Abstract
Introduction
Using data from the TackSHS survey, we aim to provide updated estimates on the prevalence and determinants of overweight and obesity in Europe.
Methods
A face-to-face survey was conducted in 2017–2018 in 12 European countries (Bulgaria, England, France, Germany, Greece, Ireland, Italy, Latvia, Poland, Portugal, Romania, and Spain). Overall, 10,810 participants, representative in each country of the general adult population, provided information on self-reported height and weight.
Results
Almost half of participants (48.1%; 95% confidence interval, CI: 47.2–49.1) reported to be overweight or obese (54.1% in men and 42.5% in women) and 12.6% (95% CI: 12.0–13.2) obese (11.3% in men and 13.8% in women). Obesity prevalence was lowest in Italy (7.5%) and France (8.8%) and highest in Greece (19.7%) and Romania (21.1%). Multilevel logistic random-effects analyses showed that prevalence of obesity was related with higher age and lower level of education and socioeconomic status. As compared to northern European countries, Western and Southern European ones showed a significantly lower obesity prevalence. When compared to a companion study conducted in 2010, Eastern and Northern European countries showed an increased trend in obesity prevalence. Conversely, countries with the lowest obesity prevalence (less than 10%), such as Italy and France, showed a decreased trend.
Conclusions
Despite a large heterogeneity across countries, overweight and obesity prevalence estimates in Europe are alarming, with most of the countries reporting obesity prevalence approaching 20% or more, particularly in Eastern and Northern Europe. Since 2010, obesity prevalence increased in most of these countries.
Keywords: Overweight, Obesity, Body mass index, Cross-sectional study, Pan-European survey
Introduction
Obesity is one of the major public health concerns of the 21st century and its prevalence has tripled in many high-income countries, including most of the World Health Organization (WHO) European Region, since the 1980s [1]. Today approximately 40% of the global adult population is considered as overweight or obese [2, 3]. This high prevalence is of concern, because obesity is a chronic complex multifactorial disease that affects nearly all physiological functions of the human body, increasing the risk of depression and other mental health conditions and being a preventable risk factor for several non-communicable diseases, including type 2 diabetes, dyslipidaemia, cardiovascular diseases, several types of cancers, and musculoskeletal disorders [4, 5]. A meta-analysis based on 239 prospective studies showed that, all-cause mortality substantially increased with increasing body mass index (BMI): compared with normal weight, the hazard ratios were 1.11 (95% confidence interval, CI: 1.10–1.11) for overweight and 1.64 (95% CI: 1.61–1.67) for obesity [6].
It has been observed that the number of global deaths and disability-adjusted life years attributable to high BMI has substantially increased between 1990 and 2017 [5]. In addition, the direct cost of treatment of obesity-induced diseases in adults in Europe has been estimated at above 7% of total healthcare costs, comparable to the costs associated with the treatment of neoplastic diseases [3].
Recent forecasts have estimated that obesity prevalence is expected to grow globally reaching maximum levels between 2026 and 2054, with highest levels in the United States of America (USA) and the United Kingdom (UK), followed by other European countries [7, 8]. Another forecast showed that the prevalence of obesity across Europe is expected to continue rising up to 2025 [8]. These projections indicate that Member States in the WHO European Region are unlikely to meet the global obesity target to halt obesity at 2010 levels by 2025, prefixed during the World Health Assembly in 2013 [8, 9, 10].
Many European countries periodically monitor the prevalence of obesity and overweight through local and national surveys. However, the different methodologies can lead to biased comparisons [8, 11]. In Europe, it has been assessed that even within specific countries, obesity estimates can vary by as much as 8% according to the survey method used [8, 11, 12]. Due to this considerable disparity, rigorous pan-European studies should be conducted to assure the reliability of comparisons and provide up-to-date information about levels and trends in overweight and obesity prevalence. These surveys represent an essential instrument to monitor the relentless increase in the obesity trend [7, 10, 13] and quantify the effects of primary prevention programmes using a population approach, aimed not only at protecting susceptible individuals but, more importantly, at identifying the underlying determinants of obesity incidence [14]. In order to perform a comprehensive assessment of prevalence of overweight and obesity in Europe, we used data from the TackSHS survey, conducted on nationally representative samples of the adult population from 12 European countries with identical protocol and comparable sampling methodology conducted in the same calendar period (2017–2018).
Methods
Within the TackSHS project (Tackling second-hand tobacco smoke and electronic cigarette emissions: exposure assessment, novel interventions, impact on lung diseases, and economic burden in diverse European populations) [15], a pan-European survey was conducted in 12 selected countries (Bulgaria, England, France, Germany, Greece, Ireland, Italy, Latvia, Poland, Portugal, Romania, and Spain), representative of the variability in geography, legislation, and culture across the European Union (EU) and covering approximately the 80% of the whole EU-28 population (at the time of the survey). The fieldwork was conducted by DOXA, the Italian branch of the Worldwide Independent Network/Gallup International Association, and its European partners [16]. This study followed the STROBE checklist for cross-sectional studies [17].
In each country, a sample of around 1,000 individuals aged 15 years and more (in England ≥16 years and in Ireland ≥18 years) was interviewed; each sample was representative of the general population in terms of age, sex, area of residence, and − in most of the countries − socioeconomic characteristics. Sampling methodology differed by country: in Bulgaria, Greece, Italy, Latvia, and Romania, a multi-stage sampling was applied with participants randomly selected to be representative of their population in terms of sex, age, and geographic area (in Italy also by socioeconomic status); in Germany, Ireland, Poland, Portugal, and Spain, stratified random sampling was applied, using also quotas on sex and age (in Ireland also social class); in England, cluster sampling was used with quotas on age, sex, socioeconomic status, region, urban/rural dwelling; in France, quotas on age, sex, region, and city size were applied. Further survey details are reported elsewhere [16].
Overall, participation rate was on average 57%, ranging between 38% (in Greece) and 80% (in Spain) and the final sample included 11,902 subjects, representative of the 342 million people aged 15 years or more of the 12 countries. Overall, 6% did not provide information on weight (from 0% in Italy to 24% in Ireland) and 3% on height (from 0% in Bulgaria, Italy, and Portugal to 20% in Ireland). 10,810 subjects aged ≥18 years with available information on self-reported height and weight were considered in the present investigation.
Trained interviewers conducted the survey with a computer-assisted personal interviewing method in the 12 countries. The pilot fieldwork was conducted on 1,059 participants in November 2016 in Italy. In the other 11 countries, data were collected between June 2017 (in Romania) and October 2018 (in Latvia).
Study approval was obtained in every country from a local Ethics Committee. The interviewers provided details of the survey to all participants and all participants provided informed consent. The study protocol was registered at ClinicalTrials.gov (ID: NCT02928536).
Dependent Variables
Participants were asked to report their height and weight at the moment of the interview. BMI was computed as the ratio between self-reported weight (kg) and height (m2). BMI was categorized into four groups, according to the standard classification by the WHO [18], i.e., underweight (BMI <18.5 kg/m2), normal weight (BMI between 18.5 and 24.9 kg/m2), overweight (BMI between 25.0 and 29.9 kg/m2), and obesity (BMI ≥30.0 kg/m2). We then categorized obesity into three classes, according to its severity (I class obesity: BMI between 30.0 and 34.9 kg/m2; II class obesity: BMI between 35.0 and 39.9 kg/m2; and III class obesity: BMI ≥40.0 kg/m2).
Independent Variables
The questionnaire included information on demographic (e.g., sex and age), socioeconomic characteristics, e.g., level of education and self-assessment of household family economic status. The latter question was relative to the country-specific population (“Much higher than average in your country”; “Quite higher than average in your country”; “As the average”; “Quite lower than average”; “Much lower than average”). Another section referred to smoking status: never smokers were defined as participants who had never smoked or had smoked less than 100 cigarettes in their lifetime. Ever smokers were the participants who reported smoking at least 100 cigarettes (including hand-rolled cigarettes) during their lifetime. Among them, current smokers were subjects who reported smoking at the time of the survey, while ex-smokers were those who had quit by the time of the interview. Countries were categorized by geographic area according to the classification by the United Nations into Northern (England, Ireland, and Latvia), Western (France and Germany), Southern (Italy, Greece, Portugal, and Spain), and Eastern regions (Bulgaria, Poland, and Romania) [19].
Statistical Analysis
With a sample size of 1,000 subjects (i.e., approximately the sample size of each country), assuming a prevalence of obesity of 16% [7, 10, 13], we obtain estimates with a standard error of 1.16%. When considering the overall sample size of the 12 countries combined, the standard error reduces to 0.35%.
In each country, statistical weights were applied. DOXA and its European partners used these “individual weights” as an integral part of the process of the sampling methodology to assure that the sample distribution reflected the distribution of the adult population of each country in terms of age, sex, and geographic area. Data from the corresponding National Institute of Statistics were used as the standard. Estimates for the entire sample were assessed using “country weights,” combining “individual weights” with an added weighting factor, each country contributing in proportion to its population aged 15 years or over, in agreement with Eurostat 2018 [20]. In a sensitivity analysis, the prevalence rates of overweight and obesity were further standardised by age, using the direct method using the EU-28 population as reference.
χ2 tests were used to compare non-continuous variables. To take into account the heterogeneity among the 12 selected countries, odds ratios (ORs) and their 95% CI for obesity versus non-obesity were calculated with multilevel logistic random-effects models. The study country effects were considered as random intercepts, whereas sex, age, level of education, and smoking status were considered as variables for adjustment. Country weights were used in all logistic regression models.
In order to derive trends in obesity prevalence, we compared our estimates with those from a companion study conducted within the PPACTE project in 2010 in 16 European countries, using the same methodology as the TackSHS survey [11]. Trends in obesity prevalence were obtained from the 9 common countries with the TackSHS survey: Bulgaria, England, France, Ireland, Italy, Latvia, Poland, Romania, and Spain [11]. Prevalence estimates for the overall population were computed weighting each country in proportion to the country-specific adult population. The same overall and country-specific obesity trend analyses were repeated for current smokers and non-smokers. All the analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA).
Results
Table 1 shows the distribution of 10,810 European adults in the 12 countries in 2017–2018, according to selected self-reported anthropometric characteristics. The mean height was 170.4 cm (176.7 cm in men, 164.6 cm in women), mean weight was 73.7 kg (80.3 kg in men, 67.5 kg in women), and mean BMI was 25.3 kg/m2 (25.7 kg/m2 in men, 25.0 kg/m2 in women). Overall, 2.9% (95% CI: 2.6–3.2) of the European adult population was underweight (1.4%, 95% CI: 1.1–1.7 of men, 4.4%, 95% CI: 3.8–4.9 of women), 49.0% (95% CI: 48.0–49.9) had normal weight (44.5%, 95% CI: 43.2–45.8 of men, 53.1%, 95% CI: 51.8–54.4 of women), 35.6% (95% CI: 34.7–36.5) was overweight (42.8%, 95% CI: 41.5–44.2 of men, 28.8%, 95% CI: 27.6–29.9 of women), and 12.6% (95% CI: 12.0–13.2) was obese (11.3%, 95% CI: 10.5–12.2 of men, 13.8%, 95% CI: 12.9–14.7 of women). In general, 9.5% (95% CI: 9.0–10.1) of the European adult population had I class obesity, 2.2% (95% CI: 2.0–2.5) had II class, and 0.8% (95% CI: 0.7–1.0) had III class obesity. Overweight (excluding obesity) was more prevalent among men than women (p < 0.001) and obesity among women than men (p < 0.001).
Table 1.
Mean values for weight, height, and BMI for 10,810 European subjects aged 18 years or more and percent prevalence according to levels of BMI and corresponding 95% CI, overall and by sexa − The TackSHS survey, 2017–2018
| Characteristics | Total | Sex | |
|---|---|---|---|
| men | women | ||
| Subjectsb, n | 10,810 | 5,163 | 5,647 |
| Height, mean ± SD, cm | 170.4±9.3 | 176.7±7.4* | 164.6±6.7* |
| Weight, mean ± SD, kg | 73.7±15.1 | 80.3±13.5* | 67.5±13.8* |
| BMI, mean ± SD, kg/m2 | 25.3±4.9 | 25.7±4.5* | 25.0±5.2* |
| BMI, % (95% CI) | |||
| Underweight (BMI <18.5) | 2.9 (2.6–3.2) | 1.4 (1.1–1.7) | 4.4 (3.8–4.9) |
| Normal weight (18.5 ≤ BMI <25.0) | 49.0 (48.0–49.9) | 44.5 (43.2–45.8) | 53.1 (51.8–54.4) |
| Overweight (25.0 ≤ BMI <30.0) | 35.6 (34.7–36.5) | 42.8 (41.5–44.2) | 28.8 (27.6–29.9) |
| Obesity (BMI ≥30.0) | 12.6 (12.0–13.2) | 11.3 (10.5–12.2) | 13.8 (12.9–14.7) |
| I class (30.0 ≤ BMI <35.0) | 9.5 (9.0–10.1) | 9.0 (8.2–9.8) | 10.0 (9.2–10.8) |
| II class (35.0 ≤ BMI <40.0) | 2.2 (2.0–2.5) | 1.8 (1.4–2.1) | 2.7 (2.2–3.1) |
| III class (BMI ≥40.0) | 0.8 (0.7–1.0) | 0.5 (0.3–0.7) | 1.1 (0.9–1.4) |
CI, confidence interval; SD, standard deviation. *Comparison between sexes: p < 0.001. a Country weights were used, combining individual weights with an additional weighting factor, with each country contributing in proportion to its population aged 15 years or over (from Eurostat) [19]. b Raw numbers.
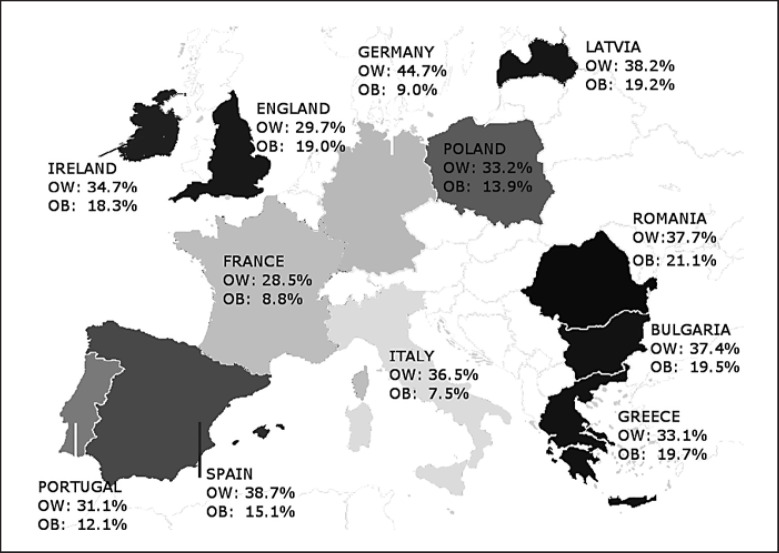
Figure 1 shows the percent prevalence distribution of overweight and obesity in the 12 European countries. Highest prevalence of overweight and obesity was observed in Romania (58.8%, 95% CI: 55.6–61.9), Latvia (57.3%, 95% CI: 54.1–60.6), and Bulgaria (56.9%, 95% CI: 53.8–59.9) and lowest one in France (37.3%, 95% CI: 34.3–40.3), Portugal (43.3%, 95% CI: 40.1–46.4), and Italy (44.0%, 95% CI: 40.9–47.0). Highest prevalence of obesity was found in Romania (21.1%, 95% CI: 18.5–23.7), Greece (19.7%, 95% CI: 17.1–22.3), and Bulgaria (19.5%, 95% CI: 17.1–22.0) and the lowest in Italy (7.5%, 95% CI: 5.9–9.1), France (8.8%, 95% CI: 7.0–10.6), and Germany (9.0%, 95% CI: 7.1–10.9).
Fig. 1.
Percent prevalence of overweight (OW; body mass index, BMI, between 25.0 and 29.9 kg/m2) and obesity (OB; BMI ≥30 kg/m2) among adults from 12 European countries. Countries are coloured according to obesity prevalence (light grey means relatively low prevalence; dark grey means relatively high prevalence). The TackSHS survey, 2017–2018.
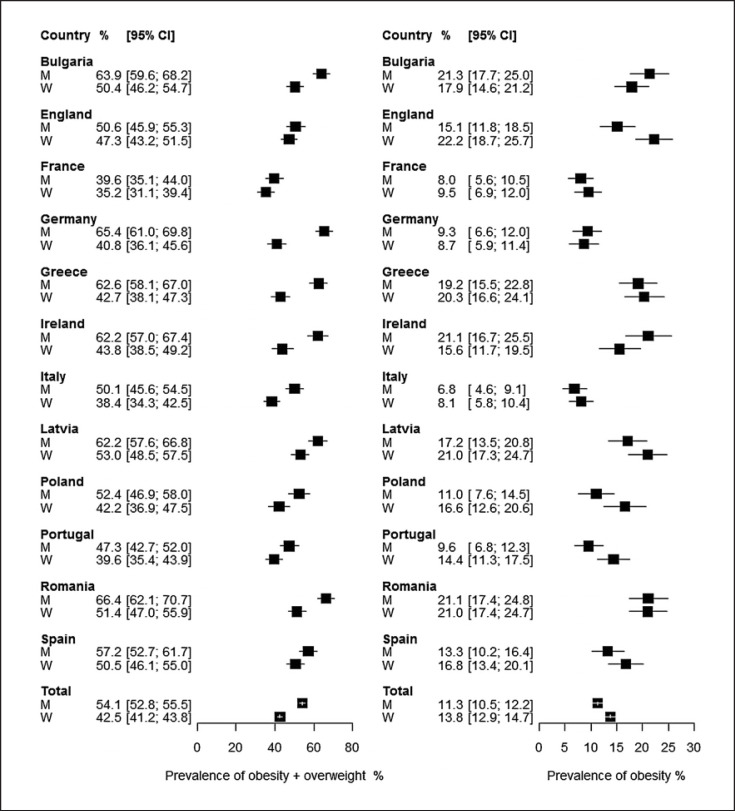
Figure 2 shows the percent prevalence and 95% CI of overweight/obesity and obesity by sex, overall and in each country. Table 2 further shows the age-standardized prevalence estimates of overweight/obesity and obesity. For both sexes, the standardization did not substantially change our results except in case of Greece, where both overweight/obesity and obesity rates estimated differed more: from 62.6% (95% CI: 58.1–67.0) to 51.9% (95% CI: 47.3–56.5) in men and from 42.7% (95% CI: 38.1–47.3) to 36.1% (95% CI: 31.6–40.6) in women for obesity/overweight; from 19.2% (95% CI: 15.5–22.8) to 16.8% (95% CI: 13.4–20.2) in men and from 20.3% (95% CI: 16.6–24.1) to 17.2% (95% CI: 13.7–20.7) in women for obesity.
Fig. 2.
Percent prevalence and 95% confidence interval (CI) of overweight/obesity (body mass index, BMI ≥25 kg/m2) and obesity (BMI ≥30 kg/m2), overall and by country, in men (M) and women (W) from 12 European countries. Prevalence estimates for the overall population were computed weighting each country in proportion to the country-specific adult population. The TackSHS survey, 2017–2018.
Table 2.
Crude and age-standardized percent prevalencea and 95% CI of overweight/obesity (BMI ≥25 kg/m2) and obesity (BMI ≥30 kg/m2), overall and by country − The TackSHS survey, 2017–2018
| Country | Sample characteristics | Prevalence (%) of overweight/obesity (95% CI) | Prevalence (%) of obesity (95% CI) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| age range, years |
mean age, years |
N c | men | women | men | women | ||||||
| men | women | crude | age-standardized | crude | age-standardized | crude | age-standardized | crude | age-standardized | |||
| Allb | ≥18 | 47 | 5,163 | 5,647 | 54.1 (52.8–55.5) | 53.8 (52.4–55.2) | 42.5 (41.2–43.8) | 43.0 (41.7–44.3) | 11.3 (10.5–12.2) | 11.2 (10.3–12.1) | 13.8 (12.9–14.7) | 13.8 (12.9–14.7) |
| Bulgaria | ≥18 | 49 | 476 | 524 | 63.9 (59.6–68.2) | 61.3 (56.9–65.7) | 50.4 (46.2–54.7) | 46.9 (42.6–51.2) | 21.3 (17.7–25.0) | 20.1 (16.5–23.7) | 17.9 (14.6–21.2) | 16.6 (13.4–19.8) |
| England | ≥18 | 43 | 437 | 545 | 50.6 (45.9–55.3) | 51.5 (46.8–56.2) | 47.3 (43.2–51.5) | 46.8 (42.6–51.0) | 15.1 (11.8–18.5) | 14.3 (11.0–17.6) | 22.2 (18.7–25.7) | 22.6 (19.1–26.1) |
| France | ≥18 | 47 | 460 | 508 | 39.6 (35.1–44.0) | 40.4 (35.9–44.9) | 35.2 (31.1–39.4) | 36.0 (31.8–40.2) | 8.0 (5.6–10.5) | 8.3 (5.8–10.8) | 9.5 (6.9–12.0) | 10.1 (7.5–12.7) |
| Germany | ≥18 | 50 | 426 | 448 | 65.4 (61.0–69.8) | 64.3 (59.8–68.8) | 40.8 (36.1–45.6) | 38.6 (34.1–43.1) | 9.3 (6.6–12.0) | 9.0 (6.3–11.7) | 8.7 (5.9–11.4) | 8.4 (5.8–11.0) |
| Greece | 18–64 | 41 | 454 | 438 | 62.6 (58.1–67.0) | 51.9 (47.3–56.5) | 42.7 (38.1–47.3) | 36.1 (31.6–40.6) | 19.2 (15.5–22.8) | 16.8 (13.4–20.2) | 20.3 (16.6–24.1) | 17.2 (13.7–20.7) |
| Ireland | ≥18 | 46 | 347 | 343 | 62.2 (57.0–67.4) | 62.4 (57.3–67.5) | 43.8 (38.5–49.2) | 44.3 (39.0–49.6) | 21.1 (16.7–25.5) | 21.4 (17.1–25.7) | 15.6 (11.7–19.5) | 15.8 (11.9–19.7) |
| Italy | ≥18 | 50 | 482 | 513 | 50.1 (45.6–54.5) | 47.9 (43.4–52.4) | 38.4 (34.3–42.5) | 37.0 (32.8–41.2) | 6.8 (4.6–9.1) | 6.4 (4.2–8.6) | 8.1 (5.8–10.4) | 7.7 (5.4–10.0) |
| Latvia | 18–74 | 46 | 454 | 433 | 62.2 (57.6–66.8) | 61.7 (57.2–66.2) | 53.0 (48.5–57.5) | 56.3 (51.6–61.0) | 17.2 (13.5–20.8) | 16.8 (13.4–20.2) | 21.0 (17.3–24.7) | 21.7 (17.8–25.6) |
| Poland | ≥18 | 45 | 268 | 384 | 52.4 (46.9–58.0) | 52.5 (46.5–58.5) | 42.2 (36.9–47.5) | 45.6 (40.6–50.6) | 11.0 (7.6–14.5) | 11.9 (8.0–15.8) | 16.6 (12.6–20.6) | 18.0 (14.2–21.8) |
| Portugal | ≥18 | 49 | 450 | 507 | 47.3 (42.7–52.0) | 46.0 (41.4–50.6) | 39.6 (35.4–43.9) | 40.5 (36.2–44.8) | 9.6 (6.8–12.3) | 9.4 (6.7–12.1) | 14.4 (11.3–17.5) | 14.2 (11.2–17.2) |
| Romania | ≥18 | 48 | 439 | 517 | 66.4 (62.1–70.7) | 63.4 (58.9–67.9) | 51.4 (47.0–55.9) | 50.3 (46.0–54.6) | 21.1 (17.4–24.8) | 20.1 (16.4–23.8) | 21.0 (17.4–24.7) | 20.1 (16.6–23.6) |
| Spain | ≥18 | 48 | 470 | 487 | 57.2 (52.7–61.7) | 56.5 (52.0–61.0) | 50.5 (46.1–55.0) | 50.8 (46.4–55.2) | 13.3 (10.2–16.4) | 13.1 (10.0–16.2) | 16.8 (13.4–20.1) | 17.1 (13.8–20.4) |
a Estimates are standardized by age, using the direct method with the population of the EU-28 as the reference population. b Prevalence estimates for the overall population were computed weighting each country in proportion to the country-specific adult population.c Raw numbers.
Table 3 shows the ORs for obesity versus non-obesity according to selected individual-level characteristics and geographic area. Women were more likely to be obese than men (OR = 1.23; 95% CI: 1.09–1.39). Obesity prevalence increased with older age (p for trend < 0.001) and with lower level of education (p for trend < 0.001) and socioeconomic status (p for trend = 0.002). When compared to never smokers, current smokers were less frequently obese (OR = 0.85; 95% CI: 0.73–0.99) whereas ex-smokers were more frequently obese (OR = 1.41; 95% CI: 1.22–1.64). Compared to adults from Northern Europe, people from Western Europe (OR = 0.39, 95% CI: 0.24–0.62) and Southern Europe (OR = 0.51, 95% CI: 0.31–0.82) were significantly less obese. The OR estimates for most determinants were rather consistent in both men and women. Obesity was more frequently reported with increasing age in both men and women (p for trend < 0.001). An increase in obesity was observed with decreasing level of education (p for trend = 0.001) and socioeconomic status in females (p for trend = 0.001) but not in males. Considering smoking status, male current smokers (OR = 0.76; 95% CI 0.61–0.95), but not female current smokers, were less likely to be obese compared to never smokers. Ex-smokers were more frequently obese compared to never smokers both in males (OR = 1.39; 95% CI: 1.12–1.71) and in females (OR = 1.40; 95% CI: 1.14–1.73).
Table 3.
Percent prevalencea of obesity (BMI ≥30 kg/m2) and odds ratios (OR)b for obesity (BMI ≥30 kg/m2) versus non-obesity (BMI <30 kg/m2) with corresponding 95% CI according to selected individual-level characteristics and geographic area, overall and by sex − The TackSHS survey, 2017–2018
| Characteristics | Total | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N c | obesity prevalence, % | OR (95% CI) | N c | obesity prevalence, % | OR (95% CI) | N c | obesity prevalence, % | OR (95% CI) | |
| Total | 10,810 | 12.6 | − | 5,163 | 11.3 | − | 5,647 | 13.8 | − |
| Sex | |||||||||
| Men | 5,163 | 11.3 | 1d | − | − | − | − | − | − |
| Women | 5,647 | 13.8 | 1.23 (1.09–1.39) | − | − | − | − | − | − |
| Age, years | |||||||||
| <25 | 1,001 | 5.1 | 1d | 536 | 4.9 | 1d | 465 | 5.3 | 1d |
| 25–44 | 3,851 | 10.3 | 2.02 (1.51–2.70) | 1,835 | 8.1 | 1.64 (1.09–2.47) | 2,016 | 12.3 | 2.41 (1.59–3.64) |
| 45–64 | 4,042 | 14.9 | 3.10 (2.33–4.13) | 1,856 | 14.5 | 3.11 (2.08–4.64) | 2,186 | 15.3 | 3.14 (2.08–4.73) |
| ≥65 | 1,916 | 16.4 | 3.41 (2.52–4.62) | 936 | 15.2 | 3.14 (2.05–4.83) | 980 | 17.4 | 3.66 (2.38–5.63) |
| p for trend | <0.001 | <0.001 | <0.001 | ||||||
| Level of educatione | |||||||||
| High | 3,063 | 11.2 | 1d | 1,382 | 10.0 | 1d | 1,681 | 12.3 | 1d |
| Intermediate | 3,813 | 10.3 | 0.97 (0.82–1.14) | 1,864 | 9.9 | 1.05 (0.83–1.34) | 1,949 | 10.7 | 0.91 (0.73–1.13) |
| Low | 3,933 | 15.7 | 1.31 (1.13–1.53) | 1,916 | 13.6 | 1.23 (0.98–1.54) | 2,017 | 17.5 | 1.38 (1.12–1.70) |
| p for trend | <0.001 | 0.069 | 0.001 | ||||||
| Socioeconomic statusf | |||||||||
| High | 1,459 | 11.0 | 1d | 746 | 10.2 | 1d | 713 | 11.9 | 1d |
| Average | 5,667 | 12.9 | 1.23 (1.02–1.49) | 2,695 | 11.9 | 1.20 (0.90–1.59) | 2,972 | 13.9 | 1.24 (0.95–1.62) |
| Low | 2,727 | 16.0 | 1.42 (1.14–1.76) | 1,246 | 13.0 | 1.21 (0.87–1.69) | 1,481 | 18.4 | 1.57 (1.17–2.10) |
| p for trend | 0.002 | 0.307 | 0.001 | ||||||
| Smoking status | |||||||||
| Never smoker | 5,726 | 12.1 | 1d | 2,272 | 10.6 | 1d | 3,454 | 13.1 | 1d |
| Current smoker | 3,146 | 10.2 | 0.85 (0.73–0.99) | 1,743 | 8.5 | 0.76 (0.61–0.95) | 1,403 | 12.4 | 0.93 (0.76–1.14) |
| Ex-smoker | 1,938 | 17.9 | 1.41 (1.22–1.64) | 1,148 | 17.2 | 1.39 (1.12–1.71) | 790 | 18.9 | 1.40 (1.14–1.73) |
| Geographic areag | |||||||||
| Northern Europe | 2,559 | 19.0 | 1d | 1,238 | 15.5 | 1d | 1,321 | 21.8 | 1d |
| Western Europe | 1,842 | 8.9 | 0.39 (0.24–0.62) | 886 | 8.8 | 0.48 (0.28–0.81) | 956 | 9.0 | 0.34 (0.21–0.53) |
| Southern Europe | 3,801 | 11.5 | 0.51 (0.31–0.82) | 1,856 | 10.4 | 0.56 (0.33–0.96) | 1,945 | 12.6 | 0.48 (0.30–0.77) |
| Eastern Europe | 2,608 | 16.8 | 0.80 (0.48–1.35) | 1,183 | 15.4 | 0.88 (0.49–1.59) | 1,425 | 18.1 | 0.76 (0.46–1.26) |
aPrevalence estimates were computed weighting each country in proportion to the country-specific adult population. bORs were estimated using multilevel logistic regression models after adjustment for age, level of education, and smoking status and with country as random effect; ORs for the total population were further adjusted for sex. Estimates were weighted for statistical weights that consider country-specific adult population. Figures in bold type are significant at 0.05.c Raw numbers.d Reference category. eThe sum does not add up to the total because of a few missing values. fSelf-assessment of household (family) economic status relative to the country-specific population. This information was missing for Germany. 9Countries were categorized by geographic area according to the classification by the United Nations into Northern (England, Ireland, and Latvia), Western (France and Germany), Southern (Italy, Greece, Portugal, and Spain), and Eastern regions (Bulgaria, Poland, and Romania) [18].
When we compared our estimates of obesity and overweight/obesity prevalence with those from 2010, we found an overall decrease of 0.3% in overweight prevalence, an overall increase of 2.3% in obesity prevalence with the majority of countries showing an increase in obesity prevalence. The rise in obesity prevalence was observed in six out of nine countries, with highest values in Bulgaria (+57.5), in Ireland (+50.3%), and Poland (+35.2%). Countries with lowest obesity prevalence (less than 10%), such as Italy and France, showed a decreased trend (Table 4). Online supplementary Table 1 (for all online suppl. material, see www.karger.com/doi/10.1159/000525792) shows the country-specific obesity trend analyses for current smokers and non-smokers. Trend estimates revealed a systematic more marked increase in obesity prevalence among current smokers.
Table 4.
Percent prevalence of overweight/obesity (BMI ≥25 kg/m2) and obesity (BMI ≥30 kg/m2), by country, in 2010 (PPACTE study) and 2017–2018 (TackSHS survey)
| Country | Overweight/obesity | Obesity | ||||
|---|---|---|---|---|---|---|
| 2010 PPACTE | 2017–18 TackSHS | Δ, % | 2010 PPACTE | 2017–18 TackSHS | Δ, % | |
| Bulgaria | 48.4 | 56.9 | + 17.5 | 12.4 | 19.5 | +57.5 |
| England | 56.0 | 48.8 | −12.9 | 20.1 | 19.0 | −5.3 |
| France | 41.7 | 37.3 | −10.6 | 12.2 | 8.8 | −28.0 |
| Ireland | 46.9 | 53.0 | + 13.0 | 12.2 | 18.3 | +50.3 |
| Italy | 38.5 | 44.0 | + 14.3 | 7.6 | 7.5 | −1.4 |
| Latvia | 51.6 | 57.3 | +11.0 | 16.2 | 19.2 | +18.5 |
| Poland | 47.8 | 47.1 | −1.4 | 10.3 | 13.9 | +35.2 |
| Romania | 48.8 | 58.8 | +20.5 | 16.0 | 21.1 | +31.6 |
| Spain | 53.2 | 53.8 | +1.1 | 14.0 | 15.1 | +7.6 |
| Total | 47.0 | 46.8 | −0.3 | 13.0 | 13.3 | +2.3 |
Prevalence estimates for the overall population were computed weighting each country in proportion to the country-specific adult population.
Discussion
In this comprehensive evaluation of overweight and obesity among European adults, obesity prevalence was 13% in 2017–2018, with higher rates in women, older adults, and those with a lower socioeconomic status. We also observed a large variability across countries, with obesity prevalence ranging between 8% in Italy and 21% in Romania. Overall, approximately half of the adult European population was overweight or obese.
Our results are in line with recent European estimates, showing that approximately 53% of the adult population is overweight or obese [10, 13]. We found that Eastern and Northern European countries showed higher obesity rates in comparison with other countries. This is in line with previous data from other multi-country surveys from Europe conducted between 2010 and 2019 [3, 11, 13, 21]. Among the possible reasons why Eastern Europe presents higher prevalence of obesity rates, there is the lower economic growth level, and consequent lower socioeconomic status and level of education, compared to more developed countries with higher per capita incomes [22, 23]. In our study, low socioeconomic status and poor level of education are significantly related to higher overweight and obesity prevalence. Household and individual-level low income, in fact, leads to greater difficulties in providing proper access to healthy food (particularly with regular intake of fresh and seasonable vegetables and fruit) and active and healthy lifestyle. Moreover, people with low income, health literacy, and health education have limited access to sports facilities, possibly living in areas where non-occupational physical activity is hardly promoted [3].
The relatively low obesity prevalence observed in Western/Southern Europe, in particular in Italy and France, might be explained by the distinctive dietary habits of their population and the adherence to the Mediterranean diet [11, 12, 24, 25] that has been proved to be effective in obesity control [26]. In general, the Mediterranean diet refers to some common dietary characteristics including seasonal vegetables and fruits, unrefined cereals, nuts, seeds, legumes, and extra virgin olive oil as primary source of added fat. Furthermore, this pattern implies a moderate intake of fish, dairy products, and a lower to mild consumption of meat, eggs, fermented beverages (mostly red wine), and sweets [27]. Although belonging to the Mediterranean basin, Spain and Greece showed higher values of obesity prevalence as compared to Italy and France, as already observed in other surveys [11]. This is likely due to a shift from Mediterranean-type diets to Western-type diets − characterised by a relatively high consumption of meat and dairy products − which has been observed specifically in Spain and Greece [11, 28].
Our European obesity estimates are 3 times lower than those observed in 2017–2018 in the USA (43% obesity prevalence in USA vs. 13% in Europe; 43% vs. 11% in men and 42% vs. 14% in women) [29]. Even the highest obesity rates we observed (21% in Bulgarian, Romanian, and Irish men and 22% in English women) are substantially lower than those from the USA [29].
In order to derive trends in obesity prevalence, we compared our estimates with those from a companion study conducted in 2010 in 9 common countries with the TackSHS survey [11]. Obesity prevalence increased in the majority of the countries, particularly in Eastern and Northern Europe. In contrast, England showed a slight decrease in obesity prevalence since 2010 [11]. However, UK estimates remain alarming. In fact, recent projection data forecasted that obesity rates are going to increase by 2025, the UK becoming the second large country (after US) with the highest obesity prevalence [7]. We also observed a large decrease in obesity prevalence in France. Other studies report a slight increase or a stabilization in obesity prevalence [30]. Due to the known impact of smoking on BMI [31, 32], we also analysed the obesity trends separately in smokers and non-smokers. The observed increases in obesity prevalence appeared to be limited to current smokers.
Our estimates confirm data from other studies showing higher prevalence of obesity in women compared to men [3, 33]; however, a significantly higher prevalence of overweight has been observed in males, in line with current literature from Europe [13]. A higher prevalence of obesity was observed among older compared to younger adults [11, 34]. The rise in life expectancy leads in fact to additional years of vulnerability to chronic conditions, many of them related to obesity. In fact, it has been estimated that age-specific rates of high-BMI-related deaths and disability-adjusted life years increase with increasing age [35].
In Europe, ex-smokers represent another subgroup of population more susceptible to obesity [11, 36]. Even if health benefits of smoking cessation outweigh any adverse effects of post-smoking cessation weight gain [31, 32], programs and policies aimed at helping smokers in quitting should consider, develop, and evaluate new strategies to avoid this subsequent side effect. Pharmacological support to limit possible post-abstinence overweight, monitoring caloric intake, and increasing caloric expenditure are among the possible strategies recommended by international guidelines to manage weight gain [37].
Among the limitations of our study, there is the use of self-reported information on height and weight, which likely resulted in an underestimation of BMI and therefore of the prevalence of overweight and obesity [38, 39]. However, it has been assessed that, particularly in large surveys covering many countries, self-reported height and weight, although varying by sex and country, still represent a valid and economic method to monitor obesity prevalence [40]. Other limitations include those inherent to the cross-sectional study design, which does not allow to assess any causal associations. In addition, that information on height and weight was not available for the entire sample of adults, particularly in Ireland, where a relevant proportion of participants had missing information in these values, and therefore had to be excluded from the analyses, causing a decrease in the available country sample size, and therefore producing less certain results. When comparing baseline characteristics, such as sex, age, level of education, and smoking status, subjects not reporting BMI were significantly different from those reporting BMI data: those not providing data on BMI were more frequently women and middle aged (45–64 years). In addition, despite the overall response rate was relatively high, possible differences occurred between responders and non-responders. Finally, the relatively limited sample size does not allow us to obtain robust estimates when analysing the prevalence of obesity in strata of single countries.
Among the strengths of our study, there is the representativeness of adult population and the possibility to make reliable comparisons across countries, taking advantage of the homogeneity of the methodology used. Moreover, the use of a computer-assisted personal interviewing survey managed by qualified interviewers allowed us to obtain consistent and reliable data [39]. The indirect standardization we applied also creates comparable estimates of results by country and with others.
In conclusion, obesity patterns in Europe, even if substantially more favourable than those in the USA, show that half of the European adult population is overweight and almost one in every eight are obese. Overall, when compared to 2010 data [11], obesity prevalence in Europe has mainly increased in most of the countries. Conversely, only a few countries, with less than 10% of self-reported obesity, including Italy and France, even showed a decreased trend in obesity prevalence since 2010.
Planning and implementing preventive intervention using a population approach, focusing on main causes of incidence of overweight and obesity, is a fundamental instrument to face and halt the ongoing obesity pandemic. Continuous monitoring of prevalence data represents an efficient instrument to measure and quantify impacts of such interventions in experimental but most importantly operational and real-life settings.
The TackSHS Project Investigators
Catalan Institute of Oncology (ICO); Bellvitge Biomedical Research Institute (IDIBELL), Spain: Esteve Fernández, Yolanda Castellano, Marcela Fu, Montse Ballbè, Beladenta Amalia, and Olena Tigova. Public Health Agency of Barcelona (ASPB), Spain: Maria José López, Xavier Continente, Teresa Arechavala, and Elisabet Henderson. Istituto di Ricerche Farmacologiche Mario Negri IRCCS (IRFMN), Italy: Silvano Gallus, Alessandra Lugo, Xiaoqiu Liu, Elisa Borroni, and Chiara Stival. Istituto DOXA, Worldwide Independent Network/Gallup International Association, Italy: Paolo Colombo. University of Stirling (UNISTIR), the UK: Sean Semple, Rachel O'Donnell, and Ruaraidh Dobson. TobaccoFree Research Institute Ireland (TFRI), Ireland: Luke Clancy, Sheila Keogan, and Hannah Byrne. Hellenic Cancer Society: George D. Behrakis Research Laboratory (HCS), Greece: Panagiotis Behrakis, Anna Tzortzi, Constantine Vardavas, Vergina Konstantina Vyzikidou, Gerasimos Bakelas, and George Mattiampa. Fondazione IRCCS Istituto Nazionale dei Tumori (INT), Italy: Roberto Boffi, Ario Ruprecht, Cinzia De Marco, Alessandro Borgini, Chiara Veronese, Martina Bertoldi, and Andrea Tittarelli. Istituto per lo Studio, la Prevenzione, e la Rete Oncologica (ISPRO), Italy: Giuseppe Gorini, Giulia Carreras, Barbara Cortini, Simona Verdi, Alessio Lachi, and Elisabetta Chellini. Polytechnic University of Cartagena (UPCT), Spain: Ángel López Nicolás, Marta Trapero-Bertran, and Daniel Celdrán Guerrero. European Network on Smoking and Tobacco Prevention (ENSP), Belgium: Cornel Radu-Loghin, Dominick Nguyen, and Polina Starchenko. Hospital Universitario La Princesa (IISP), Spain: Joan B Soriano, Julio Ancochea, Tamara Alonso, María Teresa Pastor, Marta Erro, Ana Roca, Patricia Pérez, and Elena García Castillo.
Statement of Ethics
Study approval was obtained in every country from a local Ethics Committee in each of the 12 countries. Details on the survey characteristics were provided to all participants by suitably qualified professionals through a structured information sheet, and all the participants provided their informed consents, in compliance with the Helsinki Declaration, by ticking the electronic field in the computer-assisted personal interviewing (CAPI) questionnaire. The study protocol was registered at ClinicalTrials.gov (ID: NCT02928536).
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This project has received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No 681040. The work of Silvano Gallus, Chiara Stival, and Alessandra Lugo was partially funded by the Italian League Against Cancer (LILT, Milan). Esteve Fernandez and Olena Tigova are partly supported by the Ministry of Universities and Research, Government of Catalonia (2017SGR319), and thank CERCA Programme Generalitat de Catalunya for the institutional support to IDIBELL.
Author Contributions
Silvano Gallus had the original study idea; Esteve Fernandez, Silvano Gallus, and Alessandra Lugo contributed to the finalization of the survey questionnaire; Chiara Stival and Alessandra Lugo did the statistical analysis; Chiara Stival and Silvano Gallus drafted the article in collaboration with Alessandra Lugo; all other authors made substantial contributions to conception, design, and data interpretation; all the authors approved the final version of the manuscript.
Data Availability Statement
Data are available upon reasonable request. Please see www.TackSHS.eu for the conditions of use and how to request the data.
Supplementary Material
Supplementary data
Acknowledgments
The authors thank Liliane Chatenoud, Tobias Effertz, Filippos T Filippidis, Gergana Geshanova, Sheila Keogan, Hristo Ivanov, José Precioso, Krzysztof Przewozniak, Polina Starchenko, and Vergina K Vyzikidou for help in the preparation, translation, and/or submission of the study protocol to local Ethics Committees.
Funding Statement
This project has received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No 681040. The work of Silvano Gallus, Chiara Stival, and Alessandra Lugo was partially funded by the Italian League Against Cancer (LILT, Milan). Esteve Fernandez and Olena Tigova are partly supported by the Ministry of Universities and Research, Government of Catalonia (2017SGR319), and thank CERCA Programme Generalitat de Catalunya for the institutional support to IDIBELL.
References
- 1.World Health Organization Obesity. 2021. [cited May 2021]. Available from: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/obesity.
- 2.World Health Organization Prevalence of obesity. 2021. [cited June 2021]. Available from: https://www.worldobesity.org/about/about-obesity/prevalence-of-obesity.
- 3.Krzysztoszek J, Laudanska-Krzeminska I, Bronikowski M. Assessment of epidemiological obesity among adults in EU countries. Ann Agric Environ Med. 2019;26((2)):341–349. doi: 10.26444/aaem/97226. [DOI] [PubMed] [Google Scholar]
- 4.Anstey KJ, Cherbuin N, Budge M, Young J. Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obes Rev. 2011;12((5)):e426–37. doi: 10.1111/j.1467-789X.2010.00825.x. [DOI] [PubMed] [Google Scholar]
- 5.Dai H, Alsalhe TA, Chalghaf N, Ricco M, Bragazzi NL, Wu J. The global burden of disease attributable to high body mass index in 195 countries and territories, 1990–2017: an analysis of the Global Burden of Disease Study. PLoS Med. 2020;17((7)):e1003198. doi: 10.1371/journal.pmed.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, et al. Global BMI Mortality Collaboration Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388((10046)):776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janssen F, Bardoutsos A, Vidra N. Obesity prevalence in the long-term future in 18 European countries and in the USA. Obes Facts. 2020;13((5)):514–527. doi: 10.1159/000511023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pineda E, Sanchez-Romero LM, Brown M, Jaccard A, Jewell J, Galea G, et al. Forecasting future trends in obesity across Europe: the value of improving surveillance. Obes Facts. 2018;11((5)):360–371. doi: 10.1159/000492115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization Global NCD target: halt the rise in obesity. 2022. [cited June 2021]. Available from: https://www.who.int/beat-ncds/take-action/policy-brief-halt-obesity.pdf.
- 10.World Obesity Federation Obesity: missing the 2025 global target. Trends, costs and country reports. 2020.
- 11.Gallus S, Lugo A, Murisic B, Bosetti C, Boffetta P, La Vecchia C. Overweight and obesity in 16 European countries. Eur J Nutr. 2015;54((5)):679–689. doi: 10.1007/s00394-014-0746-4. [DOI] [PubMed] [Google Scholar]
- 12.Blundell JE, Baker JL, Boyland E, Blaak E, Charzewska J, de Henauw S, et al. Variations in the prevalence of obesity among European countries, and a consideration of ossible causes. Obes Facts. 2017;10((1)):25–37. doi: 10.1159/000455952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eurostat Overweight and obesity: BMI statistics. 2022. [cited April 2022]. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Overweight_and_obesity_-_BMI_statistics.
- 14.Rose G. Sick individuals and sick populations. Int J Epidemiol. 2001;30((3)):427–432. doi: 10.1093/ije/30.3.427. discussion 433–4. [DOI] [PubMed] [Google Scholar]
- 15.Fernandez E, Lopez MJ, Gallus S, Semple S, Clancy L, Behrakis P, et al. Tackling second-hand exposure to tobacco smoke and aerosols of electronic cigarettes: the TackSHS project protocol. Gac Sanit. 2020;34((1)):77–82. doi: 10.1016/j.gaceta.2019.07.002. [DOI] [PubMed] [Google Scholar]
- 16.Gallus S, Lugo A, Liu X, Behrakis P, Boffi R, Bosetti C, et al. Who smokes in Europe? Data from 12 European countries in the TackSHS survey (2017-2018) J Epidemiol. 2021;31((2)):145–151. doi: 10.2188/jea.JE20190344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370((9596)):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 18.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 19.United Nations Statistics Division UNSD: methodology. 2021. [cited Mar 2021]. Available from: https://unstats.un.org/unsd/methodology/m49/
- 20.Eurostat Eurostat database. 2021. [cited Apr 2021]. Available from: https://ec.europa.eu/eurostat/data/database.
- 21.Marques A, Peralta M, Naia A, Loureiro N, de Matos MG. Prevalence of adult overweight and obesity in 20 European countries, 2014. Eur J Public Health. 2018;28((2)):295–300. doi: 10.1093/eurpub/ckx143. [DOI] [PubMed] [Google Scholar]
- 22.McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- 23.Roskam AJR, Kunst AE, Van Oyen H, Demarest S, Klumbiene J, Regidor E, et al. Comparative appraisal of educational inequalities in overweight and obesity among adults in 19 European countries. Int J Epidemiol. 2010;39((2)):392–404. doi: 10.1093/ije/dyp329. [DOI] [PubMed] [Google Scholar]
- 24.Sanchez-Sanchez ML, Garcia-Vigara A, Hidalgo-Mora JJ, Garcia-Perez MA, Tarin J, Cano A. Mediterranean diet and health: a systematic review of epidemiological studies and intervention trials. Maturitas. 2020;136:25–37. doi: 10.1016/j.maturitas.2020.03.008. [DOI] [PubMed] [Google Scholar]
- 25.Godos J, Zappala G, Bernardini S, Giambini I, Bes-Rastrollo M, Martinez-Gonzalez M. Adherence to the Mediterranean diet is inversely associated with metabolic syndrome occurrence: a meta-analysis of observational studies. Int J Food Sci Nutr. 2017;68((2)):138–148. doi: 10.1080/09637486.2016.1221900. [DOI] [PubMed] [Google Scholar]
- 26.Huo R, Du T, Xu Y, Xu W, Chen X, Sun K, et al. Effects of mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: a meta-analysis. Eur J Clin Nutr. 2015;69((11)):1200–1208. doi: 10.1038/ejcn.2014.243. [DOI] [PubMed] [Google Scholar]
- 27.Davis C, Bryan J, Hodgson J, Murphy K. Definition of the mediterranean diet; a literature review. Nutrients. 2015;7((11)):9139–9153. doi: 10.3390/nu7115459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WHO . Food and health in Europe: a new basis for action. No. 96. WHO Regional Publications European Series; 2004. [PubMed] [Google Scholar]
- 29.Fryar CD, Carroll MD, Afful J. NCHS Health E-Stats; 2020. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. [Google Scholar]
- 30.Ducrot P, Mejean C, Bellisle F, Alles B, Hercberg S, Peneau S. Adherence to the French eating model is inversely associated with overweight and obesity: results from a large sample of French adults. Br J Nutr. 2018;120((2)):231–239. doi: 10.1017/S0007114518000909. [DOI] [PubMed] [Google Scholar]
- 31.Rigotti NA, Clair C. Weight gain after smoking cessation: more data to refute concerns. Eur Heart J. 2018;39((17)):1532–1534. doi: 10.1093/eurheartj/ehy096. [DOI] [PubMed] [Google Scholar]
- 32.Siahpush M, Singh GK, Tibbits M, Pinard CA, Shaikh RA, Yaroch A. It is better to be a fat ex-smoker than a thin smoker: findings from the 1997–2004 National Health Interview Survey-National Death Index linkage study. Tob Control. 2014;23((5)):395–402. doi: 10.1136/tobaccocontrol-2012-050912. [DOI] [PubMed] [Google Scholar]
- 33.Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, et al. GBD 2015 Obesity Collaborators Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377((1)):13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jura M, Kozak LP. Obesity and related consequences to ageing. Age. 2016;38((1)):23. doi: 10.1007/s11357-016-9884-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lin X, Xu Y, Xu J, Pan X, Song X, Shan L, et al. Global burden of noncommunicable disease attributable to high body mass index in 195 countries and territories, 1990–2017. Endocrine. 2020;69((2)):310–320. doi: 10.1007/s12020-020-02352-y. [DOI] [PubMed] [Google Scholar]
- 36.Fernandez E, Chapman S. Quitting smoking and gaining weight: the odd couple. BMJ. 2012;345:e4544. doi: 10.1136/bmj.e4544. [DOI] [PubMed] [Google Scholar]
- 37.ENSP Guidelines for treating tobacco dependence. 2020. [cited July 2020]. Available from: http://ensp.network/wp-content/uploads/2020/10/guidelines_2020_english_forprint.pdf.
- 38.Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8((4)):307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 39.Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr. 2002;5((4)):561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]
- 40.Hodge JM, Shah R, McCullough ML, Gapstur SM, Patel AV. Validation of self-reported height and weight in a large, nationwide cohort of U.S. adults. PLoS One. 2020;15((4)):e0231229. doi: 10.1371/journal.pone.0231229. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Data Availability Statement
Data are available upon reasonable request. Please see www.TackSHS.eu for the conditions of use and how to request the data.