Abstract
Background
Evidence‐based multifactorial fall prevention interventions in clinical practice have been less effective than expected. One plausible reason is that older adults' engagement in fall prevention care is suboptimal.
Methods
This was a post‐hoc analysis of 2403 older adults' engagement in a multifactorial fall prevention intervention in the Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) pragmatic trial. Based on the direct clinical care level of the Patient and Family Continuum of Engagement (CE) framework, three indicators of progressively interactive engagement were assessed: (1) Consultation (receiving information), (2) Involvement (prioritizing risks), and (3) Partnership (identifying prevention actions). Drop off at each step was determined as well as predictors of engagement.
Results
The participants' engagement waned with increasingly interactive CE domains. Although all participants received information about their positive fall risk factors (consultation) and most (51%–96%) prioritized them (involvement), fewer participants (33%–55%) identified fall prevention actions (partnership) for most of their risk factors, except for strength gait or balance problems (95%). More participants (70%) identified home exercises than other actions. Finally, fall prevention actions were identified more commonly among participants who received two visits compared to one (OR = 2.33 [95% CI, 2.06–2.64]), were ≥80 years old (OR = 1.83 [95% CI, 1.51–2.23]), and had fewer fall risk factors (OR = 0.90 [95% CI, 0.83–0.99]).
Conclusions
The drop‐off in participants' engagement based on the level of their interaction with clinicians suggests that future multifactorial fall prevention interventions need to be more focused on interactive patient‐clinician partnerships that help older adults increase and maintain fall prevention actions. Our analyses suggest that more frequent contact with clinicians and more monitoring of the implementation and outcomes of Fall Prevention Care Plans could potentially improve engagement and help older adults maintain fall prevention actions.
Keywords: Fall Prevention, Older Adults, Patient Engagement, Primary Care
Key points
All STRIDE participants received information about their fall risk factors and relevant fall prevention interventions and most prioritized those risks.
Fewer than half of STRIDE participants partnered with their fall care managers and interdisciplinary team to implement actions to mitigate their identified risk factors.
Further research is needed to understand the types and dosages of engagement and health behavior change strategies that effectively and efficiently improve patient‐clinician partnerships and help older adults increase and maintain fall prevention actions.
Why does this paper matter?
The variable engagement of older adults in STRIDE underscores the need to improve strategies that promote fall‐reducing actions–beyond receiving assessment results. Our detailed description of engagement by fall risk factor, annual clinic visit, and domains in the direct care level of the Patient and Family Continuum of Engagement model can inform such efforts.
INTRODUCTION
Falls are the leading cause of injury and injury‐related deaths among older adults. 1 , 2 Clinical trials have shown that multifactorial fall prevention interventions are efficacious in reducing older adults' falls and injuries, yet their effectiveness in clinical settings has been less than expected. 3 , 4 , 5 As these interventions are complex and often require multiple new actions and sustained changes in behavior, 6 , 7 one possible reason for this translational gap is that older adults cannot or do not engage in fall prevention interventions to the extent required for effectiveness. Prior research in this field has addressed older adults' perspectives on fall prevention, 8 , 9 , 10 factors associated with prioritizing fall risk, 6 the influence of beliefs and attitudes on fall prevention actions, 11 and implementation barriers. 12 Exploring older adults' engagement in multifactorial interventions may provide insight about how to close the translational gap between evidence from efficacy trials of fall prevention interventions and their effectiveness in real‐world clinical settings.
In 2014, the Patient‐Centered Outcomes Research Institute (PCORI) and the National Institute on Aging funded a multi‐site, pragmatic, cluster‐randomized trial: Strategies to Reduce Injuries and Develop Confidence in Elders (STRIDE) 13 to compare the effectiveness of two fall prevention interventions delivered in primary care settings. The first was a multifactorial falls prevention intervention comprised of assessments for risk factors of fall‐relatedinjuries and the development of person‐centered Fall Prevention Care Plans. The second intervention was enhanced usual care that informed primary care providers when patients were at higher risk and provided links to recommended CDC STEADI resources to reduce fall risk. 14 As previously reported, 4 the most common risk factors for fall‐related injuries among intervention participants were problems with strength, gait, balance, osteoporosis or insufficient vitamin D intake, and vision impairment. Compared to enhanced usual care, the STRIDE's multifactorial intervention was associated with an 8% reduction (p = 0.25) in the primary outcome of adjudicated serious fall injuries and a 10% reduction (p = 0.004) in the secondary outcome of time to first self‐reported fall injury. 4 However, previous analyses have not investigated participants' engagement in the multifactorial intervention and each of their positive risk factors for fall‐related injuries, at each intervention visit.
Thus, we analyzed STRIDE participants' engagement in the multifactorial fall prevention intervention guided by the Patient and Family Continuum of Engagement (CE) framework, 15 direct care level. The CE progresses from patients just receiving information about their condition and benefits of treatment (consultation), to receiving encouragement to share their preferences and priorities (involvement) and co‐creating their plan of care (partnership). Thus, the objectives of this analysis were to: (1) evaluate the CE among STRIDE participants who received the multifactorial fall prevention intervention; (2) describe the types of fall prevention actions identified by STRIDE participants; and (3) identify factors that are potentially associated with participants' selection of fall prevention actions (interactive engagement), including baseline characteristics and the number of annual clinic visits they attended.
METHODS
Study design
This is a post‐hoc analysis of STRIDE participants' engagement in a longitudinal multifactorial fall prevention intervention designed to reduce injuries from falls. The full STRIDE pragmatic study protocol 13 is available at ClinicalTrials.gov: NCT02475850. In brief, STRIDE included 86 primary care clinics within 10 diverse US healthcare systems. Each primary clinic was randomized to one of two intervention arms: the multifactorial fall prevention intervention (n = 43) or enhanced usual care (n = 43). Prior reports of from STRIDE include recruitment 16 and retention strategies, 17 intervention design, 18 primary and secondary outcome results, 4 , 19 and implementation barriers. 12 This post‐hoc analysis focuses on participant engagement in the multifactorial intervention arm of STRIDE. A single central IRB approved the STRIDE protocol and amendments. Verbal consent was obtained from individual participants or their proxies/caregivers, with participant assent. 13
Conceptual framework
The organization of this analysis was guided by the CE framework, which was developed in response to evidence suggesting that patient engagement can contribute to better quality, affordability, and health. 15 In this framework, engagement is defined as interactions between patients–plus their families and care partners when appropriate–and health professionals at three levels: direct clinical care, organizational design and governance, and policymaking. STRIDE's multifactorial fall prevention intervention included strategies to help individuals with fall risks but did not include strategies to change organizational designs, governance, or policymaking. Therefore, this analysis focuses only on the direct clinical care level of the CE framework.
The direct clinical care level of CE has three domains that represent progressively interactive engagement: consultation, involvement, and partnership. 15 Consultation is unidirectional information from clinician to patient about a diagnosis, treatment options, and care plans. It was operationalized in this analysis as STRIDE participants' receipt of information about each of their risk factors for fall‐related injuries and the benefits of evidence‐based interventions. Involvement refers to clinicians asking patients about their preferences regarding treatment options and care plans. It was operationalized as STRIDE participants communicating whether they prioritized their positive risk factors. Partnership refers to patients and clinicians making shared decisions about treatment and care plans, based on individual preferences, empirical evidence, and clinical judgment. It was operationalized in this analysis as STRIDE participants co‐creating their Fall Prevention Care Plans with FCMs, as evidenced by their identification of fall prevention actions which they intended to implement or were currently implementing. Figure 1 illustrates the CE domains of progressively interactive engagement in direct clinical care.
FIGURE 1.
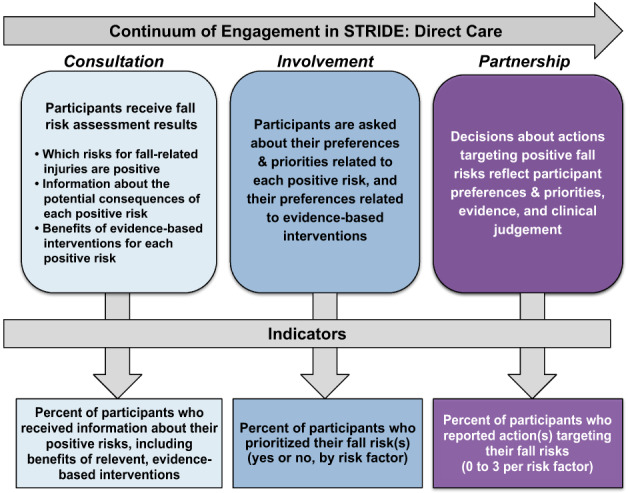
Conceptual framework for STRIDE participants' engagement in the multifactorial fall prevention intervention based on the patient and family continuum of engagement 15
Setting and participants
The STRIDE multifactorial fall prevention intervention was delivered by registered nurses trained as fall care managers (FCMs) in 43 primary care practice clinics that had no formal fall prevention programs. 13 These clinics were selected because they represent a range of rural/urban, racial/ethnic, geographic, and academic/ nonacademic diversity.
The 2403 STRIDE participants in this analysis were community‐dwelling adults who were ≥ 70 years old, received primary care at one of the 43 primary care clinics randomized to STRIDE's multifactorial fall prevention intervention, were at risk for injurious falls, 13 and received at least an initial or one of the intervention's annual clinic visits. Three hundred and ninety‐nine participants were excluded based on the last criterion. 4
Intervention
The intervention 18 was comprised of an initial clinic visit (90 min), ad‐hoc follow‐up phone calls, and two annual follow‐up clinic visits (60 min each) with FCMs and emphasized self‐management and motivational interviewing principles and practices. The initial visit and the two follow‐up annual visits included four core processes: (1) Assessment of multiple risk factors for fall‐related injuries; (2) Facilitation of conversations about each positive risk(s) and evidence‐based interventions; (3) Co‐creation of individualized Falls Prevention Care Plans, consistent with participant priorities, preferences, available resources, and evidence‐based treatment algorithms; (4) Implementation of the Fall Prevention Care Plans. When participants did not prioritize a positive risk factor, FCMs explored barriers and asked permission to continue discussing the risk factor(s) during follow‐up conversations and visits.
Follow‐up after the initial clinic visit included telephone calls and two additional annual clinic visits to facilitate the implementation of their Fall Prevention Care Plans, reassess risk factors, and revise Fall Prevention Care Plans. 18
Data collection procedures
Trained researchers in the Yale Recruitment and Assessment Center and FCMs collected data used in this analysis. Yale researchers, blinded to treatment arms, collected covariate data representing participants' baseline characteristics via telephone interviews during enrollment. 13
FCMs were trained to collect data representing the intervention processes during each clinic visit (initial, one‐year follow‐up, two‐year follow‐up), using software designed explicitly for STRIDE. 18 To improve the consistency of capturing these process data, the teams of FCMs and STRIDE intervention administrators met regularly to review procedures and problem‐solve challenges.
Outcomes
The outcomes in this analysis were indicators of participants' progressively interactive engagement in the STRIDE multifactorial fall prevention intervention. Indicators of consultation included the prevalence of individual risk factor assessments (positive or negative) and, when positive, the receipt of the risk‐specific information. The indicator of involvement was participant prioritization of each positive risk factor (yes or no). Indicators of partnership were the number and type of fall prevention actions participants identified in their Fall Prevention Care Plan for each positive and prioritized fall risk factor. Two to five prevention action types were defined for each fall risk factor were consistent with the evidence‐based STRIDE intervention algorithms and common participant‐initiated adaptations. In addition, we categorized each action as requiring personal health behavior change versus additional visits with other providers (specialists, primary care providers, physical therapists, occupational therapists).
Baseline variables
Baseline variables included baseline demographic and health characteristics. Demographic variables included age at the time of enrollment, sex (female or male), race (Black, White, or other), ethnicity (Latino/Hispanic or not Latino/Hispanic), highest formal education attained (categorized into five ordinal levels), financial difficulty (categorized into not at all/not very or somewhat/very/completely) and living situation (alone or not alone). The health variable included the number of chronic conditions, including dementia.
Data analyses
All analyses were conducted using SAS/STAT version 14.3. Summary statistics included means, standard deviations, ranges for continuous variables, and counts/percent for categorical variables. We used mixed logistic regression to identify change in fall prevention actions across annual visits and whether baseline characteristics predicted fall prevention actions. Both sets of models included two levels of random intercepts, one to account for multiple observations per participant and one to account for the nesting of participants within practices. We also adjusted for the healthcare system in both models. The first model addressed whether the odds of participants' identification of a fall prevention action, given a positive risk factor, changed with more than one annual clinic visit and whether these and risk factors interacted. The second model addressed whether baseline variables predicted the odds of participants identifying at least one risk‐specific action to prevent falls over the intervention time frame, given the presence of a risk factor. The baseline characteristics in these models included age (80+ y vs. 70–79 y), sex, fear of falling, any fracture since age 50, multi‐morbidity (having 2 or more of the 11 measured chronic conditions), number of risk factors at baseline (1–7), living alone, and financial insecurity. We present results from the multivariate model as odds ratios with 95% confidence intervals; a sensitivity analysis using a separate set of bivariate analyses considering each baseline variable gave equivalent results.
RESULTS
The 2403 participants in this analysis were primarily women (62%) who were, on average, 80 years old, and lived with 2 chronic conditions. Among participants, 18% received one of the three clinic visits (initial, one‐year follow‐up, two‐year follow‐up), 42% received 2, and 40% received 3. Table 1 summarizes baseline characteristics and receipt of clinic visits. The following paragraphs describe participants' engagement in the intervention by CE domain.
TABLE 1.
Participant characteristics (N = 2403)
| Baseline characteristics | |
|---|---|
| Female sex, n (%) | 1488 (61.9) |
| Age, mean | 79.8 ± 5.7 |
| Race | |
| White, n (%) | 2208 (91.9) |
| Black, n (%) | 105 (4.4) |
| Other, n (%) | 90 (3.7) |
| Ethnicity | |
| Latino/Hispanic, n (%) | 152 (6.3) |
| Highest formal education | |
| High school graduate or less, n (%) | 460 (19.1) |
| Some college or equivalent, n (%) | 599 (24.9) |
| College graduate, n (%) | 489 (20.3) |
| Post‐graduate, n (%) | 832 (34.6) |
| Unknown, n (%) | 1 (0.0) |
| Living alone, n (%) | 993 (41.3) |
| Financial insecurity, n (%) | 298 (12.4) |
| Chronic conditions, mean | 2.1 ± 1.3 |
| None, n (%) | 229 (9.5) |
| One, n (%) | 631 (26.3) |
| >One, n (%) | 1543 (64.2) |
| Intervention clinic visits | |
| Received at least one intervention clinic visit, n | 2403 |
| Received Initial clinic visit, n (%) | 2392 (99.5) a |
| Received 1‐year follow‐up clinic visit, n (%) | 1886 (78.5) |
| Received 2‐year follow‐up clinic visit, n (%) | 1036 (43.1) |
| Received one annual clinic visit, n (%) | 443 (18.4) |
| Received two annual clinic visits, n (%) | 1009 (42.0) |
| Received three clinic annual visits, n (%) | 951 (39.6) |
Note: a = 11 participants received their first full intervention clinic visit after being enrolled in the study for more than 11 months, and thus were not included in the count of participants who received an “initial visit.”
Consultation
Consistent with study design, all the participants in this analysis received consultation during at least one clinic visit, including information about their positive risk factor(s) for fall‐related injuries, and about the benefits of relevant evidence‐based interventions. Overall, as shown in Table 2, between 20% and 100% of participants had positive assessments for individual fall risk factors (Table 2). Figure 2 illustrates the prevalence of each risk at each clinic visit, (consultation received), using the light gray/blue bars in panels A through G.
TABLE 2.
STRIDE participants' continuum of engagement in any clinic visit a that was integral to the multifactorial fall prevention intervention, by risk factor and CE domain
| Risk factors of fall‐related injury that were assessed at any visit (n) | Continuum of engagement | |||
|---|---|---|---|---|
| Consultation (positive assessment and receipt of information/assessment received) | Involvement (prioritized risk/positive assessment) | Partnership (identified at least one action for risk/positive risk assessment and prioritized risk) | ||
| Reduced strength, gait, or balance (n) | 2354 | 100% | 95.7% | 95.4% |
| Fall‐risk inducing drugs (n) | 2402 | 34.1% | 50.5% | 33.3% |
| Postural hypotension (n) | 2331 | 20.2% | 78.7% | 48.9% |
| Vision problems (n) | 2399 | 87.0% | 84.1% | 31.7% |
| Osteoporosis/ Insufficient vit D (n) | 2402 | 96.6% | 81.3% | 39.1% |
| Home/environmental hazards (n) | 2400 | 28.3% | 60.3% | 54.9% |
| Feet or footwear problems (n) | 2375 | 62.2% | 77.2% | 35.1% |
Any clinic visit = initial visit, one‐year follow‐up visit, or two‐year follow‐up visit.
FIGURE 2.
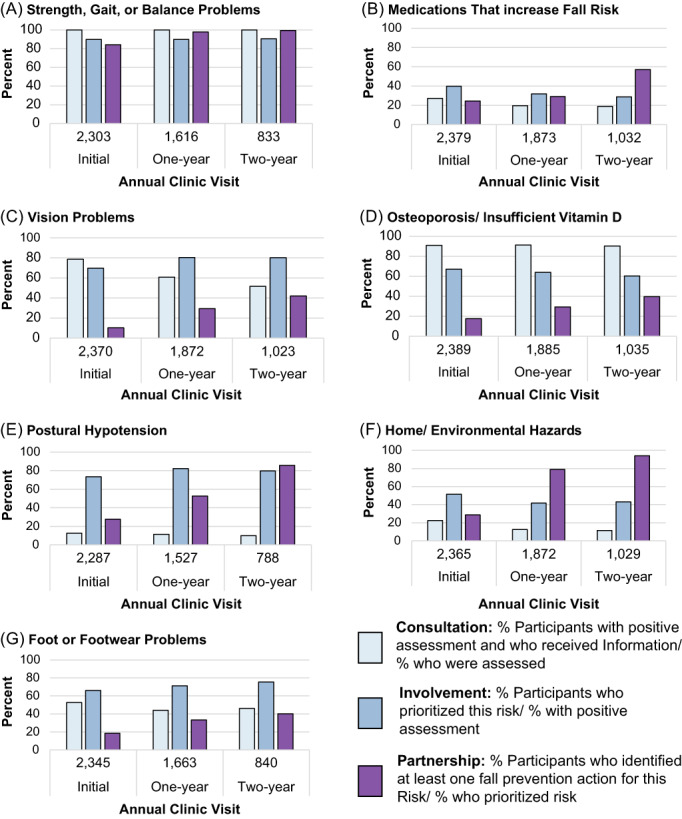
STRIDE participants' engagement in the intervention, by fall risk factor, annual clinic visit, and CE domains within direct care: Consultation, involvement, partnership. CE, patient and family continuum of engagement framework
Involvement
Involvement, indicated by participants' prioritization at any clinic visit, exceeded 75% for most positive risk factors: the exceptions fall risk‐increasings drugs (51%) and home/ environmental hazards (60%) (Table 2). Figure 2 illustrates participant involvement, by positive risk factor and clinic visit using the medium blue bars in panels A through G.
Partnership
Among participants who prioritized their fall risk factors, fewer than 50% were interactively engaged in partnership for most risk factors, indicated by their identification of at least one fall prevention action during any clinic visit (See Table 2). The exceptions were that 95% and 55% of participants identified at least one action for strength, gait, and balance problems, and home/environmental hazards, respectively. Figure 2 illustrates participant partnership in the Fall Prevention Care Plan as the purple bars in panels A through G.
The number and percent of participants who identified distinct fall prevention actions, by risk factor, by clinic visit (initial, one‐year follow‐up, two‐year follow‐up) and at any visit (overall) are detailed in Table 3. Of the 23 actions, we categorized 7 as requiring health behavior change (Table 3, shaded rows) and 16 as requiring additional visits with other healthcare providers (Table 3, non‐shaded rows). The most frequently identified health behavior change was home exercise for strength, gait, or balance problems, with 70% of participants identifying it during any of their clinic visits. Physical therapy targeting the risk of strength, gait, or balance problems was the most frequently identified action categorized as additional visits with other providers, with 40% identifying it during any of their annual visits.
TABLE 3.
Summary of fall prevention actions identified by STRIDE intervention participants, by risk factor, and annual visit
| Fall injury risk factors | Fall prevention actions n = number who identified action; % = number who identified action/number assessed as having the fall risk factor | Clinic visits | |||
|---|---|---|---|---|---|
| Initial | One‐year follow‐up | Two‐year follow‐up | Overall‐any visit | ||
| Strength, gait, or balance problems | Home exercise n (%) | 1009 (43.8) | 988 (61.1) | 507 (60.9) | 1649 (70.1) |
| Community‐based exercise n (%) | 756 (32.8) | 437 (27.0) | 204 (24.5) | 1023 (43.5) | |
| Physical Therapy n (%) | 604 (26.2) | 332 (20.5) | 165 (19.8) | 941 (40.0) | |
| Other (e.g., yoga, personal trainer) n (%) | 394 (17.1) | 521 (32.2) | 322 (38.7) | 879 (37.3) | |
| Fall‐risk inducing drugs | Visit with PCP for med review n (%) | 29 (4.5) | 24 (6.5) | 29 (14.9) | 89 (10.9) |
| Visit with pharmacist n (%) | 21 (3.2) | 9 (2.4) | 4 (2.1) | 35 (4.3) | |
| Allow Site Clinical Director to review meds n (%) | 14 (2.2) | 2 (0.5) | 0 (0.0) | 16 (2.0) | |
| Postural hypotension | Behavior changes to reduce PH | 55 (19.0) | 69 (39.4) | 47 (59.5) | 164 (34.9) |
| Visit with PCP for postural hypotension management n (%) | 47 (16.2) | 55 (31.4) | 42 (53.2) | 142 (30.2) | |
| Recheck BP in 2 weeks n (%) | 16 (5.5) | 18 (10.3) | 10 (12.7) | 45 (9.6) | |
| Vision problems | Establish annual Eye Doctor visits n (%) | 70 (3.8) | 197 (17.3) | 134 (25.3) | 404 (19.4) |
| Visit eye doctor about a specific problem (e.g., cataracts) n (%) | 66 (3.5) | 84 (7.4) | 49 (9.3) | 194 (9.3) | |
| Receive a home safety assessment n (%) | 2 (0.1) | 1 (0.1) | 0 (0.0) | 4 (0.2) | |
| Osteoporosis/insufficient Vitamin D | Visit with PCP for evaluation and treatment of OP | 149 (6.9) | 173 (10.1) | 153 (16.4) | 452 (19.5) |
| Start dietary supplement n (%) | 149 (6.9) | 175 (10.2) | 94 (10.1) | 381 (16.4) | |
| Stop treatment temporarily n (%) | 2 (0.1) | 7 (0.4) | 3 (0.3) | 13 (0.6) | |
| Home/environmental hazards | Self‐led home safety changes n (%) | 71 (13.4) | 72 (30.4) | 45 (38.1) | 206 (30.3) |
| Receive a home safety assessment n (%) | 8 (1.5) | 9 (3.8) | 3 (2.5) | 22 (3.2) | |
| Feet or footwear problems | Visit with podiatrist n (%) | 72 (5.8) | 87 (11.9) | 52 (13.4) | 199 (13.5) |
| Identify safer footwear n (%) | 66 (5.4) | 57 (7.8) | 47 (12.1) | 167 (11.3) | |
| Visit with PCP for foot evaluation and treatment n (%) | 14 (1.1) | 25 (3.4) | 10 (2.6) | 53 (3.6) | |
| Visit with orthotist n (%) | 11 (0.9) | 20 (2.7) | 12 (3.1) | 42 (2.8) | |
| Physical Therapy n (%) | 3 (0.2) | 9 (1.2) | 0 (0.0) | 11 (0.7) | |
Note: Fall prevention actions = Participants' fall prevention actions; Shaded actions = Actions representing participant identified health behavior change, Non‐shaded actions = Actions representing participant and or electronic health record identified additional visits with other providers, Any visit = Participant identified action at any visit: initial visit, 1‐year visit, or 2‐year. Order of risk‐specific actions is from most to least often identified.
Abbreviations: OP, osteoporosis; PCP, primary care provider; PH, postural hypotension.
The number of STRIDE intervention clinic visits, age, and number of positive fall risks at baseline were associated with participants' identification of fall prevention actions. Compared to identification of action at the initial visit, participants at the 1‐year visit had 2.3 times greater odds [95% CI, 2.06–2.64] of identifying fall prevention actions and 1.8 times greater odds [95% CI, 1.57–2.14] of identifying fall prevention actions at the two‐year follow‐up clinic visit relative to the one‐year visit.
Compared to participants who were between 70 and 79 years old at baseline, participants who were ≥ 80 had 1.8 times greater odds [95% CI, 1.51–2.23] of identifying one or more actions to reduce at least one risk factor. Participants with more than one fall risk factor (e.g., two to seven) had incrementally lower odds of identifying fall prevention actions. Each additional risk factor reduced the odds of identifying at least one fall prevention action by 0.90 [95% CI, 0.83–0.99]. For example, compared to participants with one positive fall risk factor, participants with two positive risk factors had 0.81 odds [95% CI, 0.75–0.89] of identifying one or more actions to reduce at least one fall risk factor.
DISCUSSION
This post‐hoc analysis of participants' engagement in the STRIDE multifactorial fall prevention intervention, informed by the CE framework, 15 provides detailed descriptions of engagement by CE domain, risk, and clinic visit. We note three important findings related to our objectives. First, the participants' engagement waned with increasingly interactive CE domains that required more commitment by the participant. All participants received information about their positive fall risk factors and the benefits of interventions (consultation) and most prioritized them (involvement). However, fewer than half of participants identified fall prevention actions (partnership) for all risk factors except for strength gait or balance problems and home/environmental risks. Second, more participants identified home exercise than other fall prevention actions. Finally, both immutable (advanced age and more risk factors) and mutable (more clinic visits) risk factors predicted partnership.
Prior literature addressing older adults' progressive engagement in fall prevention interventions focused on prioritization (involvement) or adherence to individual interventions (a concept related to partnership). These prior studies suggested that few older adults (10%) prioritized any of their fall risk factors, 6 which may have reflected beliefs that they were not at risk for falls. 20 , 21 The higher rates of prioritization in STRIDE might reflect the provision of detailed information about participants' fall risk factors and evidence‐based interventions, augmented with communication tools and infographics co‐developed with patient stakeholders This person‐centered approach 18 may have helped STRIDE participants understand their fall risk factors and the relevance of prevention interventions and, in turn, bolstered their involvement.
Our finding that partnership, the most interactive domain in the CE framework, was variable and low for most fall risk factors provides insight into why the intervention may have been less effective than expected and suggests opportunities for further research to improve adherence in this domain. More than consultation or involvement, results from prior engagement research shows that strategies targeting partnership led to better care processes and services within organizations. 22 Literature addressing older adults' partnership in fall prevention efforts has focused on adherence, a related concept defined variably as choosing or participating in a risk‐specific fall prevention intervention. Results from prior adherence research were congruent with our findings about partnership. For instance, in one review, between 25% and 95% of participants adhered to different intervention components over time. 23 One plausible explanation for older adults' lower‐than‐expected partnerships in and adherence to fall prevention interventions is that researchers have not investigated strategies that target some important barriers to engagement. For example, older people have described barriers such as complex social issues, limited social support, and inadequate access to resources. 9 , 10 , 21 Moreover, clinicians, patient stakeholders, and research staff in STRIDE have described interrelated barriers to developing and maintaining partnerships, such as visits occurring in busy clinics whose access to specialists and provider buy‐in were inconsistent and where staff turnover was often high. 12 However, most fall prevention interventions, including STRIDE, have not examined strategies that target social or organizational barriers to engagement, such as social support, broadening social networks, and technology‐augmented opportunities to help older adults raise concerns and partner with FCMs on the implementation, evaluation and adjustments to their Falls Prevention Care Plan. 24 , 25 This underscores the need for researchers and clinicians to investigate which social and organizational strategies foster patient‐clinician partnerships to empower different older adult populations to proactively self‐manage their fall risk. 24 , 25 , 26 , 27 , 28 , 29
STRIDE participants' frequent identification of home exercise as a fall prevention action implies they understood the fall risks associated with their balance, strength, or gait changes. It also indicates participants acknowledged evidence supporting the regular practice of home exercises, particularly balance‐challenging and leg‐strengthening, 30 to improve health outcomes. 31 , 32 However, prior research also shows that despite older adults' interest and initial uptake of home exercises, most do not maintain regular home exercises, 33 , 34 which may have been a factor influencing the trial's main results. 4 Because of the pragmatic design of the intervention, tracking (self or FCM) participants' fall‐reducing exercise was not part of the intervention protocol, further health behavior counseling opportunities may have been missed. Moreover, the primary behavior change strategy used in STRIDE was motivational interviewing. 18 Although promising for those who have ambivalence about change, 35 evidence of its efficacy and efficiency to help people increase and maintain health behaviors necessary to reduce fall risk, is still accumulating. 36 Additional research is also beginning to integrate behavior change science, such as long‐term evaluations of additional behavior change strategies and techniques. 37 , 38 , 39 Finally, much more research is needed to understand which strategies or techniques help older adults increase and maintain a regular practice of fall reducing home exercises, how they work, 40 and under what conditions. 41
Our finding that STRIDE participants who attended more than one intervention visit were more likely to identify action(s) suggests higher intervention dosages may have elicited stronger participant‐FCM partnerships. Indeed, other self‐management interventions that involve more clinician contacts, compared to fewer, have fostered trusting patient‐clinician partnerships 28 , 29 and have been associated with better effects on health behaviors and health outcomes, 42 and quality of life. 43 However, few published reports specify dose–response relationships, 44 , 45 limiting our understanding of which intervention dosages elicit minimally desired responses or maximal effects in different older adult populations. It would be expensive to provide interventions involving frequent visits to every person at risk for fall‐related injuries. Thus, future research should examine the affordability and dose–response relationships between interventions, and their component parts and outcomes such as the development of patient‐clinician partnerships, injurious falls and fall risks.
This study has limitations. As a post‐hoc analysis, data and methods are constrained by the design of the original pragmatic trial. Engagement data for the current study, initially collected for a different purpose, fit our study purpose, yet they were limited. Certain aspects of the fall risk assessments and fall prevention actions relied on self‐identified or electronic health record data captured by FCMs during the interview portion of each clinic visit. These data sources have known potential biases. 46 The efforts to mitigate these information biases in STRIDE, such as the systematic use of intervention manuals, procedures, and computerized standardized documentation forms, 47 may not have been adequate.
In sum, we found that clinician‐facilitated conversations about the results of fall risk assessments, benefits of interventions, and personal preferences helped STRIDE participants prioritize their fall risk factors. However, most participants did not partner with clinicians (FCMs and other interdisciplinary team members) to implement, evaluate, and revise their Fall Prevention Care Plans. This drop‐off in engagement suggests that future interventions need to be more focused on improving patient‐clinician partnerships and helping patients increase and maintain fall prevention actions that target their prioritized fall risks. Our study suggests that more frequent contacts with the clinicians, and greater feedback and monitoring of the implementation and outcomes of Fall Prevention Care Plans are potential strategies to sustain patient engagement and reduce the risk of waning of intervention dose and effectiveness.
AUTHOR CONTRIBUTIONS
All authors were involved in the study concept, design, analysis, interpretation of data, and manuscript preparation.
FUNDING INFORMATION
Supported by the Patient‐Centered Outcomes Research Institute and the National Institute on Aging of the National Institutes of Health (NIH) through a cooperative agreement (5U01AG048270) between the National Institute on Aging and Brigham and Women's Hospital. Dr. McMahon was also supported by grants (KL2TR000113 and UL1TR000114) from the University of Minnesota Clinical and Translational Science Institute, funded by the National Center for Advancing Translational Sciences (NCATS), a component of the NIH. Drs. Greene and Peduzzi were also supported by a CTSA grant (UL1TR000142) from NCATS. Dr. Gill was also supported by the Yale Claude D. Pepper Older Americans Independence Center (P30AG021342). Dr. Bhasin was supported in part by the Boston Claude D. Pepper Older Americans Independence Center (P30AG013679). This paper has not been presented.
CONFLICT OF INTEREST
The authors declare that there is no conflict of interest.
SPONSOR'S ROLE
The sponsors had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the paper.
ACKNOWLEDGMENTS
The authors thank the STRIDE study participants for engaging with fall prevention assessments and interventions. We also thank the nurses who worked as Falls Care Managers for leading the clinic visits and clinical team collaborations.
McMahon SK, Greene EJ, Latham N, et al. Engagement of older adults in STRIDE's multifactorial fall injury prevention intervention. J Am Geriatr Soc. 2022;70(11):3116‐3126. doi: 10.1111/jgs.17983
Funding information Boston Claude D. Pepper Older Americans Independence Center, Grant/Award Number: P30AG013679; National Institute on Aging, Grant/Award Number: 501AG048270; Patient‐Centered Outcomes Research Institute, Grant/Award Number: 5U01AG048270; University of Minnesota CTSI, National Center for Advancing Translational Sciences, Grant/Award Numbers: KL2TR000113, Ul1TR000114; Yale Claude D. Pepper Older Americans Independence Center, Grant/Award Number: P30AG021341; Yale CTSA, National Center of Advancing Translational Sciences, Grant/Award Number: UL1TR000142
REFERENCES
- 1. Drew JAR, Xu D. Trends in fatal and nonfatal injuries among older Americans, 2004–2017. Am J Prev Med. 2020;59(1):3‐11. doi: 10.1016/j.amepre.2020.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moreland B, Kakara R, Henry A. Trends in nonfatal falls and fall‐related injuries among adults aged ≥65 years — United States, 2012–2018. MMWR Morb Mortal Wkly Rep. 2020;69(27):875‐881. doi: 10.15585/mmwr.mm6927a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hopewell S, Adedire O, Copsey BJ, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018;2018(7):CD012221. doi: 10.1002/14651858.CD012221.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bhasin S, Gill TM, Reuben DB, et al. A randomized trial of a multifactorial strategy to prevent serious fall injuries. N Engl J Med. 2020;383(2):129‐140. doi: 10.1056/nejmoa2002183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lamb SE, Bruce J, Hossain A, et al. Screening and intervention to prevent falls and fractures in older people. N Engl J Med. 2020;383(19):1848‐1859. doi: 10.1056/nejmoa2001500 [DOI] [PubMed] [Google Scholar]
- 6. Jansen S, Schoe J, van Rijn M, et al. Factors associated with recognition and prioritization for falling, and the effect on fall incidence in community dwelling older adults. BMC Geriatr. 2015;15(1):169. doi: 10.1186/s12877-015-0165-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wilson K, Senay I, Durantini M, et al. When it comes to lifestyle recommendations, more is sometimes less: a meta‐analysis of theoretical assumptions underlying the effectiveness of interventions promoting multiple behavior domain change. Psychol Bull. 2015;141(2):474‐509. doi: 10.1037/a0038295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Montero‐Odasso M, van der Velde N, Alexander NB, et al. New horizons in falls prevention and management for older adults: a global initiative. Age Ageing. 2021;1(9):1‐9. doi: 10.1093/ageing/afab076 [DOI] [PubMed] [Google Scholar]
- 9. Naseri C, McPhail SM, Haines TP, et al. Perspectives of older adults regarding barriers and enablers to engaging in fall prevention activities after hospital discharge. Health Soc Care Community. 2020;28(5):1710‐1722. doi: 10.1111/hsc.12996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McMahon S, Talley KM, Wyman JF. Older people's perspectives on fall risk and fall prevention programs: a literature review. Int J Older People Nursing. 2011;6(4):289‐298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stevens JA, Sleet DA, Rubenstein LZ. The influence of older adults' beliefs and attitudes on adopting fall prevention behaviors. Am J Lifestyle Med. 2018;12(4):324‐330. doi: 10.1177/1559827616687263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reckrey JM, Gazarian P, Reuben DB, et al. Barriers to implementation of STRIDE, a national study to prevent fall‐related injuries. J Am Geriatr Soc. 2021;69(5):1334‐1342. doi: 10.1111/JGS.17056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bhasin S, Gill TM, Reuben DB, et al. Strategies to reduce injuries and develop confidence in elders (STRIDE): a cluster‐randomized pragmatic trial of a multifactorial fall injury prevention strategy: design and methods. J Gerontol Series A. 2018;73(8):1053‐1061. doi: 10.1093/gerona/glx190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Important Facts about Falls | Home and Recreational Safety | CDC Injury Center. Accessed June 9, 2020. https://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html
- 15. Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff. 2013;32(2):223‐231. doi: 10.1377/hlthaff.2012.1133 [DOI] [PubMed] [Google Scholar]
- 16. Gill TM, McGloin JM, Latham NK, et al. Screening, recruitment, and baseline characteristics for the strategies to reduce injuries and develop confidence in elders (STRIDE) study. J Gerontol Series A Biol Sci Med Sci. 2018;73(11):1495‐1501. doi: 10.1093/GERONA/GLY076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gill TM, McGloin JM, Shelton A, et al. Optimizing retention in a pragmatic trial of community‐living older persons: the STRIDE study. J Am Geriatr Soc. 2020;68(6):1242‐1249. doi: 10.1111/jgs.16356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Reuben D, Gazarian P, Latham N, et al. The strategies to reduce injuries and develop confidence in elders intervention: falls risk factor assessment and management, patient engagement, and nurse co‐management. J Am Geriatr Soc. 2017;65(12):2733‐2739. doi: 10.1111/jgs.15121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gill TM, Bhasin S, Reuben DB, et al. Effect of a multifactorial fall injury prevention intervention on patient well‐being: the STRIDE study. J Am Geriatr Soc. 2021;69(1):173‐179. doi: 10.1111/jgs.16854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91‐111. doi: 10.1146/annurev.clinpsy.1.102803.143833 [DOI] [PubMed] [Google Scholar]
- 21. Haines TP, Day L, Hill KD, Clemson L, Finch C. “Better for others than for me”: a belief that should shape our efforts to promote participation in falls prevention strategies. Arch Gerontol Geriatr. 2014;59(1):136‐144. doi: 10.1016/j.archger.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 22. Morris RL, Hill KD, Ackerman IN, et al. A mixed methods process evaluation of a person‐centred falls prevention program. BMC Health Serv Res. 2019;19(1):1‐15. doi: 10.1186/S12913-019-4614-Z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bombard Y, Baker GR, Orlando E, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1):1‐22. doi: 10.1186/s13012-018-0784-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nyman SR, Victor CR, Nyman SR, Victor CR. Older people's participation in and engagement with falls prevention interventions in community settings: an augment to the Cochrane systematic review. Age Ageing. 2012;41(1):16‐23. doi: 10.1093/ageing/afr103 [DOI] [PubMed] [Google Scholar]
- 25. Dykes PC, Rozenblum R, Dalal A, et al. Prospective evaluation of a multifaceted intervention to improve outcomes in intensive care: the promoting respect and ongoing safety through patient engagement communication and technology study. Crit Care Med. 2017;45(8):e806‐e813. doi: 10.1097/CCM.0000000000002449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Newman B, Joseph K, Chauhan A, et al. Do patient engagement interventions work for all patients? A systematic review and realist synthesis of interventions to enhance patient safety. Health Expect. 2021;24(6):1905‐1923. doi: 10.1111/hex.13343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ekstedt M, Børøsund E, Svenningsen IK, Ruland C. Reducing errors through a web‐based self‐management support system. Nurs Informat. 2014;201:328‐334. doi: 10.3233/978-1-61499-415-2-328 [DOI] [PubMed] [Google Scholar]
- 28. Carpenter C, Malone M. Avoiding therapeutic nihilism from complex geriatric intervention “negative” trials: STRIDE lessons. J Am Geriatr Soc. 2020;68(12):2752‐2756. doi: 10.1111/jgs.16887 [DOI] [PubMed] [Google Scholar]
- 29. Sefcik JS, Petrovsky D, Streur M, et al. “In our corner”: a qualitative descriptive study of patient engagement in a community‐based care coordination program. Clin Nurs Res. 2018;27(3):258‐277. doi: 10.1177/1054773816685746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Peart A, Barton C, Lewis V, Russell G. A state‐of‐the‐art review of the experience of care coordination interventions for people living with multimorbidity. J Clin Nurs. 2020;29:1445‐1456. doi: 10.1111/jocn.15206 [DOI] [PubMed] [Google Scholar]
- 31. King AC, Whitt‐Glover MC, Marquez DX, et al. Physical activity promotion: highlights from the 2018 physical activity guidelines advisory committee systematic review. Med Sci Sports Exerc. 2019;51(6):1340‐1353. doi: 10.1249/MSS.0000000000001945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shubert TE, Goto L, Smith ML, Ory MG, Jiang L. Otago exercise program in the United States: comparison of 2 implementation models. Phys Ther. 2017;97(2):187‐197. doi: 10.2522/ptj.20160236 [DOI] [PubMed] [Google Scholar]
- 33. Martins AC, Santos C, Silva C, Baltazar D, Moreira J, Tavares N. Does modified Otago exercise program improve balance in older people? Syst Rev Prevent Med Rep. 2018;11:231‐239. doi: 10.1016/J.PMEDR.2018.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bates A, Furber S, Sherrington C, et al. Effectiveness of workshops to teach a home‐based exercise program (BEST at home) for preventing falls in community‐dwelling people aged 65 years and over: a pragmatic randomised controlled trial. BMC Geriatr. 2022;22(1):1‐13. doi: 10.1186/s12877-022-03050-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hill KD, Hunter SW, Batchelor FA, Cavalheri V, Burton E. Individualized home‐based exercise programs for older people to reduce falls and improve physical performance: a systematic review and meta‐analysis. Maturitas. 2015;82:72‐84. doi: 10.1016/j.maturitas.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 36. Kiyoshi‐Teo H, Northup‐Snyder K, Cohen DJ, et al. Feasibility of motivational interviewing to engage older inpatients in fall prevention: a pilot randomized controlled trial. J Gerontol Nurs. 2019;45(9):19‐29. doi: 10.3928/00989134-20190813-03 [DOI] [PubMed] [Google Scholar]
- 37. Arkkukangas M, Söderlund A, Eriksson S, Johansson AC. One‐year adherence to the Otago exercise program with or without motivational interviewing in community‐dwelling older adults. J Aging Phys Act. 2018;26(3):390‐395. doi: 10.1123/JAPA.2017-0009 [DOI] [PubMed] [Google Scholar]
- 38. Arkkukangas M, Söderlund A, Eriksson S, Johansson AC. Fall preventive exercise with or without behavior change support for community‐dwelling older adults: a randomized controlled trial with short‐term follow‐up. J Geriatr Phys Ther. 2019;42(1):9‐17. doi: 10.1519/JPT.0000000000000129 [DOI] [PubMed] [Google Scholar]
- 39. Fleig L, McAllister MM, Chen P, et al. Health behaviour change theory meets falls prevention: feasibility of a habit‐based balance and strength exercise intervention for older adults. Psychol Sport Exerc. 2016;22:114‐122. doi: 10.1016/j.psychsport.2015.07.002 [DOI] [Google Scholar]
- 40. McMahon SK, Lewis B, Oakes JM, Wyman JF, Guan W, Rothman AJ. Assessing the effects of interpersonal and intrapersonal behavior change strategies on physical activity in older adults: a factorial experiment. Ann Behav Med. 2017;51(3):376‐390. doi: 10.1007/s12160-016-9863-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hunter C, Onken L, Clark D, et al. The NIH science of behavior change program: transforming the science through a focus on mechanisms of change. Behav Res Ther. 2017;101:3‐11. doi: 10.1016/j.brat.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rothman AJ, Sheeran P. The operating conditions framework: integrating mechanisms and moderators in health behavior interventions. Health Psychol. 2021;40(12):845‐857. doi: 10.1037/hea0001026 [DOI] [PubMed] [Google Scholar]
- 43. O'Connor EA, Evans CV, Rushkin MC, Redmond N, Lin JS. Behavioral counseling to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: updated evidence report and systematic review for the US preventive services task force. JAMA. 2020;324(20):2076‐2094. doi: 10.1001/JAMA.2020.17108 [DOI] [PubMed] [Google Scholar]
- 44. Wells R, Dionne‐Odom JN, Azuero A, et al. Examining adherence and dose effect of an early palliative care intervention for advanced heart failure patients. J Pain Symptom Manag. 2021;62(3):471‐481. doi: 10.1016/J.JPAINSYMMAN.2021.01.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Conn VS, Chan KC. How much, how often, how long? Addressing dosage in intervention studies. West J Nurs Res. 2016;38(1):3‐4. doi: 10.1177/0193945915605067 [DOI] [PubMed] [Google Scholar]
- 46. Rowbotham S, Conte K, Hawe P. Variation in the operationalisation of dose in implementation of health promotion interventions: insights and recommendations from a scoping review. Implement Sci. 2019;14(1):1‐12. doi: 10.1186/s13012-019-0899-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211‐217. doi: 10.2147/JMDH.S104807 [DOI] [PMC free article] [PubMed] [Google Scholar]


