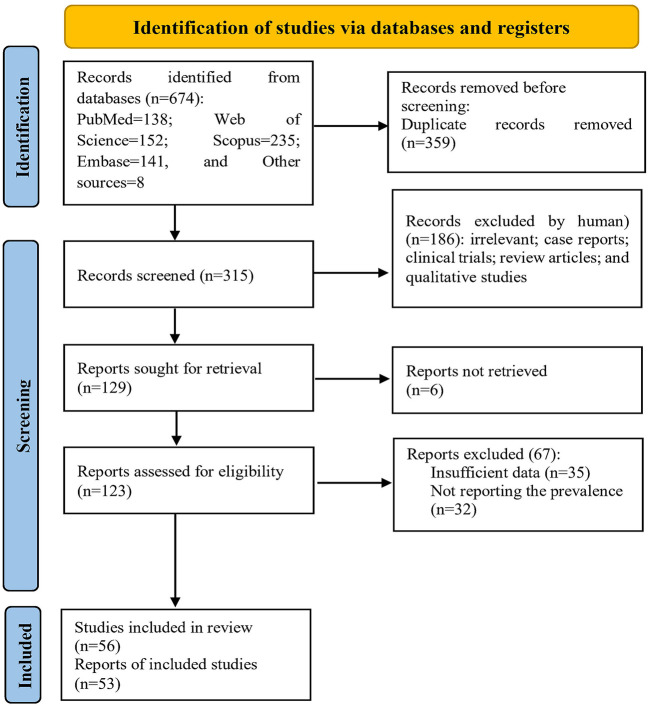
In the initial search, 674 articles were retrieved, of which 359 were removed due to duplication. Then, the authors independently reviewed the remaining articles' titles and abstracts. After screening the articles based on the inclusion and exclusion criteria, 186 articles were excluded. The full text of six articles could not be retrieved. The full text of the remaining 123 articles was reviewed. Sixty-seven articles were excluded due to not reporting the prevalence of self-medication or incomplete reports. Finally, 56 articles with a sample size of 56,063 subjects were included in the analysis (Figure 1).
Figure 1.
The process of screening and selecting the articles based on the PRISMA guidelines.
In terms of quality, 32 articles had moderate quality, and 24 studies had excellent quality (Supplementary File 2). Twenty-six studies were published in 2022, 24 in 2021, and 6 in 2020. Twelve articles published in 2022, 14 published in 2021, and two published in 2020 were high quality. Most of the studies were conducted in the Asian continent (n = 31) and on the general population (n = 29). Also, the data of 31 studies were collected in 2020. Most studies were conducted in three countries: India (n = 11), Saudi Arabia (6 studies), and Nigeria (6 studies) (Table 2). The pooled prevalence of self-medication in these three countries was 45% (95% CI: 35–55), 57% (95% CI: 43–71), and 43.5% (95% CI: 26.5–60.5), respectively.
Table 2.
The characteristics of included studies.
| First author | Year | Sample size | Country | Mean age | Target group | Prevalence (%) | Date of data collection | Self-medication agent | Findings | Quality |
|---|---|---|---|---|---|---|---|---|---|---|
| Alsaad (7) | 2022 | 1,226 | Saudi Arabia | – | General population | 59 | January to February 2021 | – | The highest prevalence of SM was in women, workers in health departments—excluding physicians and pharmacists- and people with chronic diseases. | High |
| Kashyap (13) | 2022 | 326 | India | – | Medical students | 29.8 | – | Supplementary medicines | About one-third of the participants stated they self-medicated to prevent or treat COVID-19. Also, the most common reason for SM was easy to access. | High |
| Malik (14) | 2022 | 451 | Pakistan | – | Dental patients | 86.2 | September to December 2020 | Pain relievers and Antibiotics | The most common causes of SM were toothache (56.8%), and tooth sensitivity (37.5%). | Moderate |
| Likhar (15) | 2022 | 394 | India | – | Medical students | 73.8 | – | – | The main reason for SM was convenience (23.09%) and the intention of getting quick relief (21.06%). | Moderate |
| Aitafo (6) | 2022 | 220 | Nigeria | – | HCWs | 15.9 | January to March 2022 | Vitamin C, Zinc, Azithromycin, and anti-malarial | The main reason for SM was the fear of getting infected following contact with suspected or confirmed cases of COVID-19 | High |
| Alavi Namvar (16) | 2022 | 306 | Iran | 34.9 | Dental patients | 53.9 | October 2020 and April 2021 | Ibuprofen; Acetaminophen; Novafen; Mefenamic acid; Amoxicillin; Metronidazole; Penicillin; and Salt and water mouthwash | Low education level was associated with SM. The most common problem for SM was toothache. | Moderate |
| Barakat (17) | 2022 | 245 | Egypt | – | General population | 38 | – | – | The most predictors of SM were internet use for getting medical information (OR = 2.1, p = 0.02), lack of health education about COVID-19 (OR = 2.1, p = 0.03), and younger age (OR = 0.9, p = 0.03). | Moderate |
| Yasmin (18) | 2022 | 489 | Pakistan | – | Medical students | 83 | January to February 2021 | Paracetamol and multivitamins | Most SM was reported in women, third-year medical students and people in good self-reported health. | High |
| Acharya (3) | 2022 | 383 | USA | – | Medical students and staff | 50.4 | November 2021 | Paracetamol, Vitamin C; Zinc; Multivitamins; Vitamin D; Azithromycin; Cough syrup; and Ibuprofen | More than half of the participants purchased the medicines directly from the pharmacy. | Moderate |
| Alateeq (19) | 2022 | 443 | Saudi Arabia | 37.56 | General population | 44 | July to August 2021 | Dietary Supplements | The predictors of dietary supplement use were insomnia and a history of mental health disorder diagnosis. | High |
| Amuzie (20) | 2022 | 469 | Nigeria | 39.9 ± 13.5 | General population | 30.3 | October to November 2021 | Herbal products; Antimalarial; Vitamin Supplements; Azithromycin; Ivermectin; Analgesics; Calcium Supplements; Hydroxychloroquine; Ciprofloxacin | Older age (AOR = 1.87), primary education (AOR = 2.15) and perception of cost (AOR = 2.29) were predictors of self-medication. | High |
| Bello (21) | 2022 | 356 | Nigeria | 20.34 | Students | 65.4 | May to August 2020 | Paracetamol; Tramadol; Cold syrup; Vitamin C; Herbs; Anti-Malaria; Anti-Diarrhea; Piriton; Slimming Pills and Teas; Food Supplements; and Hydroxychloroquin | Experience of COVID-19 symptoms significantly predicted SM. The prevalence of SM was not significantly different between male and female undergraduate students. | High |
| Gaviria-Mendoza (22) | 2022 | 397 | Columbia | 31 | General population | 34.3 | June to September 2020 | Acetaminophen; Antihistamines; Vitamins; and Antibiotics | The reasons for SM to prevent COVID-19 were: distrust of personnel and health centers (OR = 10.4; p = 0.013) and fear of being fined for leaving home (OR = 7.29; p = 0.026). | Moderate |
| Dehghan (23) | 2022 | 782 | Iran | – | General population | 84 | April to August 2021 | Nutritional supplements | SM was associated with sex, having children, place of residence, and COVID-19 status. | High |
| Gerbier (24) | 2022 | 5,210 | European countries | – | Pregnant and Postpartum Women | 41.4 | June to August 2021 | Paracetamol; Cetirizine; Omeprazole; Acetylsalicylic acid; Lactulose; Metoclopramide; Salbutamol; Levothyroxine sodium; and Antibiotics | Analgesics were the most commonly used drugs. Antihistamines and drugs for gastric-related disorders were the most commonly used drugs. Also, NSAIDs and antihistamines were the most commonly used drugs in women. | High |
| González-González (25) | 2022 | 284 | Mexico | – | University Students | 26 | 2020 | Herbal; Medicinal Drugs; Vitamins; and Chlorine dioxide | About 20% of the participants had self-medicated to prevent COVID-19. The prevalence of SM did not differ between men and women. | Moderate |
| Gupta (26) | 2022 | 170 | India | 38.6 ± 10.7 | Students | 57.7 | August 2020 | pain suppression; Antibiotics and anti-acid medications | Students with less educated tend to SM more than those with higher education (OR = 2.200, 95% CI = 1.116–4.336). | Moderate |
| Heemskerk (27) | 2022 | 361 | France | – | General population | 34.6 | November 2020 and January 2021 | Vitamins; herbal or home remedies | A third of the participants had used SM to protect themselves against COVID-19 and boost their immune systems. Women were more likely than men to use over-the-counter medications, vitamins, and herbal/home remedies to protect themselves from COVID-19. | Moderate |
| Joseph (28) | 2022 | 225 | India | 34.5 ± 15.2 | General population | 34.2 | August 2021 | Paracetamol | The most common symptom for which SM was performed was a cold, and the most common drug used was paracetamol. Participants with a history of self-medication among family members, relatives, or friends were more likely to self-medicate. The idea that SM is harmful was more in women than in men. | High |
| Kumari (29) | 2022 | 57 | India | 46.3± 8.8 | Faculty employed | 50.8 | – | Analgesics; Vitamins; Antibiotics; and Anti-allergic drugs | The most common reason for SM was that it was less costly. Doctors at work were the most common source of information. The most common symptom that caused SM was pain. The most common drug used was analgesics. | Moderate |
| Mahmoudi (30) | 2022 | 450 | Iran | – | COVID-19 patients | 56.1 | March to October 2020 | Not reported | Not reported | Moderate |
| Odis (31) | 2022 | 402 | Nigeria | – | Outpatients | 71.9 | February 2021 | Acetaminophen; Ibuprofen; Azithromycin; Penicillin; Antiretrovirals; and hydroxychloroquine | Older people used antiretroviral drugs more than other age groups. | Moderate |
| Okoye (32) | 2022 | 669 | Nigeria | 35.6 ± 8.7 | HCWs | 36.3 | March and April 2021 | Ivermectin; Azithromycin; Vitamin C; Chloroquine; and zinc | Factors associated with self-medication were: older age, being a pharmacist, higher income, and previous COVID-19 test. Age > 44 years (AOR = 2.77) and previous COVID-19 test (AOR = 2.68) were predictors of SM. | High |
| Rojas-Miliano (33) | 2022 | 166 | Peru | – | Students | 14.5 | October to November 2020 | Paracetamol; Aspirin; and Influenza drugs | SM was associated with the perception that SM is harmful to health (PR = 0.41; 95% CI = 0.20–0.84) and having a doctor as a source of medication information (PR = 0.46; CI = 0.21–0.99). | High |
| Toure (34) | 2022 | 975 | Guinea | – | Health centers staff | 14.1 | June 2021 | Not reported | Fatigue (OR = 2.11), sore throat (OR = 1.89), loss of smell (OR = 4.64), and sore throat of a close person (OR = 2.32) were independently associated with SM. | Moderate |
| Vasquez-Elera (35) | 2022 | 301 | Peru | 58.6 ± 16.4 | COVID-19 patients | 54.8 | May to June 2020 | Vermectin; Azithromycin; Corticosteroids; and NSAIDs | The frequency of SM in people between 30 and 59 years old was 2.53 times higher than in people between 18 and 29 years old. Also, male gender, dyslipidemia, smoking, and hepatic steatosis were related to SM. | Moderate |
| Zeng (36) | 2021 | 70 | China | – | COVID-19 patients | 31.4 | January to February 2020 | Traditional Chinese medicine; Acetaminophen Levofloxacin; Antivirals; and Antibiotics | Not reported | Moderate |
| Saleem (37) | 2021 | 520 | Saudi Arabia | 21.8 ± 1.9 | Students | 58 | March to June 2020 | Analgesics; Antibiotics; Antipyretics; Antihistamines; Antidiarrheal, Antiemetic; Antacid; Laxatives; Food supplements; and Vitamins | The most reasons for SM were: symptoms are minor, experience, saving time, pharmacist advice, and saving money. | High |
| Sadio (1) | 2021 | 955 | Togo | – | General population | 34.2 | April to May 2020 | Vitamin C and traditional medicine | Female sex (AOR = 1.90), work in the health sector (AOR = 1.89), secondary education level (AOR = 2.28), and university education level (AOR = 5.11) were associated with SM. | High |
| Ruiz-Padilla (38) | 2021 | 16,724 | Mexico | – | General population | 35.3 | March to November 2020 | Aspirin; Ibuprofen; Dexamethasone; Azithromycin, Ivermectin; Hydroxychloroquine; and Chloroquine | The factors associated with SM were age (18–25 years), female gender, low education level, low socioeconomic status, being married, unemployment, and the presence of comorbidity. | High |
| Mota (39) | 2021 | 710 | Brazil | – | HCWs | 60.3 | May to July 2020 | Insomnia medication | About two-thirds of the total sample had some sleep-related complaints, 25.8% due to difficulty initiating sleep, 29.6% due to difficulty staying asleep, and 32.5% due to early morning waking. | Moderate |
| Zhang (40) | 2021 | 2,217 | Australia | – | General population | 19.5 | March 2020 | Antibiotics | Age (OR = 0.89), gender (OR = 1.29), and education (OR = 1.13) were associated with antibiotic use for protection against COVID-19. | Moderate |
| Heshmatifar (41) | 2021 | 342 | Iran | 66.2 ± 5.67 | Elderly | 55.5 | – | Analgesics; vitamins; Anti-cold; and Antibiotics | The main factors related to SM were disease prevention, home quarantine, financial problems, previous experience of SM, and others' advice. | Moderate |
| Ainsy Goldlin (42) | 2021 | 323 | India | – | General population | 39.6 | June and July 2020 | Hydroxychloroquine; Azithromycin; Ivermectin; Herbal preparations, Vitamins; and Minerals preparations | The main factors related to SM were COVID-19 spread and mortality, fear of visiting hospitals, time saving, lack of easy access to hospitals, easy availability of drugs in local pharmacies, trust in online information and being familiar with the drugs | Moderate |
| Alonso-Castro (43) | 2021 | 2,100 | Mexico | 32.1± 13.6 | General population | 61.9 | March and June 2020 | Herbs | Female gender, age < 40 years, low education level, being single, unemployment, presence of mental illness, use of psychiatric drugs, and drug use were among the factors related to self-medication. | High |
| Azhar (44) | 2021 | 290 | Pakistan | – | General population | 46.7 | – | Analgesics; Hydroxychloroquinone; Azithromycin; and Ivermectin | The most frequent reason for SM was the unavailability of doctors. | Moderate |
| Chopra (45) | 2021 | 1,100 | India | – | General population | 25 | May 2020 | Hydroxychloroquine; Herbal drugs; Vitamins; Antimicrobials; Antihistamines | SM was more common in women than men and in married people than single people. | Moderate |
| D'arqom (46) | 2021 | 610 | Indonesia | – | Women | 75 | July to December 2020 | Anti-COVID medications; Vitamins; and Herbal Supplements | SM in housewives was related to education, and SM in working women was related to age and family income. | High |
| Faqihi (47) | 2021 | 177 | Saudi Arabia | 20 ± 3 | Nursing students | 87 | December 2019 to February 2020 | Acetaminophen; Ibuprofen; Diclofenac Meloxicam; Aspirin; Azithromycin; Amoxicillin; Doxycycline; Metronidazole; and Ampicillin | The most common self-medication causes were headaches, menstrual pain, and fever. The main reason for self-medication was a lack of time to consult a doctor. | Moderate |
| Mir (48) | 2021 | 168 | India | – | General population | 59.9 | May 2021 | Paracetamol; Azithromycin; Expectorants; Ivermectin; Doxycycline; Corticosteroids; Hydroxychloroquine | Not reported | Moderate |
| Islam (49) | 2021 | 1,002 | Bangladesh | 34.7 ± 13.9 | COVID-19 patients | 24 | September to October 2020 | Not reported | Lower socioeconomic status and persistent symptoms of COVID-19 were associated with SM. The main reasons for SM were: insufficient local medical services, dissatisfaction with local health care services, cost of a consultation with doctors, and lack of time. | Moderate |
| Elayeh (50) | 2021 | 1,179 | Jordan | 32.0 ± 12.5 | General population | 80.4 | March to April 2021 | Antihistamine; Cold preparations; Immune boosters; Omega-3; Propolis; Vitamins; Iron; Zink; Ibuprofen; Paracetamol; Magnesium | Female gender (OR = 1.603), working in the medical field (OR = 1.697), and history of COVID- 19 infection (OR = 2.026) were associated with SM. | High |
| Choudhary (51) | 2021 | 100 | India | 36.94 ± 11.83 | Dermatology patients | 48 | June 2020 | Steroids; Antibiotics; Antifungals; Immunomodulators; Antihistamines; and Dithranol | Fear of infection from healthcare facilities and reduced access to healthcare facilities due to lockdown because of COVID-19 were associated with SM. | Moderate |
| Sen Tunc (52) | 2021 | 389 | Turkey | – | Parents | 70.2 | July to October 2020 | Analgesics; antibiotics; mouthwashes; and herbal medicines | The main reason for SM was difficulty obtaining a dental consultation. | High |
| Sikdar (53) | 2021 | 2,941 | Bangladesh | – | General population | 7.14 | November to December 2020 | Sedatives; Anxiolytics; and Anti-depressant drugs | SM was more in people over 35 years old and men than in other groups. | Moderate |
| Quispe-Cañari (54) | 2021 | 3,792 | Peru | – | General population | 43.8 | May to June 2020 | Vitamin C; Traditional medicines; Chloroquine/Hydroxychloroquine | There was a relationship between age, the region where one lived, and job status with SM. | High |
| Tekeba (55) | 2021 | 416 | Ethiopia | 24.3 ± 5.1 | Pharmacy clients | 73.6 | June 2020 | Painkillers; Antibiotics; Cough syrup; Antacid; and Oral contraceptive | SM was associated with age 18–24 years (AOR = 9.28), and 25–34 years (AOR = 3.54), current single status (AOR = 0.28), government employment (AOR = 0.31), and limited knowledge (AOR = 2.31). | High |
| Tobaiqi (56) | 2021 | 281 | Saudi Arabia | – | General population | 58 | July to September 2020 | Laxatives; Antacid; Eye drops; Vitamins; Herbs; Antibiotics; Analgesics | The most common symptom that caused the use of SM was a headache. Also, the most used drug in SM was painkillers. | Moderate |
| Vinay (57) | 2021 | 39 | India | 39.6 ± 14.1 | Inflammatory Bowel Disease Patients | 17.9 | March to June 2021 | Steroids | Not reported. | Moderate |
| Wegbom (58) | 2021 | 461 | Nigeria | 42.2 ± 10.7 | General population | 41 | June to July 2020 | Hydroxychloroquine; Chloroquine; Erythromycin; Metronidazole; Herbal products; Ciprofloxacin; Vitamins | Male gender (OR = 0.79) and having sufficient knowledge about SM (OR = 0.64) were associated with SM. | High |
| Onchonga (59) | 2020 | 379 | Kenya | – | HCWs | 36.2 | – | Not reported | Physically active participants who worked during the day and were healthy were less likely to self-medicate. | High |
| Heydargoy (60) | 2020 | 168 | Iran | – | General population | 20.8 | – | Antibiotics | Not reported | Moderate |
| Makowska (61) | 2020 | 1013 | Poland | – | General population | 45.6 | June 2020 | Not reported | Not reported | High |
| Mansuri (62) | 2020 | 385 | Saudi Arabia | – | General population | 35.1 | March to April 2020 | Not reported | Not reported | Moderate |
| Nasir (63) | 2020 | 626 | Bangladesh | – | General population | 88.3 | April to May 2020 | Ivermectin; Azithromycin; Montelukast; Calcium supplements; Doxycycline; Hydroxychloroquine | The most important symptoms that caused SM were fever, throat pain, and dry cough. | Moderate |
| de los Angeles (64) | 2020 | 829 | Ecuador | – | General population | 96.2 | – | Eucalyptus; Ginger | Not reported | Moderate |
NSAIDs, non-steroidal anti-inflammatory drugs; OR, odds ratio; AOR, adjusted odds ratio; PR, prevalence ratio; CI, confidence interval.
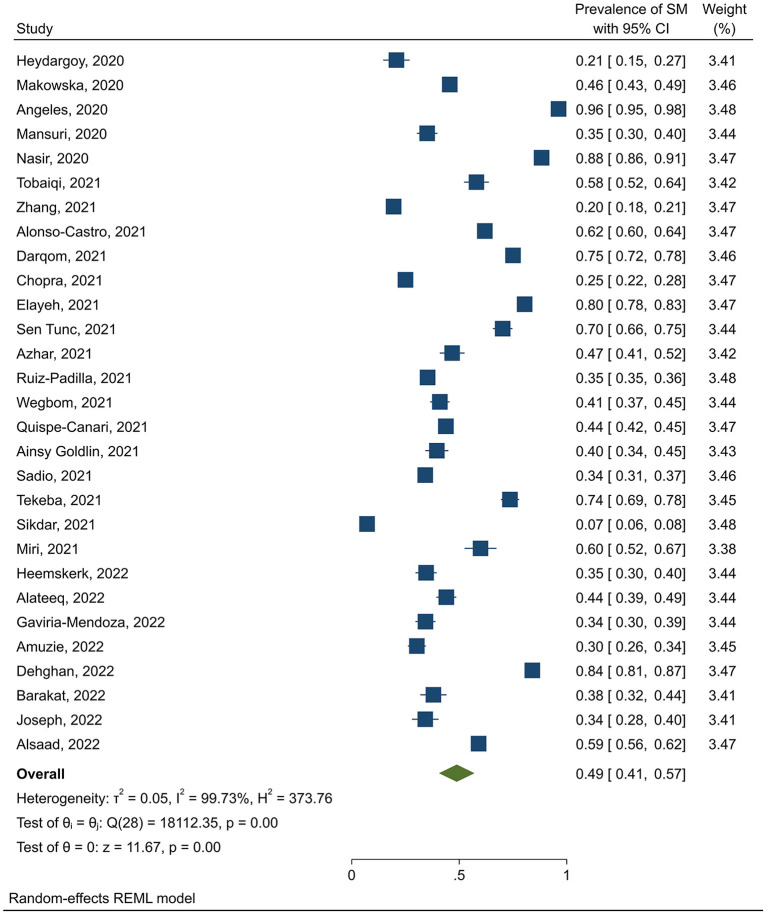
The pooled prevalence of self-medication was 49% (95% CI: 43–54). Also, the findings by continent showed that the highest and lowest prevalence of self-medication was in Asia (53%, 95% CI: 45–61) and Europe (40.8%, 95% CI: 35–46.8), respectively. The prevalence of self-medication in America (47.8%, 95% CI: 33.6–62) was higher than in Africa (41.5%, 95% CI: 29.5–53.5). By dividing the target population, the findings showed that the highest and lowest prevalence of self-treatment was related to students (54.5%, 95% CI: 40.8–68.3) and healthcare workers (35.5%, 95% CI: 16–49). The prevalence of self-medication in the general population was 49% (95% CI: 41–57) (Figure 2).
Figure 2.
Prevalence of self-medication in the general population during the COVID-19 pandemic.
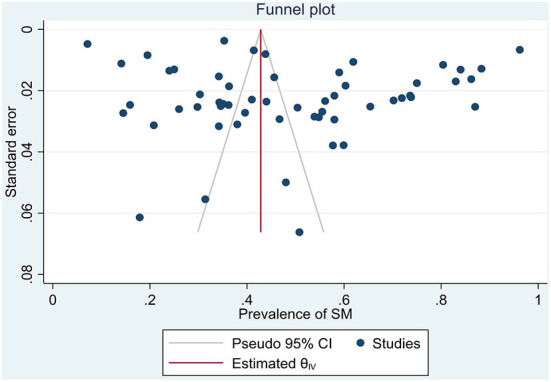
Also, the prevalence of self-medication in studies collected in 2021 (51.2%, 95% CI: 40.5–61.8) was higher than in studies collected in 2020 (48%, 95% CI: 40.3–55.7). The results of the subgroup analysis are presented in Table 3, the meta-regression results showed that the prevalence of self-medication was not related to the study sample size (p = 0.629), and the mean age of participants (p = 0.170). Publication bias was also not significant (p = 0.363) (Figure 3).
Table 3.
Prevalence of self-medication during the COVID-19 pandemic by continent, target population, time of data collection.
| Subgroup | Number of studies | Prevalence (95% CI) | Between studies | Between subgroups | ||||
|---|---|---|---|---|---|---|---|---|
| I2 | Pheterogeneity | Q | Q | Pheterogeneity | ||||
| Continent | Asia | 31 | 53 (45–61) | 99.40 | 0.001 | 11949.77 | 126.44 | 0.001 |
| Europe | 3 | 40.8 (35–46.8) | 92.06 | 0.001 | 14.43 | |||
| Africa | 11 | 41.5 (29.5–53.5) | 99.06 | 0.001 | 1160.27 | |||
| America | 10 | 47.8 (33.6–62) | 99.79 | 0.001 | 6933.03 | |||
| Target group | General population | 29 | 49 (41–57) | 99.73 | 0.001 | 18112.35 | 5.16 | 0.397 |
| Students | 11 | 54.5 (40.8–68.3) | 98.89 | 0.001 | 946.58 | |||
| Healthcare workers | 5 | 32.5 (16–49) | 99.07 | 0.001 | 520.00 | |||
| Patients with COVID-19 | 4 | 41.7 (25.5–58) | 97.72 | 0.001 | 195.87 | |||
| Others* | 6 | 53.5 (37.3–69.7) | 99.02 | 0.001 | 782.70 | |||
| Data collection time | 2020 | 31 | 48 (40.3–55.7) | 99.66 | 0.001 | 9891.97 | 23.00 | 0.891 |
| 2021 | 16 | 51.2 (40.5–61.8) | 99.34 | 0.001 | 2233.33 | |||
| Unknown | 8 | 49.7 (32.4–67) | 99.31 | 0.001 | 2061.28 | |||
*Inflammatory bowel disease patients; dental patients; pregnant and postpartum women, elderly, dermatology patients; faculty employed; and out patients.
Figure 3.
Publication bias.
Discussion
This study, which was conducted to estimate the cumulative prevalence of self-medication in the COVID-19 pandemic, showed that nearly half of the people have self-medicated. The results of a previous meta-analysis conducted on 14 relevant studies published between April 1, 2020, and March 31, 2022, showed that the pooled prevalence of self-medication was 44.9% (65). In addition to updating that study, we reported the results of 56 eligible studies by continent, target population, and time of data collection in the present study. James et al. (66) noted that people worldwide practice self-care practices, which in many cases are done through self-medication.
If self-treatment is done correctly, it can be beneficial for one's health. The WHO also recognizes correct self-medication as a type of self-medication (67). Mir et al. (48) mentioned that self-medication encourages patients to rely on themselves in making decisions for the management of minor illnesses.
The highest prevalence of self-medication was related to students. A recent meta-analysis showed that the prevalence of self-medication in students (before the COVID-19 pandemic) was 49.5% (68). The prevalence of self-medication among college students seems to have increased during this pandemic. This finding can be attributed to their higher education level compared to the general population. The lowest prevalence of self-medication was related to healthcare workers. This finding may be due to their familiarity with the consequences of self-medication. The low prevalence of self-medication in the European continent can be due to clear instructions regarding the distribution and provision of medicine and the general knowledge of the people of that region. The prevalence of self-medication was higher in studies that collected data in 2021. The reason for this finding can be the reduction of people's extreme fear of the COVID-19 virus and everyone's familiarity with this disease. False information at the beginning of the disease and the health measures applied by the governments had led to psychological distress and significant fear in the people, so in some countries, people bought and stored toilet paper, face masks and staple foods and even armed (69).
Although the high prevalence of self-medication can indicate people's self-care behavior, it can also lead to serious risks, especially for the elderly, children, pregnant women, and people with underlying diseases. Due to the fact that in the future, it is possible that other waves of the COVID-19 pandemic or other pandemics may occur, it is necessary to prepare and present instructions and guidelines to separate safe self-medication from high-risk ones so that the risks of self-medication are minimized.
Limitations
One of the limitations of this study was that gray texts were not included in the analysis. The reason was the lack of access to the databases that provided these documents. Another limitation of this study was that in this systematic review and meta-analysis, only articles published in English were analyzed.
Conclusion
This study showed that self-medication during the COVID-19 pandemic was highly prevalent, so nearly half of the people had self-medicated at this time. The prevalence of self-medication in students was higher than in other groups. Also, with increasing age, the prevalence of self-medication had an almost downward trend. Considering the consequences of self-medication, it seems necessary to educate the general population through the media to increase drug information and improve their health literacy. Awareness of drug risks can reduce the practice of self-medication now and even in pandemics that may occur in the future.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
GK and FT contributed to designing and performing this systematic review. RG and GK checked the data and conducted data analyses. SA and ML contributed to writing and editing the paper. All authors read and confirmed the final version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.1041695/full#supplementary-material
References
- 1.Sadio AJ, Gbeasor-Komlanvi FA, Konu RY, Bakoubayi AW, Tchankoni MK, Bitty-Anderson AM, et al. Assessment of self-medication practices in the context of the COVID-19 outbreak in Togo. BMC Public Health. (2021) 21:58. 10.1186/s12889-020-10145-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ray I, Bardhan M, Hasan MM, Sahito AM, Khan E, Patel S, et al. Over-the-counter drugs and self-medication: a worldwide paranoia and a troublesome situation in India during the COVID-19 pandemic. Ann Med Surg. (2022) 78:103797. 10.1016/j.amsu.2022.103797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Acharya A, Shrestha MV, Karki D. Self-medication among Medical Students and Staffs of a Tertiary Care Centre during COVID-19 pandemic: a descriptive cross-sectional study. J Nepal Med Assoc. (2022) 60:59–62. 10.31729/jnma.7247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adenike ME, Ibunkunoluwa B, Bede CA, Akinnawo OE. Knowledge of COVID-19 and preventive measures on self-medication practices among Nigerian undergraduates. Cogent Arts Humanities. (2022) 9:2049480. 10.1080/23311983.2022.2049480 [DOI] [Google Scholar]
- 5.Adebisi YA, Oladunjoye IO, Tajudeen YA, Lucero-Prisno III DE. Self-medication with antibiotics among seafarers: a public health issue. Int Maritime Health. (2021) 72:241–2. 10.5603/IMH.2021.0045 [DOI] [PubMed] [Google Scholar]
- 6.Aitafo JE, Wonodi W, Briggs DC, West BA. Self-Medication among health workers during the COVID-19 pandemic in southern Nigeria: knowledge, patterns, practice, and associated factors. Int J Health Sci Res. (2022) 12:1–14. 10.52403/ijhsr.20220223 [DOI] [Google Scholar]
- 7.Alsaad HA, Almahdi JS, Alsalameen NA, Alomar FA, Islam MA. Assessment of self-medication practice and the potential to use a mobile app to ensure safe and effective self-medication among the public in Saudi Arabia. Saudi Pharm J. (2022) 30:927–33. 10.1016/j.jsps.2022.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayalew MB. Self-medication practice in Ethiopia: a systematic review. Patient Prefer Adherence. (2017) 11:401. 10.2147/PPA.S131496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noone J, Blanchette CM. The value of self-medication: summary of existing evidence. J Med Econ. (2018) 21:201–11. 10.1080/13696998.2017.1390473 [DOI] [PubMed] [Google Scholar]
- 10.Bown D, Kisuule G, Ogasawara H, Siregar C, Williams G. WHO guidelines for the regulatory assessment of medicinal products for use in selfmedication: general information. WHO Drug Inf . (2000) 14:18–26. [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Internal Med. (2009) 151:264–9. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 12.Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS ONE. (2016) 11:e0147601. 10.1371/journal.pone.0147601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kashyap S, Budihal BR. Self medication practices for the prevention and treatment of COVID-19 among undergraduate medical students. J Asian Med Students' Assoc. (2022). Available online at: https://www.jamsa.amsa-international.org/index.php/main/article/view/401 (accessed October 21, 2022).
- 14.Malik NS, Umair M, Malik IS. Self medication among dental patients visiting Tertiary Care Hospital, during COVID-19. JPDA. (2021) 31:43–8. 10.25301/JPDA.311.4333132723 [DOI] [Google Scholar]
- 15.Likhar S, Jain K, Kot LS. Self-medication practice and health-seeking behavior among medical students during COVID 19 pandemic: a cross-sectional study. MGM J Med Sci. (2022) 9:189. 10.4103/mgmj.mgmj_107_21 [DOI] [Google Scholar]
- 16.Namvar MA, Mansori K, Gerayeli M. Self-medication for oral health problems in COVID-19 outbreak: prevalence and associated factors. Odovtos Int J Dental Sci. (2022) 516–24. 10.15517/IJDS.2022.50876 [DOI] [Google Scholar]
- 17.Barakat AM, Mohasseb MM. Self-medication with antibiotics based on the theory of planned behavior among an Egyptian rural population during the era of COVID-19 pandemic. Egypt J Commun Med. (2022) 41:1–10. 10.21608/ejcm.2022.139501.1220 [DOI] [Google Scholar]
- 18.Yasmin F, Asghar MS, Naeem U, Najeeb H, Nauman H, Ahsan MN, et al. Self-medication practices in medical students during the COVID-19 pandemic: a cross-sectional analysis. Front Public Health. (2022) 10:803937. 10.3389/fpubh.2022.803937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alateeq D, Alsubaie MA, Alsafi FA, Alsulaiman SH, Korayem GB. The use of dietary supplements for mental health among the Saudi population: a cross-sectional survey. Saudi Pharm J. (2022) 30:742–9. 10.1016/j.jsps.2022.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amuzie CI, Kalu KU, Izuka M, Nwamoh UN, Emma-Ukaegbu U, Odini F, et al. Prevalence, pattern and predictors of self-medication for COVID-19 among residents in Umuahia, Abia State, Southeast Nigeria: policy and public health implications. J Pharm Policy Prac. (2022) 15:34–43. 10.1186/s40545-022-00429-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bello I, Akinnawo E, Akpunne B, Mopa-Egbunu A. Knowledge of COVID-19 and preventive measures on self-medication practices among Nigerian undergraduates. Cogent Arts Humanities. (2022) 9:2049480. [Google Scholar]
- 22.Gaviria-Mendoza A, Mejia-Mazo DA, Duarte-Blandon C, Castrillon-Spitia JD, Machado-Duque ME, Valladales-Restrepo LF, et al. Self-medication and the 'infodemic' during mandatory preventive isolation due to the COVID-19 pandemic. Therapeutic Adv Drug Safety. (2022) 13. 10.1177/20420986221072376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dehghan M, Ghanbari A, Heidari FG, Shahrbabaki PM, Zakeri MA. Use of complementary and alternative medicine in general population during COVID-19 outbreak: a survey in Iran. J Integrative Med. (2022) 20:45–51. 10.1016/j.joim.2021.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gerbier E, Favre G, Tauqeer F, Winterfeld U, Stojanov M, Oliver A, et al. Self-reported medication use among pregnant and postpartum women during the third wave of the COVID-19 pandemic: a European multinational cross-sectional study. Int J Environ Res Public Health. (2022) 19:5335–42. 10.3390/ijerph19095335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gonzalez-Gonzalez MDR, Yeverino-Gutierrez ML, Ramirez-Estrada K, Gonzalez-Santiago O. Self-medication for prevention of COVID-19 in university students of the northeast of Mexico. Interciencia. (2022) 47:240–3. [Google Scholar]
- 26.Gupta S, Chakraborty A. Pattern and practice of self medication among adults in an urban community of West Bengal. J Fam Med Primary Care. (2022) 11:1858–62. 10.4103/jfmpc.jfmpc_1823_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heemskerk M, Le Tourneau FM, Hiwat H, Cairo H, Pratley P. In a life full of risks, COVID-19 makes little difference. Responses to COVID-19 among mobile migrants in gold mining areas in Suriname and French Guiana. Soc Sci Med. (2022) 296:114747. 10.1016/j.socscimed.2022.114747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joseph N, Colaco SM, Fernandes RV, Krishna SG, Veetil SI. Perception and self-medication practices among the general population during the ongoing COVID-19 pandemic in Mangalore, India. Curr Drug Safety. (2022). 10.2174/1574886317666220513101349. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 29.Kumari D, Lahiri B, Das A, Mailankote S, Mishra D, Mounika A. Assessment of self-medication practices among nonteaching faculty in a private dental college-a cross-sectional study. J Pharm Bioallied Sci. (2022) 14:S577–80. 10.4103/jpbs.jpbs_796_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahmoudi H. Assessment of knowledge, attitudes, and practice regarding antibiotic self-treatment use among COVID-19 patients. GMS Hygiene Infect Control. (2022) 17:1–5. 10.3205/dgkh000415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Odis A. Attitude, knowledge and use of self-medication with antibiotics by outpatients of Gbagada General Hospital Gbagada Lagos. Int J Infect Dis. (2022) 116:S16. 10.1016/j.ijid.2021.12.039 [DOI] [Google Scholar]
- 32.Okoye OC, Adejumo OA, Opadeyi AO, Madubuko CR, Ntaji M, Okonkwo KC, et al. Self medication practices and its determinants in health care professionals during the coronavirus disease-2019 pandemic: cross-sectional study. Int J Clin Pharmacy. (2022) 44:507–16. 10.1007/s11096-021-01374-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rojas-Miliano C, Galarza-Caceres DN, Zárate-Vargas AM, Araujo-Ramos G, Rosales-Guerra J, Quiñones-Laveriano DM. Characteristics and factors associated with self-medication due to COVID-19 in students of a Peruvian University. Revista Cubana de Farmacia. (2022) 55:1–10.35601942 [Google Scholar]
- 34.Toure A, Camara SC, Camara A, Conde M, Delamou A, Camara I, et al. Self-medication against COVID-19 in health workers in Conakry, Guinea. J Public Health Africa. (2022) 13:1–4. 10.4081/jphia.2022.2082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vasquez-Elera LE, Failoc-Rojas VE, Martinez-Rivera RN, Morocho-Alburqueque N, Temoche-Rivas MS, Valladares-Garrido MJ. Self-medication in hospitalized patients with COVID-19: a crosssection study in northern Peru. Germs. (2022) 12:46–53. 10.18683/germs.2022.1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zeng QL, Yu ZJ, Ji F, Li GM, Zhang GF, Xu JH, et al. Dynamic changes in liver function parameters in patients with coronavirus disease 2019: a multicentre, retrospective study. BMC Infect Dis. (2021) 21:1–15. 10.1186/s12879-021-06572-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saleem RT, Butt MH, Ahmad A, Amin M, Amir A, Ahsan A, et al. Practices and attitude of self-medication during COVID-19 pandemic in university students with interventional role of pharmacist: a regional analysis. Latin Am J Pharmacy. (2021) 40:1946–53. [Google Scholar]
- 38.Ruiz-Padilla AJ, Alonso-Castro AJ, Preciado-Puga M, Gonzalez-Nunez AI, Gonzalez-Chavez JL, Ruiz-Noa Y, et al. Use of allopathic and complementary medicine for preventing SARS-CoV-2 infection in Mexican adults: a national survey. Saudi Pharm J. (2021) 29:1056–60. 10.1016/j.jsps.2021.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mota IA, de Oliveira Sobrinho GD, Morais IPS, Dantas TF. Impact of COVID-19 on eating habits, physical activity and sleep in Brazilian healthcare professionals. Arquivos de neuro-psiquiatria. (2021) 79:429–36. 10.1590/0004-282x-anp-2020-0482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhang A, Hobman EV, De Barro P, Young A, Carter DJ, Byrne M. Self-medication with antibiotics for protection against COVID-19: the role of psychological distress, knowledge of, and experiences with antibiotics. Antibiotics. (2021) 10:1–14. 10.3390/antibiotics10030232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Heshmatifar N, Quchan ADM, Tabrizi ZM, Moayed L, Moradi S, Rastagi S, et al. Prevalence and factors related to self-medication for COVID-19 prevention in the elderly. Iran J Ageing. (2021) 16:112–27. 10.32598/sija.16.1.2983.1 [DOI] [Google Scholar]
- 42.Ainsy Goldlin TJ, Prakash M. Cyberchondria and its impact on self-medication and self care in COVID-19 pandemic - a cross sectional study. Biomed Pharmacol J. (2021) 14:2235–44. 10.13005/bpj/232232330115 [DOI] [Google Scholar]
- 43.Alonso-Castro AJ, Ruiz-Padilla AJ, Ortiz-Cortes M, Carranza E, Ramirez-Morales MA, Escutia-Gutierrez R, et al. Self-treatment and adverse reactions with herbal products for treating symptoms associated with anxiety and depression in adults from the central-western region of Mexico during the COVID-19 pandemic. J Ethnopharmacol. (2021) 272:113952. 10.1016/j.jep.2021.113952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Azhar H, Tauseef A, Usman T, Azhar Y, Ahmed M, Umer K, et al. Prevalence, attitude and knowledge of self medication during COVID-19 disease pandemic. Pakistan J Med Health Sci. (2021) 15:902–5. 10.53350/pjmhs21155902 [DOI] [Google Scholar]
- 45.Chopra D, Bhandari B, Sidhu JK, Jakhar K, Jamil F, Gupta R. Prevalence of self-reported anxiety and self-medication among upper and middle socioeconomic strata amidst COVID-19 pandemic. J Educ Health Promotion. (2021) 10:73. 10.4103/jehp.jehp_864_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.D'arqom A, Sawitri B, Nasution Z, Lazuardi R. “Anti-COVID-19” medications, supplements, and mental health status in indonesian mothers with school-age children. Int J Women's Health. (2021) 13:699–709. 10.2147/IJWH.S316417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Faqihi A, Sayed SF. Self-medication practice with analgesics (NSAIDs and acetaminophen), and antibiotics among nursing undergraduates in University College Farasan Campus Jazan University, KSA. Ann Pharmaceutiques Francaises. (2021) 79:275–85. 10.1016/j.pharma.2020.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mir S, Shakeel D, Qadri Z. Self-medication practices during COVID-19 pandemic: a cross-sectional survey. Asian J Pharm Clin Res. (2021) 14:80–2. 10.22159/ajpcr.2021.v14i10.4276133673839 [DOI] [Google Scholar]
- 49.Islam MS, Ferdous MZ, Islam US, Mosaddek AM, Potenza MN, Pardhan S. Treatment, persistent symptoms, and depression in people infected with COVID-19 in Bangladesh. Int J Environ Res Public Health. (2021) 18:1453–59. 10.3390/ijerph18041453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elayeh E, Akour A, Haddadin RN. Prevalence and predictors of self-medication drugs to prevent or treat COVID-19: experience from a Middle Eastern country. Int J Clin Prac. (2021) 75:e14860. 10.1111/ijcp.14860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Choudhary N, Lahiri K, Singh M. Increase and consequences of self-medication in dermatology during COVID-19 pandemic: an initial observation. Dermatol Ther. (2021) 34:e14696. 10.1111/dth.14696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sen Tunc E, Aksoy E, Arslan HN, Kaya Z. Evaluation of parents' knowledge, attitudes, and practices regarding self-medication for their children's dental problems during the COVID-19 pandemic: a cross-sectional survey. BMC Oral Health. (2021) 21:98. 10.1186/s12903-021-01466-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sikdar K, Anjum J, Bahar NB, Muni M, Hossain SMR, Munia AT, et al. Evaluation of sleep quality, psychological states and subsequent self-medication practice among the Bangladeshi population during COVID-19 pandemic. Clin Epidemiol Glob Health. (2021) 12:100836. 10.1016/j.cegh.2021.100836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Quispe-Canari JF, Fidel-Rosales E, Manrique D, Mascaro-Zan J, Huaman-Castillon KM, Chamorro-Espinoza SE, et al. Self-medication practices during the COVID-19 pandemic among the adult population in Peru: a cross-sectional survey. Saudi Pharm J. (2021) 29:1–11. 10.1016/j.jsps.2020.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tekeba A, Ayele Y, Negash B, Gashaw T. Extent of and factors associated with self-medication among clients visiting community pharmacies in the era of COVID-19: does it relieve the possible impact of the pandemic on the health-care system? Risk Manage Healthcare Policy. (2021) 14:4939–51. 10.2147/RMHP.S338590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tobaiqi MA, Mahrous KW, Batoot AM, Alharbi SA, Batoot AM, Alharbi AM, et al. Prevalence and association of self-medication on patient health in Medina. Med Sci. (2021) 25:2685–97. [Google Scholar]
- 57.Vinay G. Increased self-medication with steroids in inflammatory bowel disease patients during COVID-19 pandemic: time to optimize specialized telemonitoring services. Euroasian J Hepato Gastroenterol. (2021) 11:103–4. 10.5005/jp-journals-10018-1342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wegbom AI, Edet CK, Raimi O, Fagbamigbe AF, Kiri VA. Self-medication practices and associated factors in the prevention and/or treatment of COVID-19 virus: a population-based survey in Nigeria. Front Public Health. (2021) 9:606801. 10.3389/fpubh.2021.606801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Onchonga D, Omwoyo J, Nyamamba D. Assessing the prevalence of self-medication among healthcare workers before and during the 2019. SARS-CoV-2 (COVID-19) pandemic in Kenya. Saudi Pharm J. (2020) 28:1149–54. 10.1016/j.jsps.2020.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Heydargoy MH. The effect of the prevalence of COVID-19 on arbitrary use of antibiotics. Iran J Med Microbiol. (2020) 14:374–84. 10.30699/ijmm.14.4.374 [DOI] [Google Scholar]
- 61.Makowska M, Boguszewki R, Nowakowski M, Podkowińska M. Self-medication-related behaviors and Poland's COVID-19 lockdown. Int J Environ Res Public Health. (2020) 17:8344–9. 10.3390/ijerph17228344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mansuri FMA, Zalat MM, Khan AA, Alsaedi EQ, Ibrahim HM. Estimating the public response to mitigation measures and self-perceived behaviours towards the COVID-19 pandemic. J Taibah Univ Med Sci. (2020) 15:278–83. 10.1016/j.jtumed.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nasir M, Chowdhury A, Zahan T. Self-medication during COVID-19 outbreak: a cross sectional online survey in Dhaka city. Int J Basic Clin Pharmacol. (2020) 9:1325–30. 10.18203/2319-2003.ijbcp20203522 [DOI] [Google Scholar]
- 64.de los Ángeles M, Minchala-Urgilés RE, Ramírez-Coronel AA, Aguayza-Perguachi MA, Torres-Criollo LM, Romero-Sacoto LA, et al. Herbal medicine as prevention and treatment against COVID-19. Archivos Venezolanos de Farmacologia y Terapeutica. (2020) 39:948–53. [Google Scholar]
- 65.Ayosanmi OS, Alli BY, Akingbule OA, Alaga AH, Perepelkin J, Marjorie D, et al. Prevalence and correlates of self-medication practices for prevention and treatment of COVID-19: a systematic review. Antibiotics. (2022) 11:808–14. 10.3390/antibiotics11060808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med Principles Prac. (2006) 15:270–5. 10.1159/000092989 [DOI] [PubMed] [Google Scholar]
- 67.World Health Organization . The Role of the Pharmacist in Self-Care and Self-Medication: Report of the 4th WHO Consultative Group on the Role of the Pharmacist. The Hague; (1998). [Google Scholar]
- 68.Fetensa G, Tolossa T, Etafa W, Fekadu G. Prevalence and predictors of self-medication among university students in Ethiopia: a systematic review and meta-analysis. J Pharm Policy Prac. (2021) 14:1–15. 10.1186/s40545-021-00391-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Luo F, Ghanei Gheshlagh R, Dalvand S, Saedmoucheshi S, Li Q. Systematic review and meta-analysis of fear of COVID-19. Front Psychol. (2021) 12:1311. 10.3389/fpsyg.2021.661078 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.