Abstract
Backgrounds and Aims
Defect closure post-EMR and endoscopic submucosal dissection (ESD) is recommended to decrease the risk of delayed bleeding and perforation. Current methods of tissue approximation and closure of mucosal defects have their limitations, including restricted maneuverability, need for scope withdrawal, or difficulty in apposing larger defects. Through-the-scope HeliX tacking system (Apollo Endosurgery, Austin, Tex, USA) is a novel tissue apposition device designed to mimic suture closure without the need to withdraw the endoscope or insert bulky devices on the tip of the endoscope. Previous reports demonstrate its effectiveness for closure of standard postresection defects, fistulae, and peroral endoscopic myotomy mucosectomy sites. However, reports on its feasibility and technique for very large defects are scarce.
Methods
In this case series, we demonstrate a tissue approximation technique using a novel through-the-scope HeliX tacking system for a 10-cm ascending colon and a 5-cm gastric antrum postresection defects. A zig-zag running pattern and figure 8 suturing pattern were used for the colonic and gastric defect approximation, respectively.
Results
Tissue approximation was easily and successfully achieved in both cases. Four and 2 sets of tacks were used in the colonic and gastric defect, respectively. Closure of these defects otherwise would have required a substantial number of clips, withdrawal/exchange of the endoscope to mount the suturing device, or difficulty in maneuvering the closure devices. There was no immediate or delayed adverse event postprocedure.
Conclusions
Through-the-scope suturing using the HeliX tacking system is a unique tool that integrates the capabilities of current tissue apposition devices post EMR and ESD. Through-the-scope suturing is an ideal option especially for tissue approximation of large resection beds within the right side of the colon and areas with limited space for maneuverability.
Abbreviations: ESD, endoscopic submucosal dissection; OTSC, over-the-scope clip; TTSC, through-the-scope clip
Video
Endoscopic tacking for tissue approximation of very large EMR defects.
Introduction
Defect closure after EMR or endoscopic submucosal dissection (ESD) has been a topic of interest in the last few decades with advances in minimally invasive endoscopic techniques. Prophylactic closure of larger postpolypectomy defects (greater than 20 mm) would reduce incidence of severe adverse events such as bleeding and delayed perforation. There are various devices available for defect closure. The most common method is through-the-scope clip (TTSC) closure. However, TTSC closure could be incomplete in up to 31% of cases.1,2 Predictive factors for complete closure are good access, complete submucosal lifting, en bloc resection, and smaller polyp size.1 In addition, correct use of TTSC requires expertise in properly maneuvering the clip and precisely adjusting the clip to completely appose the 2 sides of the defect. As a result, closure of large mucosal defects after EMR or ESD, using TTSC, can be challenging in areas with limited maneuverability. In addition, given TTSC has lower applied force and results in mucosal layer closure only, oftentimes multiple clips are needed to achieve proper closure and tissue approximation, which could prove to be costly.3
In comparison to TTSC, over-the-scope clip (OTSC) has a reported success rate of 82% to 93% for closing postpolypectomy defects in the literature.4,5 Although OTSC can achieve-full thickness closure, it can only be used with certain endoscopes. OTSC should be mounted externally over the scope, which requires scope removal and reinsertion that can be cumbersome and time consuming. OTSC may not be ideal for defects larger than 20 mm or those with inflammatory or necrotic margins.6
A newer platform for defect closure is the endoscopic suturing system (Apollo Endosurgery, Austin, Tex, USA). The success rate of endoscopic suturing for defect closure is 88.2% to 100% in the published literature.7 In comparison to clip closure, suturing appears to be more effective and eliminates need for surgical assessment.8 OverStitch SX (Apollo Endosurgery, Austin, Tex, USA), the newer generation of endoscopic suturing system, eliminated the prior limitation of endoscopic suturing use in the right side of the colon and within the deeper parts of the small bowel with its compatibility with single-channel endoscopes. However, like OTSC, endoscopic suturing requires removing the scope and assembling the device outside the tip of the scope, which could be cumbersome, particularly in lesions within the lower gastrointestinal tracts. Maneuvering Overstitch in limited spaces also can be challenging, even in hands of an expert endoscopist.
Most recently, Apollo Endosurgery released a new through-the-scope HeliX tacking system for defect closure. This system is compatible with both gastroscope and colonoscope with a 2.8 mm or larger working channel. Currently, there are 2 various lengths of this device available in the market: 160 cm and 235 cm. Each device set contains 4 individual tacks. Four 5-mm HeliX tacks are tethered on a single 3-0 polypropylene suture. There is an eyelet within the middle of each HeliX tack, and flushing of the eyelet with the mucosal surface is an indication of correct depth placement. Applying suture tension results in approximation of HeliX tacks screwed within the healthy tissue or defect margin. The final placement is secured with placement of a cinch on top of the 4 tacks, similar to the endoscopic suturing cinching mechanism.
In this case series, we demonstrate the use of the novel through-the-scope suturing system in tissue approximation of 2 large postmucosectomy defects (Video 1, available online at www.giejournal.org).
Patients and Methods
First case
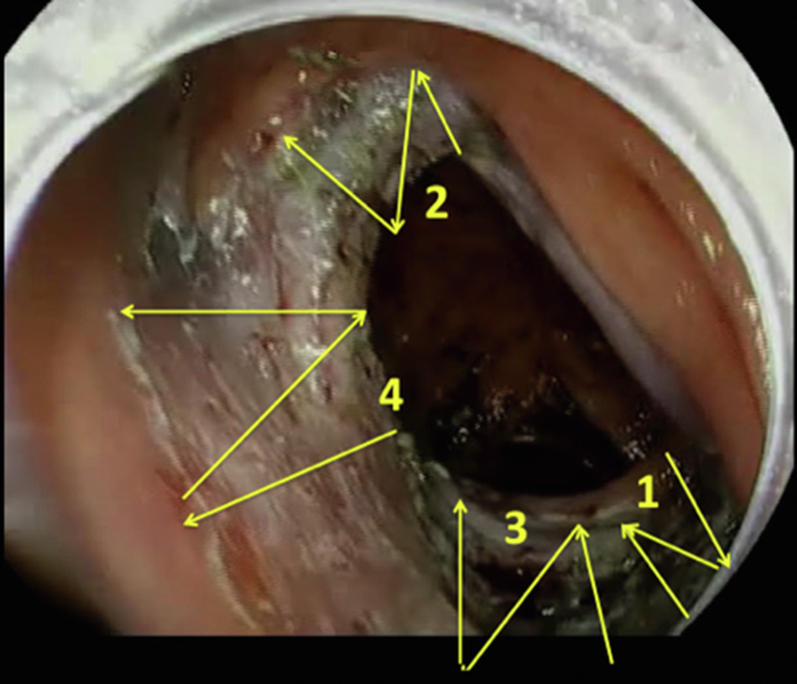
A 65-year-old woman was found to have a 10-cm granular lateral spreading polyp involving half circumference of the lumen in the ascending colon. Colonoscopy was technically challenging because of her tortuous colon. The double balloon platform was used to reach the lesion within the right side of the colon and achieve adequate stabilization for polyp removal. She underwent successful polyp removal with a hybrid EMR/ESD technique. The resection bed was measured 10 × 7 cm in length and width, respectively. Because of the large resected area, closure was deemed necessary owing to the high risk of delayed bleeding. Considering the size and location of the resection bed expanding beyond a colonic fold, we did not believe closure of the defect would be achieved by TTSC. Also, in the presence of a tortuous colon and the polyp location, endoscopic suturing was not an ideal option. The decision was made to proceed with tissue approximation using 4 sets of X-tack HeliX in a similar pattern of running sutures (z-pattern/zig zag) (Fig. 1). Proper tissue approximation of this large colonic defect was achieved using this novel technique within 40 minutes (Fig. 2). The patient was discharged postprocedure without any immediate or delayed adverse events.
Figure 1.
Z-pattern (running suture/zig-zag pattern) for tissue approximation of a large crescent shaped defect in the colon.
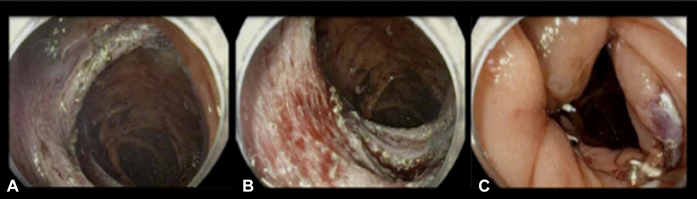
Figure 2.
A and B, 10- × 7-cm mucosal defect in the ascending colon post–hybrid EMR/endoscopic submucosal dissection expanding beyond a colonic fold. C, Successful tissue approximation with 4 sets of HeliX tacks (Apollo Endosurgery, Austin, Tex, USA).
Second case
A 68-year-old man was found to have a 5-cm semipedunculated polyp in the lesser curvature of the stomach. Successful removal of the polyp was achieved with the ESD technique, resulting in a 50- × 30-mm mucosal defect. Based on the large dimension of the resected bed, we believed TTSC closure would require at least 8 to 10 clips. Also, considering the lateral location of the defect, maneuvering the OverStitch suturing system seemed challenging because of the lack of adequate visibility of the 2 lateral edges of the defect. Thus, it was decided attempts at defect closure would be performed via the X-tack HeliX tacking system to minimize the risk of postmucosectomy bleeding and delayed perforation. Considering the circular large resection bed, we elected for tack placement in a pattern similar to a figure 8 to facilitate tissue approximation (Fig. 3). Full closure of the defect was achieved using 2 sets of X-tack HeliX systems (8 tacks in total) (Fig. 4). The patient was discharged postprocedure without any immediate or delayed adverse events. He underwent repeat EGD in 2 months for evaluation of a duodenal polyp. The tacks were noted intact, and the defect appeared to be closed (Fig. 5).
Figure 3.
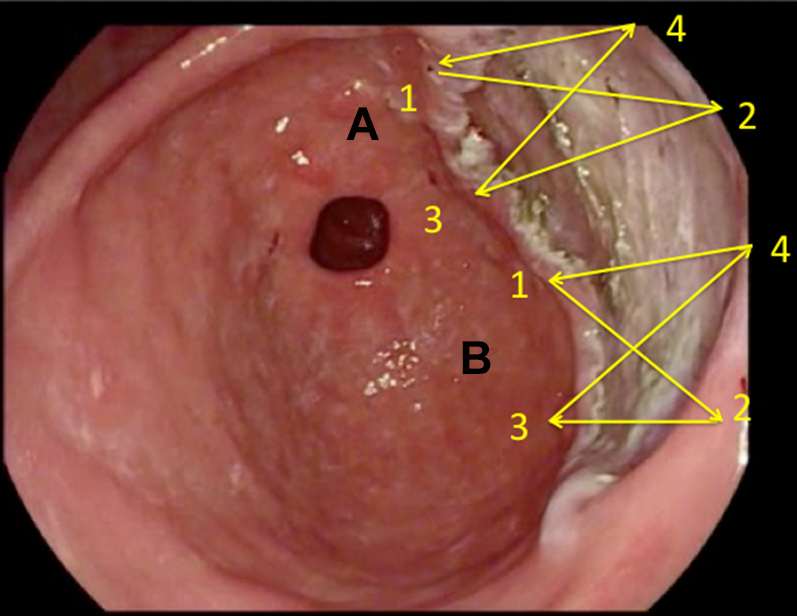
Figure 8 pattern for tissue approximation of a large circular defect.
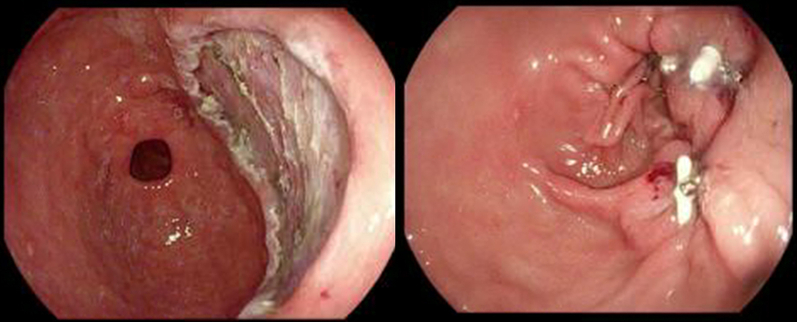
Figure 4.
A 5- × 3-cm gastric antral mucosal defect postendoscopic submucosal dissection with successful closure with 2 sets of HeliX tacks (Apollo Endosurgery, Austin, Tex, USA).
Figure 5.

Follow-up endoscopic image 2 months after endoscopic submucosal dissection and closure with HeliX tacks (Apollo Endosurgery, Austin, Tex, USA).
Discussion
X-tack has shown promising results in animal models with 100% defect closure with complete healing of the site confirmed by histopathology.9 This device provides mucosal closure in comparison to endoscopic suturing, which facilitates full-thickness closure. In contrast to the endoscopic suturing, this device is through-the-scope and could be used as an effective and convenient tool for tissue approximation and closure for large mucosal defects post-EMR or ESD. Although the lower force of this device would limit its use for closure of full-thickness defects, it facilitates tissue approximation, which is essential especially in challenging locations such as the right side of the colon with limited space. Further complete closure can be achieved with additional devices such as TTSCs.
Most recently, Zhang et al demonstrated post-EMR closure defects in a small case series.10 However, the lesions were 15 to 20 mm in diameter. According to a recent multicenter study of 93 patients, technical success of the HeliX tacking system for intended use was 90.0%, 92.3% and 86.3% in lesions <20, 20 to 30, and >30 mm in diameter, respectively.11
Although the ideal closure pattern has not yet been studied, similar to Zhang et al’s observation, we also favored a z-pattern (zig-zag) placement of HeliX tacks for linear- and crescent-shaped defects and a figure 8 pattern for circular defects. It is essential to apply enough tension over the suture for tack approximation before cinching without breaking the suture. Our observation suggests that placement of tacks on the opposite sides of a large defect, not too far from each other (approximately 1 cm), allows for ideal tissue approximation. Based on our experience, more forceful tension over the suture could be applied via a figure 8 pattern and is more ideal within the stomach mucosa or fibrotic defects in fixed locations. In comparison, optimal apposition of the 2 edges of the larger defects (larger than 50 mm) or crescent shaped over folds, could be achieved via z-pattern or running suture pattern.
Our 2 cases highlight the HeliX tacking system as a safe and effective method for tissue approximation, especially for challenging post-EMR and post-ESD defects larger than 40 mm.
Disclosure
Dr Othman is a consultant for Olympus, Boston Scientific Corporation, AbbVie, ConMed, Lumendi, and Apollo Endosurgery. Dr Jawaid is a consultant for ConMed and Lumendi. Dr Keihanian disclosed no financial relationships.
Supplementary data
Endoscopic tacking for tissue approximation of very large EMR defects.
References
- 1.Ortiz O., Rex D.K., Grimm I.S., et al. Factors associated with complete clip closure after endoscopic mucosal resection of large colorectal polyps. Endoscopy. Epub 2020 April 20 doi: 10.1055/a-1332-6727. [DOI] [PubMed] [Google Scholar]
- 2.Albéniz E., Álvarez M.A., Espinós J.C., et al. Clip closure after resection of large colorectal lesions with substantial risk of bleeding. Gastroenterology. 2019;157:1213–1221.e4. doi: 10.1053/j.gastro.2019.07.037. [DOI] [PubMed] [Google Scholar]
- 3.Mangiavillano B., Viaggi P., Masci E. Endoscopic closure of acute iatrogenic perforations during diagnostic and therapeutic endoscopy in the gastrointestinal tract using metallic clips: a literature review. J Dig Dis. 2010;11:12–18. doi: 10.1111/j.1751-2980.2009.00414.x. [DOI] [PubMed] [Google Scholar]
- 4.Bartell N., Bittner K., Kaul V., et al. Clinical efficacy of the over-the-scope clip device: a systematic review. World J Gastroenterol. 2020;26:3495–3516. doi: 10.3748/wjg.v26.i24.3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nishiyama N., Mori H., Kobara H., et al. Efficacy and safety of over-the-scope clip: including complications after endoscopic submucosal dissection. World J Gastroenterol. 2013;19:2752–2760. doi: 10.3748/wjg.v19.i18.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hagel A.F., Naegel A., Lindner A.S., et al. Over-the-scope clip application yields a high rate of closure in gastrointestinal perforations and may reduce emergency surgery. J Gastrointest Surg. 2012;16:2132–2138. doi: 10.1007/s11605-012-1983-6. [DOI] [PubMed] [Google Scholar]
- 7.Kantsevoy S.V., Bitner M., Mitrakov A.A., et al. Endoscopic suturing closure of large mucosal defects after endoscopic submucosal dissection is technically feasible, fast, and eliminates the need for hospitalization (with videos) Gastrointest Endosc. 2014;79:503–507. doi: 10.1016/j.gie.2013.10.051. [DOI] [PubMed] [Google Scholar]
- 8.Kantsevoy S.V., Bitner M., Hajiyeva G., et al. Endoscopic management of colonic perforations: clips versus suturing closure (with videos) Gastrointest Endosc. 2016;84:487–493. doi: 10.1016/j.gie.2015.08.074. [DOI] [PubMed] [Google Scholar]
- 9.Hernandez A., Marya N.B., Sawas T., et al. Gastrointestinal defect closure using a novel through-the-scope HeliX tack and suture device compared to endoscopic clips in a survival porcine model (with video) Endosc Int Open. 2021;9:E572–E577. doi: 10.1055/a-1370-9256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang L.Y., Bejjani M., Ghandour B., et al. Endoscopic through-the-scope suturing. VideoGIE. 2021;7:46–51. doi: 10.1016/j.vgie.2021.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahmoud T., Wong Kee, Song L.M., Stavropoulos S.N., et al. Initial multicenter experience using a novel endoscopic tack and suture system for challenging GI defect closure and stent fixation (with video) Gastrointest Endosc. 2022;95:373–382. doi: 10.1016/j.gie.2021.10.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic tacking for tissue approximation of very large EMR defects.
Endoscopic tacking for tissue approximation of very large EMR defects.