Abstract
Background
Lyme disease (LD) is a complex tick-borne pathology caused by Borrelia burgdorferi sensu lato bacteria. Currently, there are limited data regarding the health outcomes of people infected during pregnancy, the potential for perinatal transmission to their fetus, and the long-term effects on these children. Therefore, the primary objective of this survey study was to investigate the impact of LD in pregnancy on both the parent and their offspring.
Methods
A seven-section survey was developed and administered in REDCap. Although recruitment was primarily through LD-focused organizations, participation was open to anyone over the age of 18 who had been pregnant. Participant health/symptoms were compared across those with “Diagnosed LD,” “Suspected LD,” or “No LD” at any time in their lives. The timing of LD events in the participants’ histories (tick bite, diagnosis, treatment start, etc.) were then utilized to classify the participants’ pregnancies into one of five groups: “Probable Treated LD,” “Probable Untreated LD,” “Possible Untreated LD,” “No Evidence of LD,” and “Unclear.”
Results
A total of 691 eligible people participated in the survey, of whom 65% had Diagnosed LD, 6% had Suspected LD, and 29% had No LD ever. Both the Diagnosed LD and Suspected LD groups indicated a high symptom burden (p < 0.01). Unfortunately, direct testing of fetal/newborn tissues for Borrelia burgdorferi only occurred following 3% of pregnancies at risk of transmission; positive/equivocal results were obtained in 14% of these cases. Pregnancies with No Evidence of LD experienced the fewest complications (p < 0.01) and were most likely to result in a live birth (p = 0.01) and limited short- and long-term offspring pathologies (p < 0.01). Within the LD-affected pregnancy groups, obtaining treatment did not decrease complications for the parent themselves but did ameliorate neonatal health status, with reduced rates of rashes, hypotonia, and respiratory distress (all p < 0.01). The impact of parent LD treatment on longer-term child outcomes was less clear.
Conclusion
Overall, this pioneering survey represents significant progress toward understanding the effects of LD on pregnancy and child health. A large prospective study of pregnant people with LD, combining consistent diagnostic testing, exhaustive assessment of fetal/newborn samples, and long-term offspring follow-up, is warranted.
Keywords: pregnancy, Lyme disease, Lyme borreliosis, survey, symptoms, transmission, birth outcomes, child health
Introduction
Lyme disease (LD) is the most common tick-borne disease in North America and Europe, with known cases rising rapidly in recent years (1). Primarily transmitted through bites from infected Ixodes ticks, LD is caused by spirochetal bacteria within the Borrelia burgdorferi sensu lato species complex, also known as the Lyme borreliosis group (2). The disease generally consists of three stages (“early localized,” “early disseminated,” and “late disseminated”), although symptoms often vary and can overlap between stages. The first stage is expected to appear within days or weeks of infection, sometimes with a localized, characteristic erythema migrans (EM) (“bull’s-eye”) rash, as well as flu-like symptoms (3, 4). If left untreated, initial signs of Lyme disease progression can include multiple EM lesions, cranial nerve palsies, meningitis, and carditis, followed by inflammatory symptoms of late-stage dissemination, such as multi-system dysfunction, arthritis, and late neurologic and cutaneous pathologies (3–5). Even among people who do receive standard antibiotic therapy, 10–36% report persistent symptoms (6–9). However, despite the importance of timely and adequate treatment, rapid and accurate diagnosis is often lacking as symptoms can be difficult to identify (10–13), diagnostic criteria and physician awareness can vary significantly between regions (14–17), and current laboratory tests for Lyme disease are often insufficiently sensitive, especially in early stages (18, 19). As such, true case counts are likely highly underestimated, with many LD patients going undiagnosed and untreated (1, 20, 21).
A diagnosis or suspicion of Lyme disease is of particular concern for people who are pregnant or planning to become pregnant. Available research focused on the transmission of Borrelia burgdorferi from an infected person to their child in utero, as well as the impact of LD on pregnancy complications and the long-term health of offspring, has been both limited and discordant. Evidence to support the potential for perinatal transmission of the bacteria is drawn from multiple case studies of gestational Lyme disease where spirochetes were identified in the placenta and/or fetal tissue, including the fetal brain, heart, liver, lung, spleen, and kidney (22–28). In some cases, fetal transmission occurred even though the parent was asymptomatic and/or tested negative for Lyme disease by standard serological assays (22, 24, 26, 29). Additionally, LD-affected pregnancies have been associated with spontaneous abortion, stillbirth, premature delivery, intrauterine growth restriction, and neonatal death (30, 31), as well as a variety of neonatal conditions following a live birth, such as hyperbilirubinemia, hypotonia, cardiovascular and urinary tract defects, orthopedic and neurological abnormalities, respiratory distress, and rash (23, 24, 27–29, 32). Fortunately, there is also evidence to suggest that treating the parent for Lyme disease prior to or during pregnancy may reduce the frequency of these adverse outcomes (30, 33). However, in parallel, several cases of parental gestational LD with few pregnancy complications and no indication of Borrelia burgdorferi transmission have also been reported (34–37). Moreover, the frequency of fetal positivity is unclear and often not tested, a consistent syndrome associated with congenital infection has not been identified (38–40), and child health outcomes are rarely followed past the newborn stage (32, 37, 41, 42). As such, it is essential that additional research on the perinatal transmission of Lyme disease is conducted.
Here, we present a significant first step toward this goal with a large international cross-sectional survey of people who have experienced Lyme disease during pregnancy. The objective of our survey was to investigate the health outcomes of people with LD in pregnancy and their offspring, and to compare these to people without LD in pregnancy.
Materials and methods
Study population
Participants were eligible to complete the survey if they were at least 18 years old, had been pregnant at least once (regardless of the outcome of the pregnancy), and provided written informed consent for the collection of their and their child/children’s health information. Participants could reside in any country and could have been diagnosed with acute or chronic/late stage Lyme disease, suspected they have or had Lyme disease, or never been diagnosed with or suspected to have Lyme disease. We recruited participants directly through Lyme disease-focused organizations’ websites and social media platforms, as well as through the website and social media platforms of the McMaster Midwifery Research Centre.
Survey development
Members of the research team, including Lyme disease research experts, a pediatric infectious disease specialist, and a patient advocate, informed the creation and refinement of the survey. Questions were based on available survey and questionnaire tools that have been previously utilized in Lyme disease research (43, 44), including the General Symptom Questionnaire-30 for measuring symptom burden (45). The survey contained multi-option questions, rating scale questions, and open text fields, split across seven sections: diagnosis and treatment of Lyme disease, suspected Lyme disease and tick bite history, symptoms of Lyme disease, pregnancy information, child health information, demographics, and patient priorities (Supplementary Table 1). The survey was administered online in REDCap (46, 47) in both English (available between September 25th, 2020 and November 22nd, 2021) and French (available between January 25th, 2021 and November 22nd, 2021). Before publication, the survey was assessed for functionality and content validity by members of the research team and piloted by seven people (affiliated with a Lyme disease organization or directly/indirectly impacted by Lyme disease) who were not involved in its development.
Data collection and ethics
Survey data were collected anonymously, and participants were assigned a unique passcode. All responses were stored in REDCap and accessible only by the research members at McMaster University via a username and password. Ethics approval for this study was granted by the Hamilton Integrated Research Ethics Board (HiREB) (project #11222).
Data analysis
Data cleaning and statistical analysis were performed in R 4.1.1, using Kruskal-Wallis rank-sum tests, Wilcoxon-Mann-Whitney tests, Fisher’s exact tests, and Kendall rank correlations, as appropriate. If a participant commenced the survey multiple times (as determined by identical provided dates and data), the most complete set of responses was included. Participants were not required to complete the entire survey for their provided data to be utilized. Information from all unique, eligible participants contributed to the analysis of parent health and disease symptoms; however, pregnancies without a valid date of birth (DOB), due date, or miscarriage date were excluded from further analyses as the timing of gestation in relation to the timing of important Lyme disease-associated dates was critical for pregnancy classification. Child DOBs were considered invalid if they were biologically impossible (e.g., child bitten by a tick in 2003 but born in 2020).
We classified pregnancies into five groups: “Probable Treated LD,” “Probable Untreated LD,” “Possible Untreated LD,” “No Evidence of LD,” and “Unclear.” Pregnancies were classified as “Probable LD” if the birthing parent was diagnosed with Lyme disease and/or had an EM rash before or during the pregnancy, with the LD either “Treated” or “Untreated” before or during the pregnancy. A specific date for post-treatment symptom resolution (if any) was not queried in the survey and, therefore, a comparison of outcomes from “Resolved” vs. “Unresolved” LD pregnancies was not feasible. “Possible LD” pregnancies were those where the parent had been bitten by a tick and/or experienced an onset of non-EM Lyme disease symptoms (e.g., recurring headaches, joint swelling or pain, facial drooping, muscle spasms or twitching, numbness and tingling, etc.) before or during the pregnancy (all “Untreated”). Pregnancies were classified as “No Evidence of LD” if the parent had no diagnosis or suspicion of LD in their lifetime and either no tick bites at any point or no tick bite prior to or during the pregnancy. No Evidence of LD pregnancies also included those involving parents who eventually developed Lyme disease but provided dates for at least two of LD diagnosis, earliest tick bite, EM onset, and non-EM symptom onset, and these were all after the pregnancy. When only a post-pregnancy diagnosis date was available, or multiple dates were provided, all after the pregnancy, but the child was noted as diagnosed with congenital Lyme disease, the pregnancy was instead classified as “Unclear.” Pregnancies with one or more critical date(s) for classification (including treatment start date) in the same year as the birth and with a missing month were also classified as Unclear. Unclear pregnancies were not included in statistical analyses.
If a date that did not impact a pregnancy’s classification (e.g., parent DOB) had an available year but was missing the month, June (06) was used as a replacement. Child health outcomes were assessed using all live births with a valid DOB, as well as using similarly aged subsets of children to control for the effect of child age at the time of the survey. We selected the subsets to be as large as possible and as balanced as possible (i.e., similar proportions of included children from each group) while maintaining a non-significant p-value (p ≥ 0.05 by Fisher’s exact test) across the comparison groups for child age.
Results
Participant demographics
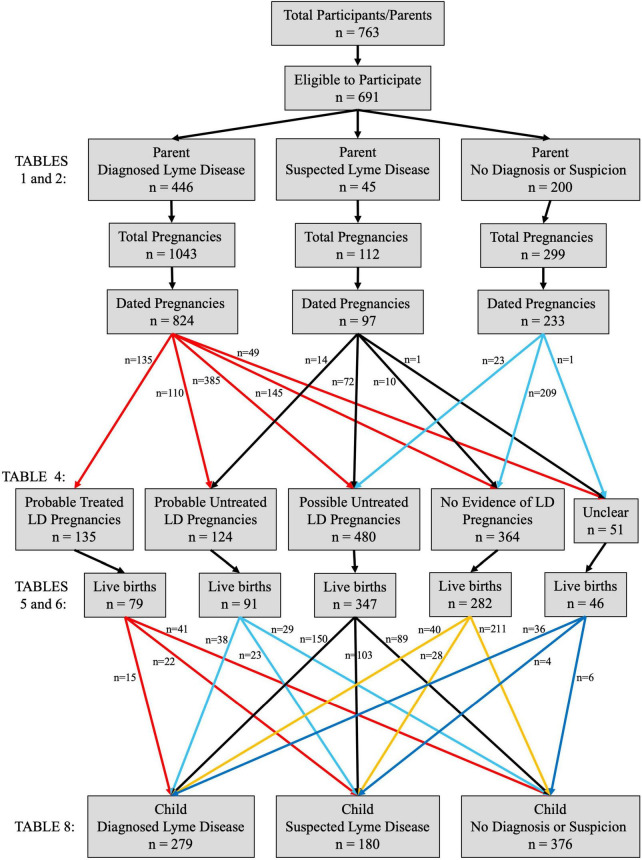
A total of 763 individuals commenced the survey (754 in English and nine in French) and 691 (91%) were eligible to participate (Figure 1). The majority of participants (n = 446, 65%) reported that they had been diagnosed with Lyme disease at some point in their lives (“Diagnosed LD” group), while some suspected they had or have Lyme disease but were never diagnosed (n = 45; “Suspected LD” group). The remaining participants (n = 200) had never been diagnosed with or suspected they had Lyme disease (“No LD” group). There were no significant differences across the three groups regarding their age at the time of participation (p = 0.16), racialized status (p = 0.33), pregnancy status at the time of participation (p = 0.87), total lifetime number of pregnancies (p = 0.52), and overall prior pregnancy outcomes (p = 0.24), although the Suspected LD group did demonstrate a somewhat increased frequency of miscarriages (30% of previous pregnancies vs. 22% in the Diagnosed LD group and 20% in the No LD group, p = 0.09) (Table 1). The No LD participants reported a higher achieved level of education (p = 0.09), as well as a significantly higher overall household income (p < 0.01), compared to both the Diagnosed LD and Suspected LD groups (Table 1). A discrepancy in household income was further observed between the two Lyme disease-affected groups (p = 0.04), with Suspected LD participants reporting the lowest overall salaries. Participant location was also unbalanced, with most No LD participants (82%) residing in Canada and more Diagnosed LD participants (56%) living in the United States (p < 0.01) (Table 1). Overall, 87% of participants resided in North America.
FIGURE 1.
Participant groups and pregnancy classifications. Of the 763 individuals who commenced the survey, 691 were eligible to participate (at least 18 years old, had been pregnant at least once, and provided written informed consent). Most participants (n = 446) had been diagnosed with Lyme disease (LD) at some point in their lives, while some suspected they had or have Lyme disease but were never diagnosed (n = 45). The remaining participants (n = 200) had never been diagnosed with or suspected they had LD. Overall, the 691 participants had been pregnant a total of 1,454 times, and a valid date of birth/miscarriage date/due date was provided for 1,154 of these pregnancies (79%), allowing for the classification of the pregnancy based on the Lyme disease status of the participant/parent. Pregnancies were classified as “Probable LD” if the parent was diagnosed with Lyme disease and/or observed an erythema migrans (EM) rash prior to or during the pregnancy (may be “Treated” or “Untreated” prior to or during the pregnancy). “Possible LD” pregnancies were those where the parent experienced a tick bite and/or onset of non-EM Lyme disease symptoms prior to or during the pregnancy (all “Untreated”). If at least two dates were provided for diagnosis, tick bite, EM onset, and other symptom onset, and they were all after the pregnancy, it was classified as a “No Evidence of LD” pregnancy, along with any pregnancy in a healthy control with no noted tick bite at any point or no tick bite prior to or during the pregnancy. Fewer than 5% of pregnancies (n = 51) could not be classified due to missing or conflicting dates (“Unclear” pregnancies). The majority (73%, n = 845) of dated pregnancies resulted in a live birth and the Lyme disease status of the child themselves at the time of parent participation in the survey was noted for 99% (n = 835) of live births.
TABLE 1.
Participant/birthing parent demographics.
| Parent diagnosed LD n = 446 | Parent suspected LD n = 45 | Parent no diagnosis or suspicion n = 200 | P-valuea | |
| Age at participation, years [mean (SD)] | 44 (10) | 44 (10) | 42 (11) | 0.16 |
| Total number of pregnancies [mean (SD)] | 2.8 (1.5) | 3.1 (1.8) | 2.8 (1.5) | 0.52 |
| Currently pregnant at participation | 6 (23/380) | 8 (3/40) | 6 (7/115) | 0.87 |
| Prior pregnancy outcomesb | 0.24 | |||
| Livebirth | 73 (647/888) | 66 (69/105) | 73 (187/255) | |
| Miscarriage | 22 (199/888) | 30 (32/105) | 20 (50/255) | |
| Stillbirth | 0.3 (3/888) | 0 (0/105) | 0.8 (2/255) | |
| Elective abortion | 4 (39/888) | 4 (4/105) | 6 (16/255) | |
| Identify as racialized | 11 (27/241) | 8 (2/24) | 6 (5/89) | 0.33 |
| Education | 0.09 | |||
| High school incomplete | 1 (3/310) | 3 (1/30) | 2 (2/100) | |
| High school diploma or equivalent | 7 (21/310) | 10 (3/30) | 2 (2/100) | |
| Some college | 13 (41/310) | 17 (5/30) | 6 (6/100) | |
| College diploma/certificate | 20 (62/310) | 20 (6/30) | 24 (24/100) | |
| Some university | 3 (9/310) | 7 (2/30) | 3 (3/100) | |
| Bachelor’s degree | 34 (104/310) | 27 (8/30) | 30 (30/100) | |
| Graduate degree | 23 (70/310) | 17 (5/30) | 33 (33/100) | |
| Household income | < 0.01 | |||
| Less than $20,000 | 8 (21/265) | 19 (5/26) | 1 (1/91) | |
| $20,000–$34,999 | 11 (30/265) | 4 (1/26) | 2 (2/91) | |
| $35,000–$49,999 | 9 (23/265) | 12 (3/26) | 3 (3/91) | |
| $50,000–$74,999 | 18 (48/265) | 19 (5/26) | 14 (13/91) | |
| $75,000–$99,999 | 13 (35/265) | 27 (7/26) | 22 (20/91) | |
| Over $100,000 | 41 (108/265) | 19 (5/26) | 57 (52/91) | |
| Country of residence | < 0.01 | |||
| Canada | 28 (89/319) | 47 (15/32) | 82 (82/100) | |
| United States | 56 (179/319) | 38 (12/32) | 17 (17/100) | |
| Other | 16 (51/319) | 16 (5/32) | 1 (1/100) | |
| Heard about the study on social media (Facebook, Instagram, and/or Twitter) | 76 (244/319) | 59 (19/32) | 68 (68/100) | 0.04 |
| Heard about the study from an organization’s website or an emailed newsletter | 16 (52/319) | 25 (8/32) | 6 (6/100) | < 0.01 |
| Heard about the study from a friend and/or family member | 12 (38/319) | 12 (4/32) | 37 (37/100) | < 0.01 |
| Heard about the study from a healthcare provider | 3 (9/319) | 0 (0/32) | 10 (10/100) | < 0.01 |
| Completed entire survey | 60 (268/446) | 60 (27/45) | 50 (100/200) | 0.05 |
Includes all individuals who were eligible to participate. Values are percentages (n/N) unless stated otherwise. aP-values calculated by Kruskal-Wallis rank sum tests (continuous data) and Fisher’s exact tests (discrete data). bPregnancy outcome data by individual pregnancy, not participant.
Participant Lyme disease symptoms, testing, and treatment
Both the Diagnosed LD and Suspected LD participants were more likely to have been bitten by a tick (p < 0.01) and experienced an EM rash (p < 0.01) in their lifetimes, compared to the No LD participants (Table 2). However, only 45% of Diagnosed LD and 61% of Suspected LD participants recalled a tick bite, and < 40% noticed an EM rash. Both LD groups also scored much higher on the General Symptom Questionnaire-30 (p < 0.01) and were more likely to identify as disabled (p < 0.01) and note that their symptoms impaired their work, social, or family functioning (p < 0.01) than the No LD group (Table 2). When the Diagnosed LD and Suspected LD participants were asked about their specific non-EM Lyme disease symptoms, they reported no significant differences, with similar rates of fever, pain, and cognitive dysfunction (Table 2).
TABLE 2.
Participant/birthing parent Lyme disease symptoms, testing, and treatment.
| Parent diagnosed LD n = 446 | Parent suspected LD n = 45 | Parent no diagnosis or suspicion n = 200 | P-valuea | |
| Resides in a Lyme disease endemic area | 56 (139/248) | 83 (20/24) | 88 (43/49) | < 0.01 |
| Any tick bite | 45 (174/385) | 61 (23/38) | 21 (26/124) | < 0.01 |
| Removed and tested tick positive for Borrelia burgdorferi | 27 (3/11) | 100 (1/1) | 0 (0/4) | 0.15 |
| Erythema migrans (EM) rash | 38 (125/329) | 39 (7/18) | 0 (0/19) | < 0.01 |
| Any non-EM Lyme disease symptoms | 99 (403/408) | 100 (44/44) | NA | 1 |
| Fever | 50 (203/408) | 57 (25/44) | NA | 0.43 |
| Recurring headaches | 73 (298/408) | 75 (33/44) | NA | 0.86 |
| Recurring neck pain | 72 (294/408) | 75 (33/44) | NA | 0.86 |
| Swelling of joints | 48 (195/408) | 59 (26/44) | NA | 0.20 |
| Joint pain | 80 (328/408) | 89 (39/44) | NA | 0.23 |
| Muscle pain | 77 (316/408) | 89 (39/44) | NA | 0.12 |
| Fatigue | 92 (375/408) | 100 (44/44) | NA | 0.06 |
| Facial drooping | 19 (78/408) | 30 (13/44) | NA | 0.11 |
| Numbness and tingling | 74 (301/408) | 84 (37/44) | NA | 0.15 |
| Muscle spasms or twitches | 67 (274/408) | 75 (33/44) | NA | 0.31 |
| Brain dysfunction (including memory issues) | 82 (333/408) | 89 (39/44) | NA | 0.30 |
| Lack of joint/muscle stability or function | 54 (221/408) | 66 (29/44) | NA | 0.15 |
| Other Lyme disease symptoms | 59 (240/408) | 52 (23/44) | NA | 0.42 |
| Ten or more of the above symptoms | 45 (183/408) | 52 (23/44) | NA | 0.43 |
| Positive ELISA or Western blot | 35 (128/368) | 9 (2/23) | NA | 0.01 |
| Positive ELISA and Western blot | 39 (145/368) | 9 (2/23) | NA | < 0.01 |
| Positive other blood test (e.g., PCR-DNA, EliSpot) | 32 (119/368) | 35 (8/23) | NA | 0.82 |
| Positive non-blood Lyme disease test | 23 (104/446) | NA | NA | NA |
| Lyme disease diagnosed at stage I (early localized) | 6 (25/392) | NA | NA | NA |
| Lyme disease diagnosed at stage II (early disseminated) | 2 (9/392) | NA | NA | NA |
| Lyme disease diagnosed at stage III (late disseminated) | 91 (358/392) | NA | NA | NA |
| Treated for Lyme disease | 94 (383/406) | NA | NA | NA |
| Oral antibiotics | 84 (322/383) | NA | NA | NA |
| Intravenous antibiotics | 26 (100/383) | NA | NA | NA |
| Other treatment | 54 (207/383) | NA | NA | NA |
| Tetracyclines | 82 (271/332) | NA | NA | NA |
| Cephalosporins | 43 (144/332) | NA | NA | NA |
| Penicillins | 41 (135/332) | NA | NA | NA |
| Azithromycin | 52 (172/332) | NA | NA | NA |
| Diagnosed with co-infections (e.g., Babesiosis, Bartonellosis, Ehrlichiosis) | 90 (321/355) | NA | NA | NA |
| GSQ-30 total score [mean (SD)]b | 60 (26) | 68 (28) | 18 (16) | < 0.01 |
| Impaired functioning in last 2 weeks | 85 (321/378) | 90 (37/41) | 29 (31/108) | < 0.01 |
| Identify as disabled | 90 (267/298) | 90 (28/31) | 41 (39/96) | < 0.01 |
Includes all individuals who were eligible to participate. Values are percentages (n/N) unless stated otherwise. aP-values calculated by Kruskal-Wallis rank sum tests (continuous data) and Fisher’s exact tests (discrete data). bMaximum score on the GSQ-30 is 120 (30 questions, each scored on a 0–4 scale).
Overall, more Diagnosed LD participants had previously tested positive for Lyme disease by standard ELISA and/or Western blot assays (p < 0.05) (Table 2). Individuals residing in the United States were more likely to receive their diagnosis in their own country (99%) compared to those living in Canada (78%) or elsewhere (82%) (p < 0.01). Almost all Diagnosed LD participants were diagnosed after they exhibited signs of late stage disseminated disease (91%), eventually received treatment specifically for LD (94%), and were further diagnosed with at least one co-infection (90%), most commonly Bartonellosis (65%) and/or Babesiosis (64%) (Table 2). Of those who received antibiotic treatment at some point in their lives, tetracyclines (e.g., doxycycline, minocycline) were most often prescribed (82%) (Table 2). An additional nine Suspected LD participants had also tested positive for Lyme disease by one or more blood test methods (ELISA, Western blot, PCR-DNA, EliSpot, and/or other), despite never receiving a formal diagnosis (Table 2).
Pregnancy complications and outcomes by participant/parent Lyme disease status
To assess the impact of Lyme disease and LD treatment on gestation and birth outcomes, participants’ pregnancies were classified into one of five groups based on the dates provided in the survey: Probable Treated LD (n = 135), Probable Untreated LD (n = 124), Possible Untreated LD (n = 480), No Evidence of LD (n = 364), and Unclear (n = 51) pregnancies (Figure 1 and Table 3). This distinction was important as many Diagnosed LD and Suspected LD participants/birthing parents did not develop Lyme disease symptoms until after their pregnancies or, conversely, did not receive a diagnosis or treatment until many years after delivery, if at all, despite being symptomatic before pregnancy. For most pregnancies classified as Probable LD based on a diagnosis date, this diagnosis date was prior to gestation. However, the Probable Treated LD group included eight cases where both diagnosis and treatment were confirmed to occur during the pregnancy, while the Probable Untreated LD group contained one case with a diagnosis during pregnancy, but treatment only commenced after delivery.
TABLE 3.
Pregnancy classifications.
| Probable Treated Lyme Disease pregnancy: |
| ● Parent diagnosed with Lyme disease (LD) before or during the pregnancy |
| AND/OR |
| ● Onset of an erythema migrans (EM) rash before or during the pregnancy |
| AND |
| ● Treatment for LD commenced before or during the pregnancy |
|
|
| Probable Untreated Lyme Disease pregnancy: |
| ● Parent diagnosed with Lyme disease before or during the pregnancy |
| AND/OR |
| ● Onset of an EM rash before or during the pregnancy |
| AND |
| ● No treatment for LD commenced before or during the pregnancy |
|
|
| Possible Untreated Lyme Disease pregnancy: |
| ● Parent bit by a tick before or during the pregnancy |
| AND/OR |
| ● Onset of non-EM Lyme disease symptoms before or during the pregnancy |
| AND |
| ● No treatment for LD commenced before or during the pregnancy |
|
|
| No Evidence of Lyme Disease pregnancy: |
| ● Parent has no diagnosis or suspicion of Lyme disease and no tick bites ever |
| OR |
| ● Parent has no diagnosis or suspicion of Lyme disease ever and no tick bite prior to or during the pregnancy |
| OR |
| ● At least two of LD diagnosis, tick bite, EM onset, and non-EM symptom onset dates provided, all of which were after the pregnancy |
|
|
| Unclear pregnancy: |
| ● Parent diagnosed with LD after the pregnancy with no other dates available |
| OR |
| ● At least two of diagnosis, tick bite, EM onset, and non-EM symptom onset dates provided, all after the pregnancy, but the child is noted as diagnosed with congenital Lyme disease |
| OR |
| ● One or more critical date(s) for classification (including treatment start) is/are the same year as the birth and the month is missing |
Pregnancies where the participant showed No Evidence of LD prior to or during gestation experienced significantly fewer complications, such as extreme fatigue (p < 0.01), memory issues (p < 0.01), fever of unknown origin (p < 0.01), exacerbation of joint pain (p < 0.01), and postpartum depression (p < 0.01), compared to all three LD-affected pregnancy groups, and were most likely to result in a live birth (p = 0.01) (Tables 4, 5). However, average parental age at the time of pregnancy was also the lowest in this No Evidence of LD group (p < 0.01) (Table 4). Rates of preeclampsia/gestational hypertension and gestational diabetes were similar across all classified pregnancy groups (p = 0.43 and p = 0.84, respectively) (Table 4). Within the Probable LD groups, obtaining treatment before or during gestation did not impact the risk of developing any of the queried complications (all p > 0.12) or affect the pregnancy outcome (p = 0.25).
TABLE 4.
Pregnancy complications and outcomes by participant/parent LD status.
| Probable treated LD pregnancies n = 135 | Probable untreated LD pregnancies n = 124 | Possible untreated LD pregnancies n = 480 | No evidence of LD pregnancies n = 364 | P-valuea | |
| Parent age at pregnancy, years [mean (SD)] | 34 (6) | 31 (5) | 31 (5) | 29 (5) | < 0.01 |
| Any pregnancy complication | 82 (108/131) | 91 (111/122) | 86 (390/453) | 53 (180/342) | < 0.01 |
| Vaginal spotting/bleeding | 34 (44/131) | 39 (48/122) | 35 (159/453) | 24 (83/342) | < 0.01 |
| Extreme fatigue unresolved by rest | 56 (74/131) | 59 (72/122) | 51 (233/453) | 15 (53/342) | < 0.01 |
| Memory issues | 44 (58/131) | 36 (44/122) | 34 (154/453) | 8 (27/342) | < 0.01 |
| Exacerbation of joint pain or swelling | 37 (49/131) | 34 (42/122) | 29 (133/453) | 6 (20/342) | < 0.01 |
| Bell’s Palsy | 4 (5/131) | 8 (10/122) | 3 (13/453) | 0 (0/342) | < 0.01 |
| Hyperemesis gravidarum | 16 (21/131) | 18 (22/122) | 21 (97/453) | 11 (36/342) | < 0.01 |
| Irritable uterus | 24 (32/131) | 24 (29/122) | 16 (72/453) | 7 (23/342) | < 0.01 |
| Prodromal labor | 15 (20/131) | 13 (16/122) | 16 (72/453) | 4 (13/342) | < 0.01 |
| Fever with unknown origin | 11 (14/131) | 16 (19/122) | 11 (50/453) | 3 (9/342) | < 0.01 |
| PUPPPs | 6 (8/131) | 5 (6/122) | 4 (16/453) | 2 (6/342) | 0.07 |
| Preterm labor | 9 (12/131) | 13 (16/122) | 9 (43/453) | 6 (19/342) | 0.05 |
| Preeclampsia or gestational hypertension | 5 (7/131) | 7 (9/122) | 9 (41/453) | 6 (22/342) | 0.43 |
| Gestational diabetes | 8 (10/131) | 7 (8/122) | 6 (28/453) | 6 (19/342) | 0.84 |
| HELLP syndrome | 5 (6/131) | 1 (1/122) | 0 (1/453) | 2 (8/342) | < 0.01 |
| Five or more complications | 23 (30/131) | 20 (24/122) | 14 (64/453) | 2 (8/342) | < 0.01 |
| Currently pregnant | 14 (19/135) | 2 (2/124) | 0 (1/480) | 1 (5/364) | < 0.01 |
| Pregnancy outcomesb | 0.01 | ||||
| Live birth | 68 (79/116) | 75 (91/122) | 72 (347/479) | 79 (282/359) | |
| Miscarriage | 32 (37/116) | 25 (30/122) | 28 (132/479) | 20 (73/359) | |
| Stillbirth | 0 (0/116) | 1 (1/122) | 0 (0/479) | 1 (4/359) | |
Only includes pregnancies with a known due date, date of birth, or miscarriage date, and excludes pregnancies with “unclear” timing in relation to diagnosis/treatment/symptoms/tick bite.
Values are percentages (n/N) unless stated otherwise. aP-values calculated by Kruskal-Wallis rank sum tests (continuous data) and Fisher’s exact tests (discrete data). bElective abortions were automatically excluded due to missing dates.
TABLE 5.
Postpartum and newborn outcomes by participant/parent LD status.
| Probable treated LD pregnancies n = 79 | Probable untreated LD pregnancies n = 91 | Possible untreated LD pregnancies n = 347 | No evidence of LD pregnancies n = 282 | P-valuea | |
| Gestational age at delivery, weeks [mean (SD)] | 39 (3) | 38 (3) | 39 (3) | 39 (2) | 0.06 |
| Delivery < 34 weeks | 4 (3/77) | 6 (5/86) | 4 (13/318) | 2 (6/271) | 0.33 |
| Delivery < 37 weeks | 18 (14/77) | 15 (13/86) | 12 (38/318) | 13 (35/271) | 0.47 |
| Newborn weight, lbs [mean (SD)] | 7.41 (1.4) | 7.41 (1.4) | 7.39 (1.4) | 7.63 (1.28) | 0.25 |
| Female | 43 (34/79) | 54 (49/91) | 49 (168/346) | 50 (141/280) | 0.54 |
| Parent postpartum depression | 51 (40/79) | 43 (39/91) | 48 (164/345) | 26 (74/281) | < 0.01 |
| Neonatal death | 0 (0/79) | 0 (0/91) | 0 (0/346) | 1 (2/279) | 0.51 |
| Breastfed | 85 (64/75) | 90 (78/87) | 90 (300/332) | 92 (251/273) | 0.38 |
| Any signs of pathology in the first 2 weeks of life | 43 (32/74) | 53 (41/78) | 47 (148/315) | 33 (87/267) | < 0.01 |
| Hyperbilirubinemia | 31 (23/74) | 31 (24/78) | 35 (111/315) | 26 (70/267) | 0.14 |
| Adenopathy | 0 (0/74) | 5 (4/78) | 2 (5/315) | 1 (2/267) | 0.05 |
| Rash | 4 (3/74) | 15 (12/78) | 7 (23/315) | 1 (3/267) | < 0.01 |
| Fever of unknown origin | 4 (3/74) | 10 (8/78) | 5 (16/315) | 3 (7/267) | 0.05 |
| Intrauterine growth restriction | 1 (1/74) | 1 (1/78) | 2 (7/315) | 1 (2/267) | 0.44 |
| Hypotonia | 1 (1/74) | 9 (7/78) | 1 (2/315) | 1 (2/267) | < 0.01 |
| Respiratory distress | 9 (7/74) | 24 (19/78) | 10 (33/315) | 5 (14/267) | < 0.01 |
| Any congenital anomaly | 9 (7/75) | 7 (6/84) | 8 (27/327) | 8 (21/272) | 0.95 |
| Syndactyly | 14 (1/7) | 17 (1/6) | 7 (2/27) | 5 (1/21) | 0.46 |
| Heart defect | 14 (1/7) | 50 (3/6) | 30 (8/27) | 19 (4/21) | 0.45 |
| Urologic/urogenital defect | 14 (1/7) | 17 (1/6) | 7 (2/27) | 0 (0/21) | 0.20 |
| Cleft lip and/or palate | 0 (0/7) | 0 (0/6) | 4 (1/27) | 0 (0/21) | 1 |
| Neural tube defect | 0 (0/7) | 0 (0/6) | 7 (2/27) | 0 (0/21) | 0.69 |
| Other | 57 (4/7) | 50 (3/6) | 67 (18/27) | 81 (17/21) | 0.37 |
Only includes live births with a known date of birth and excludes pregnancies with “unclear” timing in relation to diagnosis/treatment/symptoms/tick bite. Values are percentages (n/N) unless stated otherwise. aP-values calculated by Kruskal-Wallis rank sum tests (continuous data) and Fisher’s exact tests (discrete data).
Testing of fetal-associated tissues (cord tissue, cord blood, placental tissue, fetal tissue, or foreskin) after birth or miscarriage for evidence of gestational transmission of Borrelia burgdorferi was reported following 28 pregnancies (25 Probable LD pregnancies and three that did not provide a DOB for classification), mostly involving United States residents (76%). These 25 Probable LD pregnancies represented only 17% of all classified pregnancies where the participant had a known diagnosis of Lyme disease before the delivery or miscarriage (n = 149) and only 3% of all classified pregnancies where vertical transmission was possible (Probable or Possible LD; n = 739). Positive or equivocal (borderline/inconclusive) results were obtained in four out of 28 cases (14%; all cord blood samples, plus one placenta sample that was also positive). In one of the two positive cases, the birthing parent received oral antibiotics for Lyme disease around the third month of gestation, while in the other, the participant was treated with multiple antibiotics in the same year as the DOB, but it was unclear if this was during or after the pregnancy. In both cases with equivocal cord blood results, the participant received more than 4 weeks of treatment several years before the pregnancy but experienced a recurrence of symptoms prior to conception. All cases with confirmed negative results, in which the timing of treatment relative to pregnancy was provided, had also been treated with antibiotics before or during gestation.
Child outcomes by participant/parent Lyme disease status
Pregnancies that resulted in a live birth before the parent participated in the survey (73%, n = 845) were further investigated to examine associations between the birthing parents’ Lyme disease/treatment status and neonatal/child health outcomes (Figure 1). In the first 2 weeks of life, newborns from Probable Untreated LD pregnancies were most likely to experience rashes (p < 0.01), unexplained fevers (p = 0.05), hypotonia (p < 0.01), and respiratory distress (p < 0.01), compared to Probable Treated LD, Possible Untreated LD, and No Evidence of LD offspring (Table 5). The frequency of congenital anomalies was similar across all groups (all p > 0.20) (Table 5).
When offspring of all ages were included in the analysis of long-term outcomes, those from Untreated LD pregnancies (Probable and Possible) demonstrated the highest rates of musculoskeletal, gastrointestinal/urinary, sleep, concentration/fatigue, sensory, and vision issues, along with recurrent infections and dizziness (all p < 0.01) (Table 6). Offspring from Untreated LD parents were also most likely to eventually be diagnosed with Lyme disease themselves (p < 0.01), along with a wide range of other diagnoses, including allergy/immune, orthopedic, cardiovascular/respiratory, neurological, gastrointestinal, dermatologic, endocrine, genitourinary/renal, ocular, and mental health disorders (all p < 0.01) (Table 6). Children from Treated LD pregnancies appeared to fare significantly better than those from Untreated LD pregnancies, with LD symptoms, health issues, and rates of medical diagnoses comparable to No Evidence of LD children (Table 6). However, these Probable Treated LD offspring were the youngest at the time of their parents’ participation in the survey [mean of 5 years old and maximum of 29 years old, compared to a mean of 13–16 years old and maximum of 48–54 years old in the other three groups (p < 0.01)] (Table 6), so health issues associated with later childhood/adolescence would be less likely to have manifested in this group.
TABLE 6.
Child outcomes by participant/parent LD status.
| Probable treated LD pregnancies n = 79 | Probable untreated LD pregnancies n = 91 | Possible untreated LD pregnancies n = 347 | No evidence of LD pregnancies n = 282 | P-valuea | |
| Child age at parent participation, years [mean (SD)] | 5 (6) | 16 (11) | 13 (9) | 14 (10) | < 0.01 |
| Diagnosed with Lyme disease | 19 (15/78) | 42 (38/90) | 44 (150/342) | 14 (40/279) | < 0.01 |
| Congenital Lyme disease | 73 (11/15) | 61 (22/36) | 59 (89/150) | 0 (0/40) | < 0.01 |
| Child age at LD diagnosis, years [mean (SD)] | 3 (2) | 12 (10) | 10 (6) | 12 (6) | < 0.01 |
| Suspected Lyme disease | 28 (22/78) | 26 (23/90) | 30 (103/341) | 10 (28/278) | < 0.01 |
| Any tick bite | 21 (16/78) | 17 (15/89) | 20 (69/339) | 16 (45/279) | 0.53 |
| Any musculoskeletal symptoms | 40 (29/73) | 64 (54/84) | 61 (194/318) | 26 (71/269) | < 0.01 |
| Any gastrointestinal/urinary symptoms | 65 (46/71) | 79 (67/85) | 76 (244/319) | 40 (106/262) | < 0.01 |
| Any recurrent infections | 43 (30/70) | 74 (63/85) | 66 (212/319) | 40 (104/263) | < 0.01 |
| Any non-specific symptoms | 74 (55/74) | 87 (74/85) | 85 (278/326) | 52 (139/269) | < 0.01 |
| Night sweats | 15 (11/74) | 26 (22/85) | 24 (79/326) | 9 (23/269) | < 0.01 |
| Excessive sweating | 12 (9/74) | 19 (16/85) | 15 (50/326) | 6 (15/269) | < 0.01 |
| Sleep issues | 35 (26/74) | 52 (44/85) | 47 (153/326) | 21 (56/269) | < 0.01 |
| General fatigue | 27 (20/74) | 48 (41/85) | 47 (153/326) | 19 (50/269) | < 0.01 |
| Difficulty concentrating | 24 (18/74) | 51 (43/85) | 53 (172/326) | 19 (50/269) | < 0.01 |
| “Brain fog” | 16 (12/74) | 35 (30/85) | 38 (123/326) | 12 (32/269) | < 0.01 |
| Limb weakness | 7 (5/74) | 24 (20/85) | 15 (49/326) | 7 (19/269) | < 0.01 |
| Dizziness | 7 (5/74) | 29 (25/85) | 23 (76/326) | 10 (26/269) | < 0.01 |
| Tingling/numbness | 11 (8/74) | 29 (25/85) | 18 (58/326) | 9 (25/269) | < 0.01 |
| Palpitations | 7 (5/74) | 16 (14/85) | 17 (57/326) | 8 (22/269) | < 0.01 |
| Sensory issues | 39 (29/74) | 45 (38/85) | 47 (152/326) | 16 (42/269) | < 0.01 |
| Vision issues | 14 (10/74) | 24 (20/85) | 20 (64/326) | 9 (25/269) | < 0.01 |
| Colic | 14 (10/74) | 24 (20/85) | 25 (82/326) | 13 (34/269) | < 0.01 |
| Failure to thrive | 3 (2/74) | 11 (9/85) | 11 (35/326) | 2 (6/269) | < 0.01 |
| Hair loss/bald spots | 5 (4/74) | 12 (10/85) | 6 (18/326) | 3 (8/269) | 0.02 |
| Severe diaper rashes | 15 (11/74) | 22 (19/85) | 18 (58/326) | 6 (17/269) | < 0.01 |
| Rashes or skin lesions | 22 (16/74) | 26 (22/85) | 22 (73/326) | 10 (28/269) | < 0.01 |
| Fevers of unknown origin | 12 (9/74) | 16 (14/85) | 16 (52/326) | 3 (9/269) | < 0.01 |
| Any allergy/immunology/hematologic diagnosis | 33 (24/72) | 54 (44/82) | 51 (157/306) | 34 (90/262) | < 0.01 |
| Any orthopedic/rheumatologic diagnosis | 13 (9/67) | 40 (29/73) | 32 (93/292) | 15 (36/242) | < 0.01 |
| Any cardiovascular/respiratory diagnosis | 16 (11/68) | 46 (33/72) | 32 (92/284) | 18 (44/247) | < 0.01 |
| Any functional/psychosomatic/pain diagnosis | 16 (11/67) | 30 (21/69) | 31 (87/280) | 9 (21/246) | < 0.01 |
| Any neurological diagnosis | 15 (10/67) | 39 (29/74) | 42 (121/287) | 16 (40/250) | < 0.01 |
| Any gastrointestinal diagnosis | 21 (14/68) | 41 (29/71) | 41 (116/285) | 16 (41/251) | < 0.01 |
| Any dermatologic diagnosis | 36 (25/69) | 57 (42/74) | 48 (142/295) | 23 (58/251) | < 0.01 |
| Any endocrine diagnosis | 4 (3/67) | 20 (14/71) | 14 (39/277) | 8 (20/249) | < 0.01 |
| Any genitourinary/renal diagnosis | 8 (5/66) | 23 (17/74) | 18 (49/268) | 11 (28/250) | < 0.01 |
| Any ocular diagnosis | 9 (6/64) | 23 (17/73) | 15 (41/272) | 7 (17/242) | < 0.01 |
| Any mental health/developmental diagnosis | 45 (33/73) | 76 (65/85) | 70 (221/316) | 46 (120/262) | < 0.01 |
| Other diagnosis | 10 (6/63) | 32 (24/74) | 27 (72/267) | 12 (27/229) | < 0.01 |
| Any adverse vaccine reaction | 14 (10/74) | 22 (19/85) | 27 (87/328) | 11 (31/271) | < 0.01 |
Includes all live births with a known date of birth and excludes pregnancies with “unclear” timing in relation to diagnosis/treatment/symptoms/tick bite. Values are percentages (n/N) unless stated otherwise. aP-values calculated by Kruskal-Wallis rank sum tests (continuous data) and Fisher’s exact tests (discrete data).
A weak correlation was confirmed between child age and the overall number of symptoms (tau = 0.22, p < 0.01) or medical diagnoses (tau = 0.31, p < 0.01) noted by their parent (Supplementary Figure 1). Therefore, to reduce the confounding effect of child age on health outcomes, the data were re-analyzed with subsets of similarly aged children. When restricted to offspring 6–15 years old at the time of the study [44% of all children (29–51% of each group); p = 0.08 for age], those from Probable Treated LD pregnancies demonstrated musculoskeletal, gastrointestinal/urinary, sleep, concentration/fatigue, sensory, and vision issues, as well as rashes and unexplained fevers, at similarly elevated rates to children from Probable and Possible Untreated LD pregnancies (Table 7). Orthopedic, cardiovascular/respiratory, gastrointestinal, dermatologic, and Lyme disease diagnoses were also prevalent in all three LD-affected groups, compared to No Evidence of LD children (all p < 0.01) (Table 7). However, some pathologies were still most frequently observed in Probable (and sometimes Possible) Untreated LD 6–15-year-olds, such as recurrent infections (p < 0.01), limb weakness (p = 0.01), dizziness (p = 0.01), allergy/immune diagnoses (p = 0.02), and neurological diagnoses (p < 0.01) (Table 7). A similar pattern was identified in the smaller and/or less balanced subsets of 2–8-year-olds [30% of all children (18–59% of each group); p = 0.09 for age] (Supplementary Table 2) and 9–22-year-olds [48% of all children (16–55% of each group); p = 0.06 for age] (Supplementary Table 3).
TABLE 7.
Outcomes in children between the ages of six and 15 by participant/parent LD status.
| Probable treated LD pregnancies n = 23 | Probable untreated LD pregnancies n = 33 | Possible untreated LD pregnancies n = 178 | No evidence of LD pregnancies n = 113 | P-valuea | |
| Child age at parent participation, years [mean (SD)] | 9 (3) | 11 (3) | 10 (3) | 10 (3) | 0.08 |
| Diagnosed with Lyme disease | 48 (11/23) | 48 (16/33) | 45 (80/176) | 14 (16/113) | < 0.01 |
| Congenital Lyme disease | 82 (9/11) | 88 (14/16) | 56 (45/80) | 0 (0/16) | < 0.01 |
| Child age at LD diagnosis, years [mean (SD)] | 3 (2) | 7 (3) | 7 (3) | 7 (3) | < 0.01 |
| Suspected Lyme disease | 22 (5/23) | 27 (9/33) | 30 (53/175) | 16 (18/113) | 0.04 |
| Any tick bite | 30 (7/23) | 16 (5/32) | 23 (40/173) | 18 (20/113) | 0.40 |
| Any musculoskeletal symptoms | 68 (15/22) | 73 (22/30) | 65 (108/165) | 27 (30/110) | < 0.01 |
| Any gastrointestinal/urinary symptoms | 86 (18/21) | 87 (26/30) | 82 (134/164) | 44 (47/107) | < 0.01 |
| Any recurrent infections | 43 (9/21) | 80 (24/30) | 65 (106/164) | 42 (44/105) | < 0.01 |
| Any non-specific symptoms | 91 (20/22) | 90 (28/31) | 88 (148/168) | 52 (57/110) | < 0.01 |
| Night sweats | 18 (4/22) | 29 (9/31) | 26 (43/168) | 9 (10/110) | < 0.01 |
| Excessive sweating | 9 (2/22) | 19 (6/31) | 12 (21/168) | 5 (5/110) | 0.04 |
| Sleep issues | 50 (11/22) | 58 (18/31) | 50 (84/168) | 24 (26/110) | < 0.01 |
| General fatigue | 59 (13/22) | 52 (16/31) | 45 (75/168) | 15 (16/110) | < 0.01 |
| Difficulty concentrating | 55 (12/22) | 58 (18/31) | 50 (84/168) | 18 (20/110) | < 0.01 |
| “Brain fog” | 36 (8/22) | 35 (11/31) | 35 (59/168) | 8 (9/110) | < 0.01 |
| Limb weakness | 9 (2/22) | 32 (10/31) | 14 (24/168) | 8 (9/110) | 0.01 |
| Dizziness | 14 (3/22) | 32 (10/31) | 22 (37/168) | 10 (11/110) | 0.01 |
| Tingling/numbness | 23 (5/22) | 32 (10/31) | 15 (25/168) | 9 (10/110) | 0.01 |
| Palpitations | 18 (4/22) | 16 (5/31) | 15 (26/168) | 6 (7/110) | 0.07 |
| Sensory issues | 68 (15/22) | 55 (17/31) | 51 (85/168) | 20 (22/110) | < 0.01 |
| Vision issues | 27 (6/22) | 35 (11/31) | 21 (36/168) | 9 (10/110) | < 0.01 |
| Colic | 5 (1/22) | 13 (4/31) | 21 (35/168) | 14 (15/110) | 0.17 |
| Failure to thrive | 5 (1/22) | 10 (3/31) | 10 (16/168) | 2 (2/110) | 0.04 |
| Hair loss/bald spots | 5 (1/22) | 19 (6/31) | 1 (2/168) | 3 (3/110) | < 0.01 |
| Severe diaper rashes | 14 (3/22) | 26 (8/31) | 16 (27/168) | 9 (10/110) | 0.10 |
| Rashes or skin lesions | 41 (9/22) | 32 (10/31) | 24 (40/168) | 9 (10/110) | < 0.01 |
| Fevers of unknown origin | 18 (4/22) | 19 (6/31) | 18 (30/168) | 3 (3/110) | < 0.01 |
| Any allergy/immunology/hematologic diagnosis | 45 (10/22) | 65 (20/31) | 52 (82/158) | 36 (38/105) | 0.02 |
| Any orthopedic/rheumatologic diagnosis | 20 (4/20) | 33 (9/27) | 27 (40/149) | 8 (8/96) | < 0.01 |
| Any cardiovascular/respiratory diagnosis | 35 (7/20) | 42 (11/26) | 31 (46/147) | 13 (13/97) | < 0.01 |
| Any functional/psychosomatic/pain diagnosis | 42 (8/19) | 31 (8/26) | 23 (32/139) | 3 (3/97) | < 0.01 |
| Any neurological diagnosis | 21 (4/19) | 46 (13/28) | 43 (64/150) | 13 (13/99) | < 0.01 |
| Any gastrointestinal diagnosis | 35 (7/20) | 41 (11/27) | 36 (53/147) | 13 (13/101) | < 0.01 |
| Any dermatologic diagnosis | 55 (11/20) | 56 (15/27) | 47 (72/154) | 26 (27/104) | < 0.01 |
| Any endocrine diagnosis | 11 (2/19) | 16 (4/25) | 10 (15/143) | 4 (4/100) | 0.10 |
| Any genitourinary/renal diagnosis | 16 (3/19) | 23 (6/26) | 14 (20/142) | 10 (10/100) | 0.33 |
| Any ocular diagnosis | 24 (4/17) | 20 (5/25) | 14 (20/143) | 7 (7/101) | 0.07 |
| Any mental health/developmental diagnosis | 67 (14/21) | 81 (25/31) | 72 (118/164) | 51 (55/107) | < 0.01 |
| Other diagnosis | 12 (2/17) | 44 (12/27) | 32 (46/144) | 11 (10/93) | < 0.01 |
| Any adverse vaccine reaction | 23 (5/22) | 19 (6/31) | 30 (51/169) | 15 (16/110) | 0.02 |
Only includes live births with a known date of birth, where the child was between 6 and 15 years old when their parent participated in the survey, and excludes pregnancies with “unclear” timing in relation to diagnosis/treatment/symptoms/tick bite. Values are percentages (n/N) unless stated otherwise. aP-values calculated by Kruskal-Wallis rank sum tests (continuous data) and Fisher’s exact tests (discrete data).
Child outcomes by child Lyme disease status
Lyme disease had been diagnosed in 33% of children (n = 279) with a known DOB and LD status at the time of their parents’ participation in the survey (Figure 1 and Table 8). While 54% of these infections were noted as being congenital in origin, this was impossible to confirm given the retrospective nature of the survey. However, only 29% of Diagnosed LD offspring had a known tick bite, and only 12% had ever shown an EM rash, which might suggest an alternative infection source (Table 8). Children were diagnosed with Lyme disease at an average age of 11 years old, were tested mainly using standard ELISA and/or Western blot assays, and 84% were also positive for at least one co-infection (Table 8). An additional 180 children (22%) were suspected of having Lyme disease, while the remaining 376 (45%) had never been diagnosed, nor did their parent (the participant) suspect they ever had LD (Figure 1). When these three groups were compared, Diagnosed LD offspring were consistently associated with the highest rates of Lyme disease symptoms and comorbidities, while outcomes in Suspected LD children were also more severe than those observed in the No LD group (all p < 0.01) (Table 8). However, there was once again a significant difference in the average age of the children across these three LD groups (p < 0.01) (Table 8 and Supplementary Figure 1).
TABLE 8.
Child outcomes by child LD status.
| Child diagnosed LD n = 279 | Child suspected LD n = 180 | Child no diagnosis or suspicion n = 376 | P-valuea | |
| Parent Lyme disease status during pregnancy | <0.01 | |||
| Probable treated Lyme disease | 6 (15/243) | 12 (22/176) | 11 (41/370) | |
| Probable untreated Lyme disease | 16 (38/243) | 13 (23/176) | 8 (29/370) | |
| Possible untreated Lyme disease | 62 (150/243) | 59 (103/176) | 24 (89/370) | |
| No evidence of Lyme disease | 16 (40/243) | 16 (28/176) | 57 (211/370) | |
| Child age at parent participation, years [mean (SD)] | 15 (9) | 13 (9) | 12 (11) | <0.01 |
| Child age at LD diagnosis, years [mean (SD)] | 11 (7) | NA | NA | NA |
| Any tick bite | 29 (79/275) | 20 (36/180) | 12 (44/376) | <0.01 |
| Erythema migrans (EM) rash | 12 (33/267) | 19 (7/36) | 2 (1/44) | 0.04 |
| Flu-like symptoms of Lyme disease | 64 (171/268) | NA | NA | NA |
| Cardiac symptoms of Lyme disease | 13 (36/268) | NA | NA | NA |
| Neurological symptoms of Lyme disease | 25 (67/268) | NA | NA | NA |
| Joint symptoms of Lyme disease | 42 (112/268) | NA | NA | NA |
| Ocular symptoms of Lyme disease | 15 (39/268) | NA | NA | NA |
| Borrelial lymphocytoma | 1 (4/268) | NA | NA | NA |
| Other Lyme disease symptoms | 47 (125/268) | NA | NA | NA |
| Positive ELISA or western blot | 36 (73/203) | NA | NA | NA |
| Positive ELISA and western blot | 38 (78/203) | NA | NA | NA |
| Positive other blood test | 36 (74/203) | NA | NA | NA |
| Positive non-blood Lyme disease test | 30 (83/277) | NA | NA | NA |
| Diagnosed with co-infections (e.g., babesiosis, bartonellosis, ehrlichiosis) | 84 (194/231) | NA | NA | NA |
| Any musculoskeletal symptoms | 80 (208/261) | 60 (100/167) | 19 (68/360) | <0.01 |
| Any gastrointestinal/urinary symptoms | 88 (228/259) | 81 (137/169) | 37 (130/353) | <0.01 |
| Any recurrent infections | 74 (191/259) | 68 (112/164) | 38 (136/356) | <0.01 |
| Any non-specific symptoms | 99 (263/267) | 90 (153/170) | 47 (171/362) | <0.01 |
| Night sweats | 41 (109/267) | 18 (31/170) | 3 (10/362) | <0.01 |
| Excessive sweating | 22 (58/267) | 14 (23/170) | 5 (17/362) | <0.01 |
| Sleep issues | 60 (160/267) | 49 (83/170) | 15 (54/362) | <0.01 |
| General fatigue | 67 (180/267) | 48 (81/170) | 7 (26/362) | <0.01 |
| Difficulty concentrating | 69 (185/267) | 45 (76/170) | 13 (47/362) | <0.01 |
| “Brain fog” | 58 (154/267) | 25 (43/170) | 5 (19/362) | <0.01 |
| Limb weakness | 28 (75/267) | 14 (24/170) | 2 (7/362) | <0.01 |
| Dizziness | 40 (108/267) | 18 (30/170) | 2 (7/362) | <0.01 |
| Tingling/numbness | 36 (97/267) | 12 (21/170) | 2 (6/362) | <0.01 |
| Palpitations | 29 (78/267) | 15 (26/170) | 2 (6/362) | <0.01 |
| Sensory issues | 63 (169/267) | 41 (69/170) | 12 (44/362) | <0.01 |
| Vision issues | 33 (87/267) | 16 (27/170) | 5 (17/362) | <0.01 |
| Colic | 24 (64/267) | 22 (38/170) | 13 (47/362) | <0.01 |
| Failure to thrive | 11 (30/267) | 9 (15/170) | 4 (13/362) | <0.01 |
| Hair loss/bald spots | 8 (21/267) | 9 (15/170) | 2 (6/362) | <0.01 |
| Severe diaper rashes | 19 (51/267) | 18 (31/170) | 8 (30/362) | <0.01 |
| Rashes or skin lesions | 31 (84/267) | 26 (44/170) | 6 (23/362) | <0.01 |
| Fevers of unknown origin | 21 (57/267) | 16 (27/170) | 2 (7/362) | <0.01 |
| Any allergy/immunology/hematologic diagnosis | 64 (161/251) | 51 (80/157) | 28 (101/357) | <0.01 |
| Any orthopedic/rheumatologic diagnosis | 41 (93/226) | 33 (47/144) | 11 (39/341) | <0.01 |
| Any cardiovascular/respiratory diagnosis | 47 (107/228) | 28 (39/138) | 15 (51/345) | <0.01 |
| Any functional/psychosomatic/pain diagnosis | 46 (97/213) | 29 (41/141) | 5 (18/345) | <0.01 |
| Any neurological diagnosis | 53 (117/222) | 43 (63/148) | 11 (38/347) | <0.01 |
| Any gastrointestinal diagnosis | 52 (117/223) | 36 (51/142) | 13 (46/349) | <0.01 |
| Any dermatologic diagnosis | 53 (120/228) | 52 (77/148) | 25 (88/353) | <0.01 |
| Any endocrine diagnosis | 29 (63/219) | 7 (10/139) | 4 (14/347) | <0.01 |
| Any genitourinary/renal diagnosis | 29 (62/212) | 17 (22/133) | 8 (27/350) | <0.01 |
| Any ocular diagnosis | 20 (40/202) | 14 (20/143) | 8 (27/341) | <0.01 |
| Any mental health/developmental diagnosis | 82 (213/260) | 73 (121/165) | 39 (140/357) | <0.01 |
| Other diagnosis | 37 (75/201) | 30 (40/132) | 7 (25/334) | <0.01 |
| Any adverse vaccine reaction | 33 (87/265) | 25 (43/171) | 9 (34/368) | <0.01 |
Only includes live births with a known date of birth. Values are percentages (n/N) unless stated otherwise. aP-values calculated by Kruskal-Wallis rank sum tests (continuous data) and Fisher“2019”s exact tests (discrete data).
Discussion
Our survey is the largest survey ever conducted focused on Lyme disease in pregnancy. It represents an important step toward addressing current research gaps regarding the impact of LD on gestational complications and neonatal/child outcomes, as well as the risk of perinatal transmission. Overall, we found that both participants and their children who had been diagnosed with, or suspected that they have, Lyme disease reported managing a high symptom burden and several co-morbidities. In this study, treatment for LD was not associated with decreased pregnancy complications or improved birth outcomes but was associated with reduced rates of select neonatal pathology (e.g., rashes, hypotonia, and respiratory distress). Our findings additionally suggest that there are substantial and non-specific long-term effects of LD exposure in utero on child health, which may be somewhat attenuated by parental treatment for LD. Unfortunately, confirmation of congenital infection was unavailable in most cases, as testing of fetal/newborn tissues after birth or miscarriage occurred for only 3% of pregnancies at risk of transmission.
A concerning finding from this study was the severity of symptoms in people with Suspected LD, as well as the frequency of positive Lyme disease tests in this group, despite never receiving an official diagnosis by a medical professional. This Suspected LD group was also associated with the lowest attained education levels and household incomes, indicating that financial hardship, employment status, and/or a lack of insurance (depending on their country of residence) may be affecting their access to health care, delaying diagnosis and treatment, and negatively influencing outcomes (48). Many additional barriers preventing diagnosis in this group are also possible (1, 48). When pregnancies were classified based on the likelihood of Borrelia burgdorferi infection at the time of gestation, participants with Possible or Probable LD (including those with undiagnosed but Suspected LD) experienced much higher rates of pregnancy complications, such as extreme fatigue, joint pain, fever of unknown origin, and postpartum depression, compared to those with No Evidence of LD. These symptoms are all potentially consistent with a Lyme disease diagnosis (1, 5, 49) and are not necessarily a function of the pregnancy itself (31), although a comparison of symptoms before and during pregnancy in the same cohort of people would be of interest. LD-affected pregnancies were also associated with a higher rate of miscarriage, supporting an association between Lyme disease and spontaneous abortion, as previously documented (30, 31, 33). No significant differences in stillbirth or neonatal death rates were observed; however, these outcomes were rare (n = 5 stillbirths and n = 2 neonatal deaths).
Children born from pregnancies classified as Possible or Probable LD demonstrated a wide range of pathologies, including musculoskeletal, gastrointestinal, orthopedic, cardiovascular, respiratory, sleep, rashes, fevers, concentration, sensory, and vision issues. This is consistent with previous research (24, 30, 32), which has been unable to identify a specific syndrome associated with potential congenital Borrelia burgdorferi infection in offspring. However, unlike prior studies, we did not observe any significant differences between children from LD-affected pregnancies and No Evidence of LD pregnancies in terms of gestational age at delivery, intrauterine growth restriction diagnoses, congenital anomalies, or hyperbilirubinemia rates (24, 31, 32). Unfortunately, given the lack of Borrelia burgdorferi testing done on fetal/neonatal tissues, we cannot determine how many of the reported child outcomes were truly due to the transmission of the bacteria itself or were, instead, caused by other factors. Possible other contributors include an independent Lyme disease exposure in the child, parental or child co-infections (50, 51), a genetic predisposition to infectious or inflammatory conditions (52), and the overall impact of a parental pathological state in pregnancy on child growth and development (53–56).
The effect of birthing parent treatment for Lyme disease on offspring health outcomes was also challenging to disassociate from a confounding factor: child age at the time of parent participation in the survey. In general, we discovered a weak correlation between offspring age and the total number of LD-associated symptoms or medical diagnoses noted by their parent. Children from Treated Probable LD pregnancies were also significantly younger than those from Untreated or No Evidence of LD groups, which might indicate that timely diagnosis and subsequent treatment for Lyme disease has become more prevalent in recent years. These findings further confirm the importance of longitudinal follow-up in offspring with potential perinatal LD exposure. When this age discrepancy was appropriately considered, our results support the hypothesis that parent treatment for Lyme disease before or during pregnancy can attenuate severe pathology in neonates/children but does not eliminate poor outcomes entirely (30, 32). In this study, offspring with treated parents revealed reduced rates of neonatal rashes, fever, hypotonia, and respiratory distress. Nevertheless, over time, they developed many of the same pathologies as their counterparts with untreated parents but were still less likely to experience specific issues, such as recurrent infections, limb weakness, and dizziness. Further studies are warranted and urgently needed to compare (age-matched) long-term child outcomes from treated and untreated LD pregnancies.
Study limitations
While this research represents substantial progress toward understanding the possible effects of Lyme disease on pregnancy and offspring health, it is not without limitations. Since recruitment was primarily through North American-based Lyme disease advocacy groups, participants were more likely to have experienced chronic/late-stage disease with persistent symptoms than would be expected from a random group of LD patients (7, 57). Most participants also resided in Canada or the United States, despite international eligibility. As such, our findings may not extend to other Lyme disease populations. Additionally, as a cross-sectional survey, the accuracy of our results is dependent on the accuracy of the participant-provided information, including the LD-associated dates used for pregnancy classification. Given that many of these dates were 10–70 years prior to participation, we expected some discrepancies due to recall issues. This concern was mitigated during the data cleaning process by identifying and removing biologically impossible data points. Finally, another consequence of the data’s highly variable and self-reported nature was the necessity to group the participants very broadly, despite known differences that may have important biological effects. For example, LD diagnosed with varying criteria and tests, Borrelia burgdorferi infection before vs. during pregnancy, treatments with different efficacies, and treated vs. resolved Lyme disease were not distinguished (1, 7, 33, 57). Significant differences were also observed between the study groups in several baseline characteristics, such as participant location, household income, and parent age at the time of pregnancy (1, 48, 58, 59). It is essential that these variables are thoroughly considered in future studies employing more reliable data collection methods.
Conclusion
Overall, this survey provides an important foundation upon which hypotheses can be generated for many overdue projects focused on Lyme disease in pregnancy. Our results provide evidence of the need for rigorous prospective observational studies that can minimize bias in assessing the impact of LD on pregnancy outcomes and health outcomes of offspring exposed to LD in utero. Research priorities include consistent testing of fetal/neonatal tissues at birth for Borrelia (and other tick-vectored pathogens) to determine the true frequency of transmission, as well as to help distinguish between the various factors that may contribute to similar symptoms in children (1, 60). Hopefully, future research will lead to evidence-based clinical guidance and resources for healthcare providers, allowing for improved and prompt diagnosis, treatment, and care for both parents and children with Lyme disease.
Data availability statement
The datasets presented in this article are not readily available because consent to share the data beyond the research team was not collected from the research participants. Requests to access the datasets should be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Hamilton Integrated Research Ethics Board (HiREB) (project #11222). The patients/participants provided their written informed consent to participate in this study.
Author contributions
RM, SF, VL, CM, MW, IB, EC, AO, OM, and ED conceived and designed the survey. RM, SF, OM, and ED developed and disseminated the recruitment materials. KL and RM performed the data analysis. KL wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Acknowledgments
We wish to acknowledge the individuals who participated in this study, and the Lyme disease organizations that shared the recruitment materials and promoted the survey. We thank John Davison for translating the survey from English to French, and Carolyne Mellon and Vanessa Hebert for reviewing the translated version. We also thank Lindsay Schroeder, Rosie Numan, Maggie Shaw, Isabel Rose, Phyllis Bedford, Jennifer Wheeler, and Tamara House for testing the survey prior to publication.
Funding
This study was funded by the DH Falle Family Foundation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.1022766/full#supplementary-material
References
- 1.Bobe JR, Jutras BL, Horn EJ, Embers ME, Bailey A, Moritz RL, et al. Recent progress in lyme disease and remaining challenges. Front Med. (2021) 8:666554. 10.3389/FMED.2021.666554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudenko N, Golovchenko M, Grubhoffer L, Oliver JH. Updates on Borrelia burgdorferi sensu lato complex with respect to public health. Ticks Tick Borne Dis. (2011) 2:123–8. 10.1016/J.TTBDIS.2011.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray TS, Shapiro ED. Lyme disease. Clin Lab Med. (2010) 30:311–28. 10.1016/J.CLL.2010.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardenas-de la Garza JA, de la Cruz-Valadez E, Ocampo-Candiani J, Welsh O. Clinical spectrum of lyme disease. Eur J Clin Microbiol Infect Dis. (2019) 38:201–8. 10.1007/S10096-018-3417-1 [DOI] [PubMed] [Google Scholar]
- 5.Coburn J, Garcia B, Hu LT, Jewett MW, Kraiczy P, Norris SJ, et al. Lyme disease pathogenesis. Curr Issues Mol Biol. (2021) 42:473–518. 10.21775/CIMB.042.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marques A. Chronic lyme disease: a review. Infect Dis Clin North Am. (2008) 22:341–60. 10.1016/J.IDC.2007.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aucott JN, Yang T, Yoon I, Powell D, Geller SA, Rebman AW. Risk of post-treatment Lyme disease in patients with ideally-treated early Lyme disease: a prospective cohort study. Int J Infect Dis. (2022) 116:230–7. 10.1016/J.IJID.2022.01.033 [DOI] [PubMed] [Google Scholar]
- 8.Aucott JN, Rebman AW, Crowder LA, Kortte KB. Post-treatment Lyme disease syndrome symptomatology and the impact on life functioning: is there something here? Qual Life Res. (2013) 22:75–84. 10.1007/S11136-012-0126-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berglund J, Stjernberg L, Ornstein K, Tykesson-Joelsson K, Walter H. 5-y Follow-up study of patients with neuroborreliosis. Scand J Infect Dis. (2002) 34:421–5. 10.1080/00365540110080421 [DOI] [PubMed] [Google Scholar]
- 10.Schwartz AM, Hinckley AF, Mead PS, Hook SA, Kugeler KJ. Surveillance for Lyme disease - United States, 2008-2015. MMWR Surveill Summ. (2017) 66:1–12. 10.15585/MMWR.SS6622A1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aucott J, Morrison C, Munoz B, Rowe PC, Schwarzwalder A, West SK. Diagnostic challenges of early Lyme disease: lessons from a community case series. BMC Infect Dis. (2009) 9:79. 10.1186/1471-2334-9-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steere AC, Sikand VK. The presenting manifestations of Lyme disease and the outcomes of treatment. N Engl J Med. (2003) 348:2472–4. 10.1056/NEJM200306123482423 [DOI] [PubMed] [Google Scholar]
- 13.Pachner AR. Neurologic manifestations of Lyme disease, the new “great imitator”. Rev Infect Dis. (1989) 11(Suppl. 6):S1482–6. [PubMed] [Google Scholar]
- 14.Government of Canada,. Lyme disease: For health professionals - Canada.ca. (2022). Available online at: https://www.canada.ca/en/public-health/services/diseases/lyme-disease/health-professionals-lyme-disease.html (accessed April 8, 2022). [Google Scholar]
- 15.Mead P, Petersen J, Hinckley A. Updated CDC Recommendation for serologic diagnosis of Lyme disease. MMWR Morb Mortal Wkly Rep. (2019) 68:703. 10.15585/MMWR.MM6832A4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ontario Ministry of Health and Long-Term Care. Infectious Diseases Protocol Appendix B: Provincial Case Definitions for Diseases of Public Health Significance. Toronto, ON: Ontario Ministry of Health and Long-Term Care; (2019). [Google Scholar]
- 17.Henry B, Crabtree A, Roth D, Blackman D, Morshed M. Lyme disease: knowledge, beliefs, and practices of physicians in a low-endemic area. Can Fam Physician. (2012) 58:e289–95. [PMC free article] [PubMed] [Google Scholar]
- 18.Horn EJ, Dempsey G, Schotthoefer AM, Prisco UL, McArdle M, Gervasi SS, et al. The Lyme disease biobank: characterization of 550 patient and control samples from the east coast and upper midwest of the United States. J Clin Microbiol. (2020) 58:e00032–20. 10.1128/JCM.00032-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cook MJ, Puri BK. Commercial test kits for detection of Lyme borreliosis: a meta-analysis of test accuracy. Int J Gen Med. (2016) 9:427–40. 10.2147/IJGM.S122313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lloyd VK, Hawkins RG. Under-detection of Lyme disease in Canada. Healthcare. (2018) 6:125. 10.3390/HEALTHCARE6040125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kugeler KJ, Schwartz AM, Delorey MJ, Mead PS, Hinckley AF. Estimating the frequency of Lyme disease diagnoses, United States, 2010–2018. Emerg Infect Dis. (2021) 27:616. 10.3201/EID2702.202731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Figueroa R, Bracero LA, Aguero-Rosenfeld M, Beneck D, Coleman J, Schwartz I. Confirmation of Borrelia burgdorferi spirochetes by polymerase chain reaction in placentas of women with reactive serology for Lyme antibodies. Gynecol Obstet Invest. (1996) 41:240–3. 10.1159/000292277 [DOI] [PubMed] [Google Scholar]
- 23.Maraspin V, Cimperman J, Lotriè-Furlan S, Pleterski-Rigler D, Strle F. Erythema migrans in pregnancy. Wien Klin Wochenschr. (1999) 111:933–40. [PubMed] [Google Scholar]
- 24.MacDonald AB. Gestational Lyme borreliosis. implications for the fetus. Rheum Dis Clin North Am. (1989) 15:657–77. [PubMed] [Google Scholar]
- 25.MacDonald AB, Benach JL, Burgdorfer W. Stillbirth following maternal Lyme disease. N Y State J Med. (1987) 87:615–6. [PubMed] [Google Scholar]
- 26.Macdonald AB. Human fetal borreliosis, toxemia of pregnancy, and fetal death. Zentralbl Bakteriol Mikrobiol Hyg A. (1986) 263:189–200. 10.1016/S0176-6724(86)80122-5 [DOI] [PubMed] [Google Scholar]
- 27.Schlesinger PA, Duray PH, Burke BA, Steere AC, Stillman MT. Maternal-fetal transmission of the Lyme disease spirochete, Borrelia burgdorferi. Ann Intern Med. (1985) 103:67–8. 10.7326/0003-4819-103-1-67 [DOI] [PubMed] [Google Scholar]
- 28.Weber K, Bratzke HJ, Neubert U, Wilske B, Duray PH. Borrelia burgdorferi in a newborn despite oral penicillin for Lyme borreliosis during pregnancy. Pediatr Infect Dis J. (1988) 7:286–9. 10.1097/00006454-198804000-00010 [DOI] [PubMed] [Google Scholar]
- 29.Dattwyler RJ, Volkman DJ, Luft BJ. Immunologic aspects of Lyme borreliosis. Rev Infect Dis. (1989) 11(Suppl. 6):S1494–8. 10.1093/CLINIDS/11.SUPPLEMENT_6.S1494 [DOI] [PubMed] [Google Scholar]
- 30.Lakos A, Solymosi N. Maternal Lyme borreliosis and pregnancy outcome. Int J Infect Dis. (2010) 14:e494–8. 10.1016/j.ijid.2009.07.019 [DOI] [PubMed] [Google Scholar]
- 31.Maraspin V, Lusa L, Blejec T, Ružiæ-Sabljiæ E, Perme MP, Strle F. Course and outcome of erythema migrans in pregnant women. J Clin Med. (2020) 9:1–20. 10.3390/JCM9082364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gardner T. Lyme Disease. 5th ed. In: Remington J, Klein J. editors. Infectious Diseases of the Fetus and Newborn Infant. Philadelphia: The W.B. Saunders Co; (2001). p. 519–641. [Google Scholar]
- 33.Waddell LA, Greig J, Robbin L, Hinckley AF, Ogden NH. A systematic review on the impact of gestational Lyme disease in humans on the fetus and newborn. PLoS One. (2018) 13:e0207067. 10.1371/JOURNAL.PONE.0207067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mikkelse AL, Palle C. Lyme disease during pregnancy. Acta Obstet Gynecol Scand. (1987) 66:477–8. 10.3109/00016348709022058 [DOI] [PubMed] [Google Scholar]
- 35.Moniuszko A, Czupryna P, Pancewicz S, Kondrusik M, Penza P, Zajkowska J. Borrelial lymphocytoma–a case report of a pregnant woman. Ticks Tick Borne Dis. (2012) 3:257–8. 10.1016/J.TTBDIS.2012.06.004 [DOI] [PubMed] [Google Scholar]
- 36.Walsh CA, Mayer EW, Baxi LV. Lyme disease in pregnancy: case report and review of the literature. Obstet Gynecol Surv. (2007) 62:41–50. 10.1097/01.OGX.0000251024.43400.9A [DOI] [PubMed] [Google Scholar]
- 37.Trevisan G, Ruscio M, di Meo N, Nan K, Cinco M, Trevisini S, et al. Case report: lyme borreliosis and pregnancy - our experience. Front Med. (2022) 9:816868. 10.3389/FMED.2022.816868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mylonas I. Borreliosis during pregnancy: a risk for the unborn child? Vector Borne Zoonotic Dis. (2011) 11:891–8. 10.1089/VBZ.2010.0102 [DOI] [PubMed] [Google Scholar]
- 39.Lambert JS. An overview of tickborne infections in pregnancy and outcomes in the newborn: the need for prospective studies. Front Med. (2020) 7:72. 10.3389/FMED.2020.00072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Elliott DJ, Eppes SC, Klein JD. Teratogen update: lyme disease. Teratology. (2001) 64:276–81. 10.1002/TERA.1074 [DOI] [PubMed] [Google Scholar]
- 41.Lampert F. Infantile multisystem inflammatory disease: another case of a new syndrome. Eur J Pediatr. (1986) 144:593–6. 10.1007/BF00496045 [DOI] [PubMed] [Google Scholar]
- 42.Trevisan G, Stinco G, Cinco M. Neonatal skin lesions due to a spirochetal infection: a case of congenital Lyme borreliosis? Int J Dermatol. (1997) 36:677–80. 10.1046/J.1365-4362.1997.00217.X [DOI] [PubMed] [Google Scholar]
- 43.Wormser GP, Weitzner E, McKenna D, Nadelman RB, Scavarda C, Molla I, et al. Long-term assessment of health-related quality of life in patients with culture-confirmed early Lyme disease. Clin Infect Dis. (2015) 61:244–7. 10.1093/CID/CIV277 [DOI] [PubMed] [Google Scholar]
- 44.Citera M, Freeman PR, Horowitz RI. Empirical validation of the horowitz multiple systemic infectious disease syndrome questionnaire for suspected Lyme disease. Int J Gen Med. (2017) 10:249–73. 10.2147/IJGM.S140224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fallon BA, Zubcevik N, Bennett C, Doshi S, Rebman AW, Kishon R, et al. The general symptom questionnaire-30 (GSQ-30): a Brief measure of multi-system symptom burden in Lyme disease. Front Med. (2019) 6:283. 10.3389/FMED.2019.00283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. (2009) 42:377–81. 10.1016/J.JBI.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. (2019) 95:103208. 10.1016/J.JBI.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hirsch AG, Poulsen MN, Nordberg C, Moon KA, Rebman AW, Aucott JN, et al. Risk factors and outcomes of treatment delays in Lyme disease: a population-based retrospective cohort study. Front Med. (2020) 7:560018. 10.3389/FMED.2020.560018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fallon BA, Madsen T, Erlangsen A, Benros ME. Lyme borreliosis and associations with mental disorders and suicidal behavior: a nationwide danish cohort study. Am J Psychiatry. (2021) 178:921–31. 10.1176/APPI.AJP.2021.20091347 [DOI] [PubMed] [Google Scholar]
- 50.Saetre K, Godhwani N, Maria M, Patel D, Wang G, Li KI, et al. Congenital babesiosis after maternal infection with Borrelia burgdorferi and Babesia microti. J Pediatric Infect Dis Soc. (2018) 7:e1–5. 10.1093/JPIDS/PIX074 [DOI] [PubMed] [Google Scholar]
- 51.Jasik KP, Okła H, Słodki J, Rozwadowska B, Słodki A, Rupik W. Congenital tick borne diseases: is this an alternative route of transmission of tick-borne pathogens in mammals? Vector Borne Zoonotic Dis. (2015) 15:637–44. 10.1089/VBZ.2015.1815 [DOI] [PubMed] [Google Scholar]
- 52.Kwok AJ, Mentzer A, Knight JC. Host genetics and infectious disease: new tools, insights and translational opportunities. Nat Rev Genet. (2020) 22:137–53. 10.1038/s41576-020-00297-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gillman MW. Developmental origins of health and disease. N Engl J Med. (2005) 353:1848–50. 10.1056/NEJME058187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mulder EJH, Robles De Medina PG, Huizink AC, van den Bergh BRH, Buitelaar JK, Visser GHA. Prenatal maternal stress: effects on pregnancy and the (unborn) child. Early Hum Dev. (2002) 70:3–14. 10.1016/S0378-3782(02)00075-0 [DOI] [PubMed] [Google Scholar]
- 55.Barker DJP. In utero programming of cardiovascular disease. Theriogenology. (2000) 53:555–74. 10.1016/S0093-691X(99)00258-7 [DOI] [PubMed] [Google Scholar]
- 56.Dreier JW, Andersen AMN, Berg-Beckhoff G. Systematic review and meta-analyses: fever in pregnancy and health impacts in the offspring. Pediatrics. (2014) 133:e674–88. 10.1542/PEDS.2013-3205 [DOI] [PubMed] [Google Scholar]
- 57.Rebman AW, Aucott JN. Post-treatment Lyme Disease as a model for persistent symptoms in Lyme disease. Front Med. (2020) 7:57. 10.3389/FMED.2020.00057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marques AR, Strle F, Wormser GP. Comparison of Lyme disease in the United States and Europe. Emerg Infect Dis. (2021) 27:2017–24. 10.3201/EID2708.204763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lean SC, Derricott H, Jones RL, Heazell AEP. Advanced maternal age and adverse pregnancy outcomes: a systematic review and meta-analysis. PLoS One. (2017) 12:e0186287. 10.1371/JOURNAL.PONE.0186287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stechenberg BW. Lyme disease: the latest great imitator. Pediatr Infect Dis J. (1988) 7:402–9. 10.1097/00006454-198806000-00007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this article are not readily available because consent to share the data beyond the research team was not collected from the research participants. Requests to access the datasets should be directed to the corresponding author.