The carbapenem-resistant Acinetobacter baumannii (CRAb) bacterium poses a major public health problem, as it is a widespread pathogen and a frequent cause of nosocomial outbreaks (1– 3). Further resistance of CRAb to other classes of substances creates additional impairment in combating infections.
Between calendar week (CW) 31/2021 and CW 36/2021, several parallel outbreaks in Rhineland-Palatinate (RP), Baden-Wurttemberg (BW), and Hesse (HE) of CRAb with additional resistance, for instance to aminoglycosides and fluoroquinolones, were reported to the Robert Koch Institute. In order to clarify the suspicion of a supra-regional connection between the outbreaks and to prevent further infections, the outbreak was investigated in a cooperative manner by the National Reference Center (NRC) for multidrug-resistant gram-negative bacteria, the employees of the state health authorities as well as the responsible health authorities, and the respective hospital hygiene departments.
Acknowledgments
Translated from the original German by Veronica A. Raker, PhD.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
Methods
Data were collected in the affected institutions. In addition, the outbreak isolates were sent to the NRZ for carbapenemase determination and for relationship analysis using pulsed-field gel electrophoresis (PFGE) and sequencing. A case was defined as a patient with detection of a CRAb belonging to one of the outbreak strains. Investigations took place within the framework of §25 of the Infection Protection Act. An ethics vote was therefore not necessary.
Results
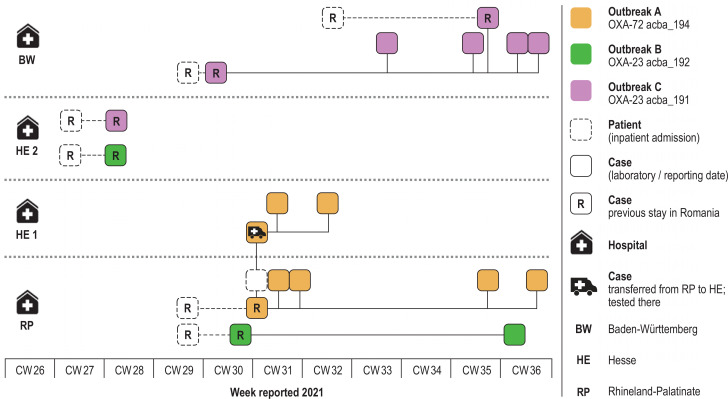
In RP, two CRAb outbreaks of different strains occurred simultaneously in an intensive care unit (ICU). Outbreak A (figure) comprised five cases (of patients from 43 to 79 years old) in which CRAb with the carbapenemase OXA-72 pulse type acba_194 was detected in various sample materials. Another patient, who was in the same ward at the same time, also tested positive for CRAb OXA-72 after being transferred to a clinic in Hesse (HE 1). There were two further cases.
FIGURE.
Spatial-temporal representation of the outbreak events of carbapenem-resistant Acinetobacter baumannii that spanned German federal states
In parallel, CRAb OXA-23 acba_192 was detected in two patients (43 and 58 years old) in the same ICU in RP (outbreak B) (figure). The two suspected index cases used for both outbreaks were burn victims from Romania who were transferred to Germany in CW 29 after staying in different Romanian clinics.
Using the NRC database, an isolate of CRAb OXA-23 acba_192 from another clinic in HE (HE 2) could also be assigned to outbreak B. The sample was taken during the admission screening of another Romanian fire victim.
Six cases with CRAb OXA-23 detection were reported from three wards of a clinic in BW (outbreak C) (figure). Two patients had been transferred to Germany as burn victims from different clinics in Romania in CW 29 and CW 32, respectively. The first patient to be admitted tested positive for CRAb OXA-23 upon admission (index case). The second patient was negative in admission screening. As in the other cases in BW, the pathogen was probably nosocomially transmitted to him. At the NRC, CRAb OXA-23 acba_191 was detected using PFGE, and a relationship with the outbreak isolates in RP and HE 1 could thereby be ruled out. The NRZ database contained an identical isolate (acba_191) from the admission screening of another Romanian burn victim from HE 2, which can therefore be assigned to outbreak C (figure).
Outbreak A included eight cases; outbreak B, three cases; and outbreak C, seven cases. Within the framework of the investigation, there were no indications of further epidemiological connections.
The pathogens were detected in blood, tracheal secretion, and in nose, throat, rectal, and wound swabs. An infection (blood, respiratory tract) was suspected in six cases, and a colonization in 12 cases.
The most likely cause of the outbreaks are CRAb strains introduced from Romania. This assumption is confirmed by the detection of pulse types previously unknown in Germany. Inpatient stays in Romania directly before transfer to Germany are documented. It was not possible to determine whether the patients with the same outbreak strains had been in the same clinics in Romania at an earlier point in time. For three of the Romanian patients, one of the outbreak pathogens was detected in the admission screening.
Discussion
Due to the high prevalence of CRAb in Southern and Eastern Europe (3, 4), admission screening (pharyngeal, rectal, wound swabs) should be carried out when patients who have had contact with the healthcare system in the relevant countries are admitted, and the relevant persons should be isolated pending the results (5). In addition, screening is also indicated for intra-German transfers between hospitals and other facilities with intensive medical care (e.g. neurological rehabilitation, outpatient ventilation) as well as after direct contact with patients with positive evidence (5). Due to the increased incidence of CRAb in ICUs, screening should also be considered when patients are transferred between ICUs.
For wound infections, colonization with CRAb is possible even if the detection test is negative, as mixed infections are often present. Sometimes a (resistant) pathogen can only be detected after treatment with antibiotics.
If carbapenem resistance is detected, isolates should be sent to the NRZ in order to identify and investigate connections. Each pathogen transmission and finding from outbreak investigations helps to reveal and close gaps in standard hygiene. In the event of an outbreak, persons who are infected or colonized should be isolated (if necessary in cohorts) and assigned personnel. Contact persons on the ward should be screened (rectally) at least once a week in order to detect further colonization and infections at an early stage.
A continuous exchange between hospital hygiene management and the personnel as well as the observation of compliance with routine processes, such as hand disinfection or wound care, support the adequate implementation of the hygiene recommendations.
As the prevalence of resistant pathogens is expected to continue to increase, it is important to stress that patient safety can only be maintained at a high level by continuously improving hygiene management.
References
- 1.Robert Koch-Institut. Infektionsepidemiologisches Jahrbuch 2020; 2021. www.rki.de/DE/Content/Infekt/Jahrbuch/Jahrbuch_2020.pdf?__blob=publicationFile (last accessed on 23 March 2022) [Google Scholar]
- 2.Murray CJL, Ikuta KS, Sharara F, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399:629–655. doi: 10.1016/S0140-6736(21)02724-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ayobami O, Willrich N, Suwono B, et al. The epidemiology of carbapenem-nonsusceptible acinetobacter species in Europe: analysis of EARS-Net data from 2013 to 2017. Antimicrob Resist Infect Control. 2020;9 doi: 10.1186/s13756-020-00750-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.European Centre for Disease Prevention and Control (ECDC), World Health Organization. Antimicrobial resistance surveillance in Europe. 2022. www.ecdc.europa.eu/sites/default/files/documents/ECDC-WHO-AMR-report.pdf (last accessed on 23 March 2022) [Google Scholar]
- 5.Kommission für Krankenhaushygiene und Infektionsprävention (KRINKO) Ergänzung zu den „Hygienemaßnahmen bei Infektionen oder Besiedlung mit multiresistenten gramnegativen Stäbchen“ (2012) im Rahmen der Anpassung an die epidemiologische Situation. Epidemiologisches Bulletin Robert Koch-Institut. 2014;21:183–184. [Google Scholar]